Escolar Documentos
Profissional Documentos
Cultura Documentos
(Walter 1209 Prednisona 1 en Infant
Enviado por
Erick MattosDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
(Walter 1209 Prednisona 1 en Infant
Enviado por
Erick MattosDireitos autorais:
Formatos disponíveis
From www.bloodjournal.org by on March 10, 2011. For personal use only.
1999 94: 1209-1217
Prednisone Response Is the Strongest Predictor of Treatment Outcome in Infant Acute Lymphoblastic Leukemia
Michael Drdelmann, Alfred Reiter, Arndt Borkhardt, Wolf-Dieter Ludwig, Nicolai Gtz, Susanne Viehmann, Helmut Gadner, Hansjrg Riehm and Martin Schrappe
Updated information and services can be found at: http://bloodjournal.hematologylibrary.org/cgi/content/full/94/4/1209 Articles on similar topics may be found in the following Blood collections: Clinical Trials and Observations (3095 articles) Information about reproducing this article in parts or in its entirety may be found online at: http://bloodjournal.hematologylibrary.org/misc/rights.dtl#repub_requests Information about ordering reprints may be found online at: http://bloodjournal.hematologylibrary.org/misc/rights.dtl#reprints Information about subscriptions and ASH membership may be found online at: http://bloodjournal.hematologylibrary.org/subscriptions/index.dtl
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved.
From www.bloodjournal.org by on March 10, 2011. For personal use only.
CLINICAL OBSERVATIONS, INTERVENTIONS, AND THERAPEUTIC TRIALS
Prednisone Response Is the Strongest Predictor of Treatment Outcome in Infant Acute Lymphoblastic Leukemia
By Michael Do rdelmann, Alfred Reiter, Arndt Borkhardt, Wolf-Dieter Ludwig, Nicolai Go tz, Susanne Viehmann, Helmut Gadner, Hansjo rg Riehm, and Martin Schrappe for the ALL-BFM Group
To define prognostic factors in infant acute lymphoblastic leukemia (ALL), the outcome of 106 infants (age I12 months) during 3 consecutive multicenter trials of the Berlin-FrankfurtMu nster group (ALL-BFM 83, 86, and 90) was retrospectively analyzed according to presenting features and early in vivo response to prednisone. The prednisone response was defined as the cytoreduction (number of blood blasts per microliter at day 8) to a 7-day prednisone prephase and 1 intrathecal dose of methotrexate on day 1. Prednisone good responder (PGR; F1,000 blasts/L) received conventional therapy and prednisone poor responder (PPR; H1,000 blasts/ L) received intensified therapy. Infant ALL was characterized by a high incidence of a white blood cell count greater than 100 103/L (57%), central nervous system leukemia (24%), lack of CD10 expression (59%), 11q23 rearrangement (49%) including the translocation t(4;11) (29%), and a comparatively high proportion of PPR (26%), which were all significantly associated with inferior outcome by univariate analysis. The estimated probability for an event-free survival at 6 years (pEFS) was by far better for PGR compared with PPR, who had a dismal prognosis despite intensified treatment (pEFS, 53% 6% v 15% 7%, P .0001). Infant PGR, who were less than 6 months of age (n 40), lacked CD10 expression (n 43), and/or had an 11q23 rearrangement (n 17) fared significantly better compared with corresponding PPR, as indicated by a pEFS of 44% 8%, 49% 8%, and 41% 12%, respectively. In multivariate analysis, PPR was the strongest adverse prognostic factor (relative risk, 3.3; 95% confidence interval, 1.9 to 5.8; P F .0001). Infants with PGR, comprising a major subgroup (74%) among infants, might successfully be treated with conventional therapy, whereas PPR require new therapeutic strategies, including early treatment intensification or bone marrow transplantation in first remission. 1999 by The American Society of Hematology.
HE IDENTIFICATION OF prognostic factors and evolution of risk-adapted therapy for children with acute lymphoblastic leukemia (ALL) represents one of the success stories in modern clinical oncology. However, despite marked advances in therapy of childhood ALL,1 the probability of event-free survival (pEFS) for infants is approximately 35% only, irrespective of different treatment protocols.2-10 Early relapse rather than excessive toxic complications has been identied as the major factor responsible for the poor outcome in infant ALL. However, the young age of infants predisposes them to suffering from late effects of therapy, in particular to the development of neuropsychological toxicity.9,11,12 Therefore, the current debate centers around whether and which infants will need intensication of front-line therapy, including bone marrow transplantation (BMT) or other innovative treatment strategies.4,5,9,13-17 Because of the rarity of infants among children with ALL, the denition of independent parameters predicting outcome has been difficult. Age less than 6 months,2,4 white blood cell count (WBC) 50 103/L,2,5 pro-B-phenotype with lack of CD10 expression,5,15,18 cytogenetic abnormalities of chromosome band 11q23,5 the translocation t(4;11),7,14,19 and most recently rearrangement of the mixed-lineage leukemia (MLL) gene at chromosome band 11q2313-15,20,21 have been related to the poor prognosis in infant ALL. In trial ALL-BFM 83, the Berlin-Frankfurt-Mu nster (BFM) group has demonstrated the prognostic signicance of blast cell reduction in peripheral blood to a 7-day prednisone prephase and 1 intrathecal dose of methotrexate on day 1 (prednisone response) as a parameter for early treatment response. Thus, a new independent risk factor called the prednisone poor response (PPR) was generated that identies approximately 10% of all children with ALL with an pEFS of less than 50%.22 In subsequent ALL-BFM studies,8,23-25 and conrmed by othBlood, Vol 94, No 4 (August 15), 1999: pp 1209-1217
ers,26,27 the prednisone response has emerged as the strongest predictor of outcome in childhood ALL. To verify whether the prednisone response could be used as a reliable stratication factor in infant ALL, we retrospectively analyzed the outcome of 106 infants with ALL according to presenting features and initial response to prednisone treatment. Our results showed that the prednisone response was the strongest prognostic factor in infant ALL and might be used as a stratication factor in risk-adapted treatment protocols for infant ALL.
PATIENTS AND METHODS Patient characteristics. Between October 1, 1983 and March 31, 1995, 3,829 evaluable children with previously untreated ALL were enrolled onto 3 consecutive multicenter trials (ALL-BFM 83, 86, and 90). One hundred nineteen (3.1%) were infants 12 months of age, of whom 106 were evaluable for this study. Thirteen infants did not meet the study criteria for evaluation: acute myeloid leukemia, pre-existing Fanconi anemia (n 2), death before start of treatment (n 2), major From the Department of Pediatric Hematology and Oncology, Medical School Hannover, Hannover, Germany; the Oncogenetic Laboratory, University of Gieen, Gieen, Germany; the Department of Hematology, Oncology and Tumor Immunology, Robert-Ro ssleClinic, Charite , Humboldt University Berlin, Berlin, Germany; and St Anna Kinderspital, Vienna, Austria. Submitted November 13, 1998; accepted April 14, 1999. Address reprint requests to Michael Do rdelmann, MD, Medical School Hannover, Childrens Hospital, Department of Pediatric Hematology/Oncology, Carl Neuberg Str.1, 30625 Hannover, Germany; e-mail: bfm.studie@MH-Hannover.DE. The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. section 1734 solely to indicate this fact. 1999 by The American Society of Hematology. 0006-4971/99/9404-0005$3.00/0
1209
From www.bloodjournal.org by on March 10, 2011. For personal use only.
1210
RDELMANN ET AL DO
protocol violation that was not enforced by the course of treatment or disease (n 7), patient treated according to pilot protocol (n 1), and patient treated in nonmember hospital (n 1). This series included 47 cases previously reported.8,22 For all studies, informed consent from the guardians was obtained for each patient. The treatment protocols had been approved by the local ethical committee. The diagnosis of ALL and extramedullary disease was based on standard morphologic studies and cytochemical staining of leukemic cells as reported previously.8,22,23 Central nervous system (CNS) disease at diagnosis was dened by a WBC count of greater than 5 cells/L with identiable blasts in cerebral spinal uid (CSF) or by a pathological mass detected by cranial computed tomography, with or without CSF pleocytosis. Blast cell immunophenotype,28 karyotype,29 ploidy,30 and screening for the MLL fusion transcripts MLL/AF4, MLL/AF9, and MLL/ENL by reverse transcriptase-polymerase chain reaction (RT-PCR)31 were determined as described previously. Therapy stratication. In all trials, patients were stratied into 1 of 3 treatment arms; there was no specic therapy branch for infants. In ALL-BFM 83, the leukemic cell burden as indicated by the BFM risk factor (RF 0.2 log [blasts 1] 0.06 liver 0.04 spleen, with organ size in centimeters below costal margin)32 was used for stratication. Children with an RF less than 1.2 were assigned to the standardrisk group (SRG). Patients with an RF between 1.2 and 1.7 were stratied into the medium-risk group (MRG) or were stratied into the high-risk group (HRG) if they had an RF 1.7 or 5% marrow blasts on day 40. In addition, the prednisone response was prospectively evaluated for its prognostic signicance, but not yet used for stratication. The number of leukemic blasts in blood was calculated on day 8 from the absolute leukocyte count and the percentage of blasts in a peripheral blood smear. All samples were centrally reviewed. The presence of more than 1,000 blasts/L blood blasts on day 8 was dened as PPR.22 Retrospectively, all PPR in trial ALL-BFM 83 met the high-risk criteria used for this protocol and received high-risk therapy. In trials ALL-BFM 86 and 90, the prednisone response was used as an overriding stratication factor in combination with the RF. Assignment to SRG and MRG required a prednisone good response (PGR; 1,000/L blood blasts on day 8). SRG was also dened by an RF less than 0.8, no CNS disease, no mediastinal mass, and non-T immunophenotype. Patients were classied at high risk if they had a PPR or 5% marrow blasts on day 33 or an acute undifferentiated leukemia. In addition, patients with a translocation t(9;22) were considered as high risk, regardless of their therapy response.8,23 In all trials, neither the translocation t(4;11) nor age less than 1 year was considered as a stratication factor. Treatment. Details of protocols ALL-BFM 83, 86, and 90 were reported previously.8,22,23 Steroid prephase, induction, reinduction, and intrathecal therapy were comparable for SRG and MRG infants within trials ALL-BFM 83 through 90. Infants who were less than 1 year of age at the intended time of cranial irradiation (CRT at 24 to 26 weeks after initial diagnosis of ALL) received neither preventive (12 Gy) nor curative (20/18 Gy) CRT. The major differences between all trials have been (1) the replacement of intermediate-dose methotrexate (ID-MTX; 500 mg/m2 4 times) in trial ALL-BFM 83 by high-dose methotrexate (HD-MTX; 5 g/m2 4 times) in trials ALL-BFM 86 and 90 during consolidation and (2) the introduction of different elements to high-risk treatment. Statistical analysis. EFS was calculated from the date of diagnosis to the last follow-up or to the rst event (failure to achieve remission, early death, resistant leukemia, relapse, or death of any cause). Patients who failed to achieve a complete response were assigned to a failure time of 0. The Kaplan-Meier method was used to estimate survival rates with comparisons based on the 2-sided log-rank test.33 Standard errors were calculated using the formula of Greenwood.34 Multivariate risk analysis to estimate the prognostic impact of prednisone response on pEFS was performed using Cox proportional hazards regression
analysis.35 Differences in clinical and biological characteristics at time of diagnosis were analyzed by Fishers exact test or Mann-Whitney U-test. The data represent patient follow-up through July 31, 1998. The median observation time for all patients in complete remission (CR) was 5.5 years; and for the infants in the most recent trial ALL-BFM 90, the median observation time was 4.9 years (range, 2.6 to 7 years). Computations were performed using SAS (Statistical Analysis System Version 6.12; SAS Institute Inc, Cary, NC). RESULTS
Table 1 depicts the presenting features of the evaluated infants. Distributions of patient characteristics were comparable between all trials, except for a higher proportion of PPR in trial ALL-BFM 86 (41%) compared with trials ALL-BFM 83 (15%) and 90 (20%). The 55 girls and 51 boys ranged in age from 5
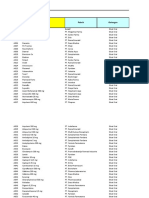
Table 1. Treatment Outcome According to Presenting Features in Infants With ALL (n 106)
Feature n (%) pEFS SE (%)
P Value
Sex Female Male Age (mo) 6 6 12 WBC (103/L) 100 100 BFM RF 1.7 1.7 CNS disease Present Absent Cytogenetics* Evaluable Normal 11q23 rearranged t(4;11) Other abnormalities Not evaluable Immunophenotype* Evaluable B-lineage Pro-B-ALL c-/pre-B ALL pro-T AUL CD 10 CD10 CD10 Myeloid marker (1) Present Absent Prednisone response* Evaluable Good (1,000/L) Poor (1,000/L)
55 (52) 51 (48) 50 (47) 56 (53) 46 (43) 60 (57) 87 (82) 19 (18) 25 (24) 81 (76) 59 18 (31) 29 (49) 17 12 (20) 47 104 52 (50) 47 (45) 3 (3) 2 (2) 62 (59) 42 (41) 29 (28) 75 (72) 105 78 (74) 27 (26)
46 7 39 7 32 6 56 7 52 8 37 6 47 6 26 10 19 8 51 6 38 7 56 12 28 8 18 9 42 14 50 7
.35
.009
.04
.06
.0008
.03 .004
30 7 56 7
.005
35 6 55 8 45 6 40 9
.02
.7
53 6 15 7
.0001
*Percentage of evaluated infants. Patients included in 11q23 rearranged. One infant with WBC of 407,000/L at diagnosis and a t(4;11) could not be evaluated for prednisone response due to exchange transfusion before day 8.
From www.bloodjournal.org by on March 10, 2011. For personal use only.
INFANT ACUTE LYMPHOBLASTIC LEUKEMIA, PROGNOSIS
1211
days to 12 months (median, 5.8 months). WBC ranged from 1 to 1,290 103/L (median, 120 103/L). CNS disease was present in one fourth of the infants. The pro-B immunophenotype predominated with 50%, followed by the common-B and pre-B immunophenotype in 25% and 20% of the infants each. Fifty-nine percent of infants were CD10, and 28% expressed 1 or more myeloid antigens in addition to lymphoid markers. Successful cytogenetic studies were performed on 59 infants (56%). One third had a normal karyotype. We observed 1 patient with hyperdiploidy (DNA index 1.16). Three infants presented with numerical aberrations (2 with trisomy 8 and 1 with trisomy 10); all were PPR. We found a high frequency of structural chromosomal aberrations (69%). One half of the infants presented with 11q23 rearrangements (n 29). The translocation t(4;11)(q21;q23) was present in 17 patients and predominantly found in infants less than 6 months of age (81%). Twelve additional infants had other chromosomal aberrations with breakpoints in 11q23, 4 of whom had t(11;19), t(9;11), or 11q23 variants each. The 59 patients with adequate cytogenetic analysis were compared as to sex, age, WBC, RF, immunophenotype, prednisone response, and pEFS with the 47 infants for whom cytogenetics were not available. There were no signicant differences both in the distribution of presenting clinical features and in pEFS (pEFS, 38% 7% v 50% 7%; P .13). Univariate analysis for prognostic features associated with poor prognosis showed signicance in descending order for PPR, CNS disease, the t(4;11), pro-B immunophenotype/lack of CD10 expression, age less than 6 months, 11q23 rearrangement, and WBC 100 103/L. Neither coexpression of myeloid markers (Table 1) nor treatment protocol had a signicant inuence on prognosis. We noted no signicant outcome difference for infants with respect to specic 11q23 rearrangements. Of the infants with the t(4;11)/MLL-AF4, 5 of 17 survived (3 in rst CR; pEFS, 18% 9%). All survivors were PGR. Of the infants with 11q23 rearrangements other than the t(4;11)/MLL-AF4, 6 of 12 survived (5 in rst CR; pEFS, 31%
14%; P .17), of whom 5 were PGR. In respect to protocol treatment as a risk factor, we noted a tendency of steady improvement in pEFS for infants from trials ALL-BFM 83 to 90 (pEFS, 23% 12% [n 13] v 37% 8% [n 34] v 51% 7% [n 59]; P .27). A similar trend could be shown for PGR (pEFS, 27% 13% v 53% 11% v 60% 7%; P .16), but the outcome for PPR remained constantly poor (pEFS, 0% v 14% 9% v 18% 12%; P .99). However, none of the differences was statistically signicant, neither in trend nor when comparing each trial separately. In the most recent trial ALL-BFM 90, investigation of MLL fusion transcripts was performed on 24 of the 59 (41%) patients treated in this trial. MLL rearrangement for MLL/AF4, MLL/ AF9, or MLL/ENL was found in 12 infants, with 6 being PGR and 6 PPR. Of the 6 infants with PGR and MLL rearrangement, 4 survived (3 in rst CR and 1 in second CR). In contrast, of the 6 infants with PPR and MLL rearrangement, 2 survived (1 in rst CR and 1 in second CR). Twelve infants presented with germline MLL conguration, all of whom had a PGR. In this group, 8 survived (6 in rst CR and 2 in second CR). The overall outcome at 6 years was worse for infants as compared with older children with ALL (pEFS, 43% 5% v 70% 2%; P .0001). Infants with a PPR had a dismal prognosis compared with infants with a PGR (pEFS, 15% 7% v 53% 6%; P .0001; Fig 1); the overall survival estimate (22% 8% v 65% 6%; P .0001; see Table 3) differed slightly from pEFS only. Table 2 shows the inuence of prednisone response on other presenting features that had been assigned to a poor prognosis within the infant cohort by univariate analysis. Only a higher WBC (median, 250 103/L for PPR v 96 103/L for PGR; P .009) was signicantly correlated with PPR. Infants who were less than 6 months of age, lacked CD10 expression, and/or had an 11q23 rearrangement, but demonstrated a PGR, had a favorable outcome (pEFS, 44%, 49%, and 41%, respectively), whereas almost all comparable PPR died (Fig 2A through C).
Fig 1. pEFS for infants with ALL according to prednisone response.
From www.bloodjournal.org by on March 10, 2011. For personal use only.
1212
RDELMANN ET AL DO
Table 2. Frequency (%) of Presenting Features and Outcome in Infants With ALL According to Prednisone Response (n 105)
PGR (n 78) Feature % pEFS SE (%) PPR (n 27) % pEFS SE (%)
P Value
Sex Female Male Age (mo) 6 6 12 WBC (103/L) 100 100 CNS disease Present Absent Immunophenotype* CD10 Negative Positive Myeloid marker Present Absent Cytogenetics Normal (n) 11q23 rearranged (n) t(4;11) (n) Other aberrations (n)
53 47 51 49 51 49 22 78
54 13 48 52 9 52 44 8 64 8 54 9 52 8 52 48 22 78
23 12 .008 7 7 .0003 0 0 .0001 31 13 .01 33 19 .24 10 6 .0002 0 0 .17 22 10 .0002
including cranial irradiation were related to the risk of isolated CNS relapse. In stepwise Cox regression analysis, PPR emerged as the most signicant adverse prognostic factor, followed by age less than 6 months and CNS disease. Infants with PPR had a 3.3-fold increased risk for relapse compared with other infants (95% condence interval, 1.9- to 5.8-fold; P .0001; Table 4). The
28 11 30 60 7 70
57 43 28 72
49 8 59 9
63 37
0 0 .0001 40 15 .14 25 15 .16 11 7 .0001 .02 .03 .06 .22
45 12 30 57 7 70
42 (16) 60 13 10 (2) 00 45 (17) 41 12 55 (11) 9 9 (9) 33 16 (7) 00 13 (5) 100 0 35 (7) 40 22
*Percentage of evaluated infants (n 104). Percentage of evaluated infants (n 58; PGR, n 38; PPR, n 20). Patients included in 11q23 rearranged.
For infants with the t(4;11), the pEFS results suggested a better outcome for PGR also, but were not signicant (pEFS, 33% v 0%; P .06). The predictive value of the prednisone response was statistically not signicant for infants with CNS disease (Table 2), but the overall result for these children was poor in general. Table 3 summarizes the outcome including causes of death and relapse pattern according to prednisone response. Both groups achieved a similar remission induction rate (93% v 96%). Regardless of prednisone response, the leading cause of failure was BM recurrence. For PPR, we noted isolated BM (74%) or CNS relapses (26%) only, whereas the relapse pattern in PGR was distributed to different sites and combinations. PPR was associated with early treatment failure. Almost two thirds (15 of 23) of all events took place during the rst 6 months after initial diagnosis: 2 infants [t(4;11) present] did not achieve remission, 2 infants died in CR from septicemia and sudden death, and 11 of 18 relapses occurred within 6 months while being on intensive treatment (BM, 7; CNS, 4). In contrast, in the PGR group, one third (11 of 31) of all events took place within 6 months. Three infants, 2 of whom had a translocation t(4;11), did not achieve remission, and 8 additional patients relapsed while on intensive treatment. In this study, 9 infants developed an isolated CNS relapse. We noted a suggestive, but not signicant association of isolated CNS relapse with PPR (5 of 9 infants) and CD10 expression (7 of 9 infants). Neither CNS disease at diagnosis of ALL, age less than 6 months, WBC 100 103/L, nor treatment protocol
Fig 2. (A through C) pEFS for infants with ALL (A) less than 6 months of age, (B) lack of CD10 expression, or (C) presenting with 11q23 rearrangements according to prednisone response.
From www.bloodjournal.org by on March 10, 2011. For personal use only.
INFANT ACUTE LYMPHOBLASTIC LEUKEMIA, PROGNOSIS
1213
Table 3. Outcome for Infants With ALL According to Prednisone Response
All Infants (105) No Infants n (%) PGR (78) n (%) PPR (27) n (%)
CR achieved 1st CCR pEFS SE (%) 6 yr-survival SE (%) Events Induction failure Death in CR Relapse Site of relapse BM CNS Testes BM/CNS BM/testes Second malignancy
100 (95) 47 (45) 43 5 48 6 58 (55) 5 (5) 4 (4) 49 (47) 26 9 3 10 1 1
75 (96) 43 (55) 53 6 65 6 35 (45) 3 (4) 1* (1) 31 (40) 13 4 3 10 1 1
25 (93) 4 (15) 15 7 22 8 23 (85) 2 (7) 3 (11) 18 (67) 13 5
*Septicemia. Treatment failure within the first 6 months (n 2): septicemia, unknown cause (despite autopsy). Congestive heart failure after 1.2 years in CR. Large-cell anaplastic lymphoma 4.5 years after diagnosis of ALL.
presence of 11q23 rearrangements including the t(4;11) did not have a signicant effect on prognosis in the multivariate model, but cytogenetic data were available in one half of the patients only (Table 4). Cox regression analysis for adverse features with data from infants for whom all data were available (n 58) showed the same risk ratios, but, whereas PPR retained its statistical power (P .002), age (P .3) and CNS disease (P .1) lost their statistical signicance. Inclusion of protocol treatment as a risk factor showed no signicance for treatment in the multivariate model.
DISCUSSION
In this large series of infants (n 106) treated with effective risk-based ALL therapy, the prednisone response was the strongest prognostic parameter for outcome. A PGR identied three fourths of infants who achieved an EFS at 6 years of 53% with conventional therapy, whereas infants with PPR had an almost fatal outcome despite therapy intensication (pEFS, 15%; P .0001). Of the other potential adverse prognostic factors studied, including WBC 100 103/L, lack of CD10 expression, cytogenetic 11q23 rearrangements, the specic translocation t(4;11), and coexpression of myeloid markers,
Table 4. Multivariate Analysis for Adverse Prognostic Features in Infants With ALL
Feature* (n 105) Worse Category Relative Risk (95% CI)
P Value
Prednisone response Age CNS disease 11q23 rearrangements
Poor 6 mo Present Present
3.3 (1.9-5.8) 1.9 (1.0-3.3) 1.8 (1.0-3.2) 1.4 (0.6-2.9)
.0001 .03 .05 .41
*Features achieving a multivariate significance level of P .1 at the last step of regression analysis. Multivariate analysis with data from patients for whom all data were available (evaluated n 58).
only age less than 6 months and CNS disease achieved marginal signicance levels in the multivariate model. It should be noted that our patients were not treated uniformly. However, pEFS did not differ signicantly for infants in trials ALL-BFM 83 versus 86 versus 90, neither for the overall cohort nor for PGR or PPR. Regarding frequency and distribution of reported adverse prognostic features in infant ALL, we demonstrated similar results as other investigators in respect to age less than 6 months,4,10 WBC 100 103/L,4,36 CNS disease,6,10,36 pro-B immunophenotype with lack of CD10 expression,6,10,37 lack of hyperdiploidy,7,38 and cytogenetic 11q23 rearrangements,4,5,7,10,13,14,20,21,39 including the t(4;11),4,7,10,13,39 the t(9; 11),7,13,15,21 and the t(11;19).7,20,21 Age less than 6 months retained signicance as a poor prognostic factor in the multivariate model, but a PPR seemed to have a major impact in this age group, as indicated by the fatal outcome of PPR compared with PGR (pEFS, 0% v 44%; P .0001; Table 2 and Fig 2A). It is noteworthy that age seemed to inuence the prognostic power of a t(4;11). During trials ALL-BFM 83 through 90, infants with a t(4;11) (n 17) fared worse as compared with children (n 17) who presented with the same translocation but were older than 1 year of age (pEFS, 18% 9% v 47% 12%; P .06; Fig 3). Similar results from 32 children with ALL (pEFS, 17% 9% v 63% 19%; P .04) were reported by Pui et al.40 These ndings are interesting, because at the molecular level, children with a t(4;11) who were 1 to 9 years of age at diagnosis have been shown to display similar defects as infant cases.41,42 In contrast to other reports,9,10 we found a signicant difference in the outcome of infants with or without CNS disease at diagnosis. However, an obvious explanation for this observation is missing. We noted neither an inuence of the different protocols, in particular with regard to the dosage of MTX or CRT, nor a signicant correlation of CNS disease with age less than 6 months, WBC 100 103/L, lack of CD10 expression, 11q23 rearrangement, or PPR. We conrmed the signicant better outcome for infants with CD10 compared with CD10 ALL.4,6,7,9,15,37 In contrast to other investigators, who demonstrated a signicantly better pEFS in myeloid antigen-negative as compared with myeloid antigen-positive cases,37 coexpression of myeloid antigens had no inuence for prognosis of infants in these ALL-BFM trials. Cytogenetic abnormalities involving chromosome band 11q23 have been correlated with a dismal prognosis in infant ALL,5 particularly the t(4;11).5-7,14-16,19 In the present study, infants with 11q23 rearrangements (pEFS, 28% 8%) and/or the specic translocation t(4;11) (pEFS, 18% 9%) fared poorly as well. However, infants with 11q23 rearrangements, including those with the t(4;11), but a PGR had a relatively favorable outcome as indicated by an pEFS of 41% 12%, whereas almost all comparable PPR died (P .03). Whereas 1 study suggested that infants with 11q23 partners other than the AF-4 gene may have a better outcome (P .09),7 we found no signicant difference (pEFS, 31 14 v 18 9; P .17), which is in accordance with most other reports.15,17,43-45 Most recently, rearrangement of the MLL gene at chromosome band 11q23 has been associated with a dismal prognosis (pEFS, 5.3% to 28%) in infant ALL. The reported frequency of MLL rearrangement differed markedly between 50% and
From www.bloodjournal.org by on March 10, 2011. For personal use only.
1214
RDELMANN ET AL DO
Fig 3. pEFS for children with ALL presenting with the t(4;11) according to age.
81%,13-16,20,21 but has been 72% to 81% in the larger series.14,15,21 The present study lacked sufficient data regarding MLL status. Because of selection bias (screening for the specic fusion transcripts MLL/AF4, MLL/AF9, and MLL/ENL only), small sample size (n 24), and the use of RT-PCR only, we were unable to draw rm conclusions regarding prognosis of MLL rearrangement and its association to prednisone response. However, we noted a correlation of germline MLL with PGR, because all 12 infants with germline MLL were PGR. Eight of them survived, of whom 6 were in rst remission (pEFS, 58% 14%); 2 patients were in second CR after allogenic BMT, which is in accordance with reported results.14,15,20,21 Of the 12 infants with MLL rearrangement, 6 were long-term survivors (4 in rst CR [3 PGR/1 PPR]; 2 remained in second CR [PPR/PGR]), which was comparable to the reported experiences.9,14,21 Therefore, half of the infants with a PGR who were evaluated for MLL rearrangements remained in rst remission, irrespective of their MLL status (pEFS, 56% 12%). Various reports suggested that infants with MLL rearrangement may not represent a homogenous group.46,47 It remains to be evaluated whether the MLL gene rearrangement itself,13,41 the partner genes,21 or the fusion transcripts48 inuence prognosis in infant ALL. In all studies evaluating prognostic factors in infant ALL, patient numbers were relatively small and, in particular, 11q23/ t(4;11)/MLL, CD10-/pro-B, and age less than 6 months were highly interrelated. Therefore, the identication of independent prognostic factors by multivariate analysis was impeded.14,15,17,20,21,49 Only 2 reports could demonstrate a signicant prognostic value of MLL gene rearrangement13 and/or cytogenetic 11q23 rearrangements5 by multivariate analysis. PPR did not correlate with other clinical or blast cell features evaluated except for high WBC. The association of PPR and high WBC seemed to be related to the denition of PPR itself. Because PPR is dened by an absolute blast cell count per microliter on day 8, the probability of being a poor responder is
theoretically higher in patients with a high WBC at diagnosis. However, multivariate analysis showed that a WBC of 100 103/L was not associated with prognosis and barely reached signicance in univariate analysis. This nding might be in accordance with in vitro results from Ito et al,50 who found no signicant correlation between the prednisolone concentration producing 50% cytotoxicity (LC50) and patient age, sex, WBC, presence of chromosomal translocations, ploidy, immunophenotype, and percentage of leukemic cells in S phase in BM samples of 28 children with B-lineage ALL. Because antileukemic treatment itself is an important prognostic factor,51 the initial response to that applied therapy should be an important prognostic factor as well. Various reports have identied initial cytoreduction in blood8,22-25,27,52,53 or BM36,54-58 as a powerful prognostic factor in childhood ALL, despite different treatment regimens or different time points of evaluation during induction. However, only 2 reports have evaluated infants in more detail. Miller et al56 found, in contrast to older children with ALL, no signicance for percentage of lymphoblasts on day 14 BMs of infants, but neither provided detailed data nor included this nding in their discussion. Differences between their study and ours may reect statistical variation resulting from small sample size, differences in treatment and outcome, or other factors not yet identied. In contrast, a retrospective study by the Childrens Cancer Study Group on the prognostic inuence of age in childhood ALL stated that day-14 BM was the most signicant predictor of disease-free survival for the infant group.36 Less infants had M1/M2 BM on day 14 as compared with older children with ALL (88% v 96%). However, because the frequency of M3 BMs was comparable (3% v 1%), it was not obvious from these data whether infants died from nonresponse or any other complications during early induction. The outcome of infants with PPR and children older than 1 year of age with PPR treated during trials ALL-BFM 83 through 90 differed signicantly (pEFS, 15% v 41%; P
From www.bloodjournal.org by on March 10, 2011. For personal use only.
INFANT ACUTE LYMPHOBLASTIC LEUKEMIA, PROGNOSIS
1215
.0003). Blast cells from infants presenting with PPR, 11q23 rearrangement, lack of CD10 expression, or other factors not yet identied may display different cellular pharmacodynamics that determine the sensitivity to antileukemic drugs. Kumagai et al59 showed that leukemic cells from infants with 11q23 abnormalities grew better on stromal cell layers in vitro, which was associated with a poor prognosis. Kersey et al60 recently demonstrated that MLL-AF4 leukemias were highly resistant to cell death that results from serum deprivation and had slower rates of proliferation and decreased cells in S phase compared with nonMLL-AF4 leukemias. Blast cells from infants with MLL rearrangements were shown to have a higher cell recovery rate when inoculated in SCID mice as compared with blast cells from other children with ALL,61 which correlated with a poor prognosis. In vitro studies showed that blasts from infants and blasts from children lacking CD10 expression were signicantly more resistant to prednisolone, daunorubicin, and Lasparaginase than blast cells from other ALL children.62-64 Particularly, blast cells with 11q23 rearrangements are thought to arise in very primitive fetal hematopoietic precursors65 and may have a higher potential for different blast cell populations,66,67 clonal evolution,37,68 or lineage switching.67 In addition, MLL gene rearrangement is frequently observed in acute myeloblastic leukemia also.13,15 Thus, the prednisone response may represent 1 subclone of the blast cell population only and other subclones theoretically could be resistant or less responsive to standard ALL therapy. A prospective international study currently in progress should further clarify the prognostic value of the prednisone reponse and blast cell markers such as 11q23 rearrangement, the specic translocations involving chromosome 11, and MLL rearrangement.
ACKNOWLEDGMENT The authors thank U. Meyer and J. Regelsberger for data management, M. Zimmermann for statistical analysis, E. Odenwald for the expert cytology, the staff of the reference laboratories for excellent cooperation, and the nurses and physicians taking care of the treated infants. REFERENCES 1. Pui CH, Evans WE: Acute lymphoblastic leukemia. N Engl J Med 339:605, 1998 2. Crist W, Pullen J, Boyett J, Falletta J, van Eys J, Borowitz M, Jackson J, Dowell B, Frankel L, Quddus F: Clinical and biologic features predict a poor prognosis in acute lymphoid leukemias in infants: A Pediatric Oncology Group Study. Blood 67:135, 1986 3. Reaman GH, Steinherz PG, Gaynon PS, Bleyer WA, Finklestein JZ, Evans R, Miller DR, Sather HN, Hammond GD: Improved survival of infants less than 1 year of age with acute lymphoblastic leukemia treated with intensive multiagent chemotherapy. Cancer Treat Rep 71:1033, 1987 4. Chessells JM, Eden OB, Bailey CC, Lilleyman JS, Richards SM: Acute lymphoblastic leukaemia in infancy: Experience in MRC UKALL trials. Report from the Medical Research Council Working Party on Childhood Leukaemia. Leukemia 8:1275, 1994 5. Pui CH, Behm FG, Downing JR, Hancock ML, Shurtleff SA, Ribeiro RC, Head DR, Mahmoud HH, Sandlund JT, Furman WL: 11q23/MLL rearrangement confers a poor prognosis in infants with acute lymphoblastic leukemia. J Clin Oncol 12:909, 1994 6. Ferster A, Bertrand Y, Benoit Y, Boilletot A, Behar C, Margueritte
G, Thyss A, Robert A, Mazingue F, Souillet G: Improved survival for acute lymphoblastic leukaemia in infancy: the experience of EORTCChildhood Leukaemia Cooperative Group. Br J Haematol 86:284, 1994 7. Heerema NA, Arthur DC, Sather H, Albo V, Feusner J, Lange BJ, Steinherz PG, Zeltzer P, Hammond D, Reaman GH: Cytogenetic features of infants less than 12 months of age at diagnosis of acute lymphoblastic leukemia: impact of the 11q23 breakpoint on outcome: A report of the Childrens Cancer Group. Blood 83:2274, 1994 8. Reiter A, Schrappe M, Ludwig WD, Hiddemann W, Sauter S, Henze G, Zimmermann M, Lampert F, Havers W, Niethammer D, Riehm H: Chemotherapy in 998 unselected childhood acute lymphoblastic leukemia patients. Results and conclusions of the multicenter trial ALL-BFM 86. Blood 84:3122, 1994 9. Silverman LB, Mclean TW, Gelber RD, Donnelly MJ, Gilliland DG, Tarbell NJ, Sallan SE: Intensied therapy for infants with acute lymphoblastic leukemia. Cancer 80:2285, 1997 10. Lauer SJ, Camitta BM, Leventhal BG, Mahoney D, Shuster JJ, Kiefer G, Pullen DJ, Steuber CP, Carroll AJ, Kamen B: Intensive alternating drug pairs after remission induction fot treatment of infants with acute lymphoblastic leukemia: A Pediatric Oncology Group study. J Pediatr Hematol Oncol 20:229, 1998 11. Mulhern RK, Kovnar E, Langston J, Carter M, Fairclough D, Leigh L, Kun LE: Long-term survivors of leukemia treated in infancy: Factors associated with neuropsychologic status. J Clin Oncol 10:1095, 1992 12. Kaleita TA, MacLean WE, Reaman GH: Neurodevelopmental outcome of childen diagnosed with ALL during infancy: A preliminary report from the Childrens Cancer Group. Med Pediatr Oncol 5:385, 1992 13. Cimino G, Rapanotti MC, Rivolta A, Lo Coco F, DArcangelo E, Rondelli R, Basso G, Barisone E, Rosanda C, Santostasi T: Prognostic relevance of ALL-1 gene rearrangement in infant acute leukemias. Leukemia 9:391, 1995 14. Hilden JM, Frestedt JL, Moore RO, Heerema NA, Arthur DC, Reaman GH, Kersey JH: Molecular analysis of infant acute lymphoblastic leukemia: MLL gene rearrangement and reverse transcriptasepolymerase chain reaction for t(4;11)(q21;q23). Blood 86:3876, 1995 15. Taki T, Ida K, Bessho F, Hanada R, Kikuchi A, Yamamoto K, Sako M, Tsuchida M, Seto M, Ueda R, Hayashi Y: Frequency and clinical signicance of the MLL gene rearrangements in infant acute leukemia. Leukemia 10:1303, 1996 16. Pui CH, Ribeiro RC, Campana D, Raimondi SC, Hancock ML, Behm FG, Sandlund JT, Rivera GK, Evans WE, Crist WM, Krance R: Prognostic factors in the acute lymphoid and myeloid leukemias of infants. Leukemia 10:952, 1996 17. Behm FG, Raimondi SC, Frestedt JL, Liu Q, Crist WM, Downing JR, Rivera GK, Kersey JH, Pui CH: Rearrangement of the MLL gene confers a poor prognosis in childhood acute lymphoblastic leukemia, regardless of presenting age. Blood 87:2870, 1996 18. Dinndorf PA, Reaman GH: Acute lymphoblastic leukemia in infants: Evidence of B-cell orign of disease by use of monoclonal antibody phenotyping. Blood 68:9756, 1986 19. Pui CH, Frankel LS, Carroll AJ, Raimondi SC, Shuster JJ, Head DR, Crist WM, Land VJ, Pullen DJ, Steuber CP: Clinical characteristics and treatment outcome of childhood acute lymphoblastic leukemia with the t(4;11)(q21;q23): A collaborative study of 40 cases. Blood 77:440, 1991 20. Chen CS, Sorensen PH, Domer PH, Reaman GH, Korsmeyer SJ, Heerema NA, Hammond GD, Kersey JH: Molecular rearrangements on chromosome 11q23 predominate in infant acute lymphoblastic leukemia and are associated with specic biologic variables and poor outcome. Blood 81:2386, 1993 21. Rubnitz JE, Link MP, Shuster JJ, Carroll AJ, Hakami N, Frankel LS, Pullen DJ, Cleary ML: Frequency and prognostic signicance of
From www.bloodjournal.org by on March 10, 2011. For personal use only.
1216
RDELMANN ET AL DO
HRX rearrangements in infant acute lymphoblastic leukemia: A Pediatric Oncology Group study. Blood 84:570, 1994 22. Riehm H, Reiter A, Schrappe M: Corticosteroid-dependent reduction of leukocyte count in blood as a prognostic factor in acute lymphoblastic leukemia in childhood (therapy study ALL-BFM 83). Klin Padiatr 199:151, 1987 23. Schrappe M, Reiter A, Sauter S, Ludwig WD, Wormann B, Harbott J, Bender-Gotze C, Dorffel W, Dopfer R, Frey E, Riehm H: Concept and interim result of the ALL-BFM 90 therapy study in treatment of acute lymphoblastic leukemia in children and adolescents: the signicance of initial therapy response in blood and bone marrow. Klin Padiatr 206:208, 1994 24. Schrappe M, Reiter, Riehm H: Cytoreduction and prognosis in childhood acute lymphoblastic leukemia. J Clin Oncol 14:2403, 1996 25. Schrappe M, Arico M, Harbott J, Biondi A, Zimmermann M, Conter V, Reiter A, Valsecchi MG, Gadner H, Basso G, Bartram CR, Lampert F, Riehm H, Masera G: Philadelphia chromosome positive (Ph) childhood acute lymphoblastic leukemia: Good initial steroid response allows early prediction of a favorable treatment outcome. Blood 92:2730, 1998 26. Sackmann Muriel F, Felice MS, Zubizarreta P, Chantada G, Barbieri MF, Rossi J: Improved outcome in higher-risk acute lymphoblastic leukemia with a hybrid (Berlin-Frankfurt-Mu nster/St. Judes) therapy. Int J Pediatr Hematol Oncol 3:439, 1996 27. Arico M, Basso G, Mandelli F, Rizzari C, Colella R, Barisone E, Zanesco L, Rondelli R, Pession A, Masera G: Good steroid response in vivo predicts a favorable outcome in children with T-cell acute lymphoblastic leukemia. Cancer 75:1684, 1995 28. Ludwig WD, Rieder H, Bartram CR, Heinze B, Schwartz S, Gassmann W, Lo ffler H, Hossfeld D, Heil Gerhard, Handt S, Heyll A, , Fonatsch C, Diedrich H, Fischer K, Weiss A, Vo lkers B, Aydemir U Go kbuget N, Thiel E, Hoelzer D: Immunophenotyping and genotypic features, clinical characteristics, and treatment outcome of adult pro-B acute lymphoblastic leukemia: Results of the German multicenter trial GMALL 03/87 and 04/89. Blood 92:1898, 1998 29. Harbott J, Ritterbach J, Ludwig WD: Clinical signicance of cytogenetic studies in childhood acute leukemia: Experience of the BFM trials. Rec Res Cancer Res 131:123, 1993 30. Hiddemann W, Wo rmann B, Ritter J: Frequency and clinical signicance of DNA aneuploidy in acute leukemia. Ann NY Acad Sci 468:227, 1986 31. Janssen JWG, Ludwig WD, Borkhardt A, Spadinger U, Rieder H, Fonatsch C, Hossfeld DK, Harbott J, Schulz A, Repp R, Sykora KW, Hoelzer D, Bartram CR: Pre-pre B acute lymphoblastic leukemia: High frequency of alternatively ALL1-AF4 transcripts and absence of minimal residual disease during complete remission. Blood 84:3835, 1994 32. Langermann HJ, Henze G, Wulf M: Abscha tzung der Tumorzellmasse bei der akuten lymphoblastischen Leuka mie im Kindesalter: Prognostische Bedeutung und praktische Anwendung. Klin Padiatr 194:209, 1982 33. Kaplan EL, Meier P: Non-parametric estimation from incomplete observation. J Am Stat Assoc 52:457, 1958 34. Greenwood M: The natural duration of cancer, in Reports on Public Health and Medical Subjects, 33. London, UK, Her Majestys Stationary Office, 1926, p 1 35. Cox DR: Regression modells and life tables. J R Stat Soc 34:187, 1972 36. Sather HN: Age at diagnosis in childhood acute lymphoblastic leukemia. Med Ped Oncol 14:166, 1986 37. Basso G, Putti MC, Cantu Rajnoldi A, Saitta M, Santostasi T, Santoro N, Lippi A, Comelli A, Felici L, Favre C: The immunophenotype in infant acute lymphoblastic leukaemia: correlation with clinical outcome. An Italian multicentre study (AIEOP). Br J Haematol 81:184, 1992
38. Pui CH, Crist WM, Look AT: Biology and clinical signicance of cytogenetic abnormalities in childhood acute lymphoblastic leukemia. Blood 76:1449, 1990 39. Biondi A, Rossi V, di Celle PF, Carbone A, Benvestito S, Busca A, Giudici G, Giachino C, Basso G, Foa R: Unique genotypic features of infant acute lymphoblastic leukaemia at presentation and at relapse. Br J Haematol 80:472, 1992 40. Pui CH, Carroll LAJ, Raimondi SC, Shuster JJ, Crist WM, Pullen DJ: Childhood acute lymphoblastic leukemia with the t(4;11)(q21; q23): An update (letter). Blood 83:2384, 1994 41. Downing JR, Head DR, Raimondi SC, Carroll AJ, Curcio Brint AM, Motroni TA, Hulshof MG, Pullen DJ, Domer PH: The der(11)encoded MLL/AF-4 fusion transcript is consistently detected in t(4; 11)(q21;q23)-containing acute lymphoblastic leukemia. Blood 83:330, 1994 42. Biondi A, Rambaldi A, Rossi V, Elia L, Caslini C, Basso G, Battista R, Barbui T, Mandelli F, Masera G: Detection of ALL-1/AF4 fusion transcript by reverse transcription-polymerase chain reaction for diagnosis and monitoring of acute leukemias with the t(4;11) translocation. Blood 82:2943, 1993 43. Gibbons B, Katz FE, Ganly P, Chessells JM: Infant acute lymphoblastic leukemia with t(11,19). Br J Haematol 74:264, 1990 44. Huret JL, Brizart A, Slater R, Charrin C, Bertheas MF, Guilhot F, Ha hlen K, Kroes W, van Leuwen E, Schoot EVD, Beishuizen A, Tanzer J, Tangemeijer A: Cytogenetic heterogenetity in t(11;19) acute leukemia: Clinical, hematological and cytogenetic analyses of 48 patients Updated published cases and 16 new observations. Leukemia 7:152, 1993 45. Moorman AV, Hagemeijer A, Charrin C, Rieder H, Secker Walker LM, on behalf of the European 11q23 Workshop participants: The translocations t(11;19)(q23;p13.1) and t(11;19)(q23;p13.3): A cytogenetic and clinical prole of 53 patients. Leukemia 12:805, 1998 46. Uckun FM, Herman-Hatten K, Crotty ML, Sensel MG, Sather HN, Tuel-Ahlgren L, Sarquis MB, Bostrom B, Nachman JB, Steinherz PG, Gaynon P, Heerema N: Clinical signicance of MLL-AF4 fusion transcript expression in the absence of a cytogenetically detectable t(4;11)(q21;q23) chromosomal translocation. Blood 92:810, 1998 47. Hunger SP, Cleary ML: What signicance should we attribute to the detection of MLL fusion transcripts? Blood 92:709, 1998 48. Bernard OA, Berger R: Molecular basis of 11q23 rearrangements in hematopoetic malignant proliferations (review). Genes Chromosom Cancer 13:75, 1995 49. Greaves MF: Infant leukaemia biology, aetiology and treatment. Leukemia 10:372, 1996 50. Ito C, Evans WE, McNinch L, Coustan Smith E, Mahmoud H, Pui CH, Campana D: Comparative cytotoxicity of dexamethasone and prednisolone in childhood acute lymphoblastic leukemia. J Clin Oncol 14:2370, 1996 51. Pinkel D: Selecting treatment for children with acute lymphoblastic leukemia. J Clin Oncol 14:4, 1996 52. Rautonen J, Hovi L, Siimes MA: Slow disappearance of peripheral blast cells: An independent risk factor indicating poor prognosis in children with acute lymphoblastic leukemia. Blood 71:989, 1988 53. Gajjar A, Ribeiro R, Hancock ML, Rivera GK, Mahmoud H, Sandlund JT, Crist WM, Pui CH: Persistence of circulating blasts after 1 week of multiagent chemotherapy confers a poor prognosis in childhood acute lymphoblastic leukemia. Blood 86:1292, 1995 54. Jacquillat C, Weil M, Gemon MF, Auclerc G, Loisel JP, Delobel J, Flandrin G, Schaison G, Izrael V, Bussel A, Dresch C, Weisgerber C, Rain D, Tanzer J, Najean Y, Seligmann M, Boiron M, Bernard J: Combination therapy in 130 patients with acute lymphoblastic leukemia (protocol 06 LA 66-Paris). Cancer Res 33:3278, 1973 55. Frei E III, Sallan SE: Acute lymphoblastic leukemia: Treatment. Cancer 42:828, 1978
From www.bloodjournal.org by on March 10, 2011. For personal use only.
INFANT ACUTE LYMPHOBLASTIC LEUKEMIA, PROGNOSIS
1217
56. Miller DR, Coccia PF, Bleyer WA, Lukens JN, Siegel SE, Sather HN, Hammond D: Early response to induction therapy as a predictor of disease free survival and late recurrence of childhood acute lymphoblastic leukemia: A report from the Childrens Cancer Study Group. J Clin Oncol 7:1807, 1989 57. Gaynon PS, Bleyer WA, Steinherz PG, Finklestein JZ, Littman P, Miller DR, Reaman G, Sather H, Hammond D: Day 7 marrow response and outcome for children with acute lymphoblastic leukemia and unfavorable presenting features. Med Pediatr Oncol 18:273, 1990 58. Steinherz PG, Gaynon PS, Breneman JC, Cherlow JM, Grossman NJ, Kersey JH, Johnstone HS, Sather HN, Trigg ME, Chapell R, Hammond D, Bleyer WA: Cytoreduction and prognosis in acute lymphoblastic leukemia-The importance of early marrow response: Report from the Childrens Cancer Group. J Clin Oncol 14:389, 1996 59. Kumagai, Manabe A, Pui CH: Stroma-supported culture of childhood B-lineage acute lymphoblastic leukemia cells predicts treatment outcome. J Clin Invest 97:755, 1996 60. Kersey J, Wang D, Oberto M: Resistance of t(4;11) (MLL-AF4 fusion gene) leukemias to cell death induced by growth factor deprivation; a possible mechanism for extensive extramedullary accumulation of cells and poor prognosis. Blood 92:1987a, 1998 (abstr, suppl 1) 61. Uckun FM, Sather H, Reaman G: Leukemic cell growth in SCID mice as a predictor of relapse in high risk B-lineage acute lymphoblastic leukemia. Blood 85:873, 1995 62. Pieters R, Kaspers GJL, Huismans DR, Loonen AH, Ha hlen K, van der Doos-van den Berg A, van Wering ER, Veerman AJP: Cellular drug resistance proles that might explain the prognostic value of
immunophenotype and age in childhood acute lymphoblastic leukemia. Leukemia 7:392, 1993 63. Kaspers GJL, Pieters R, Van Zantwijk CH, Van Wering ER, Veerman AJP: Clinical and cell biological features related to cellular drug resistance of childhood acute lymphoblastic leukemia cells. Leuk Lymphoma 19:407, 1995 64. Ramakers-van Woerden NL, Pieters R, Zwaan CM, Kaspers GJL, Beverloo HB, Loonen AH, Slater R, Harbott J, Schmiegelow K, Ha hlen K, van Wering ER, Ludwig WD, Haas O, Janka-Schaub G, Creutzig U, Veerman AJP: In vitro drug resistance proles in infant acute leukemia: Implications for treatment? Blood 92:1592a, 1998 (abstr, suppl 1) 65. Gill Super HJ, Rothberg PG, Kobayashi H, Freeman AI, Diaz MO, Rowley JD: Clonal, nonconstitutional rearrangements of the MLL gene in infant twins with acute lymphoblastic leukemia: In utero chromosome rearrangement of 11q23. Blood 83:641, 1994 66. Ridge SA, Cabrera ME, Ford AM, Tapia S, Risueno C, Labra S, Barriga F, Greaves MF: Rapid intraclonal switch of lineage dominance in congenital leukaemia with a MLL gene rearrangement. Leukemia 9:2023, 1995 67. Ludwig WD, Bartram CR, Harbott J, Koller U, Haas OA, Hansen Hagge T, Heil G, Seibt Jung H, Teichmann JV, Ritter J: Phenotypic and genotypic heterogeneity in infant acute leukemia. I. Acute lymphoblastic leukemia. Leukemia 3:431, 1989 68. Campbell M, Cabrera ME, Legues ME, Ridge S, Greaves M: Discordant clinical presentation and outcome in infant twins sharing a common clonal leukaemia. Br J Haematol 93:166, 1996
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Method Statement For Lifting WorksDocumento12 páginasMethod Statement For Lifting WorksRachel Flores85% (26)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Textbook of Dental Anatomy, Physiology and Occlusion, 1E (2014) (PDF) (UnitedVRG)Documento382 páginasTextbook of Dental Anatomy, Physiology and Occlusion, 1E (2014) (PDF) (UnitedVRG)Konstantinos Ster90% (20)
- CHAPTER 8 f4 KSSMDocumento19 páginasCHAPTER 8 f4 KSSMEtty Saad0% (1)
- PMEGP Revised Projects (Mfg. & Service) Vol 1Documento260 páginasPMEGP Revised Projects (Mfg. & Service) Vol 1Santosh BasnetAinda não há avaliações
- PMA 2015 2016 Issue 3 PDFDocumento36 páginasPMA 2015 2016 Issue 3 PDFLyndon Mercado TolentinoAinda não há avaliações
- DIP Lecture1Documento12 páginasDIP Lecture1Manish SandilyaAinda não há avaliações
- Data Obat VMedisDocumento53 páginasData Obat VMedismica faradillaAinda não há avaliações
- 2013 Audi A5 Cabriolet s5 Cabriolet 8Documento16 páginas2013 Audi A5 Cabriolet s5 Cabriolet 8Adrio BianchiAinda não há avaliações
- HSN-Lube 2007 PDFDocumento45 páginasHSN-Lube 2007 PDFCecilio Valderrama100% (3)
- Boli Vertebro MedulareDocumento12 páginasBoli Vertebro MedulareHalit DianaAinda não há avaliações
- LM 337Documento4 páginasLM 337matias robertAinda não há avaliações
- Intellectual Disability: Definition, Classification, Causes and CharacteristicsDocumento12 páginasIntellectual Disability: Definition, Classification, Causes and CharacteristicsRyan RV ViloriaAinda não há avaliações
- 224 Chinese Healing ExercisesDocumento4 páginas224 Chinese Healing ExercisesKiné Therapeut-manuelle Masseur GabiAinda não há avaliações
- Science 7 - Q2 - M7Documento16 páginasScience 7 - Q2 - M7RAMOS ERLYN P.Ainda não há avaliações
- Aquamine 50.01Documento17 páginasAquamine 50.01Armando RelajoAinda não há avaliações
- A656 GR 80 Brochure 06-26-08Documento2 páginasA656 GR 80 Brochure 06-26-08OsmanAinda não há avaliações
- Report Text: General ClassificationDocumento7 páginasReport Text: General Classificationrisky armala syahraniAinda não há avaliações
- Industrial Visit ReportDocumento8 páginasIndustrial Visit ReportAnuragBoraAinda não há avaliações
- Ethnomedicinal Plants For Indigestion in Uthiramerur Taluk Kancheepuram District Tamilnadu IndiaDocumento8 páginasEthnomedicinal Plants For Indigestion in Uthiramerur Taluk Kancheepuram District Tamilnadu IndiaGladys DjeugaAinda não há avaliações
- Biology Project Cronary Heart Diseas (CHD)Documento7 páginasBiology Project Cronary Heart Diseas (CHD)احمد المغربي50% (2)
- Educational Facility Planning: Bsarch V-2 Arch. Rey GabitanDocumento20 páginasEducational Facility Planning: Bsarch V-2 Arch. Rey Gabitanidealistic03Ainda não há avaliações
- Pre-Operative Check Up of Farm Tools, ImplementsDocumento19 páginasPre-Operative Check Up of Farm Tools, ImplementsLaurence Fabiala50% (2)
- Course Weekly Schedule Health Science TheoryDocumento6 páginasCourse Weekly Schedule Health Science Theoryapi-466810096Ainda não há avaliações
- Proposal Semister ProjectDocumento7 páginasProposal Semister ProjectMuket AgmasAinda não há avaliações
- Ethics, Privacy, and Security: Lesson 14Documento16 páginasEthics, Privacy, and Security: Lesson 14Jennifer Ledesma-Pido100% (1)
- 2015 4-H Show & Sale CatalogDocumento53 páginas2015 4-H Show & Sale CatalogFauquier NowAinda não há avaliações
- City of Atlanta - Structural Checklist: All Items Listed Herein Shall Be Complied With If Applicable To The ProjectDocumento16 páginasCity of Atlanta - Structural Checklist: All Items Listed Herein Shall Be Complied With If Applicable To The ProjectSandip SurAinda não há avaliações
- Pescatarian Mediterranean Diet Cookbook 2 - Adele TylerDocumento98 páginasPescatarian Mediterranean Diet Cookbook 2 - Adele Tylerrabino_rojoAinda não há avaliações
- LYON Conditions of Secondment 3500EUR enDocumento4 páginasLYON Conditions of Secondment 3500EUR enabdu1lahAinda não há avaliações