Escolar Documentos
Profissional Documentos
Cultura Documentos
Chapter 12 Monitoring of Surgical Patient
Enviado por
sabina_grapiniDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Chapter 12 Monitoring of Surgical Patient
Enviado por
sabina_grapiniDireitos autorais:
Formatos disponíveis
CHAPTER 12 - Physiologic Monitoring of the Surgical Patient Albert J.
Varon
Orlando C. Kirton Joseph M. Civetta The primary reason for the surgeon's involvement in bedside critical care is the opportunity to understand and enhance the patient's physiologic response and to recogni e and correct the pathophysiologic challenges. To do this effectively! the surgeon must understand physiologic monitoring. "ithout a thorough #no$ledge of the physics and methods of monitoring! ensuring the %uality of numbers obtained! perceiving their importance! and using measurements as a guide for therapy! selection of proper therapy $ould be difficult! $ithout foundation! rote! or naive. Thus there are many stimuli to obtain a fundamental #no$ledge of physiologic monitoring. This chapter is designed to initiate a lifelong process! one that e&tends the capabilities of the surgeon! improves patient outcome! and advances surgical science. '(MO)*+AM,C MO+,TO-,+. The traditional clinical evaluation! usually the initial assessment tool! is often unreliable in critically ill patients! since there may be ma/or changes in cardiovascular function that are not accompanied by obvious clinical findings. ,nvasive hemodynamic monitoring at the bedside provides information about cardiorespiratory performance and guides therapy on a rational physiologic basis. Arterial Catheteri ation ,ndications Arterial catheteri ation is indicated $henever there is a need for continuous monitoring of blood pressure and0or fre%uent sampling of arterial blood. 1tates in $hich precise and continuous blood pressure data are necessary include shoc# of any etiology! acute hypertensive crisis! use of potent vasoactive or inotropic drugs! high levels of respiratory support 2high intrathoracic pressure3! high4ris# patients undergoing e&tensive operations! controlled hypotensive anesthesia! and any situation in $hich any of the factors affecting cardiac function is rapidly changing. This is particularly true in patients $ith shoc#! because indirect measurement of blood pressure by a cuff has been proved inaccurate. 1e%uential analyses of blood gas tensions and p' are necessary in any acute illness involving cardiovascular or respiratory dysfunction or $hen hyperventilation is instituted in patients $ith central nervous system in/uries. An ind$elling arterial catheter also can provide ready access for other blood samples necessary to chart the progression of multisystemic illness. ,nserting arterial lines is a relatively safe and ine&pensive procedure. There are no absolute contraindications to arterial catheteri ation per se! although bleeding diathesis and anticoagulant therapy may increase the ris# of hemorrhagic complications. 1evere occlusive arterial disease $ith distal ischemia! the presence of a vascular prosthesis! and local infection are contraindications to specific sites of catheteri ation. Clinical 5tility "ith an ind$elling arterial catheter and monitoring system! the systolic blood pressure 21673! diastolic blood pressure 2)673! and mean arterial pressure 2MA73 can be displayed continuously. The pulse rate can be calculated from the arterial
tracing $hen the electrocardiogram 2(C.3 is not available 2e.g.! during electrocautery use in surgery3. )irect measurements of arterial pressure correlate rather poorly $ith indirect measurements. The disparities are due in part to physiologic considerations but are largely conditioned by the fre%uency response of the monitoring systems. 6ecause blood pressure trends are probably more important than absolute values! the most important aspect of direct arterial pressure monitoring is that it constantly reminds the clinician to pay attention to the patient! to thin# about $hat is happening! and to reason $hy changes are occurring. To obtain accurate data $hen measuring any pressure $ithin the vascular system! the clinician must understand the monitoring system and methods of calibration. Minor details such as the use of long tubing and the presence of air bubbles or blood clots in the system can ma#e the measurements unreliable. Observation of the arterial pressure $aveform obtained $ith an arterial catheter and monitoring system may permit a %ualitative assessment of the patient's cardiovascular status. The shape of the arterial pressure tracing represents a particular stro#e volume e/ected at a particular state of myocardial contractility. 8ualitative interpretation can be made in a hypovolemic patient $ith a small stro#e volume that $ill create a smaller pressure $ave. As intravascular volume is replenished! the stro#e volume increases! and the arterial pressure tracing $ill increase in si e until it attains normal shape. ,f myocardial contractility is diminished! the rate of increase in aortic pressure $ill diminish! and the upslope of the arterial pressure tracing $ill become less vertical and assume a more tangential tra/ectory $ith the ape& moved to the right. Although %uantitation of stro#e volume has been attempted using computers to solve the e%uations necessary to relate the shape of the peripheral arterial pressure tracing to actual stro#e volume e/ected! critical illness introduces too many variables for this measurement to be reliable. The location of the dicrotic notch on the arterial $aveform also has been advocated as an indicator of the systemic vascular resistance9 ho$ever! .erber and associates $ere unable to demonstrate any statistically significant correlation. Analysis of the 167 variation during mechanical ventilation may offer important information about the nature of lo$4flo$ states. The normal decrease in 167 after a mechanical breath is more pronounced during hypovolemia but practically none&istent during congestive heart failure. 1ites of Catheteri ation Many anatomic sites have been used to access the arterial circulation for continuous monitoring. The superficial temporal! a&illary! brachial! radial! ulnar! femoral! and dorsalis pedis arteries have all been used. Although the selection of anatomic site for arterial catheteri ation usually has an institutional bias! specific advantages and disadvantages should be considered. The dual blood supply to the hand and the superficial location of the vessel ma#e the radial artery the most commonly used site for arterial catheteri ation. Cannulation is technically easy! as is securing the catheter in place! and there is a lo$ incidence of
complications. The mean and end4 diastolic radial pressures are usually accurate estimates of the corresponding aortic pressures9 ho$ever! the systolic pressure at the radial artery is often much higher than that of the aorta due to overshoot caused by the resonant behavior of the radial artery. This e&aggeration is accentuated in stiff! arteriosclerotic radial arteries. Most authors recommend assessing the ade%uacy of collateral circulation before cannulation of the radial artery. The most commonly used test is the modified Allen test. The patient is instructed to elevate one hand! ma#e a fist! and clench it firmly! thus s%uee ing the blood from the vessels of the hand. After the e&aminer compresses at the same time both the radial and ulnar arteries! the patient lo$ers and opens the hand in a rela&ed fashion 2carefully so as not to overe&tend it3. The e&aminer then releases the pressure over the ulnar artery! and the time for return of color is noted. ,t is considered normal if the capillary blush of the hand is complete $ithin : s. Other methods such as ultrasonic )oppler techni%ue! plethysmography! and pulse o&imetry also have been used to assess the ade%uacy of the collateral arterial supply. The a&illary artery has been recommended as suitable for long4term direct arterial pressure monitoring. ,ts use has been associated $ith relatively fe$ complications and no reported permanent se%uelae. The ma/or advantages include its larger si e! freedom for the patient's hand! and close pro&imity to the aorta so that there is better representation of the aortic pressure $aveform and minimal systolic pressure overshoot. 7ulsation and pressure are maintained even in the presence of shoc# $ith mar#ed peripheral vasoconstriction. Also! because of the e&tensive collateral circulation that e&ists bet$een the thyrocervical trun# of the subclavian artery and the subscapular artery 2$hich is a branch of the distal a&illary artery3! thrombosis of the a&illary artery $ill not lead to compromised flo$ in the distal arm. Ma/or disadvantages are its rather deep location and mobility! $hich increase the technical difficulty for insertion! and its location $ithin the neurovascular sheath! $hich may increase the possibility of neurologic compromise if hematoma occurs. The femoral artery also has been used for continuous blood pressure monitoring. Ma/or advantages are its superficial location and large si e! allo$ing easier locali ation and cannulation $hen the pulses over more distal vessels are absent. The ma/or disadvantages are the presence of atherosclerotic occlusive disease in older patients and the problems associated $ith maintaining a clean dressing in the presence of draining abdominal $ounds and ostomies in surgical patients. ;urthermore! bleeding at this site may be difficult to control or may occur in an occult manner into the abdomen or thigh. )espite these potential disadvantages! studies have failed to demonstrate a higher complication rate in patients $ith femoral artery catheters. The dorsalis pedis artery has no significant cannulation ha ards if collateral flo$ can be demonstrated to the remainder of the foot through the posterior tibial artery. This can be done by occluding the dorsalis pedis artery! blanching the great toe by compressing the toenail for several seconds! and then releasing $hile observing return of color. A )oppler techni%ue also can be used. Ma/or disadvantages are its relatively small si e 2$hich ma#es it more difficult to cannulate3 and overestimation of systolic pressure at this level.
The superficial temporal artery has been used e&tensively in infants and in some adults for continuous pressure monitoring. 6ecause of its small si e and tortuousity! ho$ever! surgical e&posure is re%uired for cannulation. ;urthermore! a very small but $orrisome incidence of neurologic complications due to cerebral emboli ation has been reported in infants. The brachial artery is not used often because of the high complication rate associated $ith its use for cardiac catheteri ation. Although this artery has been used successfully for short4term monitoring! there are little data to support the use of prolonged brachial artery monitoring. ,f collateral circulation is inade%uate! obstruction of the brachial artery may be catastrophic! leading to loss of the forearm and hand. Other problems include the difficulty in maintaining the site in a$a#e! active patients and the possibility of hematoma formation in anticoagulated patients. The latter may lead to median nerve compression neuropathy and Vol#mann's contracture. Complications Common problems associated $ith arterial catheteri ation are failure to cannulate! hematoma formation! and disconnection from the monitoring system $ith bleeding. The ma/ority of reports that describe the complications follo$ing radial artery cannulation have stressed the high incidence of early radial artery occlusion and the rarity of late ischemic damage. -ecannulation of the occluded artery generally occurs but may ta#e several $ee#s. The incidence of radial artery thrombosis has declined progressively as a result of the understanding of the effects of different catheter si es 2smaller is better3 and materials 2Teflon is better3 and of the use of continuous heparin flo$ instead of intermittent flushing. ;actors associated $ith an increased ris# of radial artery occlusion include female gender! lo$ cardiac output states! use of vasoconstrictor drugs! severe peripheral vascular disease! small $rist circumference! insertion by surgical cut4do$n! multiple puncture attempts! hematoma formation! and increased duration of cannulation. ,nfections related to arterial catheteri ation also can occur. ;actors associated $ith an increased ris# of infection include placement of the catheter for more than < days! insertion by surgical cut4do$n rather than percutaneously! and local inflammation. The rate of catheter4related infection varies from = to over > percent! but the ris# of catheter4related septicemia is very lo$. Other possible complications include retrograde cerebral emboli ation 2$hen flushing catheters3! arteriovenous fistulas! and pseudoaneurysm formation. ;inally! inadvertent in/ection of vasoactive drugs or other agents into an artery can cause severe pain! distal ischemia! and tissue necrosis. Central Venous Catheteri ation ,ndications The most common indications for central venous catheteri ation are to secure access for fluid therapy! drug infusions! or parenteral nutrition and for central venous pressure 2CV73 monitoring. Central venous catheters also have been used to aspirate air in case of embolism during neurosurgical procedures in the sitting position! for placement of cardiac pacema#ers or inferior vena cava filters! and for hemodialysis access.
There are no absolute contraindications for CV7 catheter placement! although bleeding diatheses may increase the ris# of hemorrhagic complications. Vessel thrombosis! local infection or inflammation! and distortion by trauma or previous surgery are considered contraindications to specific sites of catheteri ation. Clinical 5tility "hile central venous lines are placed primarily for venous access! useful information occasionally can be obtained by measuring the CV7. The CV7 may be useful in a hypotensive trauma patient to differentiate a pericardial tamponade from hypovolemia. Analysis of the CV7 tracing also may be helpful in the differential diagnosis of certain cardiac arrhythmias 2a $aves are absent in atrial fibrillation3 and in the diagnosis of tricuspid insufficiency 2prominent v $aves3. A properly placed catheter can be used to measure right atrial pressure! $hich! in the absence of tricuspid valve disease! $ill reflect the right ventricular end4diastolic pressure. CV7! therefore! can give information about the relationship bet$een intravascular volume and right ventricular function but cannot be used to assess either of these factors independently. CV7 cannot be used to assess left ventricular function in critically ill patients because ventricular disparity and independence of right and left atrial pressures have been confirmed repeatedly in these patients. ;urthermore! CV7 is only a single parameter! in contradistinction to the more complete information concerning pressures! flo$! and venous gas measurements available $ith pulmonary artery catheters. "hen monitoring CV7! the catheter should be attached to a pressure transducer for electronic measurement rather than to a $ater manometer. "ater manometry does not permit visuali ation of the pressure tracing and cannot provide reliable measurements because of the fre%uency4response limitations of a fluid4filled column that cannot respond to the full range of pressure variations. 1ites of Catheteri ation There are many anatomic routes to obtain access to the central venous circulation. The most commonly chosen sites include the subclavian! internal /ugular! e&ternal /ugular! femoral! and brachiocephalic veins. The patient's anatomy and the operator's e&perience are the ma/or factors influencing site selection. The subclavian vein can be cannulated $ith a high rate of success and may be the easiest to cannulate in situations of profound volume depletion. Another advantage of this approach is the ease $ith $hich the catheter and the dressings can be secured. )isadvantages include the higher ris# of pneumothora& and the inability to compress the vessel if bleeding occurs. The internal /ugular vein has been cannulated $ith success rates similar to those of the subclavian approach. The ma/or advantages of internal /ugular vein catheteri ation are the lo$er ris# of pneumothora& and the ability to compress the insertion site if bleeding occurs. ,n addition! the right internal /ugular vein provides a straight path to the superior vena cava! facilitating placement of catheters and pacema#ers. The internal /ugular vein! ho$ever! may be more difficult to cannulate in patients $ith volume depletion or shoc#. ;i&ation and dressing of catheters are also more difficult.
Cannulation of the e&ternal /ugular vein has a lo$er incidence of complications but a higher incidence of failure. 1ince catheters inserted through the nec# are more difficult to fi& and dress than those in other sites! this approach is not suitable for prolonged central venous access. Although some authors have reported no higher incidence of complications from femoral cannulation than from subclavian or internal /ugular sites! concerns over the ris# of infection and thrombosis continue to limit general acceptance of long4term femoral cannulation in critically ill patients. Other peripheral veins! such as those in the antecubital fossa! have been used for central venous access! but the high incidence of thrombophlebitis and the fact that many catheters cannot be passed into the central venous circulation ma#e these routes undesirable in critically ill patients. Complications Complications can be divided into technical or mechanical complications! usually occurring during catheter placement! and long4term complications related to the length of time that the catheter remains in place. The list of technical and mechanical complications is truly impressive? catheter malposition! dysrhythmias! emboli ation 2air or catheter fragments3! vascular in/ury 2hematoma! vessel laceration! false aneurysm! or arteriovenous fistula3! cardiac in/ury 2atrial or ventricular perforation or cardiac tamponade3! pleural in/ury 2pneumothora&! hemothora&! or hydrothora&3! mediastinal in/ury 2hydromediastinum or hemomediastinum3! neurologic in/ury 2phrenic nerve! brachial ple&us! or recurrent laryngeal nerve3! and in/ury to other structures 2trachea! thyroid! or thoracic duct3. 7neumothora& is the most fre%uently reported immediate complication of subclavian vein catheteri ation! and arterial puncture is the most common immediate complication of internal /ugular vein cannulation. The literature suggests that serious mechanical complications of central venous catheteri ation! although e&tremely rare! are associated $ith a high mortality rate. @ong4term complications related to the length of time the catheter is in place are due to infection or thrombosis. +or$ood and associates studied triple4lumen catheter infections in septic and nonseptic critically ill surgical patients. They found no catheter4related infections or instances of septicemia in the nonseptic patients! but the incidence of catheter4related infection in the septic group $as A:.B percent! $ith a >.: percent incidence of septicemia. The catheter infection rate per C== days! ho$ever! $as only =.> for both septic and nonseptic patients combined! $hich is very similar to rates previously published for single4lumen catheters. 1urface4modified central venous catheters have been developed to reduce catheter4related infection. Catheters impregnated $ith silver sulfadia ine and chlorhe&idine resist bacterial adherence and biofilm formation. These catheters have been reported to have a significantly lo$er proportion of catheter4related infection compared $ith standard catheters. At least three types of thrombi can develop in patients $ith central venous catheters? mural thrombus! catheter thrombus! and Dfibrin sleeveE or sleeve thrombus. Any of these thrombi may brea# loose spontaneously or may be set loose $hen the catheter is removed. .enerally! ho$ever! symptoms or clinical conse%uences do not occur. 1uperior vena cava syndrome does occur! especially in long4term patients $ho have had many catheters placed.
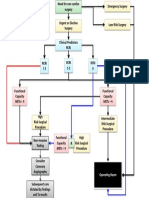
7ulmonary Artery Catheteri ation ,ndications 1everal studies in critically ill patients have sho$n that the clinical assessment is inaccurate in predicting cardiac output! pulmonary artery occlusion pressure! and systemic vascular resistance and that the information obtained from pulmonary artery catheteri ation prompts a change in therapy in <= to := percent of patients. Although the pulmonary artery catheter permits a more accurate hemodynamic assessment and therapy may be modified as a result! this does not prove that #no$ledge of these data and alteration of the therapy improve overall patient outcome. 1ome studies indicate that preoperative invasive hemodynamic monitoring and cardiac function optimi ation in high4ris# patients are associated $ith reduced intraoperative and postoperative cardiac complications and decreased mortality. "hile there are not enough carefully designed studies to definitely establish the benefit of hemodynamic monitoring to the individual patient! it is reasonable to assume that more precise bedside #no$ledge of fundamental cardiovascular parameters $ould facilitate earlier diagnosis and guide therapy. "hether morbidity can be decreased and overall survival can be improved also depend on the patient's overall response! not /ust on improved cardiovascular function! and thus should not be considered a necessary re%uirement for initiating invasive monitoring. ,n general! a pulmonary artery catheter is indicated $henever the data obtained $ill improve therapeutic decision ma#ing $ithout unnecessary ris#. Table CA4C represents the indications most often noted in the medical literature. Variables that are particularly important in assessing benefit versus ris# of perioperative use of a pulmonary artery catheter include disease severity! magnitude of anticipated surgery and fluid shifts! and practice setting. There are no specific contraindications to pulmonary artery catheteri ation! but the same cautions as those attached to central venous access apply. Clinical 5tility The pulmonary artery catheter has provided a D%uantum leapE in the physiologic information available for the management of critically ill patients. The information that can be obtained includes CV7! pulmonary artery diastolic pressure 27A)73! pulmonary arterial systolic pressure 27A173! mean pulmonary artery pressure 2M7A73! pulmonary artery occlusion 2 D$edge E3 pressure 27AO73! cardiac output 2CO3 by thermodilution! mi&ed venous blood gases by intermittent sampling! and continuous mi&ed venous o&imetry. On the basis of this information! a multitude of derived parameters also can be obtained 2see belo$3. "hen the pulmonary artery catheter balloon is inflated 2C.F m@3! the blood flo$ in a distal segment of the pulmonary artery is occluded! creating a conduit through $hich left atrial pressure 2@A73 can be measured 2;ig. CA4C A3. ,n a tubular system! flo$ can only be created if there is a pressure differential at both e&tremes. ,f there is no pressure differential! flo$ cannot be present. 5sing this principle in reverse! a stagnant system in $hich no for$ard flo$ is present $ould permit an accurate measurement of a distal pressure from a pro&imal location 2see ;ig. CA4C 63. ,n fact! simultaneous 7AO7 and @A7 measurements in patients have validated this principle. The 7AO7 is a reliable inde& of the @A7 even in the presence of elevated pulmonary vascular resistance. Although the 7A)7 also has been used as an inde& of @A7! it is
not as reliable as the 7AO7! particularly if there is tachycardia or increased pulmonary vascular resistance. The 7AO7 represents the @A7 as long as the column of blood distal to the pulmonary artery catheter tip is patent to the left atrium. This may not be so if the catheter is positioned in an area of the lung $here the alveolar pressure e&ceeds pulmonary venous pressure 2 one A! as described by "est3 2;ig. CA4A3 or both pulmonary artery and venous pressures 2"est's one C3! causing intermittent or continous collapse of the pulmonary capillaries. The 7AO7 may then reflect alveolar pressure and not @A7. This is particularly important if patients have lo$ pulmonary vascular pressures 2i.e.! hypovolemia3 and0or are treated $ith high levels of positive end4 e&piratory pressure 27((73. ;ortunately! since the pulmonary artery catheter is flo$4directed! it is most li#ely to pass into dependent areas of the lung $here blood flo$ is high and both pulmonary artery and venous pressures e&ceed alveolar pressure 2"est's one B3. ,n this location! the continuous column of blood bet$een the distal lumen of the catheter and the left atrium $ill remain patent! and the 7AO7 $ill reflect @A7. Another factor favoring appropriate catheter position is that $hen the patient is supine! the volume of lung located above the heart and the hydrostatic gradient favoring the formation of ones C and A are decreased. ,f there is any doubt! a lateral chest &4ray can be used to determine the location of the catheter tip in relation to the left atrium. ,f the tip of the catheter is belo$ this chamber! one B conditions $ill e&ist even if high levels of 7((7 are used. ,n the absence of mitral valve disease or premature mitral valve closure due to aortic regurgitation! the @A7 reflects the left ventricular end4diastolic pressure 2@V()73. ,f there are no alterations in left ventricular compliance 2the relationship bet$een pressure and volume3! @V()7 $ill reflect left ventricular end4diastolic volume 2@V()V3. ,n the intact ventricle! @V()V reflects the end4diastolic stretch of the muscle fiber! $hich represents the true preload 2discussed later3. -aising intrathoracic pressure introduces an artifact that affects all intrathoracic vascular pressures to an e&tent that depends on the state of pulmonary compliance. ,n patients $ith acute respiratory insufficiency! compliance is often diminished! and the DstiffE lungs do not transmit alveolar pressure as readily to the pulmonary circulation. ,n these patients! the 7((7 artifact on the 7AO7 measurement usually should not e&ceed C mm'g for every F cm'AO of 7((7 applied. A greater discrepancy can be seen if the patient is hypovolemic or if the catheter is malpositioned as described above. Another method of evaluating the effects of 7((7 on the 7AO7 measurement is to observe the decrement in 7AO7 $hen 7((7 is briefly removed. 7resumably! this decrement remains relatively constant and can be subtracted from subse%uent pressure measurements. Although removal of 7((7 may decrease arterial o&ygen tension and increase physiologic shunt! these changes are rapidly reversible. ,f a physician believes that the 7AO7 should be measured off 7((7! this probably should be done $hen 7((7 is discontinued for other reasons 2suctioning or changing breathing circuits3! and increased concentrations of o&ygen should be given before and after 7((7 is stopped. 7atients $ho are receiving very high levels of 7((7 or $hose condition deteriorates $hen 7((7 is discontinued 2such as immediate bradycardia3 should not have 7((7 removed for the e&clusive purpose of measuring 7AO7.
1ince intravascular pressure measurements are affected by the intrathoracic pressure changes during respiration! they should be performed at end4e&piration and obtained from a calibrated strip4chart recorder or oscilloscope rather than from a digital display. Most digital displays are inaccurate because the unselective nature of time4 based electrical sampling and averaging includes positive and negative breathing artifacts. The digital average then contains the very respiratory variations that can be e&cluded by visuali ing the tracing and selecting the appropriate value. The cardiac output is measured by the thermodilution techni%ue! $hich correlates $ell $ith both the ;ic# and the dye dilution methods. Thermodilution represents an application of the indicator dilution principle in $hich a change in the heat content of the blood is induced at one point in the circulation! and the resulting change in temperature is detected at a point do$nstream. This change is produced by a rapid in/ection of a #no$n volume of fluid at a #no$n temperature 2colder than the body3 into the right atrium via the pro&imal port of the pulmonary artery catheter. The change in temperature is registered by a thermistor located < cm from the catheter tip. This lo$ered temperature decreases the electrical resistance of the thermistor and results in a thermodilution curve. The measurement of CO is based on a modification of the 1te$art4 'amilton e%uation? C@,CK '(-( ;O- (85AT,O+ The variables in the formula are essentially fi&ed before in/ection! e&cept for the denominator. The denominator of the e%uation is the thermodilution curve produced by in/ection of the indicator. A computer integrates the area under this curve! and the resulting calculation is displayed as the cardiac output in liters per minute. The area under the curve is inversely proportional to the CO9 that is! the larger the area under the curve! the lo$er is the CO. ,n actuality! right ventricular output is being measured? ,n the absence of intracardiac shunting! right and left ventricular cardiac outputs are e%uivalent. The in/ectate solution can be either FG de&trose in $ater or normal saline. A volume of C= m@ of iced or room4temperature in/ectate is recommended. The in/ection should be smooth! completed $ithin < s! and timed $ith a specific phase of the respiratory cycleHi.e.! in/ecting at pea# inspiration or end4e&halationHrather than randomly. The measurement protocol should be consistent! and three measurements should be averaged! since a single measurement is not reliable. ,f for any reason the fluid bolus cannot be in/ected through the atrial port of the catheter 2e.g.! obstructed lumen3! it can be administered through the venous infusion port! the right ventricular port! or the introducer side port. 7itfalls in cardiac output measurement include in/ectate temperature different from the temperature used to determine the computer constant or that of the fluid being monitored by the reference probe! delivered volume less than the one entered in the computation constant! incorrect computer constant! rapid infusion of intravenous fluids during measurements! electrical noise created by electrocautery! faulty catheter lumens! improperly positioned catheter 2e.g.! if the catheter is in the $edge position or
if the pro&imal lumen is above the atrium or $ithin the introducer sheath3! and presence of intracardiac shunts or tricuspid regurgitation. A continuous thermodilution techni%ue is no$ available for measuring CO. 7ulmonary artery catheters are modified to locate a C=4cm thermal filament in the right ventricle during use. "ithout using any fluid in/ectate! the thermal filament continually transfers a safe level of heat directly into the blood in a random on4off fashion. The resulting temperature changes are detected at the distal thermistor located in the pulmonary artery. These data are collected by a computer! $hich then applies a comple& formula to cross4correlate the temperature changes $ith the heat4 input se%uence to produce the familiar thermodilution curve. CO is then computed from the area under the curve by using an e%uation similar to the one used for standard bolus thermodilution. The continuous CO monitoring techni%ue has been reported to be accurate and safe in critically ill patients. 7ulmonary artery catheters e%uipped $ith rapid4response thermistors and (C. electrodes have permitted the measurement of right ventricular e/ection fraction at the bedside9 ho$ever! the clinical utility of these systems remains unclear. Catheter ,nsertion The most commonly used pulmonary artery catheter is a I ;r CC=4cm catheter $ith a distal pulmonary artery lumen! a pro&imal lumen B= cm from the tip! a lumen for inflation of the balloon located at the catheter tip! and a thermistor for measurement of cardiac output by the thermodilution method 2;ig. CA4B3. +e$er catheters may contain an additional lumen for fluid administration or for passing a pacing electrode! fiberoptic bundles for continuous measurement of the o&ygen saturation of mi&ed venous hemoglobin 21VOA3! or a rapid4response thermistor to measure right ventricular e/ection fraction. 7reparation of the electronic monitoring e%uipment and testing of the catheter components before insertion are essential because the displayed tracing is used to locali e the position of the catheter tip during insertion. The pressure transducer must be calibrated and eroed to the level of the left atrium. The catheter should be tested before insertion by 2C3 flushing the pro&imal and distal lumens to ensure that they are patent! 2A3 inflating the balloon 2C.F m@3 to detect asymmetry or lea#s! 2B3 testing the thermistor by connecting it to the cardiac output computer! and 2<3 sha#ing the catheter tip to verify that a tracing can be obtained on the oscilloscope. Access to the central venous circulation for insertion of a pulmonary artery catheter is the same as for placement of a CV7 catheter. Once an introducer sheath is in place! the pulmonary artery catheter is inserted and advanced until the tip reaches an intrathoracic vein 2as evidenced by respiratory variations on the pressure tracing3. The balloon is then inflated $ith C.F m@ of air and the catheter advanced $hile the operator observes both the pressure $aveform and the (C. tracing. After the right atrium is entered! the catheter is advanced through the right ventricle and into the pulmonary artery until a 7AO7 tracing is obtained 2;ig. CA4<3. Maneuvers often used to facilitate passage through the pulmonary valve include elevation of the head of the bed! turning the patient into the right lateral decubitus position! performance of the Valsalva maneuver! and increasing ventricular e/ection in lo$4output states by the administration of inotropic drugs. To determine if the catheter is in the $edge
position! the $aveform needs to be inspected. The mean 7AO7 should be lo$er than the M7A7 and lo$er than or e%ual to the 7A)7. ,n the $edged position! arteriali ed blood can be aspirated! or 1VOA $ill increase to systemic arterial levels or above if an o&imetric pulmonary artery catheter is used. The latter is not an absolute criterion because incomplete arteriali ation of the sample can occur if the tip of the pulmonary artery catheter lies $edged in a lo$ ventilation4 perfusion region. Complications There are ris#s to pulmonary artery catheteri ation! although they are typically infre%uent and not usually life4threatening. ,n addition to the complications attributed to central venous cannulation! complications can occur during passage or after the catheter is in place. The most common complication during passage of the pulmonary artery catheter is the development of dysrhythmias. They can occur in up to F= percent of patients! but less than C percent of these are serious. The incidence of malignant dysrhythmias during catheteri ation seems to be lo$er $hen patients are in the head4up and right lateral tilt position. Transient right bundle branch bloc# 2-6663 has been reported in B to : percent of catheteri ations. 6ecause of the rare but grave conse%uences of -666 in patients $ith pree&isting left bundle branch bloc#! the use of standby e&ternal pacema#ers and e%uipment for transvenous pacema#er insertion has been recommended in these patients during catheteri ation. Coiling! looping! or #notting in the right ventricle can occur during catheter insertion. This can be avoided if no more than C= cm of catheter is inserted after a ventricular tracing is visuali ed and before a pulmonary artery tracing appears. Aberrant catheter location! such as pleural! pericardial! peritoneal! aortic! vertebral artery! renal vein! and inferior vena cava! also have been reported. Complications that can occur after the catheter is in place include infections! thromboembolism! and rupture of the pulmonary artery. ,nfections from pulmonary artery catheters are directly related to the length and severity of illness. The incidence of microbial coloni ation of the catheter has been reported to be bet$een F.> and A>.C percent! but only = to <.: percent of catheters produce catheter4related bacteremia. Asymptomatic thrombotic complications are fre%uent! but symptomatic complications attributable to such thrombi are rare. 7ulmonary infarction can occur due to emboli! distal migration of the pulmonary artery catheter tip! or prolonged balloon inflation occluding distal blood flo$ in the pulmonary artery. 7ulmonary artery rupture and hemorrhage are the most serious of all the pulmonary artery catheter complications and are more li#ely in patients $ith pulmonary hypertension and in the elderly. -ecurrent hemorrhage from a pulmonary artery pseudoaneurysm secondary to pulmonary artery catheterJinduced perforation also can occur. Complications related to the peripheral migration of the catheter tip can be limited by continuous monitoring of the pulmonary artery tracing! avoiding prolonged balloon inflation! ensuring pro&imal catheter placement by revie$ of daily &4rays! and the use of continuous heparin flush systems. "henever the balloon is inflated! the tracing must be observed. ,nflation must be stopped instantly $hen the $aveform changes. ,f the catheter tip has drifted distally and is in a smaller artery! inflation $ith the usual C.F m@ of air may be too much and may rupture the thin4$alled pulmonary artery. Other complications that can occur after the catheter is in place include thrombocytopenia! cardiac valve in/uries! catheter fracture! and balloon rupture.
,n addition to the complications associated $ith catheter insertion and use! complications can result from delays in treatment due to time4consuming insertion problems and from inappropriate treatment based on erroneous information or erroneous data interpretation. Complications of pulmonary artery catheteri ation can be minimi ed by meticulous attention to detail and by careful evaluation of the data obtained. )erived 'emodynamic 7arameters ,n addition to the information directly provided by arterial and pulmonary artery catheteri ation! many parameters can be calculated. The derived hemodynamic parameters 2Table CA4A3 aid the clinician by %uantitating the relationships among heart rate! filling pressures! resistance! contractility! and cardiac output. Cardiac output 2CO3 is the sum of all stro#e volumes e/ected in a given time. ,t is usually represented as the product of average stro#e volume and heart rate 2beats per minute3! $here stro#e volume is the amount of blood e/ected by the heart $ith each contraction. The primary determinants of stro#e volume are the ventricular preload! afterload! and contractility. 7reload is the passive load that establishes the initial muscle length of the cardiac fibers before contraction and therefore is not usually measured directly in critically ill patients. On the basis of the $or# by Otto ;ran# and others! 1tarling described the relationship bet$een the resting fiber length of the myocardium and ventricular $or#. As resting fiber length increases! there is an increase in $or# performed on subse%uent contraction. 6eyond a certain point! ho$ever! further increases in fiber length $ill not increase e&ternal mechanical $or#! and $or# may decreaseHa description of cardiac failure. The end4diastolic fiber length is proportional to the end4 diastolic volume. ,f there is no change in ventricular compliance 2the relationship bet$een pressure and volume3! @V()V is proportional to @V()7. 6ecause in most clinical circumstances the 7AO7 provides a reliable measure of @V()7! changes in 7AO7 fre%uently are used as an estimate of changes in left ventricular preload. ,n critically ill patients! ho$ever! changes in ventricular compliance may affect the relationship bet$een @V()7 and @V()V. Therefore! caution should be ta#en in interpretation of the 7AO7 as the sole measure of left ventricular preload. ,n clinical practice! /udgments concerning preload ade%uacy are often best made empirically! by observing the responses of 7AO7 and indices of cardiac performance to a rapid alteration of intravascular volume. The second determinant of stro#e volume is afterload. Afterload is the sum of all the loads against $hich the myocardial fibers must shorten during systole! including the aortic impedance! the arterial $all resistance! the peripheral vascular resistance! the mass of blood in the aorta and great arteries! the viscosity of the blood! and the end4 diastolic volume of the ventricle. ,n the clinical setting! the most commonly used measure of ventricular afterload is the peripheral or systemic vascular resistance 21V-3. Changes in 1V- usually reflect either altered blood viscosity or a change in the radius of the vascular circuit. 1V-! ho$ever! does not necessarily reflect left ventricular loading conditions! since the true measure of ventricular afterload must consider the interaction of factors internal and e&ternal to the myocardium. Although it is not physiologically correct to spea# of afterload in terms of 1V-! it is clinically
useful to relate changes in 1V- to changes in ventricular afterload. 1ince sympathetic control of the circulation mediated by peripheral baroreceptors is designed to maintain blood pressure $ithin relatively narro$ limits! cardiac output is inversely proportional to 1V- $henever this control is functioning. ,n the human circulatory system! ho$ever! additional factors are so often present that this relationship should not be assumed to be a substitute for direct measurements and repeated calculations. Contractility! the final determinant of stro#e volume! may be estimated in the laboratory by the ma&imum velocity of contraction of the cardiac muscle fibers. At the bedside! $e only have inferences based on the stro#e $or# performed by the ventricle as filling pressure 2DpreloadE3 changes. 7lotting the $or# done by the ventricle for each beatHthe left ventircular stro#e $or# inde& 2@V1",3 or right ventricular stro#e $or# inde& 2-V1",3Hagainst an estimate of preload and comparing that point $ith a normal range may be a useful means of assessing overall ventricular function 2;ig. CA4F3. An up$ard shift to the left has been interpreted as an improvement in ventricular performance. A shift do$n$ard and to the right has been considered as a declining ventricular performance. The Dventricular function curvesE are influenced by changes in ventricular afterload and compliance and therefore do not reflect true contractility. At present! the method for assessing myocardial contractility most $idely considered load4 independent is the end4systolic pressure4 volume relationship 2(17V-3. The logistical difficulty of obtaining fre%uent ventricular volume measurements in the intensive care unit 2,C53 limits the clinical usefulness of this method. Thus plotting 7AO7 and stro#e $or# against normal curves is an appropriate use of data currently available in the ,C5! but the underlying physiology is often better understood if it is considered in terms of the ventricular pressure4volume relation. An appreciation of the determinants of stro#e volume provides a rational approach in the management of patients $ith lo$4perfusion states. The first and most common intervention used to increase stro#e volume is to increase preload by augmentation of intravascular volume. The level of 7AO7 that corresponds to optimal left ventricular preload can be determined only by se%uentially assessing the effects of acute hemodynamic interventions on cardiac function and may vary over time in any particular patient. ;luid can be administered rapidly in predetermined increments $hile changes in 7AO7 and in the indices of cardiac performance are monitored. A ma/or increase in 7AO7 during infusion suggests poor ventricular compliance! e&hausted preload reserve! and increased ris# of pulmonary edema $ith further volume loading. ,f the 7AO7 rises modestly! if indices of cardiac performance improve! and if 7AO7 returns to $ithin several millimeters of mercury of the original value $ithin C= min of stopping the infusion! additional fluid can be given $ithout high ris# of e&acerbating pulmonary venous congestion. After a brief observation period! this se%uence can be repeated until the hemodynamic parameters are ade%uate or the 7AO7 sho$s an unacceptable rise. ,f tissue perfusion remains inade%uate after volume optimi ation! augmentation of stro#e volume may be accomplished by increasing myocardial contractility $ith inotropic drugs and0or decreasing ventricular afterload $ith vasodilators. 1ome authors have reported reduced complications and improved survival in perioperative patients $hen hemodynamic therapy $as aimed at augmenting rather than simply normali ing hemodynamic and o&ygen4 transport parameters. -ecent studies! ho$ever! found no advantage to the use of supranormal target values in a general population of critically ill patients.
-(17,-ATO-* MO+,TO-,+. Monitoring ventilation and gas e&change in critically ill surgical patients is of particular importance in deciding if mechanical ventilation is indicated! assessing response to therapy! optimi ing ventilator management! and deciding if a $eaning trial is indicated. ,n addition! gas monitoring permits an assessment of the ade%uacy of o&ygen transport and calculation of derived parameters. Ventilation Monitoring @ung Volumes 1everal lung volume measurements are useful for monitoring ventilatory function in the operating room and ,C5. These include tidal volume! vital capacity! minute volume! and dead space. Tidal volume 2VT3 is defined as the volume of air moved in or out of the lungs in any single breath. ,f the tidal volume is depressed! the patient may have difficulty in both o&ygenation and ventilation. -apid! shallo$ breathing! as reflected by the respiratory fre%uency 2f3 to tidal volume ratio 2f0VT K C==3! is an accurate predictor of failure! and its absence 2f0VT L M=3 is an accurate predictor of success! in $eaning patients from mechanical ventilation. VT can be measured at the bedside using a hand4held spirometer 2"right respirometer3. 6ecause moisture impairs its performance! the instrument is most appropriate for intermittent monitoring. Continuous VT monitoring is facilitated by the presence of pneumotachometers in the breathing circuit of modern ventilators. ,n order to obtain accurate VT measurements! the spirometer must be located bet$een the ventilator * piece and the endotracheal tube. ,f the spirometer is instead positioned on the e&piratory limb of the breathing circuit! the entire VT delivered by a ventilator! not that actually received by the patient! is measured. 5nder conditions of decreased lung compliance or increased air$ay resistance! the higher pea# inspiratory pressure 27,73 $ould result in an increase of gas volume compressed in the breathing circuit! $ith correspondingly less delivered to the patient. The product of 7,7 2cm'AO3 N F 2m@0cm'AO3 provides an estimate of the compression volume of most circuits. Vital capacity 2VC3 is defined as the ma&imal e&piration follo$ing a ma&imal inspiration. ,t can be readily measured at the bedside in a manner similar to the one used for VT. The VC is reduced in diseases involving the respiratory muscles or their neural path$ays! in obstructive and restrictive ventilatory impairment! and in patients $ho fail to cooperate fully. VC is normally :F to IF m@0#g! and a value of C= m@0#g or greater is commonly considered a favorable predictor of $eaning outcome. This value! ho$ever! is %uite dependent on patient cooperation! and its predictive po$er is rather poor. Minute volume 2or total ventilation3 2V2dot3 (3 is the total volume of air leaving the lung each minute 2product of VT and f3. Many ventilators display V2dot3 (! or it can be measured $ith a "right spirometer. An increase in the minute volume re%uired to maintain a normal arterial blood carbon dio&ide tension 27aCOA3 suggests an increased dead space relative to VT or an abnormally high carbon dio&ide 2COA3 production. A resting V2dot3 ( of less than C= @ and the ability to double the resting V2dot3 ( on command have been associated $ith successful $eaning from mechanical ventilation.
The physiologic 2or effective! or total3 dead space 2V)3 is the portion of tidal volume that does not participate in gas e&change. 7hysiologic dead space may be divided into t$o components? the volume of gas $ithin the conducting air$ays 2the anatomic dead space3 and the volume of gas $ithin unperfused alveoli 2the alveolar dead space3. The ratio of physiologic dead space to tidal volume 2V)0VT3 is calculated from the (nghoff e%uation 2modified from the 6ohr e%uation3 as follo$s? V) 0 VT O 7aCOA 4 7(COA 0 7aCOA $here 7(COA is the mean partial pressure of e&haled COA in the total e&haled volume of gas after thorough mi&ing. +ormally! e&haled gas is collected in a bag over B min and the 7(COA COA is measured from the bag. The 7(COA COA should not be confused $ith 7etCOA! the partial pressure of end4tidal COA 2discussed later3. The V)0VTratio provides a useful e&pression of the efficiency of ventilation. ,n healthy sub/ects! the ratio is bet$een =.BB and =.<F. The V)0VTratio is increased in a number of disease states associated $ith regions of the lung possessing high ventilation4 perfusion ratios! such as adult respiratory distress syndrome! emphysema! pulmonary embolism! shoc# $ith lo$ cardiac output! and the employment of positive4pressure ventilation $ith high VT or e&cessive 2more than is needed3 7((7. 7atients $hose V)0VTe&ceeds =.: are usually not $eanable from ventilatory support. 6y measuring V2dot3 ( and calculating V)0VT! the alveolar 2or effective3 ventilation 2V2dot3 A3 also may be calculated? V2dot3 A O V2dot3 ( 4 2V2dot3 ( N V)0VT3 7ulmonary Mechanics Various respiratory mechanical parameters also can be monitored in the operating room and ,C5. These include ma&imal inspiratory pressure! static compliance! dynamic characteristic! and $or# of breathing. ,nspiratory force is measured as the ma&imal pressure belo$ atmospheric that a patient can e&ert against an occluded air$ay. The measurement re%uires a connector to an endotracheal or tracheostomy tube and a manometer capable of registering negative pressure. A ma&imal inspiratory pressure 27ima&3 value more negative than 4A= to AF cm'AO has been used as one of the clinical parameters to confirm recovery from neuromuscular bloc# after general anesthesia. 7ima&values more negative than 4B= cm'AO have been used to predict successful $eaning from mechanical ventilation. 1tudies have found that 7ima& has limited po$er in predicting $eaning outcome! especially in patients receiving prolonged mechanical ventilation. These findings may be due in part to the fact that 7ima& assesses only the strength of the respiratory muscle pump $ithout ta#ing into account the demands placed on it. Compliance! a measure of the elastic properties of the lung and chest $all! is e&pressed as a change in volume divided by a change in pressure 2)V0)73. ,n patients receiving mechanical ventilation! a rough measure of total thoracic compliance 2both the lungs and chest $all3 can be obtained by dividing the delivered VT by the inflation pressure displayed on the ventilator gauge during conditions of ero gas flo$. These can be achieved by using the Dinspiratory holdE option on the ventilator! during $hich period the air$ay pressure falls to a plateau. ,f the patient is receiving
7((7! this must be first subtracted from the plateau pressure before calculating static thoracic compliance! that is! 1tatic compliance O volume delivered 0 plateau pressure 4 7((7 The usual range for adult patients receiving mechanical ventilation is := to C== m@0cm'AO. )ecreased values are observed $ith disorders of the thoracic cage or a reduction in the number of functioning lung units 2resection! bronchial intubation! pneumothora&! pneumonia! atelectasis! or pulmonary edema3. "hen the static compliance is less than AF m@0cm'AO! as in severe respiratory failure! difficulties in $eaning are common because of the increased $or# of breathing 2see belo$3. The dynamic characteristic is calculated by dividing the volume delivered by the pea# 2rather than the plateau3 air$ay pressure minus 7((7. ,t is not correct to call this value dynamic compliance because it is actually an impedance measurement and includes compliance and resistance components. The dynamic characteristic is normally about F= to M= m@0cm'AO. ,t may be decreased by disorders of the air$ays! lung parenchyma! or chest $all9 if it decreases to a greater e&tent than the static compliance! it suggests an increase in air$ay resistance 2e.g.! bronchospasm! mucous plugging! #in#ing of the endotracheal tube3 or an e&cessive flo$ rate. "or# of breathing! $hich relates to the product of the change in pressure and volume! is a measure of the process of overcoming the elastic and frictional forces of the lung and chest $all. The $or# of breathing in the critically ill patient $ho re%uires ventilatory support 2"O67t3 can be divided into three components? normal physiologic $or# 2"O67hys3! $or# to overcome the pathophysiologic changes in the lung and chest $all 2"O6)is3! and $or# to overcome the imposed $or# of breathing 2"O6,mp3 created by our methods of ventilatory support. The sum is total $or#. 7hysiologic $or# of breathing consists of three elements? elastic $or#! flo$4resistive $or#! and inertial $or#. (lastic $or# is the $or# necessary to overcome the elastic forces of the lung and is inversely proportional to the compliance of the lung. ,f compliance becomes diminished! the $or# of breathing increases dramatically. The second element of physiologic $or# is flo$4resistive $or#! or the $or# that is needed to overcome the resistance of the air$ays and parenchymal tissues. This may increase the pressure change necessary to inhale the same tidal volume but also adds another component of $or# during e&piration! that necessary to e&pel the gas from the lungs through the narro$ air$ays. The third component of physiologic $or# is the inertial $or# to overcome the tendency of gas volume to remain at rest. This element is negligible in comparison $ith the elastic and flo$4 resistive $or#. "hen a patient develops respiratory failure! in addition to the normal physiologic $or#! the patient must overcome the increased $or# of breathing associated $ith the disease. This is clinically manifest as a change from a relatively large tidal volume at a slo$ rate to a small tidal volume at a rapid rate. ;inally! the patient must do additional $or# to breath spontaneously against a breathing apparatus that consists of the ventilator itself! demand valve! tubing! e&halation valves! and most important! the endotracheal tube. 6anner and associates sho$ed that the endotracheal tube acts as a resistor in series in the breathing apparatus! thereby causing an increase in $or# of breathing. ,mposed $or# has been sho$n to e&ceed physiologic $or# of breathing by a factor of : under conditions of spontaneous breathing through a narro$4internal4diameter endotracheal tube at a high inspiratory flo$ rate demand during continuous positive
air$ay pressure. 7oor demand system sensitivity! ventilator dyssynchrony! malfunctioning demand valves! and inade%uate inspiratory flo$s are also contributing factors. The goal of ventilatory support is to carefully titrate the ventilator's contribution to minute ventilation so that the patient's effort remains a nonfatiguing $or# load. ;ailure to do so by supplying either too much or too little ventilatory support may result in unsuccessful $eaning trials and increase the duration of mechanical ventilation. +ormal range for "O67t is =.B to =.:J0@. Microprocessor4based respiratory monitors such as the C74C== 7ulmonary Monitor 26iocore Monitoring 1ystems! ,rvine! CA3 measure many mechanical ventilation and respiratory muscle parameters! including compliance! air$ay resistance! strength and endurance! and both patient and ventilator $or# of breathing. 7hysiologic data are accrued from a miniature pneumotachograph and air$ay pressure sensor positioned bet$een the * piece of the breathing circuit tubing and the endotracheal tube. A catheter $ith a distally annealed balloon is positioned in the distal esophagus to measure changes in intraesophageal pressure as an estimate of changes in intrathoracic pressure. "e have employed this pulmonary monitor to evaluate une&plained tachypnea or respiratory distress! to guide endurance and strength reconditioning! and to avoid iatrogenic ventilator dependency caused by inappropriate ventilator settings in comple& long4term ventilated patients. ,ncorporation of $or#4of4breathing analysis into our pree&tubation trial allo$ed successful e&tubation in >I 2of FM>3 patients $ho remained on mechanical ventilation because of tachypnea 2respiratory rate bet$een BA and FA breaths per minute3 secondary to e&cessive imposed $or# of breathing. (arlier e&tubation in this group of patients resulted in a pro/ected net savings in e&cess of PA>A!===. ,ncorporating $or#4 of4 breathing strategies also decreased the duration of ventilation in our trauma ,C5 from M.M to <.A days. .as Monitoring 6lood4.as Analysis 6lood4gas measurements provide information about the efficiency of gas e&change! the ade%uacy of alveolar ventilation! and the acid4base status. 6lood gas values are usually reported in terms of directly measured partial pressures 27OA or 7COA3 and calculated hemoglobin o&ygen saturations 21OA3. Calculated 1OA values are derived from the measured partial pressure and a nomogram of the o&yhemoglobin dissociation curve usually corrected for blood temperature! p'! and perhaps other factors. 6ecause these assumptions may not be accurate in critically ill patients! actual measurements of 1OA by coo&imetry are preferred. 1OA also can be measured continuously by using pulse o&imeters or pulmonary artery catheters that incorporate o&imetric fibers 2see belo$3. Arterial blood gas tensions are determined by the composition of the alveolar gas and the efficiency of gas transfer bet$een the alveoli and pulmonary capillary blood. Alveolar gas tensions depend on the mi&ture of inspired gas! ventilation! and blood flo$ in the lungs9 the matching of ventilation and perfusion9 and the composition of mi&ed venous blood gases. 7athophysiologic causes of arterial hypo&emia include ventilation4 perfusion ine%uality or venous admi&ture from regional alveolar
hypoventilation! true intrapulmonary or intracardiac shunt! and decreased mi&ed venous o&ygen content. Although diffusion abnormalities may lead to hypo&emia if pulmonary end4capillary blood fails to e%uilibrate fully $ith alveolar gas! such conditions are uncommon. A decreased cardiac output in the presence of a constant o&ygen consumption! an increased o&ygen consumption in the presence of a constant CO! and a decreased CO and an increased o&ygen consumption must all result in a lo$er mi&ed venous o&ygen content and therefore also can produce arterial hypo&emia. ;ailure to recogni e this nonpulmonary cause of hypo&emia may cause a clinician to falsely attribute a decreasing arterial blood o&ygen tension 27aOA3 to deteriorating pulmonary function. Thus pulmonary and cardiac function must be assessed to evaluate any given set of arterial blood gases accurately. A decreasing 7aOA $ithout a change in 7aCOAsuggests that blood o&ygenation is deteriorating despite constant alveolar ventilation. ,n the acutely ill patient! this finding is usually attributable to ventilation4 perfusion imbalance or intrapulmonary shunting. An important feature of shunting is that as it increases! supplemental o&ygen has progressively less effect on 7aOA because shunted blood bypasses ventilated alveoli. ,ntrapulmonary shunting usually does not result in elevation of the 7aCOA because the central chemoreceptors sense any rise in 7aCOA and respond by increasing ventilation. The relation of 7OA to 1OA is described by the o&yhemoglobin dissociation curve 2;ig. CA4:3. The flat upper portion of the dissociation curve means that even if the 7OA in alveolar gas decreases some$hat! loading of o&ygen $ill be little affected. The steep lo$er part of the curve means that the peripheral tissues can $ithdra$ large amounts of o&ygen for only a small decrease in capillary 7OA. The curve shifts as the affinity of hemoglobin for o&ygen changes. A shift to the right 2decreased affinity for o&ygen3 helps release o&ygen into the tissue. A shift to the left 2increased affinity for o&ygen3 causes less o&ygen to be available to tissue. The curve can be shifted to the right by increased erythrocyte A!B4diphosphoglycerate concentration! temperature! 7COA! and concentration of hydrogen ion 2decreased p'3. Opposite changes shift it to the left. Other conditions such as carbo&yhemoglobinemia and methemoglobinemia also can shift the o&yhemoglobin dissociation curve to the left and therefore interfere $ith peripheral o&ygen unloading. The position of the o&yhemoglobin dissociation curve is defined by the 7F=! that is! the 7OA at $hich hemoglobin is F= percent saturated. +ormal hemoglobin has a 7F= of A:.F mm'g. "hen it is greater than this value! the curve is shifted to the right9 $hen it is lo$er! the curve is shifted to the left. )espite a considerable amount of information! there is little evidence that shifts of the o&yhemoglobin dissociation curve are clinically significant in the ma/ority of patients. ,ndividuals $ith limited circulatory reserve! ho$ever! $ho cannot augment o&ygen delivery by the usual compensatory mechanisms of increased cardiac output and organ blood flo$! may develop local tissue hypo&ia $hen an increased hemoglobin4 o&ygen affinity state 2i.e.! al#alemia3 e&ists. The 7aCOA directly reflects the ade%uacy $ith $hich alveolar ventilation meets metabolic demands for COA e&cretion. The relationship bet$een 7aCOA! COAproduction 2V2dot3 COA3! and alveolar ventilation 2V2dot3 A3 in normal lungs is given by the e%uation 7aCOA O V2dot3 COA 0 V2dot3 A N K
$here K is a constant. ,n diseased lungs! the denominator V2dot3 A in this e%uation is less than the ventilation going to the alveoli because of alveolar dead space! that is! unperfused alveoli or those $ith high ventilation4 perfusion ratios. ;or this reason! the denominator is sometimes referred to as the effective alveolar ventilation. An increased 7aCOA 2hypercapnia3 reflects the failure of the ventilatory system to eliminate the COA produced during metabolism. This Dventilatory failureE is traditionally described as respiratory acidosis. 'ypercapnia can occur because of hypoventilation 2i.e.! C+1 depression3! increased COA production 2e.g.! hyperthermia! hyperthyroidism3! or increased physiologic dead space resulting in inade%uate alveolar ventilation. The mechanisms of hypocapnia are the reverse of those $hich produce hypercapnia! the most common being hyperventilation 2respiratory al#alosis3. The o&ygen tension of mi&ed venous blood 27VOA3 and the o&ygen saturation of mi&ed venous hemoglobin 21VOA3 provide valuable diagnostic information and are necessary for the calculation of various parameters! such as arteriovenous o&ygen content difference! intrapulmonary shunt! and o&ygen consumption. Mi&ed venous blood is the mi&ture of all blood that has traversed the capillary beds capable of e&tracting o&ygen. This venous effluent is thoroughly mi&ed! so its o&ygen content is a flo$4 $eighted representation of all the end4capillary contents of the body and as such $ill reflect the total body balance bet$een o&ygen delivery and o&ygen consumption of perfused tissues. The mi&ed venous o&ygen content 2and therefore 1VOA3 is determined by the variables in the ;ic# e%uation 2see section on Continuous Mi&ed Venous O&imetry3. The 7VOA is determined by the same factors and the position of the o&yhemoglobin dissociation curve. ,n critically ill patients! sampling of mi&ed venous blood can be performed accurately only in the pulmonary artery. 1ampling techni%ue is important9 blood should be $ithdra$n from the most pro&imal pulmonary artery location possible and at a very slo$ rate. A fast rate of blood $ithdra$al or a malpositioned catheter 2distal migration or $edging3 may cause a falsely elevated 7VOA and 1VOA. This is due to DcontaminationE of the mi&ed venous blood $ith arteriali ed pulmonary capillary blood and should be suspected if the COA tension of mi&ed venous blood 27VCOA3 is e%ual to or lo$er than a simultaneously determined 7aCOA. 7roper sample handling before arterial or venous blood4gas analysis is a prere%uisite to accurate blood gas measurement. The t$o principal re%uirements are that the sample be obtained under strict anaerobic conditions and immediately placed on ice until analy ed. 6ecause room air has a partial pressure of o&ygen 27OA3 of about CF= mm'g and a partial pressure of carbon dio&ide 27COA3 of essentially ero! e%uilibration of a blood sample $ith air bubbles may significantly alter the results. 7lacement of the sample on ice is necessary to reduce the metabolic rate of the red blood cells and prevent continued o&ygen consumption and COA production if analysis is to be delayed beyond CF to A= min. The addition of e&cessive heparin also $ill alter the results! and therefore! after aspiration! the heparin in the syringe should be e&pelled! leaving only the heparin $etting the barrel. Alternatively! a commercially available syringe containing dry heparin can be used. 6ecause blood gas values can change rapidly in critically ill patients! intermittent sampling for blood4gas analysis might miss significant changes. Advances in fiberoptic and microprocessor technology have been combined $ith fluorescent dye
chemistry to develop miniaturi ed intravascular gas sensors that permit continuous measurement of p'! 7OA! and 7COA. The performance of fiberoptic continuous intraarterial blood gas monitors is comparable $ith that of modern blood gas analy ers. ;urther studies are needed! ho$ever! to determine the clinical utility of this ne$ methodology. 7arameters )erived from 6lood4.as Analysis Just as the derived hemodynamic parameters can be used to evaluate the choice and effects of hemodynamic interventions! parameters derived from blood4gas analysis 2Table CA4B3 yield information about the ade%uacy of cardiopulmonary function in meeting the tissue demands for o&ygen. The o&ygen content of the blood is e%ual to the amount of o&ygen bound to hemoglobin plus the amount dissolved in plasma. The amount of bound o&ygen is directly related to the concentration of hemoglobin and to ho$ saturated this hemoglobin is $ith o&ygen 2i.e.! 1aOA or 1VOA3. The amount of o&ygen dissolved in plasma depends on the o&ygen tension 2i.e.! 7aOA or 7VOA3. O&ygen delivery 2OA3 is the volume of o&ygen delivered from the heart each minute and is calculated as the product of cardiac output and arterial o&ygen content 2CaOA3. O&ygen consumption 2V2dot3 OA3 is the amount of o&ygen that diffuses from the capillaries into all tissues and can be calculated according to the ;ic# principle as the product of CO and arteriovenous o&ygen content difference QC2a 4 7V3OAR. ,f this e%uation is rearranged! the arteriovenous o&ygen content difference relates o&ygen consumption and CO 2V2dot3 OA0CO3. An increase in the arteriovenous o&ygen content difference indicates that either consumption is too high or flo$ is too lo$. ;inally! the o&ygen utili ation coefficient or e&traction ratio 2OA5C3! relates o&ygen consumption and o&ygen delivery 2V2dot3 OA0OA3. This parameter has been used in many ,C5s to evaluate the ade%uacy of o&ygen transport. The ade%uacy of o&ygen transport also must be assessed in relation to o&ygen demand! $hich is the amount of o&ygen re%uired by the body tissues to use aerobic metabolism. Although o&ygen demand cannot be measured clinically! the relative balance bet$een consumption and demand is best indicated by the presence of e&cess lactate in the blood. @actic acidosis means that demand e&ceeds consumption and anaerobic metabolism is present. Although precise numerical end points cannot be defined! the parameters already listed provide a frame$or# for testing a clinical hypothesis? ,f o&ygen delivery or consumption is lo$! if utili ation is high! or if lactic acidosis is present! arterial o&ygen content might be augmented by increasing hemoglobin concentration or o&ygen saturation! or cardiac output might be increased by manipulation of preload! afterload! or contractility. A response might be considered beneficial if o&ygen consumption increases! if utili ation returns to the normal range! or if lactic acidosis resolves. 7hysiologic right4to4left shunt or venous admi&ture 2sp0t3 estimates the fraction of total blood flo$ reaching the left side of the circulation $ithout participating in gas e&change. 1hunt may occur 2uncommonly3 in adults via intracardiac shunts. More commonly! increased venous admi&ture in critically ill patients is due to alterations in the balance of pulmonary ventilation and perfusion 2lung areas that are perfused but
not ventilated3. 6efore calculating venous admi&ture! it is necessary to calculate arterial! mi&ed venous! and pulmonary end4capillary o&ygen contents. The latter can be calculated by using the alveolar o&ygen tension 27aOA3 to estimate pulmonary end4 capillary o&ygen tension and the o&yhemoglobin dissociation curve to estimate pulmonary end4capillary hemoglobin saturation 2assume C==G if 7aOA K CF= mm'g3 2see Table CA4B3. Other indices! such as the alveolar4arterial o&ygen partial pressure difference 27aOA 4 7aOA3 and the arterial4to4alveolar o&ygen tension ratio 27aOA07aOA3! have been suggested for evaluating the efficiency of gas e&change. These o&ygen tensionJbased indices! ho$ever! are inaccurate in predicting efficiency of gas e&change. The relationship bet$een physiologic shunt and the o&ygen tensionJbased indices is nonlinear and substantially influenced by changes in inspired o&ygen concentration and arteriovenous o&ygen content difference. The collection of the measured and derived cardiopulmonary parameters has been called the cardiopulmonary profile. +ormal values can be seen in Tables CA4A and CA4 B. The measured and derived data can be used to formulate a plan of interventions designed to improve o&ygen delivery relative to myocardial and systemic needs. This analysis is a dynamic process that evolves as ne$ data are obtained and response to therapy is incorporated. The process of generating a cardiopulmonary profile has been greatly simplified by the use of programmable calculators and microcomputers. Capnography Capnography is the graphic display of COAconcentration as a $aveform. ,t should not be confused $ith capnometry! $hich refers to only the numerical presentation of the concentration $ithout a $aveform. Capnography includes capnometry $hen the capnographic display is calibrated. Currently available systems for COAanalysis include infrared spectroscopy! mass spectrometry! and -aman scattering. ,n addition! a disposable! noninvasive! and ine&pensive colorimetric device 2(asy Cap9 +ellcor 7uritan 6ennett! ,nc.! 7leasanton! CA3 is available. This device permits a semi%uantitative measurement of the end4tidal COA concentration $hen it is attached bet$een an endotracheal tube and a resuscitation bag. ,n the ma/ority of stand4alone capnographs! the COAconcentration is measured by infrared spectroscopy. A beam of infrared light is passed through the sampled gas. COA molecules in the light path absorb some of the infrared energy. The capnograph compares the amount of infrared light absorbed by the patient gas in the sample cell $ith the amount absorbed either by gas in a reference cell or by the sample cell during a time of #no$n ero4gas concentration. The capnograph then displays the instantaneous COA concentration. .as for analysis of COA may be aspirated from the air$ay 2sidestream capnography3 or may be analy ed as it flo$s through a sensor placed in the air$ay 2mainstream capnography3. 1idestream analy ers offer advantages in that gas is sampled close to the patient's mouth $ith the use of an ine&pensive! light$eight connector! and they can be used in nonintubated patients. The ma/or disadvantage of these systems is that analysis is delayed because gas is routed through a capillary tube to the capnograph.
Mainstream analy ers generate a capnogram practically instantaneously because the gas is analy ed as it passes through a sampling cuvette. The ma/or disadvantage of these systems is the $eight of the sensor and sampling cuvette. 6ecause the sensor itself is a sophisticated instrument! it needs to be treated carefully? ,t is fragile! and replacements are e&pensive. The volume of the cuvette adds dead space to the system. +ormally! there is a fairly predictable relationship bet$een the pea# e&haled or end4 tidal COA 27etCOA3 and the 7aCOA. ,n healthy sub/ects $ith normal lungs! the 7aCOA is < to : mm'g higher than the 7etCOA. 7atients $ith chronic obstructive lung disease and other derangements associated $ith increased dead space 2see section on @ung Volumes3 have an increased arterial to end4tidal COA gradient Q72a 4 et3COAR. This difference occurs because the e&haled gas from the alveolar dead space! $hich contains little or no COA! dilutes the COA4containing gas from the normally ventilated and perfused alveoli. Measurement of 7etCOA and 72a 4 et3COAprovides insight into several normal and pathologic processes. 7etCOAmeasurement is at present perhaps one of the most reliable means of determining proper endotracheal tube placement. (sophageal intubation may produce one or a fe$ breaths containing COA during e&piration! but because there is no COA in the stomach cavity! 7etCOA rapidly decreases to ero. 7etCOA has been found to correlate $ith cardiac output and coronary perfusion pressure during cardiopulmonary resuscitation 2C7-3 and $ith successful resuscitation from and survival after cardiac arrest. 6ecause circulatory arrest creates total dead space! if ventilation is continued! 7etCOA disappears. An increase in 7etCOAprovides an immediate bedside validation of the efficacy of C7-! and if the increase is abrupt! it provides the earliest evidence of successful resuscitation. The use of 7etCOA to monitor resuscitation is predicated on maintaining a constant minute ventilation so that changes in 7etCOAresult from changes in lung perfusion 2and therefore cardiac output3 and not ventilation. 7etCOA monitoring is e&tremely useful as a diagnostic tool in several situations uni%ue to the operating room. These include the detection of air emboli during neurosurgical procedures re%uiring the sitting position! the detection of increased COA production in malignant hyperthermia! and the detection of disconnection or malfunction of the anesthesia breathing circuit. ,n the ,C5 environment! 7etCOA monitoring also can be used as a ventilator disconnect alarm as $ell as a system to determine ventilator malfunction. Measurement of 7etCOA has been proposed as a substitute for arterial blood gas sampling during mechanical ventilation ad/ustment and $eaning in critically ill patients. 7etCOAtrends in these patients! ho$ever! are often misleading because the 72a 4 et3COAvaries greatly in a single individual. The 72a 4 et3COA is primarily a reflection of dead4space ventilation! and its si e can serve as a gauge of physiologic aberration. ;actors related to the instrumentation and the techni%ue used! ho$ever! also may contribute to the 72a 4 et3COA. ;or e&le! aspiration of room air through a loose connection or brea# in the circuit or sampling
tube! a lea# around the cuff! or aspiration of fresh gases $ill dilute the e&haled COA and result in an increased 72a 4 et3COA and an altered $aveform. Analysis of the COA $aveform can provide valuable information. A detailed revie$ of $aveform analysis is outside the scope of this chapter but can be found else$here 2.ravenstein and associates3. 7ulse O&imetry 7ulse o&imetry provides a reliable! real4time estimation of arterial hemoglobin o&ygen saturation. This noninvasive monitoring techni%ue has gained clinical acceptance in the operating room! recovery room! and ,C5. 7ulse o&imeters estimate arterial hemoglobin saturation by measuring the absorbance of light transmitted through $ell4perfused tissue! such as the finger or ear. The light absorbance is measured at t$o $avelengthsH::= 2red3 and ><= nm 2infrared3Hto distinguish bet$een t$o species of hemoglobinHo&yhemoglobin and deo&yhemoglobin. O&yhemoglobin absorbs less red light than deo&yhemoglobin! accounting for its red color9 at infrared $avelengths! the opposite is true 2;ig. CA4I3. @ight absorbances at both $avelengths have t$o components? the pulsatile 2or ac3 component! $hich is attributed to the pulsating arterial blood! and the baseline 2or dc3 component! $hich represents the absorbances of the tissue bed! including venous blood! capillary blood! and nonpulsatile arterial blood 2;ig. CA4M3. The pulse o&imeter first determines the ac components of absorbance at each $avelength and divides this by the corresponding dc component to obtain a pulse4added absorbance that is independent of the incident light intensity. ,t then calculates the ratio 2-3 of these pulse4added absorbances? - O AC::=0)C::= 0 AC><=0)C><= The ratio of the pulse4added absorbances at the t$o $avelengths is used to generate the o&imeter's estimate of arterial saturation 21pOA3. The relationship bet$een this ratio and 1pOA is empirical. The algorithm $as created by measuring pulse4added absorbances in healthy! a$a#e volunteers breathing hypo&ic gas mi&tures. These absorbances $ere then correlated $ith actual 1aOA as determined by a laboratory co4 o&imeter. ,n practice! pulse o&imeters use t$o light4emitting diodes 2@()s3 and one photodiode as transmitting and sensing transducers! usually placed on opposite sides of a digit. The microprocessor of the pulse o&imeter is programmed to distinguish arterial pulse $aveforms9 minimi e the effects of ambient light! patient motion! and electrocautery9 and vary the intensity of transmitted light re%uired to obtain the $aveforms. ,n most studies of pulse o&imetry accuracy! data have been collected only $hen the pulse o&imeter heart rate e%ualed the (C. heart rate. ,t has been assumed that this is a necessary condition for accuracy because it implies that the pulse o&imeter is detecting pulses produced by heartbeats. Most manufacturers claim that their pulse o&imeters are accurate $ithin SA percent 21)3 from I= to C== percent saturation. Although pulse o&imetry may provide erroneous measurements $hen 1aOA is less than I= percent! these values occur %uite rarely 2or should occur %uite rarely3 in patients! because 7aOA $ould be less than <=
mm'g. 1aOAvalues in the range of perhaps I= to >F percent $ill reflect changes in 7aOA9 it is in this range that pulse o&imetry finds great value in monitoring cardiorespiratory disease and directing therapy. 'igh levels of saturation give no information about 7aOA. 6ecause of the sigmoid shape of the o&yhemoglobin dissociation curve 2see ;ig. CA4:3! 1aOA may not decrease despite a significant deterioration in pulmonary gas e&change! i.e.! if 7aOA fell from A== to C== mm'g. 1ince delivery of o&ygen to the tissues is proportional to 1aOA! ho$ever! pulse o&imeters $ill detect changes before tissue o&ygenation is impaired. Various physiologic and environmental factors interfere $ith the accuracy of pulse o&imetry. These include decreased amplitude of peripheral pulses 2hypovolemia! hypotension! hypothermia! vasoconstrictor infusions3! motion artifact! electrosurgical interference! bac#scatter from ambient light! and dyshemoglobinemias. 7redictors of pulse o&imeter data failure in the operating room include A1A physical status B! <! or F9 cardiac! vascular! and orthopedic surgery9 hypotension9 hypertension9 and duration of procedure. The pulse o&imeter can only distinguish o&yhemoglobin and deo&yhemoglobin. ,f other hemoglobin species are present! an error is introduced. @aboratory co4o&imeters! on the other hand! generally use more than t$o $avelengths and often can %uantify other hemoglobin species directly. "hen dyshemoglobins such as carbo&yhemoglobin and methemoglobin can be measured! it becomes meaningful to distinguish bet$een functional saturation QC== N o&yhemoglobin02o&yhemoglobin T deo&yhemoglobin3R and fractional saturation QC== N o&yhemoglobin02o&yhemoglobin T deo&yhemoglobin T carbo&yhemoglobin T methemoglobin3R. 6ar#er and colleagues have sho$n that in the presence of elevated carbo&yhemoglobin or methemoglobin levels! 1pOA overestimates fractional saturation at all saturation values. Carbo&yhemoglobinemia may occur in heavy smo#ers or in patients $ho suffer carbon mono&ide inhalation. Methemoglobinemia may be induced by a large number of drugs! including local anesthetics 2prilocaine! ben ocaine3! nitroglycerin! phenacetin! phenytoin! 7yridium! and sulfonamides. ,ntravenously administered dyes! particularly methylene blue and indocyanine green! can temporarily induce artifactually lo$ saturation readings. )eeply pigmented s#in and opa%ue nail polish coatings may significantly decrease light transmission! rendering o&imeters inoperative. The presence of fetal hemoglobin! hyperbilirubinemia! or moderate anemia 2$ith hematocrits as lo$ as CF percent3 does not affect the accuracy of pulse o&imeters. )espite its limitations! pulse o&imetry is generally ac#no$ledged as one of the most significant advances in clinical monitoring. Continuous Mi&ed Venous O&imetry Measurement of the o&ygen saturation of mi&ed venous hemoglobin 21VOA3 is helpful in the assessment of the o&ygen supply4demand relationship in critically ill patients. The use of improved fiberoptic o&imetry systems in conventional pulmonary artery catheters has permitted continuous monitoring of 1VOA and made bedside monitoring of this relationship practical. 1VOA can be derived from the ;ic# e%uation 2see Table CA4B3 that relates o&ygen consumption! cardiac output! and arteriovenous o&ygen content difference. ,f the
small %uantity of physically dissolved o&ygen in the blood is considered negligible! solving the ;ic# e%uation for 1VOAyields 1VOA O 1aOA 4 V2dot3 OA 0 CO N 'b N C.B> N C= Therefore! the determinants of 1VOAinclude the principal components of o&ygen delivery QCO! hemoglobin 2'b3! and 1aOAR and o&ygen consumption. There is a poor correlation bet$een 1VOA and any single component of the e%uation 2V2dot3 OA! CO! 1aOA! 'b3! as $ould be e&pected! because there are four separate determinants. There is! ho$ever! a good correlation bet$een 1VOA and all these components acting at once. "ith the preceding formula in mind! it is easy to understand that the 1VOA $ill decrease $hen there is an imbalance bet$een o&ygen consumption and delivery caused by an increase in V2dot3 OA or a decrease in CO! 'b! or 1aOA. 1VOA $ill increase $hen the imbalance is due to changes in the opposite direction. The normal range for 1VOA in healthy sub/ects is =.:F to =.M=! $ith an average value of =.IF corresponding to a 7VOA of <= mm'g at a normal p' of I.<. A rapid or prolonged fall from the normal range is indicative of a significant deterioration in the patient's clinical condition. Values belo$ the normal range may be associated $ith increased o&ygen consumption due to fever! shivering! sei ures! e&ercise! and agitation or associated $ith decreased o&ygen delivery due to lo$ cardiac output! anemia! or arterial hemoglobin desaturation. Values of about =.FB correspond to a 7VOA of about AM mm'g9 values at or belo$ this level often have been associated $ith anaerobic metabolism! lactic acidosis! and death. Asti and colleagues! ho$ever! $ere unable to identify the critical level of 1VOAassociated $ith lactic acidosis in patients $ith sepsis or acute myocardial infarction. Values above the normal range indicate an increase in o&ygen delivery relative to consumption and are associated $ith the hyperdynamic phase of sepsis! cirrhosis! peripheral left4to4right shunting! general anesthesia 2$hen V2dot3 OA is lo$3! cellular poisoning such as cyanide to&icity 2rare3! mar#ed arterial hypero&ia! or a technical malfunction of the system 2e.g.! $edged catheter3. +ormal or high 1VOA values do not ensure that the o&ygen supply4demand balance is satisfactory because accurate interpretation assumes intact and consistent vasoregulation! $hich is not the case in some disease states 2e.g.! sepsis3. 7ulmonary artery catheter o&imetry differs from pulse o&imetry in several $ays. ;irst! the pulmonary artery catheter measures reflected rather than transmitted light. 1econd! being immersed in blood! the pulmonary artery catheter has no need for the pulse4 added signal analysis used by the pulse o&imeter. ;inally! one of these catheters! the Opticath 2Abbott Critical Care 1ystems! Mountain Vie$! CA3 uses three $avelengths 2:I=! I==! and M== nm3 rather than the t$o $avelengths 2::= and ><= nm3 employed by most pulse o&imeters. The O&imetri& B 1ystem used by the Opticath has three light4emitting diodes 2@()s3 contained in an optical module that provide the light sources for the three selected $avelengths. @ight from each of these diodes is se%uentially transmitted through a single optical fiber to illuminate the blood flo$ing past the catheter tip. This
illuminating light is absorbed! refracted! and reflected depending on the color and! therefore! o&yhemoglobin concentration of the blood. The reflected light is collected by a second fiber and returned through the catheter to a photodetector in the optical module 2;ig. CA4>3. 5sing the relative intensities of the signals representing the light levels at the various $avelengths! a computer calculates the o&ygen saturation! and the average for the preceding F s is displayed. The saturation measured by catheter o&imetry correlates $ell $ith values obtained from a laboratory co4o&imeter. The most common sources of error $hen measuring 1vOA are incorrect calibration and catheter malposition. Carbo&yhemoglobinemia! methemoglobinemia! and intravenous administration of methylene blue also can affect the measurements. Continuous 1VOA monitoring serves three ma/or functions. ;irst! it serves as an indicator of the ade%uacy of the o&ygen supply4demand balance of perfused tissues. ,n clinically stable patients! a normal and stable 1VOA may be considered an additional assurance of cardiopulmonary stability. ;urther assessments of cardiac output and arterial and mi&ed venous blood gas analyses are not necessary. 1econd! continuously measured 1VOA may function as an early $arning signal of unto$ard events. ,n this situation! although an alert has been given! the cause of the change in 1VOA is not necessarily clear because the change in 1VOA is sensitive but not specific. ,t may be necessary to measure cardiac output! 1aOA! and 'b in this setting to identify the etiology of the 1VOAchange. Third! continuously monitored 1VOA may improve the efficiency of the delivery of critical care by providing immediate feedbac# as to the effectiveness of therapeutic interventions aimed at improving o&ygen transport balance. ;inally! an important application of continuous venous o&imetry must be one of cost containment in the ,C5. The potential of cost savings lies in the decreased use of other modes for assessing o&ygen transport balance! e.g.! cardiac output measurements and venous blood gas analyses. The savings in some institutions are greater than the price of the catheter! and its use has been /udged cost4effective. .A1T-,C TO+OM(T-* .eneral Considerations ,schemia signifies failure to satisfy the metabolic needs of the cell secondary to either impaired o&ygen delivery or impaired cellular o&ygen e&traction and utili ation. Although hemodynamic and o&ygen4transport variables document the severity of tissue hypo&ia and o&ygen debt! they fail to accurately portray the comple& interactions bet$een energy re%uirements and supplies at the tissue level. .astric tonometry has been proposed as a relatively noninvasive monitor of the ade%uacy of aerobic metabolism in organs $hose superficial mucosal lining is e&tremely vulnerable to lo$ flo$ and hypo&emia and in $hich blood flo$ is sacrificed first in both shoc# and the systemic inflammatory response syndrome. The gastrointestinal tract therefore $ill display metabolic changes before other indices of o&ygen utili ation. ,n the ano&ic cell! uncompensated adenosine triphosphate 2AT73 hydrolysis is associated $ith the intracellular accumulation of adenosine diphosphate 2A)73! inorganic phosphate! and hydrogen ions $ith resulting intracellular acidosis. These hydrogen ions lead to tissue acidosis! $ith unbound hydrogen ions combining
$ith interstitial bicarbonate to form the $ea# acid carbonic acid that dissociates to produce COA and $ater. Measurements A tonometer is comprised of a semipermeable balloon connected to a sampling tube. A dual4purpose productHa tonometer in combination $ith a standard vented gastric sumpHis commercially available 2T-,7 +.1 Catheter9 Tonometrics )ivision! ,nstrumentarium Corp.! Te$#sbury! MA3. The annealed balloon allo$s COA generated in the superficial layers of the mucosa to e%uilibrate $ithin the saline instilled into the balloon. The tonometer 7COA is multiplied by an e%uilibration factor 2based on the e%uilibration period3 to derive the tissue 7COAvalue. 5sing a modified version of the 'enderson4'asselbach e%uation! intramucosal p' 2p'i3 is then calculated as follo$s? p'i O :.C T logC= 'CO4 B 0 =.=B N 7COA ss $here 'CO4 B represents the arterial bicarbonate concentration 2from a contemporary sample of arterial blood3 in millie%uivalents per liter! 7CO Ass represents the tonometrically measured steady4state carbon dio&ide tension! and =.=B represents a constant that converts carbon dio&ide tension in plasma in millie%uivalents per liter per millimeter of mercury to millie%uivalents per liter of carbonic acid. The measurement of intramucosal p' depends also on the assumption that the bicarbonate concentration in the $all of the organ is the same as that $hich is delivered to it by arterial blood and that the pK 2the dissociation constant3 is the same as that in the plasma. The pK in plasma is not the same as that in the cytosol! but the value :.C is the best appro&imation of the pK $ithin the interstitial fluid of the superficial layers of the mucosa. Clinical 5tility ,ncomplete splanchnic cellular resuscitation has been associated $ith the development of multiple organ system failure! more fre%uent septic complications! and increased mortality in the critically ill patient. Many studies have demonstrated the utility of gut tonometry in various settings $here the perfusion status of the intestinal mucosa has been of importance! such as in patients undergoing elective cardiac or abdominal aortic operations. ,n critically ill patients! gastric tonometry has been used as a predictor of both organ dysfunction and mortality and has been sho$n to be a better predictor of mortality than base deficit! lactate! o&ygen delivery! and o&ygen consumption. ;ailure of splanchnic resuscitation correlated $ith multiple organ system failure and increased length of ,C5 stay in the hemodynamically unstable trauma patient admitted to the ,C5 at the 5niversity of Miami0Jac#son Memorial 'ospital. The relative ris# or li#elihood of death among incompletely resuscitated patients 2p'i L I.BA3 at A< h as compared $ith completely resusciated patients 2p'i U I.BA3 $as <.F. ,n parallel! the relative ris# of developing multiple organ system failure $as F.< in patients $ith p'i L I.BA. ,n a subse%uent audit! $e evaluated consecutive patients $ho met state trauma triage criteria! $ho $ere admitted to the -yder Trauma Center at Jac#son Memorial 'ospital! and $ho had a nasogastric tube placed during resuscitation. The trauma patients /udged after clinical evaluation to have minimal in/ury and $ho $ere treated
in routine care areas $ere found to have a normal p'i on transfer from the resuscitation area. The mean p'i $as I.< S =.CC! KI.A in >F percent of patients and KI.AF in MM percent of patients. All patients survived9 none developed multiple organ system failure. Measurement of p'i can provide clinicians $ith a metabolic end point of resuscitation. p'i therefore can be used to ensure the completion of resuscitation as /udged by normali ation of gastric p'i. Current methods reported in the literature focus only on increasing o&ygen delivery using fluid therapy and vasoactive agents $ith a4adrenergic action. 6ecause these induce splanchnic vasoconstriction! $hich leads to gastric intramucosal acidosis! our strategy employs splanchnic vasodilatory agents to optimi e systemic and mesenteric blood flo$ 2isoproterenol! dobutamine! nitroprusside! nitroglycerine! prostaglandin (C3! reserving those agents $hich cause splanchnic vasoconstriction 2epinephrine! high4dose dopamine! phenylephrine! norepinephrine3 to treat severe hypotension 2MA7 L FF mm'g3. ,f p'i falls une&pectedly! $e search for intraabdominal catastrophe! intraabdominal hypertension! sepsis! tissue necrosis! line sepsis! nosocomial infection! unappreciated e&cess patient ventilatory $or#! hypovolemia! and hypo&emia. ,nterventions to bloc# and modify the ischemia4reperfusion in/ury and restore splanchnic perfusion can be incorporated into a resuscitation algorithm to reduce the incidence of bacterial translocation and systemic $hite cell priming before the ensuing systemic inflammatory response. -(+A@ MO+,TO-,+. The primary reason for monitoring renal function is that the #idney serves as an e&cellent monitor of the ade%uacy of perfusion. The second ma/or indication for monitoring #idney function is to prevent acute parenchymal failure. ;inally! renal function monitoring is helpful in predicting drug clearance and proper dose management. 5rine output fre%uently is monitored but may be misleading. Although very lo$ urine outputs! less than =.F m@0#g0h! are consistently associated $ith lo$ glomerular filtration rate 2.;-3 values! levels greater than this also can be associated $ith lo$ .;- values. )iuresis created by an osmotic load 2radiographic contrast material or glucose3! administration of diuretics! or nonoliguric renal failure may give the clinician a false sense of security $hile the patient has deteriorating renal function. Other methods of monitoring renal function are necessary. These include tests of glomerular function and tests of tubular function. .lomerular ;unction Tests 6lood urea nitrogen 265+3 often has been used to estimate renal function. 65+ is affected by .;- and urea production. 7roduction may be increased if large amounts of nitrogen are administered during parenteral nutritional support! as a result of gastrointestinal bleeding! or in catabolic states induced by trauma! sepsis! or steroids. 5rea production may be lo$ered during starvation and in advanced liver disease. 6ecause these factors are often interrelated in an unpredictable manner in critically ill patients! 65+ is not a reliable monitor of renal function.
The value of plasma creatinine as a measure of renal function far e&ceeds the value of the 65+. The serum creatinine level is directly proportional to the level of creatinine production and inversely related to the .;-. ,n contrast to 65+ concentration! plasma creatinine levels are not influenced by protein metabolism or the rate of fluid flo$ through the renal tubules. "hen creatinine production is constant! the serum creatinine level reflects .;-. The plasma creatinine level $ill double $ith a F= percent reduction in .;-! assuming that creatinine production remains constant. Acute reductions in the .;- rate are not immediately reflected! ho$ever! because it ta#es A< to IA h for e%uilibration to occur. Creatinine production is directly proportional to the muscle mass and its metabolism. ,n rhabdomyolysis! creatinine formation e&ceeds its filtration rate! such that measured serum creatinine levels increase. ,n conditions $here the s#eletal muscle mass is reduced 2e.g.! advanced age! immobili ation3! the endogenous creatinine pool is diminished! and thus the serum creatinine concentration does not rise appropriately $ith impairment of renal function. Only $ith measurement of creatinine clearance can the severity of such renal function loss be determined. 1erial determination of creatinine clearance is currently the most reliable method for clinically assessing .;- and the most sensitive test for predicting the onset of perioperative renal dysfunction. Although measurements traditionally are performed using a A<4h urine collection! measurements using a A4h collection are reasonably accurate and easier to perform. "hen urine output is measured in clearance studies! special efforts should be made to ensure complete bladder emptying at the beginning and end of collection periods. Creatinine clearance 2Ccr3 is calculated from the formula Ccr O 5cr N V 0 7cr N C.IB 0 61A $here 5cr O urinary creatinine concentration! mg0d@ V O urinary volume flo$! m@0min 7cr O plasma creatinine concentration! mg0d@ 61A O body surface area! mA Clearance results are e&pressed as milliliters per minute per C.IBmA. An alternative approach to creatinine clearance estimation is to forgo urine collection and utili e criteria formulated by Coc#croft and .ault. The Coc#croft4.ault e%uation for males is Ccr O 2C<= 4 age3 N $eight in #g 0 IA N 7cr ;or females! the derived Ccr is multiplied by =.MF. 5sing the lo$er of ideal or total body $eight and the higher of actual serum creatinine or corrected serum creatinine concentration to C mg0d@ in this formula results in more accurate predictions of .;-. Although the Coc#croft4.ault e%uation provides an ine&pensive and accurate estimate of .;- in patients $ith stable renal function! it is unli#ely that it $ould detect early renal deterioration because the serum creatinine! on $hich the e%uation depends! does
not begin to increase above normal until the .;- decreases to less than F= m@0min0C.IB mA. Tubular ;unction Tests Tests that measure the concentrating ability of the renal tubules are used primarily in the differential diagnosis of oliguria to differentiate a prerenal cause unresponsive to /udicious fluid therapy from intrinsic renal failure due to tubular dysfunction. Table CA4< summari es the differential diagnosis based on tubular function studies. The utility of each depends on the ability of the renal tubular cells to physiologically respond to a decreased e&tracellular fluid volume. Thus! $ith prerenal a otemia! the tubules can appropriately reabsorb sodium and $ater. ,n intrinsic renal failure! tubular function is mar#edly compromised! and the ability to reabsorb sodium and $ater is impaired. Multifactorial renal dysfunction is most common9 rarely is an isolated etiology discovered. Tubular function tests are useful in oliguric patients 2urine output L F== m@0day3 because nonoliguric individuals typically have less severe tubular damage and their laboratory findings are li#ely to sho$ more overlap $ith the values of patients $ith prerenal a otemia. The fractional e&cretion of sodium 2;(+a3 appears to be the most reliable of the laboratory tests for distinguishing prerenal a otemia from acute tubular necrosis. This test re%uires only simultaneously collected DspotE urine and blood samples. ;(+a can be calculated as follo$s? ;(+a2G3 O 5+a07+a 0 5cr07cr N C==G $here 5+a is the urinary sodium concentration 2in millie%uivalents per liter3! and 7+a is the plasma sodium concentration 2in millie%uivalents per liter3. The ;(+a value is normally less than C to A percent. ,n an oliguric patient! a value of less than C percent is usually due to a prerenal cause. A value greater than A to B percent in this setting suggests compromised tubular function. "hen the value ranges bet$een C and B percent! the test is not discriminating. Although the ;(+a is very useful! it is no$ apparent that a number of causes of acute renal failure other than prerenal disease can! on occasion! be associated $ith a ;(+a value of less than C percent. These include nonoliguric acute tubular necrosis! acute tubular necrosis superimposed on chronic prerenal disease 2e.g.! advanced cardiac or liver disease3! administration of radiocontrast media or release of heme pigments 2hemoglobin or myoglobin3! and renal allograft re/ection. Thus the ;(+a test must be interpreted in light of the specific clinical setting and other laboratory data to be useful in patient management. Correct interpretation of ;(+a or any of the other urinary indices is not possible if the patient had received diuretics in the : to CA h preceding the test. +(5-O@O.,C MO+,TO-,+. Monitoring the function of the central nervous system may permit early recognition of cerebral dysfunction and facilitate prompt intervention in situations in $hich
aggressive early treatment favorably influences outcome. ,n the perioperative and trauma settings! several methods have been used to evaluate brain function and the effects of therapy. These include intracranial pressure monitoring! electrophysiologic monitoring! transcranial )oppler ultrasonography! and /ugular venous o&imetry. ,ntracranial 7ressure Monitoring 7hysical findings are often unreliable to ascertain the presence of increased intracranial pressure 2,C73. Thus the only direct assessment of ,C7 is obtained by measurement. Measuring ,C7 permits calculation of cerebral perfusion pressure 2C773! $hich is defined as the difference bet$een the MA7 and ,C7. Thus isolated increases in ,C7 or decreases in MA7 $ill result in a reduction in C77. The C77 may be insufficient if ,C7 increases to more than A= mm'g. Although in the past one of the end points of central nervous system monitoring $as felt to be the contol of ,C7 $ithin safe levels! emphasis has shifted to follo$ing C77 itself. Maintaining cerebral blood flo$ appears to re%uire using an elevated minimal C77 threshold $hen treating the in/ured brain. A C77 level of at least I= mm'g has been suggested. The most common indication for ,C7 monitoring is severe head in/ury. 7atients $ith a .lasgo$ Coma 1cale 2.C19 see Chap. <=! Table <=4C3 score of M or less or a .C1 motor score of F or less 2i.e.! not follo$ing commands3 should be strongly considered for ,C7 monitoring. +arayan and associates demonstrated that patients $ith a .C1 score of M or less $ho have a normal CT scan have a very lo$ probability of developing intracranial hypertension if they have fe$er than t$o of the follo$ing features? 2C3 prior episodes of hypotension! 2A3 age greater than <= years! or 2B3 motor posturing. They suggested that these patients may be managed initially $ithout monitoring ,C7. ,n such instances! ho$ever! any deterioration should prompt immediate reconsideration of ,C7 monitoring and reimaging. Other conditions for $hich ,C7 monitoring has been recommended include subarachnoid hemorrhage! hydrocephalus! postcraniotomy! and -eye's syndrome. Although some investigators also have advocated this form of monitoring in patients $ith massive stro#es! encephalitis! and postJcardiac arrest states! little evidence has been generated to suggest a beneficial impact. 1everal methods of ,C7 measurement are available 2;ig. CA4C=3. A ventricular catheter connected to a standard strain4gauge transducer via fluid4filled lines offers e&cellent $aveform characteristics and permits $ithdra$al of cerebrospinal fluid 2C1;3. This catheter! ho$ever! may be difficult to insert $hen cerebral edema or hematoma causes shifting or collapse of the lateral ventricle system. A subarachnoid bolt is easily inserted under any circumstance! although at times it may give erroneous readings! depending on its placement relative to the site of in/ury. Compared $ith ventricular catheters! the $aveforms obtained are not as good! and C1; drainage is usually not possible. (pidural bolts have a lo$er ris# of complications but are less accurate than ventricular catheters or subarachnoid bolts and do not permit $ithdra$al of C1;. +on4fluid4coupled systems utili ing fiberoptic or catheter4tip strain4gauge technology can be placed into ventricular! subdural! and parenchymal sites. These devices appear to offer advantages over conventional ,C7 monitors! especially in their ability to measure brain parenchymal pressures. "ithout an
associated ventricular catheter! ho$ever! catheter4tip strain4gauge or fiberoptic devices cannot be recalibrated after insertion. Conse%uently! if the device measurement drifts! there is potential for inaccurate measurements! especially if the ,C7 monitor is used for several days. Complications of ,C7 devices include infection! hemorrhage! malfunction! obstruction! and malposition. 6acterial coloni ation of ,C7 devices increases significantly after F days of implantation9 ho$ever! significant intracranial infections are uncommon. (lectrophysiologic Monitoring The electroencephalogram 2((.3 reflects spontaneous and ongoing electrical activity recorded on the surface of the scalp. ,ntraoperative ((. recording has been used primarily for monitoring the ade%uacy of cerebral perfusion during carotid endarterectomy. Other procedures in $hich ((. recording has been used include cerebrovascular surgery! open heart surgery! epilepsy surgery! and induced hypotension for a variety of surgical procedures. ,n the ,C5! ((. recordings can detect the e&istence of subclinical epileptic sei ures! $hich can cause a decreased level of consciousness. 1tandard ((. recording! ho$ever! is not used routinely in the ,C5 because of insufficient technical personnel! the volume of data generated in a short period! the difficulty of on4line ((. interpretation! numerous electrically induced artifacts! and drug4induced suppression of electrical activity. To simplify ((. recording and to ma#e it more useful for clinical application in the operating room and ,C5! some monitors process the ra$ data automatically. The compressed spectral array 2C1A3 is the most commonly used method of visually displaying such processed ((. information. 1ensory4evo#ed potentials 21(7s3 are minute electrophysiologic responses elicited by a stimulus and e&tracted from an ongoing ((. by signal averaging. They reflect the functional integrity of specific sensory path$ays and serve to some e&tent as more general indicators of function in ad/acent structures. 1omatosensory evo#ed potentials 211(7s3 reflect the integrity of the dorsal spinal columns and the sensory corte& and may be useful for monitoring during resection of spinal cord tumors! spine instrumentation! carotid endarterectomy! and aortic surgery. 6rainstem auditory4 evo#ed potentials 26A(7s3 reflect the integrity of the eighth cranial nerve and the auditory path$ays above the pons and are used for monitoring during surgery of the posterior fossa. Visual evo#ed potentials 2V(7s3 may be used to monitor the optic nerve and upper brainstem during resections of large pituitary tumors. 1everal studies have promoted the prognostic value of 1(7s in the ,C5! primarily in head trauma patients. Continuous monitoring in the ,C5 is still rare. Transcranial )oppler 5ltrasonography Transcranial )oppler ultrasonography 2TC)3 is one of a number of methods currently being used to monitor cerebral blood flo$. This techni%ue employs the )oppler principle to record the blood flo$ velocity in the basal cerebral arteries and can provide valuable information regarding the integrity of the intracranial circulation. TC) also may detect vasospasm follo$ing spontaneous or traumatic subarachnoid hemorrhage and can help identify hyperemic or lo$4flo$ states.
The most commonly used TC) techni%ue is Dfree4handingE the transmitter so that the ultrasound beam penetrates one of several natural Dacoustical $indo$s.E Modified probes are no$ available that may be #ept in place for prolonged periods using a headband or other device. TC) is a valuable monitoring tool that is noninvasive! portable! and reproducible. ,t re%uires! ho$ever! that the studies be performed by a technician familiar $ith its use. Jugular Venous O&imetry Jugular venous o&imetry is an invasive method of continuously monitoring /ugular venous bulb o&yghemoglobin saturation 21/vOA3. Changes in 1/vOA provide a measure of the relationship bet$een total cerebral blood flo$ and total cerebral o&ygen consumption. "hen arterial o&ygenation remains constant! a decrease in 1/vOA from control values reflects a decrease in cerebral blood flo$ or an increase in cerebral metabolic o&ygen consumption unmatched by an increase in flo$. Jugular venous o&imetry offers the potential to minimi e secondary insults after severe head in/ury by facilitating recognition of cerebral ischemia. Other applications include monitoring during neurosurgical procedures! carotid endarterectomy! and cardiopulmonary bypass. The techni%ue for determination of 1/vOA is analogous to the determination of 1VOA on a systemic basis 2see above3. A fiberoptic catheter is placed retrograde into the /ugular bulb! and the 1/vOA is recorded in a continuous fashion. The range of 1/vOA in normal sub/ects is FF to IC percent. ,n head4in/ured patients! the range for 1/vOA is considerable $ider! but most investigators agree that a sustained desaturation of F= to FF percent $arrants evaluation. 1/vOAlevels belo$ F= percent are indicative of cerebral ischemia. Artifactual recordings! ho$ever! are not uncommon and usually are caused by catheter malposition from head and nec# movement. M(TA6O@,C MO+,TO-,+. .eneral Considerations The need to substitute artificial feedings during recovery from surgery and trauma turns the simple everyday function of ingestion of food into a complicated area involving mathematics! suppositions! high technology! and the potential for creating harmful side effects. Assessment of Caloric (&penditure (nergy re%uirements depend on a number of factors including the body surface area! age! and se&. 6asal energy e&penditure 26((3 can be predicted $ith reasonable accuracy 2SF percent3 by the 'arris46enedict e%uation? Men? ::.<I T 2CB.IF N "3 T 2F.== N '3 4 2:.I: N A3 O6(( #cal0day "omen? :FF.C= T 2>.F: N "3 T 2C.MF N '3 42<.:M N A3 O 6(( #cal0day $here " O body $eight! #g 'O height! cm A O age! years
-esting energy e&penditure 2-((3 can be appro&imated from the 6(( by increasing it by C= percent! adding the calories necessary to compensate for the specific dynamic action of food. The stress of illness! the change in hormonal milieu relating to the stress state! alterations in substrate utili ation! and fever all can be predicted to increase -((. "hile early studies emphasi ed increases of AF percent for multiple4trauma patients and F= percent for burn patients! even an increase of := percent above 6(( $ould only result in a need for <= #cal0#g0day! or less than B=== #cal in a I=4#g patient. (&cessive caloric administration is potentially detrimental. Carbohydrates given in e&cess of re%uirements are turned into fat! resulting in an increase in COA production. The liver may develop fatty infiltration resulting in hepatic dysfunction. ,n addition! many patients may have protein malnutrition despite being over$eight due to obesity or overhydration. ,n a study of critically ill patients! Ma## and colleagues found that FM percent $ere over$eight. ;orty4t$o percent had a #$ashior#or4li#e pattern of malnutrition! and CC percent had a marasmus4li#e pattern. 7rotein malnutrition necessitates administration of higher levels of protein to avoid or reverse end4organ dysfunction and impaired acute4phase protein synthesis! $hich sets the stage for nosocomial infections and the multiple organ system failure syndrome. Assessment of O&ygen Consumption ,f caloric e&penditures can be considered the fuel! then another aspect of metabolic monitoring is the flame. O&idative metabolism or o&ygen consumption reflects metabolic activity. Cuthbertson described the ebb4 and4flo$ phase of the metabolic response to in/ury. ,n his terms! the ebb phase! lasting A< to <M h! is a period of Ddiminished circulatory vitalityEHdecreased cardiac output! diminishing o&ygen delivery! and resulting decreased o&ygen consumption. The recognition of the association bet$een diminished o&ygen delivery in the ebb phase $ith the late occurrence of sepsis and multiple organ system failure has focused attention on improving o&ygen delivery in an attempt to forestall this seemingly inevitable progression. Thus monitoring and optimi ing o&ygen delivery as described previously have been given additional significance in terms of minimi ing long4term detrimental metabolic effects secondary to stress and in/ury. Measurements O&ygen delivery or cardiac output times arterial o&ygen content and o&ygen consumption 2normally about CF= m@0min0mA3 assess o&idative metabolism. COA production is a measure of a by4product of o&idative metabolism. The ratio of COA production to o&ygen consumption is termed the respiratory %uotient 2-83. )uring normal oral dietary inta#e! carbohydrates! protein! and fat are ingested! giving an average -8 of appro&imately =.M. )uring prolonged starvation! the body adapts to fat metabolism! and the -8 may fall to as lo$ as =.: to =.I. On the other hand! during e&cessive carbohydrate administration! the transformation into fat releases additional COA! and the -8 rises above C.=. Thus monitoring o&ygen consumption and COAproduction and calculating the -8 provide inferences into the ade%uacy of total calories as $ell as the mi&ture of substrates.
,n the past fe$ years! clinicians! recogni ing the number of variables affecting -(( and total energy e&penditure 2T((3! have attempted direct measurements in order to meet an individual patient's needs at a particular time in the course of the illness. ,t is clear that estimates of -(( from the 'arris46enedict e%uation! even modified by estimates to ad/ust for increased metabolic activity! still lead to inaccurate assessment of T((. )irect calorimetry measures body heat production and is correlated $ith energy use. The sub/ect! ho$ever! must be placed in a closed chamber for measurement of heat production! and clearly! this is not applicable to patient care. ,ndirect calorimetry permits derivation of caloric re%uirements from the measurements of o&ygen consumption and COAproduction. Methods used include )ouglas bag collection of e&pired gases! use of the ;ic# e%uation! and computeri ed open circuit measurements. )ouglas 6ag Collection 1amples of inspiratory and mi&ed e&piratory gases are analy ed for o&ygen and COA concentrations. 5nfortunately! this techni%ue is prone to many errors. .as lea#age! incomplete emptying! inaccurate measurement of total e&pired gases! and incomplete mi&ing or lea#age through incompletely sealed connections are but a fe$ of the problems encountered. ;inally! it is a tedious method that does not lend itself to fre%uent or routine clinical use. The -everse ;ic# Method The classic ;ic# e%uation 2see Table CA4B3 relates o&ygen consumption to the product of cardiac output and arterial venous o&ygen content difference. -epeated cardiac output determinations have an accuracy in the range of SF percent but are not as important as variability in the patient's physiology! in $hich changes may e&ceed SC= percent in a short time. 7ulse o&imetry and mi&ed venous o&imetry sho$ that minute4 to4minute variations in these values also occur. 1mithies has sho$n that these factors result in a C= percent variation bet$een measurements and lo$er total values compared $ith validated spirometric techni%ues. This latter difference reflects the o&ygen consumption of the lung! $hich is included in the spirometric method but not in the reverse ;ic# techni%ue. Computeri ed Open Circuit ,ndirect Calorimetry 1everal commercial indirect calorimeters have been evaluated by Ma#ita and associates. The )ate& )eltatrac Metabolic Monitor 2)ate& ,nstrumentarium! 'elsin#i! ;inland3! the (ngstrVm Metabolic Computer 2.ambro (ngstrVm A.6.! 6roma! 1$eden3! and the 1ensorMedics MMC 'ori on 21ensorMedics! Anaheim! CA3 use slightly different techni%ues and formulas. Mean relative errors of measurement for all three monitors! ho$ever! $ere in the range of C.< to : percent for o&ygen consumption! COAproduction! and respiratory %uotient. ,n routine clinical use! ho$ever! there are many potential errors. ,nstruments lose calibration easily. 'igh inspired o&ygen concentrations 2;iOA K =.:3 render measurements inaccurate. ;luctuations in hospital gas4 line pressure cause C to A percent fluctuations in inspired ;iOA! sufficient to impair the accuracy of overall o&ygen consumption. @ea#s at /oints and connections occur fre%uently and must be eliminated before and during studies. Measurements of COA production depend on a steady4state relationship bet$een COA production at the cellular level! transport to lungs! and COA elimination via the lungs and measured in e&haled gases. Therefore!
changes in the metabolic rate! changes in cardiac output! and changes in ventilation all affect the inherent supposition that COA production and COA elimination measured by the metabolic monitor are e%ual. Minute4to4minute variations may be minimi ed by ensuring that measurements encompass at least CF min t$ice daily. Clinical 5tility ;irst! metabolic monitoring can be used to /udge the end result of the interactions of all the un#no$ns 2including degrees of illness! activity! and metabolism3 in producing the current levels of o&ygen consumption and COA production. 1econd! either too little or incorrect proportions of nutritional support are undesirable. ,f $e remember that appro&imately BA to BF #cal0day should suffice in most clinical circumstances and that there are no outcome data suggesting that SC= or even A= percent has a demonstrable adverse effect on any #no$n variable! $e should ensure that $e stay $ithin this range of measured values. Third! $e could identify patients $ith significant hypometabolism or hypermetabolic states because clinical estimates are often incorrect. Ad/usting nutritional support in these circumstances seems to be common sense! although it has not been proved that these ad/ustments ma#e any real difference. ;ourth! given the $ide variations in caloric re%uirements and in substrate utili ation! metabolic monitoring! allo$ing more appropriate partitioning of the substrates! seems more desirable than administering %uantities by rote or formula. ;ifth! measurements of respiratory %uotient may be useful in patients $ho have respiratory failure and COA retention $hile receiving high carbohydrate loads. ,dentification of a high respiratory %uotient due to e&cessive carbohydrate administration is one correctable factor. 6ecause commercially available indirect calorimeters no$ can measure o&ygen consumption and COA production and calculate other parameters of metabolic cellular activity! the demonstrated accuracy in measurement can be used to support more precise prescription of nutritional therapy. 8uestioning $hether this degree of obtainable precision alters outcome is relevant9 at the same time! inaccurate prescriptions based on invalid estimates $ould not seem to be a viable ob/ective. The costs of this approach are not inconsiderable! and $hile they may be offset by savings in $asted nutritional support! more data reflecting improvement in outcome are necessary before mandatory or daily usage even in critically ill patients can be supported. T(M7(-AT5-( MO+,TO-,+. Temperature! along $ith heart rate! blood pressure! and respiratory rate! remains one of the traditional four cardinal vital signs. Temperature is usually ta#en rectally in ill patients or orally $hen significant elevations are not e&pected. Temperatures of the periphery of the body measured at the mouth! s#in! or a&illa are often unreliable and may be influenced by factors such as mouth breathing! temperature of recently ingested food! and0or environmental temperature. Therefore! it is recommended that deeper core temperatures be ta#en in the critically ill. Core temperatures! $hich are relatively resistant to e&ternal influences! more accurately reflect the mean temperature of the body's vital organs. Core temperature can be measured by placing a thermistor probe into either the esophagus or the rectum. (sophageal $ires are uncomfortable and invasive and are used e&clusively in
patients under general anesthesia. -ectal probes are used commonly in the operating room and ,C5 but may be e&truded from the rectum and have a recogni ed ris# of bo$el $all perforation. Three devices are available commercially for bedside measurement of core temperature in ,C5 patients? pulmonary artery thermistor catheters! urinary bladder thermistor catheters! and infrared auditory canal probes. Measurement of pulmonary artery blood temperature by the pulmonary artery thermistor catheter has been used increasingly as a reliable indicator of core temperature. The need for a catheter is an obvious disadvantage of this approach. 5rinary bladder catheters have the advantage of giving both e&act measurements of urine output and continuous urine temperature. ,nfrared probes noninvasively measure tissue temperature in the ear canal9 ho$ever! their measurements have more variability than bladder readings. Moderate variation is probably inherent in infrared ear thermometry due to differences in ear canal anatomy and probe positioning. 26ib
Você também pode gostar
- Cleft Lip, Anomalies of Face, Palate Jaw, TeethDocumento11 páginasCleft Lip, Anomalies of Face, Palate Jaw, Teethsabina_grapiniAinda não há avaliações
- 46.the BreastDocumento21 páginas46.the Breastsabina_grapiniAinda não há avaliações
- Actures & DislocationsDocumento16 páginasActures & Dislocationssabina_grapiniAinda não há avaliações
- Chapter 3 Hemostasis-Surgical Bleedind-TransfusionDocumento36 páginasChapter 3 Hemostasis-Surgical Bleedind-Transfusionsabina_grapiniAinda não há avaliações
- Chapter 1 Systemic Response To InjeryDocumento46 páginasChapter 1 Systemic Response To Injerysabina_grapiniAinda não há avaliações
- Chapter 7 BurnsDocumento66 páginasChapter 7 Burnssabina_grapiniAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Diabetes Type 2Documento28 páginasDiabetes Type 2Yerlis OspinoAinda não há avaliações
- Cia CivDocumento6 páginasCia CivCamila Fda. Muñoz G.Ainda não há avaliações
- Adrenergic SystemDocumento6 páginasAdrenergic SystemdocsAinda não há avaliações
- Computation of Drips: Marla Aurora JacobaDocumento18 páginasComputation of Drips: Marla Aurora JacobaAnne Lorraine Bringas100% (1)
- Sinusnodedysfunction: Neeraj Sathnur,, Emanuel Ebin,, David G. BendittDocumento19 páginasSinusnodedysfunction: Neeraj Sathnur,, Emanuel Ebin,, David G. Bendittnicolas.sierra1Ainda não há avaliações
- SonoAce - R7 - Reference Manual - EDocumento230 páginasSonoAce - R7 - Reference Manual - EEcomedical PlussAinda não há avaliações
- STROKEDocumento9 páginasSTROKEhillary elsaAinda não há avaliações
- Pulse OximeterDocumento17 páginasPulse OximeterΑнмєɒ FσυαɒAinda não há avaliações
- Stanford Cardiovascular CT Scanning and Injection Protocols: Siemens Sensation 64Documento24 páginasStanford Cardiovascular CT Scanning and Injection Protocols: Siemens Sensation 64José GilsonAinda não há avaliações
- COC Exercise-1Documento9 páginasCOC Exercise-1Biyyaol AbiAinda não há avaliações
- Physiology Practical 2: Toad HeartDocumento10 páginasPhysiology Practical 2: Toad HeartAdams OdanjiAinda não há avaliações
- Des Fibril Ad or Welch Allyn Pic 30Documento109 páginasDes Fibril Ad or Welch Allyn Pic 30Nadia RiveraAinda não há avaliações
- IPM Blood Pressure MonitorDocumento6 páginasIPM Blood Pressure MonitorRajo LangitAinda não há avaliações
- Definition of Acute Coronary SyndromeDocumento4 páginasDefinition of Acute Coronary SyndromePratama InsaniAinda não há avaliações
- Andocor Cannula Cataloog 2015 PDFDocumento37 páginasAndocor Cannula Cataloog 2015 PDFAhmadAinda não há avaliações
- Iloilo Doctors' College College of Nursing: West Avenue, Molo, Iloilo CityDocumento2 páginasIloilo Doctors' College College of Nursing: West Avenue, Molo, Iloilo CityAudrie Allyson GabalesAinda não há avaliações
- TFG Víctor Fibla AntolíDocumento47 páginasTFG Víctor Fibla AntolíVíctor Fibla AntolíAinda não há avaliações
- Cardiac Risk Assessemnt FlowchartDocumento1 páginaCardiac Risk Assessemnt FlowchartjamesomooreAinda não há avaliações
- NFHS-5 Schedule Biomarker Survey QuestionnaireDocumento22 páginasNFHS-5 Schedule Biomarker Survey QuestionnaireDisability Rights AllianceAinda não há avaliações
- ESH-IP 2010 Validation of OMRON EVOLV (HEM-7600 T-E) v2Documento11 páginasESH-IP 2010 Validation of OMRON EVOLV (HEM-7600 T-E) v2Pub PleAinda não há avaliações
- Vital Sign #1: Body TemperatureDocumento5 páginasVital Sign #1: Body TemperaturePrimelift Safety Resources LimitedAinda não há avaliações
- Overview of The Circulation Pressure, Flow and ResistanceDocumento7 páginasOverview of The Circulation Pressure, Flow and ResistanceSalsabilla Ameranti PutriAinda não há avaliações
- Appropriation Weeks 4-5Documento6 páginasAppropriation Weeks 4-5AURA CAMILA LEÓN ÁLVAREZAinda não há avaliações
- Heart Lung InteractionDocumento29 páginasHeart Lung InteractionKARDIOLOGI STASE RSALAinda não há avaliações
- Unstable Angina - Cardiovascular Disorders - MSD Manual Professional EditionDocumento1 páginaUnstable Angina - Cardiovascular Disorders - MSD Manual Professional EditionboynextdoorpkyAinda não há avaliações
- Classification of Congenital Heart DiseaseDocumento1 páginaClassification of Congenital Heart DiseaseClaudia SanchezAinda não há avaliações
- Medical Surgical Nursing - Responses To Altered Tissue PerfusionDocumento23 páginasMedical Surgical Nursing - Responses To Altered Tissue PerfusionLouise NicoleAinda não há avaliações
- College of Nursing: Pharmacology Drug StudyDocumento1 páginaCollege of Nursing: Pharmacology Drug StudyChristine Pialan SalimbagatAinda não há avaliações
- Drug Card MetoprololDocumento3 páginasDrug Card Metoprololcelosia23100% (3)
- Comparison of Dabigatran Versus Warfarin TreatmentDocumento7 páginasComparison of Dabigatran Versus Warfarin TreatmentDivyesh AmarsedaAinda não há avaliações