Escolar Documentos
Profissional Documentos
Cultura Documentos
Avian Diseases Found in Captivity Final
Enviado por
api-250146149Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Avian Diseases Found in Captivity Final
Enviado por
api-250146149Direitos autorais:
Formatos disponíveis
Avian Diseases Found in Captivity
Disease
Acanthamoebiasis
Animal Group(s) Affected
-Birds
Transmission
-Source: soil, water -Gains entry via: breaks in skin; respiratory tract; corneal surface; hematogenous spread to central nervous system Requires ingestion of the intermediate host or a paratenic or transport host
Clinical Signs
- Cutaneous lesions - Sinusitis - Pneumonitis - Neurologic signs - Fever - Nausea - Vomiting Ill thrift, weight loss, anorexia, diarrhea, abdominal discomfort or colic; clinical signs compatible with peritonitis Granulomas of tongue and lymph nodes of head and neck. Local abscesses, chronic draining fistulas, bony infections, or infections of body cavities. Clinical signs referable to the involved area Mammal: respiratory, conjunctivitis, liver disease, gastroenteritis. Avian:
Severity
- Asymptomatic in immunecompetent individuals - Frequently fatal in immunocompromised individuals Infections can cause clinical disease and mortality. Severity of disease may not be directly correlated with the number of adult parasites present.
Treatment
Pentamidine isethionate; Sulfadiazine; Flucytosine; Fluconazole; Itraconazole Amphotericin B; Azithromycin Ivermectin and doramectin have eliminated Macracanthorhynchus species in dogs and swine. Albendazole has eliminated Moniliformis clarki from cotton-topped tamarins. Surgical debridement, systemic sodium iodide and long-term antibiotics Surgical drainage and debridement. Appropriate antibiotic therapy continued for several weeks after elimination of clinical signs. Supportive/ symptomatic.
Acanthocephalans
All vertebrates
Wooden Tongue (Actinobacillus lignieresii)
Chickens
Actinomycosis
Birds
Normal oropharyngeal and rumen flora enters tissues through epithelial damage. Endogenous infection into susceptible tissues or by bite wound
Variable; life threatening without treatment.
Can be mild if restricted to local infection but can be fatal depending on infection location, spread, and time to diagnosis. Variable: asymptomatic to death. Usually disease is sporadic and
Adenovirus
Avian
Vertical, Direct Contact, Fecaloral, Venereal.
Aeromonas Infection
Waterfowl
Aspergillosis
Vertebrates, invertebrates
Horizontal transmission, close contact with infected individual, ingestion of bacterium, direct inoculation through wounds, especially from contaminated water. Snake mite (Ophionyssus, natricis) capable of transmitting bacteria Environment -acquired via spores. It is not considered contagious. Primarily direct transmission via urofecaloral route. Viral shedding in urine, feces, choanal secretions and feathers. Increasing evidence for vertical
abnormal eggs and production, respiratory disease. Reptile: none to poor doer to unexplained death. Acute mortality, dermal hyperemia, skin wounds, pustular dermatitis, stomatitis, fasciitis, pneumonia, gastrointestinal disease
limited to the young and immunecompromised
Mild to severe depending on immune status, and route of infection
Antibiotics, appropriate wound management, supportive care
Avian Bornaviruses
Captive psittacine birds Canaries Wild freeranging goose, swan, duck and gull species.
Primarily respiratory but can become systemic. Occasionally a cutaneous disease. Proventricular dilatation disease (PDD); infection may range from asymptomatic to severe gastrointestinal signs with or without neurological signs.
May cause severe disease in immunecompromised hosts.
Antifungal drugs polyenes, azoles, allylamines, pyrimidines No specific treatment. Supportive and symptomatic treatment and good husbandry can prolong life. Possibility of complete cure is not
Birds infected with ABV may or may not show clinical disease. Once clinical signs develop, PDD is generally considered a progressive disease which ultimately becomes fatal. Acute outbreaks with high mortality have been described in psittacine aviaries.
Avian Influenza
Birds, predominantly carried by waterfowl and shorebirds,
Avian Poxvirus
Avian
transmission Fecal-oral and fecal-cloacal (i.e., contaminated water), airborne and direct contact through mucous membranes, ingestion of infected tissues, fomites and mechanical vectors Mechanical spread by invertebrate vectors. Direct contact between birds or indirect contact with contaminated surfaces.
LPAItypically asymptomatic HPAIRespirator y, digestive or nervous system signs, sudden death
Asymptomatic to fatal in all animals affected
certain. Anti-viral drugs in humans
Babesiosis
Ubiquitous in wildlife wherever tick infestations are present. Variety of species, including mammals can be affected.
Numerous species of ixodid ticks
Baylisascariasis
Avian
Ingestion of embryonated eggs or infected carrier hosts
Cutaneous or dry form: skin nodules. Diptheritic or wet form: internal lesions in upper alimentary or respiratory tracts. Systemic infection. Severe hemolytic anemia, hemoglobinemia, hemoglobinuria, fever, possible neurologic signs, anorexia, slight jaundice, or subclinical. Majority of infections in wildlife are subclinical. Depression, lethargy, agitation, tremors, head or body tilt, circling, ataxia, lateral recumbency, coma
Small, focal skin lesions to widespread severe lesions; respiratory difficulties, to peracute death in certain species.
Treat secondary bacterial infections. May need to provide supportive fluids and food.
May be severe, with acute clinical presentation and death. Clinical disease often less severe in free-ranging animals than domestic animals.
Imidicarb, tick control
Asymptomatic to fatal
Early aggressive treatment with albendazole and high dose steroids have shown to be effective, ocular larva
Lyme Disease
Some birds although they are usually asymptomatic
Campylobacteriosis
Birds
Tick vector (Ixodes sp); rodents are among the most important reservoir hosts, including white-footed mouse (Peromyscus leucopus) in N. America and Apodemus sp. in Eurasia) Food- or water-borne; fecal-oral spread; direct contact with contaminated surfaces or contact with infected animals
General: Shifting leg lameness, arthritis, fever, myocarditis, CNS signs
Varies, can be asymptomatic, mild lameness, or chronic illness
migrans can be killed using laser treatment Doxycycline x 30d, azithromycin, ceftriaxone, amoxicillin; recrudescence is possible
Host-specific: none to severe; diarrheal disease - watery or bloody; possibly with fever, abdominal cramps, nausea, and vomition; other illnesses, such as abortion and infertility, and periodontal disease
Mild to life threatening; gastroenteritis, with possible sepsis and disseminated infections; children, immunecompromised individuals and the elderly may be at greater risk. Long-term consequences (such as arthritis or Guillain-Barr) occur rarely in people Morbidity and mortality rates vary with the affected species, condition of infected individual, and strain/genotype involved.
Avian Chlamydiosis/ Chlamydophilosis
Avian
Inhalation of aerosolized fecal matter and nasal discharges primarily; also oral secretions and feathers Fomites Mechanical transmission may occur rodents and
Non-specific, oculo-nasal discharge, respiratory signs, conjunctivitis, diarrhea, weight loss, anorexia, depression, green to yellow green urates Some birds
Extra fluids to remain hydrated as long as diarrhea persists. Recovery often occurs without antibiotics, although they may be used to shorten the duration of clinical signs if administered early in course of disease. For most avian species: Doxycycline for 30-60 days. See treatment section for details
Clostridial DiseaseBotulism Toxicosis
Birds
Clostridial DiseaseTetanus
Coronavirus
Equidae; bovidae; cervidae; primates; elephant; macropods; and rodents. Multiple avian taxa.
insects Vertical transmission is infrequent Ingestion of toxin contaminated food or tissues. Wound contamination Contamination of wounds from bacteria in soil.
may have subclinical infections Mostly neurologic, involving flaccid paralysis. Gastrointestinal signs. Muscle rigidity and spasm localized or generalized. Diarrhea (often mucoid) due to enteritis, respiratory discharge, dyspnea, lethargy, death. Mammal infections may be subclinical or lead to fever, anorexia, late term abortions, infertility, retained placenta, metritis. Typically respiratory, central nervous system, ocular, or cutaneous signs; possibly in Dose related severity of mild to lethal. Supportive care; antitoxin when appropriate.
Up to 80 % mortality in clinically ill animals.
Penicillin, tetanus antitoxin, supportive care to reduce signs and support of airway. Supportive, antibiotics to reduce secondary infections.
Fecal-oral, inhalation, contaminated feed or fomites.
Often very severe.
Q Fever (Coxiella burnetii)
Birds
Cryptococcosis
Birds
Two patterns: 1) wild animals and ticks, 2) domestic ruminants independent of wildlife cycles. Shed in high numbers within amniotic fluid and placenta. Excreted in milk, urine, feces. It also may be spread through wind and dust. Inhalation of airborne organisms
Highly infectious. Humans acute form has moderate morbidity (50%), generally low mortality (12%). Mortality with endocarditis is up to 65%. Moderate to severe; guarded prognosis with neurologic signs.
Tetracycline antibiotics if showing clinical signs
Antifungal drugs; in some cases, surgical excision of granulomas may be helpful
Cryoptosporidiosis
Birds
Direct: fecal to oral. Waterborne transmission, possible paratenic host transmission, possible aerosol transmission in birds.
combination. Gastrointestinal: Diarrhea, vomiting. Respiratory disease documented in birds.
Duck Viral Enteritis (Duck Plague)
Ducks, geese, swan of all ages
Eastern Equine Encephalitis (EEE)
Birds
Bird to bird contact or via environment; water is important for transmission. Spontaneous viral shedding by duck plague carriers, particularly during spring Mosquito (Culiseta melanura)
Diarrhea, blood stained vent, cyanotic bill, inability to fly, convulsions, polydipsia, hypersensitivity to light
Depending on the affected species and organ system, severity can vary from a mild, transient, self-limiting disease to a severe and fatal disease. Severe disease is typical of immune suppressed patients, and reptiles. Moderate to severe
Nitazoxanide (Alinia) is licensed and approved for use in humans. Oral bovine hyperimmune serum is reported to be effective in reptiles. Paromomycin (Humatin) is effective against some stages of the disease, but will not eliminate infection. No effective treatment
Ehrlichia ruminatum (Heartwater)
Possibly (although not definitively proven) in birds.
Non-contagious tick borne disease via Ambylomma spp. ticks including US
Febrile, altered mentation, neurologic abnormalities, seizures, paresis, paralysis, death Acute fever, anorexia, diarrhea, serosa or mucosa
Equine fatality rate is up to 90%; survivors usually exhibit long-term neurologic signs; human fatality rate 50-75% Subclinical to peracute death. Dependent on strain, host, and
Supportive care
Remove ticks and antibiotics (e.g., tetracycline). Submit ticks
tick species: A. maculatum, A. cajennense, A. dissimile, A. americanum.
Erysipelas (Erysipelothrix rhusiopathiae)
Turkey, multiple other vertebrate species
Bacteria shed in urine, saliva, nasal secretions, and feces. Transmitted by direct contact with infected animals or body discharges (ingestion, transcutaneous). Apparently healthy swine can be carriers. Transmitted vertically (perinatal) or horizontal (percutaneous or mucosal exposure to infected body fluids, i.e. blood, saliva, sexual fluids, wound exudate)
Hepatitis B Virus
Birds
petechiae, respiratory and neurologic signs. Peracute sudden death! Acute disease pyrexia, anorexia, depression, stilted gait, diamond skin lesions, death. Chronic exercise intolerance, lameness, enlarged joints Weight loss, lethargy, anorexia, icterus, abdominal discomfort, nausea, vomiting
environment. Most common is acute clinical disease.
for diagnosis using the pCS20 RT or nested PCR.
Mild to severe. High mortality in untreated animals.
Acute disease penicillin. Chronic disease no treatment.
Klebsiella
All vertebrates
Animalanimal, human-animal, or animalhuman Environmental point sources (feed, feces, water, bedding material). Cockroach or house fly vector. Nosocomial
Normal fecal and oral cavity inhabitants. Bacterial septicemia, abscessation, multiple organ inflammation. K. pneumoniae with a unique hypermucovisco us
Often asymptomatc in non-human primates but can cause severe disease in gibbons and wooly monkeys; increased prevalence of hepatocellular carcinoma in chronic infections in woodchucks, humans. Variable
Supportive care; antivirals or -interferon can be attempted but to date unsuccessful in animal cases.
Antibiotics with Gramnegative activity pending appropriate sensitivity testing. Supportive care. It can develop a high level of
infections. Opportunistic pathogen, primary pathogen, component of normal flora, or environmental contaminant
Listeriosis
All
Lung Mites
Birds
Fecal-oral, inhalation, direct contact with affected tissues, or indirectly through contaminated milk, cheese, meat, eggs, fruits or vegetables in people. Common route in animals is hay contamination or unstable silage. Direct
Atypical Mycobacteriosis
Birds
Ingestion Inhalation Waterborne Environmental exposure via defects in respiratory, integumentary, or urogenital systems
phenotype (HMV K. pneumoniae) is an emerging disease concern in humans and NHPs as a communityacquir ed infection causing pyogenic liver abscesses Three primary forms: encephalitic, abortion septicemic (usually neonates and monogastrics) but also can see ophthalmic form. Primarily winter-spring disease in US In many cases, animals are asymptomatic; however, in severe infections, they may show signs of upper or lower respiratory disease depending on the host and species of parasite involved. Variable to none Cutaneous lesions Ascites Pneumonia Mastitis Lymphadenopat hy Lameness
resistance; common nosocomial concern.
Without aggressive treatment, encephalaitis and septicemic disease is often fatal or animals recover with permanent brain damage (encephalitic form) Dependent on the intensity of infection. Mortality is low.
Aggressive and early treatment with antibiotics, supportive care.
Ivermectin
Asymptomatic to chronic disease or acute death
May not be advised Antibiotics aminoglycoside; quinolone; macrolide
Avian Mycobacteriosis
All birds
Direct extension via Fecal-oral, environment, inhalation
Emaciation Lethargy Emaciation, weakness, lethargy, hepatosplenome galy Rarely skin lesions and respiratory disease
Variable. Severe in the individual with end stage disease
Mycoplasmosis (Mycoplasma ovipneumoniae, M. gallisepticum, M. agassizi, and others) Newcastle Disease
Birds
Birds
Psittacid Herpesvirus 1/ Pachecos Disease
Psittacines, rarely passerines
Direct contact between animals most important, fomites possible Highly contagious Avian Paramyxovirus 1 (APMV-1). Aerosol and ingestion are the primary routes. Inadvertent comingling asymptomatic with non-exposed birds. Ingestion of contaminated material from oral secretions or feces. Aerosol route is possible but not proven.
Respiratory (pneumonia, coughing), conjunctivitis, polyarthritis Death; gastrointestinal and respiratory signs
Tends to be chronic; can be severe and result in death.
Not recommended as this organism is resistant to most, if not all human antimycobacterial drugs. Euthanasia may need to be considered Difficult to treat but macrolides and fluoroquinolones are most effective. Not usually performed. In zoo specimens treatment is supportive care with consideration of vaccination.
Severe; typically fatal
Death with few premonitory signs. Rarely nonspecific signs, including lethargy and the presence of bile pigments in urine. Three of four PcHV-1 genotypes have been associated with
Dependent on viral genotype and species of birds, death can range from single birds to flock majority. Virtually all birds showing signs of the acute form will die unless treated. Mucosal papillomas cause
Acyclovir is very effective at stopping outbreaks when the entire flock is treated.
Pasteurellosis
Avian
Plasmodium
Birds especially penguins
Aerosol, mechanical via bite or scratch wounds, or environmental (food, water). Colonization of lungs by endogenous nasopharyngeal bacteria is described in ruminants and swine due to environmental stressors and/or primary infections due to viruses or Mycoplasma spp. Mosquitoes of different genera; in reptiles, also other biting flies
oral and cloacal mucosal papillomas. Primarily depression, fever, coughing, nasal and oral discharge, increased respiratory rates, tachypnea. Arthritis, gastrointestinal disease, otitis media, mastitis, bite wound abscesses and other signs are possible.
considerable morbidity but are rarely fatal. Variable. Ranges from subclinical to peracute and fatal. Supportive care, early intervention with antibiotics, ideally based on antibiotic sensitivity. Drainage of localized abscesses. Organ specific treatment for systemic infections. Peracute systemic infections may be unresponsive. Various antimalarial drugs can be used but are unlikely to eliminate infection at tissue stage; resulting in relapses of parasitemia Supportive care should be provided in isolated environments where even caretakers have no contact with other birds.
Lethargy; anorexia; minor to severe anemia; neurologic signs; paralysis
Psittacine Beak and Feather Disease
Psittacines Old World more than New World species
Direct contact with infected animals with virus presented by inhalation or ingestion. Indirect contact with contaminated excretions, secretions and feather dust. Virus remains in contaminated environments,
Peracute: Particularly common in African grey parrots with pancytopenia and death. Acute: Depression followed by appearance of dystrophic feathers and death. Chronic: Progressive
Typically of low virulence in adapted hosts; mild to severe possibly fatal disease in non-adapted hosts Aggressive disease most common in African grey, vasa, and eclectus parrots, and cockatoos. PCV-1 associated disease is fatal in most Old World psittacines. Chronic and less severe
particularly air handling systems, for years.
Pythiosis
Birds
Motile biflagellate zoospore (P. insidiosum) released into aquatic environments
Salmonellosis
Most vertebrates
Fecal-oral; direct contact by infected animals or indirectly via arthropods, or contaminated vehicles, equipment, feed, and water.
appearance of dystrophic feathers. Necrotic beak and ulcerations in some long term infected birds. Death occurs in months to years. Gastrointestinal: weight loss, vomiting, diarrhea, and hematochezia. Cutaneous: Non-healing wounds, nasopharyngeal lesions, invasive subcutaneous masses, draining nodular lesion, or ulcerated plaque-like lesions. Mild: gastroenteritis with vomiting, and diarrhea. Severe: additionally anorexia, lethargy, weight loss, pyrexia, polydipsia, dehydration, and ocular lesions; Severe acute septicemia: multifocal petechial hemorrhage, polyserositis, polyarthritis, bronchopneumo nia, meningitis or
disease in lovebirds, lories and lorikeets, particularly those birds infected with PCV-2. Devastating and often fatal unless resectable with wide margins. Surgical resection or amputation of infected tissues with wide margins. Postoperative treatment with antifungals may decrease recurrence when incomplete resection occurs. Antibiotics: streptomycin, gentamicin, tetracyclines, doxycycline.
Varies from subclinical carriage to septicemia and death. Septicemic form often is fatal without prior or unobserved clinical signs.
Screw Worm- New World
All warm blooded animals but most cases occur in cattle, goats and sheep.
Gravid female flies deposit eggs either in wounds or directly onto intact mucous membranes.
Screw Worm- Old World
All warm blooded animals, including birds
Flies are attracted to open wounds. Gravid female flies deposit eggs either into wounds or directly onto intact mucous membranes Ingestion of intermediate (invertebrate or vertebrate) or paratenic host
meningoencepha litis, death. Discomfort, decreased appetite, wounds with malodorous, reddish/brown fluid with larvae; slight movement inside a closed wound. Severe myiasis in open wounds; associated discomfort and decreased appetite
Untreated animals could die. Mortality rates in Texas when disease was endemic in the USA was 2080% in fawns. Severe infestations that remain untreated may result in the death of the host in a short time
Organophosphates (spray, foam, dip, dust) (e.g., (coumaphos, ronnel), or lindane.
Spiruridosis
Birds and insectivores
St. Louis Encephalitis
Birds (usually subclinical reservoirs, possible illness)
Bite of infected mosquito; theoretical risk of direct contact with infected tissues at necropsy. Opportunistic pathogens often involving
Variable, but may include chronic gastritis, vomiting, hemoptysis, anemia, anorexia, weight loss, conjunctivitis, keratitis, and sudden death Fever, stiff neck, seizures, coma.
Inapparent to severe; many are subclinical
Removal and killing of the larvae in lesion. Treatment of the wound with approved insecticide. Ivermectin 200-300 mcg/kg Levamisole, albendazole, mebendazole, ivermectin and other anthelminthics
Staphylococcus SPP. Infection
Birds
Can affect every organ system and clinical signs
In people, mild to severe, can be fatal although most infections are asymptomatic. Illness in animals is not completely understood. Depends upon organ(s) affected and
Supportive care - fluids, anticonvulsants; antiinflammatories.
Antibiotics: First-choice antibiotics (pending culture
breaks in the skin. Ubiquitous, and live free in the environment and commensal parasites of skin and upper respiratory tract. Droplet, direct/indirect contact transmission can occur.
Streptococcus Group C
Birds
Inhalation; ingestion; during breeding; transplacental. Indirectly via hands and/or fomites. Indirectly via hands and/or fomites. Direct contact with infectious exudates. Undercooked horsemeat. Ingestion of oocysts from felid feces; ingestion of tissue cysts; transplacental; transmammary
Toxoplasmosis
All vertebrates (primarily birds and mammals)
depend upon organ affected. Common cause of dermatitis. Fever, anorexia, pain, abscesses and infections of the skin, eyes, ears, respiratory system, mammary glands, genitourinary tract, skeleton, joints. Toxins may produce signs of food poisoning. Variable based on organ system affected. Abscesses; pharyngitis; cellulitis; septicemias; rhinitis; ocular discharge; coughing; sneezing; draining tracts. Abortions. Mastitis. Variable, depending on species and organs affected. Can range from asymptomatic to sudden death.
immune status of host.
and sensitivity testing) include cephalosporins and fluoroquinolones. Antibiotic resistance is common so sensitivity testing is recommended.
Severity can range from mild to severe or fatal, depending on age, species, and immune status of the individual.
1st choice: Procaine penicillin and ampicillin. 2nd choice: Cephalosporins, chloramphenicol, macrolides, rifampin, and trimethoprimsulfas.
Variable depending on species. Causes severe disease in Australian marsupials, New World primates, and lemurs. Usually asymptomati
Atovaquone, clindamycin, sulfonamide.
Trichostrongylosis
Birds
Fecal-oral with a direct life cycle
Heavy burdens cause weight loss, lethargy, anorexia, watery diarrhea, weakness anemia, and death
c in most felids. Low level infections are usually asymptomatic. Young animals more severely affected.
Trichuriasis
Wide range of birds
Tularemia
All warmblooded animals
Fecal/oral transmission via transmission of eggs with infective L2 Some capillarids may use earthworms as intermediate or paratenic host Arthropod vectors such as ticks, biting flies, and, in some areas, mosquitoes. Inhalation of aerosolized infectious material Ingestion of contaminated food or water
Weight loss, and diarrhea.
High morbidity, but low mortality
Benzimidazoles or macrocyclic lactones. Alternatives to anthelmintics have been investigated in artiodactylids including cooper oxide wire particles and nematophagous fungus (environmental control) Fenbendazole, milbemycin oxime
Depends on route of infection; general: lethargy, anorexia, pyrexia Transdermal exposure is marked by ulcer at site of inoculation;
lymphadenopathy.
Clinical signs can be severe and death result if untreated. Pneumonic form: severe. Septicemia often death occurs without prior signs
Antibiotics: streptomycin, gentamicin, tetracyclines, doxycycline
Oral exposure: Inhalation: pneumonia, coughing Skinning dead infected animals;
lymphadenopathy
West Nile Virus
Avian
Western Equine Encephalitits
Birds- Emus show clinical illness, while native birds serve as viral reservoirs without clinical illness
Primarily via mosquito bite, possibly ticks; less efficient means include ingestion of virus via infected carcasses or contaminated fluids (feces, urine, oral or cloacal); occupational exposure, blood transfusion, organ transplant, and maternal transmission Bite of WEE infected mosquito, but may be transmitted by ticks. Possibly from direct contact with infected tissues at necropsy (i.e. through broken skin or mucous membranes)
contaminated water Range: asymptomatic to non-specific (e.g., anorexia, weight loss, dehydration) to neurologic (e.g., ataxia, lethargy, paresis, paralysis, convulsions, seizures, death)
High fatality in some avian species (especially corvids and some raptors); 10-30% of equine clinical cases are fatal; <1% of human cases are severe (i.e., West Nile neuroinvasive disease)
Supportive care, immunoglobulin therapy
Yersiniosis
Birds
Ingestion of fecal contaminated food and
Equids: Fever, anorexia, lethargy (somnolence), impaired vision, dysphagia, circling, head pressing, paresis, paralysis, seizures Emus: asymptomatic infections are common; anorexia, watery diarrhea, weight loss, abnormal neck movements neurologic signs Diarrhea, abdominal pain, fever, weakness,
Mild to severe, may be fatal
No specific treatment but supportive care, hydration, and nutritional support are important. Anticonvulsant and antiinflammatory treatment may be used.
Ranges from subclinical to acutely fatal or a chronic
Third generation cephalosporins, fluoroquinolones; supportive
water; ingestion of raw meat and milk; blood transfusions (humans)
septicemia, weight loss, enlarged lymph nodes, sudden death
wasting form, depending on individual and species
therapy
Você também pode gostar
- Reptilian and Amphibious Diseases Found in Captivity FinalDocumento12 páginasReptilian and Amphibious Diseases Found in Captivity Finalapi-250146149Ainda não há avaliações
- Mammalian Diseases Found in Captivity FinalDocumento45 páginasMammalian Diseases Found in Captivity Finalapi-250146149Ainda não há avaliações
- Common Poultry DiseasesDocumento15 páginasCommon Poultry DiseasesMamas IpunkAinda não há avaliações
- Poultry DiseasesDocumento7 páginasPoultry DiseasesJohnMasiveAinda não há avaliações
- Poultry diseases: Causes, symptoms and treatment, with notes on post-mortem examinationsNo EverandPoultry diseases: Causes, symptoms and treatment, with notes on post-mortem examinationsAinda não há avaliações
- Diarrhoea CattleDocumento8 páginasDiarrhoea CattleAlexander GintingAinda não há avaliações
- 5 622647121207623762 PDFDocumento13 páginas5 622647121207623762 PDFNitin Kale100% (1)
- A-Z by SpeciesDocumento93 páginasA-Z by SpeciesRachel HayonAinda não há avaliações
- Abortions in Dairy Cows PDFDocumento4 páginasAbortions in Dairy Cows PDFransinghAinda não há avaliações
- Respiratory Diseases of CattleDocumento30 páginasRespiratory Diseases of CattleArwinnie SanitriaAinda não há avaliações
- CacingDocumento21 páginasCacingIhza SaputraAinda não há avaliações
- Porcine Infertility: Prof G N PurohitDocumento25 páginasPorcine Infertility: Prof G N PurohitgnpobsAinda não há avaliações
- Cpe Common Diagnoses 6-4-2021Documento9 páginasCpe Common Diagnoses 6-4-2021Shubham HarishAinda não há avaliações
- Postpartum Uterine Infection in CattleDocumento26 páginasPostpartum Uterine Infection in CattleDilip GuptaAinda não há avaliações
- Veterinary EctoparasitesDocumento3 páginasVeterinary EctoparasitesBharat KafleAinda não há avaliações
- Zuku Visual Flashnotes Distemper CondensedDocumento1 páginaZuku Visual Flashnotes Distemper CondensedRayza LubisAinda não há avaliações
- Swine 2Documento40 páginasSwine 2Keegan McElroyAinda não há avaliações
- Cytologic Patterns - Eclinpath PDFDocumento5 páginasCytologic Patterns - Eclinpath PDFJD46Ainda não há avaliações
- Canine Heartworm InfectionDocumento5 páginasCanine Heartworm InfectionnessimmounirAinda não há avaliações
- Veterinary Clinical Pathology Clerkship ProgramDocumento46 páginasVeterinary Clinical Pathology Clerkship ProgramDrVijayata ChoudharyAinda não há avaliações
- Feline Urologic Syndrome enDocumento2 páginasFeline Urologic Syndrome enSitiNurjannahAinda não há avaliações
- Bacteriology Textbook 2009 PDFDocumento298 páginasBacteriology Textbook 2009 PDFKrispinus SehandiAinda não há avaliações
- Wildlife NoteDocumento14 páginasWildlife NoteDeep PatelAinda não há avaliações
- Swine Infectious Gastrointestinal DiseasesDocumento6 páginasSwine Infectious Gastrointestinal DiseasesnessimmounirAinda não há avaliações
- VetPrep TOPDIFFERENTIAL JUL2019 v1Documento8 páginasVetPrep TOPDIFFERENTIAL JUL2019 v1Lonely WolfAinda não há avaliações
- Trematodes of Wild BirdsDocumento5 páginasTrematodes of Wild BirdsSunilAinda não há avaliações
- Bovine Disease Diagnostic ManualDocumento38 páginasBovine Disease Diagnostic ManualRachel AutranAinda não há avaliações
- Digestive System 3Documento11 páginasDigestive System 3Shubham HarishAinda não há avaliações
- Lecture 17 Canine InfertilityDocumento28 páginasLecture 17 Canine InfertilitygnpobsAinda não há avaliações
- Lumpy Skin DiseaseDocumento28 páginasLumpy Skin DiseaseShivaputraAinda não há avaliações
- Section 8 - Equine Bacterial DiseasesDocumento3 páginasSection 8 - Equine Bacterial DiseasesRakesh KumarAinda não há avaliações
- Fluidtherapy GuidelinesDocumento11 páginasFluidtherapy Guidelineshamida fillahAinda não há avaliações
- Species DiagnosesDocumento33 páginasSpecies DiagnosesJoanneYiAinda não há avaliações
- 2015 Proceeding - Management of The Patient With Canine Parvovirus EnteritisDocumento7 páginas2015 Proceeding - Management of The Patient With Canine Parvovirus EnteritisJHack2Ainda não há avaliações
- Toxin Mechanism of Action Sign of Toxicity Diagnosis Treatment Anticholinesterase InsecticidesDocumento2 páginasToxin Mechanism of Action Sign of Toxicity Diagnosis Treatment Anticholinesterase Insecticidesrayrrn00100% (1)
- Clinical Veterinary Advisor Dogs and Cats by Etienne Cote DVMDACVIMCardiology and Small Animal Internal Medicine 5 Star ReviewDocumento2 páginasClinical Veterinary Advisor Dogs and Cats by Etienne Cote DVMDACVIMCardiology and Small Animal Internal Medicine 5 Star ReviewAndres GarciaAinda não há avaliações
- Newcastle DiseaseDocumento36 páginasNewcastle DiseaseIman BorithnabanAinda não há avaliações
- Horner's Syndrome: Lid) Eye) (" ")Documento3 páginasHorner's Syndrome: Lid) Eye) (" ")D TAinda não há avaliações
- Pre Pubertal Gonadectomy in Dogs and Cats-Part IIIDocumento5 páginasPre Pubertal Gonadectomy in Dogs and Cats-Part IIItaner_soysurenAinda não há avaliações
- Veterinary Critical CareDocumento15 páginasVeterinary Critical Caresudanfx100% (1)
- Vet HandbookDocumento113 páginasVet HandbookAndreia AndreiAinda não há avaliações
- Reproductive Diseases in Cattle: Brucellosis (Bang's Disease)Documento4 páginasReproductive Diseases in Cattle: Brucellosis (Bang's Disease)Janice Li100% (1)
- Anemia and Pyometra in DogsDocumento20 páginasAnemia and Pyometra in DogsVer FajaAinda não há avaliações
- Cephalosporins in Veterinary MedicineDocumento23 páginasCephalosporins in Veterinary MedicineSunil100% (3)
- Parasites of PoultryDocumento8 páginasParasites of PoultrylisaAinda não há avaliações
- 099 - Small Ruminant HealthDocumento49 páginas099 - Small Ruminant HealthSuraj_Subedi100% (1)
- Cpe Ecfvg Appendix of Common DiagnosesDocumento9 páginasCpe Ecfvg Appendix of Common DiagnosesMayank Mj PatelAinda não há avaliações
- Standardised Nomenclature of Animal Parasitic Diseases (Snopad)Documento67 páginasStandardised Nomenclature of Animal Parasitic Diseases (Snopad)Pwaveno BamaiyiAinda não há avaliações
- Hints On Veterinary Ophthalmology: By/Sara Ahmed Hassouna BVSC, MSC Surgery Dept. Vet. Med. Alex. UniDocumento39 páginasHints On Veterinary Ophthalmology: By/Sara Ahmed Hassouna BVSC, MSC Surgery Dept. Vet. Med. Alex. UniBibek SutradharAinda não há avaliações
- The Leukotrienes: Chemistry and BiologyNo EverandThe Leukotrienes: Chemistry and BiologyLawrence ChakrinAinda não há avaliações
- Canine Ehrlichiosis With Uveitis in A Pug Breed Dog: Case StudDocumento2 páginasCanine Ehrlichiosis With Uveitis in A Pug Breed Dog: Case StudDR HAMESH RATREAinda não há avaliações
- Avian Hematology and Related DisordersDocumento22 páginasAvian Hematology and Related DisordersIban Hernández100% (1)
- Foot and Mouth DiseaseDocumento5 páginasFoot and Mouth Diseaseelvhynd beiAinda não há avaliações
- Guinea Pigs PDFDocumento1 páginaGuinea Pigs PDFYaserAbbasiAinda não há avaliações
- Special Veterinary Pathology: The Canadian Veterinary Journal. La Revue Veterinaire Canadienne February 1990Documento2 páginasSpecial Veterinary Pathology: The Canadian Veterinary Journal. La Revue Veterinaire Canadienne February 1990Alonso Guardado100% (1)
- Birds and Exotics - MCannon PDFDocumento42 páginasBirds and Exotics - MCannon PDFAl OyAinda não há avaliações
- Drug Profile 2015Documento75 páginasDrug Profile 2015api-324380555100% (1)
- Zuku Visual Flashnotes Ethylene Glycol ExtendedDocumento4 páginasZuku Visual Flashnotes Ethylene Glycol ExtendedShubham HarishAinda não há avaliações
- Classical Swine FeverDocumento143 páginasClassical Swine FeverAgus SuwarnoAinda não há avaliações
- Review Questions UAPGADocumento28 páginasReview Questions UAPGAkarenAinda não há avaliações
- G 10 ICT WorkSheetc 2.2 English MDocumento8 páginasG 10 ICT WorkSheetc 2.2 English MMohamaad SihatthAinda não há avaliações
- BR Safetymatrix enDocumento12 páginasBR Safetymatrix enHamidreza MoaddeliAinda não há avaliações
- Manual DessertDocumento32 páginasManual DessertDANIEL F. HERNANDEZ100% (1)
- Castlegar & Slocan Valley Pennywise Dec. 9, 2014Documento49 páginasCastlegar & Slocan Valley Pennywise Dec. 9, 2014Pennywise PublishingAinda não há avaliações
- Reading Week 13Documento6 páginasReading Week 13Quy PhanAinda não há avaliações
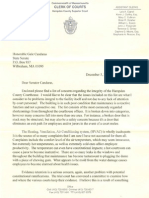
- Laura Gentile Letter On Hampden County CourthouseDocumento6 páginasLaura Gentile Letter On Hampden County CourthouseMassLiveAinda não há avaliações
- Hebrew and TamilDocumento98 páginasHebrew and TamilSreshta JustinAinda não há avaliações
- Grade 8 MAPEH ReviewerDocumento4 páginasGrade 8 MAPEH ReviewerVictoria DelgadoAinda não há avaliações
- Time Complexity in CDocumento28 páginasTime Complexity in CHîmäñshû SîñghAinda não há avaliações
- Specifications: Louie Jean Mabanag Ar - 3BDocumento8 páginasSpecifications: Louie Jean Mabanag Ar - 3BLouie Jean100% (1)
- WOHLFARTH C. - CRC Handbook of Thermodynamic Data of Polymer Solutions at Elevated Pressures - (CRC PRESS 2005 648 P) PDFDocumento648 páginasWOHLFARTH C. - CRC Handbook of Thermodynamic Data of Polymer Solutions at Elevated Pressures - (CRC PRESS 2005 648 P) PDFdavidnps100% (1)
- Shaped House With Gablehip Roof 2020Documento11 páginasShaped House With Gablehip Roof 2020Marco CamposAinda não há avaliações
- Coronary Stents: Current StatusDocumento42 páginasCoronary Stents: Current StatusMANSI SALUNKEAinda não há avaliações
- Festivals of IndiaDocumento51 páginasFestivals of IndiaDhatchayani RamkumarAinda não há avaliações
- ESL Discussion Questions To Practise IdiomsDocumento5 páginasESL Discussion Questions To Practise IdiomsElaine Mc AuliffeAinda não há avaliações
- Ok TC FlotationDocumento4 páginasOk TC FlotationWilliam SalcedoAinda não há avaliações
- Hopf 6870 - 1101Documento58 páginasHopf 6870 - 1101macakafkaAinda não há avaliações
- 1965 Elio R. Freni - Electrolytic Lead Refining in SardiniaDocumento9 páginas1965 Elio R. Freni - Electrolytic Lead Refining in SardiniaGeorgettaAinda não há avaliações
- Auto CadDocumento24 páginasAuto Cadkanchan Redas RedasAinda não há avaliações
- Genmega G2500Documento103 páginasGenmega G2500tchindaforentAinda não há avaliações
- (Complete) BLC 201 Assignment Intro Logistics SCM Sep 2021 - McdonaldDocumento12 páginas(Complete) BLC 201 Assignment Intro Logistics SCM Sep 2021 - McdonaldHf CreationAinda não há avaliações
- Elements of HardscapingDocumento57 páginasElements of HardscapingNathar ShaAinda não há avaliações
- 017 - Chapter 3 - L13Documento6 páginas017 - Chapter 3 - L13nanduslns07Ainda não há avaliações
- System Substation Commissioning TestsDocumento8 páginasSystem Substation Commissioning TestsCvijayakumar100% (1)
- Wahabism - Bala SurajoDocumento17 páginasWahabism - Bala SurajoAbu Muhammad50% (2)
- External Otitis (OE)Documento24 páginasExternal Otitis (OE)Hannah BLissAinda não há avaliações
- QB Som He306 2015 2016Documento23 páginasQB Som He306 2015 2016etayhailuAinda não há avaliações
- Job Hazard Analysis Form: Section A: Task InformationDocumento3 páginasJob Hazard Analysis Form: Section A: Task InformationHasnei NAinda não há avaliações
- INTERVIEW QUESTIONS - Verilog - PART-1Documento9 páginasINTERVIEW QUESTIONS - Verilog - PART-1charan tejaAinda não há avaliações