Escolar Documentos
Profissional Documentos
Cultura Documentos
Risk Factors Associated With Adverse Outcomes in A Population-Bgfytyased
Enviado por
Baskoro MahendraTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Risk Factors Associated With Adverse Outcomes in A Population-Bgfytyased
Enviado por
Baskoro MahendraDireitos autorais:
Formatos disponíveis
Journal of Diabetes and Its Complications 21 (2007) 341 349
Risk factors associated with adverse outcomes in a population-based prospective cohort study of people with their first diabetic foot ulcer
Kirsty Winkley a,, Daniel Stahl b , Trudie Chalder a , Michael E. Edmonds c , Khalida Ismail a
a
Department of Psychological Medicine, Institute of Psychiatry, King's College London, Weston Education Centre, SE5 9RJ London, UK b Department of Biostatistics, Institute of Psychiatry, King's College London, De Crespigny Park, SE5 8AZ London, UK c Diabetic Foot Clinic, King's College Hospital, Denmark Hill, SE5 9RS London, UK Received 13 June 2007; received in revised form 13 August 2007; accepted 6 September 2007
Abstract Aims/Hypothesis: The aim of this study was to determine which clinic-based measures of diabetes and foot status at baseline were associated with adverse outcomes 18 months later in people with diabetes presenting with their first foot ulcer. Subjects and Methods: This was a prospective population-based cohort study of adults with type 1 and type 2 diabetes mellitus presenting with their first foot ulcer (excluding those with severe ischaemia, ankle brachial pressure index b0.5). The main explanatory variables were age, sex, smoking status, ulcer site (dorsal or plantar), size and severity of ulcer, severity of neuropathy, ischaemia, glycosylated haemoglobin, presence of micro- and macrovascular complications, and depression. The main outcomes recorded were death, amputation and recurrence of ulceration, and the time taken for each outcome to occur. Results: Two hundred fifty-three people were recruited. There were 40 deaths (15.8%), 36 amputations (15.5%), and 99 recurrences (43.2%) at 18 months. Our main findings were that being older [hazard ratio (HR) 1.07, 95% CI 1.041.11], having lower glycosylated haemoglobin (HR 0.73, 95% CI 0.560.96), moderate ischaemia (HR 2.74, 95% CI 1.465.14), and depression (HR 2.51, 95% CI 1.334.73) were associated with mortality. Ulcer severity was the only explanatory factor significantly associated with amputation (HR 3.18, 95% CI 1.536.59). Microvascular complications were the only explanatory factor associated with recurrent ulceration (HR 3.34, 95% CI 1.179.56). Conclusions/Interpretation: Commonly used primary and secondary care clinic-based measures could provide the basis for a risk assessment tool for adverse outcomes following first presentation of diabetic foot ulcers. 2007 Elsevier Inc. All rights reserved.
Keywords: Diabetic foot; Clinical diabetes; Peripheral arterial disease; Cohort study
1. Introduction Adverse outcomes are common in people with diabetic foot ulcers. Survival is reduced (Ramsey et al., 1999), and foot ulcers precede almost all lower extremity amputations (Wrobel, Mayfield, & Reiber, 2001). Costs of treating diabetic foot ulcers increase dramatically if patients require inpatient care (Harrington, Zagari, Corea, & Klitenic, 2000; Van Acker et al., 2000) and represent a substantial drain on
Corresponding author. Tel.: +44 20 3299 1739; fax: +44 20 3299 1730. E-mail address: kirsty.winkley@nhs.net (K. Winkley). 1056-8727/07/$ see front matter 2007 Elsevier Inc. All rights reserved. doi:10.1016/j.jdiacomp.2007.09.004
health service resources. Sparse qualitative research suggests that diabetic foot ulceration has a profound social impact with patients reporting stigma, social isolation, loss of social role, and unemployment (Croxson, 2002; Douglas, 2001; Fox, 2005). Quality of life is also reduced (NabuursFranssen, Huijberts, Nieuwenhuijzen Kruseman, Willems, & Schaper, 2005; Vileikyte, 2001), and recent findings suggest that depression is more prevalent (Carrington, Mawdsley, Morley, Kincey, Boulton, 1996; Ismail, Winkley, Stahl, Chalder, & Edmonds, 2007) than in general diabetes. There is a general consensus that successful treatment of foot ulcers involves multidisciplinary management following an agreed protocol, such as education (Barth, Campbell, Allen, Jupp, & Chisholm, 1991), regular debridement, wound
342
K. Winkley et al. / Journal of Diabetes and Its Complications 21 (2007) 341349
dressing, and pressure relief plus management of factors that may compromise healing (Edmonds & Foster, 2000). However, the availability and quality of treatment is dependent on service provision (Edmonds, 2004) and may vary across regions (Canavan, Connolly, Airey, Burden, & Unwin, 2003). There remains a need to translate risk factors identified in studies into simple risk assessment tools which can be used by nonspecialist clinicians especially in the early stages of diabetic foot disease. Prospective studies have examined risk factors for ulceration in people with diabetes (Abbott et al., 2002; Boyko et al., 1999) and also risk factors for and rates of new ulceration, amputation, and mortality in people hospitalised for diabetic foot ulcer (Faglia, Favales, & Morabito, 2001) and those attending outpatient diabetic foot clinics (Apelqvist, Larsson, & Agardh, 1993). The multicentre Eurodiale cohort study has demonstrated a high prevalence of baseline ischaemia, infection, and comorbidity in Europeans with new-onset diabetic foot ulcers, whether hospitalised or not (Prompers et al., 2007). Psychological factors, such as depressive disorders, are increasingly being recognised as prognostic factors associated with increased mortality in people with diabetes (Katon et al., 2005; Zhang et al., 2005), and in people with their first foot ulcer, we found that there is a threefold increased risk of death (Ismail et al., 2007). However, incorporating psychological risk factors in a risk assessment for adverse outcomes in diabetic foot disease has not been studied; there are relatively simple measures for screening for depression, and it is a treatable condition. Using the same cohort as previously reported (Ismail et al., 2007), the aim of this study is to determine whether commonly used clinic-based measures of diabetes and the foot are associated with adverse outcomes at 18 months in people with first foot ulcers presenting at hospital foot and community chiropody clinics in south London, UK. Examination of potential clinical risk factors following first ulceration may provide health professionals, who do not have specialist foot knowledge, with an easy to use risk assessment guide for the diabetic foot.
defined according to the World Health Organization (WHO) criteria. Informed consent was obtained for each participant, and ethical approval was obtained through local ethics committees of the participating centres. A clinically significant case definition of diabetic foot ulcer was used: (i) the ulceration was in the anatomical foot; (ii) there was a full thickness break in the epithelium with a minimum width of 5 mm; and (iii) to exclude severely ischaemic feet, the ankle:brachial ratio was N0.5 and no greater than 1.5 (to exclude those with potential calcification of the medial arteries) at either the dorsalis pedis or posterior tibial sites using Doppler pressure readings. When subjects had more than one ulcer at first presentation, the largest ulcer was defined as the baseline ulcer. Subjects whose first ulcer healed within 3 months from the start of the study were included. Any first diabetic foot ulcers with duration of greater than 1 year at recruitment were excluded to reduce effects of chronicity on adverse outcome. The exclusion criteria were (i) not being fluent in English; (ii) current independent comorbid medical condition (such as rheumatoid arthritis); and (iii) severe mental illness, such as schizophrenia, other psychoses, dementia. 2.1. Measures At baseline, general demographics and diabetes-specific information were recorded for all participants. Clinical factors such as the severity of the ulcer, including ulcer size, and the degree of neuropathy and ischaemia were measured at baseline. Size was determined using digital imaging (Rajbhandari, Harris, Sutton, Lockett, Eaton, 1999). Images were resized using the AutoCAD R14 software (Microsoft) so that the surface area of the ulcer could be calculated in square centimeters. The severity of the ulcer was determined using the University of Texas Diabetic Wound Classification System (Armstrong, Lavery, Harkless, 1998). Wounds extending through the epidermis or dermis only were coded as superficial. Wounds penetrating tendons, joint capsule, bone, or joint were coded as severe. Two qualified podiatrists (one community, one hospital-based) independently graded the wounds from the digital photographs. Discussion of the images took place between senior podiatrists at the King's College Hospital foot clinic where there was disagreement until a consensus was reached. Duration of ulceration was recorded from first presentation (using medical records) to the date of recruitment. The degree of ischaemia was assessed using the ankle brachial pressure index (ABPI). A handheld Doppler was used to identify the foot pulses (MultiDopplex, Huntleigh Diagnostics, Huntleigh Healthcare, Unit 35, Portmanmoor Road, Cardiff, UK) and measure the brachial and ankle systolic pressure together with a sphygmanometer. Assessment of protective pain sensation and sensory neuropathy was made using a neurosthesiometer (Neurosthesiometer, Scientific Lab supplies, Wilford Industrial Estate, Ruddington Lane, Wilford, Nottingham, UK). In this study, we defined
2. Subjects, materials, and methods This was a prospective population-based cohort design with four time points: baseline, 6, 12, and 18 months. The setting was all the community chiropody and hospital foot clinics within 5 National Health Service health authorities in South London, UK (Lambeth, Southwark, Lewisham, Croydon, and Greenwich), which has approximately 80 000 people with diabetes. Between October 2001 and February 2003, adults with type 1 or type 2 diabetes and presenting with their first (baseline) diabetic foot ulcer were identified through fortnightly contact with each participating clinic and review of previous fortnight's records using a standardised checklist of case definition and exclusion criteria for all current and all new patients. Diabetes was
K. Winkley et al. / Journal of Diabetes and Its Complications 21 (2007) 341349
343
participants with a vibration perception threshold (VPT) of 25 V as neuropathic regardless of their age. Glycosylated hemoglobin was measured at baseline and at 12 and 18 months, as blood glucose levels may fluctuate markedly throughout 18 months and there is likely to be a close temporal relationship between high blood sugars and adverse outcomes (Jeffcoate, 2004). The mean percentage of glycosylated haemoglobin values were derived from baseline and 12 and 18 months to capture the assumed close temporal association between glycaemic control and risk of ulceration. Values were obtained using the Primus Ultra 2, Primus, Kansas City, MO, USA, and were Diabetes Control and Complications Trial-standardised (Colman, Goodall, Garcia-Webb, Williams, & Dunlop, 1997; Little, Rohlfing, & Wiedmeyer, 2001). Macrovascular complications were defined as prior myocardial infarct, coronary angioplasty, coronary artery bypass, and peripheral angioplasty or cerebrovascular accident. Microvascular complications were defined as retinopathy (background or proliferative) measured using digital fundal examination, nephropathy (macroalbuminuria or on dialysis) and neuropathy (VPT 25 V). The WHO's SCAN 2.1 (WHO, 1997) was administered to the patients at baseline to determine the presence or absence of minor and major depressive disorder according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSMIV) criteria. The SCAN 2.1 is a semistructured comprehensive diagnostic interview allowing the interviewer to make a clinical judgement to distinguish between psychiatric and physical basis of symptoms such as weight loss and fatigue. It is superior to rating scales as it provides a diagnosis of depression and other psychiatric disorders, using operational criteria based on accepted psychiatric classification systems such as the DSM-IV [and/or International Classification of Diseases, Tenth Revision (ICD-10)] using computerised algorithms (APA, 2000; elik, 1999). It has acceptable reliability and validity (Rijinders et al., 2000). Interrater reliability of the SCAN 2.1 was acceptable for this study and has been described previously (Ismail et al., 2007). The main confounders included were age and sex and substance use. The Alcohol Use Disorders Identification Test was used to classify patients who reported hazardous and harmful alcohol consumption; those scoring above 8 were defined as having an alcohol problem (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). Patients were coded as non- or ex-smoker vs. smokers. 2.2. Outcomes The three clinical outcomes recorded were death, first amputation, and first recurrent ulceration. The date and cause of death were obtained through the UK Central Register Office and coded according to ICD-10 codes (WHO, 1992). The podiatrist attending the patient recorded the date of first amputation, first recurrent ulceration, and date of healing. Amputation was defined as surgical removal of all or part
of lower limb and stratified as above and below the anatomical ankle. Recurrence of foot ulcers was defined as a recurrence of a full thickness break in the epithelium with a minimum width of 5 mm at the same or different site to the baseline ulcer. 2.3. Statistical analysis The main baseline characteristics of the sample were computed using percentage proportions or means and their S.D. Patients who refused to participate in the study, exclusions, and withdrawals were compared with the study sample using independent samples t tests to compare means and Fisher's Exact test to compare frequencies (Cochran, 1954). Survival was modelled from time of entry into the study up until the date of the 18-month follow-up. Those who did not die (n=213) were censored 18 months from their date of entry. Log-rank tests were used to compare the distribution of survival times between those who had amputations and recurrent ulcers with those who did not. Cox proportional hazards regression was used to measure the hazard ratios (HR) of the clinical factors on survival and the other adverse outcomes (Cox and Oates, 1984). Factors were first investigated with a univariable approach. Following this, multivariable Cox models were used to examine the effect of age and sex on adverse outcome (Model 1) and Model 1 plus relevant clinical variables identified from the univariable analysis, including smoking and depression (Model 2). Robust standard errors were used to adjust for potential misspecification of the models (Cleves, 2004). 3. Results Two hundred sixty-two people presented with their first diabetic foot ulcer during the study period, and all were invited to participate in the study. Two were excluded because they did not meet the inclusion criteria; one had a recurrent foot ulcer and the other did not speak English fluently. Seven people contacted refused to participate, and three withdrew from the study after completing the baseline interview and assessments. All three withdrawals agreed that outcome data could be collected but did not want to complete any further questionnaires. When refusers (n=7) were compared with the study sample, they were older than participants [69.8 (S.D. 12.0) vs. 62.0 (S.D. 13.9) years, P=.9], but this was not significant and more likely to be female (85.7% vs. 36.4%, P=.01), and this was significant. Our follow-up rate was 100% for mortality outcome, 92.0% and 90.5% for amputation (n=233) and recurrence (n=229), respectively. For amputation and recurrence, people with missing information had, in general, a shorter duration of diabetes (P=.02 and P=.05, respectively) and less microvascular problems (P=.01 and P=.02, respectively). There
344
K. Winkley et al. / Journal of Diabetes and Its Complications 21 (2007) 341349
were six patients for whom there was no glycosylated haemoglobin measure at any time point. 3.1. Baseline characteristics The clinical characteristics of the 253 participants who met the inclusion criteria and agreed to participate in the study can be found in Table 1. The majority of the sample were male and had Type 2 diabetes. The average duration of diabetes was more than 14 years. There were equal numbers of participants treated with oral hypoglycaemic agents and
insulin. Diabetes control of the sample was suboptimal. Most participants had superficial ulcers, i.e., not penetrating to the joint capsule, tendon, or bone; there were almost equal numbers of patients with ulcers N1 and 1 cm2; and just over half had dorsal ulcerations compared with plantar ulcerations. The majority of the sample had significant sensory neuropathy of the feet, as determined by neurosthesiometer to estimate the VPT. Almost 90% of the sample had one or more microvascular complications, and four people were on renal dialysis. A quarter of the sample had had previous cardiovascular problems documented in their medical notes
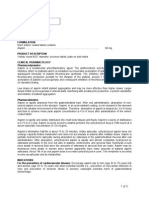
Table 1 Characteristics of the sample at baseline and univariable associations with adverse outcomes Total population (N=253) Explanatory variables Mean age (years) Sex Female Male Type of diabetes Type 1 Type 2 Treatment Insulin Tablet Current smoking status Non- or ex-smoker Smoker Alcohol problems None Yes Microvascular complications None 1 Macrovascular complications None 1 Mean duration of diabetes (years) Mean duration of ulcer (months) Mean glycated haemoglobin (%) Texas severity of ulcer Superficial Deep Mean ulcer size (cm2) 1 N1 Vibration perception threshold b25 V 25 V ABPI 0.9 0.5, b0.9 Location of ulcer Plantar Dorsal DSM-IV depression None Any Mean (S.D.) /no. (%) 62.0 (13.9) 92 (36.4) 161 (63.6) 43 (17.0) 210 (83) 114 (45.1) 139 (54.9) 213 (84.2) 40 (15.8) 214 (88.1) 29 (11.9) 32 (12.6) 221 (87.4) 185 (73.1) 68 (26.9) 14.7 (13.2) 3.1 (3.6) 8.2 (1.7) 188 (74.3) 65 (25.7) 123 (48.6) 130 (51.4) 47 (18.6) 206 (81.4) 193 (76.3) 60 (23.7) 111 (43.9) 142 (56.1) 171 (67.6) 82 (32.4) Mortality (n=40) HR (95% CI) 1.07 (1.041.09) 1 1.20 (0.622.32) 1 0.51 (0.181.40) 1 0.93 (0.481.79) 1 1.10 (0.502.43) 1 1.05 (0.422.62) 1 6.21 (0.8843.86) 1 2.35 (1.274.37) 1.01 (0.981.03) 1.05 (0.961.14) 0.67 (0.510.88) 1 2.36 (1.264.41) 1 1.46 (0.782.75) 1 3.10 (0.999.72) 1 3.81 (2.057.08) 1 1.11 (0.592.06) 1 2.24 (1.214.17) Amputation (n=36) HR (95% CI) 0.99 (0.971.01) 1 1.24 (0.622.48) 1 1.91 (0.933.89) 1 0.96 (0.491.86) 1 1.09 (0.472.57) 1 0.96 (0.342.75) 1 2.18 (0.548.84) 1 1.30 (0.652.58) 0.99 (0.971.02) 1.03 (0.951.12) 0.99 (0.811.19) 1 3.60 (1.886.91) 1 1.99 (1.003.96) 1 1.70 (0.614.72) 1 1.67 (0.833.33) 1 1.55 (0.783.12) 1 1.87 (0.973.61) Recurrence (n=99) HR (95% CI) 0.98 (0.960.99) 1 1.43 (0.932.19) 1 1.84 (1.142.95) 1 0.59 (0.390.89) 1 1.12 (0.661.91) 1 1.74 (0.993.07) 1 3.52 (1.289.67) 1 0.80 (0.511.25) 1.01 (0.991.03) 1.03 (0.981.09) 1.10 (0.991.22) 1 1.15 (0.741.79) 1 1.14 (0.771.69) 1 1.53 (0.822.84) 1 0.75 (0.451.24) 1 0.61 (0.410.90) 1 1.37 (0.902.06)
Abbreviations: HR=hazard ratio; ABPI=Ankle Brachial Pressure Index; DSM-IV=Diagnostic and Statistical Manual for Mental Disorders Fourth Edition.
K. Winkley et al. / Journal of Diabetes and Its Complications 21 (2007) 341349 Table 2 Primary causes of death (n=40) in a cohort of 253 people with their first diabetic foot ulcer Frequency (%) Total deaths Primary cause of death Cardiovascular diseases Cerebrovascular accident Infection Cancer Renal failure Complications from liver disease 40 (15.8) 10 (25.0) 10 (25.0) 14 (35.0) 4 (10.0) 1 (2.5) 1 (2.5) Male (%) 28 (70.0) 5 (50.0) 6 (60.0) 11 (78.6) 4 (100.0) 1 (100.0) 1 (100.0)
345
Mean age (S.D.) 71.80 (8.41) 69.0 (8.74) 71.0 (7.99) 71.93 (8.86) 80.75 (4.79) 72.0 70.0
Table 3 Multivariable associations of age and sex (Model 1) and clinical explanatory variables, including depression (Model 2), with adverse outcomes Mortality (n=40) Model 1 Explanatory variables Mean age (years) Sex Female Male Type of diabetes Type 1 Type 2 Treatment Insulin Tablet Current smoking status Non- or ex-smoker Smoker Alcohol problems None Yes Microvascular complications None 1 Macrovascular complications None 1 Mean duration of diabetes (years) Mean duration of ulcer (months) Mean glycated haemoglobin (%) Texas severity of ulcer Superficial Deep Mean ulcer size (cm2) 1 N1 VPT b25 V 25 V ABPI 0.9 0.5, b0.9 Location of ulcer Plantar Dorsal DSM-IV depression None Any HR (95% CI) 1.07 (1.041.09) 1 1.35 (0.672.73) Model 2 1.07 (1.041.11) 1 0.88 (0.411.89) Amputation (n=36) Model 1 HR (95% CI) 0.99 (0.971.01) 1 1.24 (0.632.47) Model 2 0.99 (0.971.02) 1 1.12 (0.562.26) Recurrence (n=99) Model 1 HR (95% CI) 0.98 (0.971.00) 1 1.43 (0.942.20) Model 2 0.99 (0.971.00) 1 1.42 (0.872.33) 1 0.84 (0.491.45) 1 0.69 (0.441.06) 1 1.36 (0.613.06) 1 0.88 (0.362.14) 1 1.16 (0.642.11)
1 3.34 (1.179.56) 1 1.11 (0.512.40) 0.73 (0.560.96) 1 1.70 (0.863.38) 1 3.18 (1.536.59) 1 1.40 (0.692.85) 1 1.80 (0.635.12) 1 2.74 (1.465.14) 1 0.68 (0.451.05) 1 2.51 (1.334.73) 1 1.38 (0.702.72) 1 1.18 (0.771.81)
346
K. Winkley et al. / Journal of Diabetes and Its Complications 21 (2007) 341349
(prior myocardial infarct, coronary angioplasty, coronary artery bypass, and peripheral angioplasty or cerebrovascular accident). Ischaemia was measured with the ABPI, and this showed that a quarter had moderate to severe ischaemia, but the majority were well perfused. 3.2. Mortality data and survival analyses Survival data were available for the entire sample. Forty participants died of natural causes during the course of the study, a survival rate of 84%. Table 2 shows the primary causes of death. Twenty-seven men (16.8%) died during the 18-month follow-up, and 13 women (14.1%) (Fisher's Exact test=0.14, P=.71). 3.3. Amputation Thirty-six (15.5%, n=233) participants underwent an amputation over the course of the study. All amputations were due to diabetic foot disease. Ten underwent major amputation (amputation above the ankle), and the remainder were minor amputations (below the ankle), mainly of the toes. Five (14%) of the 36 participants who underwent amputation died during the follow-up period, compared with 35 (18%) of the 197 who did not undergo amputation. Amputation was not significantly associated with survival (unadjusted HR 0.77, P=.58, 95% CI 0.301.96). 3.4. Recurrence Outcome data on recurrence of ulcer was available for 229 participants. Ninety-nine (43%) had a recurrence within 18 months. Seven (7%) of the 99 participants died after their first recurrence compared with 33 (26%) of the 130 participants who died but had no recurrence. Those who died but had recurrent ulceration survived longer than those who died with no recurrence (unadjusted HR 0.23, P=.001, 95% CI 0.100.53). 3.5. Clinical factors associated with mortality In a univariable analysis age, macrovascular complications, glycaemic control (% glycosylated haemoglobin), ulcer severity, neuropathy, and ischaemia were found to be associated with mortality (Table 1). In the first multivariable analysis (Model 1, Table 3), older age was still significantly associated with mortality but not sex. In Model 2 (Table 3), where clinical variables and depression were added, independent associations were found with ischaemia and better glycaemic control. 3.6. Clinical factors associated with amputation In a univariable analysis, ulcer severity and ulcer size were found to be associated with amputation (Table 1). In the first multivariable analysis (Model 1, Table 3), neither age
nor sex was significantly associated with amputation. In multivariable Model 2 (Table 3), where clinical variables and depression were added, an independent association was found with ulcer severity. 3.7. Clinical factors associated with ulcer recurrence In a univariable analysis age, type of diabetes, diabetes treatment, microvascular complications, and location of ulcer were found to be associated with recurrent ulceration (Table 1). In the first multivariable analysis (Model 1, Table 3), neither age nor sex was significantly associated with recurrent ulceration. In Model 2 (Table 3), where clinical variables and depression were added, an independent association was found with microvascular complications.
4. Discussion The aim of this prospective cohort study was to determine risk factors for adverse outcome in people with their first diabetic foot ulcer followed up for 18 months. Our main findings demonstrated that being older, having better glycaemic control, moderate ischaemia, and suffering from a depressive disorder were independent risk factors for mortality following first ulceration. Severity of ulcer was independently associated with amputation and microvascular complications were associated with recurrent ulceration. The strengths of this study include that it was a population-based cohort and had a prospective design, reducing selection bias and allowing for the temporal association between exposure and outcome to be determined. The outcomes measured were clinical and objective, and podiatrists were blind to depression status. Limitations of the study were that housebound patients with first ulcers would not have been identified, however, as patients were recruited from hospital and community clinics the results are likely to be generalisable to the population of foot ulcers as a whole. Diabetes control was suboptimal for the entire sample at baseline, and potential explanations for better control in the group who died might include increased surveillance and medical management of patients who were sicker and, second, that this group may have had more frequent hospitalisations and increased the likelihood of anorexia/ poor appetite. Previous cohorts (Boyko et al., 1999) have demonstrated that poor diabetes control is a risk factor for the development of foot ulcers, but to date, there have been no published data demonstrating a prospective association with adverse outcome following ulceration. Of greater clinical significance is the 3-fold increased risk of mortality in people with moderate ischaemia or peripheral arterial disease (PAD). In addition to coronary and carotid artery disease and hyperlipidaemia, PAD is considered to be a marker for artherosclerosis and is known to be more prevalent in people with diabetes (Jager et al., 1999; Pan et
K. Winkley et al. / Journal of Diabetes and Its Complications 21 (2007) 341349
347
al. 1986). Studies such as the Hoorn population cohort, which examined glucose disturbance in an elderly Dutch Caucasian population, have demonstrated independent associations between PAD and twofold increased risk of all-cause mortality at 5 years of follow-up (Jager et al., 1999). Hoorn defined PAD as ABPI b0.9, included those with absent foot pulses and found it was more prevalent amongst those with known diabetes (Beks et al., 1995). Similarly, in the Strong Heart study, a population cohort of American Indians investigating risk factors for cardiovascular disease (CVD), the relative risk of CVD mortality in people with PAD (ABPI b0.9) was 1.69 (Resnick et al., 2004). In our study people with severe PAD were excluded, and we found a 3-fold increased risk of death and in over 50% of cases death was due to cardiovascular cause. Amputation occurred to relatively few of the study participants, and the majority had minor amputations which may explain the absence of an association with depressive disorder (as perhaps minor is perceived as good news compared to having to undergo major amputation). Recurrent ulceration was not associated with depression and this may perhaps relate to how participants perceive reulceration, e.g., that it is not serious, especially as they already have impaired functioning from the first one and they have no or little pain sensation to match the worsening foot disease. Severity of ulcer was the only risk factor independently associated with amputation. Deep ulcerations were associated with a threefold increased risk. The absence of an independent association between PAD and amputation, found in previous cohort studies (Faglia et al., 2001; Jude, Oyibo, Chalmers, & Boulton, 2001), may be explained by the fact that this was a population of people with first ulcers, that the majority of amputations recorded were minor, and that people with severe PAD (ABPI b0.5) were excluded. A threefold increased risk of recurrent ulceration was found in participants with one or more microvascular complications. Sensory neuropathy alone, measured in this study with VPT, was not independently associated with recurrence, although associations with neuropathy (both subjective symptoms and VPT N25 V) have been described in cases with current or recent ulceration compared to diabetes controls without a history of ulceration (Lavery, Armstrong, Vela, Quebedeaux, & Fleischli, 1998). Neuropathy, measured by the 10-g monofilament, is a risk factor for the development of foot ulcers (Boyko et al., 1999). The absence of an independent association with reulceration in this study may have occurred, as only 50% of this population of people with diabetes and first ulcers met the criteria for neuropathy (VPT N25 V), although an independent association with any microvascular disease was present. This study may inform strategies to improve diabetic foot care for people with diabetes and their first ulcer. It demonstrates that measuring ABPI and monitoring depression status can help identify people at increased risk for
mortality, that the assessment of wound severity can determine amputation risk, and any microvascular complication can increase risk of recurrent ulceration. Mostly, these are simple measurements and can be done routinely in primary care. They depend on the use of low-tech and lowcost equipment, direct observation, and accurate recording of diabetes complications. Podiatrists, nurses, or general practitioners can therefore identify those at high risk for adverse outcomes in primary care, where the majority of diabetes care is delivered, and once high risk patients are identified, resources to modify their risk status can be more accurately targeted. To reduce mortality, this may involve intensification of treatment to reduce the impact of PAD (Antiplatelets Trialists' Collaboration, 1994; Beckman, Creager, & Libby, 2002) or at least manage associated problems such as coronary and carotid artery disease and hyperlipidaemia, with platelet antagonists, statins, and angiotensin-converting enzyme inhibitors, which may reduce vascular deaths (Antiplatelets Trialists' Collaboration, 1994) and strokes (Executive Committee for the Asymptomatic Carotid Artherosclerosis Study 1995; North American Symptomatic Carotid Endarterectomy Trial Collaborators 1991). Furthermore, routine monitoring of depression can also be performed and indeed in the United Kingdom, there is a national programme for screening for depression in all people with diabetes in primary care (Gilbody, Sheldon, & Wessely, 2006). We used a highly intensive semistructured interview, which is not suitable for diabetes professionals, but there are numerous screening and case finding measures available, such as the Patient Health Questionnaire 9 (Kroenke, Spitzer, & Williams, 2001). There may be local or national guidelines for the treatment of depression (NICE, 2004). To avoid amputation, those with severe first ulcers will require intensive treatment and follow-up in the foot clinic, and to prevent reulceration, patients with preexisting microvascular disease will require intensive monitoring.
References
Abbott, C. A., Carrington, A. L., Ashe, H., Bath, S., Every, L. C., Griffiths, J., Hann, H. W., Hussein, H., Jackson, N., Johnson, K. E., Ryder, C. H., Torkington, R., Van Ross, E. R., Whalley, A. M., Widdows, P., Williamson, S., & Boulton, A. J. (2002). The North-West Diabetes Foot Care Study: Incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabetic Medicine, 19, 377384. Antiplatelets Trialists' Collaboration. (1994). Collaborative overview of randomised trials of antiplatelet therapy, I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. British Medical Journal, 308, 81106. APA. (2000). Diagnostic and statistical manual of mental disorders, text revision (DSM-IV-TR). Arlington, VA: American Psychiatric Association. Apelqvist, J., Larsson, J., & Agardh, C. (1993). Long-term prognosis for diabetic patients with foot ulcers. Journal of Internal Medicine, 233, 485491.
348
K. Winkley et al. / Journal of Diabetes and Its Complications 21 (2007) 341349 nuria and peripheral arterial disease are independent predictors of cardiovascular and all-cause mortality, especially among hypertensive subjects: Five year follow-up of the Hoorn study. Arteriosclerosis Thrombosis and Vascular Biology, 19, 617624. Jeffcoate, S. (2004). Diabetes control and complications: The role of glycated haemoglobin, 25 years on. Diabetic Medicine, 21, 657665. Jude, E. B., Oyibo, S. O., Chalmers, N., & Boulton, A. J. M. (2001). Peripheral arterial disease in diabetic and nondiabetic patients. Diabetes Care, 24, 14331437. Katon, W. J., Rutter, C., Simon, G., Lin, E. H. B., Ludman, E., Ciechanowski, P., Kinder, L., Young, B., & Von Korff, M. (2005). The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care, 28, 26682672. Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606613. Lavery, L. A., Armstrong, D. G., Vela, S. A., Quebedeaux, T. L., & Fleischli, J. G. (1998). Practical criteria for screening patients at high risk for diabetic foot ulceration. Archives of Internal Medicine, 158, 157162. Little, R., Rohlfing, C., & Wiedmeyer, H. -M. (2001). The national glycohaemoglobin standardization program: A five-year progress report. Clinical Chemistry, 47, 19851992. Nabuurs-Franssen, M. H., Huijberts, M. S. P., Nieuwenhuijzen Kruseman, A. C., Willems, J., & Schaper, S. C. (2005). Health-related quality of life of diabetic foot ulcer patients and their care-givers. Diabetologia, 48, 19061910. NICE. (2004). Depression: Management of depression in primary and secondary care. London: National Institute of Clinical Excellence. North American Symptomatic Carotid Endarterectomy Trial Collaborators. (1991). Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. New England Journal of Medicine, 325, 445453. Pan, W. H., Cedres, L. B., et al. (1986). Relationship of clinical diabetes and asymptomatic hyperglycaemia to risk of coronary heart disease mortality in men and women. American Journal of Epidemiology, 123, 504516. Prompers, L., Huijberts, M., Apelqvist, J., Jude, E., Piaggesi, A., Bakker, K., Edmonds, M., Holstein, P., Jirkovska, A., Mauricio, D., RagnarsonTennvall, G., Reike, H., Spraul, M., Uccioli, L., Urbanic, V., Van Acker, K., Van Baal, J., Van Merode, F., & Schaper, N. (2007). High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia, 50, 1825. Rajbhandari, S., Harris, N., Sutton, M., Lockett, S., & Eaton, M. (1999). Digital imaging: An accurate and easy method of measuring foot ulcers. Diabetic Medicine, 16, 339342. Ramsey, S. D., Newton, K., Blough, D., McCulloch, D. K., Sandhu, N., Reiber, G. E., & Wagner, E. H. (1999). Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care, 22, 382387. Resnick, H. E., Lindsay, R. S., McCrae McDermott, M., Devereux, R. B., Jones, K. L., Fabsitz, R. R., & Howard, B. V. (2004). Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality. The Strong Heart Study. Circulation, 109, 733739. Rijinders, C., van der Berg, J., Hodiamont, P., Nienhuis, F. J., Furer, J. W., Mulder, J., & Giel, R. (2000). Psychometric properties of the schedules for clinical assessment in neuropsychiatry (SCAN-2.1). Social Psychiatry & Epidemiology, 35, 348352. Saunders, J., Aasland, O., Babor, T. F., de la Fuete, J. R., & Grant, M. (1993). Development of the Alcohol Use Disorders Test (AUDIT): WHO collaborative project on the early detection of persons with harmful alcohol consumption. Addiction, 88, 791804. Van Acker, K., Oleen-Burkey, L., De Decker, L., Vanmaele, R., Van Schil, P., Matricali, H., Dys, H., & De Leeuw, I. (2000). Cost and resource utilization for prevention and treatment of foot lesions in a diabetic foot clinic in Belgium. Diabetes Research & Clinical Practice, 50, 8795.
Armstrong, D. G., Lavery, L. A., & Harkless, L. B. (1998). Validation of a diabetic wound classification system. Diabetes Care, 21, 855859. Barth, R., Campbell, L. V., Allen, S., Jupp, J. J., & Chisholm, D. J. (1991). Intensive education improves knowledge, compliance and foot problems in type 2 diabetes. Diabetic Medicine, 8, 111117. Beckman, J. A., Creager, M. A., & Libby, P. (2002). Diabetes and artherosclerosis. Journal of the American Medical Association, 287, 25702581. Beks, P. J., Mackaay, A. J. C., Neeling, J. N. D., de Vries, H., Bouter, L. M., & Heine, R. J. (1995). Peripheral arterial disease in relation to glycaemic level in an elderly Caucasian population: The Hoorn study. Diabetalogia, 38, 8696. Boyko, E. J., Ahroni, J. H., Stensel, V., Forsberg, R. C., Davignon, D. R., & Smith, D. G. (1999). A prospective study of risk factors for the diabetic foot ulcer: The Seattle diabetic foot study. Diabetes Care, 22, 10361042. Canavan, R., Connolly, V., Airey, M., Burden, A. C., & Unwin, N. (2003). Geographic variation in lower extremity amputation rates. Diabetic Foot, 8289. Carrington, A. L., Mawdsley, S. K. V., Morley, M., Kincey, J., & Boulton, A. J. M. (1996). Psychological status of diabetic people with or without lower limb disability. Diabetes Research and Clinical Practice, 32, 1925. elik, C. (1999). I-Shell SCAN. Computer assisted personal interviewing application for the Schedules for Clinical Assessment in Neuropsychiatry Version 2.1 and diagnostic algorithms for WHO ICD-10. Chapter V DCR and for American Psychiatric Association Diagnostic and Statistical Manual Version IV. Geneva: World Health Organization. Cleves, M. (2004). Introduction to survival analysis using STATA. Texas: Stata Corp. Cochran, W. G. (1954). Some methods for strengthening the common 2 tests. Biometrics, 10, 417450. Colman, P. G., Goodall, G. I., Garcia-Webb, P., Williams, P. F., & Dunlop, M. E. (1997). Glycohaemoglobin: A crucial measurement in modern diabetes management. Progress towards standardisation and improved precision of measurement. Medical Journal of Australia, 167, 9698. Cox, D., & Oates, D. (1984). Analysis of survival data. Chapman & Hall: New York. Croxson, S. (2002). Diabetes in the elderly: Problems of care and service provision. Diabetic Medicine, 19, S66S72. Douglas, V. (2001). Living with a chronic leg ulcer an insight into patients experiences and feelings. Journal of Wound Care, 10, 355360. Edmonds, M. E. (2004). The diabetic foot, 2003. Diabetes/Metabolism Research and Reviews, 20, S9S12. Edmonds, M., & Foster, A. (2000). Managing the diabetic foot. London: Blackwell Science. Executive Committee for the Asymptomatic Carotid Artherosclerosis Study. (1995). Endarterectomy for asymptomatic carotid artery stenosis. Journal of the American Medical Association, 273, 14211428. Faglia, E., Favales, F., & Morabito, A. (2001). New ulceration, new major amputation, and survival rates in diabetic subjects hospitalized for foot ulceration from 1990 to 1993. Diabetes Care, 24, 7883. Fox, R. D. (2005). Innocent beginnings, uncertain futures: Exploring the challenges of living with diabetic foot ulcers. Canadian Journal of Diabetes, 29, 105110. Gilbody, S., Sheldon, T., & Wessely, S. (2006). Should we screen for depression? British Medical Journal, 332, 10271030. Harrington, C., Zagari, M. J., Corea, J., & Klitenic, J. (2000). A cost analysis of diabetic lower extremity ulcers. Diabetes Care, 23, 13331338. Ismail, K., Winkley, K., Stahl, D., Chalder, T., & Edmonds, M. (2007). A cohort study of people with diabetes and their first foot ulcer: The role of depression on mortality. Diabetes Care, 30, 14731479. Jager, A., Kostense, P. J., Ruhe, H. G., Heine, R. J., Nijpels, G., Dekker, J. M., Bouter, L. M., & Stehouwer, C. D. A. (1999). Microalbumi-
K. Winkley et al. / Journal of Diabetes and Its Complications 21 (2007) 341349 Vileikyte, L. (2001). Diabetic foot ulcers: A quality of life issue. Diabetes and Metabolism Research and Reviews, 17, 246249. WHO. (1992). 'The ICD-10 classification of mental and behavioural disorders. Clinical descriptions and diagnostic guidelines'. Geneva: World Health Organization. WHO. (1997). SCAN: Schedules for Clinical Assessment in Neuropsychiatry. Version 2.1. Geneva: World Health Organization.
349
Wrobel, J. S., Mayfield, J. A., & Reiber, G. E. (2001). Geographic variation of lower-extremity major amputation in individuals with and without diabetes in the Medicare population. Diabetes Care, 24, 860864. Zhang, X., Norris, S. L., Gregg, E. W., Cheng, Y. J., Beckles, G. L., & Khahn, H. S. (2005). Depressive symptoms and mortality among persons with and without diabetes. American Journal of Epidemiology, 161, 652660.
Você também pode gostar
- No. Nama Perusahaan KomoditiDocumento3 páginasNo. Nama Perusahaan KomoditiBaskoro MahendraAinda não há avaliações
- Busn218 Video17StartDocumento4 páginasBusn218 Video17StartBaskoro MahendraAinda não há avaliações
- Explores The Hidden Side of Everything. New York: William Morrow. 242 PP., $25.95Documento4 páginasExplores The Hidden Side of Everything. New York: William Morrow. 242 PP., $25.95Baskoro MahendraAinda não há avaliações
- GE Matrix Generator - Bubble-Chart Version 1.1Documento5 páginasGE Matrix Generator - Bubble-Chart Version 1.1Baskoro MahendraAinda não há avaliações
- Stanford Ecorner: Understanding Venture Capital (Entire Talk)Documento10 páginasStanford Ecorner: Understanding Venture Capital (Entire Talk)Baskoro MahendraAinda não há avaliações
- Business Model Canvas PosterDocumento1 páginaBusiness Model Canvas PosterBaskoro MahendraAinda não há avaliações
- Ebook 592 Twexcvets Posts QuotesDocumento138 páginasEbook 592 Twexcvets Posts QuotesBaskoro MahendraAinda não há avaliações
- Forum Web of Class 3ia10 Using Ruby On RailsDocumento1 páginaForum Web of Class 3ia10 Using Ruby On RailsBaskoro MahendraAinda não há avaliações
- Emmet Cheat SheetDocumento15 páginasEmmet Cheat SheetManoj KumarAinda não há avaliações
- CV TemplateDocumento2 páginasCV TemplateBaskoro MahendraAinda não há avaliações
- Stanford Ecorner: Understanding Venture Capital (Entire Talk)Documento10 páginasStanford Ecorner: Understanding Venture Capital (Entire Talk)Baskoro MahendraAinda não há avaliações
- Pengaruh Elisitasi Terhadap Pertumbuhan Dan Produksi Alkaloida Kinolin Dari Akar Rambut Tanaman Kina (Cinchona Succirubra Pavon Ex Klotzsch)Documento13 páginasPengaruh Elisitasi Terhadap Pertumbuhan Dan Produksi Alkaloida Kinolin Dari Akar Rambut Tanaman Kina (Cinchona Succirubra Pavon Ex Klotzsch)Baskoro MahendraAinda não há avaliações
- CV Lengkap Irul Terbaru1Documento9 páginasCV Lengkap Irul Terbaru1Baskoro MahendraAinda não há avaliações
- Dystocia Due To Mummified Foetal Monster in A Yankasa Ewe: A Case ReportDocumento3 páginasDystocia Due To Mummified Foetal Monster in A Yankasa Ewe: A Case ReportBaskoro MahendraAinda não há avaliações
- Academic JobsDocumento18 páginasAcademic JobsNandNAinda não há avaliações
- Soal ToeflDocumento2 páginasSoal ToeflBaskoro MahendraAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Research Proposal 2 FinalDocumento13 páginasResearch Proposal 2 Finalapi-462099014Ainda não há avaliações
- Absolute and Relative Contraindications To IV Rt-PA For Acute Ischemic StrokeDocumento12 páginasAbsolute and Relative Contraindications To IV Rt-PA For Acute Ischemic Strokeأبو أويس شرف الدينAinda não há avaliações
- Lifestyle Diseases Affecting The Nursing Faculty at Tarlac State University During Covid 19 PandemicDocumento71 páginasLifestyle Diseases Affecting The Nursing Faculty at Tarlac State University During Covid 19 PandemicDeinielle Magdangal RomeroAinda não há avaliações
- Atrial Fibrillation - Diagnosis and Treatment - AAFP PDFDocumento8 páginasAtrial Fibrillation - Diagnosis and Treatment - AAFP PDFNaufal AmanullahAinda não há avaliações
- Scientific-Benefits-Of-Meditation-Pdf-Liveanddare ComDocumento14 páginasScientific-Benefits-Of-Meditation-Pdf-Liveanddare Comapi-321697736Ainda não há avaliações
- ARTERISCLEROSISDocumento46 páginasARTERISCLEROSISAdilla Edi AriefAinda não há avaliações
- Hong Kong Baptist University Department of Sports, Physical Education & Health PERM 3016 Fitness and Recreation For Selected PopulationDocumento49 páginasHong Kong Baptist University Department of Sports, Physical Education & Health PERM 3016 Fitness and Recreation For Selected PopulationWAI YING HOAinda não há avaliações
- Aspilets ECDocumento5 páginasAspilets ECJerry SerapionAinda não há avaliações
- Panvascular Disease - Diagnosis and Management: SciencedirectDocumento9 páginasPanvascular Disease - Diagnosis and Management: SciencedirectAndikaputra Brahma WidiantoroAinda não há avaliações
- Nimesil PDFDocumento5 páginasNimesil PDFTemur LegendaryAinda não há avaliações
- Panel 1: Aims of This Policy ViewDocumento10 páginasPanel 1: Aims of This Policy ViewSeptime TyasAinda não há avaliações
- Diagnostic Errors in TelehealthDocumento8 páginasDiagnostic Errors in TelehealthKarina AuliaAinda não há avaliações
- Course Specification Emergency NursingDocumento6 páginasCourse Specification Emergency NursingWael LotfyAinda não há avaliações
- Cochrane: LibraryDocumento17 páginasCochrane: LibraryGita TikihaiAinda não há avaliações
- Aha 2018 StrokeDocumento266 páginasAha 2018 StrokeMichelle Alexandra Mendizabal LopezAinda não há avaliações
- Aflacts-With-Hospital - AflacDocumento4 páginasAflacts-With-Hospital - AflacScottAinda não há avaliações
- 4564 2934 p436 Pages Deleted EditedDocumento4 páginas4564 2934 p436 Pages Deleted EditedHaniAinda não há avaliações
- PNF 22 The Effects of PNF and Trunk Stabilization Robot Training On Trunk Stability and Balance in Patients With Chronic StrokeDocumento11 páginasPNF 22 The Effects of PNF and Trunk Stabilization Robot Training On Trunk Stability and Balance in Patients With Chronic StrokeAnonymous j0xAgHs3Ainda não há avaliações
- Admision FormDocumento8 páginasAdmision FormRyles ZenegadeAinda não há avaliações
- Diffuse Optics: Fundamentals & Tissue ApplicationsDocumento115 páginasDiffuse Optics: Fundamentals & Tissue ApplicationsGuy CohenAinda não há avaliações
- Accmm2 19Documento4 páginasAccmm2 19lmplmpAinda não há avaliações
- Neurología NatalizumabDocumento41 páginasNeurología Natalizumablorcy9Ainda não há avaliações
- StrokeConceptMap 2Documento153 páginasStrokeConceptMap 2Charm Barinos100% (2)
- November 2008 NLE Practice IDocumento15 páginasNovember 2008 NLE Practice IEJ Cubero, R☤N100% (1)
- HealthMax 20 PayDocumento11 páginasHealthMax 20 PayJulienne Mhae ReyesAinda não há avaliações
- Thunderclap Headaches: Headache ToolboxDocumento2 páginasThunderclap Headaches: Headache ToolboxLeidy Carolina Salazar ChicaAinda não há avaliações
- Scalp Acupuncture2Documento64 páginasScalp Acupuncture2Ganga Singh100% (1)
- Ventilación Mecánica en Pacientes NeurocriticosDocumento14 páginasVentilación Mecánica en Pacientes NeurocriticosJoseph Campos SanchezAinda não há avaliações
- How I Assess and Manage The Risk of Bleeding in Patients Treated For Venous ThromboembolismDocumento11 páginasHow I Assess and Manage The Risk of Bleeding in Patients Treated For Venous ThromboembolismHugo HectorAinda não há avaliações
- The Ultimate Carrom Guide - 2003tDocumento22 páginasThe Ultimate Carrom Guide - 2003tsudhakarkaipa0% (1)