Escolar Documentos
Profissional Documentos
Cultura Documentos
Roles of Renal Proximal Tubule Transport in The Pathogenesis of Hypertension
Enviado por
Vane Ordóñez VillacrésDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Roles of Renal Proximal Tubule Transport in The Pathogenesis of Hypertension
Enviado por
Vane Ordóñez VillacrésDireitos autorais:
Formatos disponíveis
Send Orders for Reprints to reprints@benthamscience.
net
148 Current Hypertension Reviews, 2013, 9, 148-155
Roles of Renal Proximal Tubule Transport in the Pathogenesis of Hypertension
Shoko Horita, George Seki*, Hideomi Yamada, Masashi Suzuki, Kazuhiko Koike and Toshiro Fujita
Department of Internal Medicine, Faculty of Medicine, University of Tokyo, Tokyo, Japan
Abstract: Hypertension is a key factor of cardiovascular disease. Many organs and systems including heart, blood vessel, kidney, sympathetic nerve, and endocrine systems are involved in the regulation of blood pressure. In particular, the kidney plays an essential role in the regulation of blood pressure, but is also quite vulnerable to hypertensive tissue damage. For example, most chronic kidney disease (CKD) patients have hypertension and are revealed to have higher mortality than normal population. Furthermore, hypertensive renal sclerosis is emerging as the third main cause of dialysis patients. This mini review is to summarize the effects of angiotensin II and dopamine on renal proximal tubule transport, which may have important roles in the regulation of blood pressure.
Keywords: Angiotensin II, AT1A, dopamine, D1, hypertension, NBCe1, renal proximal tubule, SHR. INTRODUCTION Hypertension has been, and will be, one of the big threats against our health [1, 2]. Many studies show that hypertension raises mortality and morbidity of serious diseases like coronary events and cerebrovascular disorders [1, 3]. Although there are several classes of drugs that are effective for the treatment of hypertension, the etiology of hypertension has not been fully established. According to a lot of studies based on different approaches, a variety of organs and systems including heart, blood vessel, and kidney may be involved in the onset of hypertension [4, 5]. Recently the idea of cardio-renal relationship has been claimed, which insists the importance of renal factors as the cause of heart disease [6]. Traditionally, the effects of aldosterone on distal nephrons in the pathogenesis of hypertension have been intensively investigated. Recently, however, several hormones acting on renal proximal tubules such as angiotensin II, dopamine, and insulin have been also investigated in relation to the regulation of blood pressure [7-9].� Most of the human mutations resulting in the alterations in blood pressure affect sodium transporters in distal nephrons [10]. Alterations in renal proximal tubule transport may be also linked to the onset of hypertension as well, but the mechanism is not fully clarified [11, 12]. However, there are several evidences that angiotensin II and dopamine are important regulators of blood pressure acting on the proximal tubule [13, 14]. This mini review will discuss the importance of renal proximal tubule for the regulation of blood pressure, and the importance of angiotensin II and dopamine in this aspect. BIPHASIC REGULATION OF RENAL PROXIMAL TUBULE TRANSPORT BY ANGIOTENSIN II Angiotensin II (Ang II) receptors can be divided into two major subtypes, type 1 (AT1) and type 2 (AT2). Type 1 receptor has furthermore two subtypes, AT1A and AT1B in rodents [15, 16]. So far AT1A is shown to be far more abundant than AT1B in the kidney [17-20]. In human only one AT1 receptor has been found [21, 22]. Although AT1 is the main receptor that determines blood pressure, AT2 may be also involved in the regulation of blood pressure [23]. AT2 is abundant in the developing fetus kidney but declines soon after birth [24, 25]. Ang II seems to be directly secreted into proximal tubular lumen by the epithelial cells after the conversion from angiotensinogen [26]. In hypertensive status, angiotensinogen expression is increased and the exaggerated Ang II secretion into the proximal lumen may traverse through the distal nephron and provide substrate for further production of Ang II [27, 28]. Ang II has direct effects on renal tubular functions besides on renal hemodynamics. One of its important effects is on proximal tubule transport, which is considered to have quite an important role in the regulation of whole-body fluid and salt balance [8, 29-31]. It is well known that the concentration of Ang II in kidney is much higher than in plasma. For example, the concentration of Ang II is found to be 5 to 10 nmol/L in rat kidney interstitial fluid [26, 32, 33]. The Ang II concentration in the proximal tubule is reported to be even higher (30 to 40 nmol/L) [34]. The similar concentration is found in tubular fluid collected from the downstream of proximal tubule [35]. Furthermore it is known that the regulation of circulating Ang II concentration can be dissociated from that of intratubular Ang II concentration [35, 36].
*Address correspondence to this author at the Department of Internal Medicine, Faculty of Medicine, University of Tokyo, 7-3-1, Hongo, Bunkyo, Tokyo 113-8655, Japan; Tel: +81 3 3815 5411 ext: 33004; Fax: +81 3 5800 8806; E-mail: georgeseki-tky@umin.ac.jp 1875-6506/13 $58.00+.00
2013 Bentham Science Publishers
Roles of Renal Proximal Tubule Transport in the Pathogenesis
Current Hypertension Reviews, 2013, Vol. 9, No. 2
149
It has been shown that AT1A receptors in the kidneys are important not only for normal blood pressure regulation but also for mediating the hypertensive response to Ang II infusions [37, 38]. Furthermore others have shown that AT1A knockout mice show hypotension and fail to develop hypertension by unilateral renal arterial constriction [39, 40]. These studies show the critical importance of renal AT1A receptor in the regulation of blood pressure. In the proximal tubule Ang II acts on Na+-HCO3cotransporter (NBCe1), Na+/H+ exchanger 3 (NHE3), and Na+-K+-ATPase in a biphasic way [41-45]. The biphasic effects of Ang II have been reported in proximal tubules from several species. In general, Ang II shows stimulatory effects at picomolar to nanomolar concentrations, and inhibitory effects at nanomolar to micromolar concentrations [8, 29, 46]. Controversial results have been reported as to the receptor subtype(s) mediating the biphasic effects of Ang II [41, 47]. For example, one study reported that AT1 mediates the stimulatory effect, while AT2 mediates the inhibitory effect [48]. However, this study was performed with cultured proximal tubular cells that might express apical AT2. By contrast, using the similar cultured tubular cells the other group reported that AT1 mediates both stimulatory and inhibitory effects [41]. To clarify which receptor is involved in this biphasic effects, we took advantage of AT1A knockout mice [49]. We focused on the effects of Ang II on NBCe1, which mediates a majority of sodium-coupled bicarbonate efflux from the basolateral membranes of proximal tubule [42, 43, 50-54]. In isolated proximal tubules from wild type mice, Ang II showed a stimulatory effect on the NBeC1 activity at a lower concentration (10-10M) but showed an inhibitory effect at a higher concentration (10-6M) [55]. In isolated proximal tubules from AT1A KO mice, the stimulatory effect by the lower Ang II concentration was lost, while the higher Ang II concentration exerted the stimulatory effect. These results indicate that AT1A in the basolateral membrane of wild type proximal tubule is responsible for the biphasic effects of Ang II. They further suggest that AT1B is responsible for the stimulation by the higher concentration of Ang II in the absence of AT1A. Experiments with the specific antagonists of AT1 and AT2 confirmed this hypothesis. In the luminal side, Ang II showed the similar biphasic effects on bicarbonate transport via AT1A in the luminal membrane [56]. To further clarify the signaling pathways underlying the biphasic effects of Ang II, we compared the responses to Ang II in wild type, AT1A KO, and cPLA2� knockout mice. The results revealed that the MEK/ERK signal transduction system mediates the stimulatory effect, while the cPLA2 �/P450 pathway is involved in the inhibitory effect [57]. At the same time the activation of cPLA2�/P450 pathway seems to suppress the ERK/MEK pathway [58]. These results suggest that the balance between ERK/MEK and cPLA2 �/P450 activation via AT1A may determine the final responses of proximal tubular transport to Ang II. This is quite important in view of the extremely high
concentrations of Ang II in the proximal tubular fluid [34]. For example, one study showed that high-salt diet, which suppresses the systemic Ang II concentration as expected, paradoxically raises the Ang II concentration in rat proximal tubule to a level approaching to the inhibitory range [59]. PHYSIOLOGICAL ROLES OF ANG II-MEDIATED REGULATION OF PROXIMAL TUBULE TRANSPORT A series of our studies has clarified that AT1A plays an essential role in the regulation of renal proximal tubule transport, which may have a substantial impact on blood pressure control. On the other hand, Ang II can also regulate blood pressure through the effects on extrarenal tissues including vasculatures. To clarify the relative importance of AT1A in renal and extrarenal tissues in the control of blood pressure, Coffman and colleagues have used a kidney crosstransplantation strategy in AT1A KO and wild type mice to separate the actions of AT1A in the kidney from those in systemic tissues. They demonstrated that distinct and virtually equivalent contributions of AT1A actions in the kidney and in extrarenal tissues to determining the base-line level of blood pressure [60]. They further showed that renal AT1A is absolutely required for the development of Ang IIinduced hypertension and cardiac hypertrophy [38]. To further distinguish the AT1A actions in proximal tubules and other tissues within the kidney, they [61] have made mice lacking AT1A only in the proximal receptors by crossing mice with a conditional Agtr1a allele with a PepckCre transgenic mouse line expressing Cre in proximal but not distal nephron segments [62]. These mice showed approximately 10 mmHg lower blood pressure than that of wild type mice. The transgenic mice also showed significantly lower rates of in vivo proximal fluid reabsorption and GFRs. Furthermore, the transgenic mice showed lower blood pressure elevation (23 +/- 3mmHg) compared to that of wild type mice (38 +/- 5 mmHg) in response to the Ang II infusion. The expression levels of proximal sodium transporters, such as NHE3 and NaPi2 were suppressed after the Ang II infusion in the transgenic mice but not, or suppressed less, in the wild type mice. On the other hand, there were no significant changes in the expression level of NKCC2 and ENaC in Henle loop and distal tubule after Ang II infusion. This study shows that AT1A in renal proximal tubules, by regulating fluid absorption from this segment, plays quite an important role in the regulation of blood pressure. Using androgen-dependent promoter construct, Li et al. made transgenic mice with either overexpression of a constitutively active AT1A transgene or depletion of endogenous AT1A, both specific to the proximal tubule [63]. They demonstrated that the AT1A depleted mice have reduced blood pressure, while the AT1A activated mice showed hypertension in baseline. These results are also consistent with a view that Ang II signaling via AT1A in the proximal tubule regulates systemic blood pressure under baseline conditions.
150 Current Hypertension Reviews, 2013, Vol. 9, No. 2
Horita et al.
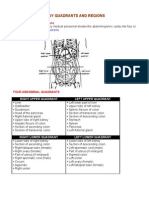
Recently proteomic analysis was performed to clarify the Ang II induced signal response and onset of hypertension. Zhuo et al. [64] studied the signal protein phosphorylation in proximal tubules of wild type rats after two week infusion of Ang II. At pressor dose 14 proteins among 38 studied proteins were phosphorylated, including PKC�, PKC�II, GSK3� and GSK3�. At non-pressor dose only 7 proteins were phophorylated, including PKC�, PKC� and GSK�. Unexpectedly, phosphorylation of MAPK and ERK1/2 were not altered in proximal tubules in vivo at pressor dose. These signal responses were largely blocked by losartan. This result suggests that signaling pathways involving PKC�, PKC�, GSK3�, GSK3�, and cAMP-dependent pathways may have an important role in this model of Ang II induced hypertension. In human, as described above, only one AT1 receptor exists. However, as AT1A is expressed predominantly in most organs such as kidney, heart, brain, adrenal gland, and vascular smooth muscle [17], rodent AT1A may correspond to human AT1 . Therefore the results obtained by AT1A knockout mice [61] may also have significant relevance to the pathogenesis of human hypertension. DOPAMINE AND RENAL PROXIMAL TUBULE Dopamine (DA) is another strong regulator of blood pressure, as well as an essential neurotransmitter. Previous studies have shown that dopamine modulates Ang II actions in the kidney, mainly antagonizing Ang II actions [65, 66]. Cheng et al. have showed that DA decreased AT1 expression in the proximal tubule via D1 receptor, suggesting that dopamine may reset the sensitivity of proximal tubule to Ang II [65]. DA receptors are classified into D1-like (D1, D5) and D2like (D2, D2 and D4) subtypes, closely related G protein-coupled receptors (GPCRs) [67-72]. D1-class dopamine receptors (D1 and D5) activate G�s/orf family of G proteins to stimulate cAMP production by adenylate cyclase (AC), while D2-class dopamine receptors (D2, D3 and D4) couple to the G�i/o family of G proteins and induce inhibition of AC [73, 74]. Fig. (1) shows a simplified scheme of dopamine signaling [74-77]. Because L-DOPA, precursor of DA, enters the cell and is converted to DA by aromatic amino acid decarboxylase (AADC), both exogenous and endogenous DA may exert signalling. When GDP is bound, G� is associated with G�/� and is inactive. DA binds to D1 receptor and promotes exchange of GDP with GTP on the G � subunit, then G � dissociates from G�/�. G � stimulates adenylate cyclase (AC), which produces cAMP. cAMP stimulates PKA and initiate signalling. G protein-coupled receptor kinase (GRK) desensitizes D1 and decreases their ability to initiate the signalling process. D1, not D5, couples to Go [78], while D5, not D1, couples to Gz and G�12/13 [79, 80]. Both are also linked to G�q [8184]. D2-like receptors, D2, D3, and D4 couple to G-proteins G�i and Go, inhibit AC and calcium channel activities, and modulate potassium channel activity [14, 85, 86].
All dopamine receptor subtypes are expressed in the renal tubules and renal vasculature, but not distributed equally along the mammalian nephron. In the renal proximal tubule, all dopamine receptor family is present. In the medullary thick ascending limb of Henle D1, D3 and D5 are expressed, while in the cortical thick ascending limb only D3 exists. In the distal convoluted tubule D1 and D3 are localized while the collecting duct expresses all except D2 [76, 85, 87]. DA inhibits sodium transporters at multiple sites along the renal tubule and acts on multiple targets possibly via D1; NHE1 [88], NHE3 [89-92], Na+-K +-ATPase [93-106], Na/PiIIa [107-110], and possibly NCC [111]. Via D4 it may also inhibit ENaC and argininie vasopressin-dependent sodium transport and water permeability [112, 113]. On the other hand, DA stimulates NKCC2 in medullary thick ascending limb. Because Na+-K+-ATPase is inhibited however, the overall transport is decreased [114]. However, the microperfusion studies on isolated proximal tubules have not consistently confirmed a direct tubular effect of DA [115, 116]. One study suggested that DA inhibits proximal transport only in the presence of norepinephrine (NE) [117]. They showed that in isolated rabbit proximal tubules DA inhibits proximal tubule volume reabsorption and net sodium reabsorption, only in the presence of NE. We also observed that DA inhibits the renal proximal NBCe1 activity only in the presence of NE. NBCe1 contributes sodium reabsorption in the basolateral side of proximal tubule, so this means that DA induces natriuresis in proximal tubule [54]. These results suggest that DA may require NE to inhibit in vivo sodium reabsorption from proximal tubule. Felder and colleagues have clarified that in the spontaneously hypertensive rat (SHR) there is a defect in the coupling mechanism of D1 and its second messenger [118]. They found that decreased ability of D1 agonists to stimulate AC activity in the proximal convoluted tubules of SHR is due to an altered D1 G protein coupling mechanism. Later they found a similar defect in D1 signaling in the human proximal tubular cells obtained from hypertensive subjects [119]. They also suggested that this uncoupling is one of the important causes of hypertension in the SHR and that the similar mechanism may be also involved in the cause of hypertension in human. [118-120] As mentioned above, DA seems to antagonize AngII effect. Harris and colleagues showed that DA reduces AT 1 expression in rat primary proximal tubular cells [65]. This effect is mediated via D1 receptor while D2 did not have inhibitory effect on AT1 expression. Later Jose and colleagues showed, using human proximal tubular cell lines, that D5 mediates AT1 degradation via a ubiquitin-proteasome pathway [66]. They also proved that D5 knockout mice have elevated AT1 expression and these mice showed raised blood pressure which is blocked by AT1 blockade. On the other hand Aperia and colleagues clarified that, D1 and AT1 make complex and function reciprocal to each other [100]. The interaction between D1 and AT1 is
Roles of Renal Proximal Tubule Transport in the Pathogenesis
Current Hypertension Reviews, 2013, Vol. 9, No. 2
151
Fig. (1). DA signaling in renal proximal tubules. G � is associated with G�/� and is inactive in corporation with GDP. L-DOPA, precursor of DA, enters the cell and is converted to DA by aromatic amino acid decarboxylase (AADC). Both endogenous and exogenous DA can bind to D1 receptor. DA promotes exchange of GDP with GTP on the G� subunit, then G� dissociates from G�/�. Released from G�/� and coupled with GTP, G� stimulates adenylate cyclase (AC), which produces cAMP. cAMP stimulates PKA that may initiate the inhibitory signalling for sodium transporters. G protein-coupled receptor kinase (GRK) desensitizes D1 and decreases their ability to initiate the signalling process.
attenuated in the presence of AII or DA agonist. They also showed later that losartan, an AT1 antagonist, increases D1 activity in HEK cells and rat proximal tubule cells [121]. The proposed relationship between D1 and AT1 is summarized in Fig. (2). DOPAMINE SIGNALING DEFECTS AND HUMAN HYPERTENSION Felder et al. [122] have shown that single nucleotide polymorphisms of a G protein-coupled receptor kinase (GRK4�) are related to human essential hypertension through the increase in G protein-coupled receptor kinase (GRK) activity. These polymorphisms cause the serine phosphorylation and uncoupling of the D1 receptor from its G protein/effector enzyme complex in the proximal tubule and in transfected Chinese hamster ovary cells. They also showed that among GRK4� polymorphisms GRK4�A142V
has the most drastic effect on D1 receptor. The GRK4�A142V transgenic mice had hypertension. There are seven GRKs, subtypes 1 to 7. Among them mainly GRK4 regulates renal proximal D1 [123]. Unlike other subtypes, GRK4 has four splice variants (GRK4�, �, �, and �) in human, five in rats, and one in mice [123-129]. The GRK4 isoform desensitizes D1 and D3 in a cell-specific manner; GRK4� in CHO and human renal proximal tubule cells [122, 126], GRK4 � also desensitizes D1 in HEK-293 cells [130, 131] and D3 in human renal proximal tubular cells [132]. On the contrary, GRK4� does not desensitize AT 1 [133] or parathyroid hormone receptor [126, 134]. The GRK4 locus on human chromosome 4p16.3 may be linked to the increase in blood pressure before adult [135] and hypertension in adult [136]. Adolescents with GRK4 65L/142V/A486 haplotype have a greater increase in blood
152 Current Hypertension Reviews, 2013, Vol. 9, No. 2
Horita et al.
Fig. (2). The interaction between AT1 signalling and D1 signalling. AT1 and D1 may make a functional complex. Activation of either AT1 or D1 may, by dissociating the complex, attenuate the expression of the other receptor. On the other hand, the binding of AT1 antagonist may facilitate the DA signalling.
pressure with age than those with wild-type GRK4 haplotype [137]. However there are some reports that GRK4 variants do not induce hypertension [138, 139]. The relation between GRK4 variants and hypertension would need further investigation. ENDOGENOUS DOPAMINE EFFECTS REGULATING BLOOD PRESSURE ON
Proximal convoluted tubules are known to contain the enzyme AADC, that converts L-DOPA to DA [140-142]. Recently Zhang et al. developed a mouse with defective intrarenal dopamine production [143]. They created the mice without AADC, which plays an essential role in the synthesis of dopamine in the proximal tubule. These mice expressed increased nephron sodium transporters, decreased natriuresis and dieresis in response to L-dihydroxyphenylalanine, and decreased medullary COX-2 expression and urinary prostaglandin E2 excretion. These mice developed saltsensitive hypertension and furthermore showed shorter lifespan than wild type mice. This indicates that dysfunction in endogenous intrarenal dopaminergic system will lead to hypertension and raised mortality, suggesting that Ang II and dopamine may have opposite actions in the viewpoint of both blood pressure and lifespan [144]. CONCLUSION Renal proximal tubule is a key site for regulating blood pressure and fluid balance. Among several factors, Ang II and dopamine are especially important in the regulation of proximal tubule transport. Ang II can increase blood pressure mainly through its effects on the kidney. Recent studies have revealed that the biphasic effects of Ang II on renal proximal tubule transport are mediated by AT1A. Furthermore, balance between ERK/MEK and cPLA2�/P450 activities may determine the final tubular responses to
Ang II. The effect of dopamine is rather complicated. DA receptors are expressed in the multiple segments of the tubule, while the proximal tubule expresses all subtypes. The uncoupling of D1-G protein in proximal tubules may be related to the occurrence of hypertension in SHR. Recently it is also suggested that the defective regulation of D1 by GRK polymorphisms may be related to the occurrence of hypertension in humans. Future studies will be warranted to further clarify the roles of renal proximal tubule transport in the regulation of blood pressure. CONFLICT OF INTEREST The author(s) confirm that this article content has no conflict of interest. ACKNOWLEDGEMENTS Declared none. REFERENCES
[1] [2] Levy D, Larson MG, Vasan RS, et al. The progression from hypertension to congestive heart failure. JAMA 1996; 275(20): 1557-62. Rosendorff C, Black HR, Cannon CP, et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation 2007; 115(21): 2761-88. Ho KK, Pinsky JL, Kannel WB, et al. The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol 1993; 22(4 Suppl A): 6A-13A. Luft FC, Mervaala E, Mller DN, et al. Hypertension-induced endorgan damage : A new transgenic approach to an old problem. Hypertension 1999; 33(1 Pt 2): 212-8. Intengan HD, Schiffrin EL. Vascular remodeling in hypertension: roles of apoptosis, inflammation, and fibrosis. Hypertension 2001; 38(3 Pt 2): 581-7. Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004; 351(13): 1296-305.
[3]
[4] [5]
[6]
Roles of Renal Proximal Tubule Transport in the Pathogenesis [7] Shibata S, Nagase M, Yoshida S, et al. Podocyte as the target for aldosterone: roles of oxidative stress and Sgk1. Hypertension 2007; 49(2): 355-64. Harris PJ, Young JA. Dose-dependent stimulation and inhibition of proximal tubular sodium reabsorption by angiotensin II in the rat kidney. Pflugers Arch 1977; 367(3): 295-7. Hall JE. The kidney, hypertension, and obesity. Hypertension 2003; 41(3 Pt 2): 625-33. Lifton RP, Gharavi AG, Geller DS. Molecular mechanisms of human hypertension. Cell 2001; 104(4): 545-56. Cogan MG. Angiotensin II: a powerful controller of sodium transport in the early proximal tubule. Hypertension 1990; 15(5): 451-8. Doris PA. Renal proximal tubule sodium transport and genetic mechanisms of essential hypertension. J Hypertens 2000; 18(5): 509-19. Navar LG, Imig JD, Zou L, et al. Intrarenal production of angiotensin II. Semin Nephrol 1997; 17(5): 412-22. Hussain T, Lokhandwala MF. Renal dopamine receptors and hypertension. Exp Biol Med (Maywood) 2003; 228(2): 134-42. Inagami T, Guo DF, Kitami Y. Molecular biology of angiotensin II receptors: an overview. J Hypertens Suppl 1994; 12(10): S83-94. Sasamura H, Hein L, Krieger JE, et al. Cloning, characterization, and expression of two angiotensin receptor (AT-1) isoforms from the mouse genome. Biochem Biophys Res Commun 1992; 185(1): 253-9. Burson JM, Aguilera G, Gross KW, et al. Differential expression of angiotensin receptor 1A and 1B in mouse. Am J Physiol 1994; 267(2 Pt 1): E260-7. Du Y, Yao A, Guo D, et al. Differential regulation of angiotensin II receptor subtypes in rat kidney by low dietary sodium. Hypertension 1995; 25(4 Pt 2): 872-7. Gasc JM, Shanmugam S, Sibony M, et al. Tissue-specific expression of type 1 angiotensin II receptor subtypes. An in situ hybridization study. Hypertension 1994; 24(5): 531-7. Llorens-Cortes C, Greenberg B, Huang H, et al. Tissular expression and regulation of type 1 angiotensin II receptor subtypes by quantitative reverse transcriptase-polymerase chain reaction analysis. Hypertension 1994; 24(5): 538-48. Balmforth AJ, Bryson SE, Aylett AJ, et al. Comparative pharmacology of recombinant rat AT1A, AT1B and human AT1 receptors expressed by transfected COS-M6 cells. Br J Pharmacol 1994; 112(1): 277-81. Chen D, Coffman TM. The kidney and hypertension: lessons from mouse models. Can J Cardiol 2012;28(3):305-10. Ichiki T, Labosky PA, Shiota C, et al. Effects on blood pressure and exploratory behaviour of mice lacking angiotensin II type-2 receptor. Nature 1995; 377(6551): 748-50. Allen AM, Zhuo J, Mendelsohn FA. Localization of angiotensin AT1 and AT2 receptors. J Am Soc Nephrol 1999; 10 Suppl 11: S23-9. Bagby SP, LeBard LS, Luo Z, et al. ANG II AT(1) and AT(2) receptors in developing kidney of normal microswine. Am J Physiol Renal Physiol 2002; 283(4): F755-64. Navar LG, Harrison-Bernard LM, Wang CT, et al. Concentrations and actions of intraluminal angiotensin II. J Am Soc Nephrol 1999; 10 Suppl 11: S189-95. Kobori H, Nishiyama A, Harrison-Bernard LM, et al. Urinary angiotensinogen as an indicator of intrarenal Angiotensin status in hypertension. Hypertension 2003; 41(1): 42-9. Navar LG, Prieto MC, Satou R, et al. Intrarenal angiotensin II and its contribution to the genesis of chronic hypertension. Curr Opin Pharmacol 2011;11(2):180-6. Schuster VL, Kokko JP, Jacobson HR. Angiotensin II directly stimulates sodium transport in rabbit proximal convoluted tubules. J Clin Invest 1984; 73(2): 507-15. Harris PJ, Navar LG. Tubular transport responses to angiotensin. Am J Physiol 1985; 248(5 Pt 2): F621-30. Liu FY, Cogan MG. Angiotensin II stimulates early proximal bicarbonate absorption in the rat by decreasing cyclic adenosine monophosphate. J Clin Invest 1989; 84(1): 83-91. Navar LG, Harrison-Bernard LM, Nishiyama A, et al. Regulation of intrarenal angiotensin II in hypertension. Hypertension 2002; 39(2 Pt 2): 316-22. [33]
Current Hypertension Reviews, 2013, Vol. 9, No. 2
153
[8] [9] [10] [11]
[34] [35] [36]
[37] [38] [39]
[12] [13] [14] [15] [16]
[40]
[41] [42]
[17]
[18] [19]
[43]
[44]
[20]
[45] [46]
[21]
[22] [23] [24]
[47] [48]
[49] [50]
[25] [26]
[51] [52]
[27] [28]
[53] [54]
[29] [30] [31]
[55] [56]
[32]
Nishiyama A, Seth DM, Navar LG. Renal interstitial fluid concentrations of angiotensins I and II in anesthetized rats. Hypertension 2002; 39(1): 129-34. Seikaly MG, Arant BS, Seney FD. Endogenous angiotensin concentrations in specific intrarenal fluid compartments of the rat. J Clin Invest 1990; 86(4): 1352-7. Braam B, Mitchell KD, Fox J, et al. Proximal tubular secretion of angiotensin II in rats. Am J Physiol 1993; 264(5 Pt 2): F891-8. Navar LG, Lewis L, Hymel A, et al. Tubular fluid concentrations and kidney contents of angiotensins I and II in anesthetized rats. J Am Soc Nephrol 1994; 5(4): 1153-8. Coffman TM, Crowley SD. Kidney in hypertension: guyton redux. Hypertension 2008; 51(4): 811-6. Crowley SD, Gurley SB, Herrera MJ, et al. Angiotensin II causes hypertension and cardiac hypertrophy through its receptors in the kidney. Proc Natl Acad Sci U S A 2006; 103(47): 17985-90. Cervenka L, Vaneckov I, Huskov Z, et al. Pivotal role of angiotensin II receptor subtype 1A in the development of twokidney, one-clip hypertension: study in angiotensin II receptor subtype 1A knockout mice. J Hypertens 2008; 26(7):1379-89. Cervenka L, Horcek V, Vaneckov I, et al. Essential role of AT1A receptor in the development of 2K1C hypertension. Hypertension 2002; 40(5): 735-41. Han HJ, Park SH, Koh HJ, et al. Mechanism of regulation of Na+ transport by angiotensin II in primary renal cells. Kidney Int 2000; 57(6): 2457-67. Coppola S, Fromter E. An electrophysiological study of angiotensin II regulation of Na-HCO3 cotransport and K conductance in renal proximal tubules. I. Effect of picomolar concentrations. Pflugers Arch 1994; 427(1-2): 143-50. Coppola S, Fromter E. An electrophysiological study of angiotensin II regulation of Na-HCO3 cotransport and K conductance in renal proximal tubules. II. Effect of micromolar concentrations. Pflugers Arch 1994; 427(1-2): 151-6. Houillier P, Chambrey R, Achard JM, et al. Signaling pathways in the biphasic effect of angiotensin II on apical Na/H antiport activity in proximal tubule. Kidney Int 1996; 50(5):1496-505. Aperia A, Holtback U, Syren ML, et al. Activation/deactivation of renal Na+,K(+)-ATPase: a final common pathway for regulation of natriuresis. FASEB J 1994; 8(6): 436-9. Wang T, Chan YL. The role of phosphoinositide turnover in mediating the biphasic effect of angiotensin II on renal tubular transport. J Pharmacol Exp Ther 1991; 256(1): 309-17. Poggioli J, Lazar G, Houillier P, et al. Effects of angiotensin II and nonpeptide receptor antagonists on transduction pathways in rat proximal tubule. Am J Physiol 1992; 263(4 Pt 1): C750-8. Haithcock D, Jiao H, Cui XL, et al. Renal proximal tubular AT2 receptor: signaling and transport. J Am Soc Nephrol 1999; 10(11): S69-74. Sugaya T, Nishimatsu S, Tanimoto K, et al. Angiotensin II type 1a receptor-deficient mice with hypotension and hyperreninemia. J Biol Chem 1995; 270(32): 18719-22. Seki G, Coppola S, Fromter E. The Na(+)-HCO3- cotransporter operates with a coupling ratio of 2 HCO3- to 1 Na+ in isolated rabbit renal proximal tubule. Pflugers Arch 1993; 425(5-6): 409-16. Yamada H, Seki G, Taniguchi S, et al. Roles of Ca2+ and PKC in regulation of acid/base transport in isolated proximal tubules. Am J Physiol 1996; 271(5 Pt 2): F1068-76. Geibel J, Giebisch G, Boron WF. Angiotensin II stimulates both Na(+)-H+ exchange and Na+/HCO3- cotransport in the rabbit proximal tubule. Proc Natl Acad Sci U S A 1990; 87(20): 7917-20. Ruiz OS, Qiu YY, Wang LJ, et al. Regulation of the renal NaHCO3 cotransporter: IV. Mechanisms of the stimulatory effect of angiotensin II. J Am Soc Nephrol 1995; 6(4): 1202-8. Kunimi M, Seki G, Hara C, et al. Dopamine inhibits renal Na+:HCO3- cotransporter in rabbits and normotensive rats but not in spontaneously hypertensive rats. Kidney Int 2000; 57(2): 534-43. Horita S, Zheng Y, Hara C, et al. Biphasic regulation of Na+HCO3- cotransporter by angiotensin II type 1A receptor. Hypertension 2002; 40(5): 707-12. Zheng Y, Horita S, Hara C, et al. Biphasic regulation of renal proximal bicarbonate absorption by luminal AT(1A) receptor. J Am Soc Nephrol 2003; 14(5): 1116-22.
154 Current Hypertension Reviews, 2013, Vol. 9, No. 2 [57] Li Y, Yamada H, Kita Y, et al. Roles of ERK and cPLA2 in the angiotensin II-mediated biphasic regulation of Na+-HCO3(-) transport. J Am Soc Nephrol 2008; 19(2): 252-9. Li Y, Yamada H, Kita Y, et al. Arachidonic acid metabolites inhibit the stimulatory effect of angiotensin II in renal proximal tubules. Hypertens Res 2008; 31(12): 2155-64. Thomson SC, Deng A, Wead L, et al. An unexpected role for angiotensin II in the link between dietary salt and proximal reabsorption. J Clin Invest 2006; 116(4): 1110-6. Crowley SD, Gurley SB, Oliverio MI, et al. Distinct roles for the kidney and systemic tissues in blood pressure regulation by the renin-angiotensin system. J Clin Invest 2005; 115(4): 1092-9. Gurley SB, Riquier-Brison AD, Schnermann J, et al. AT1A angiotensin receptors in the renal proximal tubule regulate blood pressure. Cell Metab 2011; 13(4): 469-75. Rankin EB, Tomaszewski JE, Haase VH. Renal cyst development in mice with conditional inactivation of the von Hippel-Lindau tumor suppressor. Cancer Res 2006; 66(5): 2576-83. Li H, Weatherford ET, Davis DR, et al. Renal Proximal Tubule Angiotensin AT1A Receptors Regulate Blood Pressure. Am J Physiol Regul Integr Comp Physiol 2011. Li XC, Zhuo JL. Phosphoproteomic analysis of AT(1) receptormediated signaling responses in proximal tubules of angiotensin IIinduced hypertensive rats. Kidney Int 2011. Cheng HF, Becker BN, Harris RC. Dopamine decreases expression of type-1 angiotensin II receptors in renal proximal tubule. J Clin Invest 1996; 97(12): 2745-52. Li H, Armando I, Yu P, et al. Dopamine 5 receptor mediates Ang II type 1 receptor degradation via a ubiquitin-proteasome pathway in mice and human cells. J Clin Invest 2008; 118(6): 2180-9. Andersen PH, Gingrich JA, Bates MD, et al. Dopamine receptor subtypes: beyond the D1/D2 classification. Trends Pharmacol Sci 1990; 11(6): 231-6. Niznik HB, Van Tol HH. Dopamine receptor genes: new tools for molecular psychiatry. J Psychiatry Neurosci 1992; 17(4): 158-80. Sibley DR, Monsma FJ. Molecular biology of dopamine receptors. Trends Pharmacol Sci 1992; 13(2): 61-9. Sokoloff P, Andrieux M, Besanon R, et al. Pharmacology of human dopamine D3 receptor expressed in a mammalian cell line: comparison with D2 receptor. Eur J Pharmacol 1992; 225(4): 331-7. Civelli O, Bunzow JR, Grandy DK. Molecular diversity of the dopamine receptors. Annu Rev Pharmacol Toxicol 1993; 33: 281307. Vallone D, Picetti R, Borrelli E. Structure and function of dopamine receptors. Neurosci Biobehav Rev 2000; 24(1): 125-32. Beaulieu JM, Gainetdinov RR. The physiology, signaling, and pharmacology of dopamine receptors. Pharmacol Rev 2011; 63(1): 182-217. Dohlman HG, Thorner JW. Regulation of G protein-initiated signal transduction in yeast: paradigms and principles. Annu Rev Biochem 2001; 70: 703-54. Jose PA, Eisner GM, Felder RA. Dopamine receptor-coupling defect in hypertension. Curr Hypertens Rep 2002; 4(3): 237-44. Zeng C, Sanada H, Watanabe H, et al. Functional genomics of the dopaminergic system in hypertension. Physiol Genomics 2004; 19(3): 233-46. Aperia A, Fryckstedt J, Holtbck U, et al. Cellular mechanisms for bi-directional regulation of tubular sodium reabsorption. Kidney Int 1996; 49(6): 1743-7. Kimura K, White BH, Sidhu A. Coupling of human D-1 dopamine receptors to different guanine nucleotide binding proteins. Evidence that D-1 dopamine receptors can couple to both Gs and G(o). J Biol Chem 1995; 270(24): 14672-8. Sidhu A, Kimura K, Uh M, et al. Multiple coupling of human D5 dopamine receptors to guanine nucleotide binding proteins Gs and Gz. J Neurochem 1998; 70(6): 2459-67. Zheng S, Yu P, Zeng C, et al. Galpha12- and Galpha13-protein subunit linkage of D5 dopamine receptors in the nephron. Hypertension 2003; 41(3): 604-10. Felder CC, Jose PA, Axelrod J. The dopamine-1 agonist, SKF 82526, stimulates phospholipase-C activity independent of adenylate cyclase. J Pharmacol Exp Ther 1989; 248(1): 171-5. Jin LQ, Wang HY, Friedman E. Stimulated D(1) dopamine receptors couple to multiple Galpha proteins in different brain regions. J Neurochem 2001; 78(5): 981-90. [83]
Horita et al. Vyas SJ, Eichberg J, Lokhandwala MF. Characterization of receptors involved in dopamine-induced activation of phospholipase-C in rat renal cortex. J Pharmacol Exp Ther 1992; 260(1): 134-9. Liu J, Wang F, Huang C, et al. Activation of phosphatidylinositollinked novel D1 dopamine receptor contributes to the calcium mobilization in cultured rat prefrontal cortical astrocytes. Cell Mol Neurobiol 2009; 29(3): 317-28. Zeng C, Armando I, Luo Y, et al. Dysregulation of dopaminedependent mechanisms as a determinant of hypertension: studies in dopamine receptor knockout mice. Am J Physiol Heart Circ Physiol 2008; 294(2): H551-69. Holmes A, Lachowicz JE, Sibley DR. Phenotypic analysis of dopamine receptor knockout mice; recent insights into the functional specificity of dopamine receptor subtypes. Neuropharmacology 2004; 47(8): 1117-34. Felder RA, Jose PA. Mechanisms of disease: the role of GRK4 in the etiology of essential hypertension and salt sensitivity. Nat Clin Pract Nephrol 2006; 2(11): 637-50. Lin CY, Varma MG, Joubel A, et al. Conserved motifs in somatostatin, D2-dopamine, and alpha 2B-adrenergic receptors for inhibiting the Na-H exchanger, NHE1. J Biol Chem 2003; 278(17): 15128-35. Bacic D, Kaissling B, McLeroy P, et al. Dopamine acutely decreases apical membrane Na/H exchanger NHE3 protein in mouse renal proximal tubule. Kidney Int 2003; 64(6): 2133-41. Pedrosa R, Gomes P, Hopfer U, et al. Gialpha3 protein-coupled dopamine D3 receptor-mediated inhibition of renal NHE3 activity in SHR proximal tubular cells is a PLC-PKC-mediated event. Am J Physiol Renal Physiol 2004; 287(5): F1059-66. Kocinsky HS, Girardi AC, Biemesderfer D, et al. Use of phosphospecific antibodies to determine the phosphorylation of endogenous Na+/H+ exchanger NHE3 at PKA consensus sites. Am J Physiol Renal Physiol 2005; 289(2): F249-58. Albrecht FE, Xu J, Moe OW, et al. Regulation of NHE3 activity by G protein subunits in renal brush-border membranes. Am J Physiol Regul Integr Comp Physiol 2000; 278(4): R1064-73. Chen Z, Leibiger I, Katz AI, et al. Pals-associated tight junction protein functionally links dopamine and angiotensin II to the regulation of sodium transport in renal epithelial cells. Br J Pharmacol 2009;158(2): 86-93. Cinelli AR, Efendiev R, Pedemonte CH. Trafficking of Na-KATPase and dopamine receptor molecules induced by changes in intracellular sodium concentration of renal epithelial cells. Am J Physiol Renal Physiol 2008; 295(4): F1117-25. Gildea JJ, Israel JA, Johnson AK, et al. Caveolin-1 and dopaminemediated internalization of NaKATPase in human renal proximal tubule cells. Hypertension 2009; 54(5): 1070-6. Khundmiri SJ, Lederer E. PTH and DA regulate Na-K ATPase through divergent pathways. Am J Physiol Renal Physiol 2002; 282(3): F512-22. Efendiev R, Chen Z, Krmar RT, et al. The 14-3-3 protein translates the NA+,K+-ATPase {alpha}1-subunit phosphorylation signal into binding and activation of phosphoinositide 3-kinase during endocytosis. J Biol Chem 2005; 280(16):16272-7. Gomes P, Soares-da-Silva P. Dopamine-induced inhibition of Na+K+-ATPase activity requires integrity of actin cytoskeleton in opossum kidney cells. Acta Physiol Scand 2002; 175(2): 93-101. Lucas-Teixeira VA, Hussain T, Serro P, et al. Intestinal dopaminergic activity in obese and lean Zucker rats: response to high salt intake. Clin Exp Hypertens 2002;24(5):383-96. Khan F, Spicarov Z, Zelenin S, et al. Negative reciprocity between angiotensin II type 1 and dopamine D1 receptors in rat renal proximal tubule cells. Am J Physiol Renal Physiol 2008; 295(4): F1110-6. Brismar H, Asghar M, Carey RM, et al. Dopamine-induced recruitment of dopamine D1 receptors to the plasma membrane. Proc Natl Acad Sci U S A 1998; 95(10): 5573-8. Asghar M, Kansra V, Hussain T, et al. Hyperphosphorylation of Na-pump contributes to defective renal dopamine response in old rats. J Am Soc Nephrol 2001; 12(2): 226-32. Pedemonte CH, Efendiev R, Bertorello AM. Inhibition of Na,KATPase by dopamine in proximal tubule epithelial cells. Semin Nephrol 2005; 25(5): 322-7.
[58] [59]
[84]
[85]
[60] [61]
[86]
[62] [63]
[87]
[88]
[64] [65]
[89] [90]
[66] [67]
[91]
[68] [69] [70] [71]
[92]
[93]
[94]
[72] [73] [74]
[95] [96]
[75] [76] [77]
[97]
[98] [99]
[78]
[100]
[79] [80]
[101] [102]
[81] [82]
[103]
Roles of Renal Proximal Tubule Transport in the Pathogenesis [104] Yao LP, Li XX, Yu PY, et al. Dopamine D1 receptor and protein kinase C isoforms in spontaneously hypertensive rats. Hypertension 1998; 32(6): 1049-53. Satoh T, Ominato M, Katz AI. Different mechanisms of renal NaK-ATPase regulation by dopamine in the proximal and distal nephron. Hypertens Res 1995; 18(1): S137-40. Bertorello AM, Sznajder JI. The dopamine paradox in lung and kidney epithelia: sharing the same target but operating different signaling networks. Am J Respir Cell Mol Biol 2005; 33(5): 432-7. Cunningham R, Biswas R, Brazie M, et al. Signaling pathways utilized by PTH and dopamine to inhibit phosphate transport in mouse renal proximal tubule cells. Am J Physiol Renal Physiol 2009; 296(2): F355-61. Baines AD, Drangova R. Does dopamine use several signal pathways to inhibit Na-Pi transport in OK cells? J Am Soc Nephrol 1998; 9(9): 1604-12. Glahn RP, Onsgard MJ, Tyce GM, et al. Autocrine/paracrine regulation of renal Na(+)-phosphate cotransport by dopamine. Am J Physiol 1993; 264(4 Pt 2): F618-22. Ba J, Brown D, Friedman PA. Calcium-sensing receptor regulation of PTH-inhibitable proximal tubule phosphate transport. Am J Physiol Renal Physiol 2003; 285(6): F1233-43. Jin Y, Kuznetsova T, Tikhonoff V, et al. Segmental renal sodium handling in relation to the human SAH gene. Hypertension 2008; 52(2): e12-3. Saito O, Ando Y, Kusano E, et al. Functional characterization of basolateral and luminal dopamine receptors in rabbit CCD. Am J Physiol Renal Physiol 2001; 281(1): F114-22. Sun D, Schafer JA. Dopamine inhibits AVP-dependent Na+ transport and water permeability in rat CCD via a D4-like receptor. Am J Physiol 1996;271(2 Pt 2): F391-400. Aoki Y, Albrecht FE, Bergman KR, et al. Stimulation of Na(+)K(+)-2Cl- cotransport in rat medullary thick ascending limb by dopamine. Am J Physiol 1996; 271(6 Pt 2): R1561-7. Kaneda Y, Bello-Reuss E. Effect of dopamine on phosphate reabsorption in isolated perfused rabbit proximal tubules. Miner Electrolyte Metab 1983; 9(3): 147-50. Bello-Reuss E, Higashi Y, Kaneda Y. Dopamine decreases fluid reabsorption in straight portions of rabbit proximal tubule. Am J Physiol 1982; 242(6): F634-40. Baum M, Quigley R. Inhibition of proximal convoluted tubule transport by dopamine. Kidney Int 1998; 54(5): 1593-600. Kinoshita S, Sidhu A, Felder RA. Defective dopamine-1 receptor adenylate cyclase coupling in the proximal convoluted tubule from the spontaneously hypertensive rat. J Clin Invest 1989; 84(6): 1849-56. Sanada H, Jose PA, Hazen-Martin D, et al. Dopamine-1 receptor coupling defect in renal proximal tubule cells in hypertension. Hypertension 1999; 33(4): 1036-42. Jose PA, Felder RA. What we can learn from the selective manipulation of dopaminergic receptors about the pathogenesis and treatment of hypertension? Curr Opin Nephrol Hypertens 1996; 5(5): 447-51. Li D, Scott L, Crambert S, et al. Binding of losartan to angiotensin AT1 receptors increases dopamine D1 receptor activation. J Am Soc Nephrol 2012; 23(3): 421-8. Felder RA, Sanada H, Xu J, et al. G protein-coupled receptor kinase 4 gene variants in human essential hypertension. Proc Natl Acad Sci U S A 2002; 99(6): 3872-7. Watanabe H, Xu J, Bengra C, et al. Desensitization of human renal D1 dopamine receptors by G protein-coupled receptor kinase 4. Kidney Int 2002; 62(3): 790-8. Zeng C, Villar VA, Eisner GM, et al. G protein-coupled receptor kinase 4: role in blood pressure regulation. Hypertension 2008; 51(6): 1449-55. Premont RT, Macrae AD, Aparicio SA, et al. The GRK4 subfamily of G protein-coupled receptor kinases. Alternative splicing, gene
Current Hypertension Reviews, 2013, Vol. 9, No. 2
155
[126]
[105] [106]
[127] [128]
[107]
[129]
[108] [109]
[130]
[110] [111]
[131] [132]
[112] [113]
[133]
[134]
[114] [115]
[135] [136]
[116] [117] [118]
[137]
[138] [139]
[119]
[120]
[140]
[121] [122]
[141]
[142] [143]
[123] [124]
[144]
[125]
organization, and sequence conservation. J Biol Chem 1999; 274(41): 29381-9. Premont RT, Macrae AD, Stoffel RH, et al. Characterization of the G protein-coupled receptor kinase GRK4. Identification of four splice variants. J Biol Chem 1996; 271(11): 6403-10. Sanada H, Yatabe J, Midorikawa S, et al. Amelioration of genetic hypertension by suppression of renal G protein-coupled receptor kinase type 4 expression. Hypertension 2006; 47(6): 1131-9. Virlon B, Firsov D, Cheval L, et al. Rat G protein-coupled receptor kinase GRK4: identification, functional expression, and differential tissue distribution of two splice variants. Endocrinology 1998; 139(6): 2784-95. Sallese M, Mariggi S, Collodel G, et al. G protein-coupled receptor kinase GRK4. Molecular analysis of the four isoforms and ultrastructural localization in spermatozoa and germinal cells. J Biol Chem 1997; 272(15): 10188-95. Rankin ML, Marinec PS, Cabrera DM, et al. The D1 dopamine receptor is constitutively phosphorylated by G protein-coupled receptor kinase 4. Mol Pharmacol 2006; 69(3): 759-69. Tiberi M, Nash SR, Bertrand L, et al. Differential regulation of dopamine D1A receptor responsiveness by various G proteincoupled receptor kinases. J Biol Chem 1996; 271(7): 3771-8. Villar VA, Jones JE, Armando I, et al. G protein-coupled receptor kinase 4 (GRK4) regulates the phosphorylation and function of the dopamine D3 receptor. J Biol Chem 2009; 284(32): 21425-34. Mnard L, Ferguson SS, Barak LS, et al. Members of the G protein-coupled receptor kinase family that phosphorylate the beta2-adrenergic receptor facilitate sequestration. Biochemistry 1996; 35(13): 4155-60. Munshi UM, Peegel H, Menon KM. Palmitoylation of the luteinizing hormone/human chorionic gonadotropin receptor regulates receptor interaction with the arrestin-mediated internalization pathway. Eur J Biochem 2001; 268(6): 1631-9. Chen W, Li S, Srinivasan SR, et al. Autosomal genome scan for loci linked to blood pressure levels and trends since childhood: the Bogalusa Heart Study. Hypertension 2005; 45(5): 954-9. Allayee H, de Bruin TW, Michelle Dominguez K, et al. Genome scan for blood pressure in Dutch dyslipidemic families reveals linkage to a locus on chromosome 4p. Hypertension 2001; 38(4): 773-8. Zhu H, Lu Y, Wang X, et al. The G protein-coupled receptor kinase 4 gene affects blood pressure in young normotensive twins. Am J Hypertens 2006; 19(1): 61-6. Rana BK, Insel PA, Payne SH, et al. Population-based sample reveals gene-gender interactions in blood pressure in White Americans. Hypertension 2007; 49(1): 96-106. Staessen JA, Kuznetsova T, Zhang H, et al. Blood pressure and renal sodium handling in relation to genetic variation in the DRD1 promoter and GRK4. Hypertension 2008; 51(6): 1643-50. Bertorello A, Hkfelt T, Goldstein M, et al. Proximal tubule Na+-K+-ATPase activity is inhibited during high-salt diet: evidence for DA-mediated effect. Am J Physiol 1988; 254(6 Pt 2): F795-801. Adam WR, Culvenor AJ, Hall J, et al. Aromatic L-amino acid decarboxylase: histochemical localization in rat kidney and lack of effect of dietary potassium or sodium loading on enzyme distribution. Clin Exp Pharmacol Physiol 1986; 13(1): 47-53. Hayashi M, Yamaji Y, Kitajima W, et al. Aromatic L-amino acid decarboxylase activity along the rat nephron. Am J Physiol 1990; 258(1 Pt 2): F28-33. Zhang MZ, Yao B, Wang S, et al. Intrarenal dopamine deficiency leads to hypertension and decreased longevity in mice. J Clin Invest 2011; 121(7): 2845-54. Benigni A, Corna D, Zoja C, et al. Disruption of the Ang II type 1 receptor promotes longevity in mice. J Clin Invest 2009; 119(3): 524-30.
Received: March 07, 2012
Revised: June 07, 2013
Accepted: June 12, 2013
Você também pode gostar
- Li 2011-smDocumento14 páginasLi 2011-smCLPHtheoryAinda não há avaliações
- RAS Role in Chronic Inflammation and AtherosclerosisDocumento11 páginasRAS Role in Chronic Inflammation and AtherosclerosisSukma EffendyAinda não há avaliações
- Mattias Carlström, Christopher S. Wilcox and William J. WelchDocumento7 páginasMattias Carlström, Christopher S. Wilcox and William J. WelchJulienne InostrozaAinda não há avaliações
- Endotelin and Renal IonDocumento15 páginasEndotelin and Renal IonSelly Cintya GusmanAinda não há avaliações
- Role of Thioredoxin-Interacting Protein in Mediating Endothelial Dysfunction in HypertensionDocumento13 páginasRole of Thioredoxin-Interacting Protein in Mediating Endothelial Dysfunction in HypertensionLeidy LambertinezAinda não há avaliações
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocumento25 páginasWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsManuel FierroAinda não há avaliações
- Ajprenal 00351 2005 PDFDocumento8 páginasAjprenal 00351 2005 PDFGauravAinda não há avaliações
- Ajprenal 00351 2005 PDFDocumento8 páginasAjprenal 00351 2005 PDFGauravAinda não há avaliações
- Interaction of Central Angiotensin II and Aldosterone On Sodium Intake and Blood PressureDocumento24 páginasInteraction of Central Angiotensin II and Aldosterone On Sodium Intake and Blood PressureJesus CastroAinda não há avaliações
- (2010) Tubular Reabsortion and Diabetes-Induced Glomerular FiltrationDocumento13 páginas(2010) Tubular Reabsortion and Diabetes-Induced Glomerular FiltrationEnrique MartinezAinda não há avaliações
- ANT 2 S20.fullDocumento13 páginasANT 2 S20.fulllguerreroAinda não há avaliações
- HipertensiuneDocumento9 páginasHipertensiuneCosmin CalanciaAinda não há avaliações
- Vaccine For Hypertension: Modulating The Renin - Angiotensin SystemDocumento9 páginasVaccine For Hypertension: Modulating The Renin - Angiotensin SystemRameshKrishnanAinda não há avaliações
- Ishikane 2018Documento51 páginasIshikane 2018yalocim666Ainda não há avaliações
- Larussa 2017Documento25 páginasLarussa 2017alan.rangel.puenteAinda não há avaliações
- tmpB355 TMPDocumento3 páginastmpB355 TMPFrontiersAinda não há avaliações
- Nitro-Oleic Acid Inhibits Angiotensin II-Induced HypertensionDocumento29 páginasNitro-Oleic Acid Inhibits Angiotensin II-Induced HypertensionKadek SuprajayaAinda não há avaliações
- Assessment and Treatment of Endothelial Dysfunction - 1999Documento10 páginasAssessment and Treatment of Endothelial Dysfunction - 1999Maria TraianAinda não há avaliações
- The Vasoactive Mas Receptor in Essential Hypertension: Clinical MedicineDocumento12 páginasThe Vasoactive Mas Receptor in Essential Hypertension: Clinical MedicineHesbon MomanyiAinda não há avaliações
- Review Article: Animal Models of Hypertension: An OverviewDocumento14 páginasReview Article: Animal Models of Hypertension: An OverviewrodrigodaliascienceAinda não há avaliações
- Effects of Alcohol On Intracellular PH Regulators and Electromechanical Parameters in Human MyocardiumDocumento9 páginasEffects of Alcohol On Intracellular PH Regulators and Electromechanical Parameters in Human MyocardiumAchmad LatiefAinda não há avaliações
- AT1 ReceptorDocumento6 páginasAT1 ReceptorTâm Nguyễn HữuAinda não há avaliações
- Circulation-2002-Cardiovascular Influences of A1b-Adrenergic Receptor Defect in MiceDocumento9 páginasCirculation-2002-Cardiovascular Influences of A1b-Adrenergic Receptor Defect in Miceyylf2016Ainda não há avaliações
- Calcio en La Secrecion de ReninaDocumento12 páginasCalcio en La Secrecion de ReninaJulisa Lipa CristobalAinda não há avaliações
- Angiotensin II Type 2 Receptor Deficiency Aggravates Renal Injury and Reduces Survival in Chronic Kidney Disease in MiceDocumento11 páginasAngiotensin II Type 2 Receptor Deficiency Aggravates Renal Injury and Reduces Survival in Chronic Kidney Disease in MicenovrodAinda não há avaliações
- AT R-At R Cross Talk: Cross Regulation of Angiotensin Ii Type 1 Receptor and The Angiotensin Ii Type 2 ReceptorDocumento5 páginasAT R-At R Cross Talk: Cross Regulation of Angiotensin Ii Type 1 Receptor and The Angiotensin Ii Type 2 ReceptorIrina Luciana DumitriuAinda não há avaliações
- Renal Blood Flow and OxygenationDocumento12 páginasRenal Blood Flow and OxygenationnanreAinda não há avaliações
- Pages 9 20Documento12 páginasPages 9 20Clyde R.OrtegaAinda não há avaliações
- Shishido 2006Documento8 páginasShishido 2006kevin gelaudeAinda não há avaliações
- Renin-Angiotensin System: I: (The Juxtaglomerular Apparatus)Documento1 páginaRenin-Angiotensin System: I: (The Juxtaglomerular Apparatus)reioctabianoAinda não há avaliações
- AT2 Receptor AgonistsDocumento5 páginasAT2 Receptor Agonistsfer123wizAinda não há avaliações
- CC 12031Documento200 páginasCC 12031Arti Tyagita KusumawardhaniAinda não há avaliações
- Angiotensin II, Via AT and AT Receptors and NF-Pathway, Regulates The Inflammatory Response in Unilateral Ureteral ObstructionDocumento16 páginasAngiotensin II, Via AT and AT Receptors and NF-Pathway, Regulates The Inflammatory Response in Unilateral Ureteral Obstructionarmash mominAinda não há avaliações
- Inhibition of Prostaglandin Synthesis During Polystyrenemicrosphere-Induced Pulmonary Embolism in The RatDocumento10 páginasInhibition of Prostaglandin Synthesis During Polystyrenemicrosphere-Induced Pulmonary Embolism in The RatshintaAinda não há avaliações
- Jurnal 33 PDFDocumento16 páginasJurnal 33 PDFshabrina ardeliaAinda não há avaliações
- Urea and Ammonia Metabolism and The Control of Renal Nitrogen ExcretionDocumento15 páginasUrea and Ammonia Metabolism and The Control of Renal Nitrogen ExcretionJames Cojab SacalAinda não há avaliações
- Interactions Between Thromboxane A2, Thromboxane/prostaglandin (TP) Receptors, and Endothelium-Derived HyperpolarizationDocumento9 páginasInteractions Between Thromboxane A2, Thromboxane/prostaglandin (TP) Receptors, and Endothelium-Derived HyperpolarizationMarco Antonio Garcia GonzalezAinda não há avaliações
- Salt Sensitivity of Blood Pressure in NKCC1-deficient MiceDocumento9 páginasSalt Sensitivity of Blood Pressure in NKCC1-deficient MiceHongyu LiAinda não há avaliações
- Protective Effect of 3-N-Butylphthalide Against Hypertensive Nephropathy in Spontaneously Hypertensive RatsDocumento19 páginasProtective Effect of 3-N-Butylphthalide Against Hypertensive Nephropathy in Spontaneously Hypertensive Ratsberliana syifaAinda não há avaliações
- Gastric distension causes peripheral vasoconstriction in anaesthetized pigsDocumento12 páginasGastric distension causes peripheral vasoconstriction in anaesthetized pigsHimanshu SharmaAinda não há avaliações
- 2012 Carnevale D. PI3K in Hypertension A Novel Therapeutic Target Controlling Vascular Myogenic Tone and Target Organ DamageDocumento6 páginas2012 Carnevale D. PI3K in Hypertension A Novel Therapeutic Target Controlling Vascular Myogenic Tone and Target Organ DamageAndi Suchy Qumala SarieAinda não há avaliações
- Renal Reflections: Exploring the Marvels of Nephrology: The Intricate Ballet of Kidney Functions UnveiledNo EverandRenal Reflections: Exploring the Marvels of Nephrology: The Intricate Ballet of Kidney Functions UnveiledAinda não há avaliações
- COX-2 Selectivity Alone Does Not de Ne The Cardiovascularrisks Associated With Non-Steroidal Anti-In Ammatory DrugsDocumento4 páginasCOX-2 Selectivity Alone Does Not de Ne The Cardiovascularrisks Associated With Non-Steroidal Anti-In Ammatory DrugsruleshellzAinda não há avaliações
- Interaction of TNF With Angiotensin II ContributesDocumento12 páginasInteraction of TNF With Angiotensin II ContributesMuôngAinda não há avaliações
- Inside Vitro Examination Along With Biodistribution Research Regarding HAdagrasib Copolymers Individuals Gastrin Issuing Peptide Receptor Inside Prostate Type of CancerqianiDocumento2 páginasInside Vitro Examination Along With Biodistribution Research Regarding HAdagrasib Copolymers Individuals Gastrin Issuing Peptide Receptor Inside Prostate Type of Cancerqianibottledoor0Ainda não há avaliações
- Jurnal DispanDocumento19 páginasJurnal Dispanrahmani kadarningsihAinda não há avaliações
- Devil and Angel in The Renin-Angiotensin System ACE-angiotensin II-AT1 Receptor Axis vs. ACE2-angiotensin - (1-7) - Mas Receptor AxisDocumento4 páginasDevil and Angel in The Renin-Angiotensin System ACE-angiotensin II-AT1 Receptor Axis vs. ACE2-angiotensin - (1-7) - Mas Receptor AxisLevente BalázsAinda não há avaliações
- ScienceDocumento8 páginasScienceDaniela Fantini ValeAinda não há avaliações
- Use of Inotropes and Vasopressor Agents in Critically Ill PatientsDocumento19 páginasUse of Inotropes and Vasopressor Agents in Critically Ill PatientsLong LeAinda não há avaliações
- Pharmaceuticals 03 01286Documento10 páginasPharmaceuticals 03 01286aAinda não há avaliações
- Joe 123Documento19 páginasJoe 123mohammed fayedAinda não há avaliações
- Junral 1999Documento4 páginasJunral 1999Aji Muhammad IqbalAinda não há avaliações
- Toxicology and Applied Pharmacology: Séin O'Connell, Craig Slattery, Michael P. Ryan, Tara McmorrowDocumento10 páginasToxicology and Applied Pharmacology: Séin O'Connell, Craig Slattery, Michael P. Ryan, Tara McmorrowDoyin AwodeleAinda não há avaliações
- Calcium Signaling in Health, Disease and TherapyDocumento9 páginasCalcium Signaling in Health, Disease and TherapyLeonel LedezmaAinda não há avaliações
- Endothelin, Kidney Disease, and HypertensionDocumento5 páginasEndothelin, Kidney Disease, and HypertensionRizki Cah KeratonAinda não há avaliações
- Intermittent Hypoxia-Activated Cyclooxygenase Pathway: Role in AtherosclerosisDocumento10 páginasIntermittent Hypoxia-Activated Cyclooxygenase Pathway: Role in AtherosclerosisaditAinda não há avaliações
- Review Article: The Mechanism of Acupuncture in Treating Essential Hypertension: A Narrative ReviewDocumento10 páginasReview Article: The Mechanism of Acupuncture in Treating Essential Hypertension: A Narrative ReviewpedroAinda não há avaliações
- HR 2008203Documento6 páginasHR 200820322125327Ainda não há avaliações
- Articolo 21Documento32 páginasArticolo 21Francesca BertaccaAinda não há avaliações
- Cross TalkDocumento12 páginasCross TalkWrasasena SuryatmajaAinda não há avaliações
- Queen LongevityDocumento9 páginasQueen Longevityfabiandionisio100% (1)
- Pathomorphology Final ExamDocumento262 páginasPathomorphology Final ExamMann SarwanAinda não há avaliações
- ABO Incompatibility in NewbornsDocumento4 páginasABO Incompatibility in NewbornsNollen LaquianAinda não há avaliações
- Circulatory System Peer Assessment: Examiner's NotesDocumento4 páginasCirculatory System Peer Assessment: Examiner's NotespkrajenpillaygmailcomAinda não há avaliações
- Charnley Ankle ArthrodesisDocumento12 páginasCharnley Ankle Arthrodesisdr_s_ganeshAinda não há avaliações
- IsopreneDocumento5 páginasIsopreneArdynaApriSapoetriAinda não há avaliações
- Psychology: Motivation and EmotionDocumento45 páginasPsychology: Motivation and EmotionAisyah AzmiAinda não há avaliações
- CBSE 2019 Biomolecules Project ReportDocumento15 páginasCBSE 2019 Biomolecules Project ReportRavindra JangidAinda não há avaliações
- Cormie2011 PDFDocumento22 páginasCormie2011 PDFGust AvoAinda não há avaliações
- Apgar ScoreDocumento11 páginasApgar Scorefaizura100% (1)
- Chapter 013Documento4 páginasChapter 013Nusa Koj100% (1)
- Animals Have Basic NeedsDocumento24 páginasAnimals Have Basic NeedsNarendran SubramaniamAinda não há avaliações
- Organs in The Body Quadrants and RegionsDocumento3 páginasOrgans in The Body Quadrants and RegionsDavid HosamAinda não há avaliações
- Biological Oxidation: Dr. Dalia ShaalanDocumento24 páginasBiological Oxidation: Dr. Dalia ShaalanALIYU AYUBA FUSAMIAinda não há avaliações
- Structures of Amino AcidsDocumento32 páginasStructures of Amino AcidsUsman GhaniAinda não há avaliações
- Broncho DilatorsDocumento53 páginasBroncho DilatorsDocRNAinda não há avaliações
- Aerobic Respiration: Chemiosmosis and Electron Transport ChainDocumento17 páginasAerobic Respiration: Chemiosmosis and Electron Transport ChainAihk kenneth BaronaAinda não há avaliações
- Lab ValuesDocumento3 páginasLab Valuessurviving nursing schoolAinda não há avaliações
- Jeffrey SatinoverDocumento7 páginasJeffrey SatinoverlooiiiiisAinda não há avaliações
- Cranial NervesDocumento118 páginasCranial NervesGan'sAinda não há avaliações
- DR - BD S Step 1 Guide - PDF Filename UTF-8 DR - BD S Step 1 GuideDocumento24 páginasDR - BD S Step 1 Guide - PDF Filename UTF-8 DR - BD S Step 1 GuideAdeelMunawarAinda não há avaliações
- Unit I Clothing Science Two Marks With Answer and Question BankDocumento3 páginasUnit I Clothing Science Two Marks With Answer and Question BankSivakumar KAinda não há avaliações
- Induced Lactation ANR SlidesDocumento11 páginasInduced Lactation ANR Slidesjohn cageAinda não há avaliações
- Infectiile de tract urinar: cazuri cliniceDocumento55 páginasInfectiile de tract urinar: cazuri cliniceMădălina Mihaela LuchianAinda não há avaliações
- LP Surgery ChestDocumento6 páginasLP Surgery Chestangelmd83Ainda não há avaliações
- Revision Sheet Grade 5 For Ut1Documento5 páginasRevision Sheet Grade 5 For Ut1Sudeep BhattacharyaAinda não há avaliações
- Patrick Ch19 p2Documento31 páginasPatrick Ch19 p2NizarAliAinda não há avaliações
- Biology 12 HSC NotesDocumento195 páginasBiology 12 HSC NotesShitalPatilAinda não há avaliações
- Mash MethodDocumento28 páginasMash MethodShuvajoyyy100% (5)
- g12 Bone Grafts Subs JTG Rev 10 17 10Documento57 páginasg12 Bone Grafts Subs JTG Rev 10 17 10Tudor RalucaAinda não há avaliações