Escolar Documentos
Profissional Documentos
Cultura Documentos
Cervical Spondylosis
Enviado por
Roopa KumarTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Cervical Spondylosis
Enviado por
Roopa KumarDireitos autorais:
Formatos disponíveis
Cervical
Cervical
Spondylosis
Spondylosis
;
;
Etiology, Evaluation and
Etiology, Evaluation and
Management
Management
Steven D. Wray M.D.
Steven D. Wray M.D.
Atlanta Brain and Spine Care P.C.
Atlanta Brain and Spine Care P.C.
Piedmont Spine Center
Piedmont Spine Center
Conclusion:
Conclusion:
Cervical nerve root or cord
Cervical nerve root or cord
compression from bone spur
compression from bone spur
formation (
formation (
spondylosis
spondylosis
) is a
) is a
degenerative and progressive
degenerative and progressive
process which should be referred to
process which should be referred to
a neurosurgeon early as outcome is
a neurosurgeon early as outcome is
directly related to the duration of
directly related to the duration of
symptoms.
symptoms.
Cervical
Cervical
Spondylosis
Spondylosis
; Definition
; Definition
Age related degeneration of the
Age related degeneration of the
cervical spine
cervical spine
Osteoarthritis
Osteoarthritis
Most common in persons over 40
Most common in persons over 40
Most common cause for
Most common cause for
myelopathy
myelopathy
in persons over 55
in persons over 55
Male>Female
Male>Female
Cervical
Cervical
Spondylosis
Spondylosis
;
;
Pathology
Pathology
Age Related Degeneration and
Dehydration of intervertebal Disks
Decreased cartilage between
adjacent vertebral bodies
Developmental laxity in the spinal
supportive ligaments
Hyper-mobility of spinal segment
Bone-on bone apposition
propagates bone spur formation
which narrow the cervical spinal
canal and may compress the
cervical nerve roots and spinal cord
Cervical
Cervical
Spondylosis
Spondylosis
;
;
Clinical Presentation
Mechanical
Mechanical
Pain
Pain
Stiffness
Stiffness
Muscle Spasm
Muscle Spasm
Pop and Crack
Pop and Crack
Neurologic
Neurologic
Nerve Root Compression
Nerve Root Compression
Spinal Cord Compression
Spinal Cord Compression
Cervical
Cervical
Spondylosis
Spondylosis
;
;
Spondylitic change with bone
spur/disk complex formation
Developmental narrowing of
spinal canal with
compression of spinal cord
and nerve roots
Cervical
Cervical
Spondylosis
Spondylosis
;
;
Cord Compression
Cord Compression
64 Year old patient
with severe
symptomatic
spondylitic
myelopathy.
Multilevel Cord
compression seen on
MRI.
Cervical
Cervical
Spondylosis
Spondylosis
;
;
Natural History
Natural History
Predisposition Predisposition
Some individuals have a Some individuals have a congenitally narrow spinal congenitally narrow spinal
canal canal
Increased incidence of symptom development with mild Increased incidence of symptom development with mild
to moderate to moderate spondylosis spondylosis
Pre Pre- -participation screening of athletes to asses participation screening of athletes to asses
vulnerability to spinal cord injury vulnerability to spinal cord injury
Evolution Evolution
Unlike soft cervical disk Unlike soft cervical disk herniation herniation which usually which usually
resolves, Cervical resolves, Cervical Spondylosis Spondylosis is progressive is progressive
May be insidious and then more rapidly progressive as May be insidious and then more rapidly progressive as
Spinal Fluid Spinal Fluid reserve reserve becomes depleted by enlarging becomes depleted by enlarging
bone spurs bone spurs
Cervical
Cervical
Spondylosis
Spondylosis
Symptom Pathogenesis
Symptom Pathogenesis
Hyper
Hyper
-
-
mobility / instability of spinal
mobility / instability of spinal
segments
segments
Irritation/inflammation of heavily
Irritation/inflammation of heavily
innervated vertebral body endplates
innervated vertebral body endplates
Direct compression of cervical nerve
Direct compression of cervical nerve
root or spinal cord
root or spinal cord
Repetitive trauma to cord or roots
Repetitive trauma to cord or roots
Ischemic change to the cord
Ischemic change to the cord
Cervical
Cervical
Spondylosis
Spondylosis
;
;
Presentation with
Presentation with
Headache
Headache
Kyphotic Angular deformity
creates added stress on the
paraspinal muscles and causes
severe myofascial pain and
spasm and often produces
suboccipital headaches where
the paraspinal muscles insert on
the base of the skull.
For this reason, some
degenerative cervical spine
disease can present with
headache.
Cervical
Cervical
Spondylosis
Spondylosis
;
;
Developmental Scoliosis; Facet
Developmental Scoliosis; Facet
Arthropaty
Arthropaty
Coronal Plane angulation
causes myofascial pain as
well as changes of the facet
joints. The added stress on
joints leads to joint
hypertrophy and inflammatory
change which is painful.
Cervical Spine Dynamic Instability;
Cervical Spine Dynamic Instability;
Flexion/Extension Radiographs!
Flexion/Extension Radiographs!
Nonsurgical Treatment
Nonsurgical Treatment
NSAIDS
NSAIDS
Traction
Traction
PT
PT
Ultrasound for trigger points Ultrasound for trigger points
Neuromuscular massage Neuromuscular massage
TENS TENS
Traction Traction
Interventional
Interventional
Selective nerve root block Selective nerve root block
ESI ESI
Facet block/ RFA Facet block/ RFA
Definitions
Definitions
Radiculopathy
Radiculopathy
Nerve Root Compression Nerve Root Compression
Pain, weakness, numbness in the distribution Pain, weakness, numbness in the distribution
of a nerve root (neck or back) of a nerve root (neck or back)
Myelopathy
Myelopathy
Spinal Cord Compression in the cervical or Spinal Cord Compression in the cervical or
thoracic area thoracic area
Symptoms Symptoms
Numbness, tingling of the arms/ hands Numbness, tingling of the arms/ hands
Dexterity difficulty with fine motor movements Dexterity difficulty with fine motor movements
Gait instability Gait instability
Balance and coordination difficulty Balance and coordination difficulty
Bowel/Bladder disturbances (incontinence) Bowel/Bladder disturbances (incontinence)
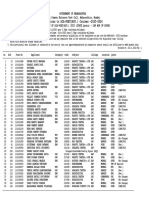
Cervical Nerve Root
Cervical Nerve Root
Symtoms
Symtoms
C4 C4- -5 5 C5 C5- -6 6 C6 C6- -7 7 C7 C7- -T1 T1
Incidence Incidence 2% 2% 19% 19% 69% 69% 10% 10%
Root Root
Affected Affected
C5 C5 C6 C6 C7 C7 C8 C8
Motor Motor Deltoid Deltoid Biceps/ Biceps/
BR BR
Triceps Triceps Intrinsics Intrinsics
Sensory Sensory Shoulder Shoulder Upper Upper
arm/ arm/
Thumb Thumb
2 2
nd nd
3 3
rd rd
finger/ all finger/ all
fingertips fingertips
4 4
th th
and 5 and 5
th th
finger finger
Incidence of
Incidence of
Myelopathy
Myelopathy
is Related
is Related
to Canal Diameter
to Canal Diameter
xxxx
xxxxxx
Canal Diameter <13mm increases
risk for myelopathy
Canal Diameter <10mm almost
always results in symptomatic
cord compression
Differential Diagnoses
Differential Diagnoses
ALS
ALS
Exclusively Motor Exclusively Motor
Tongue Tongue Fasciculations Fasciculations
Multiple Sclerosis
Multiple Sclerosis
Relapsing/remitting symptoms Relapsing/remitting symptoms
Demyelinating Demyelinating plaques on Brain MRI plaques on Brain MRI
Subacute
Subacute
Combined Degeneration
Combined Degeneration
Macrocytic Macrocytic Anemia Anemia
B12 deficiency B12 deficiency
Who Needs Surgery?
Who Needs Surgery?
Neurologic Compromise
Neurologic Compromise
Symptomatic Nerve root compression
Symptomatic Nerve root compression
refractory to non
refractory to non
-
-
surgical management
surgical management
Spinal Cord Compression with
Spinal Cord Compression with
myelopathy
myelopathy
Biomechanical Instability
Biomechanical Instability
Instability on Flexion/Extension Films
Instability on Flexion/Extension Films
Angular deformity
Angular deformity
Subluxation
Subluxation
/
/
Listhesis
Listhesis
Surgical Options; Considerations
Surgical Options; Considerations
Type of Pathology
Type of Pathology
Soft Disk Soft Disk
Bone Spur; Bone Spur; Spondylosis Spondylosis
Location of Compression
Location of Compression
anterior vs. posterior anterior vs. posterior
Angulation
Angulation
of Spine
of Spine
Preserved Preserved Lordosis Lordosis vs. vs. Kyphosis Kyphosis
Patient age and co
Patient age and co
-
-
morbidities
morbidities
Health of adjacent levels
Health of adjacent levels
Bone Density
Bone Density
Number of spinal segments involved
Number of spinal segments involved
Surgical Options
Surgical Options
Anterior vs. Posterior Decompression
Anterior vs. Posterior Decompression
Simple Decompression vs. Fusion
Simple Decompression vs. Fusion
and Stabilization
and Stabilization
Anterior Cervical Decompression
Anterior Cervical Decompression
and Fusion
and Fusion
Performed through a transverse cervical
Performed through a transverse cervical
incision
incision
Microscopic Decompression of spinal cord
Microscopic Decompression of spinal cord
by removal of compressive bone spur
by removal of compressive bone spur
Restore and maintain
Restore and maintain
intervertebral
intervertebral
height
height
using an
using an
intervertebral
intervertebral
bone graft or
bone graft or
plastic spacer
plastic spacer
Stabilize spinal segment with low profile
Stabilize spinal segment with low profile
titanium plate (promotes fusion)
titanium plate (promotes fusion)
Anterior Cervical Decompression
Anterior Cervical Decompression
and Fusion
and Fusion
Anterior Cervical
Anterior Cervical
Diskectomy
Diskectomy
and
and
Fusion
Fusion
Minimal pain as no muscle disruption
Minimal pain as no muscle disruption
Subcuticular
Subcuticular
closure
closure
Overnight observation
Overnight observation
Addresses ventral pathology without
Addresses ventral pathology without
any neural element retraction or
any neural element retraction or
manipulation
manipulation
Anterior Cervical Decompression
Anterior Cervical Decompression
and Fusion
and Fusion
High fusion rate.
Fusion promoted by good blood supply
at the ventral moment arm of the spine.
Fusion Substrate
Fusion Substrate
Historical Gold Standard; Freshly
Historical Gold Standard; Freshly
harvested iliac crest bone
harvested iliac crest bone
autograft
autograft
Donor site morbidity Donor site morbidity
Pain/ Infection Risk Pain/ Infection Risk
Banked Allograft
Banked Allograft
Small but present risk for disease transmission Small but present risk for disease transmission
PEEK Spacers
PEEK Spacers
Plastic cement restrictors which are non Plastic cement restrictors which are non- -
compressible and restore inter compressible and restore inter- -vertebral height vertebral height
Bone
Bone
Morphogenic
Morphogenic
Protein
Protein
Recombinant protein with no risk of
Recombinant protein with no risk of
disease transmission and High fusion
disease transmission and High fusion
rate
rate
Biologics to Promote Fusion
Biologics to Promote Fusion
Osteocondustion
Osteocondustion
Osteoinduction
Osteoinduction
Transverse Process
BMP and Fusion
BMP and Fusion
Goals of Surgery
Goals of Surgery
Decompress neural elements
Decompress neural elements
Restore
Restore
Intervertebral
Intervertebral
height which also
height which also
restores neural
restores neural
foraminal
foraminal
patency
patency
Restore anatomic alignment in the case of
Restore anatomic alignment in the case of
kyphosis
kyphosis
or scoliosis
or scoliosis
Stabilize spinal
Stabilize spinal
segment(s
segment(s
) to prevent
) to prevent
bone spur propagation and repetitive
bone spur propagation and repetitive
nerve root irritation
nerve root irritation
Promote solid
Promote solid
arthrodesis
arthrodesis
over time
over time
ACDF to correct Developmental
ACDF to correct Developmental
Scoliosis from
Scoliosis from
Spondylosis
Spondylosis
XXXXX
ACDF to Correct Developmental
ACDF to Correct Developmental
Kyphosis
Kyphosis
due to
due to
spondylosis
spondylosis
xxxxxxx
Posterior Cervical Fusion
Posterior Cervical Fusion
Decompress neural elements by
Decompress neural elements by
removal of the bony lamina and
removal of the bony lamina and
underlying ligament (
underlying ligament (
Laminectomy
Laminectomy
)
)
Stabilization by posterior lateral
Stabilization by posterior lateral
mass screws and rods
mass screws and rods
Fusion performed by on
Fusion performed by on
-
-
lay
lay
technique and inter
technique and inter
-
-
facet graft
facet graft
material (laminar bone or iliac crest
material (laminar bone or iliac crest
autograft
autograft
)
)
Posterior Cervical Fusion
Posterior Cervical Fusion
Posterior Cervical Decompression
Posterior Cervical Decompression
Decompression alone is
Decompression alone is
contraindicated with preexisting
contraindicated with preexisting
kyphotic
kyphotic
deformity
deformity
High risk of developing late swan
High risk of developing late swan
-
-
neck deformity
neck deformity
Post operative Pain
Post operative Pain
In case of
In case of
hyperlordosis
hyperlordosis
, posterior
, posterior
cord migration may cause cord
cord migration may cause cord
compression
compression
Surgical Outcomes
Surgical Outcomes
Anterior or Posterior approaches that
Anterior or Posterior approaches that
effectively decompress spinal cord
effectively decompress spinal cord
promote improvements in outcome
promote improvements in outcome
Higher Risk of late
Higher Risk of late
kyphosis
kyphosis
in patients
in patients
who undergo
who undergo
laminectomy
laminectomy
or anterior
or anterior
cervical decompression alone compared to
cervical decompression alone compared to
patients in whom decompression is
patients in whom decompression is
combined with fusion
combined with fusion
Fehlings MG, Arvin B. J Neurosurg Spine. 2009 Aug:11 (2): 97-100
Outcomes
Outcomes
Duration of Symptoms Duration of Symptoms and advanced age and advanced age
negatively affect outcome in patients with CSM negatively affect outcome in patients with CSM
50% improve if operated within a year 50% improve if operated within a year
compared with only 16% is operated after compared with only 16% is operated after
Abnormal Pre Abnormal Pre- -operative SSEP/EMG Findings operative SSEP/EMG Findings
adversely affect outcome adversely affect outcome
Cord Signal Change or the presence of spinal Cord Signal Change or the presence of spinal
cord atrophy negatively affect outcome cord atrophy negatively affect outcome
Fehlings MG, Arvin B. J Neurosurg Spine 2009 Aug;11(2):97-100
REFER EARLY!!
REFER EARLY!!
Patients with spinal cord or nerve
Patients with spinal cord or nerve
root compression should be referred
root compression should be referred
for neurosurgical evaluation
for neurosurgical evaluation
promptly.
promptly.
Thank You
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Atrial Fibrillation Topic DiscussionDocumento23 páginasAtrial Fibrillation Topic Discussionapi-567600964Ainda não há avaliações
- Policy Surrender Form PDFDocumento2 páginasPolicy Surrender Form PDF1012804201Ainda não há avaliações
- Biology Final Exam Grade 9Documento2 páginasBiology Final Exam Grade 9Yesha Shah100% (1)
- The Piano 2017v1Documento4 páginasThe Piano 2017v1Roopa KumarAinda não há avaliações
- English 2Documento4 páginasEnglish 2Roopa KumarAinda não há avaliações
- Eng Part1 2017 PDFDocumento2 páginasEng Part1 2017 PDFRoopa KumarAinda não há avaliações
- Eng 2 Part1 2017Documento1 páginaEng 2 Part1 2017Roopa KumarAinda não há avaliações
- Eng Part1 2017Documento2 páginasEng Part1 2017Roopa KumarAinda não há avaliações
- English 1Documento4 páginasEnglish 1Roopa KumarAinda não há avaliações
- 2017 v7 EngDocumento4 páginas2017 v7 EngRoopa KumarAinda não há avaliações
- 2017 v7 EngDocumento4 páginas2017 v7 EngRoopa KumarAinda não há avaliações
- Good English Part1 v2 2017Documento2 páginasGood English Part1 v2 2017Roopa KumarAinda não há avaliações
- 2017 v7 EngDocumento4 páginas2017 v7 EngRoopa KumarAinda não há avaliações
- 2017 v7 EngDocumento4 páginas2017 v7 EngRoopa KumarAinda não há avaliações
- Good English Part1 VQ 2017Documento2 páginasGood English Part1 VQ 2017Roopa KumarAinda não há avaliações
- 2017 v7 EngDocumento4 páginas2017 v7 EngRoopa KumarAinda não há avaliações
- American EngDocumento5 páginasAmerican EngRoopa KumarAinda não há avaliações
- American EngDocumento5 páginasAmerican EngRoopa KumarAinda não há avaliações
- Good English Part1 2017Documento6 páginasGood English Part1 2017Roopa KumarAinda não há avaliações
- American EngDocumento5 páginasAmerican EngRoopa KumarAinda não há avaliações
- American EngDocumento5 páginasAmerican EngRoopa KumarAinda não há avaliações
- American EngDocumento5 páginasAmerican EngRoopa KumarAinda não há avaliações
- American EngDocumento5 páginasAmerican EngRoopa KumarAinda não há avaliações
- American EngDocumento5 páginasAmerican EngRoopa KumarAinda não há avaliações
- Learn-Kannada in 30 DaysDocumento16 páginasLearn-Kannada in 30 DaysSatish Reddy Kunduru92% (12)
- American Eng2000Documento5 páginasAmerican Eng2000Roopa KumarAinda não há avaliações
- All LearnDocumento3 páginasAll LearnRoopa KumarAinda não há avaliações
- sb6 Unit 7Documento6 páginassb6 Unit 7Roopa KumarAinda não há avaliações
- Or Tho Rehab NeckDocumento6 páginasOr Tho Rehab NeckRobert ChuAinda não há avaliações
- Ortho: Spine Conditioning ProgramDocumento7 páginasOrtho: Spine Conditioning ProgramDrYoyoAinda não há avaliações
- Sb6 Culture 1Documento2 páginasSb6 Culture 1Roopa KumarAinda não há avaliações
- Syncsort - An Overview: Syncsort - Doc Page 1 of 6Documento6 páginasSyncsort - An Overview: Syncsort - Doc Page 1 of 6shimpoAinda não há avaliações
- ThoracentesisDocumento1 páginaThoracentesisNiño Cris PatiñoAinda não há avaliações
- Struktur Permukaan BumiDocumento162 páginasStruktur Permukaan BumifitrawatiAinda não há avaliações
- What Is The Differential Diagnosis For The Breast Mass in An Adolescent?Documento4 páginasWhat Is The Differential Diagnosis For The Breast Mass in An Adolescent?theodore_estradaAinda não há avaliações
- MPC-CPN Basics of Toxicology-HDocumento12 páginasMPC-CPN Basics of Toxicology-HNahid ParveenAinda não há avaliações
- Health and Family Welfare (C) Department: PreambleDocumento14 páginasHealth and Family Welfare (C) Department: PreambleAjish BenjaminAinda não há avaliações
- MestastaseDocumento10 páginasMestastaseCahyono YudiantoAinda não há avaliações
- 01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFDocumento26 páginas01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFawinsyAinda não há avaliações
- Assignment On DislysisDocumento10 páginasAssignment On DislysisSanhati Ghosh Banerjee100% (1)
- Steroids Other Appearance Performance Enhancing Drugs Apeds Research ReportDocumento34 páginasSteroids Other Appearance Performance Enhancing Drugs Apeds Research ReportFit and LiftAinda não há avaliações
- The Ivf Pack 2 PDFDocumento11 páginasThe Ivf Pack 2 PDFPaula BošnjakAinda não há avaliações
- VTR 214 PDFDocumento2 páginasVTR 214 PDFKimberly AndrzejewskiAinda não há avaliações
- सञ्चयकर्ता स्वास्थ्योपचार योजना सञ्चालन कार्यविधि, २०७७-50e1Documento13 páginasसञ्चयकर्ता स्वास्थ्योपचार योजना सञ्चालन कार्यविधि, २०७७-50e1crystalconsultancy22Ainda não há avaliações
- Priyanka Sen Final Practice School Internship ReportDocumento35 páginasPriyanka Sen Final Practice School Internship ReportThakur Aditya PratapAinda não há avaliações
- Rog Final MDDocumento5 páginasRog Final MDSaiAinda não há avaliações
- Graves Disease in ChildrenDocumento7 páginasGraves Disease in ChildrengarethAinda não há avaliações
- Diabetesmeds AcceptablecombDocumento2 páginasDiabetesmeds AcceptablecombCotton LogicAinda não há avaliações
- Referral LetterDocumento3 páginasReferral LetterMa. Thea Diane BillonesAinda não há avaliações
- Bates Physical Exam Video NotesDocumento3 páginasBates Physical Exam Video Notesdulcedeleche12359Ainda não há avaliações
- Chapter 21 - Nursing Care of The Family During The Postpartum PeriodDocumento11 páginasChapter 21 - Nursing Care of The Family During The Postpartum PeriodJill Hill100% (3)
- Cover LetterDocumento1 páginaCover Letterapi-400385739Ainda não há avaliações
- The Terrorist Inside My Husband's Brain PDFDocumento5 páginasThe Terrorist Inside My Husband's Brain PDFraymondnomyarAinda não há avaliações
- tmpD824 TMPDocumento12 páginastmpD824 TMPFrontiersAinda não há avaliações
- Pga R3Documento71 páginasPga R3Samruddhi PataitAinda não há avaliações
- HYPOTHYROIDISMDocumento11 páginasHYPOTHYROIDISMVarun SinghAinda não há avaliações
- News Story 3Documento2 páginasNews Story 3api-558280939Ainda não há avaliações
- Abnormal Illness BehaviorDocumento7 páginasAbnormal Illness Behavioransha2011p0% (1)
- Failures in ImplantsDocumento8 páginasFailures in ImplantsDr FarhatAinda não há avaliações
- S: "Masakit Ang Ulo at Tiyan Niya" As Verbalized byDocumento2 páginasS: "Masakit Ang Ulo at Tiyan Niya" As Verbalized bydenise-iceAinda não há avaliações