Escolar Documentos
Profissional Documentos
Cultura Documentos
Management of Competitive Athletes With Diabetes: in Brief
Enviado por
Deritanti Fitria Riskiana0 notas0% acharam este documento útil (0 voto)
37 visualizações6 páginasExercise has been recommended as an important therapeutic tool for most patients with diabetes and for those at risk for diabetes. An effective management plan must consider the typical demands of training and competition. Anecdotal descriptions of management strategies used by athletes with diabetes are few.
Descrição original:
Título original
102.full.pdf
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoExercise has been recommended as an important therapeutic tool for most patients with diabetes and for those at risk for diabetes. An effective management plan must consider the typical demands of training and competition. Anecdotal descriptions of management strategies used by athletes with diabetes are few.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
37 visualizações6 páginasManagement of Competitive Athletes With Diabetes: in Brief
Enviado por
Deritanti Fitria RiskianaExercise has been recommended as an important therapeutic tool for most patients with diabetes and for those at risk for diabetes. An effective management plan must consider the typical demands of training and competition. Anecdotal descriptions of management strategies used by athletes with diabetes are few.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 6
102
Diabetes Spectrum Volume 18, Number 2, 2005
In Brief
Management of Competitive Athletes
With Diabetes
Exercise has been recommended as an
important therapeutic tool for most
patients with diabetes and for those at
risk for diabetes.
1,2
The American
Diabetes Association (ADA) Council
on Exercise has released two valuable
handbooks to assist health care pro-
fessionals in exercise management.
3,4
The most recent of these publications
acknowledges remarkable progress
in the scientific understanding of dia-
betes and exercise, especially in the
areas of biochemical events that regu-
late muscle metabolism, diabetes pre-
vention, exercise maintenance, and
exercise prescription.
4
It is now easier
to make appropriate decisions regard-
ing who should exercise, what types
of physical activity are appropriate,
and how often, how long, and how
intense physical activity should be.
One area of scientific understand-
ing that remains extremely limited is
management of competitive athletes
with diabetes. While there are a num-
ber of anecdotal descriptions of man-
agement strategies used by these ath-
letes and several published case
reports, there are very few well-con-
trolled studies that add to our knowl-
edge of formulating effective treat-
ment plans. It is encouraging to find
that athletes with diabetes have been
able to achieve outstanding success at
all levels of competition from school-
yard playing fields to the Olympic
games. Management of competitive
athletes with diabetes presents far dif-
ferent challenges than those typically
encountered in routine patient care.
An effective management plan must
consider the typical demands of train-
ing and competition, the goals of the
athlete, factors related to sports par-
ticipation that may affect glucose
homeostasis, safety of athletic partici-
pation, adequate monitoring of blood
glucose, and possible adjustments to
diet and insulin to allow safe and
effective athletic performance.
Energy Demands of Sports
Competition
Exercise has been defined as any form
of body movement that results in an
increase in metabolic demand.
5
In
general, it is common to describe the
metabolic processes that supply ener-
gy for muscular contractions to move
the body as being either aerobic (with
oxygen) or anaerobic (without oxy-
gen).
6
In reality, most physical activity
is some combination of both aerobic
and anaerobic exercise, but the activi-
ty is typically classified based on
which energy system predominates.
We usually prescribe aerobic exercise
for development of cardiorespiratory
fitness and anaerobic exercise, such as
resistance training, for development of
muscular fitness and strength.
Physical activity recommendations
for healthy adults and for patients
with type 2 diabetes are quite similar.
W. Guyton Hornsby, Jr., PhD, CDE,
and Robert D. Chetlin, PhD, CSCS
An effective management plan for an athlete with type 1 diabetes must con-
sider the energy demands of intense competition and training, the athletes
goals, factors related to competitive sports that may affect glucose homeosta-
sis, and strategies that may be employed to allow safe, effective sports partici-
pation. Athletes should be appropriately screened, counseled to avoid risky
behaviors, and provided with specific recommendations for glucose monitor-
ing and insulin and diet adjustments so that they may anticipate and compen-
sate for glucose responses during sports competition.
103
Diabetes Spectrum Volume 18, Number 2, 2005
F
r
o
m
R
e
s
e
a
r
c
h
t
o
P
r
a
c
t
i
c
e
/
M
o
v
i
n
g
A
h
e
a
d
W
i
t
h
P
h
y
s
i
c
a
l
A
c
t
i
v
i
t
y
The American College of Sports
Medicine (ACSM) recommends aero-
bic exercise at 5085% of the maxi-
mal volume of oxygen that can be
consumed (V
.
O
2max
) for promoting car-
diorespiratory fitness and one set of
eight to twelve repetitions using eight
to ten resistance exercises for develop-
ing muscular fitness and strength in
healthy adults.
7
ACSM and ADA rec-
ommend aerobic exercise at an inten-
sity of 4070% of V
.
O
2max
and anaero-
bic exercise for a minimum of one set
of ten to fifteen repetitions using eight
to ten resistance exercises for most
patients with type 2 diabetes.
8
Mod-
ifications may be necessary depending
on comorbid conditions.
It is important to recognize that the
metabolic demands of the recom-
mended aerobic activity for healthy
adults and for the management of
patients with type 2 diabetes are a
percentage of the V
.
O
2max
and are
intended to minimize contributions of
the anaerobic energy systems. These
exercise prescriptions are intentionally
designed to be moderate in intensity
so that individuals can be active for
extended periods of time (2060 min-
utes) to allow for an adequate stimu-
lus to increase or maintain aerobic
capacity and to expend sufficient
caloric energy to assist with weight
control. The vast majority of research
in diabetes and exercise has utilized
exercise intensities from 40 to 85%
V
.
O
2max
, and this research forms the
basis for clinical decisions regarding
exercise management.
Type 2 diabetes is extremely rare in
competitive athletes. This discussion
will be limited to considering the
management of type 1 diabetes in
school-aged children and adolescents
participating in school and communi-
ty sport activities, college athletes, and
young adults participating in highly
competitive amateur and professional
sports. Many of these individuals will
be without any significant long-term
complications. General benefits of
physical activity for those with type 1
diabetes include enhancement of phys-
ical fitness, reduction in cardiovascu-
lar disease risk, and improved social
and emotional well-being. The prima-
ry risks of physical activity in type 1
patients who do not have complica-
tions are exercise-induced hypo-
glycemia and aggravation of hyper-
glycemia and ketosis.
Most competitive sports are not
aerobic in terms of the major energy
systems involved. Team sports such as
football, baseball, softball, basketball,
and soccer rely primarily on relatively
brief bursts of explosive, high-power
output and primarily rely on the
adenosine triphosphate-phosphocrea-
tine (ATP-PC) energy system for mus-
cular contractions. These energy
stores are extremely limited and can
provide maximal power output for
only 810 seconds.
9
Muscles can continue to contract
for longer periods by utilizing anaero-
bic glycolysis. This system is only
about half as fast as the ATP-PC sys-
tem but allows activity to continue at
fairly high power outputs for an addi-
tional 1.52 minutes. The anaerobic
glycolysis energy system can allow an
individual to perform all-out exercise
for longer than a few seconds, but
large amounts of lactic acid accumu-
late within the contracting muscles
and ultimately in the blood. As activi-
ty continues much beyond 2 minutes,
the intensity of activity must be
reduced, muscles must be provided
with oxygen, and there is a gradual
shift to aerobic metabolism.
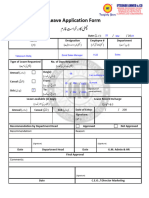
Figure 1 describes the relative
involvement of energy systems for
many competitive sports.
10
Obviously,
the energy requirements may differ
depending on the level of competition
and may also vary from position to
position for team sports, but should
serve to illustrate the importance of
the ATP-PC system and anaerobic gly-
colysis for athletic competition.
The energy demands of training for
a particular sport can be quite differ-
ent depending on the age of the ath-
lete, the level of competition, and the
specific metabolic goals of training.
Exercise training for an athlete with
diabetes is usually determined by a
coach rather than by any member of
the health care team. Health care pro-
fessionals should attempt to gather
information about the specific train-
ing practices and be able to provide
recommendations for blood glucose
monitoring and reasonable adjust-
ments to diet and insulin therapy so
that athletes may be able to achieve
peak performance in their chosen
sport activities.
Goals of the Athlete
Motivation to become involved in
sport activities typically has little to
do with benefits of health. One group,
observing that children and adoles-
cents with diabetes are more likely to
spend time in sport activities than
those without diabetes, has proposed
this may be a result of diabetes educa-
tion encouraging active lifestyles or
may be a compensating social behav-
ior that allows young people with
diabetes to feel more accepted by their
peers.
11
Studies that have examined
motives for sport participation have
identified factors related to excitement
and competition, appearance, fun,
team atmosphere, friendship, achieve-
ment, and skill development.
12,13
Athletes in high school, college, and
professional sports may be motivated
by these factors as well but may have
the additional incentive of potential or
actual financial rewards. College
scholarships can be worth as much as
$200,000, and professional sports
contracts and endorsements may
bring from hundreds of thousands to
millions of dollars. Whether the moti-
Figure 1. Relative energy system involvement for competitive sports. Adapted
from Ref. 10.
Weightlifting, Power lifting
Track (sprinting and field events), Diving (platform & springboard)
Golf, American football, Swimming (sprints), Gymnastics, Fencing
Wrestling, Baseball, Softball, Volleyball, Ice hockey, Track cycling
Basketball, Soccer, Tennis, Lacrosse
Speed skating (5001000 m)
Skiing (slalom & downhill), Field hockey
Rowing
Running (middle distance), Speed skating (> 1500 m)
Road cycling
In-line skating
Cross country skiing
Race walking
Marathon running
Iron Man triathlon
Ultra-marathon running
Aerobic
Anaerobic
Glycolysis
ATP - PC
Anaerobic
104
Diabetes Spectrum Volume 18, Number 2, 2005
vating factor is the desire for an
Olympic gold medal or simply to be
part of the team, it should be
remembered that the specific goals of
the athlete may be far more important
than blood glucose control or avoid-
ance of complications.
One common goal in competitive
sports is to improve performance.
Unfortunately, athletes may resort to
a number of practices that can com-
promise blood glucose control and
health in general in an attempt to gain
a competitive advantage. These may
include unsafe dietary patterns, use of
nutritional supplements and other
ergogenic aids, and the use of illegal
drugs.
Common dietary problems seen in
athletes include the female athlete
triad (described below), rapid weight
loss to make weight, and excessive
consumption of a single macronutri-
ent, such as protein. It is important to
be familiar with these practices and to
counsel athletes appropriately.
Minimizing Risky Behaviors
The female athlete triad of disordered
eating, amenorrhea, and osteoporosis
was first identified in 1997 and is
often found in womens endurance
sports that emphasize low body
weight, such as distance running, or
aesthetic sports, such as gymnastics,
figure skating, cheering, and bal-
let.
14,15
A study of weight control
practices in type 1 diabetes reported
unhealthy weight control in 37.9% of
adolescent females and found that
methods used included skipping
insulin or taking less insulin in an
effort to control body weight.
16
The
topic of eating disorders in adolescent
girls and young women with type 1
diabetes has been explored in depth,
and it is clear that the problem is fair-
ly common and is associated with
poor metabolic control.
17
Anyone
managing female athletes with dia-
betes, especially those involved in
sports having a high prevalence of the
female athlete triad, should be sensi-
tive to prevention and early identifica-
tion and treatment of this problem.
Omission of insulin is a common
practice for athletes with diabetes
who compete in sports having weight
categories, such as wrestling, boxing,
and weightlifting. Practices frequently
used by athletes without diabetes to
make weight include dehydration
through perspiration, use of laxatives,
diet pills, and diuretics, as well as
vomiting.
18
Even though the National
Collegiate Athletic Association and
most state high school leagues have
implemented programs to reduce
unhealthy weight loss in the sport of
wrestling, the practice of significantly
reducing weight before competition
with subsequent weight gain after the
event still persists.
19
Athletes with dia-
betes quickly discover they can rapid-
ly lose weight by withholding insulin
until after weighing in. Metabolic
control is obviously poor during the
time that insulin is omitted, and there
is always the serious risk of ketoaci-
dosis. This is a difficult problem
because the practice obviously works,
and athletes with type 1 diabetes are
often willing to take the associated
risks.
Athletes with or without diabetes
require adequate amounts of macro-
nutrients to support their training and
sustain performance during competi-
tion. A joint position statement issued
by the ACSM, the American Dietetic
Association, and the Dietitians of
Canada summarized general nutrient
requirements for competitive ath-
letes.
20
These included:
Carbohydrate consumption ranging
from 6 to 10 g/kg of body weight/
day to maintain blood glucose and
replace muscle glycogen during
activity. It was stated that a speci-
fied amount was dependent on the
individuals daily total energy
expenditure, sport type, sex, and
environmental circumstances.
Protein consumption ranging from
1.2 to 1.4 g/kg of body weight/day
for endurance-trained athletes to
maintain nitrogen balance and 1.6
to 1.7 g/kg of body weight/day for
strength-trained athletes to permit
the accretion and maintenance of
muscle mass. If total energy intake
is adequate to maintain body
weight, adequate protein can be
obtained solely through the diet,
without fortification from protein
supplements.
Fat consumption should range from
20 to 25% of total daily calories,
the majority of which should be in
unsaturated form. Fat is critically
important in athletic diets because
it provides energy, fat-soluble vita-
mins, and essential fatty acids for
daily activity and health. Some
investigators have quantified this
amount from 5 to 10 g/kg of body
weight/day, depending on training
intensity.
21,22
There is no scientific
evidence indicating that high-fat
diets enhance athletic performance.
Total energy consumption ranging
from 37 to 41 kcal/kg of body
weight/ day for endurance athletes
training at moderate intensity to 44
to 50+ kcal/kg of body weight/day
for resistance-trained athletes.
Strength and power athletes
attempting to increase lean mass
should consume sufficient amounts
of energy to support muscle
growth. Numeric estimations of
energy intake, the authors noted,
are somewhat crude in approximat-
ing the energy requirements of indi-
vidual athletes. However, any ath-
lete must consume enough energy
to maintain desirable weight and
body composition while training
for and competing in specific
sports.
Though some diets have become
popular in weight-loss circles (e.g.,
Atkins, South Beach, Pritikin,
Zone), there is no scientific data that
suggests that any of these approach-
es will improve performance. Some
of these strategies, in fact, promote
low or very low consumption of car-
bohydrates, with the stated intent of
producing ketoacidosis, the mobi-
lization of ketone bodies for metab-
olism. Ketoacidosis, however, is a
serious metabolic disturbance, and
its detrimental effects in people with
diabetes have been well established.
It is, therefore, recommended that
athletes with type 1 diabetes avoid
carbohydrate-restricted diets. A
balanced diet composed of
5560% of energy from carbohy-
drate, 1218% of energy from pro-
tein, and 2530% of energy from fat
is recommended for competitive
athletes.
These recommendations for nutri-
tion were developed for athletes with-
out special consideration for type 1
diabetes. They should be used only
within the guidelines set forth in the
ADA position statement Nutrition
Principles and Recommendations in
Diabetes.
23
Strength-trained athletes with dia-
betes require adequate amounts of
protein just like all other individuals
engaged in resistance exercise. While
the needs of resistance-trained ath-
letes and individuals engaged in
chronic intense exercise are higher
than those of sedentary individuals,
this need is usually met by eating a
balanced diet that is higher in energy
intake. There is evidence that indi-
cates that large amounts of protein
105
Diabetes Spectrum Volume 18, Number 2, 2005
F
r
o
m
R
e
s
e
a
r
c
h
t
o
P
r
a
c
t
i
c
e
/
M
o
v
i
n
g
A
h
e
a
d
W
i
t
h
P
h
y
s
i
c
a
l
A
c
t
i
v
i
t
y
(i.e., > 2.4 g/kg/day), including that
provided through supplementation,
may place additional stress on the
kidneys.
24
Individuals with preexist-
ing renal conditions may be particu-
larly susceptible to impaired kidney
function during heightened protein
consumption.
Athletes often turn to nutritional
supplements in the belief that perfor-
mance will be improved. Competitive
athletes with type 1 diabetes should
recognize which products may result
in harmful effects as well as those that
are likely to be a waste of money.
Some of the popular nutritional sup-
plements include fat burners, thermo-
genic enhancers, boosters, ephedra,
chitin, medium-chain triglycerides, cre-
atine monohydrate, and androstene-
dione. These supplements and their
use in diabetes management have been
previously described in detail.
25
Anabolic steroids are synthetic
derivatives of testosterone. Though
access to anabolic steroids is restricted
to specific medical interventions, their
use in sports remains widespread in
the United States, perhaps involving as
many as 3 million athletes.
26
Recent
media coverage has heightened public-
ity surrounding anabolic steroids.
Available studies have used untrained
men taking both pharmacological and
suprapharmacological doses of the
drug. Whereas most investigations
examining pharmacological adminis-
tration have shown little if any
improvement in body composition or
strength, some studies employing
suprapharmacological doses have
indeed shown beneficial changes in
lean mass, strength, and perfor-
mance.
27,28
Studies involving the high
doses believed to improve performance
in athletes are nonexistent, largely
because of the ethical considerations
of administering large amounts of dan-
gerous drugs to nonclinical popula-
tions. Anecdotal evidence indicates
that suprapharmacological administra-
tion of anabolic steroids in competitive
athletes definitively improves perfor-
mance.
Reports of adverse side effects asso-
ciated with anabolic steroid use have
been documented and included car-
diovascular disease, hypertension,
hepatic disease, hormonal dysfunc-
tion, abnormal lipoprotein changes
(increased LDL cholesterol, decreased
HDL cholesterol), and personality dis-
orders. No evidence, even anecdotal
reports, of the effects of anabolic
steroid use in athletes with type 1 dia-
betes is available. However, because
of the known systemic disturbances
associated with anabolic steroid use, it
is clear that athletes with type 1 dia-
betes should not experiment with this
class of drugs.
Competitive sports are generally
safe for anyone with type 1 diabetes
who is in good metabolic control and
without long-term complications.
2
A
careful medical history and physical
examination can minimize risk. The
examination should attempt to identi-
fy whether the athlete is at increased
risk of orthopedic injuries, back or
neck injuries, and dental trauma and
should also include visual acuity and
hearing screening. For long-term com-
plications of diabetes, the exam
should focus on signs and symptoms
of disease affecting the heart and
blood vessels, eyes, kidneys, feet, and
nervous system. A formal graded
exercise test is usually not necessary
but may be helpful if the athlete has
one of the following:
Age > 35 years
Age > 25 years and type 1 diabetes
of duration > 15 years
Presence of any additional risk fac-
tor for coronary artery disease
Presence of proliferative retinopa-
thy or nephropathy including
microalbuminuria
Peripheral vascular disease
Autonomic neuropathy
2
The most common acute risks for
competitive athletes with diabetes are
exercise-induced hypoglycemia and
deterioration of hyperglycemia and
ketosis brought on by physical activity
during periods of hypoinsulinemia.
Blood glucose is relatively unchanged
during exercise in individuals without
diabetes because glucose uptake by
skeletal muscles is precisely matched
by glucose released from the liver.
One important control over this
mobilization of fuel is a reduction in
circulating insulin. People with type 1
diabetes must rely on exogenous
insulin and are unable to reduce circu-
lating insulin at the onset of exercise.
This frequently results in hypo-
glycemia because there is an imbal-
ance of increased glucose uptake by
skeletal muscles with inadequate
hepatic glucose release.
When insulin is not available to
assist in the transport of glucose into
skeletal muscles during exercise, glu-
cose uptake is decreased, glucose
release from the liver is increased, and
there is a rise in blood glucose.
Without adequate insulin, skeletal
muscles will be forced to rely on fat as
fuel, and eventually this can lead to an
increase in ketone bodies. Individuals
with diabetes should not exercise if
insulin is inadequate. Athletes with
diabetes should not exercise when
blood glucose is > 250 mg/dl and
ketosis is present. If glucose is > 300
mg/dl, it is probably inadvisable to
exercise even without ketosis.
2
The Management Plan
There are a number of recommenda-
tions for strategies that may be useful
in the management of competitive ath-
letes with type 1 diabetes, but they are
not well supported by the scientific lit-
erature.
2932
Most competitive athletes
learn by trial and error and by sharing
personal experiences with other ath-
letes.
33
The Diabetes Exercise and
Sports Association (http://www.diabetes-
exercise.org) may be a valuable
resource for any athlete with diabetes
who is interested in sports competi-
tion.
Of those investigations that have
examined athletes with diabetes, one
study reported blood glucose respons-
es for two consecutive years in ath-
letes using different diet and insulin
adjustments while competing in a 75-
km cross-country ski race,
34
and
another reported fuel homeostasis and
insulin sensitivity in 11 athletes with
diabetes from a variety of endurance
and power sports.
35
Subjects in the
cross-country skiing study began the
consecutive annual races with blood
glucose levels at 365 32.4 mg/dl
and 232 28.8 mg/dl.
34
Athletes in
the second study were found to have
lower total insulin doses but did not
have improved insulin sensitivity and
had higher hemoglobin A
1c
(A1C) lev-
els when compared to sedentary sub-
jects with type 1 diabetes.
35
One addi-
tional observation reported that chil-
dren and adolescents with type 1 dia-
betes involved in competitive sports
had a lower daily insulin dose, but
these activities were not associated
with improved A1C.
11
These findings suggest that athletes
with type 1 diabetes are not achieving
good blood glucose control. This may
be because athletes are intentionally
competing with high blood glucose
levels to prevent exercise-induced
hypoglycemia, or diet and insulin
strategies are simply not yet good
enough to achieve tight control. A
case study providing guidelines for the
management of a collegiate football
106
Diabetes Spectrum Volume 18, Number 2, 2005
player describes setting target blood
glucose levels between 150 and 250
mg/dl.
36
Using a very detailed manage-
ment plan, the authors were able to
limit hypoglycemia during football
games to only two episodes, and these
were reported as 55 and 65 mg/dl.
The Diabetes Control and Comp-
lications Trial conclusively demon-
strated that the risk of development
or progression of long-term complica-
tions can be reduced by intensive
treatment resulting in a reduction in
A1C.
37
The risk of hypoglycemia was
increased threefold with intensive
management. It is likely that many
athletes with type 1 diabetes are
chronically hyperglycemic to avoid
exercise-induced hypoglycemia.
Questions remaining to be answered
include the following:
Does hyperglycemia interfere with
athletic performance?
Does improved glucose control
translate into improved perfor-
mance?
What blood glucose targets are
appropriate for competitive athletes
with type 1 diabetes?
It is likely that poor control of
blood glucose increases susceptibility
to infection.
38
Sport activities are fre-
quently associated with cuts, scrapes,
and blisters, which must be treated
appropriately. It is important for ath-
letic training personnel to be aware of
athletes with type 1 diabetes and to
pay special attention to any injury
that is susceptible to infection. It is
also important for athletic training
staff to be aware of treatment modali-
ties that may alter absorption of
injected insulin. These may include
massage therapy, ice therapy, or heat
and whirlpool therapy.
The management plan for athletes
with type 1 diabetes must attempt to
anticipate blood glucose responses to
sports training and competition.
Ideally, blood glucose will be moni-
tored and recorded before and after
each meal, as well as before, during,
and after each training session and
athletic contest. It is also helpful to
have descriptions of the exercise per-
formed with the type, duration, and
intensity of exercise, as well as any
significant environmental conditions.
If sports training is just beginning, or
if training is dramatically increased,
blood glucose should also be moni-
tored at 2:00 a.m.
Appropriate blood glucose targets
can be established based on the pat-
tern of blood glucose responses and
the ability of the individual athlete to
make appropriate adjustments to keep
glucose in the target range. At the
beginning of sports training, it is often
necessary to adjust insulin therapy by
decreasing the total insulin dose by
2050%. Reductions may be needed
in both short- or rapid-acting insulin
and intermediate- or long-acting
insulin. Athletes on pump therapy
may need to decrease bolus doses by
2050% and may choose to discon-
tinue basal insulin during exercise and
decrease the basal insulin by 25%
after exercise is completed.
The site and timing of insulin injec-
tion can affect the glucose response to
exercise. If subcutaneous insulin is
injected over muscles that will be
actively contracting, insulin absorp-
tion will be accelerated. Insulin may
be also be absorbed at a faster rate if
exercise begins < 30 minutes after
injection. It is recommended that
insulin should be injected > 60 min-
utes before the start of activity.
Changing the region of the injection
site (thigh vs. abdomen, for example)
is generally not recommended because
this may also alter the time course of
insulin absorption. The general rec-
ommendation is to rotate the injection
sites within the same region rather
than to alter the region that is used.
Once the athlete is accustomed to
training, most adjustments to prevent
exercise-induced hypoglycemia will be
made by dietary supplementation with
carbohydrate. Typically, this will
involve a specified amount of carbo-
hydrate at an appropriate time to
match the anticipated reduction in
blood glucose. The amount of carbo-
hydrate required is usually 1560 g.
Drinks containing 510% carbohy-
drate may be good choices to assist
with fluid loss during exercise. Most
commercial sports drinks have
approximately 67% carbohydrate.
Actual amounts are easily determined
from the labels. Drinks containing
> 10% carbohydrate may cause gas-
trointestinal distress and should prob-
ably be diluted.
Sport activities by their nature are
unpredictable. A tennis match that is
expected to take 40 minutes may turn
into a 2-hour contest. The glucose
response to exercise is affected by fac-
tors such as exercise intensity, exercise
duration, time of day, environmental
conditions, emotional stress or excite-
ment, and absorption of insulin and
dietary supplements. When the man-
agement plan does not adequately
adjust for the glucose response, there
should be a plan for appropriate com-
pensation. Rapidly absorbable carbo-
hydrate should be readily available.
Coaches, athletic trainers, team physi-
cians, teammates, and parents should
be familiar with signs of hypo-
glycemia, be trained to monitor blood
glucose, and be able to assist athletes
in case of hypoglycemia.
A successful early experience in
competitive sports can be an impor-
tant foundation for a lifetime of
active living. Sports can improve
health, fitness, psychological well-
being, and social interaction. Safe
participation is possible for the large
majority of athletes with diabetes.
Most of these individuals have a
strong drive to make the most of their
abilities, and a properly devised man-
agement plan can be an important
tool to help them reach their competi-
tive performance goals.
References
1
American College of Sports Medicine: Exercise
and type 2 diabetes (Position Stand). Med Sci
Sports Exerc 32:13451360, 2000
2
American Diabetes Association: Physical activi-
ty/exercise and diabetes (Position Statement).
Diabetes Care 27 (Suppl. 1):S58S62, 2004
3
Ruderman N, Devlin JT, Schneider SH (Eds.):
Handbook of Exercise in Diabetes. Alexandria
Va., American Diabetes Association, 2001
4
Ruderman N, Devlin JT (Eds.): The Health
Professionals Guide to Diabetes and Exercise.
Alexandria Va., American Diabetes Association,
1995
5
Caspersen CJ, Powell KE, Christenson GM:
Physical activity, exercise, and physical fitness:
definitions and distinctions for health-related
research. Public Health Rep 100:126131, 1985
6
Ivy JL: Exercise physiology and adaptations to
training. In The Health Professionals Guide to
Diabetes and Exercise. Ruderman N, Devlin JT,
Eds. Alexandria Va., American Diabetes
Association, 1995, p. 2362
7
American College of Sports Medicine: The rec-
ommended quantity and quality of exercise for
developing and maintaining cardiorespiratory
and muscular fitness in healthy adults (Position
Statement). Med Sci Sports Exerc 22:265274,
1990
8
Albright A, Franz M, Hornsby G, Kriska A,
Marrero D, Ullrich I, Verity LS: American
College of Sports Medicine Position Stand:
Exercise and type 2 diabetes. Med Sci Sports
Exerc 32:13451360, 2000
9
Sherwood L: Human Physiology: From Cells to
Systems. 5th ed. Pacific Grove, Calif., Brooks
Cole Publishing, 2004
10
Foss ML, Keteyian SJ: Foxs Physiological
Basis for Exercise and Sport. 6th ed. Boston,
Mass., McGraw Hill, 1998
107
Diabetes Spectrum Volume 18, Number 2, 2005
F
r
o
m
R
e
s
e
a
r
c
h
t
o
P
r
a
c
t
i
c
e
/
M
o
v
i
n
g
A
h
e
a
d
W
i
t
h
P
h
y
s
i
c
a
l
A
c
t
i
v
i
t
y
11
Raile R, Kapellen T, Schweiger A, Hunkert F,
Nietzshmann U, Dost A, Kiess W: Physical activ-
ity and competitive sports in children and adoles-
cents with type 1 diabetes. Diabetes Care
22:19041905, 1999
12
Koivula N: Sport participation: differences in
motivation and actual participation due to gen-
der typing. J Sports Behav 22:360380, 1999
13
Zahariadis PN, Biddle SJH: Goal orientations
and participation motives in physical education
and sport: their relationship in English school-
children. Athletic Insight: The Online Journal of
Sport Psychology. vol. 2, 2002. Available online
at http://www.athleticinsight.com
14
American College of Sports Medicine: Position
Stand: The female athlete triad. Med Sci Sports
Exerc 29(5):iix, 1997
15
Hobart JA, Smucker DR: The female athlete
triad. Am Fam Phys 61:33573364, 2000
16
Neumark-Sztainer D, Patterson J, Mellin A,
Ackard DM, Utter J, Story M, Sockalosky J:
Weight control practices and disordered eating
behaviors among adolescent females and males
with type 1 diabetes: associations with sociode-
mographics, weight concerns, familial factors,
and metabolic outcomes. Diabetes Care
25:12891296, 2002
17
Daneman D (Ed): From research to practice:
eating disorders. Diabetes Spectrum15:83105,
2002
18
Kiningham RB, Gorenflo DW: Weight loss
methods of high school wrestlers. Med Sci Sports
Exerc 33:810813, 2001
19
Ransone J, Hughes B: Body-weight fluctuation
in collegiate wrestlers: implications of the
National Collegiate Athletic Association weight-
certification program. J Athl Train 39:162168,
2004
20
American College of Sports Medicine: Joint
Position Statement: Nutrition and athletic perfor-
mance. Med Sci Sports Exerc 32:21302145,
2000
21
Jacobs KA, Sherman WM: The effect of carbo-
hydrate supplementation and chronic high-car-
bohydrate diets for improving endurance perfor-
mance. Int J Sport Nutr 9:92115, 1999
22
Sherman WM, Doyle JA, Lamb DR, Strauss
RH: Dietary carbohydrate, muscle glycogen, and
exercise performance during seven days of train-
ing. Am J Clin Nutr 62 (Suppl.):228S241S,
1993
23
American Diabetes Association: Nutrition prin-
ciples and recommendations in diabetes (Position
Statement). Diabetes Care 27 (Suppl. 1):S36
S46, 2004
24
Eisenstein J, Roberts SB, Dallal G, Saltzman E:
High protein weight-loss diets: are they safe and
do they work? A review of the experimental and
epidemiologic data. Nutr Rev 60:189200, 2002
25
Chetlin RD, Hornsby WG: Strength training
and nutritional supplements. In The Health
Professionals Guide to Diabetes and Exercise.
Ruderman N, Devlin JT, Eds. Alexandria, Va.,
American Diabetes Association, 1995, p.
625638
26
Silver MD: Use of ergogenic aids by athletes. J
Am Acad Orthop Surg 9:6170, 2001
27
Bhasin S, Storer TW, Berman N, Callegari C,
Clevenger B, Phillips J, Bunnell TJ, Tricker R,
Shirazi A, Casaburi R: The effects of supaphysio-
logic doses of testosterone on muscle size and
strength in normal men. N Engl J Med 335:52
53, 1996
28
Scroeder ET, Terk M, Sattler FR: Androgen
therapy improves muscle mass and strength but
not muscle quality: results from two studies. Am
J Physiol Endocrinol Metab 285:E16E24, 2003
29
Dorchy H, Poortmans J: Sport and the diabetic
child. Sports Med 7:248262, 1989
30
Fahey PJ, Stallkamp ET, Kwatra S: The athlete
with diabetes: managing insulin, diet, and exer-
cise. Am Fam Phys 53:16111617, 1996
31
Greenhalgh PM: Competitve sport and the
insulin-dependent diabetic patient. Postgrad Med
J 66:803806, 1990
32
Hough DO: Diabetes mellitus in sports. Med
Clin North Am78:423437, 1994
33
Thurm U, Harper PN: Im running on insulin:
summary of the history of the International
Diabetic Athletes Association. Diabetes Care
15:18111813, 1992
34
Sane T, Helve E, Pelkonen R, Koivisto VA: The
adjustment of diet and insulin dose during long-
term endurance exercise in type 1 (insulin-depen-
dent) diabetic men. Diabetologia 31:35 40,
1988
35
Ebeling P, Tuominen JA, Bourey R, Koranyi L,
Koivisto VA: Athletes with IDDM exhibit
impaired metabolic control and increased lipid
utilization with no increase insulin sensitivity.
Diabetes 44:471477, 1995
36
Gregory RP, Boswell EJ, Crofford OB:
Nutrition management of a collegiate football
player with insulin-dependent diabetes: guide-
lines and a case study. J Am Diet Assoc
94:775777, 1994
37
The DCCT Research Group: The effect of
intensive treatment on the development and pro-
gression of long-term complications in insulin-
dependent diabetes mellitus. N Engl J Med
329:977986, 1993
38
Shah BR, Hux JE: Quantifying the risk of infec-
tious disease for people with diabetes. Diabetes
Care 26:510513, 2003
W. Guyton Hornsby, Jr., PhD, CDE,
is an associate professor of exercise
physiology and associate chair of the
Division of Exercise Physiology, and
Robert D. Chetlin, PhD, CSCS, is an
assistant professor of occupational
therapy in the Department of Human
Performance and Applied Exercise
Science at the School of Medicine of
West Virginia University in
Morgantown.
Você também pode gostar
- Chapter II Review of Related Literature and StudiesDocumento2 páginasChapter II Review of Related Literature and StudiesAnthone Manjeron70% (33)
- Sports NutritionDocumento11 páginasSports Nutritionacads stuffAinda não há avaliações
- Final Written EssayDocumento15 páginasFinal Written Essayswimmercass35Ainda não há avaliações
- Nutrition and Hydration Issues For Combat Sport Athletes (Hoffman J.R.) (2011)Documento9 páginasNutrition and Hydration Issues For Combat Sport Athletes (Hoffman J.R.) (2011)AnaAinda não há avaliações
- Train Low Race HighDocumento11 páginasTrain Low Race HighVasco PintadoAinda não há avaliações
- T1DM and ExerciseDocumento9 páginasT1DM and ExerciserobertjoshuasantosAinda não há avaliações
- AJGP 0102 2020 Focus Desbrow Sports Nutrition Amateur Athletes WEBDocumento6 páginasAJGP 0102 2020 Focus Desbrow Sports Nutrition Amateur Athletes WEBIgor PavlovicAinda não há avaliações
- Nutrition For Endurance Sports: Marathon, Triathlon, and Road CyclingDocumento9 páginasNutrition For Endurance Sports: Marathon, Triathlon, and Road CyclingcakebakeshakeAinda não há avaliações
- Long QuizDocumento6 páginasLong QuizMae EsmadeAinda não há avaliações
- What Is The Optimal Composition of An Athlete's DietDocumento10 páginasWhat Is The Optimal Composition of An Athlete's Dietkriszty10Ainda não há avaliações
- Resources To Guide Exercise Specialists Managing Adults With DiabetesDocumento11 páginasResources To Guide Exercise Specialists Managing Adults With DiabetesArie AnggaAinda não há avaliações
- Resources To Guide Exercise Specialists Managing Adults With DiabetesDocumento13 páginasResources To Guide Exercise Specialists Managing Adults With Diabeteslaura valentina ochoa ordoñezAinda não há avaliações
- Benefits of Exercise in The Older PopDocumento11 páginasBenefits of Exercise in The Older PopRafael PortoAinda não há avaliações
- Prescription of Resistance Training For Healthy PopulationsDocumento12 páginasPrescription of Resistance Training For Healthy PopulationsChristine LeeAinda não há avaliações
- The Overtraining Syndrome NeuroDocumento11 páginasThe Overtraining Syndrome NeurodserraAinda não há avaliações
- The Essential Role of Exercise in The Management of Type 2 DiabetesDocumento11 páginasThe Essential Role of Exercise in The Management of Type 2 DiabetesRadu MaricicaAinda não há avaliações
- Exercise - Physical Activity in Individuals With Type 2 Diabet... - Medicine & Science in Sports & ExerciseDocumento51 páginasExercise - Physical Activity in Individuals With Type 2 Diabet... - Medicine & Science in Sports & ExerciseRicardo Arellano GarcíaAinda não há avaliações
- Sports NutritionDocumento10 páginasSports NutritionmihaelaAinda não há avaliações
- Alimentacion OxidantesDocumento12 páginasAlimentacion OxidantesAlejandro BecerraAinda não há avaliações
- Exercise For GeriatricsDocumento9 páginasExercise For GeriatricsP.Senthil SelvamAinda não há avaliações
- Diabetes and Physical ActivityDocumento6 páginasDiabetes and Physical ActivityFahmi Fauzi SugandiAinda não há avaliações
- Fasting and Recovery - BJSMDocumento9 páginasFasting and Recovery - BJSMElddingAinda não há avaliações
- 516 Physical Activity and Exercise and Diabetes MellitusDocumento5 páginas516 Physical Activity and Exercise and Diabetes MellituslaurentiaoktaviaAinda não há avaliações
- Sports Nutrition Thesis StatementDocumento8 páginasSports Nutrition Thesis StatementKayla Jones100% (1)
- IOC Nutrition ConsensusDocumento19 páginasIOC Nutrition Consensusdredogg9Ainda não há avaliações
- Nutrition and Hydration For HandballDocumento23 páginasNutrition and Hydration For HandballGiorgianaAinda não há avaliações
- The Use of Dietary Supplements by AthletesDocumento18 páginasThe Use of Dietary Supplements by AthletesSamMKSAinda não há avaliações
- Nutrition For Endurance Sports Marathon, Triathlon, PDFDocumento10 páginasNutrition For Endurance Sports Marathon, Triathlon, PDFSheilla ElfiraAinda não há avaliações
- Physical Activity, Sport, and Pediatric Diabetes: Review ArticleDocumento11 páginasPhysical Activity, Sport, and Pediatric Diabetes: Review ArticleNicole GreeneAinda não há avaliações
- Sports Nutritionfroryoung AthletesDocumento6 páginasSports Nutritionfroryoung Athletesgaming indoAinda não há avaliações
- FULL - Dietary Protein For Athletes From Requirements To Optimum AdaptationDocumento11 páginasFULL - Dietary Protein For Athletes From Requirements To Optimum AdaptationmamithemadAinda não há avaliações
- Nutrition in Combat Sports PDFDocumento13 páginasNutrition in Combat Sports PDFJuan David Velez Arredondo100% (1)
- FCB-GSSI Sports Nutrition Guide - English v1 16.4.v1430213934 PDFDocumento88 páginasFCB-GSSI Sports Nutrition Guide - English v1 16.4.v1430213934 PDFpredragbozicAinda não há avaliações
- Develop Med Child Neuro - 2016 - Verschuren - Exercise and Physical Activity Recommendations For People With Cerebral PalsyDocumento11 páginasDevelop Med Child Neuro - 2016 - Verschuren - Exercise and Physical Activity Recommendations For People With Cerebral PalsyCláudia SilvaAinda não há avaliações
- Effectiveness and Safety of High-Intensity Interval Training in Patients With Type 2 DiabetesDocumento6 páginasEffectiveness and Safety of High-Intensity Interval Training in Patients With Type 2 DiabetesMumtaz Maulana HidayatAinda não há avaliações
- InglesDocumento6 páginasInglesKuroKy KrausserAinda não há avaliações
- Exercício Físico e Autofagia Seletiva Benefício e Risco Na Saúde CardiovascularDocumento18 páginasExercício Físico e Autofagia Seletiva Benefício e Risco Na Saúde CardiovascularHenrique WilliamAinda não há avaliações
- Ishrana Sportista: Sports NutritionDocumento7 páginasIshrana Sportista: Sports NutritionComikvAinda não há avaliações
- 3 Special PopulationDocumento57 páginas3 Special Populationfaariyaabdullah03Ainda não há avaliações
- Lactic Acid On AthleteDocumento4 páginasLactic Acid On AthleteSafira NugrohoAinda não há avaliações
- Antioxidants and Exercise Performance: With A Focus On Vitamin E and C SupplementationDocumento26 páginasAntioxidants and Exercise Performance: With A Focus On Vitamin E and C SupplementationkarinaAinda não há avaliações
- Contemporary Nutrition Interventions To Optimize Performance in Middle-Distance RunnersDocumento11 páginasContemporary Nutrition Interventions To Optimize Performance in Middle-Distance RunnersAdri MunizAinda não há avaliações
- Carboidrato No Contexto Do Exercício Físico em Diabéticos Tipo 1Documento21 páginasCarboidrato No Contexto Do Exercício Físico em Diabéticos Tipo 1Duda FranchiAinda não há avaliações
- The Importance of Exercise For Glycemic Control in Type 2 DiabetesDocumento10 páginasThe Importance of Exercise For Glycemic Control in Type 2 DiabetesAhmed AmerAinda não há avaliações
- Diet and TherapyDocumento3 páginasDiet and TherapyKatty AlevonAinda não há avaliações
- 10 1016@j Mcna 2019 10 003Documento10 páginas10 1016@j Mcna 2019 10 003Arnold BarraAinda não há avaliações
- Strength Training For KidsDocumento8 páginasStrength Training For KidsMike HaughtAinda não há avaliações
- 5.energy RequirementsDocumento14 páginas5.energy RequirementsAlejandro EVAinda não há avaliações
- 2.0 Introduction To Exercise Physiology SPS135Documento53 páginas2.0 Introduction To Exercise Physiology SPS135MUHAMMAD ARIF BIN MOHAMAD NOOR AZMANAinda não há avaliações
- Impact of Resistance Circuit Training On Neuromuscular, Cardiorespiratory and Body Composition Adaptations in The ElderlyDocumento8 páginasImpact of Resistance Circuit Training On Neuromuscular, Cardiorespiratory and Body Composition Adaptations in The ElderlyBryan HuaritaAinda não há avaliações
- University of Education, Winneba: Department of Health, Physical Education, Recreation and SportsDocumento11 páginasUniversity of Education, Winneba: Department of Health, Physical Education, Recreation and SportsNinfaazuma BenedictAinda não há avaliações
- Effects of A Ketogenic Diet On Muscle Fatigue in Healthy, Young, Normal-Weight Women A Randomized Controlled Feeding TrialDocumento15 páginasEffects of A Ketogenic Diet On Muscle Fatigue in Healthy, Young, Normal-Weight Women A Randomized Controlled Feeding TrialRubinhoAinda não há avaliações
- Fitness 2 and 3 - NewDocumento46 páginasFitness 2 and 3 - NewFikeduAinda não há avaliações
- Principles of Nutrition in Sports Training and Health TrainingDocumento11 páginasPrinciples of Nutrition in Sports Training and Health TrainingIsmail DzaficAinda não há avaliações
- Treinamento Dinâmico e de Força e Melhora Da Saúde Cardiovascular em ObesosDocumento11 páginasTreinamento Dinâmico e de Força e Melhora Da Saúde Cardiovascular em ObesosDinho MengoAinda não há avaliações
- Nutritional Strategies To Optimize Training and RaDocumento21 páginasNutritional Strategies To Optimize Training and RaHArsh AroraAinda não há avaliações
- Exercise PhysiologyDocumento50 páginasExercise Physiologymohamed.sewaAinda não há avaliações
- High-Intensity Interval Training: A Time-Efficient Strategy For Health Promotion?Documento3 páginasHigh-Intensity Interval Training: A Time-Efficient Strategy For Health Promotion?neilh39Ainda não há avaliações
- 12 MythsInSportsDocumento20 páginas12 MythsInSportsAlejandro EVAinda não há avaliações
- Kraemer Et Al. 2002 - Resistance Training For Health and PerformanceDocumento7 páginasKraemer Et Al. 2002 - Resistance Training For Health and PerformanceSakip HirrimAinda não há avaliações
- NCM-112-RESP (Sanaani, Nur-Fatima, M.) (Drug Study)Documento2 páginasNCM-112-RESP (Sanaani, Nur-Fatima, M.) (Drug Study)Nur SetsuAinda não há avaliações
- FLUOROURACIL Drug StudyDocumento8 páginasFLUOROURACIL Drug StudyAlexandrea MayAinda não há avaliações
- Common Spinal Disorders Explained PDFDocumento2 páginasCommon Spinal Disorders Explained PDFTamekaAinda não há avaliações
- A Heavy Burden On Young Minds The Global Burden of Mental and Substance Use Disorders in Children and YouthDocumento13 páginasA Heavy Burden On Young Minds The Global Burden of Mental and Substance Use Disorders in Children and YouthNatasha AlbaShakiraAinda não há avaliações
- Spanish 4 Midyear Exam Study GuideDocumento5 páginasSpanish 4 Midyear Exam Study GuidelevanshhsAinda não há avaliações
- Vaccines For COVID-19 - The Current State of Play PDFDocumento8 páginasVaccines For COVID-19 - The Current State of Play PDFdiana.alyAinda não há avaliações
- Drug Data For TomDocumento2 páginasDrug Data For TomAbdelmar SusulanAinda não há avaliações
- Skew Deviation RevisitedDocumento24 páginasSkew Deviation RevisitedPriscila Verduzco MartínezAinda não há avaliações
- Alternative ModalitiesDocumento16 páginasAlternative Modalitiesmariet abraham100% (3)
- Report of The Sixth Annual Meeting of The London Mesmeric Infirmary (1855)Documento48 páginasReport of The Sixth Annual Meeting of The London Mesmeric Infirmary (1855)marcinlesniewiczAinda não há avaliações
- Afriwardi: Bagian Fisiologi Fakultas Kedokteran Universitas Andalas PadangDocumento35 páginasAfriwardi: Bagian Fisiologi Fakultas Kedokteran Universitas Andalas PadangAlvin ArifAinda não há avaliações
- Nursing Management of PatientDocumento30 páginasNursing Management of PatientShreyas WalvekarAinda não há avaliações
- Getweightloss in Intragastric BalloonDocumento2 páginasGetweightloss in Intragastric Balloongetweightloss2023Ainda não há avaliações
- Lyme Disease Symptoms ChecklistDocumento5 páginasLyme Disease Symptoms ChecklistElek TesztAinda não há avaliações
- B1. CHN Care of Normal and at Risk Families CommunitiesDocumento28 páginasB1. CHN Care of Normal and at Risk Families CommunitiesMarco RapadasAinda não há avaliações
- Activity Intolerance NCPDocumento3 páginasActivity Intolerance NCPGen RodriguezAinda não há avaliações
- HypocalcemiaDocumento23 páginasHypocalcemiarayrrn00Ainda não há avaliações
- Health Benefits of Yoga For Kids Sylwia JonesDocumento15 páginasHealth Benefits of Yoga For Kids Sylwia JonesAlfonso BpAinda não há avaliações
- Poster-SessionsDocumento105 páginasPoster-SessionsjishnuAinda não há avaliações
- Drug StudyDocumento8 páginasDrug StudyStephanie Zafico PalalayAinda não há avaliações
- HistoryDocumento15 páginasHistoryDanica Mae PepitoAinda não há avaliações
- Mentally Retarded Children-IDocumento35 páginasMentally Retarded Children-Iqaiser khanAinda não há avaliações
- Drugs Affecting The Central Nervous SystemDocumento22 páginasDrugs Affecting The Central Nervous Systemአብይ በላይነሽ ጥላሁንAinda não há avaliações
- Parkinson DiseaseDocumento10 páginasParkinson DiseaseparthibaneAinda não há avaliações
- Angina PectorisDocumento17 páginasAngina PectorisRakesh Reddy100% (1)
- Valvular Heart Disease: Bekele T. (MD)Documento47 páginasValvular Heart Disease: Bekele T. (MD)alehegn beleteAinda não há avaliações
- Sample History and Physical ExaminationDocumento7 páginasSample History and Physical Examinationricksaha23100% (1)
- Leave Application FormDocumento1 páginaLeave Application FormsalescoordinatorAinda não há avaliações
- Brochure in Health Ed PDFDocumento3 páginasBrochure in Health Ed PDFHannalene DolorAinda não há avaliações