Escolar Documentos
Profissional Documentos
Cultura Documentos
6096 Sroisiri
Enviado por
sanjay6969Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
6096 Sroisiri
Enviado por
sanjay6969Direitos autorais:
Formatos disponíveis
Asia Journal of Public Health, May August 2011
Vol.2 No. 2
Asia Journal of Public Health
Journal homepage:http://www.ASIAPH.org Original Articles
Effect of Oil-Pulling on Oral Microorganisms in Biofilm Models
Sroisiri Thaweboon * Jurai Nakaparksin ** Boonyanit Thaweboon*
*Department of Oral Microbiology, Faculty of Dentistry, Mahidol University, Bangkok, Thailand ** Department of Prosthodontics, Faculty of Dentistry, Mahidol University, Bangkok, Thailand
ARTICLE INFO
Article history : Received December 2010 Received in revised form June 2010 Accepted July 2011 Available online August 2011 Keywords: Oil-pulling Oral microorganisms Biofilm
ABSTRACT
Objective: To investigate the effect of oil-pulling against oral microorganisms in biofilm models. Materials and Methods: The effect of oil-pulling using coconut oil, corn oil, rice bran oil, palm oil, sesame oil, sunflower oil and soy bean oil was evaluated on biofilm models formed by Streptococcus mutans KPSK2, Lactobacillus casei ATCC 6363 and Candida albicans ATCC 13803 on salivary-coated microtiter plates. Saline solution and 0.2% chlorhexidine gluconate solution were used as negative and positive controls, respectively. Results: It was found that coconut oil exhibited antimicrobial activity against S. mutans and C. albicans. Sesame oil had antibacterial activity against S. mutans whereas sunflower oil had antifungal activity against C. albicans. However, L. casei was found to be resistant to all tested oils. Conclusion: Results from the present study could be scientific evidence to demonstrate that oil-pulling therapy with some edible oils could probably be used as a preventive home therapy to maintain oral hygiene against dental caries especially in developing countries.
Corresponding Author: Thaweboon S, Department of Oral Microbiology, Faculty of Dentistry, Mahidol University, 6 Yothi Road, Rajthewee, Bangkok 10400, Thailand. Email : dtstw@mahidol.ac.th
Asia J Public Health 2011; 2(2): 62-66
INTRODUCTION Dental caries are an infection associated with microorganisms embedded in a matrix of polymers of bacterial and salivary origin. The occurrence of dental caries is directly linked to the ability of microorganisms to colonize the tooth surface and form biofilm or dental plaque. Formation of biofilm begins with the attachment of free-floating microorganisms to a surface. These first colonists facilitate the arrival of others by providing adhesion sites and the matrix that holds the biofilm together. Streptococcus mutans, Lactobacilli spp. and
Candida albicans are the predominant microorganisms found in dental plaque associated with a caries lesion1. Streptococcus mutans, Lactobacilli spp. are considered crucial for the initiation and progression of dental caries as they have shown by their more acidogenic and acidophilic properties than those of other oral bacteria 2. They can convert dietary carbohydrates into acid, which lowers the pH of the environment, and solubilizes the calcium phosphate of the enamel to produce a caries lesion. Conditions of low pH created by these bacteria shift the balance of plaque
62
Asia Journal of Public Health, May August 2011
Vol.2 No. 2
microflora and favor the proliferation of Candida spp. Oil-pulling or oil-swishing is a procedure in which the practitioners swish or rinse oil in their mouth for oral health benefit to prevent dental caries, oral malodor, bleeding gums, dryness of the throat and cracked lips 3. In addition, this simple method is claimed to cure many diseases ranging from thrombosis, eczema, intestinal infection, and diabetes, to bronchitis and asthma 3. This procedure is typically performed daily by sipping or sucking oil and pulling it between the teeth for 1-10 min before brushing. The oil will turn thin and milky white. This should be followed by brushing the teeth and is preferably done on an empty stomach in the morning. Scientific evidence shows that oil-pulling therapy could reduce the plaque index, modify gingival scores and the total oral bacteria count in gingivitis patients 4-5 . Moreover, it can convert caries susceptibility from marked susceptibility to slight or moderate susceptibility 6. Therefore, the aim of the present study was to investigate the effect of oil-pulling against oral microorganisms in biofilm models. MATERIALS AND METHODS Oil All of the oils used in the present study were Thai products. They included: coconut oil (Grandmom Herbal House), corn oil (Thai Vegetable Oil Public Company), rice bran oil (Thai Edible Oil Company), palm oil (Thai Vegetable Oil Public Company), sesame oil (Grandmom Herbal House), sunflower oil (Thanakorn Vegetable Oil), and soy bean oil (Thai Vegetable Oil Public Company). Microorganisms The tested microorganisms were obtained from the culture collections of the Department of Microbiology, Faculty of Dentistry, Mahidol University, Thailand. Organisms were as follows: Streptococcus mutans KPSK2, Lactobacillus casei ATCC 6363 and Candida albicans ATCC 13803. They were maintained on Brain Heart Infusion (BHI) agar (BBL, USA). Overnight cultures were prepared by inoculating approximately 2 ml of Mueller Hinton broth (Difco, USA) with 2-3 colonies of each organism taken from BHI agar. The broth was incubated overnight at 37 C. Inocula were prepared by diluting overnight cultures with saline to
approximately 108 CFU/ml for bacteria and 107 CFU/ml for yeast. These suspensions were further used for antimicrobial determination. Effect on biofilm models The effect of the oils was evaluated on biofilm models formed by S. mutans KPSK2, L. casei ATCC 6363 and C. albicans ATCC 13803 on the bottom of microtiter plates. Biofilm assays were done using the protocol modified from Loo et al 7 and Guggenheim et al8. Briefly, all microorganisms were cultivated in a fluid thioglycolate medium (Difco, USA) supplemented with 0.3% glucose for seven hours. Each microbial suspension (106 CFU/ml) was combined and placed at cold temperature for six hours. Approximately 60 ml of unstimulated saliva were collected from three volunteers two hours after eating, drinking or having a hygiene procedure. The pooled saliva was centrifuged at 20,000 g for thirty minutes at 4C. The supernatant was filtered through a 0.45 mpore membrane (Sartorius, Germany). Absence of any viable microorganisms in the saliva was checked by culturing on blood agar. Salivary components were absorbed onto ninety-six polystyrene, flat-bottomed well microtiter plates for four hours at room temperature to form an acquired pellicle. After removal of excess saliva, the coated microtiter plates were inoculated with a mixture of saliva, thioglycolate medium supplemented with 3% glucose, and a pool of microorganisms. The final density of inoculum in each well of the microtiter plate was 105 CFU/ml. The microtiter plates were then incubated at 37C for twenty-four hours under anaerobic conditions. Saline solution and a 0.2% chlorhexidine gluconate solution were used as negative and positive controls, respectively. The biofilms were exposed to controls or the tested oils for 1 min. During this time the fluid was pulled up and down 20 times. Then the oils and unattached cells were removed and the biofilms were washed three times in PBS, and then scrapped and sonicated. Serial dilutions of sonicated cells were cultivated in MitisSalivarius Bacitracin agar (Difco, USA), Rogosa SL agar (Difco, USA) and Sabouraud dextrose agar (Difco, USA) to determine the number of S. mutans, L. casei and C. albicans, respectively.
63
Asia Journal of Public Health, May August 2011
Vol.2 No. 2
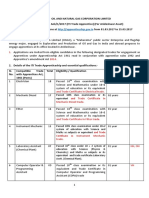
Statistical analysis All experiments were performed in triplicate and results were expressed as mean + standard deviation. Statistical analysis of the differences between mean values obtained for the experimental groups were analyzed by one-way analysis of variance, followed by Tukeys test using SPSS 11.5 software. A pvalue less than 0.05 was taken as statistically significant. RESULTS Multi-species biofilm of S. mutans, L. casei and C. albicans were prepared and then exposed to the tested oils for 1 min. Responses of the microbial populations in biofilm models to different oils are summarized in Table 1. Coconut oil exhibited antimicrobial activity against S. mutans (2.5 log reductions) and C. albicans (1 log reduction). Sesame oil had antibacterial activity against S. mutans (1 log reduction) and sunflower oil had antifungal activity against C. albicans (1 log reduction). For chlorhexidine, which was used as a positive control, S. mutans was completely removed from the biofilm and 1.5 log reductions of C. albicans were observed. L. casei was found to be resistant to all tested oils, whereas three log reductions were shown after chlorhexidine exposure
DISCUSSION Oil-pulling therapy with sesame oil or sunflower oil has been extensively used as a traditional Indian folk remedy for many years. It is claimed to have advantages over commercial mouthwashes since it causes no staining, has no lingering after taste, causes no allergic reactions and is readily available in the household 5. The mechanisms of oil-pulling action are not known. It has been proposed, however, that the viscosity of the oil can inhibit bacterial adhesion and plaque coaggregation6. The other possible mechanism might be the saponification process that occurs as a result of alkali hydrolysis of oil by bicarbonates in saliva 9. These soaps are good cleansing agents and might be effective in removing microorganisms or plaque materials. Sufficient scientific research has not been carried out to evaluate the beneficial effect of oil pulling therapy on oral health and this needs to be addressed. This study was therefore planned to investigate the effect of oil-pulling with several edible oils on oral microorganisms related to dental caries using biofilm models.
Table1 Effect of oil-pulling on oral microorganisms in biofilm models
S. mutans p-value 2.59+0.13 0.008* 5.05+0.17 0.596 4.91+0.12 0.631 5.15+0.06 0.940 4.01+0.14 0.039* 5.13+0.13 0.805 4.79+0.24 0.568 5.11+0.13 0 L. casei 5.44+0.16 5.61+0.14 5.52+0.06 5.67+0.21 5.58+0.13 5.06+0.12 5.56+0.05 5.42+0.21 2.27+0.10 p-value 0.950 0.734 0.702 0.598 0.821 0.405 0.840 C. albicans p-value 2.03+0.12* 0.022* 3.27+0.10 0.772 3.34+0.14 0.853 3.11+0.08 0.750 3.50+0.13 0.387 1.95+0.19 0.014* 3.31+0.20 0.826 3.30+0.14 1.84+0.08
coconut oil corn oil palm oil rice bran oil sesame oil sunflower oil soy bean oil saline solution chlorhexidine
Data presented as mean log10 CFU/ml of microorganisms * significantly different from saline solution, negative control chlorhexidine was used as positive control
In the present study it was found that coconut oil exhibited antimicrobial activity against S. mutans and C. albicans whereas sesame oil had activity against S. mutans and sunflower oil showed only antifungal activity. Other oils such as corn oil, palm oil, rice bran oil and soy bean oil showed no antimicrobial activity against tested microorganisms.
Coconut oil has a unique role in the diet as an important physically functional food. Besides the health and nutritional benefits, coconut oil has been shown to have anticarcinogenic effects against colon tumors 10. What makes coconut oil different from most other dietary oils are the basic building blocks, or fatty acids, making up the oil. The predominant composition of coconut oil is a
64
Asia Journal of Public Health, May August 2011
Vol.2 No. 2
medium chain fatty acid, whereas the majority of common edible fats in our diet are composed almost entirely of long chain fatty acids. This influences the physical and chemical properties of the oil. Coconut oil contains 92% saturated acids, approximately 50% of which is lauric acid 11. Recognition of the antimicrobial activity of coconut oil has been reported since 1982 by Hierholzer and Kabara 12. This early research was directed at the virucidal effects because of possible problems related to food preservation. Recently, results from many studies revealed that monolaurin, the monoglycerides of lauric acid from coconut oil had antimicrobial activity against various gram positive and gram negative organisms, including Escherichia vulneris, Enterobcater spp.13, Helicobacter pylori 14, Staphylococcus aureus 15 , Candida spp., including C. albicans, C. glabrata, C. tropicalis, C. parapsilosis, C. stellatoidea and C. krusei 16 , as well as enveloped viruses 17-18. Electron microscopic images showed that 15 minutes exposure to monoglycerides caused gram positive cocci cell shrinkage and cell membrane disintegration. Data from clinical studies confirm the efficacy of coconut oil in the treatment of atopic dermatitis and removing S. aureus from colonized skin lesions 15. In addition, soap made from coconut oil had antimicrobial properties against Escherichia coli 19. Though the exact antibacterial mechanism of the action of coconut oil is still unclear, it was hypothesized that monolaurin and other medium chain monoglycerides had the capacity to alter bacterial cell walls, penetrate and disrupt cell membranes, inhibit enzymes involved in energy production and nutrient transfer, leading to the death of the bacteria 15. In the case of viruses, the virucidal effects of monolaurin appeared to be that of solubilizing the lipids and phospholipids in the envelope leading to disintegration of the virus particles 20. Sesame oil was demonstrated to have antibacterial activity against S. mutans. It contains high amounts of unsaturated fatty acids. Linoleic acid and oleic acid are the predominant compositions. Oil-pulling therapy with sesame oil significantly reduced S. mutans counts in plaque and saliva of adolescents within one week 6. In accordance with these previous investigations, our result showed that sesame oil reduced S. mutans to approximately 1 log compared with saline solution.
Oil-pulling therapy with sunflower oil was shown to reduce plaque scores after 45 days 4. However, the pre- and post- values of bacterial count reduction were not statistically different. To our knowledge, little information regarding antimicrobial properties of sunflower oil exists. Infants treated with sunflower oil are less likely to experience bacterial skin infections than are control infants 21-22. This may be the result of skin barrier enhancing effects, or some antimicrobial actions of the oil. Ozonized sunflower oil (oleozon) showed antimicrobial acitivity against S. aureus, E. coli, Pseudomonas aeruginosa, Enterococcus faecalis, Mycobacterium spp., Streptococcus pyogenes and C. albicans 23-24. However, the activity might be due to the powerful oxidant properties of the ozone itself. Considering the antimicrobial effect of other oils, including corn oil, palm oil, rice bran oil and soy bean oil, it was proposed that small amounts of saturated fatty acid, i.e. lauric acid, in these oils may play a role in their antimicrobial properties. In conclusion, results from the present study could be scientific evidence to demonstrate that oil-pulling therapy with some edible oils could be used as a preventive home therapy to maintain oral hygiene, especially in developing countries. However, further studies are needed to investigate the mechanisms of the action of the oil on these microorganisms or dental plaque, as well as long-term effects in clinical trials. REFERENCES 1. Signoretto C, Burlacchini G, Faccioni F, Zanderigo M, Bozzola N, Canepari P. Support the role of Candida spp. in extensive caries lesions of children. New Microbiol 2009; 32: 101-7. Shu M, Wong L, Miller JH, Sissons CH. Development of multi-species consortia biofilms of oral bacteria as an enamel and root caries model system. Arch Oral Biol 2000; 45: 27-40. Asokan S. Oil pulling therapy. Indian J Dent Res 2008; 19: 169. Amith HV, Ankola AV, Nagesh L. Effect of oil pulling on plaque and gingivitis. J Oral Health Comm Dent 2007; 1: 12-8. Asokan S, Emmadi P, Chamundeswari R. Effect of oil pulling on plaque induced gingivitis: A randomized, controlled, triple-blind study. Indian J Dent Res 2009; 20: 47-51.
2.
3. 4.
5.
65
Asia Journal of Public Health, May August 2011
Vol.2 No. 2
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
Asokan S, Rathan J, Muthu MS, Rathna P V, Emmadi P, Raghuraman C, et al. Effect of oil pulling on Streptococcus mutans count in plaque and saliva using Dentocult SM strip mutans test: A randomized, controlled, triple-blind study. J Indian Soc Pedod Prev Dent 2008; 26: 12-7. Loo CY, Corliss DA, Ganeshkumar N. Streptococcus gordonii biofilm formation: identification of genes that code for biofilm phenotypes. J Bacteriol 2000;182; 1374-82. Guggenheim B, Guggenheim M, Gmur R, Giertsen E, Thurnheer T. Application of the Zurich biofilm model to problems of cariology. Caries Res 2004; 38: 212-22. Ambika S. Fundamentals of biochemistry for medical students. Kartik Offsets Printers; 2001, p 50-4. Lim-Sylianco CY. Anticacinogenic effect of coconut oil. Phillipine J Coconut Studies 1987; 12: 89-102. Pehowick D J, Gomes A V, Barnes J A. Fatty acid composition and possible health effects of coconut constituents. West Indain Med J 2000; 49: 128-93. Hierholzer JC, Kabara JJ. In vitro effects Of monolaurin compounds on enveloped RNA and DNA viruses. J Food Safety 1982; 4: 1-12. Carpo BG, Verallo-Rowell VM, Kabara J. Noval antibacterial activity of monolaurin compared with conventional antibiotics against organisms from skin infections: an in vitro study. J Drugs Dermatol 2007; 6: 991-8. Bergsson G, Steingrimsson O, Thormar H. In vitro susceptibilities of Neisseria Gonorrhoeae to fatty acids and monoglycerides. Antimicrob Agents Chemother 1999; 43: 2790-2. Verallo-Rowell VM, Dillague KM, SyahTjundawan BS. Novel antibacterial and emollient effects of coconut and virgin olive oils in adult atopic dermatitis. Dermatitis 2008; 19: 308-15.
16. Ogbolu DO, Oni AA, Daini OA, Oloko AP. In vitro antimicrobial properties of coconut oil on Candida species in Ibadan, Nigeria. J Med Food 2007; 10: 384-7. 17. Bartolotta S, Garcia CC, Candurra NA, Damonte EB. Effect of fatty acids on arenaviruses replication: inhibition of virus production by lauric acid. Arch Virol 2001; 146: 777-90. 18. Clarke NM, May JT. Effect of antimicrobial factors in human milk on rhinoviruses and milk-borne cytomegalovirus in vitro. J Med Microbiol 2000; 41: 719-23. 19. Jitjumroonchokchai P, Hirankerd K. Study on the efficiency of antibiotic soap made from 8 various kinds of plant oil. Agricultural Sci J 2009; 40: 221-4. 20. Thormar H, Hilmarsson H. The role of microbicidal lipids in host defense against pathogens and their potential as therapeutic agents. Chem Phys Lipids 2007; 150: 1-11. 21. Darmstadt G L, Saha S K, Ahmed A S, Chowdhury MA, Law PA, Ahmed S, et al. Effect of tropical treatment with skin barrier-enhancing emollients on nosocomial infections in preterm infants in Bangladesh: a randomized controlled trail. Lancet 2005; 365: 1039-45. 22. Darmstadt G L, Badrawi N, Law P A, Ahmed S, Bashir M, Iskander I, et al. Topically applied sunflower seed oil prevents invasive bacterial infections in preterm infants in Egypt: a randomized, controlled clinical trail. Pediatr Infect Dis J 2004; 23: 719-25. 23. Sechi LA, Lezcano I, Nunez N, Espim M, Dupr I, Pinna A, et al. Antibacterial activity of ozonized sunflower oil (Oleozon). J Appl Microbiol 2001; 90: 279-84. 24. Menndez S, Falcn L, Simn DR, Landa N. Efficacy of ozonized sunflower oil in the treatment of tinea pedis. Mycoses 2000; 45: 329-32.
66
Você também pode gostar
- Effects of Tesla Purple PlateDocumento5 páginasEffects of Tesla Purple Platesanjay6969100% (4)
- Introducing The Sorush Cancer Treatment Protocol (SCTP)Documento18 páginasIntroducing The Sorush Cancer Treatment Protocol (SCTP)SorushAinda não há avaliações
- Rigging TechniquesDocumento27 páginasRigging TechniquesDeepak ShettyAinda não há avaliações
- No Sweat - Chapter 2: Escape The Vicious Cycle of FailureDocumento27 páginasNo Sweat - Chapter 2: Escape The Vicious Cycle of FailureAMACOM, Publishing Division of the American Management AssociationAinda não há avaliações
- Magnesium The Miracle MineralDocumento4 páginasMagnesium The Miracle MineralScott SheltonAinda não há avaliações
- Magnesium The Miracle MineralDocumento4 páginasMagnesium The Miracle MineralScott SheltonAinda não há avaliações
- Checklist Auditoria SQF 2010Documento21 páginasChecklist Auditoria SQF 2010cramirez48Ainda não há avaliações
- Chapter III Pharmacokinetics: Durge Raj GhalanDocumento64 páginasChapter III Pharmacokinetics: Durge Raj GhalanDurge Raj Ghalan100% (3)
- Herbal Medicine For Insomnia: Eric Yarnell, ND, RH (AHG)Documento7 páginasHerbal Medicine For Insomnia: Eric Yarnell, ND, RH (AHG)GururajBalse0% (1)
- State of the Art Answers to 500 Mold QuestionsNo EverandState of the Art Answers to 500 Mold QuestionsAinda não há avaliações
- Nursepreneurs Essay by J. BacarisasDocumento17 páginasNursepreneurs Essay by J. BacarisasCris GalendezAinda não há avaliações
- Karma YogaDocumento120 páginasKarma Yogasanjay6969Ainda não há avaliações
- Top 10 Myco Toxic FoodsDocumento3 páginasTop 10 Myco Toxic Foodsradikalgrl100% (1)
- Employee Benefits India PDFDocumento2 páginasEmployee Benefits India PDFshahidki31100% (1)
- Microbiological Examination of Dairy ProductsDocumento7 páginasMicrobiological Examination of Dairy Productskolita kamal100% (5)
- Applications of Flow Cytometry in Stem Cell Research and Tissue RegenerationNo EverandApplications of Flow Cytometry in Stem Cell Research and Tissue RegenerationAinda não há avaliações
- DR - Bach & A Medicine For The Soul PDFDocumento20 páginasDR - Bach & A Medicine For The Soul PDFsanjay6969100% (1)
- Health Tourism Presentation IBMDocumento65 páginasHealth Tourism Presentation IBMMd. Ashraf Hossain SarkerAinda não há avaliações
- Repertoar Flori de BachDocumento74 páginasRepertoar Flori de BachLidia Dicu100% (1)
- Repertoar Flori de BachDocumento74 páginasRepertoar Flori de BachLidia Dicu100% (1)
- Repertoar Flori de BachDocumento74 páginasRepertoar Flori de BachLidia Dicu100% (1)
- Ashtanga Yoga FundamentalDocumento2 páginasAshtanga Yoga FundamentalMarina Rolla De LeoAinda não há avaliações
- Human Tumours Secreting Catecholamines: Clinical and Physiopathological Study of the PheochromocytomasNo EverandHuman Tumours Secreting Catecholamines: Clinical and Physiopathological Study of the PheochromocytomasNota: 5 de 5 estrelas5/5 (1)
- Grades: - 3 Midterms (20%) Held in Lab - Final (15%) - Comprehensive - Labs (25%) - 94% Is An A - Powerpoints Online!Documento3 páginasGrades: - 3 Midterms (20%) Held in Lab - Final (15%) - Comprehensive - Labs (25%) - 94% Is An A - Powerpoints Online!Keesha Mae Urgelles TimogAinda não há avaliações
- Anticonvulsant Therapy in DogsDocumento21 páginasAnticonvulsant Therapy in DogsConstanza Aedo SibilaAinda não há avaliações
- Nutrigenetics & Fatty Acid Metabolism: Genes Analysed in ThisDocumento21 páginasNutrigenetics & Fatty Acid Metabolism: Genes Analysed in ThisPetra JobovaAinda não há avaliações
- Antibiofilm Activity and Post Antifungal Effect of Lemongrass Oil On Clinical Candida Dubliniensis IsolateDocumento7 páginasAntibiofilm Activity and Post Antifungal Effect of Lemongrass Oil On Clinical Candida Dubliniensis Isolatezila_w2gAinda não há avaliações
- Foods 08 00175 v2Documento14 páginasFoods 08 00175 v2C1Muhammad Iqbal FarozinAinda não há avaliações
- (23915412 - Open Life Sciences) The Effects of Various Mouthwashes On Osteoblast Precursor CellsDocumento8 páginas(23915412 - Open Life Sciences) The Effects of Various Mouthwashes On Osteoblast Precursor CellsDragos CiongaruAinda não há avaliações
- Chemical Composition Antibacterial Activity and Mechanism of Action of Essential Oil From Seeds of Fennel Foeniculum Vulgare Mill 2014 Food ControlDocumento8 páginasChemical Composition Antibacterial Activity and Mechanism of Action of Essential Oil From Seeds of Fennel Foeniculum Vulgare Mill 2014 Food ControlAni IoanaAinda não há avaliações
- 234687214Documento6 páginas234687214Yosivak Maulisa BlangidikoAinda não há avaliações
- Jop 2008Documento8 páginasJop 2008Evelyng Taype EspinozaAinda não há avaliações
- Efficacy of Natural Antimicrobials in Toothpaste Formulations Against Oral Biofilms in VitroDocumento7 páginasEfficacy of Natural Antimicrobials in Toothpaste Formulations Against Oral Biofilms in VitroRobert ShawAinda não há avaliações
- Cryopreservation of Streptococcus Mutans For Microcalorime - 2000 - ThermochimicDocumento7 páginasCryopreservation of Streptococcus Mutans For Microcalorime - 2000 - ThermochimicJerusalen BetancourtAinda não há avaliações
- Antibacterial and AntibioflmDocumento8 páginasAntibacterial and AntibioflmHoàng HuyAinda não há avaliações
- Food Control: Milene Zezzi Do Valle Gomes, Marcia NitschkeDocumento7 páginasFood Control: Milene Zezzi Do Valle Gomes, Marcia Nitschkezulaika22Ainda não há avaliações
- Probiotic Efficiency of Spirulina Platensis - Stimulating Growth of Lactic Acid BacteriaDocumento4 páginasProbiotic Efficiency of Spirulina Platensis - Stimulating Growth of Lactic Acid BacteriastanleystAinda não há avaliações
- The Effect of Coconut Oil Pulling On Streptococcus Mutans Count in Saliva in Comparison With Chlorhexidine MouthwashDocumento4 páginasThe Effect of Coconut Oil Pulling On Streptococcus Mutans Count in Saliva in Comparison With Chlorhexidine MouthwashMelk SalesAinda não há avaliações
- Atmajaya WD. 2015Documento7 páginasAtmajaya WD. 2015Shankar arumugamAinda não há avaliações
- 32 LSA Prem PDFDocumento6 páginas32 LSA Prem PDFLife Science ArchivesAinda não há avaliações
- Lactobacillus reuteri extracts promoted wound healing via PI3K/AKT/ β-catenin/ TGF β1 pathwayDocumento11 páginasLactobacillus reuteri extracts promoted wound healing via PI3K/AKT/ β-catenin/ TGF β1 pathwayYuniarAinda não há avaliações
- Direct Spray Drying and Microencapsulation of Probiotic Lactobacillus Reuteri From Slurry Fermentation With Whey PDFDocumento8 páginasDirect Spray Drying and Microencapsulation of Probiotic Lactobacillus Reuteri From Slurry Fermentation With Whey PDFpniramolAinda não há avaliações
- Pan, X., Chen, F., Wu, T., Tang, H., Dan Zhao, Z. 2009. The Acid, Bile Tolerance and Antimicrobial Property of Lactobacillus Acidophilus NIT. J. Food Control. 20 598-602.Documento5 páginasPan, X., Chen, F., Wu, T., Tang, H., Dan Zhao, Z. 2009. The Acid, Bile Tolerance and Antimicrobial Property of Lactobacillus Acidophilus NIT. J. Food Control. 20 598-602.AfdhalRuslanAinda não há avaliações
- Pemanfaatan Limbah Kulit Melinjo Sebagai Sumber ANTIBIOTIK TERHADAP BAKTERI (Escherichia Coli)Documento7 páginasPemanfaatan Limbah Kulit Melinjo Sebagai Sumber ANTIBIOTIK TERHADAP BAKTERI (Escherichia Coli)Nada Syafa TitaniaAinda não há avaliações
- Biosynthesis and Properties of Extracellular Amylase by Encapsulation Bifidobatrium Bifidum in Batch CultureDocumento8 páginasBiosynthesis and Properties of Extracellular Amylase by Encapsulation Bifidobatrium Bifidum in Batch Cultureray m deraniaAinda não há avaliações
- Cytotoxicity and Arecoline Mechanisms in Human Gingival Fibroblasts in VitroDocumento7 páginasCytotoxicity and Arecoline Mechanisms in Human Gingival Fibroblasts in VitroRetta Gabriella PakpahanAinda não há avaliações
- Bacteriocins From Lactic Acid Bacteria Inhibit Food Borne Pathogens.Documento7 páginasBacteriocins From Lactic Acid Bacteria Inhibit Food Borne Pathogens.International Organization of Scientific Research (IOSR)Ainda não há avaliações
- Mustafa UlkerDocumento8 páginasMustafa UlkerTasha FarahAinda não há avaliações
- Inhibition Effect of Zataria Multiflora On Lactobacillus SPDocumento3 páginasInhibition Effect of Zataria Multiflora On Lactobacillus SPsukriti bajpaiAinda não há avaliações
- Efficay Essential OilDocumento3 páginasEfficay Essential OilatikramadhaniAinda não há avaliações
- Nisin 4Documento9 páginasNisin 4ritikkvs1Ainda não há avaliações
- Cengkehob 3Documento8 páginasCengkehob 3barcimAinda não há avaliações
- Test For LipstickDocumento16 páginasTest For LipstickMeuTia RumondangAinda não há avaliações
- 182014paper AntimicobialActivityVCOSundariLoung PDFDocumento7 páginas182014paper AntimicobialActivityVCOSundariLoung PDFHeryMafirajiAmirsyahAinda não há avaliações
- Ifrj 2011 043Documento11 páginasIfrj 2011 043Raul Diaz TorresAinda não há avaliações
- Anaerobe: E.M. Costa, S. Silva, F.K. Tavaria, M.M. PintadoDocumento5 páginasAnaerobe: E.M. Costa, S. Silva, F.K. Tavaria, M.M. PintadoAdhitya Sofiyati DewiAinda não há avaliações
- Activity of Virgin Coconut Oil, Lauric Acid or Monolaurin in Combination With Lactic Acid Against Staphylococcus AureusDocumento17 páginasActivity of Virgin Coconut Oil, Lauric Acid or Monolaurin in Combination With Lactic Acid Against Staphylococcus AureusMonyet...Ainda não há avaliações
- Pistacia Oil and Experimental ColitisDocumento7 páginasPistacia Oil and Experimental ColitisRihabAinda não há avaliações
- Molecules 25 00792 v2Documento15 páginasMolecules 25 00792 v2Khela Pagol ManushAinda não há avaliações
- Fish ScaleDocumento13 páginasFish ScaleRhea May Lourene MagsinoAinda não há avaliações
- 16-D23 2774 Tetiana Haniastuti IndonesiaDocumento7 páginas16-D23 2774 Tetiana Haniastuti IndonesiakhamilatusyAinda não há avaliações
- In-Vitro Cytotoxicity and Antioxidant Property Evaluation From Methanolic Extract of Cuscuta Reflexa FlowersDocumento7 páginasIn-Vitro Cytotoxicity and Antioxidant Property Evaluation From Methanolic Extract of Cuscuta Reflexa FlowersASIF AL MAHMOODAinda não há avaliações
- Jurnal 2Documento7 páginasJurnal 2SasaAinda não há avaliações
- Food Fruit PreservationDocumento7 páginasFood Fruit PreservationEricka JennAinda não há avaliações
- Effects of Oregano in S. AureusDocumento5 páginasEffects of Oregano in S. AureusLindberg MedinaAinda não há avaliações
- Aceite de Coco PeriodontalDocumento8 páginasAceite de Coco PeriodontalErick PiñerosAinda não há avaliações
- Dialnet ObtainingOfTheEssentialOilOfSyzygiumAromaticumIden 4914911Documento7 páginasDialnet ObtainingOfTheEssentialOilOfSyzygiumAromaticumIden 4914911Erick ZevallosAinda não há avaliações
- Artikel 4 - Curcuma ZedoariaDocumento10 páginasArtikel 4 - Curcuma Zedoariamonika puspitasariAinda não há avaliações
- Antimicrobial Activity of Gac Fruit (Momordica Cochinchinensis) PDFDocumento6 páginasAntimicrobial Activity of Gac Fruit (Momordica Cochinchinensis) PDFPham Thi Cam TuAinda não há avaliações
- Week 8 Aerobic Plate CountDocumento7 páginasWeek 8 Aerobic Plate CountSam 0505Ainda não há avaliações
- Coconut Oil and Virgin Coconut Oil An Insight IntoDocumento3 páginasCoconut Oil and Virgin Coconut Oil An Insight IntoMSKCAinda não há avaliações
- Plugin 42686Documento4 páginasPlugin 42686Manupati PrasanthAinda não há avaliações
- Purification Micro AlgaeDocumento8 páginasPurification Micro Algaembah37Ainda não há avaliações
- Original Research Article: Lucida BenthDocumento19 páginasOriginal Research Article: Lucida BenthmelendezjmanuelAinda não há avaliações
- Agro India - MAY 2021Documento41 páginasAgro India - MAY 2021sanjay6969Ainda não há avaliações
- Give Us A Call at 1-800-214-2850: Proudly DistributingDocumento59 páginasGive Us A Call at 1-800-214-2850: Proudly Distributingsanjay6969Ainda não há avaliações
- Cells & TissuesDocumento8 páginasCells & Tissuessanjay6969Ainda não há avaliações
- A Study On The Effect of Dinacharya For Healthy Living in Modern Age PDFDocumento5 páginasA Study On The Effect of Dinacharya For Healthy Living in Modern Age PDFsanjay6969Ainda não há avaliações
- LLL ResearchDocumento2 páginasLLL Researchsanjay6969Ainda não há avaliações
- L CT 1000 BrochureDocumento6 páginasL CT 1000 Brochuresanjay6969Ainda não há avaliações
- The Photobiology of LED PhototherapyDocumento2 páginasThe Photobiology of LED Phototherapysanjay6969Ainda não há avaliações
- LLL ResearchDocumento12 páginasLLL Researchsanjay6969Ainda não há avaliações
- Laser Cure Worli 101, 1 ST Floor, Citizen Society, Nariman Road, Mumbai-4000025 Phone - 24370655, 9372415985/87, 9325126107/109Documento2 páginasLaser Cure Worli 101, 1 ST Floor, Citizen Society, Nariman Road, Mumbai-4000025 Phone - 24370655, 9372415985/87, 9325126107/109sanjay6969Ainda não há avaliações
- Form 9Documento2 páginasForm 9rahul_khanna4321Ainda não há avaliações
- Golf View Apartment - 6th Floor PlanDocumento1 páginaGolf View Apartment - 6th Floor Plansanjay6969Ainda não há avaliações
- LLL ResearchDocumento12 páginasLLL Researchsanjay6969Ainda não há avaliações
- Ashtanga Yoga Mantra-1Documento4 páginasAshtanga Yoga Mantra-1sanjay6969Ainda não há avaliações
- Low Level LasersDocumento1 páginaLow Level Laserssanjay6969Ainda não há avaliações
- Ekadantaya Vakratundaya Song Lyrics - HilyricsDocumento1 páginaEkadantaya Vakratundaya Song Lyrics - Hilyricssanjay69690% (2)
- State Bank of India Beneficiary Approval FormDocumento1 páginaState Bank of India Beneficiary Approval Formsanjay6969Ainda não há avaliações
- ONGC JobDocumento4 páginasONGC Jobsanjay6969Ainda não há avaliações
- Yoga 1Documento8 páginasYoga 1in678Ainda não há avaliações
- IOCL NotificationDocumento9 páginasIOCL NotificationNDTVAinda não há avaliações
- MTNL Mumbai - CustomerDocumento1 páginaMTNL Mumbai - Customersanjay6969Ainda não há avaliações
- MTNL Mumbai - CustomerDocumento1 páginaMTNL Mumbai - Customersanjay6969Ainda não há avaliações
- Irradiated Foods 2003 PDFDocumento52 páginasIrradiated Foods 2003 PDFDiana BratuAinda não há avaliações
- Genflex Roofing Systems, LLC Material Safety Data SheetDocumento4 páginasGenflex Roofing Systems, LLC Material Safety Data SheetgjroddyAinda não há avaliações
- Quiz BukasDocumento3 páginasQuiz BukasDYRAH GRACE COPAUSAinda não há avaliações
- Quantitative Analysis of Lead, Cadmium and Chromium Found in Selected Fish Marketed in Metro Manila, PhilippinesDocumento6 páginasQuantitative Analysis of Lead, Cadmium and Chromium Found in Selected Fish Marketed in Metro Manila, PhilippinesMstkasrAinda não há avaliações
- Prof Nik Marzuki Data PDFDocumento3 páginasProf Nik Marzuki Data PDFsue labanAinda não há avaliações
- Amal ResumeDocumento2 páginasAmal Resumeapi-242600239Ainda não há avaliações
- Toxoplasmosis Serologic Testing AlgorithmDocumento1 páginaToxoplasmosis Serologic Testing AlgorithmHanny Prasetiana YuriantiAinda não há avaliações
- Essay (DUNGARAN, JOHN KLENN) (BSCE-1CDocumento2 páginasEssay (DUNGARAN, JOHN KLENN) (BSCE-1CJohn KlennAinda não há avaliações
- BW Health-5Documento2 páginasBW Health-5Michael JaballasAinda não há avaliações
- BKV Application Form (Sea Staff) Rev08Documento5 páginasBKV Application Form (Sea Staff) Rev08Mehmet ErgeanAinda não há avaliações
- Therapy General Objective Specific Objective Indication Activities Rationale Dance Therapy 1. Jumping RhythmsDocumento2 páginasTherapy General Objective Specific Objective Indication Activities Rationale Dance Therapy 1. Jumping RhythmsSabrina Porquiado Magañan SNAinda não há avaliações
- B.inggris Weny LestariDocumento5 páginasB.inggris Weny LestariRatna SusantiAinda não há avaliações
- Common Childhood Rashes: Has The Rash Got Fluid-Filled (Vesiculobullous) Lesions?Documento4 páginasCommon Childhood Rashes: Has The Rash Got Fluid-Filled (Vesiculobullous) Lesions?abu ubaidahAinda não há avaliações
- 2017 ESC Guidelines For The Management of Acute Myocardial Infarction in Patients Presenting With ST Segment ElevationDocumento66 páginas2017 ESC Guidelines For The Management of Acute Myocardial Infarction in Patients Presenting With ST Segment ElevationMoises Torres AlvarezAinda não há avaliações
- ResearchDocumento3 páginasResearchMervin AlbercaAinda não há avaliações
- Anatomi Dan Fisiologi Mata 1Documento61 páginasAnatomi Dan Fisiologi Mata 1MAWANAinda não há avaliações
- Laporan IKM KSM PK FEBRUARI 2022Documento28 páginasLaporan IKM KSM PK FEBRUARI 2022Nur iffahAinda não há avaliações
- BAYBAY AwardsDocumento63 páginasBAYBAY AwardsClennil Palmes SustraidoAinda não há avaliações
- Spelling 101Documento10 páginasSpelling 101Arellano CheireyAinda não há avaliações
- Ejsr Vol 97 Issue 1 159 171Documento171 páginasEjsr Vol 97 Issue 1 159 171Raja ChandruAinda não há avaliações
- Trends in Diagnosed Chronic Hepatitis B in A US Health System Population, 2006-2015Documento8 páginasTrends in Diagnosed Chronic Hepatitis B in A US Health System Population, 2006-2015farid ahmadAinda não há avaliações
- Quizizz: DM Bronze Recap (Final)Documento10 páginasQuizizz: DM Bronze Recap (Final)Mahika ManeshAinda não há avaliações
- MSDS Dross AluminiumDocumento18 páginasMSDS Dross AluminiumNurul muzayyanahAinda não há avaliações