Escolar Documentos
Profissional Documentos
Cultura Documentos
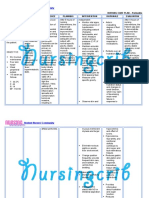
Low Back Pain
Enviado por
Lili Juniarti0 notas0% acharam este documento útil (0 voto)
22 visualizações10 páginasa
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoa
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
22 visualizações10 páginasLow Back Pain
Enviado por
Lili Juniartia
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 10
Low back pain
From Wikipedia, the free encyclopedia
Low back pain
The five vertebrae in the lumbar region of the back are the largest and
strongest in the spinal column.
ICD-10 M54.4-M54.5
ICD-9 724.2
MedlinePlus 003108
eMedicine pmr/73
MeSH D017116
Low back pain (or lumbago) is a common musculoskeletal disorder affecting 80% of people at
some point in their lives. It accounts for more sick leave and disability than any other medical
condition. It can be either acute, subacute or chronic in duration. Most often, the symptoms of low
back pain show significant improvement within a few weeks from onset with conservative
measures.
Contents
[hide]
1 Classification
2 Cause
3 Pathophysiology
4 Diagnostic approach
o 4.1 Imaging
o 4.2 Red flags
5 Prevention
6 Management
o 6.1 Conservative
o 6.2 Acute back pain
o 6.3 Chronic back pain
o 6.4 Surgery
o 6.5 Some or no benefit
7 Prognosis
8 Epidemiology
9 In pregnancy
10 See also
11 References
12 External links
Classification
One method of classifying lower back pain is by the duration of symptoms: acute (less than 4
weeks), sub acute (412 weeks), chronic (more than 12 weeks).
Cause
Most cases of lower back pain are due to benign musculoskeletal problems and are referred to
as non specific low back pain. They are generally believed to be due to a sprain or strain in
the muscles of the back and the soft tissues,especially if the pain arose suddenly during physical
load to the back, and the pain is lateral to the spine. The rate of serious causes is less than
1%. The full differential diagnosis includes many other less common conditions.
Mechanical:
Apophyseal osteoarthritis
Diffuse idiopathic skeletal hyperostosis
Degenerative discs
Scheuermann's kyphosis
Spinal disc herniation ("slipped disc")
Spinal stenosis
Spondylolisthesis and other congenital abnormalities
Fractures
Leg length difference
Restricted hip motion
Misaligned pelvis - pelvic obliquity, anteversion or
retroversion
Abnormal Foot Pronation
Inflammatory:
Seronegative spondylarthritides (e.g. ankylosing spondylitis)
Rheumatoid arthritis
Infection - epidural abscess or osteomyelitis
Neoplastic:
Bone tumors (primary or metastatic)
Intradural spinal tumors
Metabolic:
Osteoporotic fractures
Osteomalacia
Ochronosis
Chondrocalcinosis
Psychosomatic
Tension myositis syndrome
Paget's disease
Referred pain:
Pelvic/abdominal disease
Prostate Cancer
Posture
Depression
[citation needed]
Oxygen deprivation
Pathophysiology
The lumbar region in regards to the rest of the spine.
The lumbar region (or lower back region) is made up of five vertebrae (L1-L5). In between these
vertebrae lie fibrocartilage discs (intervertebral discs), which act as cushions, preventing the
vertebrae from rubbing together while at the same time protecting the spinal cord. Nerves stem
from the spinal cord throughforamina within the vertebrae, providing muscles with sensations and
motor associated messages. Stability of the spine is provided through ligaments and muscles of
the back, lower back and abdomen. Small joints which prevent, as well as direct, motion of the
spine are called facet joints (zygapophysial joints).
Causes of lower back pain are varied. Most cases are believed to be due to a sprain or strain in
the muscles and soft tissues of the back.Overactivity of the muscles of the back can lead to an
injured or torn ligament in the back which in turn leads to pain. An injury can also occur to one of
the intervertebral discs (disc tear, disc herniation). As the body ages, the spine does as well. Due
to aging, discs begin to diminish and shrink in size, resulting in vertebrae and facet joints rubbing
against one another. Ligament and joint functionality also diminishes as one ages, leading
to spondylolisthesis, which causes the vertebrae to move much more than they should. Pain is
also generated through spinal stenosis, sciatica and scoliosis. At the lowest end of the spine, some
patients may have tailbone pain (also called coccyx pain or coccydynia). Others may have pain
from their sacroiliac joint, where the spinal column attaches to the pelvis, called sacroiliac joint
dysfunction. Physical causes may include osteoarthritis, rheumatoid arthritis, degeneration of the
discs between the vertebrae or aspinal disc herniation, a vertebral fracture (such as
from osteoporosis), or rarely, an infection or tumor.
In the vast majority of cases no noteworthy or serious cause is ever identified. Usually the pain
resolves on its own after a few weeks. Intensive testing for a physical cause without waiting for the
pain to recede is not prudent because any problems identified may be irrelevant and misleading.
Diagnostic approach
Acute back pain is defined as pain less than 6 weeks while chronic back pain is defined as pain
that has been present for over three months. The intermediate time period is known as sub acute
back pain. Determination of the underlying cause is usually made through a combination of a
medical history, physical examination, and, when necessary, diagnostic testing, such as an x-
ray, CT scan, orMRI.
Imaging
From 1994 to 2006, MRI scans of the lumbar region increased by 307%. Imaging rates and
surgery rates are directly related. Where imaging rates are highest in the country, surgery rates
are the highest. The American College of Physicians as well as the American Pain Society both
highly advise against consistent imaging in patients who deal with nonspecific low back
pain. However, the use of MRI and CT scans is recommended when a patient deals with
consistent leg and back pain. There is no relation between MRI/CT scans and positive patient
outcomes.
X-ray
X-rays are useful in determining deformities in one's bones. They can provide one with the most
obvious causes of low back pain due to bone fractures or changes in bone due to aging.
Bone density test
Osteoporosis does not cause low back pain; however, bone fractures may occur due
to osteoporosis, resulting in low back pain.
X-rays and CT scans are not required in lower back pain except in the cases where "red flags"
(listed below) are present. If the pain is of a long duration X-rays may increase patient satisfaction.
Red flags
Recent significant trauma
Milder trauma if age is greater than 50 years
Unexplained weight loss
Unexplained fever
Immunosuppression
Previous or current cancer
Intravenous drug use
Osteoporosis
Chronic corticosteroid use
Age greater than 70 years
Focal neurological deficit
Duration greater than 6 weeks
Prevention
Low back pain is common and there are several methods of prevention. Although exercise show
conflicting results in treatment of acute episodes, it is effective in preventing recurrences. Proper
lifting technique may also be important.
A number of studies were conducted about the relationship between the spine and nicotine.
Cigarette smoking is a factor that inversely affects the success and proper healing of spinal fusion
surgery. In patients who underwent cervical fusion, a smokers rate of nonunion was much greater
than a nonsmoker. Smoke and nicotine cause the spine to age faster than normal. Smoking also
reduces blood flow to the lower spine and causes the spinal discs to degenerate.
Management
Conservative
For the vast majority of people, low back pain can be treated conservatively. A number of
recommendations which may help alleviate symptoms include: applying heat or cold,physical
therapy, and continued activity within the limits of the pain with bed rest being discouraged. Firm
mattresses are less likely to lead to improvement when compared with a medium-firm mattress.
Acute back pain
Medications
Short term use of pain and antiinflammatory medications, such as NSAIDs or acetaminophen can
help with the symptoms of lower back pain. However, these medications are not without risk and
for persistent pain a health care practitioner should be consulted. Muscle relaxants for acute and
chronic pain have some benefit, however, there are concerns with side effects, and their routine
use is discouraged. Muscle relaxants are more effective in relieving pain and spasms when they
are used in combination with NSAIDs.
Activity
Staying as physically active as possible is recommended by most guidelines. Bed rest is
discouraged as not being helpful. Even when the pain is severe, some activity is still preferable to
prolonged sitting or lying down, as long as it does not involve movements such as heavy lifting that
would further strain the back. Structured exercise in acute low back pain, however, leads to
neither improvement nor harm.
Spinal manipulation
Most reviews and guidelines have found that spinal manipulation (SM) therapy for low back pain of
unknown cause is of no benefit beyond standard conservative management. A 2007 U.S. guideline
weakly recommended SM as one alternative therapy for spinal low back pain in nonpregnant
adults when ordinary treatments fail,
[32]
. The Swedish guideline for low back pain in 2002 does not
recommend considering SM therapy for acute low back pain in patients needing additional help,
possibly because the guideline's recommendations were based on a higher evidence level. A 2008
review found that SM is similar to other forms of conventional care. A 2007 literature synthesis,
however, found good evidence supporting SM and mobilization for low back pain and exercise for
chronic low back pain. Of four systematic reviews published between 2000 and May 2005, only
one recommended SM, and a 2004 Cochrane review stated that SM or mobilization is no more or
less effective than other standard interventions for back pain. A 2008 systematic review found
insufficient evidence to make any recommendations concerning medicine-assisted manipulation
for chronic low back pain.
[37]
. However, the American College of Physicians and the American pain
Society still recommend spinal manipulation when other conservative forms of treatment for lower
back pain have failed.
Chronic back pain
Low back pain is more likely to be persistent among people who previously required time off from
work because of low back pain, those who expect passive treatments to help, those who believe
that back pain is harmful or disabling or fear that any movement whatever will increase their pain,
and people who have depression or anxiety. A systematic review (2010) published as part of the
Rational Clinical Examination Series in the Journal of the American Medical Association reviews
the factors that predict disability from back pain. The data quantified that patients with back pain
who have poor coping behaviors or who fear activity are about 2.5 times as likely to have poor
outcomes at 1 year.
The following measures have been found to be effective for chronic non-specific back pain :
Exercise appears to be slightly effective for chronic low back
pain. The Schroth method, a specialized physical exercise
therapy for scoliosis, kyphosis, spondylolisthesis, and related
spinal disorders, has been shown to reduce severity and
frequency of back pain in adults with scoliosis.
Tricyclic antidepressants are recommended in a 2007 guideline
by the American College of Physicians and the American Pain
Society.
Acupuncture may help chronic pain
[25]
; however, a more
recent randomized controlled trial suggested insignificant
difference between real and sham acupuncture.
Intensive multidisciplinary treatment programs may help
subacute or chronic low back pain.
Behavioral therapy
The Alexander Technique was shown in a UK clinical trial to have
long term benefits for patients with chronic back pain.
Back schools have shown some effect in managing chronic back
pain.
Spinal manipulation was shown to have a clinical effect similar to
that of other commonly used therapies and was considered safe.
Clinical research shows that treatment according to McKenzie
method is as effective as other commonly used methods
Prolotherapy, facet joint injections, and intradiscal steroid injections have not been found to be
effective. Epidural corticosteroid injections are said to supply the patient with temporary relief
ofsciatica. However studies show that they do not decrease the rate of ensuing
operations. Therapeutic massage is proven to be effective for chronic back pain. Traditional
Chinese Medical acupuncture was proven to be relatively ineffective for chronic back pain.
Surgery
Surgery may be indicated when conservative treatment is not effective in reducing pain or when
the patient develops progressive and functionally limiting neurologic symptoms such as leg
weakness, bladder or bowel incontinence, which can be seen with severe central lumbar disc
herniation causing cauda equina syndrome or spinal abscess.
[citation needed]
Spinal fusion has been
shown not to improve outcomes in those with simple chronic low back pain.
The most common types of low back surgery include microdiscectomy, discectomy, laminectomy,
foraminotomy, or spinal fusion. Another less invasive surgical technique consists of an
implantation of a spinal cord stimulator and typically is used for symptoms of chronic radiculopathy
(sciatica). Lumbar artificial disc replacement is a newer surgical technique for treatment
of degenerative disc disease, as are a variety of surgical procedures aimed at preserving motion in
the spine. According to studies, benefits of spinal surgery are limited when dealing with
degenerative discs.
A medical review in March 2009 found the following: Four randomised clinic trials showed that the
benefits of spinal surgery are limited when treating degenerative discs with spinal pain (no
sciatica). Between 1990 and 2001 there was a 220% increase in spinal surgery, despite the fact
that during that period there were no changes, clarifications, or improvements in the indications for
surgery or new evidence of improved effectiveness of spinal surgery. The review also found that
higher spinal surgery rates are sometimes associated with worse outcomes and that the best
surgical outcomes occurred where surgery rates were lower. It also found that use of surgical
implants increased the risk of nerve injury, blood loss, overall complications, operating times and
repeat surgery while it only slightly improved solid bone fusion rates. There was no added
improvement in pain levels or function.
Spinal fusion
The logic behind spinal fusion is that by fusing two vertebrae together, they will act and function as
a solid bone. Since lumbar pain may be caused by excessive motion of the vertebra the goal of
spinal fusion surgery is to eliminate that extra motion in between the vertebrae, alleviating pain. If
scoliosis or degenerative discs is the problem, the spinal fusion process may be recommended.
There are several different ways of performing the spinal fusion procedure; however, none are
proven to reduce pain better than the others.
Some or no benefit
Additional treatments have been more recently reviewed by the Cochrane Collaboration:
Massage therapy may benefit some patients.
Heat application may have a modest benefit. The evidence for
cold therapy is limited.
Yoga has been found beneficial.
Correcting leg length difference may help by inserting a heel lift or
building up the shoe.
The role of narcotics for chronic low back pain is uncertain.
A 2008 review found antidepressants ineffective in the treatment
of chronic back pain even though some previous studies did find
them helpful.
Transcutaneous electrical nerve stimulation (TENS) has not been
found to be effective in chronic lower back pain.
Prognosis
Most patients with acute lower back pain recover completely over a few weeks regardless of
treatments. With the usual lumbar muscle strain or sprain as the cause, over 90% of patients are
completely recovered within one month. Although an episode of lower back pain may settle
quickly, recurrence rates are about 50% in the following 12 months. About 2% of the population
with low back pain are temporarily or chronically disabled by their form of low back pain. 41% of
adults aged between 26 and 44 years reported having back pain in the previous 6 months. Most
had occasional episodes of pain that lasted a few days, was mild or moderate in intensity, and did
not limit activities. Although a high percentage of individuals have persistent lower back pain, 75%
of them self-manage their problem and a few become significantly disabled by low back pain. In
the United States, the costs of low back pain range between $38 and $50 billion a year and there
are 300,000 operations annually. Along with neck operations, back operations are the 3rd most
common form of surgery in the United States.
Epidemiology
Over a life time 80% of people have lower back pain,with 26% of American adults reporting pain of
at least one day in duration every three months.
In pregnancy
50-70% of all pregnant women experience back pain.
As one gets farther along in the pregnancy, due to the additional weight of the baby, ones center
of gravity will shift forward causing ones posture to change. This change in posture leads to
increasing lower back pain.
The increase in hormones during pregnancy is in preparation for birth. This increase of hormones
softens the ligaments in the pelvic area and loosens joints. This change in ligaments and joints
may alter the support in which ones back is normally used to.
Você também pode gostar
- Brain DeathDocumento25 páginasBrain DeathLili JuniartiAinda não há avaliações
- Terminal Branches: HomonymousDocumento1 páginaTerminal Branches: HomonymousSheiLa AdelinaAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (894)
- Blood VesselsDocumento29 páginasBlood VesselsLili JuniartiAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Tumor CerebriDocumento36 páginasTumor CerebriLili JuniartiAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Tumor CerebriDocumento36 páginasTumor CerebriLili JuniartiAinda não há avaliações
- 2012 Spring/Summer Issue of Arthritis ActionDocumento9 páginas2012 Spring/Summer Issue of Arthritis ActionAFIndianaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Evidence Based Practice in Postgraduate Healthcare EducationDocumento29 páginasEvidence Based Practice in Postgraduate Healthcare EducationGab FgilzcheAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- 1948 Staff Listing for PREPPO HospitalDocumento481 páginas1948 Staff Listing for PREPPO Hospitalpriya selvarajAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Intimacy and Solitude Chapter SamplerDocumento21 páginasIntimacy and Solitude Chapter SamplerAllen & Unwin100% (1)
- Consumer preference towards tea consumption in Ahmedabad CityDocumento6 páginasConsumer preference towards tea consumption in Ahmedabad CityVrushang MaturkarAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Leading and Managing in Canadian Nursing 1st Edition Yoder Wise Test Bank Full Chapter PDFDocumento30 páginasLeading and Managing in Canadian Nursing 1st Edition Yoder Wise Test Bank Full Chapter PDFKristyCarterctdr100% (12)
- Nursing Care Plan For Peritonitis NCPDocumento2 páginasNursing Care Plan For Peritonitis NCPderic83% (6)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Mee 235Documento28 páginasMee 235EmmanuelAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Microbiology 2012 13Documento101 páginasMicrobiology 2012 13Qurratulain AliAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Stock report for drug store sectionDocumento113 páginasStock report for drug store sectionsriramAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Roche Upath IVD Algorithm GuideDocumento42 páginasRoche Upath IVD Algorithm Guide肥塚泰Ainda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Interventions For Preventing Falls in People After Stroke (Review)Documento68 páginasInterventions For Preventing Falls in People After Stroke (Review)Abdelrhman AhmedAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- Stihl Ts 410 420 Owners Instruction ManualDocumento112 páginasStihl Ts 410 420 Owners Instruction ManualLucyan IonescuAinda não há avaliações
- Psychiatric Outcomes After Temporal Lobe Surgery in Patients With Temporal Lobe Epilepsy and Comorbid Psychiatric IllnessDocumento8 páginasPsychiatric Outcomes After Temporal Lobe Surgery in Patients With Temporal Lobe Epilepsy and Comorbid Psychiatric IllnessFrancisco Javier Fierro RestrepoAinda não há avaliações
- Foronda Et Al - Cultural Humility - A Concept AnalysisDocumento8 páginasForonda Et Al - Cultural Humility - A Concept AnalysisabcAinda não há avaliações
- Ice Storage ThesisDocumento8 páginasIce Storage Thesisvaj0demok1w2100% (2)
- Comparing Anxiety and Clinical Success of Composites vs Colored CompomersDocumento7 páginasComparing Anxiety and Clinical Success of Composites vs Colored CompomersRaul GhiurcaAinda não há avaliações
- Visible Safety and Induction: Hse Management Visit ChecklistDocumento6 páginasVisible Safety and Induction: Hse Management Visit ChecklistHARSHALAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Health Systems in EthiopiaDocumento44 páginasHealth Systems in EthiopiaFuad Aman AbjAinda não há avaliações
- The Age of Anxiety: Baroque EclogueDocumento124 páginasThe Age of Anxiety: Baroque EclogueSatish100% (4)
- An Introduction to EFTDocumento25 páginasAn Introduction to EFTdiplomat0Ainda não há avaliações
- Good Clinical Laboratory Practice (GCLP) : Quality Demanding From Clinical LaboratoriesDocumento5 páginasGood Clinical Laboratory Practice (GCLP) : Quality Demanding From Clinical LaboratoriesJaneAinda não há avaliações
- Explore The Role of The HCA in The Promotion of Positive AgeingDocumento9 páginasExplore The Role of The HCA in The Promotion of Positive Ageing1chirciu1976floAinda não há avaliações
- How to Cite Patient Safety Incident Reporting SystemDocumento7 páginasHow to Cite Patient Safety Incident Reporting System'Amel'AyuRizkyAmeliyahAinda não há avaliações
- Formulation and Evaluation of Enteric CoatedDocumento13 páginasFormulation and Evaluation of Enteric Coatedvanvu buiAinda não há avaliações
- Clinical Case ConferenceDocumento22 páginasClinical Case ConferenceTallal BurwagAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Pico 2Documento14 páginasPico 2Hend maarofAinda não há avaliações
- Anthropology: Anthropology Is The Scientific Study of Humans, Human BehaviorDocumento26 páginasAnthropology: Anthropology Is The Scientific Study of Humans, Human BehaviorAliaAinda não há avaliações
- REPUBLIC ACT NO. 10354 (The Responsible Parenthood and Reproductive Health Act of 2012) PDFDocumento15 páginasREPUBLIC ACT NO. 10354 (The Responsible Parenthood and Reproductive Health Act of 2012) PDFYappi NaniAinda não há avaliações
- Biotechnology & Genetic EngineeringDocumento16 páginasBiotechnology & Genetic EngineeringMohammed RidzuwanAinda não há avaliações