Escolar Documentos
Profissional Documentos
Cultura Documentos
History Taking
Enviado por
vinodksahuDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
History Taking
Enviado por
vinodksahuDireitos autorais:
Formatos disponíveis
Taking a Psychiatric History: Notes by Jason Hancock
Taking a Psychiatric History
1) Referral And Informants Patients details. When and where is patient being seen? Legal status of admission: voluntary or detained. Why are they being seen? Who was history taken from; patient or carer? 2) Introduction Who I am, my purpose and how long I have to interview the patient. Consent confidentiality, permission to take notes. Demographics, name, date of birth, occupation, marital status. 3) Presenting Complaint What is the complaint(s), is this all of them? If we could sort out all of these would things be all right? 4) History of Presenting Complaint When did you last feel well? SOCRATES! The mnemonic for taking a history of a pain may be helpful for some symptoms: Site, Onset, Character, Radiation, Alleviating factors , Time course and periodicity, Exacerbating and precipitating factors, Severity When/ how did problems start? Can you think of any potential triggers? Duration, course of the problem. These questions then vary depending on the specific problem that the patient has presented with; DEPRESSION (treat feelings of low mood in the same way you would treat pain, find out everything about the depression before moving on to ask about other features/ associated symptoms). How has mood been? How long has mood been long for, is mood always low, when is it at its worst? Can you do anything to lift your mood? Do you ever look forward to anything? Are you ever tearful? Do you ever feel guilty, worthless or hopeless? Do you ever self harm? Have you ever thought of ending it all? Associated symptom; Is patient experiencing other physical symptoms? Is appetite reduced, any weight loss, lack of motivation, sleep effected (trouble getting to sleep, sign of mild depression, or early waking a sign of more severe depression). Do you suffer from any other physical symptoms aches and pains etc, has sex drive been effected? Have these symptoms caused you any problems at work or at home? PSYCHOSIS May be difficult to work out what symptoms patient is experiencing as they are unlikely to tell you they are suffering from delusions etc. Have you been had any thoughts recently that you now accept as being strange or that others have commented on being strange? Are there any plots against you?
www.askdoctorclarke.com
Taking a Psychiatric History: Notes by Jason Hancock Have people been interfering with your thoughts (thought insertion) or are your thoughts being withdrawn or broadcast? (Thought alienation). Do you ever see or hear things that other people seem unable to see or hear? (Hallucinations). If yes, are the voices talking about you (third person) or to you (second person), are they commenting on what you are doing (running commentary) or are they telling you to do certain things, if so what? Do you believe the voices and do you do what they tell you to do? Does the patient have any insight? Try to get an idea of how long these problems have been going on and how they have changed over time. ANXIETY Generalised anxiety; general feelings of anxiousness, feeling on edge, worry, irritable, unable to relax. Panic attacks; hyperventilation, SOB, chest pain/ palpitations, sweating, tremor, how long do attacks last, what brings them on. Phobias; any fears that you or others may consider to be irrational, any thoughts you would consider obsessive. Important to ask for all What does patient think the cause is? Any recent events that have precipitated the presenting complaint that the patient feels may have had an effect. These events may be negative (separation, death in family) or can be positive (promotion at work, increased stress). Timing, did this event occur before or after the presenting complaint? What are the patients coping strategies? 5) Present Social Situation And Effect That The Illness Is Having Effect that the condition is having on lifestyle: mainly work, family and friends. Who does patient live with? Who cares for them? SOCIAL SUPPORT, Do they have anybody they can confide in? Remember that some close family members can have a negative effect if they show high expressed emotion (especially causing relapses of schizophrenia). What is patients normal level of functioning, how do they cope with activities of daily living (ADL)? Does patient receive/ require any additional support? Does patient have any financial, employment or legal problems?
6) Previous history: psychiatric and general medical (i) All PMH, Tell me about your birth, were you ever told you had any problems at birth or during childhood? Has patient ever suffered a head injury, meningitis or from epilepsy? (ii) Past psychiatric history, past contact with psychiatric or mental health services, dates, diagnosis, treatment, duration, legal status of admissions, history of self-harm or suicide attempts. What has triggered problems in the past?
www.askdoctorclarke.com
Taking a Psychiatric History: Notes by Jason Hancock 7) Drug History All current medications, prescribed, over the counter and street drugs. Treatments that have been already tried/ used in the past, did they work, if not why not? Does patient have any problems with medications, do medications have any side effects, does patient find it easy to comply with treatment, what are patients thoughts towards treatments e.g. do they feel they need medication? 8) Family Medical And Psychiatric History Is there a family history of neurological or psychiatirc disorders, suicides, criminal behaviour or alcoholism? For Asian patients it is important to ask about a family history of possession. For afrocarabean patients it is important to ask about a family history of witchcraft. 9) Personal History How did patient find their childhood? Did patient get on well with siblings? Did patient enjoy their childhood? Does patient remember being separated from their parents for a period of time? What was patients relationship with their family like in the past is there a history of abuse; were you ever touched as a child in a way that made you feel uncomfortable? Did patient enjoy school, did they find it easy to make friends, what were their hobbies, what were their educational achievements, and did patient go onto further education? Is patient able to read and write confidently? Are they able to manage their own money? Occupational history, types of job, length at each, and reasons for leaving. What does patient currently do for a living and how are patients relationships with colleagues? If patient currently unemployed what do they fill their day with, any hopes for future employment? Psychosexual development, loss of virginity, orientation, if appropriate. Personal relationships, length, reason for ending, marital status and history, any children? Degree of support from partner, current or past problems with sexual performance (if appropriate). What levels of stress has patient been exposed to in their life and how do they feel they have coped? Reproductive history If female, history of teenage pregnancy? Abortions? History of menstruation, first period, any PMT or heavy periods? Attitudes to periods? Forensic history Has patient ever been in trouble with the law?
10) Premorbid Personality (Can be difficult for some patient to assess their own personality and so a witness may help) Personality, Are you happy go lucky, tense, shy, greedy, insecure? Are you an anxious person? Evidence of obsessional traits, what is patients predominant mood? Relationships with superiors, and peers. Hobbies and interests?
www.askdoctorclarke.com
Taking a Psychiatric History: Notes by Jason Hancock 11) Alcohol And Drug History Alcohol use at present; how much does patient drink a week, types of alcohol as well as quantity. In what situations does patient drink, alone, in pub with friends? Remember CAGE; Have you ever felt you should cut down the amount you drink? Have you ever felt annoyed by somebody commenting on the amount you drink? Have you ever felt guilty about the amount you drink? Have you ever had an eye opener, a drink first thing in the morning to get you going? Alcohol use in the past; what has been the patients maximum regular usage? Any use of illicit drugs in the past or substance misuse? *Remember that a full psychiatric assessment requires a full history and a full mental state examination. Although some of the questions may overlap generally the history aims to find out what has been going on recently (leading up to this point), while the mental state examination aims to assess the patients mood, thoughts etc at the time of assessment.
Mental State Examination
� APPERANCE AND BEHAVIOUR Self care (reduced with dementia and depression). Eye contact, (reduced in depression, staring with Parkinsonism and following use of some drugs). Face, pupils dilated and horizontal creases on forehead = anxiety, corners of mouth turned down vertical lines on forehead = depression. Agitation, can appear as either i) Excessive motor activity with depression or anxiety, ii) high level of activity with no anxiety i.e. mania. Psychomotor retardation, posture slumped, slowing down of thought and a reduction of physical movements, often seen in clinical depression and can be accompanied by psychosis. Abnormal movements can have many causes: � Tardive dyskinesias, involuntary movements of the face and neck, may follow use of antipsychotics. � Tremors. � Stupor. � Waxy flexibility patients stays in any position that they are placed in, e.g. schizophrenia or structural brain disorder. � Forced grasping, takes examiners hand whenever offered, dementia or chronic schizophrenia. � Stereotypies uniform, repetitive non goal directed actions, found in schizophrenia. SPEECH, � Form (rate), � Content, FORM, rate and flow; 1) If increased may indicate anxiety or a thought disorder, if goal directed this is pressure of speech - thoughts jump from one thought to another with a connection between thoughts then think mania, if no connection between thoughts this indicates www.askdoctorclarke.com 4
Taking a Psychiatric History: Notes by Jason Hancock schizophrenia. 2) Decreased, may indicated psychomotor retardation, mutism maybe present with schizophrenia or severe depression. 3) Incoherent? 4) Perseveration, repeating same words or phrases mainly seen in dementia. CONTENT, is speech appropriate, is speech congruent? Neologisms: words created by schizophrenic patients to describe morbid experiences, Echolalia (repeating same words phrases as examiner), echopraxia (repeating movements of examiner), are both common in schizophrenia. � MOOD Subjective (how patient tells you it is) and objective, how it looks to you that they are. DEPRESSION Do you feel your mood is low? Feeling tearful? Can you do anything to cheer yourself up? Have they ever felt guilty about the past, pessimistic about the present or hopeless about the future? It must be difficult feeling so worthless and hopeless about the future, have you ever thought of ending it all? ANXIETY, how do you feel when you get anxious? Any palpitations, dry mouth, sweating, trembling. MANIA, how are your spirits, unusually good? Objective Do emotions appear appropriate; is range of emotions restricted as may be the case with depression or schizophrenia, are emotions incongruent as may be the case with mania, Do emotions appear to be labile (excessively changing)? THOUGHTS Delusions; Have you noticed that you have been having any odd thoughts? Or thoughts that others have found strange? � Primary delusions, thought alienation, persecutory delusions in schizophrenia. � Nihilistic, hypochondrical, worthless, guilt, hopelessness in depression. � Grandiose delusions in mania. Thought disorders; Do you find it hard to concentrate/ notice that your thoughts fly from place to place. Any thought block? Obsessional phenomena; do thoughts keep entering your head even though you try hard to stop them? Ask about compulsive rituals. Thought alienation, schizophrenia; Are your thoughts being interfered with, are people putting thoughts into your head or listening to your thoughts, is anybody harming you or plotting to harm you? Depersonalisation; do you feel unreal or that any part of your body is unreal? Derealisation; do you feel ever that things around you are unreal? Depersonalisation and derealisation can occur in anxiety disorders.
www.askdoctorclarke.com
Taking a Psychiatric History: Notes by Jason Hancock 5) PERCEPTION Can you see or hear things others can not? Does sense come from within or is it external e.g. can you hear voice in the same way you can hear me now? Have you ever seen something and thought that it was something else? (Illusions). Auditory hallucination, 3rd person, is there only one voice or are there more? commentary schizophrenia, 2nd person abusing them. Visual hallucinations, think organic brain disease. Depersonalisation or derealisation can occur with anxiety or fatigue. COGNITIVE FUNCTION Best to perform a full mini mental state examination however Hodgkinsons abbreviated mental test score is quicker. Score out of ten, serial scores are better than one off values; � Present year and your age (2) � Time to nearest hour (1) � Recognition of people (1) � Name of place (1) � Birthday (1) � Name of prime minister (1) � Memorise address (1) � Date of second world war (1) � Count backwards from 20 � 1 (1) Other useful questions; abstract thought, can patient understand how a phrase like a rolling stone gathers no moss could relate to humans, (if not think schizophrenia). i. ii. iii. iv. Abnormal experiences are extraordinary. That they are a result of the disease process. That they can be prevented by medical treatment. CRUCIALLY, must assess if patient is a risk to themselves or others.
6)
7)
INSIGHT
Full mini mental state examination Orientation; What is the (year) (season) (date) (day) (month)? [5] Where are we: (country) (county) (town/city) (building) (floor)?
[5]
Registration Name 3 common objects (apple, table, penny) take 1 second to say each word. Ensure patient has understood; ask them to repeat three words. Give 1 point for each correct answer. Record how many trials it takes for patient to understand all three words. [3] Attention Spell WORLD backwards. The score is the number of letters in the correct order. [5]
www.askdoctorclarke.com
Taking a Psychiatric History: Notes by Jason Hancock Recall Ask for the 3 objects named above. Give 1 point for each correct answer. [3] Language Point to a pencil and watch ask patient to name. [2] Repeat: No ifs ands or buts. [1] Follow a three stage command: Take a piece of paper in your right hand, fold it in half and place it on the floor. (Do not gesture to the patient at all while doing this, they must follow auditory commands) [3] Read and obey the following: [1]
Close your eyes
Write a sentence. [1] Copy the following design; [1]
Full score out of 30. Bibliography; Chapter 4, Psychiatry, Oxford handbook of clinical specialties, seventh edition, New York, oxford university press, 2006, Chapter 4, Anxiety disorders, Master medicine, psychiatry, first edition, London, Churchill Livingstone, 2002, Design for MMSE taken from; http://app1.unmc.edu/geriatricsed/delirium/mini_mental_satus_exam.htm Accessed on the 11/11/07
Note These notes were written by Jason Hancock as a medical student in 2008. They are presented in good faith and every effort has been taken to ensure their accuracy. Nevertheless, medical practice changes over time and it is always important to check the information with your clinical teachers and with other reliable sources. Disclaimer: no responsibility can be taken by either the author or publisher for any loss, damage or injury occasioned to any person acting or refraining from action as a result of this information
www.askdoctorclarke.com
Você também pode gostar
- Psychiatric Case History NotesDocumento8 páginasPsychiatric Case History NotesTysle100% (1)
- Psychiatric History TakingDocumento6 páginasPsychiatric History TakingNurul Nadzri100% (1)
- Mr. Cjy Cwu 1Documento9 páginasMr. Cjy Cwu 1ameerAinda não há avaliações
- Psychiatric History GuideDocumento8 páginasPsychiatric History GuideBobet ReñaAinda não há avaliações
- History TakingDocumento3 páginasHistory Takingmkct111100% (1)
- Psychiatric History SummaryDocumento24 páginasPsychiatric History SummaryfahmiAinda não há avaliações
- H&P Cheat SheetDocumento3 páginasH&P Cheat SheetWilliam YangAinda não há avaliações
- USM Psychiatry Student GuideDocumento43 páginasUSM Psychiatry Student GuideAhmad Syahmi YZ100% (1)
- History Taking in PsychiatryDocumento3 páginasHistory Taking in PsychiatryJuan Cruz FenrirAinda não há avaliações
- History and MSEDocumento13 páginasHistory and MSEG.Sangeetha bnchAinda não há avaliações
- History Taking in PsychiatryDocumento45 páginasHistory Taking in PsychiatryShashah Rau100% (3)
- History Taking in PsychiatryDocumento3 páginasHistory Taking in PsychiatryReza Parker50% (2)
- Psychiatry Osce PackDocumento4 páginasPsychiatry Osce PackzipppppppAinda não há avaliações
- Psychiatric History - MSEDocumento7 páginasPsychiatric History - MSEDeepbluex100% (1)
- The Importance of Psychiatry History TakingDocumento19 páginasThe Importance of Psychiatry History TakingManoj Bala100% (1)
- Medical History Taking TemplateDocumento2 páginasMedical History Taking TemplateAnwar Hammoud100% (1)
- IM 1 History TakingDocumento10 páginasIM 1 History TakingJoan Timbol100% (1)
- Hypochondriacal DisorderDocumento61 páginasHypochondriacal Disorderdrkadiyala2Ainda não há avaliações
- Psychiatric Case PresentationDocumento52 páginasPsychiatric Case PresentationdoreenAinda não há avaliações
- Psychiatry Made EasyDocumento14 páginasPsychiatry Made EasyTinesh Rajah83% (6)
- Psy Cwu 2Documento12 páginasPsy Cwu 2Nadhirah ZulkifliAinda não há avaliações
- History Taking of a 17-Year-Old Male with Addiction and Sexual DysfunctionDocumento3 páginasHistory Taking of a 17-Year-Old Male with Addiction and Sexual Dysfunctionmybuddies15875% (12)
- 2011 09 PsychiatryDocumento40 páginas2011 09 PsychiatryGurpreet Chara100% (1)
- DSM-IV Criteria MnemonicsDocumento4 páginasDSM-IV Criteria Mnemonicsleonyap100% (1)
- Epilepsy NotesDocumento6 páginasEpilepsy NotesPrarthana Thiagarajan100% (1)
- Clinical Methods in Psychiatry 2nd EditionDocumento92 páginasClinical Methods in Psychiatry 2nd Editionprachirb100% (1)
- Organic Brain SyndromeDocumento107 páginasOrganic Brain SyndromeRashrosha MohamedAinda não há avaliações
- Checklist MseDocumento6 páginasChecklist MseHerlene Lyneth ZalamedaAinda não há avaliações
- Depression History Checklist OSCEDocumento2 páginasDepression History Checklist OSCENur Farhana Athirah AzhariAinda não há avaliações
- Past Psychiatric History ExamplesDocumento11 páginasPast Psychiatric History ExamplesEzra Denise Lubong RamelAinda não há avaliações
- Psychiatric History Taking EssentialsDocumento108 páginasPsychiatric History Taking Essentialsdev86% (37)
- Understanding the Mental Status ExamDocumento87 páginasUnderstanding the Mental Status Examabhishek agarwalAinda não há avaliações
- Cwu PsyDocumento14 páginasCwu PsyAmirul HafizAinda não há avaliações
- History Taking TemplateDocumento4 páginasHistory Taking TemplateLucas Lima100% (1)
- Psychiatry Ward HistoryDocumento5 páginasPsychiatry Ward HistoryMahnoor Zafar100% (1)
- CNS Symptoms Guide for Neurological ExamDocumento39 páginasCNS Symptoms Guide for Neurological Examsekaralingam100% (1)
- Suicide Risk Assessment: OSCE ChecklistDocumento3 páginasSuicide Risk Assessment: OSCE ChecklistNur Farhana Athirah AzhariAinda não há avaliações
- History Taking Scheme PsychiatryDocumento2 páginasHistory Taking Scheme PsychiatryaliAinda não há avaliações
- History Taking in PsychiatryDocumento13 páginasHistory Taking in PsychiatryvinodksahuAinda não há avaliações
- Formal Patient Case Presentation FormatDocumento2 páginasFormal Patient Case Presentation FormatMichael ChangAinda não há avaliações
- Psych Osce Reviewer 1Documento10 páginasPsych Osce Reviewer 1pasambalyrradjohndarAinda não há avaliações
- Major Depressive Disorder With Psychtoic Feature DR AKK Case 23-1-20Documento55 páginasMajor Depressive Disorder With Psychtoic Feature DR AKK Case 23-1-20thu thuAinda não há avaliações
- Kirby's ToolDocumento2 páginasKirby's ToolIsha BhusalAinda não há avaliações
- Case Write Up 2Documento16 páginasCase Write Up 2Amirul Hafiz100% (3)
- Psychiatry: Taking A Psychiatric HistoryDocumento48 páginasPsychiatry: Taking A Psychiatric Historyfdjslajf100% (1)
- SPMM Smart Revise Descriptive Psychopathology Paper A Syllabic Content 5.22 Mrcpsych NoteDocumento43 páginasSPMM Smart Revise Descriptive Psychopathology Paper A Syllabic Content 5.22 Mrcpsych NoteBakir JaberAinda não há avaliações
- Mastering Psychiatry 2013 (Final)Documento363 páginasMastering Psychiatry 2013 (Final)melvynzhangweibin100% (5)
- Assessment and Evaluation: 2008 Edition Rhoda K Hahn, MD Lawrence J. Albers, MDDocumento85 páginasAssessment and Evaluation: 2008 Edition Rhoda K Hahn, MD Lawrence J. Albers, MDAlbghdadi CristianAinda não há avaliações
- History Taking and Psychiatric Interview GuideDocumento18 páginasHistory Taking and Psychiatric Interview GuideMujeeb ChoudharyAinda não há avaliações
- Mental Status ExaminationDocumento13 páginasMental Status ExaminationJosé Ramón Pérez-Accino100% (1)
- History Taking: A Concise Medical HistoryDocumento8 páginasHistory Taking: A Concise Medical HistoryDarian BurkettAinda não há avaliações
- Organization and Presentation of Psychiatric InformationDocumento6 páginasOrganization and Presentation of Psychiatric InformationRoci ArceAinda não há avaliações
- Notes On Psychiatry: TypesDocumento17 páginasNotes On Psychiatry: TypesMAY100% (1)
- Psychiatry Case Clearking Updated Feb April 2018Documento12 páginasPsychiatry Case Clearking Updated Feb April 2018nurulAinda não há avaliações
- Mood StabilizerDocumento2 páginasMood Stabilizernmyza89Ainda não há avaliações
- Psychiatry VIVA Preparation DocumentDocumento24 páginasPsychiatry VIVA Preparation DocumentPhiNguyen83% (6)
- Psychiatry PDFDocumento53 páginasPsychiatry PDFArushiAinda não há avaliações
- Mental H Assessment CWDocumento37 páginasMental H Assessment CWAYO NELSONAinda não há avaliações
- Aids ManiaDocumento3 páginasAids ManiavinodksahuAinda não há avaliações
- Comprehensive review of musical obsessionsdDocumento61 páginasComprehensive review of musical obsessionsdvinodksahuAinda não há avaliações
- 2013 Draft BillDocumento73 páginas2013 Draft Billbluetooth191Ainda não há avaliações
- The Treatment of ClaustrophobiaDocumento8 páginasThe Treatment of ClaustrophobiavinodksahuAinda não há avaliações
- Hormonal Correlations of Premature EjaculationDocumento6 páginasHormonal Correlations of Premature EjaculationvinodksahuAinda não há avaliações
- Assessing Disability in Schizophrenia and OCD Using IDEAS ScaleDocumento5 páginasAssessing Disability in Schizophrenia and OCD Using IDEAS Scalevinodksahu100% (1)
- CBT in DhatDocumento8 páginasCBT in DhatvinodksahuAinda não há avaliações
- Effectiveness of Cognitive Behavioral Therapy On Premature Ejaculation in An Iranian SampleDocumento13 páginasEffectiveness of Cognitive Behavioral Therapy On Premature Ejaculation in An Iranian SamplevinodksahuAinda não há avaliações
- Benefits of Cancer Patients Engaging in Complimentary TherapiesDocumento53 páginasBenefits of Cancer Patients Engaging in Complimentary TherapiesvinodksahuAinda não há avaliações
- Breast Cancer TrreatmentDocumento10 páginasBreast Cancer TrreatmentvinodksahuAinda não há avaliações
- 1311Documento6 páginas1311Ahmed El AlfyAinda não há avaliações
- BMJ Open-2014-Chang PDFDocumento9 páginasBMJ Open-2014-Chang PDFvinodksahuAinda não há avaliações
- Breast Cancer SurvivorsDocumento30 páginasBreast Cancer Survivorsvinodksahu100% (1)
- Claustrophobia VRDocumento8 páginasClaustrophobia VRvinodksahuAinda não há avaliações
- Breast Cancer ActivismDocumento6 páginasBreast Cancer ActivismvinodksahuAinda não há avaliações
- Temperament and EvolutionDocumento35 páginasTemperament and EvolutionvinodksahuAinda não há avaliações
- BRCADocumento7 páginasBRCAvinodksahuAinda não há avaliações
- The Evolving Epidemiology of HIV AIDS.9Documento9 páginasThe Evolving Epidemiology of HIV AIDS.9vinodksahuAinda não há avaliações
- Crucial Conversations For Women in Business SummaryDocumento1 páginaCrucial Conversations For Women in Business Summaryvinodksahu100% (1)
- Special Article: Words: Psycho-Oncology, Cancer, Multidisciplinary Treatment Approach, AttitudesDocumento16 páginasSpecial Article: Words: Psycho-Oncology, Cancer, Multidisciplinary Treatment Approach, AttitudeshopebaAinda não há avaliações
- Depression and Health Related Quality of Life in Breast Cancer PatientsDocumento4 páginasDepression and Health Related Quality of Life in Breast Cancer PatientsvinodksahuAinda não há avaliações
- Holding Slacking Coworkers Accountable DataDocumento4 páginasHolding Slacking Coworkers Accountable DatavinodksahuAinda não há avaliações
- Life-Changing Crucial Conversations SummaryDocumento1 páginaLife-Changing Crucial Conversations SummaryvinodksahuAinda não há avaliações
- Susanne Bengesser - Genetics of Bipolar DisorderDocumento227 páginasSusanne Bengesser - Genetics of Bipolar Disordervinodksahu100% (1)
- Anatomical Organization of The Eye FieldsDocumento11 páginasAnatomical Organization of The Eye FieldsvinodksahuAinda não há avaliações
- Crucial Conversations Book Discussion QuestionsDocumento2 páginasCrucial Conversations Book Discussion Questionsvinodksahu83% (12)
- How To Confront The Workplace BullyDocumento1 páginaHow To Confront The Workplace BullyvinodksahuAinda não há avaliações
- Four Crucial Conversations For Uncertain Times SummaryDocumento1 páginaFour Crucial Conversations For Uncertain Times SummaryvinodksahuAinda não há avaliações
- Holding Slacking Coworkers Accountable SummaryDocumento1 páginaHolding Slacking Coworkers Accountable SummaryvinodksahuAinda não há avaliações
- Weighty Crucial Conversations With Your Child SummaryDocumento1 páginaWeighty Crucial Conversations With Your Child SummaryvinodksahuAinda não há avaliações
- Anxiety Scale - ChildDocumento2 páginasAnxiety Scale - Childbrian@coombsmd.com90% (20)
- Psychiatry OutlineDocumento13 páginasPsychiatry Outlinegemazy123Ainda não há avaliações
- 25 Psychiatric Nursing Mnemonics and Tricks - NurseBuffDocumento24 páginas25 Psychiatric Nursing Mnemonics and Tricks - NurseBuffMelissa100% (3)
- Gluten Free Diet Study On Celiac DiseaseDocumento9 páginasGluten Free Diet Study On Celiac DiseaseJahson WillnotloseAinda não há avaliações
- 72 Children With Oppositional Defiant DisorderDocumento3 páginas72 Children With Oppositional Defiant Disorderapi-83101465Ainda não há avaliações
- Machine Learning Technique Based Wrist Radial Pulse DiagnosisDocumento37 páginasMachine Learning Technique Based Wrist Radial Pulse DiagnosisVarunapriyan KumaranAinda não há avaliações
- Anxiety Treatment Protocol Norton2008 PDFDocumento17 páginasAnxiety Treatment Protocol Norton2008 PDFmirelaAinda não há avaliações
- GC 02 Block 03 1506099755Documento48 páginasGC 02 Block 03 1506099755Van LopezAinda não há avaliações
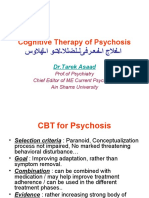
- Cognitive Therapy of PsychosisDocumento18 páginasCognitive Therapy of Psychosisبسمة أملAinda não há avaliações
- Detection of Adult Attention Deficit Hyperactivity Disorder With Cognitive Complaint Experience of A French Memory CenterDocumento9 páginasDetection of Adult Attention Deficit Hyperactivity Disorder With Cognitive Complaint Experience of A French Memory CenterJasonAinda não há avaliações
- The Great Depression - SpeechDocumento2 páginasThe Great Depression - SpeechJams Florendo100% (2)
- Veterinary Surgery and Radiology MCQDocumento66 páginasVeterinary Surgery and Radiology MCQJihad Anad81% (59)
- Clinical Diagnoses Following Zipf'S LawDocumento11 páginasClinical Diagnoses Following Zipf'S LawNicolas DemidovAinda não há avaliações
- Robust Computational Phenotypes in Severe Mental IllnessDocumento86 páginasRobust Computational Phenotypes in Severe Mental IllnessRomulo ElizardoAinda não há avaliações
- Community As ClientDocumento13 páginasCommunity As ClientVirus50% (2)
- 6WG1 e 01 (1 - 2) PDFDocumento688 páginas6WG1 e 01 (1 - 2) PDFmohan89% (9)
- 12SL Statement of Validation and AccuracyDocumento26 páginas12SL Statement of Validation and Accuracycygnus8929Ainda não há avaliações
- Adhd EssayDocumento3 páginasAdhd Essayapi-241238813Ainda não há avaliações
- BSN Nursing Process & Family AssessmentDocumento27 páginasBSN Nursing Process & Family AssessmentLeo Santos MagnoAinda não há avaliações
- Functional Analysis and Treatment of Inappropriate Verbal BehaviorDocumento3 páginasFunctional Analysis and Treatment of Inappropriate Verbal BehaviorMariaAinda não há avaliações
- Medical Errors Malpractice and DefensiceDocumento7 páginasMedical Errors Malpractice and DefensiceAlvaro Rodriguez A.Ainda não há avaliações
- PMK No. 44 TTG Pedoman Manajemen PuskesmasDocumento18 páginasPMK No. 44 TTG Pedoman Manajemen Puskesmasheri heriansyahAinda não há avaliações
- Chief Medical Officer's Annual Report 2023Documento68 páginasChief Medical Officer's Annual Report 2023BernewsAdminAinda não há avaliações
- Autism Quotient Test PDFDocumento3 páginasAutism Quotient Test PDFTonny Aldo Aprillino100% (1)
- SOP Stroke RehabilitationDocumento43 páginasSOP Stroke RehabilitationThanty Putrantii WijayantiAinda não há avaliações
- fUNDA Rationale 2007 EditedDocumento30 páginasfUNDA Rationale 2007 EditedQuia Benjch Uayan100% (1)
- QIM 2011 Abstracts E-BookDocumento150 páginasQIM 2011 Abstracts E-BookAleksandra MaodušAinda não há avaliações
- Latest Inform Enter-GynEyeDocumento4 páginasLatest Inform Enter-GynEyesreevidyaAinda não há avaliações
- Psychiatry (1) 1Documento26 páginasPsychiatry (1) 1esmatAinda não há avaliações
- Clinical: Association Treatment OutcomesDocumento9 páginasClinical: Association Treatment OutcomesAngela RamirezAinda não há avaliações