Escolar Documentos
Profissional Documentos
Cultura Documentos
Normocytic Anemia
Enviado por
Paula ArayaDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Normocytic Anemia
Enviado por
Paula ArayaDireitos autorais:
Formatos disponíveis
1
Normocytic Anemia
http://www.aafp.org/afp/2000/1115/p2255.html para quien desee ontener el paper de la
web
JOHN R. BRILL, M.D., and DENNIS J. BAUMGARDNER, M.D., University of Wisconsin
Medical School, Milwaukee Clinical Campus, Milwaukee, Wisconsin
Am Fam Physician. 2000 Nov 15;62(10):2255-2263.
See related patient information handout on normocytic anemia, written by the authors of
this article..
ARTICLE SECTIONS
Abstract
Etiology
Decreased Red Blood Cell Production
Increased Red Blood Cell Destruction or Loss
Diagnosis
Treatment
References
Anemia is a common problem that is often discovered on routine laboratory tests. Its
prevalence increases with age, reaching 44 percent in men older than 85 years.
Normocytic anemia is the most frequently encountered type of anemia. Anemia of
chronic disease, the most common normocytic anemia, is found in 6 percent of adult
patients hospitalized by family physicians. The goals of evaluation and management are
to make an accurate and efficient diagnosis, avoid unnecessary testing, correct
underlying treatable causes and ameliorate symptoms when necessary. The evaluation
begins with a thorough history and a careful physical examination. Basic diagnostic
studies include the red blood cell distribution width, corrected reticulocyte index and
peripheral blood smear; further testing is guided by the results of these studies.
Treatment should be directed at correcting the underlying cause of the anemia. A recent
advance in treatment is the use of recombinant human erythropoietin.
Anemia is defined as a decrease in the circulating red blood cell mass to below age-specific
and gender-specific limits. In normocytic anemias, the mean corpuscular volume (MCV) is
within defined normal limits, but the hemoglobin and hematocrit are decreased. The MCV is
also age-specific (Figure 1),
1
with normal values ranging from 70 femtoliter (fL) at one year of
age to 80 fL at seven years and older.
2
2
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing
item, see the original print version of this publication.
FIGURE 1.
Most patients with anemia are asymptomatic. Therefore, the condition is most often discovered
by laboratory evaluation, usually on routine testing as part of the general physical examination
or for reasons other than suspected anemia. Anemia should be considered a sign, not a
disease.
3
It can be caused by a variety of systemic disorders and diseases, as well as primary
hematologic disorders.
Approximately 4.7 million Americans have anemia.
4
Population-based estimates indicate that
this condition affects 6.6 percent of males and 12.4 percent of females. The prevalence of
anemia increases with age and is 44.4 percent in men 85 years and older.
5
Although the
elderly are more prone to develop anemia, older age is not of itself a cause of the condition.
6
Etiology
Normocytic anemias may be thought of as representing any of the following: a decreased
production of normal-sized red blood cells (e.g., anemia of chronic disease, aplastic anemia);
an increased destruction or loss of red blood cells (e.g., hemolysis, posthemorrhagic anemia);
an uncompensated increase in plasma volume (e.g., pregnancy, fluid overload); or a mixture of
conditions producing microcytic and macrocytic anemias.
It should be noted that in the initial stage, nearly all anemias are normocytic. The major primary
causes of normocytic anemia are given in Table 1.
TABLE 1
Primary Causes of Normocytic Anemias*
Increased red blood cell loss or destruction
Acute blood loss
Hypersplenism
Hemolytic disorders
Congenital conditions
Hemoglobinopathies
3
Homozygous sickle cell disease (hemoglobin SS disease)
Heterozygous sickle hemoglobin C disease (hemoglobin SC disease)
Disorders of red blood cell membranes
Hereditary spherocytosis
Hereditary elliptocytosis
Red blood cell enzyme deficiencies
Glucose-6-phosphate dehydrogenase deficiency
Pyruvate kinase deficiency
Acquired conditions
Mechanical hemolysis
Macrovascular disorders
Microangiopathic disorders
Disseminated intravascular coagulopathy
Hemolytic-uremic syndrome
Thrombotic thrombocytopenic purpura
Autoimmune hemolytic anemias
Warm-reactive anemias
Cold-reactive anemias
Drug-induced anemias
4
*Mean corpuscular volume of 81 to 99 fL.
TABLE 1 Primary Causes of Normocytic Anemias*
View Table
Decreased Red Blood Cell Production
Paroxysmal nocturnal hemoglobinuria
Decreased red blood cell production
Primary causes
Marrow hypoplasia or aplasia
Myelopathies
Myeloproliferative diseases
Pure red blood cell aplasia
Secondary causes
Chronic renal failure
Liver disease
Endocrine deficiency states
Anemia of chronic disease
Sideroblastic anemias
Overexpansion of plasma volume
Pregnancy
Overhydration
5
ANEMIA OF CHRONIC DISEASE
Anemia of chronic disease is the most common normocytic anemia and the second most
common form of anemia worldwide (after iron deficiency anemia).
7
The MCV may be low in
some patients with this type of anemia. The pathogenesis of anemia of chronic disease is
multifactorial and is related to hypo-activity of the bone marrow, with relatively inadequate
production of erythropoietin or a poor response to erythropoietin, as well as slightly shortened
red blood cell survival.
Anemia of chronic disease is associated with a wide variety of chronic disorders, including
inflammatory conditions, infections, neoplasms and various systemic diseases. The diagnosis
of anemia of chronic disease is not usually applied to the anemias associated with renal,
hepatic or endocrine disorders. Patients with these disorders may not display the hallmark
ferrokinetic profile of anemia of chronic disease (i.e., decreased serum iron level, decreased
transferrin level, or normal or elevated ferritin levels, all of which result in iron being present but
inaccessible for use).
3,810
ENDOCRINE DEFICIENCY
Endocrine deficiency states, including hypothyroidism, adrenal or pituitary insufficiency, and
hypogonadism, may cause secondary bone marrow failure because of reduced stimulation of
erythropoietin secretion. Hyperthyroidism may also cause normocytic anemia.
3,9
RENAL FAILURE
Anemia occurs in acute and chronic renal failure. The anemia is usually normocytic but may be
microcytic. In renal failure, anemia occurs in part because uremic metabolites decrease the
lifespan of circulating red blood cells and reduce erythropoiesis.
Anemia secondary to uremia is characterized by inappropriately low erythropoietin levels, in
contrast to the normal or high levels that occur with most other causes of anemia. To further
confuse the presentation, serum iron levels and the percentage of iron saturation are often low,
apparently because of negative acute-phase reactions.
10
Furthermore, the serum creatinine
level and the degree of anemia may not correlate well.
3
OTHER CAUSES
Other causes of decreased red blood cell production include bone marrow infiltration, fibrosis,
various myeloproliferative diseases and sideroblastic anemias. These uncommon disorders are
generally diagnosed by bone marrow biopsy.
Increased Red Blood Cell Destruction or Loss
HEMOLYTIC ANEMIAS
Hemolytic anemias other than the alloimmune hemolytic anemias of newborns (e.g., Rh or
ABO incompatibility) can be categorized as congenital or acquired (Table 2).
3,9,1113
TABLE 2
6
Selected Causes of Hemolytic Anemias
DISORDER
MOST COMMON
CLINICAL
FEATURES
FEATURES OF
PERIPHERAL
BLOOD SMEAR
LABORATORY
TESTS
Congenital conditions
Homozygous sickle
cell disease
(hemoglobin SS
disease)
Vaso-occlusive
crises,
splenomegaly,
cerebrovascular
accidents,
priapism, hand-foot
syndrome, acute
chest syndrome
Sickle cells Hemoglobin
electrophoresis
Heterozygous sickle
hemoglobin C
disease (hemoglobin
SC disease)
Generally similar to
homozygous sickle
cell disease, except
associated with
fewer infections,
less hemolysis and
fewer crises, but
more retinopathy
and aseptic
necrosis
Sickle cells, target
cells
Hemoglobin
electrophoresis
Hereditary
spherocytosis
Childhood anemia,
splenomegaly,
jaundice
Spherocytes Osmotic fragility test
Hereditary
elliptocytosis
Variable:
asymptomatic
carrier state to
severe hemolysis
Elliptocytes 25 percent or more of
red blood cells
elliptocytic on
peripheral blood smear
G6PD deficiency Transient
hemolysis following
exposure to
Normal G6PD activity
7
DISORDER
MOST COMMON
CLINICAL
FEATURES
FEATURES OF
PERIPHERAL
BLOOD SMEAR
LABORATORY
TESTS
oxidative drug
Pyruvate kinase
deficiency
Variable: severe
anemias in
newborns to no
symptoms in adults
Normal Red blood cell P-50
level (screening); red
blood cell pyruvate
kinase activity
(confirmatory)
Acquired conditions
Microangiopathic
disorders
Thrombocytopenia,
schistocytes
Disseminated
intravascular
coagulopathy
Bleeding and/or
intravascular
hemolysis
Hypofibrinogenemia;
increases in partial
thromboplastin time,
prothrombin time, fibrin
split products and
thrombin time
Hemolytic-uremic
syndrome
Fever, jaundice,
bleeding, central
nervous system
changes, renal
failure; generally
occurs in children
Increased creatinine
level
Thrombotic
thrombocytopenic
purpura
Purpura, fever,
central nervous
system changes;
generally occurs in
adults
Mechanical hemolysis Mild to moderate
anemia; frequently,
Schistocytes None
8
DISORDER
MOST COMMON
CLINICAL
FEATURES
FEATURES OF
PERIPHERAL
BLOOD SMEAR
LABORATORY
TESTS
iron deficiency,
second-degree
chronic urinary
loss; history of
heart valve
replacement or
valvular disease
Paroxysmal nocturnal
hemoglobinuria
Recurrent
abdominal pain,
vomiting,
headache, eye
pain; venous
thromboses; leads
to iron deficiency
anemia
Normal Sucrose hemolysis
(screening); Ham's test
(confirmatory)
G6PD = glucose-6-phosphate dehydrogenase; P-50 = oxygen half-saturation pressure of
oxygen.
Information from references 3, 9 and 11 through 13.
TABLE 2 Selected Causes of Hemolytic Anemias
View Table
Congenital hemolytic anemias include the hemoglobinopathies (homozygous sickle cell
disease [hemoglobin SS disease], heterozygous sickle hemoglobin C disease [hemoglobin SC
disease]), red blood cell membrane disorders and red blood cell enzyme deficiencies.
11,12
Homozygous sickle cell disease is the most common cause of hemolytic normocytic anemias
in children. Because of longevity, this disease is also becoming an increasingly prevalent
cause of these anemias in adults.
1113
Hereditary spherocytosis is the most common red blood cell membrane disorder. It usually
presents in childhood with anemia, jaundice and splenomegaly. Pigment gallstones, delayed
growth and dysmorphic features may occur. Hereditary elliptocytosis ranges from an
asymptomatic carrier state to severe hemolytic anemia.
1113
9
Red blood cell enzyme deficiencies include glucose-6-phosphate dehydrogenase (G6PD) and
pyruvate kinase deficiencies. More than 300 varieties of G6PD deficiency have been identified.
The southern Mediterranean variety, referred to as favism, is best known, but the most
common variant in the United States is a less severe X-linked disorder that affects 10 percent
of black males. Persons with the U.S. variant may experience an acute, self-limited hemolytic
episode after exposure to causes of oxidative stress, including sulfa drugs, nitrofurantoin
(Furadantin), phenazopyridine (Pyridium) and antimalarial drugs.
11,12
Acquired hemolytic anemias include autoimmune hemolytic anemias, mechanical hemolysis
and paroxysmal nocturnal hemoglobinuria.
12
Autoimmune hemolytic anemias primarily occur in
persons older than 40 years. The most common and typically most severe of these anemias
are those caused by warm-reactive antibodies. Autoimmune hemolytic anemias caused by
cold-reactive antibodies most commonly follow Mycoplasma pneumonia or infectious
mononucleosis.
Drugs that induce autoimmune hemolytic anemias include methyldopa (Aldomet), penicillins,
cephalosporins, erythromycin, acetaminophen (e.g., Tylenol) and procainamide (Pronestyl).
Paroxysmal nocturnal hemoglobinuria generally presents as a chronic hemolytic anemia.
Classic nocturnal hemoglobinuria is seldom seen.
12
UNCOMPENSATED BLOOD LOSS
Acute posthemorrhagic anemia occurs with gastrointestinal bleeding, bleeding from an external
wound or, less obviously, retroperitoneal bleeding or bleeding into a hip fracture. A healthy
young person would be expected to tolerate rapid loss of 500 to 1,000 mL of blood (10 to 20
percent of the total blood volume) with few or no symptoms, although about 5 percent of the
general population would have a vasovagal reaction.
14
Indeed, healthy young persons at rest
may tolerate an acute isovolemic reduction of hemoglobin volume to a level of 5 g per dL (50 g
per L) without impairment of critical oxygen delivery.
15
HYPERSPLENISM
Hypersplenism leads to anemia only after the spleen reaches three to four times its normal
size, as may occur in cirrhosis, chronic infections and myeloproliferative diseases. The anemia
is primarily caused by the removal of red blood cells from the circulation, but increased
destruction of red blood cells is usually a contributing factor.
16
NORMOCYTIC ANEMIA IN CHILDREN
The prevalence of anemias caused by iron deficiency or lead toxicity continues to decline in the
United States.
17
As a result, normocytic anemias are constituting a larger proportion of cases in
the pediatric age group.
Iron deficiency, which in its early stages is usually characterized by a normal MCV, is still a
common cause of mild normocytic anemia in children beyond the neonatal period. Other
common childhood normocytic anemias are the result of acute bleeding, sickle cell anemia, red
10
blood cell membrane disorders and current or recent infections (particularly in younger
children).
2,17
Aplastic crises in patients of any age who have chronic hemolytic anemias are
frequently precipitated by human parvovirus B19 infection.
2,12,13,18
Most anemias in children can be diagnosed with a basic work-up that includes a complete
blood cell count (CBC), a corrected reticulocyte index, a peripheral blood smear and targeted
studies of the peripheral blood (e.g., hemoglobin electrophoresis).
Although bone marrow examinations are generally unnecessary, one study found that when
the basic laboratory studies and historical and physical evidence were unrevealing, bone
marrow specimens yielded a specific diagnosis in 92 percent of children.
18
The most frequent
diagnosis in this study was transient erythroblastopenia of childhood, a common, generally
mild, self-limited red blood cell aplasia of unknown etiology. This entity must be distinguished
from Blackfan-Diamond syndrome, a rare, usually macrocytic and probably genetic disorder of
infants. Blackfan-Diamond syndrome is a congenital erythroid hypoplasia that usually does not
spontaneously remit.
3,9
Diagnosis
Physicians are sometimes inefficient in their evaluation of normocytic anemia, either ordering
an excessive battery of tests or foregoing testing entirely in the belief that a cause is not likely
to be found.
19
The first step in the evaluation of anemia is to correlate the finding of anemia with
the information obtained from the patient's history and physical examination. In many
instances, this approach allows a working diagnosis to be made and many disorders to be
eliminated.
Most published algorithms for the diagnosis of normocytic anemia begin with an examination of
the peripheral blood smear
20
or a corrected reticulocyte index.
2,9,21
The red blood cell distribution
width is a measure of the variability of the size (anisocytosis) of the cells and is usually
reported as a component of automated CBCs. Therefore, a practical and useful first step is to
use the red blood cell distribution width to help categorize the normocytic anemia as
heterogeneous (e.g., hemolytic anemia) or homogeneous (e.g., anemia of chronic disease).
2
In
patients with a mild homogeneous normocytic anemia (hematocrit of 30 percent or greater) and
a known chronic disease, anemia of chronic disease is highly likely, and bone marrow biopsy
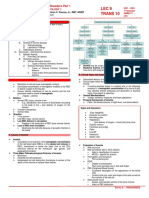
may not be necessary (Figure 2).
21
11
Evaluation of Normocytic Anemia
FIGURE 2.
Approach to the evaluation of normocytic anemia in adults. (RBC = red blood cell; CRI = corrected reticulocyte
index; ACD = anemia of chronic disease; AIHA = autoimmune hemolytic anemia)
12
Adapted with permission from Brown RG. Normocytic and macrocytic anemias. Postgrad Med 1991;89(8):125
32,1356.
DRAW AND HOLD STRATEGY
Because the diagnosis of normocytic anemia usually proceeds in a step-wise fashion that
begins with the corrected reticulocyte index and examination of the peripheral blood smear, a
patient-friendly, cost-effective and time-efficient strategy is to use a draw and hold order for
possible later testing. Most laboratories do not charge to hold tubes, and tests can usually be
added up to one week after specimens are obtained. The physician should check with the local
laboratory to determine the number and type of specimens that need to be obtained.
PERIPHERAL BLOOD SMEAR
The examination of the peripheral blood smear often yields diagnostic clues or confirmatory
evidence. Easily recognized red blood cell findings related to normocytic anemias include the
following: large polychromatic shift cells, which represent reticulocytosis; target cells, which
may be found in liver disease; basophilic stippling, which may be present in hemolytic anemias;
and mixtures of large and small red blood cells, which may suggest the presence of mixed
microcytic and macrocytic disease processes (a finding that should be suggested by an
elevated red blood cell distribution width).
Other findings include burr cells (uremia), spherocytes (hereditary spherocytosis, autoimmune
hemolysis, G6PD deficiency), elliptocytes (hereditary elliptocytosis), schistocytes
(microangiopathic processes), bite or blister cells (where all of the hemoglobin appears to be
pushed to one side of the cell, G6PD deficiency) and nucleated red blood cells (hemolytic
anemia, acute blood loss). These findings may be present in other anemias and in other
conditions.
3,9,10
The corrected reticulocyte index, along with the white blood cell and platelet counts, indicates
whether the bone marrow is functioning appropriately. The corrected reticulocyte index should
be elevated in patients with an acute anemia but a competent bone marrow.
ILLUSTRATIVE CASES
Case 1. A 50-year-old woman who had been taking aspirin for a flare of rheumatoid arthritis
presented with mild epigastric pain. A CBC was ordered, and a guaiac test for occult blood was
performed. The guaiac test was negative.
The CBC revealed a normocytic anemia (hemoglobin count, 11 per mm
3
[11 10
6
per L];
hematocrit, 33 percent [0.33]; MCV, 84 fL), with a red blood cell distribution width of 41 fL
(normal range: 39 to 47 fL). A reticulocyte count and draw and hold specimens were ordered.
The corrected reticulocyte index was 1.0 percent.
Ferritin and serum iron levels were obtained from the stored specimens. These tests revealed
an elevated ferritin level and a low serum iron level, findings consistent with a diagnosis of
anemia of chronic disease related to the patient's rheumatoid arthritis.
13
Case 2. A 44-year-old woman presented with the complaint of fatigue. Her physical
examination was unremarkable.
A CBC revealed normocytic anemia (hemoglobin count, 11 per mm
3
[11 10
6
per L];
hematocrit, 33 percent [0.33]; MCV, 84 fL), with an elevated red blood cell distribution width of
53 fL. A reticulocyte count and draw and hold specimens were ordered. The corrected
reticulocyte index was elevated (3.6 percent).
Examination of a peripheral blood smear from the stored specimens was normal. A direct
antiglobulin test (direct Coombs' test) was positive, and a preliminary diagnosis of autoimmune
hemolytic anemia was made.
Treatment
The treatment of a normocytic anemia begins with timely identification of its cause. In most
patients, therapy is individualized to the underlying disorder. Treatments may include
avoidance of trigger exposure in patients with hemolytic anemia, correction of iron, folate or
vitamin B12 deficiency in patients with mixed disorders, or splenectomy in patients with
hypersplenism.
12,13
Anemia of renal disease is associated with a relative underproduction of erythropoietin, and
inappropriate erythropoietin levels appear to contribute significantly to anemia of chronic
disease. With the development of recombinant human erythropoietin (r-HuEPO; epoetin alfa
[Epogen]), there has been considerable interest in finding out whether exogenous
erythropoietin administration would improve anemia.
The effects of r-HuEPO administration have been studied in a variety of disorders. In a trial
conducted in 1990,
22
all 11 patients with anemia related to rheumatoid arthritis reached a
normal hematocrit after 24 weeks. Since then, r-HuEPO has been tested in patients with
anemia of chronic disease secondary to acquired immunodeficiency syndrome, malignancy,
inflammatory bowel disease, renal disease and other disorders.
23,24
Quality-of-life parameters in
responders improved significantly.
Therapy with r-HuEPO is very expensive and should never replace treatment of the underlying
cause of an anemia. R-HuEPO is an indicated therapy for anemia of renal disease. In this
situation, its use should be based on clinical and quality-of-life issues rather than specific
hemoglobin levels.
10
There are no consistent guidelines for r-HuEPO therapy in patients with
anemia of chronic disease, although response rates of 40 to 80 percent may be achieved.
8
Erythropoietin also appears to be useful prophylactically in patients undergoing autologous
blood donation and certain surgical procedures.
25
In all patients, treatment of anemia should include the provision of optimal nutrition and
supportive care.
The Authors
14
JOHN R. BRILL, M.D., is assistant professor and medical director of Community Health
Programs in the Department of Family Medicine at the Milwaukee Clinical Campus of the
University of Wisconsin Medical School. Dr. Brill graduated from the Medical College of
Wisconsin, Milwaukee, and completed a faculty development fellowship and residency at St.
Luke's Medical Center, also in Milwaukee.
DENNIS J. BAUMGARDNER, M.D., is professor and residency director at St. Luke's Family
Practice Residency Program, which is affiliated with the Department of Family Medicine at the
Milwaukee Clinical Campus of the University of Wisconsin Medical School. Dr. Baumgardner
graduated from the University of Illinois at Chicago College of Medicine and completed a family
medicine residency at the Rockford (Ill.) Medical Education Foundation.
Address correspondence to John R. Brill, M.D., St. Luke's Family Practice Residency, 2801 W.
Kinnickinnic River Pkwy., Suite 175, Milwaukee, WI 53215 (e-mail: jbrill@fammed.wisc.edu).
Reprints are not available from the authors.
REFERENCES
1. Dallman PR, Siimes MA. Percentile curves for hemoglobin and red cell volume in infancy
and childhood. J Pediatr. 1979;94:2631.
2. Bessman JD, Gilmer PR, Gardner FH. Improved classification of anemias by MCV and
RDW. Am J Clin Pathol. 1983;80:3226.
3. Schnall SF, Berliner N, Duffy TP, Benz EF Jr. Approach to the adult and child with anemia.
In: Hoffman R, et al., eds. Hematology: basic principles and practice. 3d ed. New York:
Churchill Livingstone, 2000:36782.
4. Adams PF, Marano MA. Current estimates from the National Health Interview Survey, 1994.
Hyattsville, Md.: U.S. Dept. of Health and Human Services, Public Health Service, Centers for
Disease Control, National Center for Health Statistics, 1995. Vital and health statistics. Series
10: Data from the National Health Survey; no. 193; DDHS publication no. (PHS) 951521.
5. Ania BJ, Suman VJ, Fairbanks VF, Melton LJ 3d. Prevalence of anemia in medical practice:
community versus referral patients. Mayo Clin Proc. 1994;69:7305.
6. Izaks GJ, Westendorp RG, Knook DL. The definition of anemia in older persons. JAMA.
1999;281:17147.
7. Krantz SB. Pathogenesis and treatment of the anemia of chronic disease. Am J Med Sci.
1994;307:3539.
8. Gardner LB, Benz EJ Jr. Anemia of chronic diseases. In: Hoffman R, et al., eds.
Hematology: basic principles and practice. 3d ed. New York: Churchill Livingstone, 2000:383
8.
15
9. Lee GR. Anemia: a diagnostic strategy. In: Lee GR, et al., eds. Wintrobe's Clinical
hematology. 10th ed. Baltimore: Williams &Wilkins, 1999:90840.
10. Abramson SD, Abramson N. Common uncommon anemias. Am Fam Physician.
1999;59:8518.
11. Weatherall DJ. ABC of clinical haematology. The hereditary anaemias. BMJ.
1997;314:4926.
12. Sackey K. Hemolytic anemia: Part 1. Pediatr Rev. 1999;20:1528.
13. Sackey K. Hemolytic anemia: Part 2. Pediatr Rev. 1999;20:2048.
14. Levine E, Rosen A, Sehgal L, Gould S, Sehgal H, Moss G. Physiologic effects of acute
anemia: implications for a reduced transfusion trigger. Transfusion. 1990;30:114.
15. Weiskopf RB, Viele MK, Feiner J, Kelley S, Lieberman J, Noorani M, et al. Human
cardiovascular and metabolic response to acute, severe isovolemic anemia. JAMA.
1998;279:21721 [Published erratum appears in JAMA 1998;280:1404]
16. Erslev AJ. Hypersplenism and hyposplenism. In: Beutler E, Lichtman MA, et al., eds.
Williams Hematology. 5th ed. New York: McGraw-Hill, Health Professions Division, 1995:709
14.
17. Sherry B, Bister D, Yip R. Continuation of decline in prevalence of anemia in low-income
children: the Vermont experience. Arch Pediatr Adolesc Med. 1997;151:92830.
18. Abshire TC. The anemia of inflammation. A common cause of childhood anemia. Pediatr
Clin North Am. 1996;43:62337.
19. Meyers FJ, Welborn JL, Lewis JP. Improved approach to patients with normocytic anemia.
Am Fam Physician. 1988;38(2):1915.
20. Farhi DC, Luebbers EL, Rosenthal NS. Bone marrow biopsy findings in childhood anemia:
prevalence of transient erythroblastopenia of childhood. Arch Pathol Lab Med. 1998;122:638
41.
21. Brown RG. Normocytic and macrocytic anemias. Postgrad Med. 1991;89(8):12532.
22. Pincus T, Olsen NJ, Russell IJ, Wolfe F, Harris ER, Schnitzer TJ, et al. Multicenter study of
recombinant human erythropoietin in correction of anemia in rheumatoid arthritis. Am J Med.
1990;89:1618.
23. Krantz SB. Erythropoietin and the anaemia of chronic disease. Nephrol Dial Transplant.
1995;10(suppl 2):107.
16
24. Ludwig H, Fritz E, Kotzmann H, Hocker P, Gisslinger H, Barnas U. Erythropoietin treatment
of anemia associated with multiple myeloma. N Engl J Med. 1990;322:16939.
25. Goodnough LT, Monk TG, Andriole GL. Erythropoietin therapy. N Engl J Med.
1997;336:9338.
Members of various family practice departments develop articles for Problem-Oriented
Diagnosis. This article is one in a series coordinated by the Department of Family Medicine at
the University of Wisconsin Medical School, Madison. Guest editor of the series is William E.
Scheckler, M.D.
Você também pode gostar
- Emergency Medicine Clinics of North America Volume Issue 2014 (Doi 10.1016 - J.emc.2014.04.007) Vieth, Julie T. Lane, David R. - AnemiaDocumento16 páginasEmergency Medicine Clinics of North America Volume Issue 2014 (Doi 10.1016 - J.emc.2014.04.007) Vieth, Julie T. Lane, David R. - AnemiaJeffrey Stefan Pal RiveraAinda não há avaliações
- Anemia: Differential DiagnosisDocumento7 páginasAnemia: Differential DiagnosisZaman MigozaradAinda não há avaliações
- Anemia (: /Ə Ni Miə/ Also Spelled Greek Red Blood Cells HemoglobinDocumento13 páginasAnemia (: /Ə Ni Miə/ Also Spelled Greek Red Blood Cells HemoglobinAryana BudiawanAinda não há avaliações
- Continuing Education Activity: ObjectivesDocumento7 páginasContinuing Education Activity: ObjectivesMihu DragostinAinda não há avaliações
- Hemolytic AnemiaDocumento18 páginasHemolytic AnemiaAdisurya NugrahaAinda não há avaliações
- Anemia For The Primary Care PhysicianDocumento16 páginasAnemia For The Primary Care PhysicianAbdón Guerra FariasAinda não há avaliações
- AnemiaDocumento21 páginasAnemiaMarie WagasAinda não há avaliações
- Anemia (Pronounced: o o o o o o oDocumento12 páginasAnemia (Pronounced: o o o o o o opamela100181Ainda não há avaliações
- Haematological Manifestationsin SLE PDFDocumento21 páginasHaematological Manifestationsin SLE PDFLe DungAinda não há avaliações
- Physiology Group 2Documento58 páginasPhysiology Group 2Akinmade AyobamiAinda não há avaliações
- Module 1 Blok Hi Tutor 8Documento47 páginasModule 1 Blok Hi Tutor 8Mentariasih Maulida SudibyoAinda não há avaliações
- Hematology Physiology 1Documento6 páginasHematology Physiology 1Kyoheirwe vanessaAinda não há avaliações
- Emergencymedicine Evaluationandmanagement Ofanemia: Brit Long,, Alex KoyfmanDocumento22 páginasEmergencymedicine Evaluationandmanagement Ofanemia: Brit Long,, Alex KoyfmanVictor ChisAinda não há avaliações
- Anemia: Signs and SymptomsDocumento4 páginasAnemia: Signs and SymptomssujithasAinda não há avaliações
- Hemolytic AnemiaDocumento9 páginasHemolytic AnemiaTheeya QuigaoAinda não há avaliações
- Anemi Aplastik Dan MielodisplasiaDocumento34 páginasAnemi Aplastik Dan MielodisplasiaRoby KieranAinda não há avaliações
- 209-Hematology Review - Case StudiesDocumento129 páginas209-Hematology Review - Case StudiesKhalid Khalidi100% (2)
- Pharmacotherapy of Hematological Disorders by Hailu C. (Asst - Prof)Documento132 páginasPharmacotherapy of Hematological Disorders by Hailu C. (Asst - Prof)Esubalew TeshomeAinda não há avaliações
- Blood Disorders in GeriatricDocumento29 páginasBlood Disorders in GeriatricdheaAinda não há avaliações
- Anemia GDocumento47 páginasAnemia GkalfAinda não há avaliações
- Dr. Ali's Uworld Notes For Step 2 CKDocumento46 páginasDr. Ali's Uworld Notes For Step 2 CKuyesAinda não há avaliações
- PallorDocumento16 páginasPallorManal AlQuaimi100% (1)
- AntmiaDocumento85 páginasAntmiafrendirachmadAinda não há avaliações
- INTRO in AnemiaDocumento3 páginasINTRO in AnemiaJeraiza Mendoza-LizarondoAinda não há avaliações
- Haemolytic Anaemia and Sickle Cell DiseaseDocumento26 páginasHaemolytic Anaemia and Sickle Cell DiseaseGideon HaburaAinda não há avaliações
- 21 Anaemia and PancytopeniaDocumento42 páginas21 Anaemia and PancytopeniaLeon Hui MingAinda não há avaliações
- Tinjauan Pustaka 2Documento12 páginasTinjauan Pustaka 226 ThufailAinda não há avaliações
- Approach To Anemia: Bisrat DDocumento45 páginasApproach To Anemia: Bisrat Dyared getachewAinda não há avaliações
- Anemia DIC NotesDocumento6 páginasAnemia DIC NotesJeanna ChongAinda não há avaliações
- Adrian Hardec Nasdal Modul 6 LBM 2Documento9 páginasAdrian Hardec Nasdal Modul 6 LBM 2Rizqon Yassir KuswondoAinda não há avaliações
- Anemia of Chronic Disease in The ElderlyDocumento7 páginasAnemia of Chronic Disease in The ElderlyAkbarAinda não há avaliações
- Chapter 49Documento6 páginasChapter 49Melissa Aina Mohd YusofAinda não há avaliações
- Anemia: Classification of AnemiasDocumento54 páginasAnemia: Classification of Anemiasammar amerAinda não há avaliações
- MEDSEM2LE4 Approach To AnemiaDocumento19 páginasMEDSEM2LE4 Approach To AnemiaAndrea Ann MagpayoAinda não há avaliações
- Anemias Aplastic Anemia Is A Condition Where Bone Marrow Does Not Produce Sufficient NewDocumento15 páginasAnemias Aplastic Anemia Is A Condition Where Bone Marrow Does Not Produce Sufficient NewZoreyca RiveraAinda não há avaliações
- Hematologic DisordersDocumento108 páginasHematologic DisordersEmma IntiaAinda não há avaliações
- Ha I by AbdifatahDocumento109 páginasHa I by AbdifatahAbdifatah AhmedAinda não há avaliações
- Complicaciones Hematológicas ARDocumento30 páginasComplicaciones Hematológicas ARTra21798siempreAinda não há avaliações
- ANEMIADocumento4 páginasANEMIAcabelin randy amenAinda não há avaliações
- Study of Anemia and Its Correlation With Hematological Parameters in Patient of Various Age GroupDocumento7 páginasStudy of Anemia and Its Correlation With Hematological Parameters in Patient of Various Age GroupIOSRjournal0% (1)
- Manifestaciones Inusuales en HipotiroidismoDocumento6 páginasManifestaciones Inusuales en HipotiroidismoDario Neri CortezAinda não há avaliações
- Grade 7 Math ModuleDocumento5 páginasGrade 7 Math ModuleAndre Labiste Aninon100% (2)
- Jurnal AnastesiDocumento12 páginasJurnal AnastesilissamariasianiparAinda não há avaliações
- Update On (Approach To) Anemia1 (Changes)Documento39 páginasUpdate On (Approach To) Anemia1 (Changes)Balchand KukrejaAinda não há avaliações
- Bone Marrow Failure VoiceoverDocumento18 páginasBone Marrow Failure Voiceoverياسر كوثر هانيAinda não há avaliações
- AnemiaDocumento10 páginasAnemiaGulzada ShadymanovaAinda não há avaliações
- Erythrocyte Life Cycle: PathophysiologyDocumento15 páginasErythrocyte Life Cycle: PathophysiologyYeniAinda não há avaliações
- Salinan Terjemahan 307211717 Laporan Pendahuluan AnemiaDocumento16 páginasSalinan Terjemahan 307211717 Laporan Pendahuluan AnemiaRidho HidayatullahAinda não há avaliações
- GGFHGFJKL KJKHGFDGHJKLDocumento14 páginasGGFHGFJKL KJKHGFDGHJKLVania Millenia MelindaAinda não há avaliações
- Approach To Anemia and PolycythemiaDocumento7 páginasApproach To Anemia and PolycythemiaambutlangnimoAinda não há avaliações
- Approuch Anemia PBLDocumento31 páginasApprouch Anemia PBLAndy XiaoAinda não há avaliações
- MRCPCH Guide Heme: A Hypochromic MicrocyticDocumento8 páginasMRCPCH Guide Heme: A Hypochromic MicrocyticRajiv KabadAinda não há avaliações
- AnemiaDocumento14 páginasAnemiaHermawan HmnAinda não há avaliações
- Clinical Hematological: Assist Prof. Dr. Mudhir S. ShekhaDocumento24 páginasClinical Hematological: Assist Prof. Dr. Mudhir S. ShekhaAhmed. Masud.OthmanAinda não há avaliações
- Anemia Pada Kondisi CKDDocumento3 páginasAnemia Pada Kondisi CKDNiken DiazAinda não há avaliações
- Now Get From Our Live Expert On Rea Ltime Basis Join Us and Get Homework HelpDocumento24 páginasNow Get From Our Live Expert On Rea Ltime Basis Join Us and Get Homework HelplicservernoidaAinda não há avaliações
- Hemolytic AnaemiaDocumento60 páginasHemolytic AnaemiaAthul GurudasAinda não há avaliações
- Anemia.: Seminar OnDocumento24 páginasAnemia.: Seminar OnAlma Susan100% (1)
- The Complete Guide on Anemia: Learn Anemia Symptoms, Anemia Causes, and Anemia Treatments. Anemia types covered in full details: Iron-deficiency, Microcytic, Autoimmune Hemolytic, Sideroblastic, and Normocytic AnemiaNo EverandThe Complete Guide on Anemia: Learn Anemia Symptoms, Anemia Causes, and Anemia Treatments. Anemia types covered in full details: Iron-deficiency, Microcytic, Autoimmune Hemolytic, Sideroblastic, and Normocytic AnemiaNota: 3.5 de 5 estrelas3.5/5 (9)
- Normocytic AnemiaDocumento101 páginasNormocytic AnemiaSindhu AdhikariAinda não há avaliações
- Hematology and Coagulation Essentials HandbookDocumento78 páginasHematology and Coagulation Essentials HandbookSadat NazirAinda não há avaliações
- RBC & It's DisorderDocumento101 páginasRBC & It's DisorderSAinda não há avaliações
- The Complete Blood Cell Count A PowerfulDocumento16 páginasThe Complete Blood Cell Count A PowerfulGabriele VitorAinda não há avaliações
- Xenotransfusion of Canine Blood To A CatDocumento3 páginasXenotransfusion of Canine Blood To A CatFelipe GonzalezAinda não há avaliações
- HemolysisDocumento22 páginasHemolysisMohamoud MohamedAinda não há avaliações
- Mini VET GuideDocumento186 páginasMini VET GuideemitibiAinda não há avaliações
- Special Pathology Viva Questions by AMS 46Documento32 páginasSpecial Pathology Viva Questions by AMS 46Mohan Dass100% (1)
- Hereditary SpherocytosisDocumento23 páginasHereditary SpherocytosisKashan SiddiquiAinda não há avaliações
- Sepsis Induced CholestasisDocumento12 páginasSepsis Induced CholestasisYusuf Hakim AjiAinda não há avaliações
- A Review On Anaemia - Types, Causes, Symptoms and Their TreatmentsDocumento9 páginasA Review On Anaemia - Types, Causes, Symptoms and Their TreatmentsCindy AnggraeniAinda não há avaliações
- Hematology and Oncology ' Hematology and Oncology ' Section IiiDocumento20 páginasHematology and Oncology ' Hematology and Oncology ' Section IiiLuis Jose VelazquezAinda não há avaliações
- Approach To The Child With AnemiaDocumento13 páginasApproach To The Child With AnemiavessAinda não há avaliações
- Acquired Hemolytic AnemiaDocumento48 páginasAcquired Hemolytic AnemiaJeena RajAinda não há avaliações
- deGruyter-In Vitro and in Vivo HemolysisDocumento112 páginasdeGruyter-In Vitro and in Vivo HemolysisSAinda não há avaliações
- Approach To The Adult Patient With Anemia - UpToDateDocumento23 páginasApproach To The Adult Patient With Anemia - UpToDateNicole SierraAinda não há avaliações
- Classification of AnaemiaDocumento14 páginasClassification of AnaemiaAbdallah AlasalAinda não há avaliações
- Course Code: NSC 410 Course Title: Practicum and Teaching Methodology MATRIC NUMBER: 19001748Documento6 páginasCourse Code: NSC 410 Course Title: Practicum and Teaching Methodology MATRIC NUMBER: 19001748Kenan Gawinan KekeAinda não há avaliações
- RBCs - Abnormal - Morphology FinalDocumento33 páginasRBCs - Abnormal - Morphology FinalInahkoni Alpheus Sky OiragasAinda não há avaliações
- Hematology 1 Quiz 2 3Documento27 páginasHematology 1 Quiz 2 3Jam Ramos100% (1)
- G6PD, GalactosemiaDocumento32 páginasG6PD, GalactosemiaEricka B. BanaszczukAinda não há avaliações
- 209-Hematology Review - Case StudiesDocumento129 páginas209-Hematology Review - Case StudiesKhalid Khalidi100% (2)
- Haematology Ascp RecallDocumento7 páginasHaematology Ascp RecallMona AliAinda não há avaliações
- First Aid HaematologyDocumento9 páginasFirst Aid Haematologynaeem2009100% (1)
- Pathology - Chapter 14Documento14 páginasPathology - Chapter 14Cory GrayAinda não há avaliações
- Nursing Care of at Risk/ High Risk/ Sick ClientDocumento256 páginasNursing Care of at Risk/ High Risk/ Sick ClientAaron ConstantinoAinda não há avaliações
- Blood Reviews: ReviewDocumento22 páginasBlood Reviews: ReviewJair Alexander Quintero PanucoAinda não há avaliações
- Hematology Trans 10Documento6 páginasHematology Trans 10Claire GonoAinda não há avaliações
- 2019 Pathophysiology Textbook Part2 ZsmuDocumento58 páginas2019 Pathophysiology Textbook Part2 ZsmuSagar KhairwalAinda não há avaliações
- Hematologic System and DisordersDocumento68 páginasHematologic System and DisordersRellie Castro100% (1)