Escolar Documentos
Profissional Documentos
Cultura Documentos
Acute Biologic Crisis
Enviado por
Arianne BugnaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Acute Biologic Crisis
Enviado por
Arianne BugnaDireitos autorais:
Formatos disponíveis
ACUTE BIOLOGIC CRISIS ACUTE BIOLOGIC CRISIS Severe, decisive critical period Life threatening condition CRITICAL CARE
UNIT Unique environment Sophisticated medical nursing Integrated to combat life-threatening condition Technical intervention GOAL IN CRITICAL SETTING 1. Continuous, optimal nursing care 2. Holistic 3. Physiologic problem main concern of goal NURSING PROCESS Same as any other patient setting ASSESSMENT: offers reference to the types of technical devices available to assist in data collection NURSING INTERVENTION: o IMMEDIATE GOAL: Ensure patient survival o PRIORITY: Physiologic problem o HIGHEST PRIORITY: Patent airway and adequate ventilation & circulation (ABC) CARDIAC FAILURE PUMP FAILURE or HEART FAILURE Inability of the heart to pump sufficient blood to meet the needs to the tissue for oxygen and nutrients Clinical syndrome characterized by signs and symptoms of fluid overload or inadequate tissue perfusion HF indicates myocardial disease diastolic dysfunction (contraction/filling) systolic dysfunction perfusion to the tissue HYPOXIA ETIOLOGIC FACTORS: (in general) o cardiac workload (HPN, cardiomyopathy) o Structural or functional alterations in myocardium (MI, cardiomyopathy, dysrhythmias) o Obstruction with pumping capacity of the heart MOST COMMON CAUSE: A. CAD ischemia & MI ATHEROSCLEROSIS (fatty plaque deposition) o MYOCARDIAL ISCHEMIA Hypoxia and acidosis (accumulation of lactic acid) Compensatory mechanism HF o MYOCARDIAL INFARCTION RESULT TO: Focal necrosis of the heart muscle Death of myocardial cell Loss of contractility Extent of infarction will correlate with the severity of HF Can cause sudden cardiac death B. CARDIOMYOPATHY disease of the myocardium TYPES: DILATED most common o Diffused cellular necrosis & fibrosis contractility of heart o IDIOPATHIC (unknown cause) MAYBE CAUSED BY: MYOCARDITIS inflammatory condition Exposure to cytotoxic agent (doxorubicin & intake of alcohol) RESTRICTED & HYPERTROPHY - distensibility & ventricular filling (diastolic failure) HF r/t cardiomyopathy could become chronic & progressive HF could be resolved by alcohol consumption C. HPN (systemic/pulmonary) afterload, cardiac workload = hypertrophy of the myocardium Ventricular hypertrophy (compensatory mech) forceful contraction of myocardium Enlargement of the ventricular muscle contractility & CO FRANK-STERLING LAW hypoxia If compensatory mech is exhausted = HF D. VALVULAR HEART DISEASE VALVE prevent backflow of the blood Difficulty of blood to move forward pressure within the heart cardiac workload HF PREVENTION: o No smoking o Exercise o Modify eating habits SYSTEMIC CONDITIONS THAT MAY CONTRIBUTE TO THE DEVELOPMENT OF HF: (cardiac output to meet O2 demand worsen myocardial function) o
o metabolic rate (fever, thyrotoxicosis) o Iron overload (HEMOCHROMATOSIS ( deposition of Iron in liver) hereditary/multiple BT) o Hypoxia (CO HF) o Severe anemia (Hct <25%) OTHER FACTORS: o Metabolic/respiratory acidosis o Electrolyte abnormalities o Anti-arrhythmic medications worsen myocardial function inability of the heart to pump blood COMPENSATORY MECHANISM activated when CO (insufficient to meet required pumping of blood) A. SYMPATHETIC NERVOUS SYSTEM STIMULATION immediate response catecholamines (epinephrine, norepinephrine) heart rate & BP Improved cardiac output Improved stroke volume * if prolonged BP = systemic vasoconstriction B. RENIN-ANGIOTENSIN SYSTEM ACTIVATION vasoconstriction Stimulate production of ALDOSTERONE (adrenal cortex) (Na reabsorption at tubules Na retention) and ADH (posterior pituitary gland) (inhibit H2O excretion H2O retention) preload and afterload Angiotensin contributes to VENTRICULAR REMODELLING Adaptive mechanism of myocardium Adapt to fluid & pressure Ventricular chamber would dilate (to accommodate fluid) More effective contraction Ventricular hypertrophy (myocyte would enlarge) contractile element and force of contraction Progressive myocyte contractile dysfunctional overtime VENTRICULAR HYPERTROPHY C. OTHER CHEMICAL RESPONSES Release of pro-inflammatory cytokines (interleukin, TNF) Ventricular remodeling For px with L sided HF Beta Natriuretic peptide (BNP) Neurohormones that would promote vasodilation & diuresis (Na loss @ renal tubules) Produced by ventricles r/t fluid overload (result of HF) Enlargement of myocardium Endothelin (endothelial cells) Potent vasoconstrictor ( peripheral resistance & HPN) Worsening HF D. MYOCARDIAL HYPERTROPHY (with or without chamber dilation) Thickening of muscle mass (enlargement of myocardium) O2 demand HF Forceful contraction CO E. LIMITATION OF COMPENSATORY MECHANISM: O2 cardiac reserve exhausted HF If the heart is normal its okay But if with myocardial dysfunction loss of 300-400% cardiac reserve (not able to meet the demand of heart) PATHOPHYSIOLOGY MYOCARDIAL DYSFUCTION A. CO, systemic BP, and perfusion to kidneys Activation of RAAS aldosterone/ADH Na & H2O retention Arginine vasopressin (vasoconstrictor), endothelin, and cytokines (ventricular remodeling) B. Activation of baroreceptors Vasomotor center stimulated Activation of SNS catecholamines HR, CO, stroke volume venous return ventricular filling & myocardial stretch force contraction CO Vasoconstriction (afterload, BP & HR) BOTH WILL LEAD TO: aldosterone Release of cytokines Ventricular remodeling (adaptation of chambers and myocardium to pressure & fluid volume) Hypertrophy and dilation of ventricles o Enlarged cells o Impaired contractility Failure in compensatory mechanism
HF LEFT-SIDED HEART FAILURE o TYPICAL CAUSE: HPN, CAD, Valvular heart disease (Mitral & Aortic) o RESULT TO: cardiac output & pulmonary congestion tissue perfusion o TYPES: SYSTOLIC HF FORWARD FAILURE SYSTOLIC VENTRICULAR DYSFUNCTION preload ( contractility & afterload) peripheral resistance (not able to contract forcefully during systole in order to eject adequate amount of blood to circulation) Ejection fraction drops to 40% with ventricular dilation SYMPTOMS: inadequate tissue perfusion and pulmonary & systemic congestion DIASTOLIC HF HF with preserved L ventricular function Occurs when the left ventricle cannot relax adequately during diastole Prevent the ventricles from filling with sufficient blood to ensure an adequate CO Ejection fraction is >40 % (ventricles less compliant over time) SYMPTOMS: similar to systolic dysfunction o PATHOPHYSIOLOGY: amount of blood remaining at L ventricle ventricles capacity to receive blood from L atrium L atrium works harder to eject blood (dilation & hypertrophy of L atrium) Blood begins to back up in the pulmonary circulation s/sx of pulmonary congestion & pulmonary edema o MANIFESTATIONS: SOB Dyspnea on exertion Crackles & rales at base of the lungs Orthopnea (provide 3-4 pillows) Dry, hacking cough at night (early sign) Tachycardia S3 gallop (ventricular gallop) attempt of the heart to fill the already distended vessel Pallor urine output Activity intolerance (early sign) Fatigue Weakness Paroxysmal nocturnal dyspnea (PND) Sudden awakening after 2-5 H or sleep with SOB/feeling of breathlessness Pink, frothy sputum pulmonary congestion/edema RIGHT-SIDED HEART FAILURE o MAYBE CAUSED BY: Left ventricular failure (most common cause MI & pulmonary HPN) o DUE TO: Inability of the right ventricle to empty completely volume & pressure at venous system peripheral edema congestion of abdominal organs (ascites) o PATHOPHYSIOLOGY: Right ventricle dilate & hypertrophies (workload) PVR, R ventricle generate more work (O2 demand of the heart) Amount of blood ejected from R ventricle declines Blood begins to back up in the systemic circulation Systemic manifestation o MANIFESTATIONS: CVP Jugular vein distention visible even when in upright position/standing/HBR Peripheral/pitting edema Hepatomegaly with tenderness (+) RUQ pain Abdominal distention Ascites Nausea, anorexia GI tract is congested Swelling of the hands/fingers Nocturia Spleenomegaly, fatigue Hepatospleenomegaly engorgement of the portal venous system Diuresis at night & at rest fluid at peripheral tissue is immobilized at night time) nocturia (+) weight gain fluid retention BIVENTRICULAR FAILURE o No more cardiac reserve o MANIFESTATION: (both R & L failure) PND Dyspnea at rest & activity S3 and S4 gallop COMPLICATIONS: Congestive hepatomegaly & spleenomegaly Engorgement of portal venous system abdominal pressure, ascites, GI problems
Prolonged RHF impaired liver function GI congestion interference with absorption & congestion of nutrients Myocardial distention (dysrhythmias) impaired CO sudden cardiac death Pleural effusion MAJOR COMPLICATION: CARDIOGENIC SHOCK & PULMONARY EDEMA (severe cardiac decompensation) ACUTE HEART FAILURE o PATHOPHYSIOLOGY: Result of chronic HF, pulmonary edema (failure of contractility of the heart) Myocardial scarring distensibility of the L ventricle Inadequate L ventricular contraction workload of the heart & resistance to L ventricular filling hydrostatic pressure in pulmonary capillaries Fluid shift to interstitial spaces alveoli stiffness of lungs Impairment of lung expansion & gas exchange s/sx of perfusion & pulmonary congestion o MANIFESTATIONS: (ACUTE HF PULMONARY EDEMA) restlessness & anxiety (confusion, stupor, coma) - cerebral O2 Onset of breathlessness/dyspnea/SOB acute/severe Sense of suffocation sense of impending doom Cyanotic nailbed Cool, clammy skin gray color Productive cough with pink, frothy sputum Crackles on auscultation Weak, rapid pulse Jugular vein distention (even when upright/standing) Rapid, moist breathing urine output HPN/ BP Presence of PVC/dysrhythmias COLLABORATIVE CARE: o GOAL: excess fluid & improve gas exchange o LABORATORY/DX TEST: (IN GENERAL) ABG respiratory status, O2 stat Initially Co2 (due to rapid breathing) CO2 ELECTROLYTES baseline Na, K, Cl to evaluate F & E status LFT liver function AST, ALT, LDH, bilirubin albumin level & coagulation BNP key indicator of HF CXR pulmonary vascular congestion, alveolar edema, cardiomegaly (enlargement of the heart) ECG changes with ventricular enlargement, dysrhythmias, myocardial ischemia/infarct ECHOCARDIOGRAPHY when stable Evaluation of L ventricular function Confirm the dx of client (identify underlying cause) Determine ejection function (identify severity & type of HF) o MEDICAL MANAGEMENT (ACUTE PHASE): OXYGEN THERAPY FACE MASK 100% (8-10 L/min or 6-10 L/min) NON REBREATHER MASK initially ordered o Provide concentration of O2 & FiO2 >90 % ET & MECHANICAL VENTILATOR WITH PEEP o ET if with pulmonary failure o PEEP venous return fluid movement from pulmonary capillaries to alveoli (improved O 2) PHARMACOLOGY: MORPHINE o Small dosage via IV titration (1-2 mg) o venous return, anxiety, work of breathing o Monitor RR respiratory depression o NALOXONE HCl antidote DIURETICS o FUROSEMIDE (loop diuretics) produce rapid diuretic effect o Promote excretion of Na & H2O by the kidney o 40 mg direct IV for 1-2 mins ( autotoxicity) o If with K BEMETANIDE (Bumex) & METOLAZONE Could cause further dysrhythmias NESERITIDE (Natrecor) BETA TYPE NATRIURETIC PEPTIDE o For acutely decompensated HF o ACTION:
Rapid improvement in symptoms of HF (binding with vascular smooth muscle & endothelial cell dilation of arteries & veins) Suppress neurohormones responsible for fluid retention (diuresis, preload & afterload, stroke volume) DOBUTAMINE (Dobutrex) o For px with BP; and L ventricular dysfunction o & improves cardiac contraction MILRINONE (Primacor) PHOSPHODIESTERASE INHIBITOR o Delays the release of Ca from intracellular reservoir o Prevents uptake of extracellular Ca by the cells o Promotes vasodilation (preload & afterload; cardiac workload) o MAJOR SIDE EFFECTS: (px is asymptomatic) BP, GI dysfunction, dysrhythmias, platelet count ANTICOAGULANT px with a-fib & myocardial infarct (neural) ANTIANGINAL DRUGS o Avoid anti-inflam agent ( systemic vascular resistance, renal perfusion) NURSING INTERVENTION (EMERGENT CARE) o Ensure AIRWAY patency Assess the effectiveness of respiratory effort & airway clearance Encourage to cough out secretions Suction, if necessary o BREATHING Assist with intubation and mechanical ventilator Assess respiratory status Skin color of px bluish coloration Auscultate crackles & adventitious sounds High back rest with legs dangling to promote breathing & venous return Administer O2 by mask/nasal cannula o CIRCULATION V/S & hemodynamic parameters (CVP) - CVP if with RHF IV line for meds KVO only if with pulmonary edema/congestion MEDS: morphine, diuretics, inotropic meds, bronchodilator Indwelling/foley catheter Urine output <30 ml/hr refer Weigh OD Restrict fluid intake Monitor O2 sat & other lab results Rotating tourniquet as advised - fluid in the body Elevated slightly above systolic pressure BP cuff at 3 extremities Remove alternately Stay for 15 mins but not <5 mins Remove one at a time (LUE) clockwise pulmonary pressure, venous return (improve gas exchange) Can remove 1L of circulating blood o PROVIDE EMOTIONAL SUPPORT o OTHER NURSING DX: (FOR ACUTE HF) Ineffective airway clearance Ineffective breathing pattern Impaired gas exchange Fluid volume excess PHARMACOLOGIC THERAPY: (FOR HF) o ACE INHIBITOR CAPTOPRIL (Capoten), MOEXIPRIL (Univasc), ELANAPRIL MALEATE (Vasotec) Slows progression of HF Interrupt the conversion of Angiotensin I to II Blocks the RAS ( cardiac workload, CO, edema & Na retention) PO; or IV slow dosage (via infusion pump) o ANGIOTENSIN II RECEPTOR BLOCKER VALSARTAN (Divan) BP & systemic vascular resistance (improved CO) Blocks the effect of Angiotensin II at Angiotensin II receptor o HYDRALAZINE APRESOLIN systemic vascular resistance of L ventricular afterload o ISOSORBITE DINITRATE (Isordril) Venous dilation (amount of blood flow to heart & preload) o BETA-BLOCKER CARVEDILOL Routine med added to ACE inhibitor, diuretics, & digitalis CI: seizures & uncontrollable asthma SE: dizziness, BP, HR o DIURETICS FUROSEMIDE If with K SPIRONOLACTONE/ALDACTONE THIAZIDE DIURETICS (DIURIL, CHLORTHIAZIDE, METOLAZONE) o CA-CHANNEL BLOCKERS VERAPAMIL (Isoptin) & DILTIAZEM (Cardizem) Diastolic dysfunction & failure CI: systolic dysfunction & failure
DIGITALIS DIGOXIN & CANOXIN force of myocardial contraction S/SX OF DIGITALIS TOXICITY: anorexia, nausea, vomiting, fatigue, depression, body malaise, changes in heart rate & rhythm, ECG changes SA/AV block Hold the drug & refer if HR <60 bpm DIGOXIN IMMUNE FAB (Digibind) antidote RISK: K level GI symptoms: anorexia, vomiting, abdominal pain, distention
OTHER INTERVENTIONS: o CORONARY ARTERY REVASCULARIZATION CORONARY ARTERY BYPASS (CABG) Artery/vein from another part of the body is connected to the blocked coronary artery Allows new route of O2-rich blood around the blockage to the heart muscles CO = preventing HF IMPLANTABLE CARDIOVERTER DEFIBRILLATOR (ICD) PACEMAKER Uses electrical pulses to help control life-threatening arrhythmias CARDIAC RESYNCHRONIZATION THERAPY (CRT) Use of biventricular pacemaker to treat electrical conduction defects Synchronizes the contraction of the R & L ventricles Improves cardiac contractility of the heart o CARDIAC TRANSPLANT for end-stage HF ORTHOTROPIC Problematic heart is replaced with new heart HETEROTROPIC PIGGYBACK HEART Donors heart is implanted @ R chest 2 functioning heart (donors heart & sick heart) Main workload is carried by the donors heart MONITOR: Infection, possible rejection Give immunosuppressive drugs to prevent rejection INDICATED FOR: Pulmonary HPN o CARDIAC REHAB Done when the client is free of symptoms GOAL: To help patient live a life that is full, vital & productive but within the hearts ability to respond to an stress or activity STARTED: Upon admission until discharge OBJECTIVES: Limit the effects and progression of atherosclerosis Return px to work & pre-illness lifestyle Enhance the psychological and vocational status of px Prevent another cardiac event Same cardiac rehab is done if patient has MI EXERCISE under clinical supervision, depending on the ability of the patients heart Progressive & continuous until discharge HEALTH TEACHING: Control HPN (with continued med. supervision) Diet/special diet (Na) o Possible hidden Na (read food label) o List of different foods that are rich in Na, fat, cholesterol Weight reduction program (as necessary) Progressive exercise under medical supervision SEXUAL ACTIVITIES o When to resume 4-6 weeks after initial incidence o If too weak, 4-6 weeks after discharge o Assume position that is fatiguing o When client complaints of dyspnea, chest pain, palpitation (do it in moderation) o If with severe sx stop (other means of sexual intimacy, instead) o NUTRITIONAL THERAPY Na 2-3 g/day (fluid retention & sx of peripheral & pulmonary congestion) OFI to 800 ml 1L/day (dependent on the fluid status of body) 3 bottles per shift fat & cholesterol Liquid diet (initially) - cardiac workload & O2 demand Soft to full diet, thereafter OXYGEN THERAPY Need based on the degree to pulmonary HPN & resulting hypoxia If with COPD not >4L/min of O2 NURSING INTERVETION (HF) o Monitor & record VS Tachycardia at rest (significant) most common in HF (compensatory mech) o Auscultate heart & breath sounds Murmur, S3 & S4 gallop o
o o o
o o
S3 gallop (ventricular gallop) attempt of the heart to fill the already distended ventricle (early sign of HF) S1 & S2 cardiac function is poor crackles, dyspnea, SOB worsening HF MANIFESTATIONS OF CO: Changes in LOC (early signs of cerebral hypoxia restlessness, confusion, agitation, irritability) Cool, clammy skin pulses Pallor & cyanosis Dysrhythmias urine output (failing kidney tissue perfusion) Administer O2 as needed to improve oxygenation Administer meds as ordered to cardiac workload & effectiveness Encourage client to rest HOB 30-45 - improve ventilation Dangle legs - venous return to the heart AVOID: valsalva maneuver/straining isometric exercises (to cardiac workload) catheterization (to avoid straining) Psychological rest & anxiety quiet environment O2 consumption & explain procedure to the patient improve cardiac output Fluid volume excess Assess respiratory status respiratory status worsening L ventricular HF (SOB, orthopnea, PND, DOB, cough) Auscultate lung sounds Q4H Refer if client manifests s/sx of pulmonary edema EMERGENCY! Jugular vein distention even on upright position hallmark s/sx RHF cause is LHF MIO a drop in UO is significant (renal perfusion) Weigh OD - sudden weight gain = fluid retention (1 lb of fluid = 1 lb of body wt) Abdominal girth Qshift fluid retention at abdominal cavity (ascites) Maintain bedrest with HOB at 45 - venous return & improve ventilation Assess for other manifestations of fluid volume excess (jugular vein distention, etc.) Monitor & record hemodynamic parameters CVP 3-8 mmHg (>10 mmHg refer); 10 mmHg is the upper limit Administer diuretics & other meds as ordered Na & H2O excetion Restrict fluids as ordered Ice chips, hard candies (sugar-free, if diabetic) relieve dry mouth & to provide comfort Mouth care OTHER NURSING DX: Activity intolerance Little to no cardiac reserve Organize nursing care (provide rest period between activity) Assist with self-care activity (promote independence) Plan and implement progressive activity plan Passive and active ROM (as appropriate) Prevent complications of immobility massage bony prominence (circulation) Knowledge deficit on Na diet Teach client to read food label (hidden Na) Encourage to eat small amount at frequent intervals
ACUTE MYOCARDIAL INFARCTION HEART ATTACK, UNSTABLE ANGINA, ACUTE CORONARY SYNDROME LIFE THREATENING due to conditions causing ischemia (80-90% O2) reversible Necrosis of cells in an area of cardiac muscle irreversible RISK FACTORS: (CAD) o ATHEROSCLEROSIS PRIMARY RF o SMOKING CO2 damage BV lining deposition of cholesterol @ vessel area Nicotine (stimulant) vasoconstriction Activation of SNS catecholamines HR, BP, cardiac workload & O 2 demand o OBESITY Body wt >30 % of IBW Deposition of fat @ abdominal area (risk for CAD) Waist-hip ratio of >1:1 significant o PHYSICAL INACTIVITY Associated with CAD Benefits of exercise: burns calories, circulation, availability of O2 at muscle O2 demand & cardiac workload myocardial function & electrical stability BP, blood lipid level, insulin, weight, platelet aggregation
MENOPAUSE PREMATURE MENOPAUSE (reproductive problem) ESTROGEN protective effect on heart (LDL, HDL) >35 y.o. with surgically induced menopause 720x risk as compared with normal menopause >35 y.o. with natural menopause - risk during the next 10 years after onset of menopause Estrogen-replacement therapy - risk of CAD but risk of uterine cancer o DM Contribute to the devt of CAD (lipid, BP & obesity) Affecting large & small tissues atherosclerosis Negate the (+) effects of estrogen o HYPERLIPIDEMIA triglyceride & LDL; HDL; and glucose intolerance LDL primary carrier of cholesterol atherosclerosis HDL - cholesterol from arteries by transporting it to the liver for excretion >35 mg/dl - risk for CAD HDL by exercise, wt loss, estrogen replacement therapy o HPN Systolic pressure of >140 mmHg & diastolic pressure of >90 mmHg damage the BV lining o TYPE A PERSONALITY TYPE B moderate ambition, relaxed, easy giving, accommodating, cooperative (risk for CAD) PATHOPHYSIOLOGY: o ATHEROSCLEROTIC PLAQUE PRIMARY RF o ULCERATION & RUPTURE OF THE WALL deposition of cholesterol @ wall friable wall (easily broken) o Activation of platelets o Thrombus formation vasospasm ( O2) o Ischemia of tissue in the region supplied by artery ( O2 demand but with O2) o Coronary blood supply less than demand o Myocardial cell death contractility o STROKE VOLUME CARDIAC OUTPUT BP TISSUE PERFUSION (inability of the heart to contract O 2 demand multisystem organ failure) o HYPOXIA Local vasodilation and acidosis Imbalance of K, Ca, Mg at the cellular level Change in normal conduction and contractile function and pain Release of catecholamines (HR and BP compensatory mech) EXTENT OF ZONE OF INFARCTION DEPENDS ON: o COLLATERAL CIRCULATION o ANAEROBIC METABOLISM - tissue perfusion o WORKLOAD DEMANDS ON THE MYOCARDIUM Often begins in the SUBENDOCARDIUM spread to the epicardium TRANSMURAL (all layers) ZONES: o ISCHEMIA outer portion O2 but tissue is still viable can be resolved if given meds (thrombolytic therapy) o INJURY injured tissue but not necrotic (can be improved) o NECROSIS infarcted area with tissue death (tissue is not viable) SEQUENCE OF EVENTS: o Ischemic tissue viable Center of the infarcted zone (area of non-viable cells) Subendocardium suffers initial damage within 6H o Cell death lysis and release of isoenzymes (CK -MB & LDH1) into the circulation Prolonged ischemia (20-45 mins) irreversible Physical change not obvious until 6H after infarction Intervention needed within 4-6H of onset of sx o Within 4-6H: blue & swollen (early infarct) After 48H: infarcted area turns gray with yellow streaks By 8-10 days: granulation tissue forms at the edges of necrotic tissue Over 2-3 months: necrotic tissue shrunk with thin & firm scar ( ventricular function HF) * (Ischemia vasospasm further impair blood flow ischemic zone necrosis) CLASSIFICATION: o ACCORDING TO THE DAMAGED AREA: ANTERIOR WALL/SEPTAL WALL MI left anterior descending artery POSTERIOR WALL/LATERAL WALL MI circumflex artery INFERIOR WALL MI right coronary artery * if the main artery is involved ischemia of entire L ventricle GRAVE PROGNOSIS o ACCORDING TO THE DAMAGED MUSCLE LAYER: TRANSMURAL all the layers of myocardium SUBENDOCARDIAL inner half of endocardium o ACCORDING TO ECG CHANGES: Q-WAVE INFARCT (WIDENED/ABNORMAL Q WAVE) Hallmark characteristic of MI Classic ECG change of px with MI Indicates necrosis
NON-Q WAVE INFARCT T wave inversion ischemia of myocardium ST elevation injury at myocardium CLINICAL MANIFESTATION: o CARDIOVASCULAR CHEST PAIN main sx Severe, crushing pressure Heavy or squeezing sensation Substernal area (initially) Radiates to the shoulder, neck, arms or jaw (L side) Not relieved by rest & nitroglycerin 15-20 minutes of pain Epigastric pain/heartburn painless MI (common with DM sensory neuropathy) TACHYCARDIA SNS stimulation ALTERATION IN BP BP release of catecholamines (SNS stimulation) BP - contractility/side effect of meds (impending sx of cardiogenic shock) DIMINISHED PERIPHERAL PULSES DYSRHYTHMIAS PAC/PVC common/1st hour post MI PVC primary cause of sudden cardiac death SIGNS OF LEFT CARDIAC FAILURE S3 GALLOP (hallmark man) attempt of the heart to fill the distended ventricles DIAPHORESIS, COOL & CLAMMY SKIN (SNS stimulation) may indicate cardiogenic shock o RESPIRATORY TACHYPNEA, DYSPNEA, SOB PULMONARY EDEMA CRACKLES With crackles pulmonary edema Without crackles pulmonary congestion o NEUROLOGIC (cerebral O2) LOC (stupor, lethargy, coma) ANXIETY, RESTLESSNESS, FEELINGS OF IMPENDING DOOM o GIT NAUSEA & VOMITING irritation of the vagus nerve o GENITOURINARY URINE OUTPUT cardiogenic shock r/t kidney perfusion o LABORATORY/DX CHANGES ECG CHANGES T wave inversion ischemia of myocardium ST elevation injury at myocardium Widened/abnormal Q wave necrosis of myocardium (MI) CARDIAC ENZYMES CK-MB, LDH 1 troponin I MI troponin T ischemia o TEMPERATURE & LEUKOCYTOSIS inflammatory manifestation due to tissue injury/necrosis COLLABORATIVE CCARE o GOAL: Relieve chest pain Maintain cardiovascular stability cardiac workload Prevent complication o Rapid assessment/immediate evaluation essential with MI May be conscious at ER but may be in a sudden coma after a few mins ( tissue perfusion sudden cardiac death) o Definitive tx within 1H of arrival in emergency center (AHA) TIME IS MUSCLE save myocardium for better chance of survival (medical truism) o FACTORS FOR DELAY OF TREATMENT: Advanced age Clients perception of illness Denial Access to medical care Availability of EMS In-hospital delays LABORATORY TEST o CARDIAC ENZYMES: CK-MB within 4H and peaks within 12-24H and declines within 48-72H tissue necrosis = CK-MB MYOGLOBIN Hemiprotein that helps with transport of O2 at cardiac & skeletal muscle
within 1-3H and peaks within 12H after onset of sx If (-) = r/o MI TROPONIN I & T Protein found in myocardium (regulates myocardial contractile process) Reliable & critical markers for cardiac injury Specific for cardiac muscle within few hours up to 3 weeks (acute MI) LDH (most specific to cardiac damage) Rises within 24-72H Peaks in 3-4 days Returns to normal in 10-14 days
CBC WBC inflammatory response to tissue injury o ESR inflammation o ABG O2 sat & acid base balance o COAGULATION PROFILE (PT, PTT) Clotting mechanism precipitation of thrombus formation o LIPID PROFILE cholesterol & triglyceride Baseline is important before starting anticoagulant therapy DIAGNOSTIC TEST: o ECG (may appear on admission) INVERTED T WAVE (ISCHEMIA) Due to altered & delayed myocardial repolarization Appears within 1-3 days ELEVATED ST SEGMENT (INJURY) Myocardial cells depolarize normally but repolarize more rapidly than normal cells ABNORMAL/WIDENED Q WAVE (INFARCTION) There is no depolarization conducted from necrotic tissue Appears within 1-3 days o ECHOCARDIOGRAPHY When the px is stable Ventricular function Assist dx of px especially if ECG would reveal non-dx (no abnormal/widened Q wave) characteristic of MI o CARDIAC RADIONUCLEAR SCAN changes in coronary blood flow and changes in myocardial tissue o HEMODYNAMIC MONITORING (SWAN-GANZ CATHETER) PULMONARY ARTERY CATHETERIZATION (PAC) Determine atrial, ventricular & pulmonary artery pressure Catheter inserted via femoral vein or R internal jugular vein (preferred site nearer to heart) POSSIBLE COMPLICAIONS: ventricular aneurysm, muscle rupture NORMAL VALUES: PULMONARY PRESSURE o SYSTOLIC 15-30 mm H2O o DIASTOLIC 4-12 mm H2O PULMONARY CAPILLARY WEDGE PRESSURE (PCWP) 2-15 mmHg o >20 mmHg pulmonary edema MEDICAL MANAGEMENT (EMERGENT) o Admit in CCU/ICU for 24-48 H o CBR without BP o Bedside commode (after 48-72H) unless unstable o Provide calm, quiet environment to O2 demand & cardiac workload o Provide O2 by nasal cannula at 2-5 L/min If with COPD 4L/min If by facial mask 6-10L/min o Liquid diet in 1st 24H (O2 demand & cardiac workload) o Once stable, Na & cholesterol diet With pulmonary congestion/edema Na restriction Without depends on the Na level If no evidence of HF Na restriction is lifted o Small, frequent feeding o Limit caffeine & very hot (vasodilation)/very cold (vasoconstriction) food - blood flow PHARMACOLOGY: o THROMBOLYTIC THERAPY 1st line of drug 1st 3-6 H confirm dx within 1st 6H to start meds STREPTOKINASE most common TISSUE PLASMINOGEN ACTIVATOR (Altepase) INDICATION: Chest pain >20 mins, unrelieved by nitroglycerin ST segment elevation in at least 2 leads (injury) <6H from onset of pain
NURSING CONSIDERATIONS: Avoid IM injection dissolve clot by activating fibrinolytic ... o Fibrins bleeding Minimize puncture of clients skin o If serial PT/PTT, CBG is needed apply pressure at punctured site Draw blood for laboratory test when starting IV line before thrombolytic therapy Check s/sx of bleeding Check for coagulation profile (bleeding time, coagulation time, PT, PTT) Must be given within 6H on MI onset CONTRAINDICATIONS: Client with bleeding disorder Hx of CVD embolism/bleeding Uncontrolled HPN systolic BP >140 mmHg; diastolic BP >90 mmHg Pregnancy Recent trauma or surgery of head/spine bleeding ANALGESIC MORPHINE SO4 analgesic of choice Administered IV bolus Q15mins until pain is relieved (low dose) preload/afterload & cardiac output pain Monitor for morphine toxicity (assess RR) NALOXONE HCl antidote HYDROMORPHONE (Dilaudid) & MEPERIDINE HCl (Demerol) Alternative analgesic if with bradycardia ANTI-ANXIOLYTIC (Valium) anxiety ( cardiac workload & pain) ACE INHIBITORS Prevent conversion of angiotensin I II (BP) Excretes Na & H2O by the kidney cardiac workload & O2 demand MONITOR: Na, K, creatinine level, BP, output level
ANTIDYSRHYTHMIC Treat & prevent dysrhythmias LIDOCAINE 1st 1-2 days following MI For v-fib 1st H for PVC ATROPINE SO4 Bradycardia & BP 0.5-1 mg (usual dosage) VERAPAMIL (Isoptin) Ca-channel blocker For a-fib & supraventricular tachydysrhythmias o BETA BLOCKER (METOPROLOL, ATENOLOL, PROPANOLOL) HR, cardiac workload, O2 demand o VASODILATOR (ISOSORBIDE DINITRATE, NITROGLYCERIN) afterload & myocardial workload blood flow to save myocardial tissue at risk o CA-CHANNEL BLOCKER (NIFEDIPINE, DILTIAZEM, VERAPAMIL) Prevent re-infection & ischemia in px with non-Q wave infarct o ANTICOAGULANT (HEPARIN) IV bolus initially IV drip via infusion pump, thereafter CLOPIDOGREL most common in the clinical area LOW MOLECULAR WT HEPARIN (Clexane) abdomen (SQ) Daily for 7-14 days Do not massage/aspirate 45 if with longer needled o ANTIPLATELET (ASPIRIN) With ischemia but without injury As maintenance therapy (low dose) o VASOPRESSOR (DOPAMINE/DOBUTAMINE) INOTROPIC AGENT myocardial contraction DOPAMINE improve blood flow especially to vital organs (kidney) UO dose by titration (by 5) after 30 mins until target BP is reached myocardial contractility vasoconstriction improved BP & CO Long term vasoconstriction blood flow REVASCULARIZATION PROCEDURE o PTCA immediate or after thrombolytic therapy Balloon-tipped catheter used to open blocked coronary vessels & resolve ischemia PURPOSE: Improve blood flow within coronary artery (compressing/cracking the atheroma) o INTRA-AORTIC BALLOON PUMP Insertion of balloon-tipped catheter Inflated during diastole (push more oxygenated blood to the coronary artery)
Deflated during systole (pressure of blood in the aorta to cardiac workload) amount of O2 at heart while workload of heart (improved circulation) o VENTRICULAR ASSIST DEVICE Type of artificial heart Design to assist one ventricle to pump oxygenated blood through aorta to body tissues With battery pack Control unit is carried by px (thru backpack) CARDIAC REHABILITATION o Done when the client is free of symptoms o INDICATOR: when the client is able to climb up to 2 flights of stairs o GOAL: To help px live a life that is full, vital & productive but within the hearts ability to respond to an stress or activity OBJECTIVE: Limit the effects and progression of atherosclerosis Return px to work and pre-illness lifestyle Enhance the psychosocial & vocational status of px Prevent another cardiac event TREATMENT FOR ACUTE MI: o Rapid transport to the hospital (immediate tx) o 12-lead ECG read within 10 mins (pain associated with ECG changes) o Obtain specific lab test o Obtain dx test (to confirm fx) ECG only plus lab tests during acute phase px is unstable o BEGIN ROUTINE MEDICAL INTERVENTION: MONA (MORPHINE, OXYGEN, NITROGLYCERIN, ASPIRIN) MORPHINE pain (cardiac workload & O2 demand) SUPPLEMENTAL OXYGEN NITROGLYCERIN will not relieve pain but will improve blood flow (vasodilator) ASPIRIN (162-325 mg) only if with ischemia BETA-BLOCKER ACE INHIBITOR within 24H o EVALUATION FOR INDICATION OF REPERFUSION THERAPY: PTCA THROMBOLYTIC THERAPY o CONTINUE THERAPY AS INDICATED: IV HEPARIN CLOPIDOGREL/TICLOPIDINE GLYCOPROTEIN IIb/IIIa INHIBITOR used during PTCA Prevent platelet aggregation & thrombus formation BEST REST 1st 24H up to 48H (depending on px condition) NURSING INTERVENTION: o PAIN Assess & document V/S HR &BP (clues about unreported pain of client) O2 @ 2-5L/min (O2 supply ischemia & pain) Pain = myocardial perfusion Physical & psychological rest - anxiety (cardiac workload & comfort) Morphine, nitroglycerin, beta-blocker, ca-channel blocker (O2 supply & O2 demand) o ALTERED TISSUE PERFUSION Assess & document V/S report abnormal HR & rhythm; BP & RR Document altered LOC Auscultate heart & breath sounds S3 gallop L side HF S3 & S4 gallop biventricular HF Crackles pulmonary edema If with pain 12-leads ECG Cardiac monitor push button & print lead If with PVC indicate time & attach to chart Continued, unrelieved chest pain further myocardial, ischemic & extension of infarct O2 sat Give O2 ABG results Antidysrhythmic meds Serial CK-MB, LDH 1, troponin I & T (greater damage = cardiac enzymes) Invasive intubation & hemodynamic monitoring prepare emergency equipment Digitalis, Dopamine, Dobutamine medications to improve CO & cardiac contractility Nitroglycerin, Diuretics drugs to myocardial workload o INEFFECTIVE INDIVIDUAL COPING o FEAR Promote psychological rest OTHER NURSING DIAGNOSIS: o RISK FOR CO o RISK FOR INJURY o ALTERED SEXUAL PATTERN o
o o
INEFFECTIVE BREATHING ALTERED ROLE PERFORMANCE
ACUTE RESPIRATORY FAILURE Sudden, life-threatening deterioration of the gas exchange function of the lungs PaO2 <60 mmHg (hypoxemia) PaCO2 >50 mmHg (hypercarbia/hypercapnia) pH (acidosis) <7.30 (acidemia) VENTILATORY FAILURE (HYPOXEMIC RF) o Type of problem in O2 intake & blood delivery ventilator/perfusion mismatch o Inadequate ventilation (O2 delivery) & normal perfusion (blood delivery) o Occurs as a result of too little O2 that reaches the alveoli and CO2 is retained (hypoxemia & hypercapnia) o OFTEN THE RESULT OF: Physical problem of the chest wall Defect in the respiratory control center in the brain Poor function of respiratory muscle o CONDITIONS THAT CAUSED VENTILATORY RF: EXTRAPULMONARY CAUSES: NEUROMUSCULAR GBS, MG, poliomyelitis, spinal cord injury, CNS dysfunction (stroke, ICP, meningitis) Chemical depression r/t opioid analgesics, sedatives, anesthetics Massive obesity Sleep apnea External obstruction/constriction INTRAPULMONARY CAUSES: COPD, pulmonary embolism, pneumothorax, pleural effusion, ARDS OXYGEN FAILURE (HYPERCAPNEIC RF) o Chest pressure is normal o Air moves in & out without difficulty but does not oxygenate the pulmonary blood sufficiently o PROBLEMS INCLUDE: Impaired diffusion of O2 at the alveolar level R to L shunting of the blood in the pulmonary vessels venous blood is shunted into the arterial system without being oxygenated Ventilation/perfusion mismatch Breathing of air with low PaO 2 Abnormal hemoglobin that fails to bind with O2 o COMMON CAUSES: Low atmospheric O2 concentration (high altitude) Smoke inhalation & carbon monoxide poisoning PNA CHF with pulmonary edema Pulmonary embolism ARDS Abnormal hemoglobin Hypovolemic shock Hypoventilation PATHOPHYSIOLOGY: o HYPOXEMIC RF CAUSES: VENTILATORY/PERFUSION MISMATCH, IMPAIRED GAS EXCHANGE, HYPOVENTILATION MANIFESTATIONS: DYSPNEA TACHYPNEA good indicator of severely ill px o PROGRESSES TO: bradycardia & BP CYANOSIS RESTLESSNESS, APPREHENSION CONFUSION, IMPAIRED JUDGMENT TACHYCARDIA, DYSRHYTHMIAS HPN METABOLIC ACIDOSIS - pH, HCO3 DOB HEADACHE o HYPERCAPNEIC RF CAUSE: HYPOVENTILATION MANIFESTATIONS: DYSPNEA HEADACHE PAPILLEDEMA redness & swelling of optic disk TACHYPNEA PCO2 (progress to bradypnea) HPN DROWSINESS SYSTEMIC VASODILATION HF
RESPIRATORY ACIDOSIS - pH, pCO2 (vasodilating effect depression of CNS) TACHYCARDIA PROGNOSIS depends on underlying disease process COLLABORATIVE CARE: o TREATMENT IS DIRECTED TOWARDS: Correcting the underlying cause/disease process Supporting ventilation of px Correcting hypoxemia/hypercapnia LABORATORY/DX TEST: o ABG basis of dx (best info for dx &tx) NORMAL VALUES: pH 7.35-7.45 PaO2 80-100 mmHg PaCO2 35-45 mmHg HCO3 22-28 mmHg HYPOXEMIC RF PaCO2 (<50-60 mmHg) RF without COPD If with COPD value would drop to 10-15 mmHg Normal PaCO2 TACHYPNEIC/HYPERCAPNEIC RF PaCO2 PHARMACOLOGY: o BRONCHODILATOR inhalation/metered dose inhaler (most common route) Seldom PO/IV UNDESIRABLE SIDE EFFECTS: nervousness, irritability, tachycardia, cardiac dysrhythmias o BETA-ADRENERGIC (SYMPATHOMIMETIC) Aerosol form (inhalation/MDI) In-line nebulization if attached to mechanical ventilator Promote vasodilation ISOPROTERENOL (Isoprel), METAPROTERENOL (Alupent), SALMETEROL (Serevent), TERBUTALINE (Brethaire) ACTION: stimulate SNS receptors at respiratory tract (relaxation of the smooth muscle and bronchodilation) o ANTICHOLINERGIC (ATROPINE SO4, IPATROPIUM BROMIDE [Atrivent]) Potent bronchodilator Blocks input from parasympathetic nervous system ADVERSE EFFECT: dryness of the secretion of the mucous membrane PO/IV/INHALATION o ANTIBIOTIC THERAPY prophylaxis (prevent infection) o NEUROMUSCULAR BLOCKER (PANCURONIUM BROMIDE) Paralysis of the muscles (voluntary muscles) Face eyes & mouth (initially) Limbs, neck, trunk Diaphragmatic and intercostals muscle Given to conscious px who is attached to mech ventilator (for effective ventilation) WHEN DISCONTINUED: return of function (in reverse); would have difficulty in talking ACETYLCHOLINESTERASE INHIBITOR (NEOSTIGMINE/PROSTIGMINE) ANTAGONIST NURSING RESPONSIBILITY: (BEFORE INJECTION) Assess placement of ET tube o To ensure mechanical ventilation is functioning well o To prevent hypoxemia Administer by slow IV infusion Keep acetylcholinesterase inhibitor at bedside for rapid reversal, if necessary Administer with morphine SO4, anti-anxiety & sedative to treat anxiety Administer only fresh solution & do not through syringe Not able to close eyes/blink: Artificial tears to lubricate eyes Suction oral cavity as necessary Never turn ventilator alarm off Reassure px that ability to move and to communicate will be restored if D/C Teach about the effects & reason for using the drug OXYGEN THERAPY: o To reverse hypoxemia of acute RF o If with COPD O2 at 1-3L/min via nasal cannula o if with PNA or ARDS 40-60% (must be used for a short period of time to prevent O 2 toxicity( AIRWAY MANAGEMENT: o INTUBATION o TRACHEOSTOMY TUBE o MECHANICAL VENTILATOR INDICATORS: APNEA, ACUTE VENTILATORY FAILURE HYPOXEMIA unresponsive to O2 therapy alone WORK OF BREATHING PROGRESSIVE RF CLASSIFICATIONS NEGATIVE PRESSURE VENTILATOR
o Creates sub-atmospheric pressure externally to draw chest upward & air into the lungs POSITIVE PRESSURE VENTILATOR o Inflate cuff of ET tube to maintain (+) pressure o Limit passage of air to nose & mouth o COMPLICATIONS: area near the cuff can be necrotic, laryngeal damage PREVENT BY: ordering high volume with lower pressure of O 2 cuff must not be fully inflated (FLOPPY CUFF) o Used for 3-4 weeks o At risk for damage (due to movement of the tube; not r/t necrosis) o TYPES: PRESSURE-CYCLED VENTILATOR VOLUME-CYCLED VENTILATOR
OTHER THERAPIES: o FLUID AND ELECTROLYTE STATUS SWAN-GANZ CATHETERIZATION at pulmonary artery S. ELECTROLYTES DAILY WEIGHT I & O if <30 ml, refer ENTERAL/PARENTERAL NUTRITION J- TUBE (preferred) - risk of regurgitation & aspiration Suction first if with secretions (due feeding is hold temporarily) NURSING INTERVENTION: o INABILITY TO SUSTAIN SPONTANEOUS VENTILATION Assess & document VS Q15-30 Assess for s/sx of respiratory distress Monitor ABG & pulse oximeter for evidence of improving/worsening respiratory status Administer O2 monitor response, observe for signs of respiratory depression Fowlers position Minimize activities & energy expenditures Avoid sedatives and respiratory depressant drugs Prepare for intubation & mechanical ventilation o INEFFECTIVE AIRWAY CLEARANCE Assess respiratory status Assess coordination of respiratory effort & ventilator Monitor and assess O2 sat and ABG Suction PRN Obtain specimen for culture Perform CPT as ordered Use minimal occluding volume technique, minimal leak technique or measured pressure in the cuff of ET Firmly secure ET/TT Provide adequate slack on ventricular tubing Assess fluid balance Maintain adequate hydration Change position frequently o RISK FOR INJURY Assess frequently head-to-toe plus complete respiratory assessment Do not bypass or turn off any alarm Report changes in clients condition or response to mechanical ventilation If there is airleak in the cuff /absent BS (ET tube is out of place/atelectasis) Turn and reposition frequently To help maintain tissue perfusion preventing skin impairment Prevent pressure ulcer Keep skin and linens dry, clean & wrinkle-free Apply lotion/powder as necessary Massage bony prominences frequently improve circulation of bony prominences Perform passive ROM Q4-8H Prevent problem of immobility such as contractures If able to perform active ROM, assist px Perform passive ROM once during at night shift Keep side rails up px has LOC Use soft restraints (linens) with doctors order To prevent removing the tube accidentally esp if px is restless Mitten restraints o Check the coloration of the hand of the px o Must not be too tight not to hamper the circulation Administer H2 blocker/antacid secretion of HCl Preventing stress ulcer (from physiologic stress) preventing hemorrhage o ANXIETY Monitor level of anxiety frequently (hypoxia anxiety & panic because of DOB) Stay with the client as much as possible Explain all procedures, monitors, unusual sounds If ventilator alarm is ringing call the nurse
o Px needs suctioning/tubes are entangled, dislodged, etc. Provide a means of communication Magic slate, flash cards, questions answerable by the hand * Problem would arise if px is under neuromuscular blocker px is not able to move hand, blink eyes, & nod head Encourage family to visit as often as possible and to participate in care Provide distraction let px watch TV, listen to music, etc. (anxiety) Attend to physical needs promptly & completely prevent panic attacks & provides reassurance Reassure that intubation and mechanical ventilation is a TEMPORARY measure If pxs condition is improved, it is removed Provide sedation as needed must be avoided, unless ordered It can further depress the respiratory function Other anti-anxiety meds as necessary OTHER NURSING DIAGNOSIS o Risk for aspiration r/t presence of ET If with DOB/SOB/tachypnea do not give feeding if with NGT o Impaired gas exchange o Powerlessness r/t inability to control environment o Impaired verbal communication o Impaired physical immobility If px is conscious, he can ambulate even if with mechanical ventilator WEANING o Process of removing the client from ventilator support o Reestablishing spontaneous, independent respirations o THE PROCESS & LENGTH OF WEANING DEPENDS ON: Pre-existing lung condition Duration of mechanical ventilation General condition both physiologic and psychologic o DURATION: SHORT-TERM Detach client from ventilator Then attach the T-piece to O2 LONG-TERM (3-4 weeks); maximum is 4 weeks Detach from ventilator for 5-15 mins (start at 5 mins) Promote rest Attach again to ventilator for several number of hours Doctor would determine period of attachment/detachment from ventilator for how many days (period of detachment from ventilator) If tolerated remove; if not TRACHEOSTOMY TUBE TERMINAL Gradual withdrawal of mechanical ventilator from a patient who is not expected to survive without assisted ventilation Family who decides to remove px from ventilator Should be done at home (ideally) Poor prognosis detach from mechanical ventilator and remove the ET (DAMA) Doctor is going switch off the ventilator and remove ET tube Done if the family is about to go o DIFFERENT COMPLICATIONS OF ET TUBE/MECHANICAL VENTILATOR: Pressure necrosis of lips, nose and trachea Nose nasopharyngeal intubation (seldom used) Trachea inflation of ET tube saliva production Improper measurement/dislodgement of ET tube Ventilation of one lung only overdistension of inflated lung & atelectasis collapse of uninflated lung Infection Respiratory alkalosis from hyperventilation, barotraumas, & CO BAROTRAUMA lung injury due to pressure at lungs SUBCUTANEOUS EMPHYSEMA Presence of air at subcutaneous tissue Indicator of damage resulting from barotraumas PNEUMOTHORAX r/t alveolar rupture overdistention with mechanical ventilator MAN: unequal chest expansion with sudden loss/significant in BS on the affected side Insertion of CTT Risk for CO Development of stress ulcer painless GI hemorrhage
ACUTE RENAL FAILURE A rapid loss of renal function due to damage of the kidneys collection of metaboli c waste product in the body Involves the sudden, usually reversible disruption of normal kidney function If untreated CRF CAUSE:
ISCHEMIA Hypovolemia BP CO & HF Bilateral obstruction of renal arteries & veins presence of tumor, blood clot & kidney stones o NEPHROTOXINS MAJOR CATEGORIES: o PRE-RENAL renal perfusion pressure GFR (ability of kidney to filter blood that goes into the kidney metabolic waste excretion) Not able to filter metabolic waste metabolic waste (AZOTEMIA) CAUSE: Hemorrhage and dehydration Account for 40-80% If treated early condition is reversible o INTRARENAL Actual damage to the renal parenchymal & nephrons of the kidney DUE TO: KIDNEY DISEASE o Acute glomerulonephritis - blood flow o Vascular disease vasculitis (inflammation of BV) Malignant HPN (both will damage nephron ARF) MARKED ATN (ACUTE TUBULAR NECROSIS) o ISCHEMIA o NEPHROTOXINS MEDICATIONS Amikacin (Amikin) most common Streptomycin, Gentamycin, Tobramycin Other meds: cephalosporin, penicillin, tetracycline, NSAIDs, ACE inhibitos, phenytoin, sulfonamide, cisplastin Exposure to chemicals carbon tetrachloride, ethylene glycol Exposure to heavy metals gold and mercury toxins in nephrons Endogenous nephrotoxin (found within the body) Hgb (release of myoglobin) o POST-RENAL OBSTRUCTIVE CAUSES: BPH, calculi, tumors, blood clots PATHOPHYSIOLOGY:
HEMORRHATE, DHN, VASCULAR OBSTRUCTION
GLOMERULAR INFLAMMATION
DRUGS, MYELO/HEMOGLOBINEMIA
RENAL BLOOD FLOW ISCHEMIA
NEPHROTOXICITY TUBULAR PERMEABILITY
GFR & IMPAIRED TUBULAR SECRETION OLIGURIA, AZOTEMIA, ELECTROLYTE IMBALANCE, ACID BASE-IMBALANCE
PHASES OF ACUTE RENAL FAILTURE o INITIATION PHASE ONSET PHASE (hours-days) Begins with initial onset tubular necrosis Ends when oliguria develops Few manifestations identified after man of later phase occurs Gradual accumulation of nitrogenous waste (creatinine & BUN) o OLIGURIC PHASE MAINTENANCE PHASE (6-8 weeks; maybe 1-3 wks or >3 weeks) Begins within hours of initiating event & lasts several hours up to 6 weeks CHARACTERISTICS: (due to persistent reduction in GFR & tubular necrosis) AZOTEMIA -creatinine, BUN, nitrogenous waste, H ions FLUID & Na RETENTION ELECTROLYTE IMBALANCE o K, Mg, PO4, uric acid Ca = PO4 UO - <30 ml or <100-400 ml/day METABOLIC ACIDOSIS ANEMIA inability of the kidney to produce erythropoietin shorten RBC life of body RISK FOR INFECTION impaired immune function (leading cause of death) o DIURETIC PHASE HIGH OUTPUT PHASE (2-6 weeks when intervention is given immediately) Indicates that the nephrons have recovered sufficiently to permit urine excretion 10 L/day of diluted urine signals the glomerular filtration rate is starting to recover but kidney function is not back to its normal function
creatinine, BUN, K, PO4 kidneys function is still not normal (AZOTEMIA) RECOVERY PHASE (3-12 months complete recovery) GFR and tubular function have recovered (BUN & creatinine) Renal function improves during the 5-25 days ASSESSMENT FINDINGS: o PRE-RENAL AZOTEMIA BP Tachycardia - CO & response to hypoxia and ischemia CO, CVP, UO Lethargy - O2 at brain Nitrogenous waste is starting to elevate o INTRA-RENAL (INTRINSIC) & POST-RENAL AZOTEMIA: Oliguria/anuria urine specific gravity o CARDIAC MANIFESTATIONS: BP Tachycardia Jugular venous distention fluid & Na retention CVP Tall T-waves o RESPIRATORY MANIFESTATIONS: SOB Orthopnea Crackles congestion Pulmonary edema Pink & frothy sputum (+) pleuritic chest pain pain on inspiration Friction rub on auscultation o GI MANIFESTATIONS: Anorexia Nausea Vomiting Flank pain o NEUROLOGIC MANIFESTATIONS: (r/t accumulation of nitrogenous waste) Lethargy Headache Tremors confusion o GENERAL MANIFESTATIONS: Generalized edema abd congestion with sacral edema; pulmonary, peripheral edema Weight gain COLLABORATIVE CARE o GOALS OF CARE: Identify/correct underlying cause, if possible Prevent additional injury to the kidney Restore UO and elimination of metabolic waste product Compensate for renal impairment until the kidneys regain its function LABORATORY TEST o URINALYSIS Specific gravity 1.010 (normal: 1.010 -1.025) (+) abnormal protein glomerular damage (+) RBC glomerular dysfunction (+) WBC inflammation (+) tubular epithelial cells ATN Casts protein & cellular debris o S. CREATININE/BUN o S. ELECTROLYTES K, Na o ABG METABOLIC ACIDOSIS (pH, HCO3) o CBC - RBC DX TEST: o BLADDER CATHETERIZATION Obtain specimen for C/S Straight catheterization Indwelling catheter if severe o UTZ Identify obstructive cause of RF Differentiate ARF from ESRF o o CT SCAN Evaluate kidney size and locate possible urinary tract obstruction (calculi, tumor) With contrast note creatinine level and refer to doctor before scheduling IVP (INTRAVENOUS PYELOGRAPHY) In general administration of a contrast medium in order to visualize the kidney o
RETROGRADE contrast agent injected into ureters ANTEGRADE contrast agent injected into renal pelvis Normalize creatinine level before scheduling px Done to evaluate the structure and functions of the kidney Done if there is no findings with UTZ/CT scan Commonly ordered for px with recurrent UTI o RENAL BIOPSY definitive dx Determine when the cause of ARF is uncertain PHARMACOLOGY MGT: o DOPAMINE for hypotensive clients (restore blood flow in the kidney) Low dosage = renal dose (tissue perfusion improve UO) Monitor UO myocardial contractility tissue perfusion of the body o LOOP DIURETIC (FUROSEMIDE) Indicated when perfusion of the kidney does not improve UO Wash out the nephrons of toxins concentration of metabolic waste Prevent oliguria o OSMOTIC DIURETIC (MANNITOL) Pull extracellular fluid into the vascular space (GFR improve UO) H2 ANTAGONIST Prevent GI hemorrhage o KAYEXELATE Tx of K (PO/retention enema) Remove K by exchanging Na ions for K ions in the large intestine Excreted by defecation Administered with sorbitol to induce diarrhea (K level would return to normal) Administered through the rectum, retained for 30-60 mins Irrigated out with the use of tap H2O enema Problem: how they will retain solution within 30-60 mins (uncontrollable urge to defecate) o DEXTROSE 50% & INSULIN Shift K back into the cells to K level o Ca REPLACEMENT to treat Ca and PO4 level PO4 to K level o ALBUTEROL SO4 as nebulizer Lower plasma K concentration by 0.5-1.5 mEq o ALUMINUM HYDROXIDE (Amphogel) antacid Control PO4 in RF Bind PO4 in GI tract excreted in the feces o Ca-CHANNEL BLOCKER Prevent movement of Ca into the kidney Maintain cell integrity Improve GFR HEALTH TEACHING FOR MEDICATION ADMINISTRATION: o Ca given IV causes lightheadedness Remain in recumbent position for 30 mins after administration o NaHCO3 Chew tablets followed by 8 oz of H2O Not to take with milk o Kayexelate as retention enema Retain as long as possible (30-60 mins) o Diuretics as discharge meds Assess weight Monitor BP before taking diuretics Record of I/O with calibrated glass limitation of fluid intake s/sx of ototoxicity maintain OFI at 2-3 L/day or as ordered CONSERVATIVE MGT: o FLUID RESTRICTION 500 ml for insensible H2O (+) previous urine output from the last 24H Ex: 500 + 300 = 800 ml (allowable fluid intake) Record accurate output o DIETARY MGT CHON not able to excrete nitrogenous waste products (end product of protein metabolism) CHO adequate caloric intake lipid level TPN with intralipid (exchange for protein source of energy/calorie) Parenteral nutrition, as indicated inadequate consumption of oral intake Restrict food rich in K banana, mango, apples, green leafy vegetables K (severely elevated) dialysis o DIALYSIS In ARF dialysis is not a permanent tx Clients kidney function would improve stop dialysis BUN/CREATININE LEVEL - indicator that dialysis needs to be performed PERITONEAL DIALYSIS EMERGENT CONDITION o
After several cycles of peritoneal dialysis family may decide to make it permanent Exchange of dialysate that would occur within the peritoneum TENKOFF CATHETER catheter that is used o Inserted inside the peritoneum o Peritoneal membrane dialyser NSG RESPONSIBILITY: o Monitor UO especially the color of output o Left in place for 20 mins o Drained thereafter and the output from the peritoneum note the color o CLOUDY COLOR PERITONITIS (refer immediately) o Any changes in the fluid that comes out of the peritoneum, refer! HEMODIALYSIS Initially the px will be inserted with a fistula (AV fistula) IV access line JUGULAR VEIN initial access site for emergent phase Later on, if dialysis is still needed, fistula formation is performed (AV fistula) Graft clients with CKD Blood that comes out from the patient will go into the machine It will be metabolized/cleared by the machine Blood is returned to the pxs body without metabolic waste NURSING DIAGNOSIS: o FLUID VOLUME EXCESS Na & H2O retention Assess & document I/O QH guide therapy, especially on fluid restriction Weigh OD even more often as prescribed (to have an accurate assessment of fluid status) Fluid retention sudden weight Monitor & record V/S Q4H BP, tachycardia, tachypnea HYPERVOLEMIA Assess for breath & heart sounds Crackles pulmonary congestion & edema S3 (LHF) & S4 gallop HF Semi-fowlers position enhance cardiac & respiratory function Monitor electrolytes K, Na, PO4 Restrict fluid intake Dry mouth & thirst hard candies, ice chips, mouth care (to promote comfort) Administer meds with meals Turn and provide good skin care impaired skin integrity r/t edema Monitor response of px to diuretics o ALTERED NUTRITION: LESS THAN BODY REQUIREMENTS Monitor and document food intake (specific amount) Weigh OD Consult with dietician, including preferred food (Na, CHON, K) Allow family to prepare meals know the dietary restriction Provide frequent feeding in small amount In-between meals (snacks) anorexic, nauseated (esp. if metabolic waste) Anti-emetics as prescribed 30 mins before meals Mouth care 30 mins before meals Parenteral nutrition, as prescribed oral intake inadequate
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Building Group Cohesion Through IcebreakersDocumento2 páginasBuilding Group Cohesion Through IcebreakersArianne BugnaAinda não há avaliações
- Ego Integrity Vs Despair (Comp App)Documento10 páginasEgo Integrity Vs Despair (Comp App)Arianne BugnaAinda não há avaliações
- Gunshot WoundDocumento4 páginasGunshot WoundArianne BugnaAinda não há avaliações
- CancerDocumento13 páginasCancerArianne BugnaAinda não há avaliações
- Use of Social Networking Websites Frequency Percent TotalDocumento3 páginasUse of Social Networking Websites Frequency Percent TotalArianne BugnaAinda não há avaliações
- Leukemia)Documento66 páginasLeukemia)Arianne BugnaAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Trailer Axle Spare Parts ListingDocumento12 páginasTrailer Axle Spare Parts ListingMata AlamAinda não há avaliações
- Week 1 Workout: Total Body Workout ADocumento4 páginasWeek 1 Workout: Total Body Workout ASam100% (2)
- SHEILA Fitness TrainingDocumento8 páginasSHEILA Fitness TrainingMaria Stella DavinesAinda não há avaliações
- WiitdbDocumento161 páginasWiitdbteknoallahAinda não há avaliações
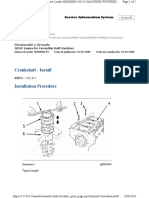
- 3024C Crankshaft - InstallDocumento2 páginas3024C Crankshaft - Installmiguel_catAinda não há avaliações
- AlyssaDocumento1 páginaAlyssaicetrolaAinda não há avaliações
- Equipment TipsDocumento9 páginasEquipment Tipsapi-247767242Ainda não há avaliações
- Bullets-history&typology-1-1Documento77 páginasBullets-history&typology-1-1Ryl-annAinda não há avaliações
- Cambridge English Young Learners' Picture BankDocumento47 páginasCambridge English Young Learners' Picture BankSara Hidalgo100% (1)
- Technical Self-Assesment SheetDocumento2 páginasTechnical Self-Assesment SheetAzeddine LAAinda não há avaliações
- Lastexception 63733199203Documento19 páginasLastexception 63733199203The GadiatorAinda não há avaliações
- 694+ Illustrated Parts Catalog Revision 3.1 FROM SERIAL TRX01694CDGL11965Documento549 páginas694+ Illustrated Parts Catalog Revision 3.1 FROM SERIAL TRX01694CDGL11965Martín Lescano ParedesAinda não há avaliações
- Engargoladora de LatasDocumento21 páginasEngargoladora de LatasAngel PerezAinda não há avaliações
- System ToolsDocumento16 páginasSystem ToolsJohn SuarezAinda não há avaliações
- Verbs 2Documento2 páginasVerbs 2bruceAinda não há avaliações
- 5a8fbc22d0ce57481 PDFDocumento80 páginas5a8fbc22d0ce57481 PDFMahendra SofyanAinda não há avaliações
- Chapter 4 Motion in Two Dimensions and ThreeDocumento25 páginasChapter 4 Motion in Two Dimensions and Threefitri dwi hartatiAinda não há avaliações
- Setup Log for Left 4 Dead InstallationDocumento963 páginasSetup Log for Left 4 Dead InstallationHestu NugrohoAinda não há avaliações
- 28 Auxiliary Percussion LessonsDocumento4 páginas28 Auxiliary Percussion LessonsJeremy WilliamsonAinda não há avaliações
- Grade 8 Science Forces and Motion Multiple ChoiceDocumento1 páginaGrade 8 Science Forces and Motion Multiple ChoiceIan Gabriel Oliquiano83% (6)
- Fostech Product Catalog 2017Documento24 páginasFostech Product Catalog 2017KenshironokenAinda não há avaliações
- 2009 Toyota Car Engine (G Series)Documento2 páginas2009 Toyota Car Engine (G Series)Shahid JavidAinda não há avaliações
- Grila All ChannelsDocumento24 páginasGrila All ChannelsCiprianCristeaAinda não há avaliações
- Chasing Adventure: A Fast-Paced Fantasy RPGDocumento41 páginasChasing Adventure: A Fast-Paced Fantasy RPGEugene YunakAinda não há avaliações
- HFF Carquest Friction 2010Documento29 páginasHFF Carquest Friction 2010gearhead1Ainda não há avaliações
- Character Sheet SummaryDocumento2 páginasCharacter Sheet SummarysynistarAinda não há avaliações
- C32 Gear Group (Front) - Install PDFDocumento4 páginasC32 Gear Group (Front) - Install PDFmanu luvungaAinda não há avaliações
- Knee PainDocumento2 páginasKnee PainKKAinda não há avaliações
- Calisthenics Calisthenics Training Plan Training Plan: Powered byDocumento7 páginasCalisthenics Calisthenics Training Plan Training Plan: Powered byLibardo Varon YazoAinda não há avaliações
- Ford 2533d-Lr Eng Euro6-Li46Xgk2Documento2 páginasFord 2533d-Lr Eng Euro6-Li46Xgk2Paul CiobanuAinda não há avaliações