Escolar Documentos
Profissional Documentos
Cultura Documentos
Chronic Allograft Nephropathy Score Before Sirolimus Rescue Predicts Allograft Function in Renal Transplant Patients
Enviado por
Dr. Antik BoseDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Chronic Allograft Nephropathy Score Before Sirolimus Rescue Predicts Allograft Function in Renal Transplant Patients
Enviado por
Dr. Antik BoseDireitos autorais:
Formatos disponíveis
NIH Public Access
Author Manuscript
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Published in final edited form as: Transplant Proc. 2007 ; 39(1): 9498. doi:10.1016/j.transproceed.2006.10.017.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Chronic Allograft Nephropathy Score Before Sirolimus Rescue Predicts Allograft Function in Renal Transplant Patients
Antik Basu, John L. Falcone, Henkie P. Tan, David Hassan, Igor Dvorchik, Komal Bahri, Ngoc Thai, Parmjeet S. Randhawa, Amadeo Marcos, Thomas E. Starzl, and Ron Shapiro Thomas E. Starzl Transplantation Institute, Pittsburgh, Pennsylvania, USA
Abstract
Chronic allograft nephropathy (CAN) is a major indication for initiation of sirolimus (SRL) in renal transplantation (TX) to prevent deterioration of renal function. We evaluated whether the CAN score at time of sirolimus rescue (SRL-R) predicts renal allograft function. CAN score is the sum of the following 4 categories: glomerulopathy (cg, 0 3), interstitial fibrosis (ci, 03), tubular atrophy (ct, 03), and vasculopathy (cv, 03). This is a retrospective cohort study of renal transplant recipients from July 2001 to March 2004. Immunosuppression consisted of preconditioning with rabbit anti-thymocyte globulin or alemtuzumab and maintenance with tacrolimus (TAC) monotherapy with spaced weaning, if applicable, SRL-R was achieved by conversion from TAC, or by addition to reduced doses of TAC. Ninety patients received SRL. Thirty-three of these patients met the inclusion criteria of the following: (1) receipt of SRL for >6 months, and (2) follow-up of 6 months. There were 16 patients in the lowCAN (04) group and 17 patients in the high-CAN (>4) group. Cockcroft-Gault (C-G) glomerular filtration rate (GFR) was calculated at SRL-R and at 1, 3, 6, and 12 months. The GFR was significantly better in the low-CAN group at 1, 3, and 6 months. A trend toward an improved GFR was present at 12 months in the low-CAN group (P = .16). CAN scoring at the time of SRL-R predicts recovery of renal allograft function (as measured using GFR), and should be used in preference to biochemical markers (Cr and C-G GFR), which may not be reliable predictors.
The most common causes of late renal allograft loss are chronic renal allograft dysfunction (CRAD) and death with a functioning graft (DWFG). CRAD is chronic allograft nephropathy (CAN). 2 ,3
A major cause of
CAN is progressive long-term condition characterized by interstitial fibrosis, tubular atrophy, vascular occlusive changes, and glomerulosclerosis. There are 2 distinct phases of injury: an initial phase and a later phase. Each phase represents cumulative and progressive damage from both immunologic and nonimmunologic etiologies. Chronic changes are scored for the glomerulopathy (cg), interstitial fibrosis (ct), tubular atrophy (ct), and vasculopathy (cv). It is possible to apply relative weightings and calculate overall severity scores (such as the CAN score) using this coding system. In the Banff classification, the following histological patterns have been defined: CAN (a): interstitial fibrosis, tubular atrophy and/or loss, glomerulopathy, and mesangial matrix increase (grades 13a); CAN (b): interstitial fibrosis, tubular atrophy and/or loss, together with typical vascular lesions and mononuclear infiltrates (grades 1 3b); and calcineurin inhibitor (CNI) nephrotoxicity: hyaline changes particularly in the afferent arterioles of the glomerulus and vacuolation of tubular epithelial cells.
The CNIs Tacrolimus (TAC) and cyclosporine (CsA) have been mainstays of chronic immunosuppression because of a decreased incidence of acute rejection and also improved
Address reprint requests to A. Basu, Thomas E Starzl Transplantation Institute, MUH 7 South, 3459 Fifth Avenue, Pittsburgh, PA 15213.
Basu et al.
Page 2
allograft and patient survival rates in recent decades. CNI drugs cause progressive renal injury related to direct nephrotoxicity; the continued use of CNI agents contributes to the 5 development of CAN. There is a high incidence of CAN in patients using Tacrolimus as maintenance immunosuppression 67% at 2 years after renal transplantation. Thus, although there has been a dramatic increase in kidney graft survival with TAC, CNI-related 7 nephrotoxicity may compromise long-term outcomes. The reduction or withdrawal of CNI in combination with alternative immunosuppressive regimens such as sirolimus (SRL) has become a popular practice in renal transplantation.
SRL is a macrocyclic lactone antibiotic produced by Streptomyces hygroscopicus. It inhibits the mammalian target of rapamycin (mTOR), a kinase in costimulatory and cytokine-driven pathways of T-cell regulation. SRL lacks the acute and chronic nephrotoxic profile of the CNIs. Because it inhibits growth-factorinduced proliferation of fibroblasts, endothelial cells,
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
810
hepatocytes, and smooth muscle cells, it offers an important alternative to CNI drugs to prevent CAN.
11
The reduction or withdrawal of CNI in combination with sirolimus rescue (SRL-R) has been a growing topic of interest. Improvements in renal function have been shown in patients with CAN (b) and CNI nephrotoxicity with SRL-R therapy. Allograft function was less likely to improve for patients with CAN (a) or serum creatinine level >400 mol/L.
12
At the American Transplant Congress (ATC) in 2003, we presented the University of Pittsburgh Medical Centers (UPMC) experience with SRL -R in kidney and kidney/pancreas transplant recipients.
13
Other clinical studies have tried to identify independent factors that
predict successful conversion from TAC to SRL in patients with CAN. Among the factors that predict success in conversion from TAC to SRL in CAN are serum creatinine level at the time of conversion, and degree of CAN, as assessed using the CAN score at the time of SRL conversion. No clinical studies have evaluated the allograft outcomes in antibody preconditioned patients with regard to SRL-R from TAC-based immunosuppression. The purpose of this current retrospective study was to determine if the CAN score at the time of SRL-R predicts subsequent renal allograft function. Changes in calculated glomerular filtration rate (GFR) were evaluated in patients who had received antibody preconditioning with rabbit antithymocyte globulin or alemtuzumab to see if CAN score predictor of subsequent renal allograft function.
14,15
14
2,3
at SRL-R was a significant
PATIENTS AND METHODS
This retrospective cohort study used the in-house database, Electronic Data Interface for Transplantation (EDIT), at the Thomas E. Starzl Transplantation Institute at the University of Pittsburgh Medical Center. Evaluation of all the renal allograft recipients from July 1, 2001 to March 31, 2004 yielded 190 patients diagnosed with CAN based on renal biopsy specimen. Of these 190 patients with CAN, 90 had received SRL-R from TAC. From this patient population, 33 satisfied the inclusion criteria of the following: (1) no extra-renal transplant, (2) receipt of SRL for at least 6 months, and (3) follow-up maintenance of at least 6 months. Patients satisfying all inclusion criteria were divided into 2 groups based on the biopsy-reported CAN scoring done by a blinded pathologist using the 1997 Banff classification system. CAN score was calculated as the sum of the following 4 categories: glomerulopathy (eg. 0 3), interstitial fibrosis (ci, 03), tubular atrophy (ct, 03), and vasculopathy (cv, 03). Of these 33 patients, 16 were in the lowCAN score group with a score 4, and 17 were in the high-CAN score group with a score >4. Review was made of the clinical course, including laboratory values, dosage and trough levels of immunosuppressive agents, and steroid and antibody
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Basu et al.
Page 3
treatment of rejection episodes. Data collection was approved by the Institutional Review Board (IRB) of the UPMC.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript RESULTS
Immunosuppressive preconditioning had been achieved with either Thymoglobulin 5 mg/kg (Sangstat, Fremont, Calif, United States (n = 30) or Campath-1 H 30 mg (Berlex, Montvale, NJ, United States) (n = 3) preoperatively followed by TAC monotherapy, with target trough levels of around 10 ng/mL. The IRB of the University of Pittsburgh judged the above immunosuppressive regimen to be within the boundaries of historically based standard treatment, not needing formal IRB approval. The Presbyterian University Hospital Innovative Practices Committee and the Pharmacy and Therapeutics Committee both approved the protocol. After biopsy-reported CAN scoring, SRL conversion was accomplished either by converting (n = 19) from TAC to SRL or by an addition (n = 14) of SRL to tapered doses of TAC Eight patients in the low-CAN score group had TAC abruptly changed to SRL, whereas the remaining 8 patients in the low-CAN score group had SRL added to tapered doses of TAC; the other patients in each category belonged to the high CAN score group. SRL levels were maintained at a trough serum level of 510 ng/mL either as monotherapy or when used with TAC. TAC levels were maintained at a trough level between 5 and 10 ng/mL when used with SRL. Spaced weaning was not carried out for patients on SRL monotherapy. Patients with acute rejection based on biopsy specimen were treated with corticosteroids and mycophenolate mofetil (MMF) as indicated (low-CAN, n = 3; high-CAN, n = 4). Serum creatinine level was determined for each patient at the time of SRL-R. CockcroftGault glomerular filtration rate (GFR) was calculated for each patient at the time of SRL-R and at 1,3, 6, and 12 months after SRL-R. The low-CAN and high-CAN groups were compared for significant differences in GFR changes with Mann-Whitney U tests using SPSS 12.0 software (Chicago, Ill, United States), defining statistical significance as P < .05. The dynamics of change in the GFR in the low-CAN score and high-CAN score groups were evaluated using the Wilcoxon signed rank test using SPSS 12.0 software, defining statistical significance as P < .05.
1618
The characteristics of the study population (n = 33) at the time before SRL-R are shown in Table 1. The median age in the low-CAN and high-CAN groups was 50.5 years and 50.0 years, respectively. The low-CAN group was 56% male and the high-CAN group was 59% male with no age or gender differences between CAN groups. The median GFR for the low-CAN and highCAN groups were 33.0 mL/min and 33.3 mL/min, respectively (P = .51). The time from transplantation to the initiation of SRL-R and the serum creatinine values at the time of SRL-R were not statistically significant between the groups (P = .12 and P = .36, respectively). The changes in GFR after SRL-R for patients in the low-CAN and high-CAN groups are shown in Table 2. For patients in the low-CAN group, the average GFR increased significantly from baseline at 1, 3, and 6 months after SRL-R (P = .006, P = .002, and P = .004, respectively)
(Wilcoxon signed rank test). The net change in GFR in this group was +2.8 mL/min at 12 months; however, this positive change was not statistically significant ( P = .21). In the highCAN group, there was no significant change in GFR at 1, 3, 6, or 12 months from initiation of SRL-R (P = .78, P = .49, P = .6, and P = .61, respectively) (Wilcoxon signed rank test).
At the time of SRL-R, there was no difference in GFR values between the groups. However, statistically significant changes in GFR dynamics did occur between the 2 patient groups at 1, 3, and 6 months (P = .008, P = .001, and P = .004, respectively) (Mann-Whitney U test). At
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Basu et al.
Page 4
12 months, the change in GFR was not significantly better in the low-CAN score group (P = . 16).
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
There was 1 patient death each in the low-CAN group and the high-CAN group during the 1-year follow-up period (Table 2). The patient in the low-CAN group died of cardiovascular causes with a failing allograft during the eighth month following SRL-R. The patient in the high-CAN group suffered from bipolar disorder and died during the 12th month after SRL-R with a functioning allograft.
Patient survival, graft survival, and serum creatinine level year after SRL-R are shown in Table 3, and are not significantly different. One graft was lost in the low-CAN group in a 75-year-old woman after she developed pulmonary aspergillosis in the ninth month following SRL-R.
DISCUSSION
CAN is a major determinant of CRAD leading to worsening allograft function and allograft loss after renal transplantation. Traditional CNI-based therapies are being reevaluated because they cause direct nephrotoxicity and worsen CAN. The mammalian target of rapamycin (mTOR) inhibitor SRL has been recently investigated as a subsequent substitution therapy for CNI therapy. Because of its lack of direct nephrotoxicity, low side effect profile, antitumor activity, and effectiveness. SRL-R is an intensely studied area in renal transplantation, using the initial benefits of TAC while reducing long-term exposure using SRL.
Previous comparisons of renal transplant recipients with CAN (n = 51) receiving SRL-R with a historical control group (n = 292) receiving SRL-R did not show any differences in patient survival or allograft survival during a period of 5 years of follow-up (unpublished data from the University of Pittsburgh). This result suggests that patients receiving SRL-R had no benefit of therapy, but raised the possibility that many of these patients had undergone SRL-R when CAN was too advanced. The current study suggests that a cohort of patients with a CAN score 4 will benefit from SRL-R as measured by significantly improved GFR measurements for up to 6 months of follow-up after SRL-R.
This study shows that CAN scoring at the time of SRL-R can predict recovery of renal allograft function as measured using changes in GFR. Statistical significance for improved GFR was reached at 1, 3, and 6 months after SRL-R in the low-CAN group compared with the high-CAN group. For patients within the low-CAN group, the mean GFR increased significantly at 1, 3, and 6 months after SRL-R; GFR improvement did not reach statistical significance after 1 year of follow-up (P = .21), although a net change of +2.8 mL/min was seen. Within the high-CAN group, improvement in GFR did not occur. In spite of these differences, there were no differences in patient or graft survival or quality of kidney function.
Factors predicting the success of SRL-R are still under investigation for different patient groups. Previous studies have shown that serum creatinine level <2.8 mg/dL, degree of CAN, and proteinuria <800 mg/d can predict renal allograft function after SRL-R.
14,15,19
In the report by Diekmann et al, although proteinuria was the only significant independent factor, responders had a significantly lower grade of CAN and significantly lower grade of vascular fibrous intimal thickening than nonresponders. This analysis specifically demonstrates that patients with a CAN score 4 can benefit from SRL-R. In this study, patients in the low-CAN group had a median serum creatinine level of 2.9 mg/dL, higher than the significant level shown in the study by Egidi et al. Patients in the high-CAN group had a median serum creatinine level of 2.5 mg/dL. Differences were not significant between the groups (P = .36). Serum creatinine level may not be a reliable predictor of recovery of renal allograft function in these patients.
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
15
14
Basu et al.
Page 5
Proteinuria was not systemically assessed at the time of SRL-R in the patient groups in this study. This information could have provided additional insight about the value of proteinuria in predicting SRL-R success, and is a limitation of this study. Sankaranarayanan et al showed that the Chronic Allograft Damage Index (CADI) score at the time of conversion from CNI to SRL was a reliable predictor of renal outcome. The CADI consists of the 6 histological changes characteristic of chronic rejection, ie, interstitial inflammation and fibrosis, glomerular sclerosis and mesangial matrix increase, vascular 20 intimal proliferation, and tubular atrophy. The Banff schema and CADI score provide equivalent information. The change in GPR was significantly worse in the high-CADI (median, 7.5) group compared with the low-CADI (median, 3) group at 3, 6, and 12 months 19 following conversion. In this study, there were 15 patients in the low-CADI score group and 16 patients in the high-CADI score group.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
19
19
MDRD formula, unlike the Cockcroft-Gault formula in our study. The small number of patients (n = 33) in this study makes it less powerful to determine smaller differences between groups. However, even given the low power of this study, there were statistically significant changes in GFR not only within the low-CAN group, but also between groups at 1, 3, and 6 months after SRL-R. The changes in GFR were not significant between the low-CAN and high-CAN groups at 12 months, although a trend toward an improvement in change in GFR was noted for the low-CAN group. Likewise, the retrospective nature of this study is suboptimal. Variations in the antibody used for preconditioning and differences in the SRL-R protocol decrease the validity of the study design. However, this analysis was performed in an unselected group of patients of varying ethnicity with prior kidney transplants and with varying number of comorbidities.
Two kinds of protocols exist for switching from CNI-based to SRL-based immunosuppression. In the protocols with an overlap period between CNI and SRL therapy, there exists the potential for excessive initial immunosuppression and the need for careful therapeutic drug monitoring. immediate conversion to SRL has the advantage of simplicity and avoids potential
19
GFR, however, was calculated using the
The
overimmunosuppression. In the protocols with immediate conversion, the possibility of acute rejection might be increased, if the time to achieve target SRL levels is prolonged.
21
In a single-center, randomized controlled trial 40 renal transplant recipients between 6 months and 8 years post-transplantation were randomly assigned to remain on their CNI (CsA or TAC) or to switch to SRL. The principal inclusion criteria in this study was suboptimal renal function, defined as serum creatinine level between 120 and 400 mol/L (1.364.52 mg/dL). Two patients never took their study drugs, leaving 19 patients in each group. At 12 months, there was a significant change in GFR following conversion to SRL (12.9 mL/min, 95% confidence interval, 6.1 19.7; P < .001). No patient in either group experienced an acute rejection episode. The availability of SRL allows substitution for CNI therapy with a nonnephrotoxic agent and potentially avoids risk of acute rejection.
21
21
No
attempt was made in this study to quantify the burden of CAN prior to switching to SRL.
21
We did not do protocol kidney transplant biopsies in our study. Such biopsies could help in documenting the progression of CAN in the low-CAN and high-CAN score groups during the period of follow-up. The Rapamune Maintenance Regimen Trial showed that early CsA withdrawal from a SRL-CsA-steroid (ST) regime improved renal function and histology. Protocol mandated biopsies were done at engraftment and at 12 and 36 months after transplantation. All 6 componenets of the CADI score were lower in the patients in the SRLST group, who had undergone early CsA withdrawal. Inflammation and tubular atrophy scores decreased significantly in the SRL-ST groups between 12 and 36 months.
22
22
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Basu et al.
Page 6
In summary, the presence of a CAN score 4 was predictive of improved GFR at 1, 3, and 6 months after SRL-R compared with a group of patients with a CAN score >4. CAN scoring may be a more reliable predictor of allograft function rather than serum creatinine level or Cockcroft-Gault GFR measurements. Prospective SRL-R trials should be done to confirm the conclusions of this study.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Acknowledgments
Support provided by Thomas E Starzl Transplantation Institute.
References
1. Cecka, JM. The UNOS Scientific Renal Transplant Registry2000. In: Cecka, JM.; Teraski, PI., editors. Clinical Transplants 2000. 1. Los Angeles, Calif: UCLA Immunogenetics Center; 2001. p. 1 2. Solez K, Axelsen RA, Benediktsson H, et al. International standardization of criteria for the histologic diagnosis of renal allograft rejection: the Banff working classification of kidney transplant pathology. Kidney Int 1993;44:411. [PubMed: 8377384] 3. Racusen LC, Solez K, Colvin RB, et al. The Banff 97 working classification of renal allograft pathology. Kidney Int 1999;55:712. 4. Nankivell BJ, Borrows RJ, Fung CL-S, et al. The natural history of chronic allograft nephropathy. N Engl J Med 2003;349:2326. [PubMed: 14668458] 5. Flechner SM. Calcineurin inhibitor free protocols in organ transplantation. Curr Opin Organ Transpl 2004;9:383. 6. Solez K, Vincenti F, Filo RS. Histopathologic findings from 2-year protocol biopsies from a US multicenter kidney transplant trial comparing Tacrolimus with Cyclosporine: a report of the FK 506 kidney transplant study group. Transplantation 1998;66:1736. [PubMed: 9884269]
7. McKane W, Kangana C, Preston R, et al. Treatment of calcineurin inhibitor toxicity by dose reduction plus introduction of mycophenolate mofetil. Transplant Proc 2001;33:1224. [PubMed: 11267268]
8. Chueh S-CJ, Kahan BD. Clinical application of sirolimus in renal transplantation: an update. Transplant Int 2005;18:261. 9. Sehgal SN. Rapamune (RAPA, rapamycin, sirolimus): mechanism of action immunosuppressive effect results from blockade of signal transduction and inhibition of cell cycle progression. Clin Biochem 1998;31:335. [PubMed: 9721431] 10. Basu A, Tan HP, Shapiro R. Sirolimus. Curr Opin Organ Transpl 2003;8:299. 11. Morales JM, Wrammer L, Kreis H, et al. Sirolimus does not exhibit nephrotoxicity compared to cyclosporine in renal transplant recipients. Am J Transplant 2002;2:436. [PubMed: 12123209] 12. Weber T, Abendroth D, Schelzig H. Rapamycin rescue therapy in patients after kidney transplantation: first clinical experience. Transplant Int 2005;18:151. 13. Basu A, Ramkumar M, Gray E, et al. Sirolimus as rescue treatment in kidney and kidneypancreas transplantation in patients receiving tacrolimus-based immunosuppression (abstract). Am J Transplant 2003;3:353. 14. Egidi MF, Cowan PA, Naseer A, et al. Conversion to sirolimus in solid organ transplantation: a single-center experience. Transplant Proc 2003;35:131S. [PubMed: 12742485] 15. Diekmann F, Budde K, Oppenheimer F, et al. Predictors of success in conversion from calcineurin inhibitor to sirolimus in chronic allograft dysfunction. Am J Transplant 2004;4:1869. [PubMed: 15476488] 16. Starzl TE, Murase N, Abu-Elmagd K, et al. Tolerogenic immunosuppression for organ transplantation. Lancet 2003;361:1502. [PubMed: 12737859] 17. Shapiro R, Jordan M, Basu A, et al. Kidney transplantation under a tolerogenic regimen of recipient pre-treatment and low-dose postoperative immunosuppression, with subsequent weaning. Ann Surg 2003;238:520. [PubMed: 14530723] 18. Shapiro R, Basu A, Tan H, et al. Kidney transplantation under minimal immunosuppression after pretransplant lymphoid depletion with thymoglobulin or campath. J Am Coll Surg 2005;200:505. [PubMed: 15804464]
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Basu et al.
Page 7
19. Sankaranarayanan N, Balarezo F, Alleman K, et al. Chronic allograft damage index (CADI) scoring at conversion from calcineurin inhibitors (CI) to sirolimus predicts renal outcome in kidney transplant recipients (abstract). Am J Transplant 2004;4:296. 20. Isoniemi H, Taskinen E, Hayry P. Histological chronic allograft damage index accurately predicts chronic renal allograft rejection. Transplantation 1994;58:1195. [PubMed: 7992362] 21. Watson CJE, Firth J, Williams PF, et al. A randomized controlled trial of late conversion from CNI-based to sirolimus-based immunosuppression following renal transplantation. Am J Transplant 2005;5:2496. [PubMed: 16162200] 22. Mota A, Arias M, Taskinen EI, et al. Sirolimus-based therapy following early cyclosporine withdrawal provides significantly improved renal histology and function at 3 years. Am J Transplant 2004;4:953. [PubMed: 15147430]
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Basu et al.
Page 8
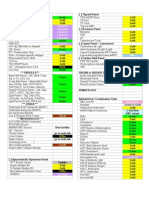
Table 1
Patient Information Before Initiation of SRL-R
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Low-CAN Group (n = 16) CAN score Age (y) Male:female ratio Time from transplantation to SRL-R (d) Cockcroft-Gault GFR (mL/min) SCr at SRL-R (mg/dL) Abbreviation: SCr, serum creatinine. Note: All values are expressed as median. Median, 3.5 50.5 9:7 208 33.0 2.9
High-CAN Group (n = 17) Median, 6.0 50.0 10:7 372 33.3 2.5
.66
.12 .51 .36
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Basu et al.
Page 9
Table 2
Effect of SRL-R on Change ( ) in GFR in Patients in the Low-CAN and High-CAN Groups (Mann-Whitney U Test)
Low-CAN Group Cockcroft-Gault GFR at SRL-R (mL/min) GFR 1 mo after SRL-R (mL/min) GFR 3 mo after SRL-R (mL/min) GFR 6 mo after SRL-R (mL/min) GFR 12 mo after SRL-R (mL/min) Note: All values are expressed as median. 33.0 +11.6 +9.1 +10.2 +2.8 (n=15) High-CAN Group 33.3 +2.05 1.4 0.05 2.75 (n=16) P .51 .008 .001 .004 .16
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Basu et al.
Page 10
Table 3
Patient and Graft Survival Rates and Serum Creatinine Levels 1 Year After SRL-R
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Low-CAN Group Patient survival Graft survival Death-censored graft survival Median SCr (mg/dL) 94% 87.5% 93.3% 3.0
High-CAN Group 94% 94% 100% 2.85
Transplant Proc. Author manuscript; available in PMC 2010 October 25.
Você também pode gostar
- Lavender Lavender Lavender Lavender Lavender Lavender: UrineDocumento3 páginasLavender Lavender Lavender Lavender Lavender Lavender: UrineJonathan A. Sarmiento67% (6)
- Abstracts of The 2016 TTS CongressDocumento929 páginasAbstracts of The 2016 TTS CongresspksdfpksdAinda não há avaliações
- Rosary Med BottleDocumento2 páginasRosary Med BottlescrugglenampAinda não há avaliações
- Acute Renal Failure in Critically Ill Surgical Patients PDFDocumento7 páginasAcute Renal Failure in Critically Ill Surgical Patients PDFRomán Jiménez LópezAinda não há avaliações
- Nefrectomia OFF Clamp Vs ON ClampDocumento7 páginasNefrectomia OFF Clamp Vs ON Clampfelipe laraAinda não há avaliações
- Literatur Tentang AllergiDocumento9 páginasLiteratur Tentang Allergifajar alatasAinda não há avaliações
- Liver TransplantDocumento16 páginasLiver TransplantNephrology On-DemandAinda não há avaliações
- BTT 4437 Koch 010909Documento6 páginasBTT 4437 Koch 010909Achmad DainuriAinda não há avaliações
- Jco 2001 19 18 3852Documento9 páginasJco 2001 19 18 3852Luis SanchezAinda não há avaliações
- HLA-Matched Kidney Transplantation in The Era of Modern Immunosuppressive TherapyDocumento6 páginasHLA-Matched Kidney Transplantation in The Era of Modern Immunosuppressive TherapyDavid FallaAinda não há avaliações
- Model For End-Stage Liver Disease (MELD) and Allocation of Donor LiversDocumento6 páginasModel For End-Stage Liver Disease (MELD) and Allocation of Donor LiversIna MartianaAinda não há avaliações
- Sarcopenia Defined by Psoas Muscle Index Independently Predicts Long Term Survival in Post Liver TransplantDocumento14 páginasSarcopenia Defined by Psoas Muscle Index Independently Predicts Long Term Survival in Post Liver TransplantSvt Mscofficial2Ainda não há avaliações
- TP 0000000000001513Documento5 páginasTP 0000000000001513Muhammad RiefkyAinda não há avaliações
- Annsurg00185 0122Documento6 páginasAnnsurg00185 0122Fajr MuzammilAinda não há avaliações
- Sharawey2011 PDFDocumento7 páginasSharawey2011 PDFIkram DibAinda não há avaliações
- Safety and Efficacy of Levofloxacin Versus Rifampicin in Tuberculous Meningitis: An Open-Label Randomized Controlled TrialDocumento6 páginasSafety and Efficacy of Levofloxacin Versus Rifampicin in Tuberculous Meningitis: An Open-Label Randomized Controlled TrialSri AgustinaAinda não há avaliações
- Paper 017Documento6 páginasPaper 017made dediAinda não há avaliações
- Misra 2012Documento7 páginasMisra 2012Carlos RiquelmeAinda não há avaliações
- TransfusiDocumento9 páginasTransfusiabbhyasa5206Ainda não há avaliações
- Kolagocarsinoma PDFDocumento7 páginasKolagocarsinoma PDFBerlyan RuslanAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 17: OncologyNo EverandComplementary and Alternative Medical Lab Testing Part 17: OncologyAinda não há avaliações
- RRP Radical ProstatectomyDocumento6 páginasRRP Radical ProstatectomybojanvuckovicAinda não há avaliações
- Urinary Neutrophil Gelatinase-Associated Lipocalin (NGAL) For The Detection of Acute Kidney Injury After Orthotopic Liver TransplantationDocumento3 páginasUrinary Neutrophil Gelatinase-Associated Lipocalin (NGAL) For The Detection of Acute Kidney Injury After Orthotopic Liver TransplantationRadias ZasraAinda não há avaliações
- Management of Liver CirrhosisDocumento4 páginasManagement of Liver Cirrhosisfarkad rawiAinda não há avaliações
- Contoh Jurnal Meta AnalisisDocumento17 páginasContoh Jurnal Meta AnalisisMia Audina Miyanoshita100% (1)
- Hypothermic Machine Preservation in Human Liver Transplantation: The First Clinical SeriesDocumento10 páginasHypothermic Machine Preservation in Human Liver Transplantation: The First Clinical SeriesRodolpho ViégasAinda não há avaliações
- Papillary Microcarcinoma of The Thyroid-Prognostic Significance of Lymph Node Metastasis and MultifocalityDocumento10 páginasPapillary Microcarcinoma of The Thyroid-Prognostic Significance of Lymph Node Metastasis and MultifocalityAZ RPAinda não há avaliações
- Journal of Antimicrobial Chemotherapy Volume Issue 2016Documento7 páginasJournal of Antimicrobial Chemotherapy Volume Issue 2016Ulima Mazaya GhaisaniAinda não há avaliações
- Survival PcaDocumento6 páginasSurvival PcaMuhammad Arie Wibisono RangkutiAinda não há avaliações
- Diagnosis Dan Pentalaksanaan Acute Kidney Injury Pada Pasien Sirosis: Rekomendasi Revisi Konsensus Dari International Club of AscitesDocumento14 páginasDiagnosis Dan Pentalaksanaan Acute Kidney Injury Pada Pasien Sirosis: Rekomendasi Revisi Konsensus Dari International Club of AscitesNur UlayatilmiladiyyahAinda não há avaliações
- Joy 1998Documento9 páginasJoy 1998Nguyễn Đức LongAinda não há avaliações
- Glomerular and Tubular Kidney Stress Test: New Tools For A Deeper Evaluation of Kidney FunctionDocumento4 páginasGlomerular and Tubular Kidney Stress Test: New Tools For A Deeper Evaluation of Kidney FunctionPaola ZuluagaAinda não há avaliações
- Radical Vs Partial Nephrectomy in Small Renal MassesDocumento41 páginasRadical Vs Partial Nephrectomy in Small Renal MassesTamer.AbouYoussif .AbouYoussifAinda não há avaliações
- BCSH Diagnosis and Management of PlasmacytomasDocumento14 páginasBCSH Diagnosis and Management of PlasmacytomasEva YustianaAinda não há avaliações
- 2017 Article 584Documento6 páginas2017 Article 584Victoria ViurcosAinda não há avaliações
- Jurnal KK 2006-1Documento9 páginasJurnal KK 2006-1Devvi Riasari BunardiAinda não há avaliações
- Out 5Documento11 páginasOut 5Kie Amelia SuwantoAinda não há avaliações
- Acute Allograft Rejection in Liver Transplant Recipients: Incidence, Risk Factors, Treatment Success, and Impact On Graft FailureDocumento12 páginasAcute Allograft Rejection in Liver Transplant Recipients: Incidence, Risk Factors, Treatment Success, and Impact On Graft Failurenathalialusman98Ainda não há avaliações
- Analysis of The Risk Factors of Untransplantable Recurrence After Primary Curative Resection For Patients With Hepatocellular CarcinomaDocumento8 páginasAnalysis of The Risk Factors of Untransplantable Recurrence After Primary Curative Resection For Patients With Hepatocellular CarcinomaJoão Gabriel Ferreira ArgondizziAinda não há avaliações
- Outcomes After Listing For Liver Transplant in Patients With Acute-on-Chronic Liver Failure - The Multicenter North American Consortium For The Study of End-Stage Liver Disease ExperienceDocumento9 páginasOutcomes After Listing For Liver Transplant in Patients With Acute-on-Chronic Liver Failure - The Multicenter North American Consortium For The Study of End-Stage Liver Disease ExperienceRubia Moresi Vianna De OliveiraAinda não há avaliações
- Preoperative Proteinuria Is Associated With Increased Rates of Acute Kidney Injury After Partial NephrectomyDocumento9 páginasPreoperative Proteinuria Is Associated With Increased Rates of Acute Kidney Injury After Partial NephrectomyyuliyantoAinda não há avaliações
- Does Advanced Cirrhosis With Affect The: Portosystemic ShuntingDocumento5 páginasDoes Advanced Cirrhosis With Affect The: Portosystemic ShuntingThuvija DarshiniAinda não há avaliações
- 17TOHJDocumento4 páginas17TOHJAriffa DiazAinda não há avaliações
- Rodrigues 2010Documento7 páginasRodrigues 2010Илија РадосављевићAinda não há avaliações
- Gurusamy Et Al-2011-Cochrane Database of Systematic ReviewsDocumento4 páginasGurusamy Et Al-2011-Cochrane Database of Systematic ReviewsfiskaderishaAinda não há avaliações
- Acute Pancreatitis and Hepatic FailureDocumento7 páginasAcute Pancreatitis and Hepatic FailureRestu TriwulandaniAinda não há avaliações
- PSB MGCH - OdpDocumento22 páginasPSB MGCH - OdpdrpsbAinda não há avaliações
- JCTH 2016 00035Documento8 páginasJCTH 2016 00035Rengganis PutriAinda não há avaliações
- Abnormal Pre-Operative Creatinine Levels and Renal Failure Following Abdominal Aortic Aneurysm Repair TDocumento3 páginasAbnormal Pre-Operative Creatinine Levels and Renal Failure Following Abdominal Aortic Aneurysm Repair TMALINI LAinda não há avaliações
- Survival After Transarterial Embolization For Spontaneous Ruptured Hepatocellular CarcinomaDocumento5 páginasSurvival After Transarterial Embolization For Spontaneous Ruptured Hepatocellular CarcinomaRollin SidaurukAinda não há avaliações
- Pandrowala2021 Article PortalAnnularPancreasPAPAnUndeDocumento8 páginasPandrowala2021 Article PortalAnnularPancreasPAPAnUndeAdeTriansyahEmsilAinda não há avaliações
- JurnalDocumento6 páginasJurnalmade dediAinda não há avaliações
- Long-Term Outcomes of Hepatitis B Virus-Related Cirrhosis Treated With Nucleos (T) Ide AnalogsDocumento10 páginasLong-Term Outcomes of Hepatitis B Virus-Related Cirrhosis Treated With Nucleos (T) Ide AnalogsZulfiana NabilaAinda não há avaliações
- Model For End Stage Liver Disease (MELD) and Child-TurcottePugh (CTP) PDFDocumento4 páginasModel For End Stage Liver Disease (MELD) and Child-TurcottePugh (CTP) PDFPaulus AnungAinda não há avaliações
- Child Turcotte Pugh: Correlation Between Neutrophil To Lymphocyte Ratio With in Liver Cirrhosis PatientsDocumento8 páginasChild Turcotte Pugh: Correlation Between Neutrophil To Lymphocyte Ratio With in Liver Cirrhosis PatientsainunnadzAinda não há avaliações
- Cha BH Clin Endosc. 2021 Survival Benefit of Intraductal Radiofrequency Ablation For Malignant Biliary Obstruction Meta Ce-2020-254Documento7 páginasCha BH Clin Endosc. 2021 Survival Benefit of Intraductal Radiofrequency Ablation For Malignant Biliary Obstruction Meta Ce-2020-254Byung ChaAinda não há avaliações
- 2014 Kemeny Kras Influence Recurrence PatternDocumento15 páginas2014 Kemeny Kras Influence Recurrence Patternnasifahsankhan4Ainda não há avaliações
- Expression of Bone Morphogenetic Proteins 4, 6 and 7 Is Downregulated in KidneyDocumento11 páginasExpression of Bone Morphogenetic Proteins 4, 6 and 7 Is Downregulated in KidneyJosé Guadalupe Pinedo MuñozAinda não há avaliações
- ProcalcitoninaDocumento16 páginasProcalcitoninaOscar Enrique Peña QuembaAinda não há avaliações
- Evaluation of Neutrophiltolymphocyte Ratio NLR and Itscorrelation With Severity of Liver Cirrhosis Based On Childturcott PDFDocumento6 páginasEvaluation of Neutrophiltolymphocyte Ratio NLR and Itscorrelation With Severity of Liver Cirrhosis Based On Childturcott PDFSilent StalkerAinda não há avaliações
- SC 2015242Documento7 páginasSC 2015242resi ciruAinda não há avaliações
- Complementary and Alternative Medical Lab Testing Part 8: UrologyNo EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyNota: 3 de 5 estrelas3/5 (1)
- Cellular and Physiological Mechanisms of New-Onset Diabetes Mellitus After Solid Organ TransplantationDocumento12 páginasCellular and Physiological Mechanisms of New-Onset Diabetes Mellitus After Solid Organ TransplantationDr. Antik BoseAinda não há avaliações
- Acanthosis Nigricansin PCOS Patients and Its Relation With Type 2 Diabetes Mellitus and Body Mass at A Tertiary Care Hospital in Southern IndiaDocumento3 páginasAcanthosis Nigricansin PCOS Patients and Its Relation With Type 2 Diabetes Mellitus and Body Mass at A Tertiary Care Hospital in Southern IndiaDr. Antik BoseAinda não há avaliações
- A Critical Appraisal of Methods To Grade Transplant Glomerulitis in Renal Allograft BiopsiesDocumento11 páginasA Critical Appraisal of Methods To Grade Transplant Glomerulitis in Renal Allograft BiopsiesDr. Antik BoseAinda não há avaliações
- TMP E572Documento6 páginasTMP E572FrontiersAinda não há avaliações
- Alemtuzumab Pre-Conditioning With Tacrolimus Monotherapy in Pediatric Renal TransplantationDocumento7 páginasAlemtuzumab Pre-Conditioning With Tacrolimus Monotherapy in Pediatric Renal TransplantationDr. Antik BoseAinda não há avaliações
- Alemtuzumab Pre-Conditioning With Tacrolimus Monotherapy in Pediatric Renal TransplantationDocumento7 páginasAlemtuzumab Pre-Conditioning With Tacrolimus Monotherapy in Pediatric Renal TransplantationDr. Antik BoseAinda não há avaliações
- Purification, Peptide Sequencing, Modelling and Characterisation of Extracellular Laccase Secreted by Pleurotus Sajorcaju MTCC 141Documento2 páginasPurification, Peptide Sequencing, Modelling and Characterisation of Extracellular Laccase Secreted by Pleurotus Sajorcaju MTCC 141Dr. Antik BoseAinda não há avaliações
- Transplantation of en Bloc Kidneys From Very Small Pediatric DonorsDocumento1 páginaTransplantation of en Bloc Kidneys From Very Small Pediatric DonorsDr. Antik BoseAinda não há avaliações
- Impact of Genomic Sequence Variability On Quantitative PCR Assays For Diagnosis of Polyomavirus BK InfectionDocumento6 páginasImpact of Genomic Sequence Variability On Quantitative PCR Assays For Diagnosis of Polyomavirus BK InfectionDr. Antik BoseAinda não há avaliações
- The Penumbra System: A Mechanical Device For The Treatment of Acute Stroke Due To ThromboembolismDocumento5 páginasThe Penumbra System: A Mechanical Device For The Treatment of Acute Stroke Due To ThromboembolismDr. Antik BoseAinda não há avaliações
- Tomatoes Versus Lycopene in Oxidative Stress and Carcinogenesis: Conclusions From Clinical TrialsDocumento11 páginasTomatoes Versus Lycopene in Oxidative Stress and Carcinogenesis: Conclusions From Clinical TrialsDr. Antik BoseAinda não há avaliações
- Purification, Peptide Sequencing and Modelling of Ostreolysin From Pleurotus Ostreatus Strain Plo5. Formation of A Modified Ostreolysin With Anticancer Activity Against Cancer Cell LinesDocumento23 páginasPurification, Peptide Sequencing and Modelling of Ostreolysin From Pleurotus Ostreatus Strain Plo5. Formation of A Modified Ostreolysin With Anticancer Activity Against Cancer Cell LinesDr. Antik BoseAinda não há avaliações
- A Comparison of Physiological & Biochemical Changes of Ricinus Communis L. Leaf in Fresh and Polluted Environment.Documento2 páginasA Comparison of Physiological & Biochemical Changes of Ricinus Communis L. Leaf in Fresh and Polluted Environment.Dr. Antik BoseAinda não há avaliações
- Adjuvant Effect and TLR4 Mediated Activation of Macrophages by Polysaccharide From Polyporus AlbicansDocumento21 páginasAdjuvant Effect and TLR4 Mediated Activation of Macrophages by Polysaccharide From Polyporus AlbicansDr. Antik BoseAinda não há avaliações
- Purification and Characterization of Isozyme 1 and 2 of Acid Phosphatase From Cicer ArietinumDocumento2 páginasPurification and Characterization of Isozyme 1 and 2 of Acid Phosphatase From Cicer ArietinumDr. Antik BoseAinda não há avaliações
- Purification and Characterization of Alkaline Phosphatse From Pleurotus Sajor-CajuDocumento2 páginasPurification and Characterization of Alkaline Phosphatse From Pleurotus Sajor-CajuDr. Antik BoseAinda não há avaliações
- Purification of Urease From Pleurotus Sajor-Caju. Characterization of GTPase Activity of UreG and Biochemical Properties of The EnzymeDocumento1 páginaPurification of Urease From Pleurotus Sajor-Caju. Characterization of GTPase Activity of UreG and Biochemical Properties of The EnzymeDr. Antik BoseAinda não há avaliações
- Adjuvant Effect and TLR-4 Mediated Activation of Macrophages by Polysaccharide From Polyporus AlbicansDocumento2 páginasAdjuvant Effect and TLR-4 Mediated Activation of Macrophages by Polysaccharide From Polyporus AlbicansDr. Antik BoseAinda não há avaliações
- Purification, Peptide Sequencing and Study of Anti-Proliferative Activity of Laccase Against Liver Cancer Cell Line HepG2 and Human Breast Cancer Cell Line MCF7Documento1 páginaPurification, Peptide Sequencing and Study of Anti-Proliferative Activity of Laccase Against Liver Cancer Cell Line HepG2 and Human Breast Cancer Cell Line MCF7Dr. Antik BoseAinda não há avaliações
- Purification and Characterisation of Alkaline Phosphatase From Fruticose Lichen UsneaDocumento2 páginasPurification and Characterisation of Alkaline Phosphatase From Fruticose Lichen UsneaDr. Antik BoseAinda não há avaliações
- Patterson - Allergic Diseases 6th EdDocumento370 páginasPatterson - Allergic Diseases 6th Edvasile100% (2)
- 2.PCC Bp3iDocumento36 páginas2.PCC Bp3iRSUD INDRAMAYU PMKPAinda não há avaliações
- Occupational Therapy - Kids Health Information: Scar ManagementDocumento4 páginasOccupational Therapy - Kids Health Information: Scar Managementmuambany1Ainda não há avaliações
- Wellness Check PrintableDocumento2 páginasWellness Check PrintablethubtendrolmaAinda não há avaliações
- Prob PDFDocumento12 páginasProb PDFwallace120Ainda não há avaliações
- A Report On Depression: Mental HealthDocumento12 páginasA Report On Depression: Mental HealthArchiev KumarAinda não há avaliações
- Systematic Review - The Effectiveness ofDocumento15 páginasSystematic Review - The Effectiveness ofSabrinaAinda não há avaliações
- Medicinal Plant (Rahul Sharma) ChambaDocumento17 páginasMedicinal Plant (Rahul Sharma) ChambaRahul SharmaAinda não há avaliações
- Diagnosis of PregnancyDocumento23 páginasDiagnosis of PregnancyNeelesh BhandariAinda não há avaliações
- Hospital PharmacyDocumento13 páginasHospital PharmacySridivya SrihariAinda não há avaliações
- Benefits at A Glance: TexasDocumento10 páginasBenefits at A Glance: Texasakula_rupeshAinda não há avaliações
- Corrected Ortho QsDocumento48 páginasCorrected Ortho QsMuhamad Danial Kholili Al-JaloriAinda não há avaliações
- CNA Practice TestDocumento12 páginasCNA Practice TestJoe Prempeh50% (4)
- Branches of ZoologyDocumento3 páginasBranches of ZoologyVivek Morya100% (1)
- Masterfile Let ReviewerDocumento644 páginasMasterfile Let ReviewerApril Claire Pineda Manlangit50% (4)
- Pharmacology of Oleanolic Acid and Ursolic Acid: Review ArticleDocumento12 páginasPharmacology of Oleanolic Acid and Ursolic Acid: Review ArticlepunitAinda não há avaliações
- Genotropin RefresherDocumento4 páginasGenotropin RefresherJessica BascoAinda não há avaliações
- Final Announcement - 6721760944 PDFDocumento23 páginasFinal Announcement - 6721760944 PDFthifla farhaniAinda não há avaliações
- 2006 TOUCH FOR HEALTH Annual Meeting ReporDocumento80 páginas2006 TOUCH FOR HEALTH Annual Meeting Reporlectavares100% (2)
- Game-Based Cognitive-Behavioral Therapy (GB-CBT) LEER PDFDocumento7 páginasGame-Based Cognitive-Behavioral Therapy (GB-CBT) LEER PDFkarenAinda não há avaliações
- Intravenous TherapyDocumento30 páginasIntravenous TherapyKoass14 2012Ainda não há avaliações
- Components of General Anesthesia: UnconsciousnessDocumento17 páginasComponents of General Anesthesia: UnconsciousnessDanieleAinda não há avaliações
- UtangDocumento11 páginasUtangpyriadAinda não há avaliações
- Adult Drug Court Discretionary Grant Program FY 2019 Competitive Grant AnnouncementDocumento49 páginasAdult Drug Court Discretionary Grant Program FY 2019 Competitive Grant AnnouncementepraetorianAinda não há avaliações
- WEB VTH 01292009Documento28 páginasWEB VTH 01292009Dave L100% (1)
- Biokimia NeurupsikiatriDocumento40 páginasBiokimia Neurupsikiatrisuyudi kimikoAinda não há avaliações
- J&J CompanyDocumento127 páginasJ&J CompanyRam TyagiAinda não há avaliações
- Carrubba Botanical Guide RDocumento247 páginasCarrubba Botanical Guide Rafridikhanjan100% (3)