Escolar Documentos
Profissional Documentos
Cultura Documentos
Predictors of Positive Chest Radiography in Non-Traumatic Chest Pain in The Emergency Department
Enviado por
Hario Tri HendrokoDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Predictors of Positive Chest Radiography in Non-Traumatic Chest Pain in The Emergency Department
Enviado por
Hario Tri HendrokoDireitos autorais:
Formatos disponíveis
Predictors of Positive Chest Radiography in NonTraumatic Chest Pain in the Emergency Department
Nabil Al Zadjali,1 Rasha Al-Senawi,1 Abdullah Al Reesi,1 Ibrahim Al-Zakwani,2 Joe Nemeth,3 Jerey J. Perry 4
Abstract
Objectives: To determine predictors associated with positive chest x-ray nding in patients presenting with non-traumatic chest pain in the Emergency Department (ED). Methods: Health records, including the nal radiology reports of all patients who presented with non-traumatic chest pain and had a chest x-ray performed in an urban Canadian tertiary care ED over four consecutive months were reviewed. Demographic and clinical variables were also extracted. Chest x-ray ndings were categorized as normal (either normal or no signicant change from previous x-rays) or abnormal. Descriptive statistics were used to describe the data. Multivariable logistic regression was used to determine the association between various predictors and chest x-ray nding (positive/negative). Results: The 330 study patients had the following characteristics: mean age 5820 years; female 41% (n=134). Patients chief complaints were only chest pain 75% (n=248), chest pain with shortness of breath 12% (n=41), chest pain with palpitation 4% (n=14), chest pain with other complaints 9% (n=28). Chest x-rays were reported as normal or no acute changes in 81% (n=266) of patients, and abnormal in 19% (n=64) of patients. The most common abnormal chest x-ray diagnoses were congestive heart failure (n=28; 8%) and pneumonia (n=17; 5%). Those with abnormal chest x-ray ndings were signicantly older (71 versus 55 years; p<0.001), had chest pain with shortness of breath (36% versus 11%; p<0.001), had signicant past medical history (39% versus 14%; p<0.001), and were also tachypnoic (31% versus 12%; p<0.001). Conclusion: This study found that patients with non-traumatic chest pain are likely to have a normal chest x-ray if they were young, not tachypnoeic or short of breath, and had no signicant past medical history. A larger study is required to conrm these ndings.
From the 1Department of Emergency Medicine SQU, Muscat, Oman, 2Department of Pharmacy, SQU, Muscat, Oman, 3Department of Emergency Medicine, McGill University, Montreal , QC, Canada, 4Department of Internal Medicine, University of Ottawa, Ottawa, ON, Canada. Received: 29 Aug 2008 Accepted: 21 Nov 2008 Address correspondence and reprint request to: Dr. Rasha Al-Senawi, Department of Accident and Emergency, Sultan Qaboos University Hospital, 123 Al-Khod, Muscat, Sultanate of Oman. E-mail: senawer@yahoo.com
Introduction
adiology accounts for 6-10 % of all health care expenditures and chest radiography examination represents up to 50 % of the whole diagnostic radiology workup performed. It is a common tool used to evaluate patients in the Emergency Department (ED) with a wide variety of suspected chest and non-chest related complaints. Although this modality has been described as inexpensive, it is time consuming and potentially unnecessary in a large number of ED patients.1-5 Presently, chest radiography is a recommended initial screening test in traumatic patients as per the Advanced Trauma Life Support (ATLS) guidelines. In non-traumatic patients, plain lm radiography reveals acute abnormalities in anywhere from 2.5 to 37% of ED patients selected to undergo chest x-ray.3,6-10 The low rate of positive lms in most studies and the wide variability of signicant abnormal lms indicates there is a signicant variation in clinical practice in the use of chest x-ray.11 This suggests that there is a potential for improved eciency in current medical practice through the development of guidelines or a clinical
decision rule.11 There has been a lot of confusion in the literature regarding the utility of chest radiography in an acute setting coupled with the lack of ED specic literature. Most previous studies of chest x-rays are conned to patients with asthma or chronic obstructive pulmonary disease (COPD) with varying recommendations. There have been few studies that have addressed the importance of chest radiography as a screening tool in non-emergency settings. In 1985, Hubbell et al. reviewed the literature on routine chest radiographs in internal medicine wards. They found that abnormalities were found in 36% of the patients but these ndings resulted in treatment changes in only 4% of these patients. This study questions the value of indiscriminate use of chest x-rays. Another review of 997 ED asthmatics found that only 2.2% of adults had abnormal radiographs with all abnormalities occurring in those who had rhonchi or rales, or who were unresponsive to treatment.5 Based on their results, the authors did not recommend routine chest radiography in patients with asthma.2 Another
Oman Medical Journal 2009, Volume 24, Issue 1, January 2009
Predictors of Positive Chest Radiography... Al-Senawi et al.
review of 847 ED patients with COPD found that 16% had acute chest x-ray abnormalities with a quarter of these not predicted by previously developed high-yield criteria (prior congestive heart failure, coronary artery disease, peripheral edema, chest pain, or a white blood cell (WBC) count 15,000 cells/mm3.4,12 The authors of this study recommended routine chest radiography in all ED patients with COPD.4 Others have attempted to predict chest x-ray abnormalities in patients with nontraumatic chest complaints and have been unable to develop sensitive criteria for predicting signicant abnormalities.3,13 These studies did not address a focused clinical question. They attempted to predict abnormal chest x-ray ndings in all the complaints (e.g. productive cough, fever, shortness of breath, palpitation, syncope, headache, traumatic chest pain) and not just patients with chest pain as in our study. This study is attempting to dene reasons behind non-traumatic chest complaints as well as factors associated with positive chest xray nding in an emergency room.
as abnormal. We dened signicant past medical history as the presence of COPD, cancer, asthma or congestive heart failure (CHF). All the data were extracted by one individual, the rst author. Statistical Analyses Descriptive statistics were used to describe patient characteristics and clinical variables. For categorical variables, frequencies and percentages were reported. Dierences between groups were analyzed using Pearsons 2 tests (or Fishers Exact tests for cells less than ve). For continuous variables, means and standard deviations (SD) were presented. Mean dierences between groups were analyzed using Students ttests. A multivariate logistic regression analysis for the outcome of abnormal chest x-ray was conducted. The association of the following variables to an abnormal chest x-ray nding: age, chest pain type, past medical history, respiratory rate, last admitted location as the independent variables were determined. Independent variables were selected based on prior research.2-5 According to Peduzzi and colleagues,14 the useful rule of thumb from simulation studies is that for every parameter in the model, one needs at least ten outcomes. In this study, with the sample size of 330, of which 64 had positive chest x-ray nding, the ratio of positive outcomes to independent variables was approximately 10.7 to 1 (64/6), while the ratio of negative outcomes (n=340; 35%) to independent variables was approximately 44.3 to 1 (266/6). Both of the estimates are well within the recommended threshold. A priori two-tailed level of signicance was set at the 0.05 level. Statistical analyses performed using STATA version 8.2 software.
Methods
Patient Population This study was performed in the ED of an urban teaching hospital with an annual census of 75,000 in Canada. All patients presenting to the ED with chest pain between November 4, 2004 and February 28, 2005 and who underwent chest radiography were enrolled. Patients with a history of acute trauma and patients younger than 18 years of age were excluded. The institutional review board (IRB) approved this study without the need for informed patient consent as no change in patient management took place. Data Collection Health records were reviewed and patients identied from an ED computerized database. All patients (18 years and above) presenting with non-traumatic chest pain during the study period were enrolled into the study The standardized data extraction form for all patients included demographic data, their presenting symptoms to the ED, past medical history, vital signs, physical ndings and a nal discharge diagnosis. In addition, ocial radiologist reports were obtained for each of the patients who underwent chest radiography from the radiology database system (Magic web). Old radiographs were used by radiologists for comparison where available. Chest radiographs were dened as normal if this was the interpretation of the radiologist or if there were no new changes from previous imaging, despite a presence of non-signicant ndings. All other radiographs were dened
Results
A total of 330 patients were enrolled into the study. The demographic and clinical characteristics of the study cohort are shown in Table 1. Patients with positive chest x-ray ndings were signicantly older compared to those that had negative chest x-ray results (71 versus 55 years; p<0.001). They also had signicantly higher proportion of subjects with chest pain and shortness of breath (SOB) or cough than other types of chest pain (36% versus 11%; p<0.001). The positive chest x-ray nding cohort had also higher percentage of patients with signicant past medical history (39% versus 14%; p<0.001) and higher respiratory rate (>16 beats/ minute) (31% versus 12%; p<0.001). Of note also was the fact that those with positive chest x-ray nding had higher proportion of subjects that ultimately required admission in ICU/CCU than with those that had negative chest x-ray nding (19% versus 6%; p=0.003).
Oman Medical Journal 2009, Volume 24, Issue 1, January 2009
Predictors of Positive Chest Radiography... Al-Senawi et al.
Table 1: Demographic and clinical characteristics of the study cohort stratied by chest x-ray ndings (N=330) Characteristics Age, meanSD*, years Male gender, n (%) Chest pain type, n (%) Chest pain with SOB** or cough All other types of chest pain Past medical history (PMH), n (%) Respiratory Rate (RR), n (%) Normal RR (12-16 /minute) Heart Rate (HR), n (%) Normal HR (60-100 /minute) Low HR (<60 /minute) High HR (>100 /minute) Blood Pressure (BP), n (%) Normal BP (SBP*** 100-140 and DBP 50-90 mmHg) High BP (SBP >140 or DBP >90 mmHg) Low BP (SBP <100 or DBP 50 mmHg) Oxygen saturation Normal saturation (95%) Respiratory examination, n (%) Normal Basal Crepitations Decrease Breath Sound Wheezing Bronchial Breathing Cardiovascular examination, n (%) Normal sound Last admitted location, n (%) Discharged home ICU/CCU Normal admission on regular ward 275 (83%) 28 (9%) 27 (8%) 225 (85%) 16 (6%) 25 (9%) 50 (78%) 12 (19%) 2 (3%) 0.003 317 (96%) 256 (96%) 61 (95%) 0.722 283 (86%) 15 (4.6%) 12 (3.6%) 11 (3.3%) 9 (2.7%) 230 (86%) 11 (4.1%) 10 (3.8%) 7 (2.6%) 8 (3.0%) 53 (83%) 4 (6.3%) 2 (3.1%) 4 (6.3%) 1 (1.6%) 0.522 315 (95%) 254 (95%) 61 (95%) 1.000 219 (66%) 102 (31%) 9 (2.7%) 175 (66%) 85 (32%) 6 (2.3%) 44 (69%) 17 (27%) 3 (4.7%) 0.396 277 (84%) 12 (3.6%) 41 (12%) 224 (84%) 10 (3.8%) 32 (12%) 53 (83%) 2 (3.1%) 9 (14%) 0.887 279 (85%) 235 (88%) 44 (69%) <0.001 53 (16%) 277 (84%) 63 (19%) 30 (11%) 236 (88%) 38 (14%) 23 (36%) 41 (64%) 25 (39%) <0.001 <0.001 Total (N=330) 5820 196 (59%) Chest X-Ray Finding Negative (n=266) 5520 159 (60%) Positive (n=64) 7116 37 (58%) P-value <0.001 0.774
*SD: Standard Deviation; **SOB: Shortness of Breath; PMH was dened as the presence of either Chronic Obstructive Pulmonary Disease (COPD), Cancer, Asthma, or Congestive Heart Failure (CHF); ***SBP=Systolic Blood Pressure; DBP=Diastolic Blood Pressure; ICU: Intensive Care Unit; CCU: Critical Care Unit; #P-values were generated using Students ttests, Pearsons 2 test, and Fishers Exact test whenever appropriate.
Oman Medical Journal 2009, Volume 24, Issue 1, January 2009
Predictors of Positive Chest Radiography... Al-Senawi et al.
The most frequent chief complaint was chest pain (n=248; 75%), followed distantly by chest pain with SOB (n=41; 12%), and chest pain with palpitation (n=14; 4%). Other presenting complaints are listed on Table 2. Despite the fact that all the subjects had chest pain, the majority (n=266; 80.6%) had normal chest x-ray nding. Table 2: Chief complaint stratied by Negative and Positive Chest Findings (N=330) Chest Finding Diagnosis Plain Chest Pain (CP) CP with Shortness of Breath CP with Cough CP with Fever CP with Palpitation CP with Syncope CP with Weakness CP with Epigastric Pain CP with Miscellaneous CP: Chest Pain Table 3 showed the most frequent diagnoses stratied by the positive and negative chest x-rays. The most frequent preliminary diagnoses were CHF (n=28; 8%) and pneumonia (n=17; 5%). Table 3: Final diagnoses stratied by Negative and Positive chest ndings (N=330) Chest Finding Diagnosis Normal Pneumonia Congestive Heart Failure Pleural Eusion Cancer Pulmonary Embolism Miscellaneous Negative (n=266) 251 0 0 0 0 0 15 Positive (n=64) 0 17 28 11 6 2 0 Total (%) 251 (76%) 17 (5.2%) 28 (8.5%) 11 (3.3%) 6 (1.8%) 2 (0.6%) 15 (4.6%) Negative (n=266) 213 22 8 3 12 5 0 2 1 Positive (n=64) 35 19 4 1 2 1 1 1 0 Total (%) 248 (75%) 41 (12%) 12 (3.6%) 4 (1.2%) 14 (4.2%)
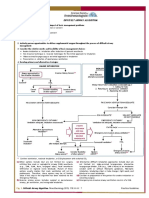
Figure 1 outlines the probability of a positive chest x-ray nding while varying age, generated using multivariable logistic regression. The gure clearly demonstrates that the association is positive. The probability of a positive chest x-ray result increased with age. The graph also indicates that those with chest pain and SOB (or cough), signicant past medical history, and higher respiratory rate had clinically signicantly higher probability of a positive chest x-ray nding than those with other types of chest pain, insignicant past medical history, and normal respiratory rate. Even at the minimum age of the cohort, the probability of having a positive chest x-ray result was already nearly four times higher for those with chest pain and SOB (or cough), signicant past medical history, and higher respiratory rate compared to their counterparts.
1 (0.3%) 3 (0.9%) 1 (0.3%)
Figure 1: A graph of the probability of a positive chest x-ray nding while varying age generated using multivariable logistic regression (N=330).
Discussion
This was the rst study, which looked at patients with nontraumatic chest pain who presented to the ED as well as determining various factors that could potentially predict abnormal chest x-ray ndings. Among the chief complaints observed were chest pain only, chest pain with shortness of breath, and chest pain with palpitation. Only 19% of all non-traumatic chest x-rays were positive. The study also demonstrated that a positive chest x-ray nding was associated with those who were older, had chest pain with shortness of breath, signicant past medical history, and those who were tachypnoeic. Unexpectedly, this study noted that reduced air entry, rhonchi or crackles were not predictive variables although previous studies have showed this to the contrary. This could be due to either
Oman Medical Journal 2009, Volume 24, Issue 1, January 2009
Resperatory Rate
6 (1.8%)
Predictors of Positive Chest Radiography... Al-Senawi et al.
inappropriate documentation of ndings in a very busy ED and/or due to the smaller number of patients in our cohort. By using the multivariable logistic regression model, this study also found that patients age is one of the important predictors to increase the probability of having signicant chest x-ray abnormalities. Two groups of patients could be deduced from this study with regards to chest x-ray nding. High-risk group are those patients who presented to the ED with chest pain associated with cough, SOB, signicant past medical history (COPD, cancer, asthma or CHF) or high respiratory rate. On the other hand, the low-risk patients are those who presented to the ED with chest pain but with no signicant past medical history or with low respiratory rate. Age over 65 years, in the low-risk group, was associated with 15% probability of having a signicant nding on chest x-ray, and the probability of a positive chest x-ray result was increasing with age thereafter. However, in the high-risk group, signicant chest xray abnormalities were found even in younger age groups, and the probability increased dramatically as age increased (Figure 1). This study was conducted at a single center, which is aliated to an Emergency Medicine Residency Training Program. While this was a large, busy ED, the results of this study should be validated in other centers to conrm our ndings. It can be argued that the physical examination assessment is performed by the training residents. Their ndings may dier from one resident to another depending on their training level, which could have aected the ndings. Unfortunately, we could not calculate the kappa to compare the degree of agreement between the residents and the emergency department sta because of inadequate information in the Magic-Web database. In addition, this was a retrospective study, so there was no uniform denition of historical key features as well as a standardization of the physical examination ndings. The character of the chest pain was not included in the study, which could have led to dierent working strategy of patients. The ndings should be interpreted in light of the present limitations.
x-ray requests in the ED in such patients and could potentially lead to a shorter patient stay in the ED. A larger prospective study is required to conrm these ndings.
Acknowledgments
The authors report no conict of interest and no funding has been received in this work.
References
1. Buenger RE. Five thousand acute care/emergency department chest radiographs: comparison of requisitions with radiographic ndings. J Emerg Med. 1988; 6:197-202. 2. Russell NJ. The role of chest radiography in patients presenting with anterior chest pain to the Accident & Emergency Department. J R Soc Med. 1988; 81:626-628. 3. Rothrock SG. High yield criteria for obtaining non-trauma chest radiography in the adult emergency department population. J Emerg. Med. 2002 Jan; Vol 23, No. 2, pp. 117-124. 4. Clinton JE, Yaron M, Tsai SH. Chest radiography in the emergency department. Ann Emerg Med 1986; 15:254-256. 5. Aronson S, Gennis P, Kelly D, Landis R, Gallagher J. The value of routine admission chest radiographs in adult asthmatics. Ann Emerg Med 1989; 18:1206-1208. 6. Diehr P, Wood RW, Bushyhead J. Prediction of pneumonia in outpatients with acute cough-a statistical approach. J Chron Dis 1984; 37:2215-2225. 7. Emermann CL, Cydulka RK. Evaluation of high-yield criteria for chest radiography in acute exacerbation of chronic obstructive pulmonary disease. Ann Emerg Med 1993; 22:680-684. 8. Zieverink SE, Harper AP, Holden RW, Klatte EC, Brittain H. Emergency room radiography of asthma: an ecacy study. Radiology 1982; 145:27-29. 9. Benacerraf BR, McLoud TC, Rhea JT, Tritschler V, Libby P. An assessment of the contribution of chest radiography in outpatients with acute chest complaints: a prospective study. Radiology 1981; 138:293-299. 10. Russell NJ, Pantin CF, Emerson PA, Crichton. The role of chest radiography in patients presenting with anterior chest pain to the Accident and Emergency Departments. J Royal Soc Med 1988; 4:383. 11. Sherman S, Skoney JA, Ravikrishnan KP. Routine chest radio-graphs in exacerbations of chronic obstructive pulmonary disease: diagnostic value. Arch Intern Med 1989; 149:2493-2496. 12. Landis RJ, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33:159-174. 13. Noeller TP, Bessleer R, Meldon SW, et al. Does a normal physical exam preclude the need for chest radiographs in ED patients with non-traumatic chest pain? (abstract) Acad Emerg Med 1998; 6:541-542. 14. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49:1373-1379.
Conclusion
Our study of an urban tertiary care ED found that patients with chest pain are likely to have a normal chest x-ray if they were young, not tachypnoeic or short of breath, and had no signicant past medical history. This could lead to reduction in unnecessary chest
Oman Medical Journal 2009, Volume 24, Issue 1, January 2009
Você também pode gostar
- Jurnal Onko RiaDocumento13 páginasJurnal Onko RiaMuzdatul KhairiahAinda não há avaliações
- Hyper Tiro IdDocumento5 páginasHyper Tiro Idkonstantin balabalaAinda não há avaliações
- (2009) Radiographic Improvement and Its Predictors in Patients With Pulmonary TuberculosisDocumento6 páginas(2009) Radiographic Improvement and Its Predictors in Patients With Pulmonary TuberculosisMohd RahimiAinda não há avaliações
- Cervical Traction For Neck Pain Patients A Clinical Prediction Rule 1266428336Documento4 páginasCervical Traction For Neck Pain Patients A Clinical Prediction Rule 1266428336qwrertyuiopAinda não há avaliações
- 10 - (Rahman) The Relationship Between Chest Tube Size and Clinical Outcome in Pleural InfectionDocumento8 páginas10 - (Rahman) The Relationship Between Chest Tube Size and Clinical Outcome in Pleural InfectionfaisaldanyaniAinda não há avaliações
- Atm 07 05 100Documento10 páginasAtm 07 05 100Farhan IrhamsyahAinda não há avaliações
- Idiopathic First Seizure in Adult Life: Who Be Treated?: ShouldDocumento4 páginasIdiopathic First Seizure in Adult Life: Who Be Treated?: ShouldJessica HueichiAinda não há avaliações
- Jurnal ApendisitisDocumento6 páginasJurnal ApendisitisHilda MarsellaAinda não há avaliações
- Trait Anxiety Predicts Disease-Specific Health Status in Early-Stage Breast Cancer PatientsDocumento9 páginasTrait Anxiety Predicts Disease-Specific Health Status in Early-Stage Breast Cancer PatientsPreda LoredanaAinda não há avaliações
- The Association Between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients With Chest PainDocumento10 páginasThe Association Between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients With Chest PainGrace Angelica Organo TolitoAinda não há avaliações
- Impact of Time From Completion of Neoadjuvant Chemotherapy To Surgery On Survival Outcomes in Breast Cancer PatientsDocumento7 páginasImpact of Time From Completion of Neoadjuvant Chemotherapy To Surgery On Survival Outcomes in Breast Cancer PatientsPani lookyeeAinda não há avaliações
- THR-morbid ObesityDocumento5 páginasTHR-morbid ObesityMohan DesaiAinda não há avaliações
- Iranian Decision Making Abdominal PainDocumento7 páginasIranian Decision Making Abdominal Painghaffari.eli5912Ainda não há avaliações
- Screening Utility of Umbilical Artery Doppler Indices in Patients With PreeclampsiaDocumento6 páginasScreening Utility of Umbilical Artery Doppler Indices in Patients With PreeclampsiaAlhajiAinda não há avaliações
- Chest Tube SizeDocumento10 páginasChest Tube SizeilpollolocoAinda não há avaliações
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDocumento6 páginasSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedAinda não há avaliações
- KJR 14 350Documento11 páginasKJR 14 350sepputriAinda não há avaliações
- Physioooo Research SamplesDocumento5 páginasPhysioooo Research Samplesmeggan3Ainda não há avaliações
- Hta Versus IncidentalomaDocumento10 páginasHta Versus IncidentalomaClaudia IrimieAinda não há avaliações
- Yeung TeenagersDocumento5 páginasYeung TeenagersAnonymous YyLSRdAinda não há avaliações
- CTNeoBC Pooled AnalysisDocumento9 páginasCTNeoBC Pooled AnalysistabaresgonzaloAinda não há avaliações
- 1 Sttri 3Documento6 páginas1 Sttri 3parkfishyAinda não há avaliações
- Peerj 1374Documento12 páginasPeerj 1374David Restu Prasetia ManikAinda não há avaliações
- Abdominal Pain in The ED A 35Documento7 páginasAbdominal Pain in The ED A 35RobertAinda não há avaliações
- US en EndometritisDocumento7 páginasUS en EndometritisRubí FuerteAinda não há avaliações
- Clinical Guideline Diagnosing Syncope Part 1: Value of History, Physical Examination, and ElectrocardiographyDocumento8 páginasClinical Guideline Diagnosing Syncope Part 1: Value of History, Physical Examination, and ElectrocardiographyPriya JainAinda não há avaliações
- Glycemic Control and Radiographic Manifestations of Tuberculosis in Diabetic PatientsDocumento17 páginasGlycemic Control and Radiographic Manifestations of Tuberculosis in Diabetic PatientsGlenda B AjilaAinda não há avaliações
- Chen 2013Documento9 páginasChen 2013Santa Maria PangaribuanAinda não há avaliações
- 1756 0500 6 477 PDFDocumento6 páginas1756 0500 6 477 PDFanon_118437533Ainda não há avaliações
- J Ahj 2019 12 007Documento29 páginasJ Ahj 2019 12 007Adriana MartinsAinda não há avaliações
- 2006-Lepousé - Delirio en Adultos en La Unidad Cuidados PostanestesicosDocumento7 páginas2006-Lepousé - Delirio en Adultos en La Unidad Cuidados PostanestesicosYuribeyAinda não há avaliações
- Yeo Et AlDocumento10 páginasYeo Et AlAna MoraisAinda não há avaliações
- Low-Dose Abdominal CT For Evaluating Suspected Appendicitis: Original ArticleDocumento10 páginasLow-Dose Abdominal CT For Evaluating Suspected Appendicitis: Original ArticleNia MidfordAinda não há avaliações
- Advanced Non-Small Cell Lung Cancer in Patients Aged 45 Years or Younger: Outcomes and Prognostic FactorsDocumento8 páginasAdvanced Non-Small Cell Lung Cancer in Patients Aged 45 Years or Younger: Outcomes and Prognostic FactorsAnnisa DiendaAinda não há avaliações
- Is It Worth Preserving The Uterus? Unanticipated Pathology in Hysterectomy For Pelvic Organ Prolapse (POP)Documento38 páginasIs It Worth Preserving The Uterus? Unanticipated Pathology in Hysterectomy For Pelvic Organ Prolapse (POP)Anonymous kte9KuGAinda não há avaliações
- Early Intervention Can Improve Clinical Outcome of Acute Interstitial PneumoniaDocumento9 páginasEarly Intervention Can Improve Clinical Outcome of Acute Interstitial PneumoniaHerbert Baquerizo VargasAinda não há avaliações
- 9 FullDocumento15 páginas9 FulllipemagalhaesAinda não há avaliações
- Prediction of Pneumonia in A Pediatric Emergency Department: PediatricsDocumento10 páginasPrediction of Pneumonia in A Pediatric Emergency Department: PediatricsLeslie Lindsay AlvarezAinda não há avaliações
- PIH Renal Doppler Pregnancy - CutDocumento4 páginasPIH Renal Doppler Pregnancy - CutAnonymous 9QxPDpAinda não há avaliações
- Ebm SeptemberDocumento29 páginasEbm SeptemberJulius OentarioAinda não há avaliações
- JurnalDocumento6 páginasJurnalIzzyAinda não há avaliações
- Oral AbstractsDocumento210 páginasOral AbstractspascutaAinda não há avaliações
- Factors Associated With Acute and Late Dysphagia in The DAHANCA 6 7 Randomized Trial With Accelerated Radiotherapy For Head and Neck CancerDocumento9 páginasFactors Associated With Acute and Late Dysphagia in The DAHANCA 6 7 Randomized Trial With Accelerated Radiotherapy For Head and Neck CancerNurul Afika LubisAinda não há avaliações
- JPCC 2380 0534 01 0002 PDFDocumento4 páginasJPCC 2380 0534 01 0002 PDFLuiggi D. Chambi MaidaAinda não há avaliações
- Research: Pain Over Speed Bumps in Diagnosis of Acute Appendicitis: Diagnostic Accuracy StudyDocumento7 páginasResearch: Pain Over Speed Bumps in Diagnosis of Acute Appendicitis: Diagnostic Accuracy StudydimasAinda não há avaliações
- Historical Overview: Abstract: Several Studies Have Demonstrated That A Diagnosis Based SolelyDocumento8 páginasHistorical Overview: Abstract: Several Studies Have Demonstrated That A Diagnosis Based SolelyLuh Tu PebriyantiAinda não há avaliações
- Critical Appraisal of Prognostic StudiesDocumento3 páginasCritical Appraisal of Prognostic StudiesDesy Randiahartika Sagita ZukhrinAinda não há avaliações
- Apendicitis y EmbarazoDocumento6 páginasApendicitis y EmbarazoBernardo RomeroAinda não há avaliações
- Psychosomatics. 2010 MarDocumento12 páginasPsychosomatics. 2010 MarMario Gabriel CarignaniAinda não há avaliações
- Back To Cardiology ArticlesDocumento10 páginasBack To Cardiology ArticlesmrezasyahliAinda não há avaliações
- Neoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesDocumento6 páginasNeoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesSubhash SugathanAinda não há avaliações
- HHS Public Access: Achalasia Treatment, Outcomes, Utilization, and Costs: A Population-Based Study From The United StatesDocumento12 páginasHHS Public Access: Achalasia Treatment, Outcomes, Utilization, and Costs: A Population-Based Study From The United StatesInomy ClaudiaAinda não há avaliações
- Detrano 1989Documento7 páginasDetrano 1989Lilims LilithAinda não há avaliações
- Clinical Correlation of Acute Appendicitis With Histopathological Diagnosis: A Prospective StudyDocumento5 páginasClinical Correlation of Acute Appendicitis With Histopathological Diagnosis: A Prospective StudyHarun NasutionAinda não há avaliações
- Screening of Asymptomatic Children For Tuberculosis:: Is A Lateral Chest Radiograph Routinely Indicated?Documento7 páginasScreening of Asymptomatic Children For Tuberculosis:: Is A Lateral Chest Radiograph Routinely Indicated?jayyidahafifahAinda não há avaliações
- PIIS1098301514020567Documento2 páginasPIIS1098301514020567Defriyan RamziAinda não há avaliações
- 2003-Academic Emergency MedicineDocumento154 páginas2003-Academic Emergency MedicinealiceAinda não há avaliações
- Abses HeparDocumento4 páginasAbses HeparIecHa RizkaMaulidaAinda não há avaliações
- Precision in Pulmonary, Critical Care, and Sleep Medicine: A Clinical and Research GuideNo EverandPrecision in Pulmonary, Critical Care, and Sleep Medicine: A Clinical and Research GuideJose L. GomezAinda não há avaliações
- Diagnostic Problems in Tumors of Central Nervous System: Selected TopicsNo EverandDiagnostic Problems in Tumors of Central Nervous System: Selected TopicsAinda não há avaliações
- Low Back Pain in Children and Adolescents: An Algorithmic Clinical ApproachDocumento12 páginasLow Back Pain in Children and Adolescents: An Algorithmic Clinical ApproachHario Tri HendrokoAinda não há avaliações
- Parade - 2017 02 06edDocumento52 páginasParade - 2017 02 06edHario Tri HendrokoAinda não há avaliações
- Magnetic Resonance Imaging Features of Fallopian Tube CarcinomaDocumento3 páginasMagnetic Resonance Imaging Features of Fallopian Tube CarcinomaHario Tri HendrokoAinda não há avaliações
- Laporan Pagi OK IGD 4feb2017 TF Rev1Documento8 páginasLaporan Pagi OK IGD 4feb2017 TF Rev1Hario Tri HendrokoAinda não há avaliações
- J Physiol 2014 Dimaline Jphysiol.2014.272435Documento23 páginasJ Physiol 2014 Dimaline Jphysiol.2014.272435Hario Tri HendrokoAinda não há avaliações
- Thorax00020 0093Documento11 páginasThorax00020 0093Hario Tri HendrokoAinda não há avaliações
- Thorax:: Annual Report OctoberDocumento2 páginasThorax:: Annual Report OctoberHario Tri HendrokoAinda não há avaliações
- Chest X Ray As A Screening Tool For J Trauma Acute Care Surg 2013 Pubmed NcbiDocumento2 páginasChest X Ray As A Screening Tool For J Trauma Acute Care Surg 2013 Pubmed NcbiHario Tri HendrokoAinda não há avaliações
- Thorax00291 0009Documento1 páginaThorax00291 0009Hario Tri HendrokoAinda não há avaliações
- Lung Alert: Chest Wall Tenderness Does Not Exclude Pulmonary EmbolismDocumento1 páginaLung Alert: Chest Wall Tenderness Does Not Exclude Pulmonary EmbolismHario Tri HendrokoAinda não há avaliações
- Fluids, Electrolytes, and Dehydration: Mark Davenport and S. H. S. SyedDocumento12 páginasFluids, Electrolytes, and Dehydration: Mark Davenport and S. H. S. SyedHario Tri HendrokoAinda não há avaliações
- Femtosecond Laser Cataract Surgery: Sepehr Feizi, MDDocumento1 páginaFemtosecond Laser Cataract Surgery: Sepehr Feizi, MDHario Tri HendrokoAinda não há avaliações
- Pi Is 1319453411000580Documento5 páginasPi Is 1319453411000580Hario Tri HendrokoAinda não há avaliações
- 10 Penile Cancer PDFDocumento29 páginas10 Penile Cancer PDFHario Tri HendrokoAinda não há avaliações
- Ambulance Response Protocol DraftDocumento3 páginasAmbulance Response Protocol DraftCommand CenterAinda não há avaliações
- Telaah Jurnal KGDDocumento17 páginasTelaah Jurnal KGDriska eka fatma HasibuanAinda não há avaliações
- Sepsis: Dr. Cristhian Huanca Panozo Medicina InternaDocumento25 páginasSepsis: Dr. Cristhian Huanca Panozo Medicina InternafranciAinda não há avaliações
- Cardiac Trauma 2Documento4 páginasCardiac Trauma 2charlietuna1Ainda não há avaliações
- Lesson Plan On CPRDocumento3 páginasLesson Plan On CPRanimesh pandaAinda não há avaliações
- Standard Assessment Form For PG Courses Subject - Emergency MedicineDocumento18 páginasStandard Assessment Form For PG Courses Subject - Emergency MedicineAbhi ThamminainaAinda não há avaliações
- Chest TubeDocumento8 páginasChest TubeTaufik Nur YahyaAinda não há avaliações
- Chapter 1 Answer KeyDocumento2 páginasChapter 1 Answer Keyashleymurrieta2005Ainda não há avaliações
- Heat EmergenciesDocumento3 páginasHeat EmergenciesScott KAinda não há avaliações
- Code Blue StepsDocumento2 páginasCode Blue StepshardeepAinda não há avaliações
- Press Ganey and PainDocumento13 páginasPress Ganey and PainmeganAinda não há avaliações
- MdLuvw UnknownDocumento42 páginasMdLuvw Unknownmohammed ahmedAinda não há avaliações
- Basic First Aid.Documento132 páginasBasic First Aid.Christian PhelpsAinda não há avaliações
- Zachary Knable Resume 12-23 - No Contact InfoDocumento1 páginaZachary Knable Resume 12-23 - No Contact Infoapi-644926887Ainda não há avaliações
- A Brief OverviewDocumento10 páginasA Brief Overviewphat lippAinda não há avaliações
- First Aid Course Powerpoint 4 5hDocumento47 páginasFirst Aid Course Powerpoint 4 5hAndrea Ponce100% (2)
- Product - 978 1 61669 400 5Documento2 páginasProduct - 978 1 61669 400 5Jigar GandhiAinda não há avaliações
- BLS & AclsDocumento112 páginasBLS & AclsPriya SharmaAinda não há avaliações
- Week No. 3: Rizal Technological UniversityDocumento23 páginasWeek No. 3: Rizal Technological UniversityEdrei MercadoAinda não há avaliações
- EM CurriculumDocumento150 páginasEM CurriculumAd MinAinda não há avaliações
- 2012 BLS HCP Exam Binder C and D 01 20 2012Documento19 páginas2012 BLS HCP Exam Binder C and D 01 20 2012Chandler Bearden100% (2)
- First Aid Basics A2Documento1 páginaFirst Aid Basics A2bmdesign123Ainda não há avaliações
- Manajemen Code Blue Di Ruang Covid-19-1Documento57 páginasManajemen Code Blue Di Ruang Covid-19-1Dwi ayu oktaveniAinda não há avaliações
- The Sample of PediatricsDocumento47 páginasThe Sample of PediatricsWaseem UllahAinda não há avaliações
- Medico-Legal Aspect of InjuryDocumento25 páginasMedico-Legal Aspect of InjuryShahriar Shaon100% (1)
- Cardiopulmonary Resuscitation in Low-Resource SettingsDocumento10 páginasCardiopulmonary Resuscitation in Low-Resource SettingsVICTORIA GONZALES ESPADAAinda não há avaliações
- Emergency Medical Technician Student HandbookDocumento27 páginasEmergency Medical Technician Student HandbookMartinRampersadAinda não há avaliações
- CPR Procedure For GRDDocumento4 páginasCPR Procedure For GRDAngelie PantajoAinda não há avaliações
- Special Articles: Awake Intubation Intubation After Induction of General AnesthesiaDocumento1 páginaSpecial Articles: Awake Intubation Intubation After Induction of General AnesthesiaOKE channelAinda não há avaliações
- Full Download Emergency Care in Athletic Training 1st Edition Grose Test BankDocumento35 páginasFull Download Emergency Care in Athletic Training 1st Edition Grose Test Banksaabatmandearnestus100% (35)