Escolar Documentos
Profissional Documentos
Cultura Documentos
Cebu (Velez) General Hospital Department of Pediatrics
Enviado por
Janelle Estrabela GargaritanoTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Cebu (Velez) General Hospital Department of Pediatrics
Enviado por
Janelle Estrabela GargaritanoDireitos autorais:
Formatos disponíveis
CEBU (VELEZ) GENERAL HOSPITAL DEPARTMENT OF PEDIATRICS Cebu City
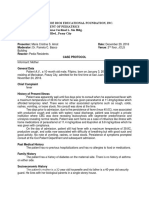
DISCHARGE SUMMARY
P()IE*)+, *(-E )ABC*.6, %ylvestre ?lint Cadungog DI(G*3,I, (GE 2 months ,E. ,)()/, C2ild C(,E */-0E1 #"92#8#, #"388-
1. Pneumonia -oderate 1isk D()E *5(
3PE1()I3* PE1431-ED *5(
PROBLEM: Pneumonia moderate risk S: About one week PTA, patient had onset of non productive cough and coryza. No fever, dyspnea nor
cyanosis. Condition was tolerated, no treatment given. Two days PTA, patient had productive cough with tenacious sputum, non bloody and non foul smelling, amounting to one spoonful associated with fever, coryza and vomiting ! of previously ingested milk amounting to "##cc per episode. No diarrhea, anore!ia, retractions nor dyspnea mentioned. $e was given %albutamol &A'(A)*N+ mg,-m) .- m) &A./#." mkd+ and Phenylpropanolamine $cl 0 1rompheniramine (aleate &Nasatapp+ 2. -mg, mg,m) #.2 m) &A./#.34mkd+ which provided temporary relief of symptoms. 5 hours PTA, cough and fever still persisted associated with dyspnea and cyanosis thus prompting admission.
O: 6n admission, patient was e!amined conscious, awake, alert, afebrile, not in respiratory distress, with the ff vital
signs7 HR: "2#bpm RR: 82cpm Temp: 54.4 C,a!illa Wt: 4.4 kg &zscore7 # %.+ Ht: 29.-cm &zscore7 :" %.+ HC: 95 cm &zscore7 # %.+ BMI: "8.- kg,m &zscore7 below 0 %.+ Skin: warm, dry, fair skin, no gross lesions, no rashes, good skin turgor and mobility con;unctivae, &:+ tug test, nasal septum midline Neck: short, supple, trachea at midline, no lymphadenopathy C/L: CVS: Abd: GUT: e<ual chest e!pansion, resonant, harsh breath sounds, &0+ rales adynamic precordium, %" and % distinct, normal rate, regular rhythm, &:+ murmurs globular, no rashes, umbilicus at midline, normoactive bowel sounds, &:+ mass, &:+ tenderness. bladder not distended, grossly male
HEENT: normocephalic, eyes not sunken, anicteric sclerae, pink palpebral con;unctivae, &0+ nasal discharges
Extremitie : no gross deformity, full range of motion all e!tremities, strong peripheral pulses, no edema, C'T of = seconds CNS: CN I: Cerebr!": awake and alert cannot be assessed SIGNATURE OF AP Ellen Gasendo .r. Dr. >ean ?rancis ?lores : i! "# 90$$% Alcantara )icense @7 2-"84 Cr!ni!" Ner#e : CN II$ III: &0+ P)', direct and consensual, both eyes & mm, mm+ ADMISSION DISCHARGE CONDITION IN-PATIENT DATE DATE DISCHARGED DAYS 4 9 2014 4 12 2014 Improved 4 PREPARED BY: PIIC &ane ou E. Gar'aritano RESIDENT-IN-CHARGE: .r. %erah %aphira Allera )ic @7 #" 988-
CN III$ IV$ VI: CN V: CN VII:
full e!traocular movements good suck symmetrical facial e!pressions
CN VIII: CN I%$ %: CN %I: CN %II: Sen &r': M&t&r:
turns to the source of sound, hearing intact &0+ gag refle! symmetrical shoulders tongue midline on protrusion arouses with painful stimuli good muscle tone, no atrophy
Cerebe""!r: no nystagmus M&t&r: no tremors, no atrophy, no fasciculations
1e6le7es#
C(URSE IN THE WAR): 6n admission, patient was afebrile, not in respiratory distress with stable vital signs. Chest Dray was taken and revealed radiologic findings of Pneumonia in the left lower lung. Cefuro!ime &Einacef+ -#mg *FTT " st dose was given over 5# minutes as *F drip then continued as *FTT every 8 hours. %albutamol " nebule ordered to be given via nebulization every 2 hours and Paracetamol "##mg,m) " m) &A./" .33 mkd+ ordered to be given orally every 9 hours. *F? was started with .- #.5 NaCl at 5 cc,hr as maintenance fluid. *nput and output monitored every shift with vital signs monitoring every hours. 6n the first hospital day, patient was comfortable, afebrile with stable vital signs. No dyspnea, no cyanosis and had a good appetite. Patient still with cough and nasal discharges. C1C was taken and result showed increased leukocyte count with monocytic predominance &G1C H "5.5I (onophils H "#.9J+ and anemia &$gb H ""." g,d)I $ct H 5-.#JI (CF H 4 .4JI (C$ H 5." pgI '.G H "".5J+. Platelet count was normal & 99+. (edications were continued. 6n the nd hospital day, vital signs are stable. No dyspnea, afebrile, no bleeding diathesi s noted. Patient was started with chemotherapy with Cytarabine 52 mg *F push <" h for # doses in "# days and .o!orubucin "8 mg *F drip in -# ml of .-water to run for " hour using microset given every other day for 5 days. Patient then monitored for any allergic reactions. 6n the 5rd hospital , vital signs were stable. Patient was able to sleep well and was afebrile throughout the night. No episodes of vomiting nor diarrhea. Patient had onset of generalized maculopapular rashes due to skin contact with bed linens. Cetirizine "#mg,m) drops #. m) 6. every night was prescribed and given with relief. (onitored every hours. Patient stable and may go home instructions given. *F? discontinued prior to discharge. Patient discharged improved. *: ". . Take home medications7 Cefuro!ime -#mg,-m) m) &A./" .38 mkd+ 1*. for 4 days &8am : 2pm+ %albutamol &Fentolin+ " neb T*. for 5 days &4am:5pm:""pm+
To come back for follow up check up at .r. AlcantaraKs clinic on April "2, #"9
Você também pode gostar
- Written Arguments of Maintenance Case On Behalf of PetitionerDocumento4 páginasWritten Arguments of Maintenance Case On Behalf of PetitionerSridhara babu. N - ಶ್ರೀಧರ ಬಾಬು. ಎನ್85% (53)
- Case Study - Chronic Bronchitis ABG DeteriorationDocumento5 páginasCase Study - Chronic Bronchitis ABG DeteriorationNikki M. ArapolAinda não há avaliações
- Sujok InpancreatitisDocumento70 páginasSujok InpancreatitisFedericoz Zarra100% (1)
- AMC-2007 Clinical Examination RecallsDocumento156 páginasAMC-2007 Clinical Examination Recallsbreezingthru100% (1)
- Sample Case ProtocolDocumento6 páginasSample Case ProtocoljheyfteeAinda não há avaliações
- History and Physical ExaminationDocumento71 páginasHistory and Physical ExaminationJanelle Estrabela Gargaritano100% (2)
- Audience AnalysisDocumento7 páginasAudience AnalysisSHAHKOT GRIDAinda não há avaliações
- Sba 1&2 Conjoint Exam Part II April 2017 Doc-1Documento21 páginasSba 1&2 Conjoint Exam Part II April 2017 Doc-1Fadhly SharimanAinda não há avaliações
- Case Report 2Documento37 páginasCase Report 2Halima TusadiaAinda não há avaliações
- PCC CaseDocumento9 páginasPCC CaseKaila AbeledaAinda não há avaliações
- CC 5 October 2017 W JDocumento39 páginasCC 5 October 2017 W JLilik NatasubrataAinda não há avaliações
- Soal CBT MCQ Stase Dalam 2014Documento13 páginasSoal CBT MCQ Stase Dalam 2014andretegarAinda não há avaliações
- Medicine 42qDocumento12 páginasMedicine 42qmedico30026Ainda não há avaliações
- Anaesthetic Man-WPS OfficeDocumento21 páginasAnaesthetic Man-WPS OfficeAnuja KumaresonAinda não há avaliações
- Laporan Kasus AppendicitisDocumento21 páginasLaporan Kasus AppendicitisjessicaAinda não há avaliações
- Sample Medical ReportsDocumento6 páginasSample Medical ReportsMayAinda não há avaliações
- Grand Conference: Clinical Clerks Openiano, Oquendo, Pasaporte, PangandianDocumento65 páginasGrand Conference: Clinical Clerks Openiano, Oquendo, Pasaporte, PangandianJessa MeaAinda não há avaliações
- CC 4 Nov 2017 SeizureDocumento44 páginasCC 4 Nov 2017 SeizurenisaAinda não há avaliações
- Byol Meridians Body MeridiansDocumento70 páginasByol Meridians Body Meridianspbi tv100% (1)
- CC 18 Mei 19 HidrocephalusDocumento50 páginasCC 18 Mei 19 HidrocephalusAisya FikritamaAinda não há avaliações
- Clerk GCPDocumento19 páginasClerk GCPNikki DiocampoAinda não há avaliações
- Easter College: Department of NursingDocumento13 páginasEaster College: Department of NursingShaii shanAinda não há avaliações
- Emcase 1 Juli EnglishDocumento38 páginasEmcase 1 Juli EnglishAndi Nurjannah KaddirajaAinda não há avaliações
- Case Presentation RADocumento6 páginasCase Presentation RAdocv526Ainda não há avaliações
- CASE CONFERENCE FOR PEDIATRIC PATIENTSDocumento39 páginasCASE CONFERENCE FOR PEDIATRIC PATIENTSAisya FikritamaAinda não há avaliações
- Casos Clinicos NEJM 2018Documento287 páginasCasos Clinicos NEJM 2018Eduarda RosasAinda não há avaliações
- IM-Generalized Peritonitis HX PEDocumento20 páginasIM-Generalized Peritonitis HX PETrisAinda não há avaliações
- 289 324Documento13 páginas289 324ashighaAinda não há avaliações
- Medicine and Surgery Review QuestionsDocumento5 páginasMedicine and Surgery Review QuestionsLamya BanderAinda não há avaliações
- CC 4 Nov 2017 SeizureDocumento44 páginasCC 4 Nov 2017 SeizureLilik NatasubrataAinda não há avaliações
- Labrato - Kayla AHN596-801 SOAP#1Documento10 páginasLabrato - Kayla AHN596-801 SOAP#1Kayla LabratoAinda não há avaliações
- Final Mock Case StudiesDocumento22 páginasFinal Mock Case StudiesDolly creationsAinda não há avaliações
- CC 17 Feb 2017 1st Epilepsy OkeDocumento43 páginasCC 17 Feb 2017 1st Epilepsy OkeLucky Yoga -satria NatasukmaAinda não há avaliações
- Wates - Presentasi Transport Anak KritisDocumento27 páginasWates - Presentasi Transport Anak Kritisbayu ariani chandrasariAinda não há avaliações
- "Don't Take My Breath Away" A Case Presentation On Pneumocystis PneumoniaDocumento20 páginas"Don't Take My Breath Away" A Case Presentation On Pneumocystis PneumoniaNikki DiocampoAinda não há avaliações
- IM Gastro FinalDocumento10 páginasIM Gastro FinalIzzyMaxinoAinda não há avaliações
- Block 7 Active Phase 1st Stage of LaborDocumento29 páginasBlock 7 Active Phase 1st Stage of LaborRoselle Joy D. RosalejosAinda não há avaliações
- Morning Report Rev 26 Agustus 2021 TetanusDocumento25 páginasMorning Report Rev 26 Agustus 2021 TetanusMelindaAinda não há avaliações
- Final Exam Flash Cards - PDocumento37 páginasFinal Exam Flash Cards - PReut shapiraAinda não há avaliações
- January 9 SGDDocumento7 páginasJanuary 9 SGDRONALDO CUAAinda não há avaliações
- Subdural Empyema Case ReportDocumento22 páginasSubdural Empyema Case ReportAndi Efri Rangga AdityaAinda não há avaliações
- ROSIMO - AUG 2021 NB VomitingDocumento5 páginasROSIMO - AUG 2021 NB VomitingcarlosAinda não há avaliações
- Steven Johnson SyndromeDocumento70 páginasSteven Johnson SyndromeAiram P NatingaAinda não há avaliações
- Pneumonia - The forgotten killerDocumento38 páginasPneumonia - The forgotten killerMishaDehalAinda não há avaliações
- Empyema ThoracisDocumento14 páginasEmpyema ThoracisMara AbantoAinda não há avaliações
- Case Write Up Faculty of Medicine Emergency DepartmentDocumento13 páginasCase Write Up Faculty of Medicine Emergency DepartmentDinesh KumarAinda não há avaliações
- Major Case 3Documento3 páginasMajor Case 3Christine Evan HoAinda não há avaliações
- Acute Exacerbation On Chronic Obstructive Pulmonary DisorderDocumento30 páginasAcute Exacerbation On Chronic Obstructive Pulmonary DisorderFitri NurullahAinda não há avaliações
- Obstetrics Patient M.L. 26/F Date Admitted: December 17, 2018 Date Discharged: December 19, 2018 Informant: Patient Reliability: 80%Documento6 páginasObstetrics Patient M.L. 26/F Date Admitted: December 17, 2018 Date Discharged: December 19, 2018 Informant: Patient Reliability: 80%Justin LamAinda não há avaliações
- CC 13 October 2017 (Demam Neutropenia) 2Documento35 páginasCC 13 October 2017 (Demam Neutropenia) 2febrydwiAinda não há avaliações
- Discharge Summary - Villalobos Kheannah A - 03aug2019Documento3 páginasDischarge Summary - Villalobos Kheannah A - 03aug2019นีล ไบรอันAinda não há avaliações
- San Juan de Dios Educational Foundation, Inc. Department of Pediatrics 4th Floor Jaime Cardinal L. Sin Bldg. 2772 Roxas BLVD., Pasay CityDocumento5 páginasSan Juan de Dios Educational Foundation, Inc. Department of Pediatrics 4th Floor Jaime Cardinal L. Sin Bldg. 2772 Roxas BLVD., Pasay CityNiña AmatAinda não há avaliações
- Congenital Heart Disease in Trisomy 21Documento20 páginasCongenital Heart Disease in Trisomy 21Emily EresumaAinda não há avaliações
- Liver Abscess Risk FactorsDocumento7 páginasLiver Abscess Risk FactorsJoan junioAinda não há avaliações
- Morning Report June 10, 2017 Dept of Internal Medicine G26Documento21 páginasMorning Report June 10, 2017 Dept of Internal Medicine G26Deasy Arindi PutriAinda não há avaliações
- Congenital Pneumonia Case ReportDocumento17 páginasCongenital Pneumonia Case ReportHendra WardhanaAinda não há avaliações
- Stroke in Covid May 2021Documento6 páginasStroke in Covid May 2021Louie MercadoAinda não há avaliações
- ACFrOgBkr4aZ1Zsv2aeDPukwoupHYAHI9-5rxWQvNUi8ieV5gRm4eoP2on6KvEa-YneunqXgvtLptEqd x8lP28R7PCD9g-89a SfTJckcaszb9lKHWC J5kUwNM9HuwTeM9ieN3fFbkGEQNGozDocumento8 páginasACFrOgBkr4aZ1Zsv2aeDPukwoupHYAHI9-5rxWQvNUi8ieV5gRm4eoP2on6KvEa-YneunqXgvtLptEqd x8lP28R7PCD9g-89a SfTJckcaszb9lKHWC J5kUwNM9HuwTeM9ieN3fFbkGEQNGozyebadem228Ainda não há avaliações
- Clinical Case Presentation Congenital Heart DiseaseDocumento27 páginasClinical Case Presentation Congenital Heart DiseaseAdityaAinda não há avaliações
- 1 Jan Mekong PeritonitisDocumento14 páginas1 Jan Mekong PeritonitisDr Ari SembiringAinda não há avaliações
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicNo EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicNota: 5 de 5 estrelas5/5 (1)
- Different in the therapy of pressure negtotheeva single-useNo EverandDifferent in the therapy of pressure negtotheeva single-useAinda não há avaliações
- The Meditations of The Emperor Marcus Aurelius AntoninusDocumento248 páginasThe Meditations of The Emperor Marcus Aurelius AntoninusMMMMM99999Ainda não há avaliações
- Diarrhea World Health OrganizationDocumento49 páginasDiarrhea World Health OrganizationJanelle Estrabela GargaritanoAinda não há avaliações
- IELTS Advantage - Reading SkillsDocumento139 páginasIELTS Advantage - Reading SkillsYashel Bartolome100% (9)
- Leadman Ni HenzDocumento110 páginasLeadman Ni HenzJanelle Estrabela GargaritanoAinda não há avaliações
- Leadman Ni HenzDocumento110 páginasLeadman Ni HenzJanelle Estrabela GargaritanoAinda não há avaliações
- MCN Jane Lou GargaritanoDocumento918 páginasMCN Jane Lou GargaritanoJanelle Estrabela GargaritanoAinda não há avaliações
- 11 Recurrent Aphthous Stomatitis Caused by Food AllergyDocumento6 páginas11 Recurrent Aphthous Stomatitis Caused by Food AllergyramaAinda não há avaliações
- Masala Kitchen Menus: Chowpatty ChatDocumento6 páginasMasala Kitchen Menus: Chowpatty ChatAlex ShparberAinda não há avaliações
- Us Aers Roadmap Noncontrolling Interest 2019 PDFDocumento194 páginasUs Aers Roadmap Noncontrolling Interest 2019 PDFUlii PntAinda não há avaliações
- Engb546 NP RevisedDocumento5 páginasEngb546 NP RevisedRafaelaAinda não há avaliações
- Engineering: Ronnapee Chaichaowarat, Jun Kinugawa, Kazuhiro KosugeDocumento8 páginasEngineering: Ronnapee Chaichaowarat, Jun Kinugawa, Kazuhiro Kosugelaura bemudezAinda não há avaliações
- Edukasyon Sa Pagpapakatao (Esp) Monitoring and Evaluation Tool For Department Heads/Chairmen/CoordinatorsDocumento3 páginasEdukasyon Sa Pagpapakatao (Esp) Monitoring and Evaluation Tool For Department Heads/Chairmen/CoordinatorsPrincis CianoAinda não há avaliações
- Practical and Mathematical Skills BookletDocumento30 páginasPractical and Mathematical Skills BookletZarqaYasminAinda não há avaliações
- The "5 Minute Personality Test"Documento2 páginasThe "5 Minute Personality Test"Mary Charlin BendañaAinda não há avaliações
- Emotion and Decision Making: FurtherDocumento28 páginasEmotion and Decision Making: FurtherUMAMA UZAIR MIRZAAinda não há avaliações
- Signal WordsDocumento2 páginasSignal WordsJaol1976Ainda não há avaliações
- Dravyaguna VijaDocumento1.095 páginasDravyaguna VijaSilas Chagas100% (1)
- FIRE Protection Engineering Winter 2002Documento64 páginasFIRE Protection Engineering Winter 2002Hany RifaatAinda não há avaliações
- The ADDIE Instructional Design ModelDocumento2 páginasThe ADDIE Instructional Design ModelChristopher Pappas100% (1)
- NWABSD Lesson PlansDocumento5 páginasNWABSD Lesson Plansapi-379699844Ainda não há avaliações
- Detect Organic Elements with Sodium FusionDocumento10 páginasDetect Organic Elements with Sodium FusionMukundAinda não há avaliações
- Brittney Gilliam, Et Al., v. City of Aurora, Et Al.Documento42 páginasBrittney Gilliam, Et Al., v. City of Aurora, Et Al.Michael_Roberts2019Ainda não há avaliações
- Veerabhadra Swamy MantrasDocumento6 páginasVeerabhadra Swamy Mantrasगणेश पराजुलीAinda não há avaliações
- BtuDocumento39 páginasBtuMel Vin100% (1)
- Sample Front Desk Receptionist ResumeDocumento5 páginasSample Front Desk Receptionist ResumeReyvie FabroAinda não há avaliações
- Rangkuman Corporate GovernanceDocumento21 páginasRangkuman Corporate GovernanceAlissa JanssensAinda não há avaliações
- Chapter 2Documento26 páginasChapter 2Dinindu Siriwardene100% (1)
- Solutions To Basic Economic Problems - AllDocumento27 páginasSolutions To Basic Economic Problems - AllAsha GeorgeAinda não há avaliações
- 1402 2046Documento11 páginas1402 2046Luca PilottiAinda não há avaliações
- Determinants of Consumer BehaviourDocumento16 páginasDeterminants of Consumer BehaviouritistysondogAinda não há avaliações
- Sample File: Official Game AccessoryDocumento6 páginasSample File: Official Game AccessoryJose L GarcíaAinda não há avaliações
- Planning Levels and Types for Organizational SuccessDocumento20 páginasPlanning Levels and Types for Organizational SuccessLala Ckee100% (1)
- Portal ScienceDocumento5 páginasPortal ScienceiuhalsdjvauhAinda não há avaliações
- Sta. Ignacia High School: Philosophy 101Documento1 páginaSta. Ignacia High School: Philosophy 101Mira VeranoAinda não há avaliações