Escolar Documentos
Profissional Documentos
Cultura Documentos
Epistaxis
Enviado por
Fika Khulma SofiaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Epistaxis
Enviado por
Fika Khulma SofiaDireitos autorais:
Formatos disponíveis
309
REVIEW
Epistaxis: an update on current management
L E R Pope, C G L Hobbs
............................................................................................................................... Postgrad Med J 2005;81:309314. doi: 10.1136/pgmj.2004.025007
Epistaxis is one of the commonest ENT emergencies. Although most patients can be treated within an accident and emergency setting, some are complex and may require specialist intervention. There are multiple risk factors for the development of epistaxis and it can affect any age group, but it is the elderly population with their associated morbidity who often require more intensive treatment and subsequent admission. Treatment strategies have been broadly similar for decades. However, with the evolution of endoscopic technology, new ways of actively managing epistaxis are now available. Recent evidence suggests that this, combined with the use of stepwise management plans, should limit patient complications and the need for admission. This review discusses the various treatment options and integrates the traditional methods with modern techniques.
...........................................................................
which can result in persistent nasal bleeding despite unilateral arterial ligation. Anterior bleeds are responsible for about 80% of epistaxis. They occur at an anastomosis called Kiesselbachs plexus on the lower part of the anterior septum known as Littles area. Posterior bleeding derives primarily from the posterior septal nasal artery (a branch of the sphenopalatine artery), which forms part of the Woodruff plexus.
AETIOLOGY
The aetiology of epistaxis can be divided into local and general causes (box 1), however most (80% 90%) are actually idiopathic. An important contributing factor, in addition to the prominent vascularity and dual blood supply to the nose, is that blood vessels within the nasal mucosa run superficially and are therefore comparatively unprotected. In most cases, it is damage to this mucosa and to vessel walls that results in bleeding. Spontaneous rupture of blood vessels may occur occasionally, such as during extreme valsalva when weightlifting. Although uncommon, it is important to exclude neoplasia as a cause for unexplained recurrent unilateral epistaxis.
pistaxis, whether spontaneous or otherwise, is experienced by up to 60% of people in their lifetime, with 6% requiring medical attention.1 Although our understanding of this condition has improved considerably, the principle of packing the nose for a nosebleed has changed little since Hippocrates used sheeps wool on pugilistic noses in ancient Greece.
MANAGEMENT
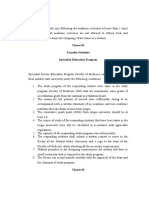
The traditional management of acute epistaxis entails identification of the bleeding point by using a head mirror or other light source. If a bleeding point is localised, then chemical or electrocautery is performed. If unsuccessful, further management takes a stepwise approachinitially anterior packing with some form of gauze or sponge and then failing this, more advanced techniques such as compressive balloons or posterior packing. Finally, arterial ligation or embolisation can be used to stem intractable bleeds. Figure 1 outlines a suggested management plan. Resuscitation Epistaxis is a potential life threatening event. All patients who are actively bleeding need full assessment and resuscitation if necessary. The clinical state of an elderly patient may deteriorate rapidly so aggressive resuscitation is vital. Universal precautions should be worn before starting any treatment including a facemask and eye protection. Vital signs must be monitored regularly. A full blood count should be taken and blood group and saved. Studies have shown that routine clotting studies need to be performed only if there is a suspected clotting diathesis or the patient is anticoagulated.3 Fluid management should be instigated if signs of hypovolaemia are present or admission is required. During resuscitation, bleeding can commonly be controlled by digital pressure over the lower soft cartilaginous part of the nose. This is often best performed by
EPIDEMIOLOGY
The incidence of epistaxis varies greatly with age. There is a bimodal distribution with peaks in children and young adults and the older adult (4565 years).2 Anecdotal evidence suggests that certain stereotypical groups are more prone (for example, elderly women or young boys).
ANATOMY
One of the primary functions of the nose is to warm and humidify air. It therefore has a profuse blood supply arising from both the internal and external carotid arteries. Epistaxis is normally classified into anterior or posterior, but it can also be classed as superior or inferior depending on the carotid supply. Broadly, the internal carotid (via the ethmoidal arteries) supplies the region above the middle turbinate while the remaining areas are supplied by branches of the external carotid artery. This includes the sphenopalatine artery, which supplies most of the septum and turbinates on the lateral wall. The interface between the two carotid systems varies in position according to the pressure in each one. There is also crossover between the right and left arterial systems,
See end of article for authors affiliations ....................... Correspondence to: Mr C G L Hobbs, Department of Otolaryngology and Head and Neck Surgery, St Michaels Hospital, Southwell Street, Bristol BS2 8EG, UK; chris. hobbs@doctors.org.uk Submitted 4 June 2004 Accepted 14 September 2004 .......................
www.postgradmedj.com
310
Pope, Hobbs
Box 1 Causes of epistaxis
Local
the nasopharynx, which is less uncomfortable for the patient and will help to reduce swallowing of blood and its subsequent nausea.
N N N N N N N N
Idiopathic Trauma Nose picking Facial injury Foreign body Inflammation Infection Allergic rhinosinusitis Nasal polyps Neoplasia Benign (for example, juvenile angiofibroma) Malignant (for example, squamous cell carcinoma) Vascular Congenital (for example, hereditary haemorrhagic telangiectasia) Acquired (for example, Wegeners granulomatosis) Iatrogenic Surgery (for example, ENT/maxillofacial/ophthalmic) Nasal apparatus (for example, nasogastric tube) Structural Septal spurs or deviation Septal perforations Drugs Nasal sprays (for example, topical decongestants) Abuse (for example, cocaine) Haematological Coagulopathies (for example, haemophilia) Thrombocytopenia (for example, leukaemia) Platelet dysfunction (for example, Von Willebrands disease) Environmental Temperature Humidity Altitude Drugs Anticoagulants (for example, heparin, warfarin) Antiplatelet (for example, aspirin, clopidogrel) Organ failure Uraemia Liver (for example, cirrhosis) Other Atherosclerosis/hypertension Alcohol
Nasal preparation Good nasal preparation is critical to elucidate and treat the cause of epistaxis. The nasal cavity is often obscured by clots. Thus immediately before examination a forceful blow by the patient through the nose can clear these clots. Although this action may restart bleeding it will enable improved access for anaesthetic. A precautionary view of the cavity should be undertaken by anterior rhinoscopy using a Thudicums speculum; this will enable stubborn clots to be evacuated by suction and permit initial assessment of the bleeding point. Local anaesthetic, ideally including a vasoconstrictor, should be applied to the nasal mucosa over Littles area (box 2). The application method varies on the preparation, but most entail either a solution applied on cotton wool or as a nasal spray. Time should be allowed for the anaesthetic to work. Generally, systemic analgesia is not necessary when inspecting or packing the nose, although mild sedation (with a small dose of diazepam) is often used in hypertensive or anxious patients. Once adequate local anaesthesia is achieved, the nasal cavity can be examined and treatment instigated to stem the haemorrhage. Littles area is viewed first. Cautery Chemical cautery is achieved by a using silver nitrate stick (75% silver nitrate, 25% potassium nitrate BP w/w) that reacts to the mucosal lining to produce local chemical damage. The technique entails applying the stick to the bleeding point with firm pressure for 510 seconds. The effect varies with concentration and exposure. Feeding vessels can also be cauterised to limit recurrence. Careful removal of excess silver nitrate helps prevent staining of the vestibule or upper lip. If staining does occur, it should be neutralised immediately by applying normal saline. Only one side of the septum should be cauterised, as there is a small risk of septal perforation resulting from decreased vascularisation to the septal cartilage. For this reason, we suggest a four to six week interval between cautery treatments. Electrocautery is usually performed in clinic by otolaryngologists under local anaesthetic; it consists of an electrical circuit that heats up a metal loop. With this technique thermal energy seals the bleeding vessel by radiation, not by direct contact. A potential complication is heat damage to the anterior nares and inferior turbinate. This risk can be reduced by using a large aural speculum under microscopic examination. Anterior packing The nose should be packed if bleeding continues despite cautery or if no obvious bleeding is seen. There are many forms of anterior nasal packing although nasal sponges have become predominant as they offer a simple and effective mechanism for applying pressure to the bleeding vessel.
General
N N N N
Nasal tampons
There are several types available. Merocel is made of polyvinyl alcohol, a compressed foam polymer that is inserted into the nose (fig 2) and expanded by application of water. This causes the tampon to swell and fill the nasal cavity, applying pressure over the bleeding point. It may also allow clotting factors to localise and reach a critical level, thereby facilitating coagulation. Merocels are easy to insert within a casualty setting and require minimal training. They are effective in 85% of cases, with no difference between the success rates when compared with traditional ribbon gauze.4 Rapid Rhino is an example of a carboxymethylcellulose pack. This is a hydrocolloid material, which acts as a platelet aggregator and also forms a lubricant on contact with water.
an assistant (nurse or healthcare assistant) and can be improved by a cold compress or the patient sucking on ice. Leaning the patient forward will decrease blood flow through
www.postgradmedj.com
Epistaxis
311
Assessment and first aid RESUS Initial medical review
Figure 1 Epistaxis management protocol.
Nasal preparation
Visualise bleeding point Controlled Yes No Bleeding
Endoscopic cautery available Controlled
Cauterise
Bleeding
Anterior pack Bleeding
Observe
Controlled Controlled
Observe
Posterior pack
Controlled Admit to ward
Bleeding Surgery
Follow up
Unlike Merocel, it has a cuff that is inflated by air and the hydrocolloid or Gel-Knit is supposed to preserve newly formed clot during removal.
Formal anterior packing
If nasal tampon packing fails to stem epistaxis, then one should consider formal packing with ribbon gauze. Again, there are many pre-prepared packs on the market, but the most common are Vaseline or bismuth-iodoform paraffin paste impregnated packs. These packs should be inserted under direct vision into a locally anaesthetised nasal cavity. After nasal packing, the patient is examined for ongoing bleeding through the pack, from the contralateral nares or posteriorly. This is done using a tongue depressor to obtain a good view of the oropharynx. If any bleeding is witnessed, packing of the other side should be considered before removal of the already inserted pack. This
may increase the tamponade pressure over the septum and stop the bleeding. Because of the risks associated with nasal packing (box 3), most patients are admitted to the ward. Some units will discharge a haemodynamically stable person home with packing in situ, for review in 2448 hours, although this is controversial because of the potential complications. If packs are left in for more than 48 hours, then antibiotics should be started to prevent toxic shock syndrome. Packs are usually removed within three days. Posterior packing Anterior packing is often insufficient to control vessels bleeding from the posterior nasal cavity. These bleeds can be difficult to treat and may require either balloon insertion or a formal posterior pack.
Balloon insertion Box 2 Common local anaesthetic preparations
This relies on either direct pressure or more commonly, the accumulation of blood within the nasal cavity leading to tamponade. There are several types that can be used; some have been designed especially for epistaxis management. Two of the important types are discussed.
Foley catheter
N N N N
Lidocaine injection (0.5%, 1%, or 2%) with adrenaline (epinephrine) 1/200 000 Cocaine topical solution (2% or 5%) Cocaine paste (10%) Lidocaine topical solution (5%) with 0.5 % phenylephrine (cophenylcaine)
This uses a standard urinary catheter that is inserted through the anterior nares and passed back until the tip is seen in the oropharynx. It is then inflated with 34 ml of water or air. The catheter is pulled forward until the balloon engages the
www.postgradmedj.com
312
Pope, Hobbs
pressure necrosis. The patient should always be admitted to hospital and consideration given to placing elderly patients or young children in a high dependency or intensive care environment for monitoring. Surgery Any bleeding that fails to stop despite an escalation of clinic room management requires surgical intervention. This includes bleeding that continues after pack removal. Before theatre, the patient needs to be haemodynamically stable. In most cases surgical management requires a general anaesthetic, although in frail elderly patients, local anaesthesia with sedation can be used. Surgical intervention can be divided into diathermy, septal surgery, or arterial ligation.
Diathermy
Figure 2 Correct insertion of a nasal tampon (note that the direction is along the floor of the nasal cavity).
posterior choana. The nasal cavity is then packed anteriorly with ribbon gauze or a nasal sponge. The balloon is held firmly in place with an umbilical clamp at the anterior nares. It is important in this case to protect the columella with a soft dressing, otherwise it is susceptible to pressure necrosis. Other complications include posterior displacement of the balloon with potential airway compromise, deflation in situ (which is more likely to occur with air inflation) and rupture of the balloon, which when it contains water, could result in aspiration. Recent evidence suggests that balloon rupture is more likely with the use of paraffin paste.5 It is important to note the Foley catheter is in fact, not licensed for nasal use.
Brighton balloon
The localisation of a bleeding point under general anaesthetic is easier because of improved nasal access and instrumentation. The use of bipolar rather than monopolar diathermy is recommended, as there are reports of optic or oculomotor nerve damage after the use of monopolar in6 or close to the orbit.7
Septal surgery
Septal surgery is sometimes performed to allow access to the nasal cavity. As most haemorrhages occur from the septum, raising a mucoperichondral flap during septal surgery can be beneficial as this will decrease blood flow to the mucosa, which often in itself stems bleeding. Surgery is also used to correct a deviated septum or remove a septal spur, which may be the cause of epistaxis. This occurs either by altering air flow through the nose or in severe cartilage deformities, by persistent mucosal irritation.
This is specifically manufactured for the treatment of epistaxis. It has a postnasal balloon and a mobile anterior balloon that are independently inflated (fig 3). Other specialised balloons include the Simpson plug and the Epistat nasal catheter.
Sphenopalatine artery ligation
In cases of ongoing haemorrhage despite the above methods, this procedure is normally attempted first. It is performed under direct rigid endoscopy and the vessel is normally clipped or coagulated using bipolar diathermy. Its success rate is reported to be better than other forms of arterial ligation probably because it is an end artery with little collateral flow.8
Formal posterior packing
In this rather uncomfortable procedure (hence it is normally performed under general anaesthetic), a gauze pad is sutured to a catheter inserted through the nose and using the catheter, is manoeuvred via the oral cavity into the nasopharynx so that it lodges against the choana. It is important to protect the columella with a dental roll to stop
Anterior/posterior ethmoidal artery ligation
This is occasionally required for severe bleeding from the ethmoidal region and is traditionally performed via an external ethmoidectomy incision, through a subperiosteal plane on the medial orbital wall. An endoscopic technique has been described9 and also, more recently, an endoscopically assisted external approach.10
Box 3 Complications of nasal packing
N N N
Failure to stem bleeding Toxic shock syndrome Blockage of
nasolacrimal duct leading to epiphora sinus drainage leading to acute sinusitis nasal airway leading to hypoxia
N N N N
Nasovagal reflex: this reflex occurs during insertion of a pack or instrumentation of the nasal cavity. It leads to vagal stimulation, with consequent hypotension and bradycardia Sleep apnoea, attributable to decreased nasal air entry leading to hypoxia during somnolence Displacement of pack into oropharynx with risk of acute airway obstruction Removal may induce bleeding
Figure 3 Sagittal view of the nasal cavity with a Brighton balloon in situ.
www.postgradmedj.com
Epistaxis
313
Maxillary artery ligation
This is rarely performed now since the introduction of endoscopic nasal surgery, but it has been shown to be effective in 87% of cases.11 The approach is a modified Caldwell-Luc operation, through the posterior wall of the maxillary sinus into the pterygopalatine fossa. The maxillary vessel can be either clipped or diathermied. Complications of this include devitalised gums and teeth, sinusitis, and problematic intraoperative bleeding.
Hot water irrigation The use of hot water irrigation is an alternative management strategy for posterior epistaxis. Techniques vary, but essentially a balloon catheter is used to close off the posterior choana and water at 45 C50 C is inserted into the nasal cavity. As well as helping to clear blood clots from the nose, it probably reduces local blood flow by causing mucosal oedema.20 Laser Laser has proved to be particularly useful in cases of recurrent epistaxis, such as those occurring in hereditary haemorrhagic telangiectasia (Osler-Weber-Rendu disease). Neodymium yttrium-aluminium-garnet (Nd:YAG) laser is commonly used (via endoscopy), although the application of other lasers such as argon or carbon dioxide has also been described.21
External carotid artery ligation
Ligation of the carotid artery for intractable epistaxis was first reported by Pilz in 1869 (performed on the common carotid artery in this case). It is a non-specific method of decreasing blood flow to the nose and, studies have shown a long term failure rate of 45%. This is because the nasal blood supply has marked watershed areas supplied by the contralateral external carotid.12 In general, it should be considered a last resort, useful in profound uncontrolled haemorrhage, when the above methods fail.
FOLLOW UP
All patients with a history of severe epistaxis require a formal examination of the nasal cavity to rule out a neoplastic lesion. This can be performed before discharge or in clinic at a later date. Patients should be given a leaflet showing first aid procedures for epistaxis and simple precautions to decrease recurrence including refraining from activities that may stimulate bleeding (blowing or picking their nose, heavy lifting, strenuous exercise) and abstinence from alcohol or hot drinks that can cause vasodilatation of the nasal vessels. To limit recurrent bleeds, topical antiseptic cream (Naseptin) or petroleum jelly (Vaseline) can be prescribed, although its efficacy is questionable.22 Patients with high blood pressure on admission need assessment by their general practitioner after discharge from hospital. Patient medication, especially anticoagulants, raise concerns in management; although a prospective study showed warfarin does not need to be stopped if its levels are within therapeutic range.23 Aspirin medication has been shown to be independently associated with epistaxis hospitalisation.24 However, cessation of aspirin therapy should be weighed up against thromboembolic complications and the time delay between stopping aspirin and the return of normal platelet function.
OTHER MANAGEMENT OPTIONS
Angiographic embolisation Sokoloff first undertook angiographic embolisation for epistaxis in 1972.13 Embolisation is routinely performed in some centres as a means of treating intractable epistaxis. The technique entails cannulation of the external carotid artery and location of the bleeding point by water soluble contrast. Coils, gel foam, and polyvinyl alcohol can then embolise the causative artery. The success rate has been reported to be as high as 87%, which is similar to arterial ligation.14 The techniques limiting factors include; lack of specialist radiologists and equipment, the inability to embolise ethmoidal arteries because of the risk of blindness, false aneurysm development at the insertion site, cerebrovascular accidents, and imaging difficulties after nasal packing. Studies have reported a complication rate of 17%27%.15 Fibrin glue Fibrin glue is developed from human plasma cryoprecipitate and binds itself to damaged vessels. The technique entails spraying a thin layer of glue over the bleeding site and can be repeated as needed. A recent randomised trial has reported that complications of local swelling, nasal mucosa atrophy, and excessive nasal discharge were lower than the electrocautery, silver nitrate, and nasal packing group. The rebleed rate was 15%, which is comparable to electrocautery.16 Endoscopic electrocautery The invention of the Hopkins rod in 1960s has revolutionised nasal surgery. Only recently has this new technology been adapted for the treatment of epistaxis (fig 4).1719 The nose should be prepared as described previously. Examination of the nasal cavity is performed using a rigid Hopkins rod endoscope (0 or 30 angle). Clots are removed using suction, which will also elicit the bleeding point. It is good practice to adopt a routine when examining the nasal cavity, viewing the septum first. On location of the bleeding point, electrocautery is used to seal the vessel. The authors recommend a bipolar cautery device with integrated suction tip to improve the field of view and increase efficiency of the cautery. Nasal packing is only instigated if the bleeding fails to cease after the procedure or if the bleeding point cannot be identified. The patient should be kept under observation for two hours and can be discharged home if no re-bleeding occurs. A recent study showed that this procedure was successful in treating 89% of patients with epistaxis with 74% not requiring admission.19 This reduction in the need for admission, added to the benefits of not inserting a pack, makes it a useful and cost effective procedure.
CONCLUSIONS
Over the past 10 years, there has been a significant expansion in the options available for the management of epistaxis. Traditional strategies like nasal packing have been supplemented by modern technology using the latest optic and electrical devices. Treatment should ideally use a systematic protocol, such as described in this review; starting with simple procedures that can be undertaken in the clinic environment and proceeding to endoscopic techniques for more difficult cases.
Figure 4 Endoscopic electrocautery equipment.
www.postgradmedj.com
314
Pope, Hobbs
Key references
(B) (C) (D) (E)
N N N N N
Watkinson JC. Epistaxis. In: Mackay IS, Bull TR, eds. Scott Browns otolaryngology. London: Butterworths, 1997:18/57. Burton M, Doree C. Interventions for recurrent idiopathic epistaxis (nosebleeds) in children. Cochrane Library. Issue 1. Oxford: Update Software, 2004. Shin EJ, Murr AH. Managing epistaxis. Curr Opin Otolaryngol Head Neck Surg 2000;8:3742. Stankiewicz JA. Nasal endoscopy and control of epistaxis. Curr Opin Otolaryngol Head Neck Surg 2004;12:435. Ahmed A, Woolford TJ. Endoscopic bipolar diathermy in the management of epistaxis: an effective and costefficient treatment. Clin Otolaryngol 2003;28:273 275.
Hot water irrigation is used for anterior bleeds Patients are normally admitted after endoscopic electrocautery A 0 Hopkins rod is used in rigid endoscopy Bleeding recurs in 50% of cases when using fibrin glue
.....................
Authors affiliations
L E R Pope, Department of Otolaryngology and Head and Neck Surgery, Addenbrookes Hospital, Cambridge, UK C G L Hobbs, Department of Otolaryngology and Head and Neck Surgery, St Michaels Hospital, Bristol, UK Funding: none. Competing interests: none.
REFERENCES
1 Petruson B, Rudin R. The frequency of epistaxis in a male population sample. Rhinology 1975;13:12933. 2 Watkinson JC. Epistaxis. In: Mackay IS, Bull TR, eds. Scott Browns otolaryngology. London: Butterworths, 1997;18/57. 3 Thaha MA, Nilssen EL, Holland S, et al. Routine coagulation screening in the management of emergency admission for epistaxisis it necessary? J Laryngol Otol 2000;114:3840. 4 Corbridge RJ, Djazaeri B, Hellier WP, et al. A prospective randomised controlled trial comparing the use of merocel nasal tampons and BIPP in the control of acute epistaxis. Clin Otolaryngol 1995;20:3057. 5 Holland NJ, Sandhu GS, Ghufoor K, et al. The Foley catheter in the management of epistaxis. Int J Clin Pract 2001;55:1415. 6 Schietroma JJ, Tenzel RR. The effects of cautery on the optic nerve. Ophthal Plast Reconstr Surg 1990;6:1027. 7 Green KM, Board T, OKeeffe LJ. Oculomotor nerve palsy following submucosal diathermy to the inferior turbinates. J Laryngol Otol 2000;114:2856. 8 OFlynn PE, Shadaba A. Management of posterior epistaxis by endoscopic clipping of the sphenopalatine artery. Clin Otolaryngol 2000;25:3747. 9 Woolford TJ, Jones NS. Endoscopic ligation of anterior ethmoidal artery in treatment of epistaxis. J Laryngol Otol 2000;114:85860. 10 Douglas SA, Gupta D. Endoscopic assisted external approach anterior ethmoidal artery ligation for the management of epistaxis. J Laryngol Otol 2003;117:1323. 11 Strong EB, Bell DA, Johnson LP, et al. Intractable epistaxis: transantral ligation vs. embolization: efficacy review and cost analysis. Otolaryngol Head Neck Surg 1995;113:6748. 12 Spafford P, Durham JS. Epistaxis: efficacy of arterial ligation and long-term outcome. J Otolaryngol 1992;21:2526. 13 Sokoloff J, Wickbom I, McDonald D, et al. Therapeutic percutaneous embolization in intractable epistaxis. Radiology 1974;111:2857. 14 Vitek J. Idiopathic intractable epistaxis: endovascular therapy. Radiology 1991;181:11316. 15 Tseng EY, Narducci CA, Willing SJ, et al. Angiographic embolization for epistaxis: a review of 114 cases. Laryngoscope 1998;108:61519. 16 Vaiman M, Segal S, Eviatar E. Fibrin glue treatment for epistaxis. Rhinology 2002;40:8891. 17 Frikart L, Agrifoglio A. Endoscopic treatment of posterior epistaxis. Rhinology 1998;36:5961. 18 McGarry GW. Nasal endoscope in posterior epistaxis: a preliminary evaluation. J Laryngol Otol 1991;105:42831. 19 Ahmed A, Woolford TJ. Endoscopic bipolar diathermy in the management of epistaxis: an effective and cost-efficient treatment. Clin Otolaryngol 2003;28:2735. 20 Shin EJ, Murr AH. Managing epistaxis. Curr Opin Otolaryngol Head Neck Surg 2000;8:3742. 21 Stankiewicz JA. Nasal endoscopy and control of epistaxis. Curr Opin Otolaryngol Head Neck Surg 2004;12:435. 22 Burton M, Doree C. Interventions for recurrent idiopathic epistaxis (nosebleeds) in children. Cochrane Library. Issue 1. Oxford: Update Software, 2004. 23 Srinivasan V, Patel H, John DG, et al. Warfarin and epistaxis: should warfarin always be discontinued? Clin Otolaryngol 1997;22:5424. 24 Tay HL, Evans JM, McMahon AD, et al. Aspirin, nonsteroidal antiinflammatory drugs, and epistaxis. A regional record linkage case control study. Ann Otol Rhinol Laryngol 1998;107:6714.
MULTIPLE CHOICE QUESTIONS (TRUE (T)/FALSE (F); ANSWERS AT END OF REFERENCES)
1. (A) (B) (C) (D) (E) 2. (A) (B) (C) (D) (E) 3. (A) (B) (C) (D) (E) 4. (A) (B) (C) (D) (E) 5. (A) Possible causes of epistaxis include: Nasotracheal intubation Disseminated intravascular coagulation (DIC) Hyperthyroidism Scurvy Pseudogout (chondrocalcinosis) The following steps are appropriate in the management of an 80 year old man with acute epistaxis: Pressure should be applied to the bridge of the nose to help stop bleeding After resuscitation, he should be examined in theatre under general anaesthetic A full blood count should be performed There is no need to check for ongoing bleeding if an anterior pack is inserted If he lives alone, he can be discharged home with a merocel nasal tampon in situ The following are recognised complications of nasal packing: Septal perforation Aspiration Hypoxia Optic nerve damage Epiphora In surgery for epistaxis: Local anaesthesia can be used for elderly patients Bipolar diathermy is safer The maxillary artery is normally approached endoscopically Removing a septal spur may help Ligation of the external carotid artery is useful as a last resort In the alternative management options for epistaxis: Angiographic embolisation has a similar success rate to arterial ligation
ANSWERS
1. T, (B) T, (C) F, (D) T, (E) F; 2. F, (B) F, (C) T, (D) F, (E) F; 3. F, (B) T, (C) T, (D) F, (E) T; 4. T, (B) T, (C) F, (D) T, (E) T. 5; T, (B) F, (C) F, (D) T, (E) F.
www.postgradmedj.com
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Hal 1-4Documento8 páginasHal 1-4Fika Khulma SofiaAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- 3553 FullDocumento10 páginas3553 FullFika Khulma SofiaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Case Headache On PregnancyDocumento5 páginasCase Headache On PregnancyFika Khulma SofiaAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Morning Report Februari 2016: A 36-Year-Old-Man With Moderate Acute Asthma DD Acis DD CopdDocumento14 páginasMorning Report Februari 2016: A 36-Year-Old-Man With Moderate Acute Asthma DD Acis DD CopdFika Khulma SofiaAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Dapusimun 1Documento7 páginasDapusimun 1Fika Khulma SofiaAinda não há avaliações
- 3553 FullDocumento10 páginas3553 FullFika Khulma SofiaAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Hal 58-62Documento9 páginasHal 58-62Fika Khulma SofiaAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Tambahan ImunologiDocumento5 páginasTambahan ImunologiFika Khulma SofiaAinda não há avaliações
- Psikimetab10 2012Documento2 páginasPsikimetab10 2012Fika Khulma SofiaAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Costa MDocumento1 páginaCosta MFika Khulma SofiaAinda não há avaliações
- InTech - Mechanisms in Erectile Function and Dysfunction An OverviewDocumento21 páginasInTech - Mechanisms in Erectile Function and Dysfunction An OverviewFika Khulma SofiaAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Interpreting D DimerDocumento8 páginasInterpreting D DimerFika Khulma SofiaAinda não há avaliações
- Abstrak DR SariDocumento2 páginasAbstrak DR SariFika Khulma SofiaAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Venous Air Embolism During Anterior Lumbar Surgery: Case ReportDocumento3 páginasVenous Air Embolism During Anterior Lumbar Surgery: Case ReportFika Khulma SofiaAinda não há avaliações
- CRD 8Documento7 páginasCRD 8Fika Khulma SofiaAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Incidence of Venous Air Embolism During Craniectomy For Craniosynostosis RepairDocumento4 páginasIncidence of Venous Air Embolism During Craniectomy For Craniosynostosis RepairFika Khulma SofiaAinda não há avaliações
- Jurnal Vian 4Documento12 páginasJurnal Vian 4Fika Khulma SofiaAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Evolving Role of Hysterectomy in Gestational Trophoblastic Neoplasia at The New England Trophoblastic Disease CenterDocumento2 páginasThe Evolving Role of Hysterectomy in Gestational Trophoblastic Neoplasia at The New England Trophoblastic Disease CenterFika Khulma SofiaAinda não há avaliações
- Jurnal Vian 4Documento12 páginasJurnal Vian 4Fika Khulma SofiaAinda não há avaliações
- Venembol 2Documento19 páginasVenembol 2Fika Khulma SofiaAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- CRD 6Documento7 páginasCRD 6Fika Khulma SofiaAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- CRD 9Documento12 páginasCRD 9Fika Khulma SofiaAinda não há avaliações
- CRD 1Documento2 páginasCRD 1Fika Khulma SofiaAinda não há avaliações
- Br. J. Anaesth.-2012-S Rensen-682-9Documento8 páginasBr. J. Anaesth.-2012-S Rensen-682-9Fika Khulma SofiaAinda não há avaliações
- Cardioplegia in Pediatric Cardiac Surgery: Do We Believe in Magic?Documento12 páginasCardioplegia in Pediatric Cardiac Surgery: Do We Believe in Magic?Fika Khulma SofiaAinda não há avaliações
- Spinal 6Documento3 páginasSpinal 6Fika Khulma SofiaAinda não há avaliações
- Time Course of Elevations in Plasma Olprinone Concentration During Pediatric Cardiac SurgeryDocumento4 páginasTime Course of Elevations in Plasma Olprinone Concentration During Pediatric Cardiac SurgeryFika Khulma SofiaAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Single Dose Inamrinone in Terminal Warm Cardioplegia in On-Pump Coronary Artery Bypass PatientsDocumento5 páginasSingle Dose Inamrinone in Terminal Warm Cardioplegia in On-Pump Coronary Artery Bypass PatientsFika Khulma SofiaAinda não há avaliações
- 2 Myocardial Protection in Pediatric Cardiac SurgeryDocumento6 páginas2 Myocardial Protection in Pediatric Cardiac SurgeryFika Khulma Sofia100% (1)
- Practice Essentials: Essential Update: Chemotherapy Following Radiation May Improve Survival in Low-Grade GliomasDocumento19 páginasPractice Essentials: Essential Update: Chemotherapy Following Radiation May Improve Survival in Low-Grade GliomasFika Khulma SofiaAinda não há avaliações
- Identifyingandmanagingacutestroke 150520143046 Lva1 App6892Documento62 páginasIdentifyingandmanagingacutestroke 150520143046 Lva1 App6892Raghu NadhAinda não há avaliações
- Nursing Care Plan (CVA)Documento2 páginasNursing Care Plan (CVA)Mel Rodolfo50% (2)
- LBP 1 PDFDocumento10 páginasLBP 1 PDFGusti Ayu KrisnayantiAinda não há avaliações
- Good Radio Pharmacy Practice - OriginalDocumento34 páginasGood Radio Pharmacy Practice - OriginalTusvedran PillaiAinda não há avaliações
- Cert Yoga - Therapy - Diploma - Reference - Spring - 2021FINAL 5Documento13 páginasCert Yoga - Therapy - Diploma - Reference - Spring - 2021FINAL 5E. AAinda não há avaliações
- Ob Management Septic AbortionDocumento8 páginasOb Management Septic AbortionspringdingAinda não há avaliações
- Burnout Among NursesDocumento6 páginasBurnout Among NursesYousef KhalifaAinda não há avaliações
- 10 Ways To Boost Your Emotional Health Through Improving Your SelfDocumento6 páginas10 Ways To Boost Your Emotional Health Through Improving Your SelfDOLORES LEE CORPUZAinda não há avaliações
- Medicated Nail Lacquers - For Effective Treatment of Nail DisordersDocumento12 páginasMedicated Nail Lacquers - For Effective Treatment of Nail DisordersBaru Chandrasekhar RaoAinda não há avaliações
- Pain As 5th Vital SignDocumento70 páginasPain As 5th Vital SignPoornima GopalAinda não há avaliações
- KATH - DCH Treatment GuidelinesDocumento173 páginasKATH - DCH Treatment GuidelinesCarterine ListAinda não há avaliações
- Hydrocollator Pack ApplicationDocumento4 páginasHydrocollator Pack ApplicationSreeraj S R100% (1)
- Adult Lead PoisoningDocumento14 páginasAdult Lead PoisoningyhonangelAinda não há avaliações
- Nerve Injuries: Radial Nerve, Median Nerve and Ulnar NerveDocumento26 páginasNerve Injuries: Radial Nerve, Median Nerve and Ulnar NerveaisiyaahAinda não há avaliações
- Surehands LMNDocumento1 páginaSurehands LMNapi-383151067Ainda não há avaliações
- Case Study Presentation - CGDocumento37 páginasCase Study Presentation - CGapi-290866384Ainda não há avaliações
- Post-Stroke Rehabilitation English Brochure 508CDocumento24 páginasPost-Stroke Rehabilitation English Brochure 508CAnonymous Ezsgg0VSEAinda não há avaliações
- Walsall Medical PosterDocumento1 páginaWalsall Medical Posterlaur_rbAinda não há avaliações
- New IG SubclassDocumento13 páginasNew IG SubclassBrîndușa PetruțescuAinda não há avaliações
- Dr. S.P. Hewawasam (MD) Consultant Gastroenterologist/Senior Lecturer in PhysiologyDocumento33 páginasDr. S.P. Hewawasam (MD) Consultant Gastroenterologist/Senior Lecturer in PhysiologyAjung SatriadiAinda não há avaliações
- ACT: A Brief Intervention To Reduce ProcrastionDocumento14 páginasACT: A Brief Intervention To Reduce ProcrastionCamAinda não há avaliações
- Referat asma-PARUDocumento26 páginasReferat asma-PARUPutri Andansari100% (1)
- Lange Q&A: Radiography ExaminationDocumento18 páginasLange Q&A: Radiography ExaminationSamuel JeebanAinda não há avaliações
- Spitzer 1981Documento13 páginasSpitzer 1981Chima2 SantosAinda não há avaliações
- Brochure Gelofusine Ef PDFDocumento4 páginasBrochure Gelofusine Ef PDFJeshwinder KaurAinda não há avaliações
- Acute Wound CareDocumento0 páginaAcute Wound CareMihaela MitroiAinda não há avaliações
- Office of The Secretary: Administrative Order 2017Documento12 páginasOffice of The Secretary: Administrative Order 2017Paula ValeraAinda não há avaliações
- Evelyn M Monahan The Miracle of Metaphysical Healing PDFDocumento224 páginasEvelyn M Monahan The Miracle of Metaphysical Healing PDFdidinbinyohousekeep100% (7)
- Antihistamines Case StudyDocumento5 páginasAntihistamines Case StudySpaynkterAinda não há avaliações
- Book Review of Practical Counselling and Helping Skills - Chapter 16Documento3 páginasBook Review of Practical Counselling and Helping Skills - Chapter 16woanling leeAinda não há avaliações
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNo EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedNota: 5 de 5 estrelas5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossNo EverandThe Obesity Code: Unlocking the Secrets of Weight LossNota: 4 de 5 estrelas4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNo EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDNota: 5 de 5 estrelas5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNota: 2 de 5 estrelas2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (26)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNo EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisNota: 4.5 de 5 estrelas4.5/5 (42)