Escolar Documentos
Profissional Documentos
Cultura Documentos
Ceftazidime
Enviado por
Nakorn Baisri0 notas0% acharam este documento útil (0 voto)
552 visualizações16 páginasFortum
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoFortum
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
552 visualizações16 páginasCeftazidime
Enviado por
Nakorn BaisriFortum
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 16
Ceftazidime
Ceptaz | Fortaz | Tazicef | Tazidime
Drug Information Provided by Gold Standard
Classifications
Antiinfective Agents
Cephalosporins
Third-generation cephalosporins
Description: Ceftazidime is a parenteral third-generation cephalosporin. As a rule, third-generation
cephalosporins are more active and have a broader spectrum against aerobic gram-negative bacteria than do
either first- or second-generation agents. Ceftazidime, like other third-generation cephalosporins, is less active
against gram-positive organisms than are first-generation drugs. Clinically, ceftazidime is commonly used in
the empiric treatment of fever in neutropenic patients, although the emergence of resistant Enterobacter
cloacae during therapy has been noted. [23601] It also is extremely active against Pseudomonas aeruginosa.
Other therapeutic uses of ceftazidime include lower respiratory tract infections, skin and soft-tissue infections,
urinary tract infections, bone and joint infections, and meningitis. Ceftazidime was approved by the FDA in July
1985 and will come off patent in 1999.
Mechanism of Action: Ceftazidime, a beta-lactam antibiotic like the penicillins, is mainly bactericidal. It
inhibits the third and final stage of bacterial cell wall synthesis by preferentially binding to specific penicillin-
binding proteins (PBPs) that are located inside the bacterial cell wall. Penicillin-binding proteins are
responsible for several steps in the synthesis of the cell wall and are found in quantities of several hundred to
several thousand molecules per bacterial cell. Penicillin-binding proteins vary among different bacterial
species. Thus, the intrinsic activity of ceftazidime as well as the other cephalosporins and penicillins against a
particular organism depends on their ability to gain access to and bind with the necessary PBP.
In particular, ceftazidime preferentially binds to PBP-3 of gram-negative rods. Since PBP-3 is responsible for
formation of the septum during cell division, ceftazidime's inhibition of these proteins causes elongation of the
bacteria, inhibition of bacterial cell division, and breakage of the cell wall resulting in cell lysis and death. Lysis
is mediated by bacterial cell wall autolytic enzymes (i.e., autolysins). The relationship between PBPs and
autolysins is unclear, but it is possible that the beta-lactam antibiotic interferes with an autolysin inhibitor.
Due to the presence of an aminothiazolyl side chain, ceftazidime displays enhanced antibacterial activity
against particularly the Enterobacteriaceae. In addition, because ceftazidime also contains a 2-carboxy-2-
oxypropane imino group, it shows increased activity against Pseudomonas aeruginosa, which gives it an
important advantage over other cephalosporins. Its gram-negative spectrum includes E. coli, Klebsiella, H.
influenzae (including ampicillin-resistant strains), Enterobacter, Proteus, Citrobacter, Morganella, Providencia,
Serratia, Moraxella (Branhamella) catarrhalis, N. meningitidis, N. gonorrhoeae, and Pseudomonas aeruginosa.
Ceftazidime is more active against P. aeruginosa than are the antipseudomonal penicillins and is synergistic
with the aminoglycosides. It is inactive against the anaerobe B. fragilis. Ceftazidime has limited activity
against most gram-positive bacteria including nonpencillinase- and pencillinase-producing staphylococci (e.g.,
S. aureus) and streptococci and offers no clinical advantage over the first-generation cephalosporins in treating
gram-positive infections.
Pharmacokinetics: Ceftazidime is administered intravenously or intramuscularly. It is not absorbed from the
GI tract. Approximately 10% of the circulating drug is protein-bound. Ceftazidime is distributed into most body
tissues and fluids. Average tissue or fluid ceftazidime concentrations after a 2 g IV dose include bile (36.4
mcg/ml), synovial fluid (25.6 mcg/ml), peritoneal fluid (48.6 mcg/ml), sputum (9 mcg/ml), CSF (9.8 mcg/ml),
CSF with inflamed meninges (9.4 mcg/ml), aqueous humor (11 mcg/ml), blister fluid (19.7 mcg/ml), lymphatic
fluid (23.4 mcg/ml), bone (31.1 mcg/ml), heart muscle (12.7 mcg/ml), skin (6.6 mcg/ml), skeletal muscle (9.4
mcg/ml), and myometrium (18.7 mcg/ml). Ceftazidime does cross the placenta. The drug is excreted into the
urine primarily via glomerular filtration; urine concentrations average 2100 mcg/ml after a 500 mg IM dose and
12,000 mcg/ml after a 2 g IV dose. Mean renal clearance is about 100 ml/min. Since there is very little tubular
secretion of the drug, concomitant use of probenecid will not affect the serum levels of ceftazidime. A small
percentage is excreted in breast milk. In patients with normal renal function, the elimination half-life of
ceftazidime is 1.52 hours, but half-life increases as renal function declines.
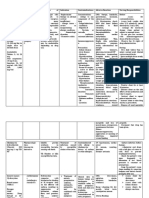
Route-Specific Pharmacokinetics
Intravenous Route
After intravenous (IV) administration of ceftazidime 500 mg, 1g, and 2g doses over 20 to 30 minutes, mean
peak serum concentrations were 42, 69, and 170 mcg/ml, respectively, in normal adult male volunteers.
Serum concentrations at 4 hours after IV dosing were 6, 11, and 13 mcg/ml for the 500 mg, 1g and 2g doses,
respectively; at 8 hours, the concentrations were 2, 3, and 5 mcg/ml, respectively.
Intramuscular Route
After intramuscular (IM) administration of ceftazidime 500mg and 1g doses, mean peak serum concentrations
occurred within 1 hour and were 17 and 39 mcg/ml, respectively, in healthy volunteers. Serum concentrations
remained above 4 mcg/ml for 6 and 8 hours after IM dosing of 500 mg and 1g, respectively.
Special Populations
Hepatic Impairment
Ceftazidime is not metabolized by the liver and hepatic dysfunction does not affect ceftazidime
pharmacokinetics as long as renal function is not impaired.
Renal Impairment
Ceftazidime is almost completely eliminated by the kidneys. Elimination half-life is expected to increase as
renal function declines. In patients with end-stage renal disease, the elimination half-life may be as long as 35
hours. Dosages should be adjusted accordingly (see Dosage, renal impairment). Ceftazidime is removed by
hemodialysis.
Pediatrics
In children, ceftazidime pharmacokinetics may vary with age, weight, renal function, and underlying disease
states (e.g., cystic fibrosis). Neonates exhibit a larger volume of distribution and clearance is dependent on
gestational age and renal function.
2014-01-03T12:37:00
Indications
Acinetobacter sp.
bacteremia
bone and joint infections
bronchiectasis
Burkholderia pseudomallei
Citrobacter diversus
Citrobacter freundii
Citrobacter sp.
Clostridium sp.
Eikenella corrodens
endometritis
Enterobacter aerogenes
Enterobacter agglomerans
Enterobacter cloacae
Enterobacter sp.
Escherichia coli
Eubacterium sp.
febrile neutropenia
gynecologic infections
Haemophilus ducreyi
Haemophilus influenzae (beta-lactamase negative)
Haemophilus influenzae (beta-lactamase positive)
Haemophilus parainfluenzae
intraabdominal infections
Klebsiella oxytoca
Klebsiella pneumoniae
Klebsiella sp.
Lactobacillus sp.
lower respiratory tract infections
melioidosis
meningitis
Moraxella catarrhalis
Morganella morganii
Neisseria gonorrhoeae
Neisseria meningitidis
nosocomial pneumonia
Pasteurella multocida
pelvic cellulitis
Peptococcus sp.
Peptostreptococcus sp.
peritonitis
pneumonia
pneumonia prophylaxis
Propionibacterium sp.
Proteus mirabilis
Proteus vulgaris
Providencia rettgeri
Providencia sp.
Providencia stuartii
Pseudomonas aeruginosa
Pseudomonas sp.
Salmonella sp.
septicemia
Serratia marcescens
Serratia sp.
Shigella sp.
skin and skin structure infections
Staphylococcus aureus (MSSA)
Staphylococcus epidermidis
Streptococcus agalactiae (group B streptococci)
Streptococcus pneumoniae
Streptococcus pyogenes (group A beta-hemolytic streptococci)
urinary tract infection (UTI)
Viridans streptococci
Yersinia enterocolitica
NOTE: To reduce the development of drug-resistant bacteria and maintain the effectiveness of antibacterial
drugs, this drug should be used only to treat or prevent infections that are proven or strongly suspected to be
caused by susceptible bacteria. When culture and susceptibility information are available, they should be
considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and
susceptibility patterns may contribute to the empiric selection of therapy.
Per the manufacturer, this drug has been shown to be active against most strains of the following
microorganisms either in vitro and/or in clinical infections: Acinetobacter sp., Citrobacter diversus,
Citrobacter freundii, Citrobacter sp., Clostridium sp., Enterobacter aerogenes, Enterobacter cloacae,
Enterobacter sp., Escherichia coli, Haemophilus influenzae (beta-lactamase negative), Haemophilus
influenzae (beta-lactamase positive), Haemophilus parainfluenzae, Klebsiella pneumoniae, Klebsiella sp.,
Morganella morganii, Neisseria gonorrhoeae, Neisseria meningitidis, Peptococcus sp., Peptostreptococcus
sp., Proteus mirabilis, Proteus vulgaris, Providencia rettgeri, Providencia sp., Pseudomonas aeruginosa,
Pseudomonas sp., Salmonella sp., Serratia sp., Shigella sp., Staphylococcus aureus (MSSA),
Staphylococcus epidermidis, Streptococcus agalactiae (group B streptococci), Streptococcus pneumoniae,
Streptococcus pyogenes (group A beta-hemolytic streptococci), Yersinia enterocolitica
NOTE: The safety and effectiveness in treating clinical infections due to organisms with in vitro data only have
not been established in adequate and well-controlled clinical trials.
This drug may also have activity against the following microorganisms: Burkholderia pseudomallei,
Eikenella corrodens, Enterobacter agglomerans, Eubacterium sp., Haemophilus ducreyi, Klebsiella oxytoca,
Lactobacillus sp., Moraxella catarrhalis, Pasteurella multocida, Propionibacterium sp., Providencia stuartii,
Serratia marcescens, Viridans streptococci
NOTE: Some organisms may not have been adequately studied during clinical trials; therefore, exclusion from
this list does not necessarily negate the drugs activity against the organism.
For the treatment of meningitis; serious intraabdominal infections (e.g., peritonitis) and gynecologic
infections (e.g., endometritis, pelvic cellulitis); and very severe life-threatening infections (e.g.,
bacteremia, septicemia), especially in immunocompromised patients:
Intravenous or Intramuscular dosage:
Adults and Adolescents: 12 g IV/IM every 8 hours. The higher doses should be used in serious gynecologic
and intra-abdominal infections, meningitis, or severe life-threatening infections, especially in
immunocompromised patients. The usual maximum dosage is 6 g/day.
Elderly: See adult dosage; adjust to renal function; give dose no more frequently than every 12 hours.
Infants > = 1 month and Children: 3050 mg/kg IV every 8 hours (sodium carbonate formulation), maximum
of 6 g/day. Higher doses (e.g., 50 mg/kg IV every 8 hours) should be reserved for CNS infections,
immunocompromised patients, or patients with cystic fibrosis.
Neonates 04 weeks of age weighing < 1200 g: 30 mg/kg IV every 12 hours (sodium carbonate formulation).
Neonates > 7 days of age weighing >= 1200 g: 50 mg/kg IV every 8 hours (sodium carbonate formulation).
Neonates <= 7 days of age weighing 12002000 g: 50 mg/kg IV every 12 hours (sodium carbonate
formulation).
Neonates <= 7 days of age weighing > 2000 g: 100150 mg/kg/day IV divided every 812 hours (sodium
carbonate formulation).
for peritonitis in patients undergoing peritoneal dialysis:
Intravenous or Intramusclar dosage:
Adults and Adolescents: 1 g IV/IM loading dose, followed by 0.5 g IV/IM every 24 hours; some clinicians
recommend 0.5 g IV/IM every 24 hours, with a supplemental 0.5 g IV/IM dose at the end of each dialysis.
Intraperitoneal dosage:
Adults and Adolescents: An intraperitoneal (IP) loading dose of 500 mg/L can be given IP, followed by a
maintenance dose of 125 mg/L of peritoneal dialysate. [24878]
For the treatment of bone and joint infections:
Intravenous dosage:
Adults and Adolescents: 2 g IV every 12 hours.
Elderly: See adult dosage; adjust to renal function; give dose no more frequently than every 12 hours.
Infants > = 1 month and Children: 3050 mg/kg IV every 8 hours (sodium carbonate formulation), maximum
of 6 g/day.
Neonates 04 weeks of age weighing < 1200 g: 30 mg/kg IV every 12 hours (sodium carbonate formulation).
Neonates > 7 days of age weighing >= 1200 g: 50 mg/kg IV every 8 hours (sodium carbonate formulation).
Neonates <= 7 days of age weighing 12002000 g: 50 mg/kg IV every 12 hours (sodium carbonate
formulation).
Neonates <= 7 days of age weighing > 2000 g: 100150 mg/kg/day IV divided every 812 hours (sodium
carbonate formulation).
For the initial management of febrile neutropenia:
Intravenous dosage:
Adults and Adolescents: 2 g IV every 8 hours with or without an aminoglycoside (i.e., gentamicin, tobramycin,
amikacin). Ceftazidime may also be used with vancomycin with or without an aminoglycoside; however, the
use of vancomycin in initial therapy is only recommended when there is a high risk of resistant gram-positive
organisms being involved. [32108] [32109]
Infants > = 1 month and Children: 25 mg/kg IV every 12 hours up to 50 mg/kg IV every 8 hours (sodium
carbonate formulation); maximum of 6 g/day. [32108] [32109]
For the treatment of lower respiratory tract infections (e.g., pneumonia) and skin and skin structure
infections:
for severe lower respiratory tract infections, moderate to severe skin and skin structure infections,
or pulmonary infection secondary to complications of cystic fibrosis (e.g., bronchiectasis):
Intravenous or Intramuscular dosage:
Adults and Adolescents: 12 g IV/IM every 8 hours. The higher doses should be used severe life-threatening
infections, especially in immunocompromised patients or patients with cystic fibrosis. The usual maximum
dosage is 6 g/day.
Elderly: See adult dosage; adjust to renal function; give dose no more frequently than every 12 hours.
Infants >= 1 month and Children: 3050 mg/kg IV every 8 hours (sodium carbonate formulation), maximum of
6 g/day. Higher doses (e.g., 50 mg/kg IV every 8 hours) should be reserved for immunocompromised patients,
or patients with cystic fibrosis. In patients with cystic fibrosis, doses as high as 75 mg/kg IV every 8 hours
have been recommended for the treatment of pulmonary infections due to P. aeruginosa. [24951]
Neonates 04 weeks of age weighing < 1200 g: 30 mg/kg IV every 12 hours (sodium carbonate formulation).
Neonates > 7 days of age weighing >= 1200 g: 50 mg/kg IV every 8 hours (sodium carbonate formulation).
Neonates <= 7 days of age weighing 12002000 g: 50 mg/kg IV every 12 hours (sodium carbonate
formulation).
Neonates <= 7 days of age weighing > 2000 g: 100150 mg/kg/day IV divided every 812 hours (sodium
carbonate formulation).
for uncomplicated lower respiratory tract infections or mild skin and skin structure infections:
Intravenous or Intramuscular dosage:
Adults and Adolescents: 500 mg to 1 g IV/IM every 8 hours.
Elderly: See adult dosage; adjust to renal function; give dose no more frequently than every 12 hours.
Intravenous dosage ( sodium carbonate formulation only):
Infants >= 1 month and Children: 3050 mg/kg IV every 8 hours (sodium carbonate formulation), maximum of
6 g/day.
for the empiric treatment of nosocomial pneumonia, including ventilator-associated pneumonia,
and healthcare-associated pneumonia in patients with late-onset disease or risk factors for
multidrug-resistant organisms:
Intravenous or Intramuscular dosage:
Adults: 2 g IV every 8 hours plus an antipseudomonal fluoroquinolone (ciprofloxacin or levofloxacin) or an
aminoglycoside (amikacin, gentamicin, or tobramycin). If extended-spectrum beta-lactamase-producing
positive (ESBL+) strain such as K. pneumoniae, or an Acinetobacter species is suspected, a carbapenem
(imipenem or meropenem) should be used. If L. pneumophila is suspected, the regimen should include a
macrolide (e.g., azithromycin) or a fluoroquinolone rather than an aminoglycoside. If MRSA suspected,
linezolid or vancomycin should also be included. [33389]
for ventilator-associated pneumonia prophylaxis (VAP):
Inhalation dosage:
Adults: A placebo-controlled study evaluated the safe and effective use of aerosolized ceftazidime for
prevention of ventilator-associated pneumonia (VAP). Forty critically ill trauma patients at high risk for VAP
were randomly assigned to receive via nebulization either ceftazidime 250 mg every 12 hours or placebo
(normal saline) for up to 7 days. Aerosolized ceftazidime significantly reduced the frequency of VAP without
significantly altering bacterial sensitivity patterns in the intensive care unit. The study results also suggested
that aerosolized ceftazidime may attenuate endotoxin-stimulated release of proinflammatory cytokines in the
lung, a mechanism which is thought to be related to decreased development of VAP. [27015]
For the treatment of urinary tract infection (UTI):
Intravenous or Intramuscular dosage:
Adults and Adolescents: 250 mg IV or IM every 12 hours for an uncomplicated UTI or 500 mg IV or IM every 8
12 hours for a complicated UTI. [29916] [49880]
Infants and Children: 3050 mg/kg IV every 8 hours to a maximum dose of 6 g/day. The higher dose should
be reserved for immunocompromised pediatric patients. [29916]
Neonates: 30 mg/kg IV every 12 hours. [29916]
For the treatment of melioidosis due to Burkholderia pseudomallei:
for severe systemic melioidosis:
Intravenous dosage:
Adults, Adolescents, and Children: 100120 mg/kg/day IV in 3 divided doses given in combination with
sulfamethoxazole; trimethoprim IV for at least 1014 days. Or, ceftazidime may be given with ciprofloxacin for
2 weeks. If clinical improvement is achieved, switch to oral maintenance combination therapy with
sulfamethoxazole; trimethoprim and doxycycline for 36 months (with or without an initial 4-week regimen of
chloramphenicol). Oral amoxicillin; clavulanic acid alone may be used as a 2nd-line maintenance agent in
adults and as 1st-line in children and pregnant women. [31391] [31392] [31393]
for B. pseudomallei bacteremia:
Intravenous dosage:
Adults, Adolescents and Children: 100120 mg/kg/day IV in 3 divided doses given alone or in combination
with sulfamethoxazole; trimethoprim or doxycycline for at least 1014 days. If clinical improvement is
achieved, switch to oral maintenance combination therapy with sulfamethoxazole; trimethoprim and
doxycycline for 36 months (with or without an initial 4-week regimen of chloramphenicol). Oral amoxicillin;
clavulanic acid alone may be used as a 2nd-line maintenance agent in adults and as 1st-line in children and
pregnant women. [31391] [31392] [31393]
Maximum Dosage Limits:
Adults
6 g/day IM/IV.
Geriatric
6 g/day IM/IV.
Adolescents
6 g/day IM/IV.
Children
150 mg/kg/day IM/IV, not to exceed 6 g/day IM/IV.
Infants
>= 1 month: 150 mg/kg/day IM/IV.
Neonates
Individualize based on weight, post-natal age, and indication for use.
Patients with Hepatic Impairment Dosing
No dosage adjustment needed. [29916]
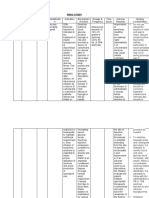
Patients with Renal Impairment Dosing
FDA-labeled renal adjustment: [29916]
NOTE: In patients with severe infections who would normally receive a 6 g/day dose were it not for renal
impairment, the adjusted renal dose listed below may be increased by 50% or the dosing frequency listed
below may be increased appropriately. Further dosing should be determined by therapeutic monitoring,
severity of the infection, and susceptibility of the causative organism.
CrCl > 50 ml/min: no dosage adjustment needed.
CrCl 3150 ml/min: 1 g IV/IM every 12 hours.
CrCl 1630 ml/min: 1 g IV/IM every 24 hours.
CrCl 615 ml/min: 1 g IV/IM loading dose, then 500 mg IV/IM every 24 hours.
CrCl < 5 ml/min: 1 g IV/IM loading dose, then 500 mg IV/IM every 48 hours.
Alternative guideline renal adjustment: [32569]
CrCl > 50 ml/min: 12 g IV/IM every 812 hours.
CrCl 1050 ml/min: 12 g IV/IM every 1224 hours.
CrCl < 10 ml/min: 12 g IV/IM every 2448 hours.
Intermittent hemodialysis
In adults, give an initial 1 g IV loading dose, then a 1 g IV dose after each standard dialysis session. [29916]
[32569]
Continuous renal replacement therapy (CRRT)
A dose of 12 g every 12 hours or a 2 g load then a 3 g/day continuous infusion is recommended. [32569]
Ceftazidime is significantly removed by CAVHD or CVVHD. A daily dose 2.4 times that used for anuric non
dialyzed patients has been recommended, assuming a combined dialysis and ultrafiltrate flow rate of 1.5 L/hr.
[24879]
Peritoneal dialysis:
In adults, give 1 g IV/IM loading dose, then 500 mg IV/IM every 24 hours. In addition to IV use, the drug may
be added to the peritoneal dialysis fluid at a concentration of 250 mg per 2 L dialysate. [29916] [32569]
Plasmapheresis:
Administer IV doses at least 2 hours before plasmapheresis and IM doses at least 3 hours before
plasmapheresis. [33359] [33362]
non-FDA-approved indication
Administration
General Administration Information
For storage information, see specific product information within the How Supplied section.
Route-Specific Administration
Injectable Administration
Ceftazidime is administered intravenously or intramuscularly.
Visually inspect parenteral products for particulate matter and discoloration whenever solution and
container permit.
Intravenous Administration
Reconstitution:
Sodium carbonate formulations (Fortaz, Tazicef, or Tazidime) produce carbon
dioxide gas upon reconstitution; arginine (Ceptaz) formulations do not.
Infusion packs of Fortaz, Tazicef, or Tazidime: reconstitute 1 or 2 g with 100 ml of
sterile water for injection or a compatible IV solution to give concentrations of 10 or
20 mg/ml, respectively. Reconstitution should be in two stages. First, inject 10 ml of
the diluent into the pack and shake well to dissolve the drug; the solution should
become clear within 12 minutes. Pressure inside the container will increase due
to CO
2
production. To release pressure, insert a vent needle only after the drug has
completely dissolved. Add the remaining diluent and remove the vent needle.
Infusion packs of Ceptaz: reconstitute 1 or 2 g with 100 ml of sterile water for
injection or a compatible IV solution to give concentrations of 10 or 20 mg/ml,
respectively. Reconstitution should be in two stages. First, inject 10 ml of the diluent
into the pack and shake well to dissolve the drug; the solution should become clear
within 12 minutes. Add the remaining diluent. Insert a vent needle only after
positive pressure is generated. Remove the vent needle before administration.
Vials of Fortaz, Tazicef, or Tazidime: reconstitute 500 mg, 1 g, or 2 g with 5, 10, or
10 ml, respectively, of sterile water for injection or a compatible IV solution to give
concentrations of 100, 95100, or 170180 mg/ml, respectively. Shake well to
dissolve the drug; the solution should become clear within 12 minutes.
Vials of Ceptaz: reconstitute 1 or 2 g with 10 ml of sterile water for injection or a
compatible IV solution to give concentrations of 9095 or 170180 mg/ml,
respectively.
Pharmacy bulk packages of Fortaz, Tazicef, or Tazidime: reconstitute 6 grams with
26 ml of a compatible solution to give a concentration of 200 mg/m. Pressure inside
the container will increase due to CO
2
production. To release pressure, insert a vent
needle only after the drug has completely dissolved. Remove the vent needle before
using solution. FURTHER DILUTION IS REQUIRED.
Pharmacy bulk packages of Ceptaz: reconstitute 10 grams with 40 ml of a
compatible solution to give a concentration of 200 mg/ml. FURTHER DILUTION IS
REQUIRED.
ADD-Vantage vials of Fortaz or Tazidime: for IV infusion only. Reconstitute 1 or 2 g
with NS, 1/2NS, or D
5
W in the appropriate 50 or 100 ml flexible diluent container.
Pressure inside the container will increase due to CO
2
production. To release
pressure, insert a vent needle only after the drug has completely dissolved. Remove
the vent needle before using solution.
ADD-Vantage vials of Ceptaz: for IV infusion only. Reconstitute 1 or 2 g with NS,
1/2NS, or D
5
W in the appropriate 50 or 100 ml flexible diluent container.
Intermittent IV infusion:
Vials: withdraw the appropriate dose, making sure that the needle opening remains
in the solution. Add to a compatible IV solution ensuring that no CO
2
bubbles are
present in the syringe.
Infusion packs and ADD-Vantage systems: are ready for infusion after
reconstitution (see above).
Pharmacy bulk packages: withdraw appropriate dose and dilute in a compatible IV
solution.
Infuse IV over 1530 minutes.
Direct intermittent IV infusion:
Vials: withdraw the appropriate dose, making sure that the needle opening remains
in the solution. Ensure that no CO
2
bubbles are present in the syringe before
injection.
Inject directly into a vein over 35 minutes or slowly into the tubing of a freely-
flowing compatible IV solution.
Intramuscular Administration
Vials of Fortaz and Tazidime: reconstitute 500 mg or 1 g with 1.5 or 3 ml,
respectively, of sterile or bacteriostatic water for injection or 0.51% lidocaine HCl
to give solutions containing approx. = 280 mg/ml.
Vials of Tazicef: reconstitute 1 g with 3 ml of sterile water for injection to give
solutions containing approx. = 280 mg/ml.
Vials of Ceptaz: reconstitute 1 g with 3 ml of sterile or bacteriostatic water for
injection or 0.51% lidocaine HCl to give solutions containing approx. = 250
mg/ml.
Withdraw the appropriate dose, making sure that the needle opening remains in the
solution. Ensure that no CO
2
bubbles are present in the syringe before injection.
Inject deeply into a large muscle (i.e., upper outer quadrant of the gluteus maximus
or lateral part of the thigh). Aspirate prior to injection to avoid injection into a blood
vessel.
Contraindications
antimicrobial resistance
breast-feeding
cephalosporin hypersensitivity
coagulopathy
colitis
diarrhea
geriatric
GI disease
inflammatory bowel disease
penicillin hypersensitivity
pregnancy
pseudomembranous colitis
renal failure
renal impairment
ulcerative colitis
viral infection
vitamin K deficiency
The administration of ceftazidime may result in a false-positive reaction for glucose in the urine in patients with
diabetes mellitus using CLINITEST tablets, Benedict's solution, or Fehling's solution. It is recommended that
glucose tests based on enzymatic glucose oxidase reactions (such as CLINISTIX) be used.The administration
of ceftazidime may result in a false-positive reaction for glucose in the urine in patients with diabetes mellitus
using CLINITEST tablets, Benedict's solution, or Fehling's solution. It is recommended that glucose tests
based on enzymatic glucose oxidase reactions (such as CLINISTIX) be used.
Ceftazidime does not treat viral infection (e.g., common cold). Prescribing ceftazidime in the absence of a
proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the
patient and increases the risk of the development of drug-resistant bacteria (antimicrobial resistance). Patients
should be told to complete the full course of treatment, even if they feel better earlier.
Ceftazidime is contraindicated in patients with cephalosporin hypersensitivity or cephamycin hypersensitivity.
Ceftazidime should be used cautiously in patients with hypersensitivity to penicillin. The structural similarity
between ceftazidime and penicillin means that cross-reactivity can occur. Penicillins can cause a variety of
hypersensitivity reactions ranging from mild rash to fatal anaphylaxis. Patients who have experienced severe
penicillin hypersensitivity should not receive ceftazidime. Cross-reactivity to cephalosporins is approximately 3
7% with a documented history to penicillin.
Almost all antibacterial agents, including ceftazidime, have been associated with pseudomembranous colitis
(antibiotic-associated colitis) which may range in severity from mild to life-threatening. In the colon, overgrowth
of Clostridia may exist when normal flora is altered subsequent to antibacterial administration. The toxin
produced by Clostridium difficile is a primary cause of pseudomembranous colitis. It is known that systemic
use of antibiotics predisposes patients to development of pseudomembranous colitis. Consideration should be
given to the diagnosis of pseudomembranous colitis in patients presenting with diarrhea following antibacterial
administration. Systemic antibiotics should be prescribed with caution to patients with inflammatory bowel
disease such as ulcerative colitis or other GI disease. If diarrhea develops during therapy, the drug should be
discontinued. Following diagnosis of pseudomembranous colitis, therapeutic measures should be instituted. In
milder cases, the colitis may respond to discontinuation of the offending agent. In moderate to severe cases,
fluids and electrolytes, protein supplementation, and treatment with an antibacterial effective against
Clostridium difficile may be warranted. Products inhibiting peristalsis are contraindicated in this clinical
situation. Practitioners should be aware that antibiotic-associated colitis has been observed to occur over two
months or more following discontinuation of systemic antibiotic therapy; a careful medical history should be
taken.
All cephalosporins, including ceftazidime, may rarely cause hypothrombinemia and have the potential to cause
bleeding. Cephalosporins which contain the NMTT side chain (e.g., cefoperazone, cefamandole, cefotetan)
have been associated with an increased risk for bleeding. Cephalosporins should be used cautiously in
patients with a preexisting coagulopathy (e.g., vitamin K deficiency) since these patients are at a higher risk
for developing bleeding complications.
Ceftazidime should be used with caution in patients with renal impairment or renal failure since the drug is
eliminated via renal mechanisms. High and prolonged serum ceftazidime concentrations can occur from usual
dosages in patients with transient or persistent reduction of urinary output because of renal insufficiency.
Elevated levels of ceftazidime in patients with renal insufficiency can lead to neurotoxicity, including seizures,
encephalopathy, asterixis, neuromuscular excitability, and myoclonia. Dosage and dose frequency should be
adjusted in patients with impaired renal function (see Dosage, renal impairment). No overall differences in
safety or effectiveness were observed between the geriatric and younger adult subjects in clinical trials or other
reported clinical experience. However, because elderly patients are more likely to have decreased renal
function, care should be taken in ceftazidime dose selection, and it may be useful to monitor renal function.
Ceftazidime is classified as FDA pregnancy risk category B. Animal data reveal no teratogenic effects. There
are, however, no adequate and well-controlled studies in pregnant women. Because animal studies are not
always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Ceftazidime has not been studied for use during labor and delivery. Treatment should be given only if clearly
needed.
Ceftazidime is excreted in human breast milk in small quantities. The manufacturer recommends to exercise
caution with use during breast-feeding. [29916] Rare potential complications in the nursing infant include
alterations of gut flora that might result in diarrhea or related complications (e.g., dehydration). Because the
risk of serious reactions is relatively rare, the use of many cephalosporins is considered compatible with
breast feeding. Ceftazidime is generally considered compatible for use for breast-feeding women by the
American Academy of Pediatrics (AAP). [27500] Consider the benefits of breast-feeding, the risk of potential
infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant
experiences an adverse effect related to a maternally administered drug, healthcare providers are encouraged
to report the adverse effect to the FDA.
Interactions
Aminoglycosides
Anticoagulants
Chloramphenicol
Loop diuretics
Macrolides
Polymyxin B
Probenecid
Tetracyclines
Vancomycin
Concominant use of some cephalosporins with nephrotoxic drugs, such as vancomycin, polymyxin B, colistin,
loop diuretics, and aminoglycosides, increases the risk of developing nephrotoxicity. [6664] This problem was
noted mainly with the older cephalosporin, cephaloridine. Ceftazidime is not generally considered a
nephrotoxic drug.
As with other cephalosporins, cefotazidime may have additive or synergistic activity with aminoglycosides,
aztreonam, carbapenems, and the penicillins in its bactericidal effects. Concomitant use of ceftazidime with
the aminoglycosides may be desirable due to synergistic activity against some strains of Pseudomonas
aeruginosa and Enterobacteriaceae. [6664] Concomitant use of ceftazidime with clavulanic acid can result in
synergistic activiy against some strains of B. fragilis that are resistant to ceftazidime alone.
Since there is very little tubular secretion of ceftazidime, co-administration of probenecid should not
significantly increase ceftazidime serum concentrations. [6664]
Concomitant use of cephalosporins and some bacteriostatic antibiotics, such as chloramphenicol, have
interfered with the bactericidal activity of the cephalosporins. [6664] Many texts warn not to use bacteriostatic
and bactericidal antibiotics together since the bactericidal actions of, for example, a penicillin may be inhibited
by the bacteriostatic agent. The clinical significance of these interactions is debatable. The classic
explanation of this antagonism is that the bacteriostatic antimicrobial agent inhibits the growth of the target
organism, and interferes with the action of the bactericidal agent, which is dependent on cell growth/replication
for proper activity. [5677] However, despite reports of pharmacologic antagonism in vitro with such
combinations, few clinical data to substantiate in vivo antagonism exist. [5677] Combination antimicrobial
therapy has been a useful strategy for treating clinical infections. For example, the concomitant clinical use of
cephalosporins and tetracyclines (e.g., doxycycline) is common in some mixed bacterial infections without
loss of clinical efficacy of either agent. Similarly, many mixed bacterial infections are treated safely and
efficaciously with the concomitant administration of cephalosporins and macrolides (e.g., azithromycin,
clarithromycin, erythromycin). Although the potential for antagonism should be considered when prescribing
antibiotics, in general it is safe to administer combinations, refining treatment based on the nature of the
clinical infection and individual parameters such as susceptibility data.
Cephalosporins have been associated with decreased prothrombin activity. Cephalosporins with a
methylthiotetrazole (MTT) side ring (e.g., cefamandole, cefotetan, cefoperazone) are more frequently
associated with hypoprothrombinemic activity. Decreased vitamin K activity due to depletion of gut flora may
also be a contributing factor. Patients previously stabilized on anticoagulants may be at an increased risk for
prolonged prothrombin time. Cephalosporins should be used cautiously when administered to patients already
receiving anticoagulants. [5279] [6664]
Adverse Reactions
abdominal pain
acute generalized exanthematous pustulosis (AGEP)
agranulocytosis
angioedema
aplastic anemia
asterixis
bronchospasm
candidiasis
cholestasis
coma
diarrhea
dizziness
elevated hepatic enzymes
encephalopathy
eosinophilia
erythema multiforme
fever
headache
hemolytic anemia
hyperbilirubinemia
hypoprothrombinemia
hypotension
injection site reaction
interstitial nephritis
jaundice
leukopenia
lymphocytosis
maculopapular rash
myoclonia
nausea
neutropenia
pancytopenia
paresthesias
phlebitis
pruritus
pseudomembranous colitis
seizures
Stevens-Johnson syndrome
superinfection
thrombocytopenia
thrombocytosis
toxic epidermal necrolysis
urticaria
vaginitis
vomiting
An injection site reaction following intramuscular (IM) injection has been reported in fewer than 2% of
ceftazidime patients. Phlebitis and inflammation at the injection site were the most common reactions. Pain
and induration have also been reported post-marketing. [29916]
Gastrointestinal reactions were reported in fewer than 2% of ceftazidime patients. The most frequently reported
were diarrhea (1 in 78), nausea (1 in 156), vomiting (1 in 500), and abdominal pain (1 in 416). It should be
noted that treatment with antibiotics can alter the normal intestinal flora, resulting in overgrowth of other
organisms and superinfection. Prolonged antibiotic use is more likely to result in an overgrowth of non-
susceptible organisms such as Candida and Clostridium difficile. Diarrhea may be indicative of an antibiotic-
associated colitis, and the possible development of pseudomembranous colitis from toxins produced by
Clostridium difficile should be considered. Clostridium difficile associated diarrhea (CDAD) may range in
severity from mild diarrhea to fatal colitis. If CDAD is suspected or confirmed, ongoing antibiotic use not
directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management,
protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as
clinically indicated. Pseudomembranous colitis can occur during use of or following discontinuance of
ceftazidime, but this effect is rare. Candidiasis (including oral thrush) and vaginitis were reported in fewer than
1% of patients. [29916]
Transient agranulocytosis, neutropenia, leukopenia, lymphocytosis, and thrombocytopenia have been reported
rarely with cephalosporin antibiotics. Other adverse effects seen with ceftazidime therapy include hemolytic
anemia (rare), eosinophilia (7.7%), positive Coombs' test without hemolysis (4.3%), and thrombocytosis
(2.2%). As with some other cephalosporins, transient elevations of blood urea, blood urea nitrogen, and/or
serum creatinine were observed occasionally. Prolonged prothrombin time (hypoprothrombinemia), false-
positive test for urinary glucose, pancytopenia, hemorrhage, and aplastic anemia were all reported during
postmarketing surveillance. [29916]
Central nervous system adverse reactions reported in < 1% of patients during ceftazidime therapy have
included dizziness, headache, and paresthesias. Seizures are rare, but a serious complication of
cephalosporin therapy. More commonly associated with penicillins, the epileptogenic properties of both
penicillins and cephalosporins are thought to be related to their beta-lactam ring. High doses and renal
impairment are associated with an increased risk of seizures. [23981] Encephalopathy, coma, asterixis,
neuromuscular excitability, and myoclonia have been reported in renally impaired patients treated with
unadjusted dosage regimens of ceftazidime. [29916]
Hypersensitivity reactions were reported in 2% of ceftazidime patients as pruritus, maculopapular rash, and
fever. Immediate hypersensitivity reactions, generally manifested by rash and/or pruritus, occurred in 1 in 285
patients. Toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme have also been
reported with cephalosporin antibiotics, including ceftazidime. Angioedema and anaphylaxis (bronchospasm
and/or hypotension) have been reported very rarely. Interstitial nephritis, a hypersensitivity reaction, has been
reported in < 1% of patients receiving other cephalosporins, but has not been reported with ceftazidime.
[44649] Anaphylaxis; allergic reactions, which, in rare instances, were severe (e.g., cardiopulmonary arrest);
and urticaria were reported during postmarketing surveillance. [29916]
Ceftazidime has been associated with acute generalized exanthematous pustulosis (AGEP). The nonfollicular,
pustular, erythematous rash starts suddenly, is associated with fever above 38 degrees C, and is distinct from
pustular psoriasis, although biopsy results in each reveal spongiform subcorneal pustules. Drugs are the main
cause of AGEP. A period of 23 weeks after an inciting drug exposure appears necessary for a first episode
of AGEP. Unintentional reexposure may cause a second episode within 2 days. Clinical presentation is
diverse with cutaneous lesions beyond erythema and pustules present in half of the cases. For example,
bullous lesions, edema, purpura, pruritus, and mucosal erosions are possible. The mean duration of the
pustules is 9.7 days followed by an annular desquamation, as long as the causative drug or factor is
discontinued. The physiopathological mechanisms of AGEP have not been determined but the pathological
criteria of edema, leukocytoclastic vasculitis, eosinophil exocytosis, and keratinocyte focal necrosis are
distinctive. Pustule confluence or very small pustules may lead a clinician to make an incorrect diagnosis of
TEN, of drug-induced erythroderma, or of staphylococcal scalded skin syndrome. [27736]
Laboratory test changes during ceftazidime therapy were transient and included slight elevated hepatic
enzymes of one or more tests: AST: 1 in 16, ALT: 1 in 15, LDH: 1 in 18, GGT: 1 in 19, and alkaline
phosphatase: 1 in 23. Cholestasis, jaundice, and hyperbilirubinemia have been reported rarely during
postmarketing surveillance of ceftazidime. [29916]
Monitoring Parameters
serum creatinine/BUN
References
5279: Coumadin (warfarin) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2007 Aug.
5677: Cohn JR, Jungkind DL, Baker JS. In vitro antagonism by erythromycin of the bactericidal action
of antimicrobial agents against common respiratory pathogens. Antimicrob Agents Chemother
1980;18:8726.
6664: Ceptaz (ceftazidime for injection) L-arginine formulation package insert. Research Triangle
Park, NC: GlaxoSmithKline; 2002 Apr.
23601: Quinn JP, DiVincenzo CA, Foster J. Emergence of resistance to ceftazidime during therapy for
Enterobacter cloacae infections. J Inf Dis 1987;155:942-7.
23981: Nicholls PJ. Neurotoxicity of penicillins. J Antimicrob Chemother 1980;6:161-72.
24878: Keane WF, Everett ED, Golper TA, et al. Peritoneal dialysis-related peritonitis treatment
recommendations, 1993 update. Perit Dial Int 1993;13:21.
24879: Reetze-Bonorden P, Bohler J, Keller E. Drug dosage in patients during continuous renal
replacement therapy. Clin Pharmacokinet 1993;24:362-79.
24951: Ramsey BW. Management of pulmonary disease in patients with cystic fibrosis. N Engl J Med
1996;335:179-88.
27015: Wood GC, Boucher BA, Croce MA, et al. Aerosolized ceftazidime for prevention of ventilator-
associated pneumonia and drug effects on the proinflammatory response in critically ill trauma patients.
Pharmacotherapy 2002;22:972-982.
27500: American Academy of Pediatrics (AAP) Committee on Drugs. Transfer of drugs and other
chemicals into human milk. Pediatrics 2001;108:776-89.
27736: Beylot C, Doutre M, Beylot-Barry M. Acute generalized exanthematous pustulosis. Semin
Cutan Med Surg 1996;15(4):244-249.
29916: Fortaz (ceftazidime for injection) package insert. Research Triangle Park, NC: GlaxoSmithKline
LLC; 2010 Aug.
31391: Raja NS, Ahmed MZ, Singh NN. Melioidosis: an emerging infectious disease. J Postgrad Med
2005;51(2):140-145.
31392: Cheng AC, Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin
Microbiol Rev 2005;18(2):383-416.
31393: White NJ. Melioidosis. Lancet 2003;361:1715-22.
32108: Paul M, Yahav D, Fraser A, et al. Empirical antibiotic monotherapy for febrile neutropenia:
systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother
2006;57:176-189.
32109: Hughes WT, Armstrong D, Bodey GP, et al. 2002 Guidelines fo the use of antimicrobial agents
in neutropenic patients with cancer. Clin Infect Dis 2002;34:730-51.
32569: Aronoff GR, Bennett WM, Berns JS, et al. Drug prescribing in renal failure: dosing guidelines for
adults and children, 5th ed. Philadelphia: American College of Physicians; 2007.
33359: Kintzel PE, Eastlund T, Calis KA. Extracorporeal removal of antimicrobials during
plasmapheresis. J Clin Apher 2003;18(4):194-205.
33362: Bozkurt F, Schollmeyer P, Keller E. Kinetics of ceftazidime during plasmapheresis. Eur J Clin
Pharmacol 1987;33(2):197-201.
33389: American Thoracic Society; Infectious Diseases Society of America. Guidelines for the
management of adults with hospital-acquired, ventilator-associated, and healthcare-associated
pneumonia. Am J Respir Crit Care Med 2005;171(4):388-416.
44649: Andes DR, Craig WA. Cephalosporins. In: Mandell GL, Bennett JE, Dolin R, eds. Principles
and Practice of Infectious Diseases, 7th ed. New York: Churchill Livingstone; 2009:323-39.
49880: Gupta K, Hooton TM, Naber KG, at al. International clinical practice guidelines for the treatment
of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases
Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis
2011;52:e103-e120.
Você também pode gostar
- LOSARTANDocumento3 páginasLOSARTANReinell GoAinda não há avaliações
- Drug Study - CefradoxilDocumento13 páginasDrug Study - CefradoxilJohara G'naid0% (1)
- PrednisoneDocumento3 páginasPrednisoneMaja DeraAinda não há avaliações
- PROPYLTHIOURACILDocumento35 páginasPROPYLTHIOURACILMagdy Ali ELsherbenyAinda não há avaliações
- JINANG's Drug Data SummaryDocumento4 páginasJINANG's Drug Data SummaryiammaiaAinda não há avaliações
- Omeprazole, Potassium Chloride, Citicoline, GlimepirideDocumento5 páginasOmeprazole, Potassium Chloride, Citicoline, GlimepirideJenivic Empig PuedanAinda não há avaliações
- A) First Degree Burns (Superficial Burns)Documento4 páginasA) First Degree Burns (Superficial Burns)Art Christian RamosAinda não há avaliações
- Ertapenem (Invanz)Documento1 páginaErtapenem (Invanz)Adrianne BazoAinda não há avaliações
- PrednisoneDocumento22 páginasPrednisoneAlthea AlicandoAinda não há avaliações
- Drug Study MetforminDocumento5 páginasDrug Study MetforminSabita PaudelAinda não há avaliações
- Insulin Mechanism of Action and Nursing ResponsibilitiesDocumento7 páginasInsulin Mechanism of Action and Nursing ResponsibilitiesGrape JuiceAinda não há avaliações
- AtroventDocumento2 páginasAtroventKatie McPeekAinda não há avaliações
- Drug Study - TerbutalineDocumento2 páginasDrug Study - TerbutalineRock With YouAinda não há avaliações
- DRUG STUDY PATIENT PROFILEDocumento2 páginasDRUG STUDY PATIENT PROFILEYakumaAinda não há avaliações
- AlgesiaDocumento1 páginaAlgesiaSaf DicamAinda não há avaliações
- Amiodarone (PACERONE)Documento1 páginaAmiodarone (PACERONE)Amanda CoadAinda não há avaliações
- Azathioprine Drug StudyDocumento1 páginaAzathioprine Drug StudyAlexa Lexington Rae Zagado100% (1)
- DrugStudy - CamaristaColeenMaeC (BSN III-G) (Prednisone)Documento2 páginasDrugStudy - CamaristaColeenMaeC (BSN III-G) (Prednisone)Coleen Mae CamaristaAinda não há avaliações
- P 398Documento1 páginaP 398Arup Ratan PaulAinda não há avaliações
- Lasilactone PI 201801Documento9 páginasLasilactone PI 201801Shivam GuptaAinda não há avaliações
- Drug Study - BaclofenDocumento5 páginasDrug Study - BaclofenRocco WalksAinda não há avaliações
- Drug StudyDocumento3 páginasDrug StudyKwin SaludaresAinda não há avaliações
- Glipizide Glucotrol XL Drug CardDocumento1 páginaGlipizide Glucotrol XL Drug CardSheri490Ainda não há avaliações
- OxaliplatinDocumento10 páginasOxaliplatinlum_albertAinda não há avaliações
- Course in The Ward Date, Doctor'S Order AnalysisDocumento8 páginasCourse in The Ward Date, Doctor'S Order AnalysisbillyktoubattsAinda não há avaliações
- Dobutamine It Stimulates Heart Muscle and Improves Blood Flow by Helping The Heart Pump BetterDocumento3 páginasDobutamine It Stimulates Heart Muscle and Improves Blood Flow by Helping The Heart Pump BetterJinky Nacar DomingoAinda não há avaliações
- Filgrastim Boosts Neutrophil Recovery After ChemotherapyDocumento3 páginasFilgrastim Boosts Neutrophil Recovery After ChemotherapyKyla Barrera TabungarAinda não há avaliações
- CoversylDocumento3 páginasCoversylianecunarAinda não há avaliações
- New DS3Documento3 páginasNew DS3dakieAinda não há avaliações
- TB Drug StudyDocumento15 páginasTB Drug StudyKaloy KamaoAinda não há avaliações
- Indometacin MonographDocumento9 páginasIndometacin MonographQuiKe PvAinda não há avaliações
- Suxamethonium Chloride Injection BP Product Information SummaryDocumento8 páginasSuxamethonium Chloride Injection BP Product Information SummarynanaAinda não há avaliações
- Name Mucosta Tablets 100 Description PDFDocumento7 páginasName Mucosta Tablets 100 Description PDFnanda RaharjaAinda não há avaliações
- Drug - Htm#description.: Reference: Submitted By: Date Submitted: Submitted ToDocumento2 páginasDrug - Htm#description.: Reference: Submitted By: Date Submitted: Submitted ToSHEILA MAE SACLOTAinda não há avaliações
- Meloxicam drug study overviewDocumento5 páginasMeloxicam drug study overviewABARAJAinda não há avaliações
- AzithromycinDocumento4 páginasAzithromycinBrittany ClontzAinda não há avaliações
- Case Pre Drug StudyDocumento5 páginasCase Pre Drug StudyJoule PeirreAinda não há avaliações
- Drug StudyDocumento1 páginaDrug StudyNeil Floyd VenturaAinda não há avaliações
- VecuroniumDocumento2 páginasVecuroniumAmanda La SalaAinda não há avaliações
- AztreonamDocumento2 páginasAztreonamHannahShaeHayesAinda não há avaliações
- DRUGS Study OrigDocumento17 páginasDRUGS Study OrigKiersten Karen Policarpio Verina100% (1)
- A Drug Study On Vincristine SulfateDocumento9 páginasA Drug Study On Vincristine SulfateTrio San LuisAinda não há avaliações
- Allopurinol Drug Study for Gout TreatmentDocumento1 páginaAllopurinol Drug Study for Gout TreatmentAbigail CastroAinda não há avaliações
- Non-Steroidal Anti Inflammatory Drugs (NSAIDS)Documento5 páginasNon-Steroidal Anti Inflammatory Drugs (NSAIDS)Pardhasaradhi PantaAinda não há avaliações
- UROKINASE (Kinlytic)Documento4 páginasUROKINASE (Kinlytic)Mikaela Gabrielle GeraliAinda não há avaliações
- Drug Analysis CefoxitinDocumento2 páginasDrug Analysis CefoxitinNika LoAinda não há avaliações
- Xarelto PDFDocumento33 páginasXarelto PDFNovita Dewi LestariAinda não há avaliações
- (Product Name) MR Tablet 30mg (Product Name) MR Tablet 60mgDocumento10 páginas(Product Name) MR Tablet 30mg (Product Name) MR Tablet 60mggmsanto7Ainda não há avaliações
- Olmesartan Drug StudyDocumento2 páginasOlmesartan Drug StudydyndzAinda não há avaliações
- Treatment Options for Coronary InsufficiencyDocumento7 páginasTreatment Options for Coronary InsufficiencyMae Navidas DigdiganAinda não há avaliações
- Nursing Responsibilities for Salbutamol and PrednisoneDocumento7 páginasNursing Responsibilities for Salbutamol and PrednisoneAlvin LimAinda não há avaliações
- Verapamil HCLDocumento3 páginasVerapamil HCLMae Ann Bueno CastillonAinda não há avaliações
- F&E Drug StudyDocumento2 páginasF&E Drug Studychelle_asenjoAinda não há avaliações
- Drug Study-Ceftriaxone ClindamycinDocumento2 páginasDrug Study-Ceftriaxone ClindamycinDavid VillanuevaAinda não há avaliações
- Salazar DsDocumento4 páginasSalazar DsDjayAinda não há avaliações
- Profort VialDocumento8 páginasProfort Vialelcapitano vegetaAinda não há avaliações
- Damage To Cell MembraneDocumento7 páginasDamage To Cell MembraneEsteph CortesAinda não há avaliações
- Cefprozil Final ProductDocumento18 páginasCefprozil Final ProductRathnaganpathi ThulasikumarAinda não há avaliações
- Essential Update For SNDocumento11 páginasEssential Update For SNshanksAinda não há avaliações
- Ceftriaxone + TazobactumDocumento10 páginasCeftriaxone + Tazobactumnikoseamit7460100% (1)
- Chronic Kidney Disease and Coronary Heart DiseaseDocumento20 páginasChronic Kidney Disease and Coronary Heart DiseaseNakorn BaisriAinda não há avaliações
- MD Consult - Drug Monograph TATDocumento1 páginaMD Consult - Drug Monograph TATNakorn BaisriAinda não há avaliações
- Adenosine - AHFS 24 - 04.04Documento2 páginasAdenosine - AHFS 24 - 04.04Nakorn BaisriAinda não há avaliações
- TB Adverse Drug Management อ วิชัยDocumento56 páginasTB Adverse Drug Management อ วิชัยNakorn BaisriAinda não há avaliações
- What's New in Drug TherapyDocumento9 páginasWhat's New in Drug TherapyNakorn BaisriAinda não há avaliações
- Imaging of the Urinary TractDocumento58 páginasImaging of the Urinary TractNakorn BaisriAinda não há avaliações
- ASIAN LIVESTOCK PERSPECTIVESDocumento18 páginasASIAN LIVESTOCK PERSPECTIVESMuadz AbdurrahmanAinda não há avaliações
- Niryana Shoola DasaDocumento7 páginasNiryana Shoola DasaSuryasukraAinda não há avaliações
- 2nd - Science-Second-Quarter-Week-1Documento37 páginas2nd - Science-Second-Quarter-Week-1Arlene AranzasoAinda não há avaliações
- 1B Cosmos-Standard - Technical - Guide - v40Documento45 páginas1B Cosmos-Standard - Technical - Guide - v40carla deiddaAinda não há avaliações
- Mouse Deer and TigerDocumento2 páginasMouse Deer and Tigeralan.nevgan100% (1)
- Approach To Malabsorption (SANJAY)Documento58 páginasApproach To Malabsorption (SANJAY)Sanjay KumarAinda não há avaliações
- Dimensions and Relations of The Dentogingival Junction in Humans. Gargiulo 1961Documento7 páginasDimensions and Relations of The Dentogingival Junction in Humans. Gargiulo 1961Linda Garcia PAinda não há avaliações
- CEFIC Guidelines Transport Equipment Packed Cargo (2010)Documento7 páginasCEFIC Guidelines Transport Equipment Packed Cargo (2010)sl1828Ainda não há avaliações
- Nest Installation GuideDocumento8 páginasNest Installation GuideOzzyAinda não há avaliações
- 1830PSS R36 QuickReferenceGuide 8DG60888JAAADocumento66 páginas1830PSS R36 QuickReferenceGuide 8DG60888JAAAFelippe CanatoAinda não há avaliações
- Gas Turbine Performance Enhancement Update: GE Energy ServicesDocumento45 páginasGas Turbine Performance Enhancement Update: GE Energy Servicesesteban100% (1)
- 2 History of OrthodonticsDocumento11 páginas2 History of OrthodonticsMeiz JaleelAinda não há avaliações
- Ficha Tecnica Cat. Bard 36kbtu Act.Documento15 páginasFicha Tecnica Cat. Bard 36kbtu Act.Jehison M Patiño TenorioAinda não há avaliações
- ETHICS NOTES PART 1 - IAS PCS PathshalaDocumento15 páginasETHICS NOTES PART 1 - IAS PCS PathshalaATULAinda não há avaliações
- Kaustubh Laturkar Fuel Cell ReportDocumento3 páginasKaustubh Laturkar Fuel Cell Reportkos19188Ainda não há avaliações
- Service Manual: EQ1030T47D-820 Light Commercial TruckDocumento175 páginasService Manual: EQ1030T47D-820 Light Commercial TruckYonny ColqueAinda não há avaliações
- Delay-Tolerant NetworksDocumento66 páginasDelay-Tolerant NetworksMegi YantoAinda não há avaliações
- Borneo SporenburgDocumento2 páginasBorneo SporenburgDorin TecuceanuAinda não há avaliações
- Home Contents Vehicle Boat Cover Policy Sample Westpac NZDocumento27 páginasHome Contents Vehicle Boat Cover Policy Sample Westpac NZRobin Rutter-BaumannAinda não há avaliações
- Booster Pump Service ManualDocumento11 páginasBooster Pump Service ManualSGI AUTOMOTIVE PVT LTDAinda não há avaliações
- PRN Maths Midterm QP Aug 18Documento3 páginasPRN Maths Midterm QP Aug 18JanakChandPAinda não há avaliações
- INChO 2008 Question PaperDocumento23 páginasINChO 2008 Question PaperChaitanya GaurAinda não há avaliações
- The LM393Documento2 páginasThe LM393mayron vasquezAinda não há avaliações
- Turbine Stress EvaluatorDocumento14 páginasTurbine Stress EvaluatorsumitAinda não há avaliações
- Class 10 Trigonometry and Application of TrigonometryDocumento1 páginaClass 10 Trigonometry and Application of TrigonometryTanmay SanchetiAinda não há avaliações
- CDI-500 Specialized Crime Investigation and Legal MedicineDocumento20 páginasCDI-500 Specialized Crime Investigation and Legal MedicineCherry Len FaroniloAinda não há avaliações
- Syllabi - EE 5004 - Power ElectronicsDocumento2 páginasSyllabi - EE 5004 - Power ElectronicsKalum ChandraAinda não há avaliações
- Chapter 1 - Introduction To Machinery PrinciplesDocumento27 páginasChapter 1 - Introduction To Machinery PrinciplesYousab CreatorAinda não há avaliações
- Dental Radiographs and Photographs in Human Forensic IdentificationDocumento8 páginasDental Radiographs and Photographs in Human Forensic IdentificationBudi PurnomoAinda não há avaliações
- Infinera Product BrochureDocumento4 páginasInfinera Product Brochurebarry_fieldAinda não há avaliações