Escolar Documentos
Profissional Documentos
Cultura Documentos
Git 20
Enviado por
Patrick RamosDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Git 20
Enviado por
Patrick RamosDireitos autorais:
Formatos disponíveis
7.20. Jaundice (D.
Maasova) 547
the process of the break down of proteins by intesti-
nal bacteria. Further factors co-acting in the de-
velopment of encephalopathy are mercaptanes, free
fatty acids, intestinal endotoxins, activation of the
inhibitory neurotransmitter system GABA and as-
sumedly also the accumulation of false neurotrans-
mitters (octopamine).
Acute onset of PSE, e.g. in cirrhosis in a stable
state, has a predominantly apparent inducing cause.
Most frequently it involves bleeding into GIT which
is a massive source of nitrogen substances absorbed
in the intestine. A similar situation is developed due
to a diet rich in proteins. The disturbances of elec-
trolyte balance can signicantly contribute to the
development of PSE. Foremostly the hypokalemic
metabolic alkalosis, but also the metabolic alkalosis
alone increases the NH
3
: NH
4
ratio. Hypokalemia,
often caused by intensive diuretic therapy, stimulates
the renal production of ammonia. Further inducing
factors include the drugs which aect the CNS func-
tions, hypoxia and acute infections, assumedly by
means of the protein-catabolic eect.
PSE is manifestant by a wide range of distur-
bances of conciousness frominconspicuous changes in
behaviour through marked confusion to heavy coma.
These disturbances can be accompanied by neuro-
logical symptomatology, e.g. by non-specic changes
in EEG, rigidity, hyperreexia. A very characteris-
tical symptom is the coarse tremor of ngers, which
later develops into apping tremor (tremor of hands
from the wrist). The cause of the apping tremor is
considered to reside in a sudden intermitent inhibi-
tion of the motor tonus. Alterations in personality,
mood disturbancies, loss of social barriers, confusion,
inability to concentrate, apraxia and daytime somno-
lence are further symptoms of the amount of clinical
symptoms of the hepatic encephalopathy.
7.19.9 Hepatorenal syndrome
Hepatorenal syndrome signies renal insuciency in
the patients with a severe impairment of the liver,
whereas the kidneys do not display any morpholog-
ical cause of this state. This denition involves nei-
ther simultaneous impairments of both organs, nor
the cases of cirrhosis during which the circulatory
collapse has brought about acute tubular necrosis
with subsequent renal failure.
The renal functions promptly improve after the
recovery of liver functions. The development of the
syndrome is typically heralded by oliguria, associ-
ated with the increase of urea and creatinine con-
centration in the blood. Pathophysiology of the renal
failure remains unclear. The decrease in glomerular
ltration and in elimination of sodium are evident.
There are hints that the pathogenetic cause can re-
side in the disbalance of metabolites of the arachi-
donic acid.
In acute hepatic failure or advanced chronic liver
disease the renal insuciency can quickly progress to
death.
7.20 Jaundice
Jaundice (icterus) signies a yellow colouring of
sclerae, skin and mucosae determined by accumula-
tion of the bile pigment bilirubin. Jaundice devel-
ops in pathological states of various etiology. They
are commonly characteristic by the disbalance be-
tween the production and excretion of bilirubin.
Physiological level of the total bilirubin in the plasma
of adults is 321mol/l. When the concentration
in the plasma increases c. three-fold, bilirubin inl-
trates the tissues. It accumulates predominantly in
the tissues with high contents of elastine, to which it
has a signicant anity, but penetrates also into the
somatic uid with high contents of proteins (e.g. ex-
udate). The accumulation of bilirubin in organism
takes place due to:
1. increased production of bilirubin prehepatic
jaundice,
2. hepatic impairment, providing the hepatocytes
are not normally able to take up, conjugate,
or secrete bilirubin, or bile, or if bile stagnates
within the liver on the level of minute bile ducts
intrahepatic jaundice,
3. reduction or stopping of the drainage of bile due
to mechanical obstruction in extrahepatic bile
pathways posthepatic jaundice.
548 Chapter 7. Pathophysiology of the gastrointestinal tract ( I. Huln, I.
Duris et al.)
7.20.0.1 Prehepatic jaundice
This group includes the impairments which develop
by an excessive production of bilirubin. If the supply
of bilirubin excceds the maximal conjugation capac-
ity of the liver, it accumulates in the blood (hyper-
bilirubinaemia). Overproduction of bilirubin takes
place due to:
increased haemolysis (hereditary or acquired
haemolytic anaemias, posttransfusion haemoly-
tic reaction),
resorption of excessive haematomas (injury,
catheterisation, rupture of vascular aneurysm)
or excessive infarction (pulmonary infarction),
ineective erythropoiesis, when the produced
haemoglobin is not eective in peripheral tissues
and has been broken down already in the bone
marrow. This group referred to as shunt hyper-
bilirubinaemia, includes megaloblastic anaemia
caused by the deciency of the intrinsic fac-
tor (pernicious anaemia, resection of stomach,
polyposis of the stomach) or deciency of folic
acid and vitamin B
12
(resection of the terminal
ileum, blind intestinal loop, intestinal diverticu-
losis, fuctional intestinal impairments). A pro-
nounced jaundice in this group of hyperbilirubi-
naemia is rare.
Prehepatic jaundice is characterized by an in-
creased level of non-conjugated bilirubin in the
blood. As the liver takes up and degradates the
high amount of pigment, the bile and stools are
dark (pleiochromic bile, hypercholic stool). Uro-
bilinogen produced and absorbed in the intestine in
an increased amount is not taken up by overloaded
hepatocytes and it appears in urine. Also in se-
vere anaemia, when complicated by e.g. hypoxaemia,
fever or vascular collapse, the liver ability to elimi-
nate bilirubin decreases.
7.20.0.2 Intrahepatic jaundice
Due to didactic purposes it is wise to divide intra-
hepatic jaundice into groups according to the site of
the most marked disturbance taking place during the
metabolism and transport of bilirubin.
1. Disturbances of bilirubin uptake
The Gilberts syndrome (icterus iuvenilis inter-
mittens) is characterized as a functional impair-
ment of the transport of organic anions in hepato-
cytes. This dominantly hereditary disease resides in
the decrease of bilirubin uptake, assumedly due to
a decreased binding capacity of the transport pro-
tein (ligandin). At the same time the process of
conjugation is hindered due to the defect of UDP-
glucuronosyltransferase (so called infantile conjuga-
tion system). This moderate hereditary disturbance
is manifestant usually as late as in the second decade
of life. A permanently subicteric patient develops a
pronounced jaundice usually only due to stress (in-
tercurrent infection, physical exercise, fasting, alco-
hol).
Transient non-conjugated hyperbilirubinaemia
which develops after administration of drugs (certain
tetracyclines), x-ray contrast substances, pigments
(bromsulphthalein) is explained by a competitive in-
hibition of the ligandin. This mechanism assumedly
evokes also a moderate hyperbilirubinaemia in coin-
cidence with fasting, when the produced metabolites
compete with bilirubin in binding to ligandin.
2. Impairments of bilirubin conjugation
Impairments of bilirubin conjugation develop due
to absolute or relative insuciency of UDP-
glucuronosyl transferase (UDP-GT). An impairment
of bilirubin conjugation most frequently occurs in
newborns in whom it is already possible to nd sev-
eral dierences:
conjugation system during the intrauterine de-
velopment of the foetus matures already in the
tenth lunar months and closely after birth it is
still relatively incapable of increasing its activ-
ity appropriately. Ligandin is similarly imma-
ture.
in this period the foetal haemoglobin is broken
down implying an increased bilirubin supply
binding capacity of serum albumin to bilirubin
is lower,
the blood-brain barrier is still not suciently
mature which enables the entrance of bilirubin
into CNS
The above mentioned facts imply that the pres-
ence of jaundice in 50% of healthy newborns is not
7.20. Jaundice (D. Maasova) 549
considered to be a pathological state (physiological
jaundice of the newborn). It supervenes on the sec-
ond or third day after birth, and in consequence of
a rapid increase in the conjugation capacity it dis-
appears up to six days. The level of unconjugated
bilirubin in the blood is on the upper limits of the
physiological standard for newborn (130mol/l).
In the premature infant, the glucuronosyltrans-
ferase activity is less, and the neonatal jaundice may
be more pronounced. It supervenes also on the sec-
ond or third day, but fades away slower in accordance
with the process of maturing of the conjugation sys-
tem. The most dicult cases can yield an increase
in bilirubin above the critical value of 340mol/l.
Such values indicate that unconjugated bilirubin is
apt to enter CNS. The deposition of bilirubin in
the basal ganglia rich in lipids leads to the develop-
ment of bilirubin encephalopathy (kernicterus). Ker-
nicterus is the most severe complication of unconju-
gated hyperbilirubinaemia. It is manifestant by in-
appetence, apathy, hypotonia, decreased tendon re-
exes, tonic spasms. If the infant survives, it usually
remains permanently handicapped (rigidity, chorea,
deafness for high tones, etc.). The danger of the de-
velopment of bilirubin encephalopathy in newborn
increases the presence of substances in the blood
which compete with the unconjugated bilirubin in
its bond to albumin (organic anions in acidosis, sal-
icylates, sulphonamides, some antibiotics). In such
a case the proportion of the free fraction of the un-
conjugated bilirubin is higher, and can lead to the
entrance of pigment into CNS already at values of
total bilirubin being 150200mol/l.
Some substances of steroid nature can cause a
transient inhibition of UDP-GT, assumedly by com-
petition. A typical representation of this dis-
turbance is familial neonatal hyperbilirubinaemia
(Lucey-Priscoll syndrome). Essentially it is a tran-
sient inhibition of UDP-GT by steroid factor, present
in the maternal serum. Jaundice appears already af-
ter birth.
In some breast-fed infants, jaundice has been as-
cribed to the presence in breast milk of pregnane
3beta, 20alpha-diol, an inhibitor of glucuronosyl-
transferase. Jaundice supervenes later, and persists
for more than three weeks. When the infant is re-
moved ved from the breast, the breast-milk jaun-
dice subsides.
Hypothyreoidism delays the normal maturation of
UDP-GT and the neonatal jaundice can be prolonged
for weeks or months.
Crigler-Najjar syndrome is an especially severe
congenital disease. It occurs in two forms:
Type I, originally described by Crigler and Naj-
jar is an autosomally recessive disease caused by
the absence of the genetic equipment for UDP-
GT. The unconjugated bilirubin exceeds 1520-
fold its normal values and if therapy is not ap-
plied immediately, the child dies due to the con-
sequences of the bilirubin encephalopathy.
Type II is an autosomally dominant form with
a moderate clinical course. It involves a par-
tial deciency of UDP-GT. In comparison with
form I it ussually does not occur in newborns,
but in adolescents and adults. Therefore the
neurologic complications are uncommon. The
bile contains a variable amount of conjugated
bilirubin with a signicant increase in monocon-
jugates.
All types of jaundice of this group show an in-
creased level of unconjugated bilirubin in the blood.
3. Impairments of elimination through the
canalicular membrane
A. Isolated impairments in bilirubin secretion
Dubin-Johnson syndrome is a genetically deter-
mined disorder of the excretion of the conjugated
bilirubin and other organic anions (e.g. bromsulph-
thalein) from hepatocytes into bile. The impairment
resides in the transport systems on the canalicular
membrane of the cell. The disease is characterized
by chronic jaundice caused by an increased level of
the conjugated bilirubin in the blood. In the liver
the striking feature is the presence of a dark brown
pigment in the hepatocytes localised centrilobullarly
(so-called black liver). Patient with Dubin-Johnson
syndrome may be asymptomatic with the exception
of jaundice. Despite the icteric colouring, the patient
does not suer from pruritus, hence already the clin-
ical picture gives the hint of isolated impairment of
the excretion of pigment.
Rotor syndrome in many aspects resembles the
Dubin-Johnson syndrome, however the brown pig-
ment is not present in hepatocytes. This rare dis-
ease is inherited as an autosomal recessive trait
and is genetically distinct from the Dubin-Johnson
550 Chapter 7. Pathophysiology of the gastrointestinal tract ( I. Huln, I.
Duris et al.)
syndrome. The presented functional hyperbilirubi-
naemias (Gilbert, Dubin-Johnson, as well as Rotor
syndrome) have the attribute of being benign. Even
a long-term observation of patients with these im-
pairments (15 and more years) has not revealed any
signs of hepatic damage.
B. Impairment of bile secretion (intrahepatic
functional cholestasis)
This disease includes an extensive group of patho-
logical states which are characterized by a de-
creased, or blocked transport of all components of
bile through the canalicular membrane. The canalic-
ular membrane is energetically very demanding and
therefore also the most vulnerable site of the hepa-
tocyte. The functional impairment of bile elimina-
tion comes into consideration in all states leading to
hepatocyte injury. The conjugation processes do not
have to be damaged for a length of time and the
impairment supervenes in the later phases of cellu-
lar damage. The components of bile stagnate before
the canalicular membrane and regurgitate into the
blood. This type of cholestasis occurs in:
all types of hepatitis (viral, alcoholic, drug-
induced, toxic, non-specic)
cirrhosis (postinfectious, congestive)
focal lesions of the liver (toxoplasmosis, malaria,
etc.)
The listed impairments of the liver are not char-
acterized only by jaundice, but (and furthermore)
by a wide scale of manifestations of functional hep-
atic impairment from moderate dyspepsia to hepatic
coma. The decrease or even absence of bile acids in
the intestine results in an disturbance in the resorp-
tion of fat and vitamins. The deciency in vitamin K
is manifestant by a coagulopathy which is enhanced
also by the inability of the damaged hepatocytes to
synthesize prothrombin suciently. Since the excre-
tory step is the one which is rate-limiting and most
readily aected by injury, signicant amounts of con-
jugated bilirubin and bile acids reenter the systemic
circulation. Later also the conjugation process be-
comes retarded. The cause can reside in the profound
impairment of cells and/or feedback suppression of
the activity of UDP-GT by the accumulated conju-
gated bilirubin in hepatocytes. The laboratory ex-
aminations reveal an increase in both forms of biliru-
bin in the blood, and that of conjugated bilirubin
in urine. Stool is hypocholic or completely acholic.
Urobilinogen in urine is present only if the stasis of
bile is not total. In case of total stasis, the reappear-
ance of urobilinogen in urine is a good sign of the
recovery of bile ow.
4. Intrahepatic mechanic cholestasis
The cause of this type of intrahepatic cholesta-
sis is an impairment at the level of the minute bile
ducts canaliculi and ductuli. Under the inuence
of pathological reactions their lumen becomes narrow
by hypersensitive reaction in their walls and periduc-
tal oedema or cellular reaction in their surround-
ing. This mechanic obstacle of bile ow consequently
brings about bile stagnation and condensation lead-
ing to the formation of bile plug.
Intrahepatic cholestasis of pregnancy (reccurrent
jaundice of pregnancy) appears in a small percentage
of pregnant women usually in the last trimester but
may develope any time after the seventh week of ges-
tation. It is assumed that in these women an abnor-
mal metabolism of oestrogens produces a cholestati-
cally eective metabolites. Jaundice often reappears
not only in subsequent pregnancies, but also after
contraceptives. This fact suggests an equal, or simi-
lar mechanism of cholestasis development. The clin-
ical features consist primarily of pruritus and jaun-
dice. Pruritus is explained by retention of bile salts
while the decisive factor resides in the local increase
in concentration of bile salts in the skin. These symp-
toms of cholestasis quickly fade out after parturition.
Drug-induced cholestasis may occur in some pa-
tients following the use of oral contraceptives (oe-
strogens), anabolic steroids and drugs, e.g. chlor-
promazine. In contrast to cholestasis after oestro-
gens, the cholestasis after administration of anabolic
steroids can transgress to chronicity. Chlorpro-
mazine is a typical example for the development of
idiosyncratic reaction. In about 1% of patients re-
ceiving chlorpromazine, intrahepatic cholestasis with
jaundice develops after 5 weeks of treatment. It is as-
sumed that the metabolisation of the drug results in
free radicals which on the sensitive terrain change the
structure of minute biliary ducts. The walls become
antigenic, which is the cause of the development of
local immune reaction. The development of the id-
iosyncratic reaction was anticipated on the grounds
of the presence of eosinophilia.
Cholestasis in the culminating phase of the vi-
ral hepatitis can be explained by the fact that the
7.20. Jaundice (D. Maasova) 551
functional impairment of the canalicular membrane
which is present in hepatitis, leads to the increase
in its permeability with the penetration of macro-
mulecules and condensation of bile. The dense bile
stagnates and irritates the adjacent structures thus
causing inammation and brosis. This condition
results in the narrowment of the ducts. Despite the
nal functional recovery of hepatocytes this mechan-
ical factor disables the free drainage of bile for a cer-
tain period.
Patients with intrahepatic mechanic cholestasis
usually present with signs and symptoms of cholesta-
sis, but without pronounced signs of hepatic damage
(with the exception of viral hepatitis).
7.20.0.3 Posthepatic jaundice (extrahepatic
biliary obstruction)
Posthepatic jaundice develops due to partial or total
obstruction of extrahepatic bile ducts. It most fre-
quently involves an obstructions of large bile ducts
(common bile duct and ductus hepaticus communis).
The functional reserve of the liver is large, and there-
fore partial enclosures result in jaundice only in cases
of obstructions taking place in a larger number of bil-
iary ducts (75% of draining ducts under experimen-
tal conditions). Mechanical obstacle can be caused
by an intraductal enclosure (stones, parasites, struc-
tures) or compression of the biliary ducts from the
outside (tumours, scars). A severe and long-lasting
obstacle of bile drainage damages the walls of biliary
ducts by a retrograde increase in the pressure of the
stagnating bile. This condition results in regurgita-
tion of bile. After the transgression of the pressure
in biliary ducts above 25 mmHg (3.1kPa), the su-
pervening condition then ranges from disturbances
to a complete failure of hepatocytes to secrete bile.
Later, the accumulation of bilirubin in hepatocytes
and high pressure negatively inuence also the pro-
cess of conjugation.
A total enclosure of biliary pathways is character-
ized by a pronounced icterus, generalized pruritus
and increased bleeding due to the deciency of vita-
min K. Stools are acholic and contain fat (steator-
rhea). Biochemical examinations reveal an increased
level of conjugated bilirubin, bile acids, cholesterol
and alkaline phosphatase in the blood and bilirubin
in urine. After a certain period, in accordance with
the suppression of the process of conjugation, also
the level of unconjugated bilirubin increases in the
blood. Total enclosures do not bring about urobilino-
gen in urine.
7.20.0.4 Postoperative jaundice
Owing to the performance of gradually more de-
manding surgical interventions, the problem of post-
operative jaundice appears in the centre of attention.
After so-called major surgical procedures, 17% of pa-
tients develop a moderate and 4% exhibit a strongly
pronounced jaundice. Pathogenic mechanisms par-
ticipating in the development of jaundice have their
foundations in the overproduction of bilirubin, hep-
atocellular damage and/or extrahepatic obstruction.
Overproduction of bilirubin is caused most fre-
quently by transfusion of stored blood. After the
transfusion, within 24 hours, approximately 10% of
the administered erythrocytes break down. That
means that 500 ml of blood provides c. 430mol
of bilirubin which a healthy liver eliminates with-
out any problems. Transfusions repeated closely
one after another transgress however the capacity of
the liver to eliminate bilirubin. The further source
of bilirubin resides in the resorption of the blood
from extravascular spaces. Rarely, e.g. in patients
with the glucoso-6-phosphate-dehydrogenase defect,
haemolytic anaemia occurs after anaesthesia, drugs,
or after surgical intervention per se.
Hepatocellular impairment varying in its degree
develops due to a number of causes. It can develop as
a reaction to the administered drugs or anaesthetics,
e.g. halotane. Repeated anaesthesia, in rare cases,
incur hepatitis which is put into association with the
hypersensitivity to halotane. Moderate reactions are
however more frequent, especially in obese patients
as fat-soluble halotan accumulates in the fat tissue
and slowly oats away. Hepatocellular necrosis may
follow profound shock. With lesser degrees of hy-
potension or hypoxaemia, signicant impairment of
hepatic function may occur. Renal impairment due
to hypotension and hypoxaemia may enhance the de-
gree of jaundice because the renal excretion of conju-
gated bilirubin is decreased. Sepsis as well can pro-
duce the impairment of hepatocytes and bring about
jaundice, often of a cholestatic type.
Extrahepatic obstruction may occur in conse-
quence of a surgical intervention in the abdominal
cavity.
Você também pode gostar
- Tourniquet TestingDocumento6 páginasTourniquet TestingPatrick RamosAinda não há avaliações
- Serum Surfactant Protein D Is Steroid Sensitive and Associated With Exacerbations of COPDDocumento8 páginasSerum Surfactant Protein D Is Steroid Sensitive and Associated With Exacerbations of COPDPatrick RamosAinda não há avaliações
- Assessmentof Fetal Lungmaturity:Lecithin/ Sphingomyelinratiovs. Cortisoland Foam-Test AssaysDocumento4 páginasAssessmentof Fetal Lungmaturity:Lecithin/ Sphingomyelinratiovs. Cortisoland Foam-Test AssaysPatrick RamosAinda não há avaliações
- 8699 36053 1 PBDocumento7 páginas8699 36053 1 PBPatrick RamosAinda não há avaliações
- Viral Hepatitis: Information For Gay/Bisexual MenDocumento2 páginasViral Hepatitis: Information For Gay/Bisexual MenPatrick RamosAinda não há avaliações
- Antenatal Steroids and The Developing Brain: Current TopicDocumento4 páginasAntenatal Steroids and The Developing Brain: Current TopicPatrick RamosAinda não há avaliações
- Hcca Rev Nri 2005Documento15 páginasHcca Rev Nri 2005Patrick RamosAinda não há avaliações
- Ni Hms 448407Documento14 páginasNi Hms 448407Patrick RamosAinda não há avaliações
- Abnormal Liver Function Tests in The Symptomatic Pregnant Patient: The Local Experience in SingaporeDocumento5 páginasAbnormal Liver Function Tests in The Symptomatic Pregnant Patient: The Local Experience in SingaporePatrick RamosAinda não há avaliações
- Jaqt 05 I 3 P 215Documento3 páginasJaqt 05 I 3 P 215Patrick RamosAinda não há avaliações
- ObGyn Handbook2011 2012Documento185 páginasObGyn Handbook2011 2012Patrick RamosAinda não há avaliações
- J. Biol. Chem.-1989-Boggaram-11421-7Documento7 páginasJ. Biol. Chem.-1989-Boggaram-11421-7Patrick RamosAinda não há avaliações
- Medical Faculty of Lampung UniversityDocumento10 páginasMedical Faculty of Lampung UniversityPatrick RamosAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Traditional Perceptions and Treatment of Mental Illness in EthiopiaDocumento7 páginasTraditional Perceptions and Treatment of Mental Illness in EthiopiaifriqiyahAinda não há avaliações
- Song Book Inner PagesDocumento140 páginasSong Book Inner PagesEliazer PetsonAinda não há avaliações
- Multinational MarketingDocumento11 páginasMultinational MarketingraghavelluruAinda não há avaliações
- A Comparative Study of Public Private Life Insurance Companies in IndiaDocumento5 páginasA Comparative Study of Public Private Life Insurance Companies in IndiaAkansha GoyalAinda não há avaliações
- VimDocumento258 páginasVimMichael BarsonAinda não há avaliações
- MFE Module 1 .Documento15 páginasMFE Module 1 .Adarsh KAinda não há avaliações
- GGG Sri MDocumento2 páginasGGG Sri MGiovanni LuigiAinda não há avaliações
- 3400 MD IomDocumento52 páginas3400 MD IomIhabAinda não há avaliações
- Case Study - Suprema CarsDocumento5 páginasCase Study - Suprema CarsALFONSO PATRICIO GUERRA CARVAJALAinda não há avaliações
- PDFDocumento3 páginasPDFAhmedraza123 NagdaAinda não há avaliações
- AISOY1 KiK User ManualDocumento28 páginasAISOY1 KiK User ManualLums TalyerAinda não há avaliações
- Simran's ResumeDocumento1 páginaSimran's ResumesimranAinda não há avaliações
- Jonathan Livingston Seagull - Richard Bach - (SAW000) PDFDocumento39 páginasJonathan Livingston Seagull - Richard Bach - (SAW000) PDFAdrià SonetAinda não há avaliações
- Invisible CitiesDocumento14 páginasInvisible Citiesvelveteeny0% (1)
- 0012 Mergers and Acquisitions Current Scenario andDocumento20 páginas0012 Mergers and Acquisitions Current Scenario andJuke LastAinda não há avaliações
- 19 Dark PPT TemplateDocumento15 páginas19 Dark PPT TemplateKurt W. DelleraAinda não há avaliações
- Dialectical Relationship Between Translation Theory and PracticeDocumento5 páginasDialectical Relationship Between Translation Theory and PracticeEverything Under the sunAinda não há avaliações
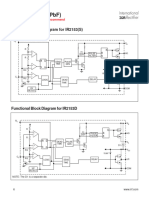
- IR2153 Parte6Documento1 páginaIR2153 Parte6FRANK NIELE DE OLIVEIRAAinda não há avaliações
- NHD Process PaperDocumento2 páginasNHD Process Paperapi-203024952100% (1)
- Importance of Skill Based Education-2994Documento5 páginasImportance of Skill Based Education-2994João Neto0% (1)
- Practice Problems - Electrochemical CellDocumento5 páginasPractice Problems - Electrochemical CellYehia IbrahimAinda não há avaliações
- John DrydenDocumento3 páginasJohn DrydenDunas SvetlanaAinda não há avaliações
- FMEA Minus The PainDocumento7 páginasFMEA Minus The PainMUNISAinda não há avaliações
- Combined South Dakota Motions To Reconsider in ICWA CaseDocumento53 páginasCombined South Dakota Motions To Reconsider in ICWA CaseLee StranahanAinda não há avaliações
- Sla At&tDocumento2 páginasSla At&tCésar Lainez Lozada TorattoAinda não há avaliações
- Session 1Documento18 páginasSession 1Akash GuptaAinda não há avaliações
- AIIMS 2015 Solved PaperDocumento436 páginasAIIMS 2015 Solved PaperSurya TejaAinda não há avaliações
- Origin ManualDocumento186 páginasOrigin ManualmariaAinda não há avaliações
- Test Bank For Psychology 6th Edition Don HockenburyDocumento18 páginasTest Bank For Psychology 6th Edition Don HockenburyKaitlynMorganarwp100% (42)
- Claim of FactDocumento11 páginasClaim of FactXeb UlritzAinda não há avaliações