Escolar Documentos
Profissional Documentos
Cultura Documentos
Cardiovascular Dysfunction in Parkinsonian Disorders: Christopher J. Mathias
Enviado por
ramadan0 notas0% acharam este documento útil (0 voto)
98 visualizações9 páginaskji
Título original
Article
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentokji
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
98 visualizações9 páginasCardiovascular Dysfunction in Parkinsonian Disorders: Christopher J. Mathias
Enviado por
ramadankji
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 9
INTRODUCTION
Parkinsonian disorders comprise a variety
of diseases, with differing pathology, natural
history and prognosis. Although the most com-
mon is idiopathic (classical) Parkinsons disease
(PD), there is increasing recognition of atypi-
cal parkinsonian disorders, such as multiple
system atrophy (MSA), progressive supranu-
clear palsy (PSP) and Lewy body disease
(LBD) (1) (Fig. 1, see over). In some parkinson-
ian patients, and in particular in MSA, autonom-
ic failure characterised by cardiovascular disturb-
ances is a prominent feature. However, the ma-
jority of patients with parkinsonism are over the
age of 50, when there is an increasing incidence
of cardiovascular disease; this may create diag-
nostic difficulties and also compound problems
with management. This review will focus on
cardiovascular autonomic dysfunction, especial-
ly in MSA, and will deal predominantly with
blood pressure and heart rate control together
with newer information on cardiac sympathetic
innervation in parkinsonian patients.
FUNCTIONAL NEUROLOGY (16)3 2001 257
CARDIOVASCULAR DYSFUNCTION IN PARKINSONIAN DISORDERS
Christopher J. Mathias
Neurovascular Medicine Unit, Division of Neuro-
science & Psychological Medicine, Imperial Col-
lege School of Medicine at St Marys and Auto-
nomic Unit, National Hospital for Neurology &
Neurosurgery, Queen Square/University Depart-
ment of Clinical Neurology, Institute of Neurology,
University College London, UK.
Reprint requests to: Prof. Christopher J. Mathias, Neurovas-
cular Medicine Unit, St Marys Hospital, Imperial C o l l e g e
Praed Street, London W2 1NY, UK.
E-mail: c.mathias@ic.ac.uk
Many environmental and occupational chemicals are
known to affect the central and/or peripheral nervous
system, causing changes that may result in neurologi-
cal and psychiatric disorders. Because of the limited
accessibility of the mammalian nervous tissue, new
strategies are being developed to identify biochemical
parameters of neuronal cell function, which can be
measured in easily obtained tissues, such as blood
cells, as potential markers of the chemically-induced
alterations occurring in the nervous system. This re-
view includes a comparative analysis of the effects of
mercurials on calcium signalling in the neuroadrener-
gic PC12 cells and rat splenic T lymphocytes in an at-
tempt to characterize this second messenger system as
a potential indicator of subclinical toxicity. The suit-
ability of neurotransmitter receptors in blood cells,
such as the sigma binding sites, as biological markers
of psychiatric disorders is also discussed.
KEY WORDS: Autonomic failure, Lewy body dis-
ease, multiple system atrophy, orthostatic hypotension,
Parkinsons disease, progressive supranuclear palsy.
FUNCT NEUROL 2001;16: 257-265
BLOOD PRESSURE ABNORMALITIES
Orthostatic hypotension
Orthostatic (postural) hypotension is a car-
dinal feature of autonomic failure [defined as a
fall in systolic blood pressure of at least 20
mmHg or in diastolic of at least 10 mmHg on
either standing or head-up tilt to at least 60
(2)]; in a patient with parkinsonism its pres-
ence often leads to consideration of MSA (Fig.
2) (3). The symptoms arising from orthostatic
hypotension result from hypoperfusion of vital
organs. Prominent are those from cerebral hy-
poperfusion, such as dizziness, visual disturb-
ances and sometimes impaired cognition,
which often precede loss of consciousness
( Table I); there is a variety of non-cerebral
symptoms (4,5). Symptoms vary substantially
between subjects and even in the same subject
in different situations and times of the day (Fig.
3, see p. 260). This is because many factors,
some relating to essential activities in daily
life, such as food ingestion and exercise, influ-
ence the degree of orthostatic hypotension
(Table II, see p. 260). Non-neurogenic factors,
which include the effect of drugs and condi-
tions resulting in fluid and volume depletion,
also exacerbate orthostatic hypotension (Fig. 4,
see p. 261) (6). Sometimes non-specific symp-
toms, such as weakness, letharg y, fatigue or
falls, may be the only features resulting from
orthostatic hypotension (Table I).
Evaluation of orthostatic hypotension is
n e c e s s a r y, both in the clinic and ideally in an au-
tonomic laboratory. Details have been described
elsewhere, together with methods to evaluate
neurogenic and non-neurogenic factors (3); this
C.J. Mathias
258 FUNCTIONAL NEUROLOGY (16)3 2001
MSA
Autonomic
Parkinsonian
Cerebellar/
Pyramidal
Dementia
P C M PD PD+AF PSP DLBD PAF
Fig. 1 - Schematic representation indicating the major clinical features in some of the parkinsonian disorders. These in-
clude the parkinsonian, cerebellar and mixed forms of multiple system atrophy (MSA-P, C & M respectively), idiopathic
Parkinsons disease (PD), PD with autonomic failure (PD+AF), progressive supranuclear palsy (PSP), diffuse Lewy
body disease (DLBD) and pure autonomic failure (PAF). (Adapted from ref. 1).
evaluation is important in parkinsonian disorders
where there may be many reasons for orthostatic
hypotension (Table III, see p. 261) (7,8).
In the majority of PD cases, symptomatic
orthostatic hypotension is not a major feature,
although its prevalence varies (9-12). In a rela-
tively rarer sub-group, with drug-responsive
PD, symptomatic orthostatic hypotension re-
sults from autonomic failure (PD+AF). In such
patients the autonomic lesion is thought to be
peripheral, as based on a combination of fea-
tures that include a low basal level of plasma
noradrenaline, and the inability of drugs such
as yohimbine (that act on pre-synaptic recep-
tors to activate sympathetic terminals) to raise
blood pressure (13,14). These observations are
in contrast to MSA where the lesions are pre-
dominantly central and pre-ganglionic (15,16);
in MSA basal levels of plasma noradrenaline
are often within the normal range and there is a
pressor response to drugs such as ephedrine,
whose activation is dependent on post-gan-
glionic sympathetic innervation (17). In PD,
there is a varying incidence of symptomatic
and asymptomatic orthostatic hypotension that
may reflect additional factors, ranging from the
influence of increasing age, to duration of the
FUNCTIONAL NEUROLOGY (16)3 2001 259
Cardiovascular dysfunction in Parkinsonian disorders
Fig. 2 - Blood pressure and heart rate before, during and
after head-up tilt in a normal subject (top panel), and a
patient with pure autonomic failure (lower panel). In the
normal subject there is no fall in blood pressure during
head-up tilt, unlike the patient in whom blood pressure
falls promptly and remains low with a blood pressure
overshoot on return to the horizontal. In the patient with
autonomic failure there is only a minimal change in heart
rate despite the marked blood pressure fall. In each case
continuous blood pressure and heart rate were recorded
with the Portapres II. (From ref. 3).
Table I - Some of the symptoms resulting from orthostatic
(postural) hypotension.
Cerebral hypoperfusion
Dizziness
Visual disturbances
blurred-tunnel
scotoma
greying out - blacking out
colour defects
Loss of consciousness
Impaired cognition
Muscle hypoperfusion
Paracervical and suboccipital (coathanger) ache
Lower back/buttock ache
Cardiac hypoperfusion
Angina pectoris
Spinal cord hypoperfusion
Renal hypoperfusion
Oliguria
Non-specific
Weakness, lethargy, fatigue
Falls
(Reproduced from Ref. 3)
Normal
Autonomic failure
45Head-up tilt
45Head-up tilt
2 mins
2 mins
200
0
200
0
200
0
200
0
disorder and drug therapy. Furthermore, in PD,
there may be dissociation between symptoms
and signs of orthostatic hypotension that may
occur, albeit occasionally, also in MSA (5).
In atypical parkinsonian disorders diff e r-
ences in autonomic function have been de-
scribed. In PSP, detailed physiological and neu-
ropharmacological studies indicate that ortho-
static hypotension and cardiovascular auto-
nomic failure do not constitute a feature (18).
This differs from LBD where orthostatic hy-
potension may be a presenting feature (19,20);
orthostatic hypotension has been reported in up
to 50% of such patients (21).
The management of orthostatic hypoten-
sion due to neurogenic failure should incorpo-
rate non-pharmacological approaches and
when needed the use of drugs (Table IV, see p.
262). The benefit of therapeutic strategies is
enhanced by knowledge of the putative site of
lesion and known mechanism of action of
drugs; thus with central lesions as in MSA,
ephedrine (an indirectly-acting sympath-
omimetic) is likely to be effective, unlike pe-
ripheral lesions (such as PD+AF) where mido-
drine (an -adrenoceptor agonist) is often
needed. Treatment should combine information
from clinical evaluation and appropriate auto-
nomic investigations (such as determining the
e ffect of food and exercise on orthostatic hy-
potension) to ensure that management is tai-
lored specifically to individual needs (22).
There may be differences in responses in the
C.J. Mathias
260 FUNCTIONAL NEUROLOGY (16)3 2001
F i g . 3 - Twenty-four hour non-invasive ambulatory blood
pressure profile showing systolic (- - - -) and diastolic
( ---- ) blood pressure and heart rate at intervals
through the day and night. (a) Changes in a normal sub-
ject with no postural fall in blood pressure; there was a
fall in blood pressure at night whilst asleep, with a rise in
blood pressure on wakening. (b) Marked fluctuations in a
patient with autonomic failure; the falls are usually the re-
sult of postural changes, either sitting or standing. Supine
blood pressure, particularly at night, is elevated. Getting
up to micturate causes a marked fall in blood pressure
(03.00 hours). There is a reversal of the diurnal changes
in blood pressure. There are relatively small changes in
heart rate, considering the marked changes in blood pres-
sure. (From ref. 3).
Table II - Factors influencing orthostatic (postural) hypo-
tension
Speed of positional change
Time of day (worse in the morning)
Warm environment (hot weather, central heating,
hot bath)
Raising intrathoracic pressure - micturition, defaecation
or coughing
Food and alcohol ingestion
Physical exertion
Manoeuvres and positions (bending forward, abdominal
compression, leg crossing, squatting, activating calf
muscle pump)*
Drugs with vasoactive properties (including dopaminergic
agents)
* These manoeuvres usually reduce the postural fall in blood
pressure, unlike the others (Reproduced from ref. 3)
various disorders; thus even the recent observa-
tion of the pressor response to oral water in
MSA and pure autonomic failure (PAF) (23,24)
does not appear to apply to PD +AF (25). Edu-
cation of the patient and, where relevant, of
family and care-givers is important, as is delin-
eation of treatment limitations and discussion
of realistic expectations, especially where the
motor deficits impair mobility and enhance
susceptibility to the fainting sequela.
Hypertension
The incidence of essential hypertension in-
creases with age. Its presence in parkinsonian
patients may reflect other factors. In MSA,
supine hypertension occurs despite severe or-
thostatic hypotension, probably because of
movement of intra- and extra-vascular fluid
from the peripheral to the central compartment
during postural change, in combination with
FUNCTIONAL NEUROLOGY (16)3 2001 261
Cardiovascular dysfunction in Parkinsonian disorders
F i g . 4 - The effect of a single standard oral dose of L-dopa (250 mg) and a dopadecarboxylase inhibitor, carbidopa (25 mg)
given at time zero on the blood pressure of a patient with parkinsonian features. There was a marked fall in blood pressure
after 30 min., resulting in the patient being first placed supine and then head-down. On investigation the patient had auto-
nomic failure with orthostatic hypotension unmasked by L-dopa; the final diagnosis was the parkinsonian form of multiple
system atrophy. SBP = systolic blood pressure; DBP = diastolic blood pressure; HR = heart rate. (From ref. 6).
Table III - Possible causes of orthostatic hypotension in a
patient with parkinsonian features
Side effects of anti-parkinsonian therapy, including:
L-dopa, bromocriptine, pergolide, the combination of
L-dopa and COMT inhibitors (tolcapone)
The MAO b inhibitor, selegiline
Coincidental disease causing autonomic dysfunction,
e.g. diabetes mellitus
Coincidental administration of drugs for an allied
condition
Antihypertensives
Alpha-adrenoceptor blockers (for benign prostatic
hypertrophy)
Vasodilators (for ischaemic heart disease)
Diuretics (for cardiac failure)
Multiple system atrophy (Shy-Drager syndrome)
Parkinsons disease with autonomic failure
Lewy body disease
(Adapted from ref.s 7 and 8)
Sitting Supine Head-down tilt
Time (min)
SBP
DBP
HR
impaired baroreflexes and pressor supersensi-
tivity to small amounts of circulating cate-
cholamines or pressor agents used for therapy.
Transient hypertension may occur even in nor-
motensive PD patients on L-dopa (26) and dur-
ing end-of-dose akinesia, being higher in the
o ff than the on phase (27). In PSP, pre-
symptomatic hypertension, mainly transient,
with large fluctuations in blood pressure has
been reported in 80% of patients and on neu-
roimaging, small vessel cerebral disease was
observed in 50% (28); whether this is due to
involvement of brain stem autonomic nuclei or
other factors is unclear.
HEART RATE ABNORMALITIES
Impairment of parasympathetic heart rate
control in response to various respiratory stimu-
li is common in MSA. Abnormalities of heart
rate variability have also been reported in PD,
although it is unclear whether this is a reflec-
tion of disease duration, age, drug therapy or a
parasympathetic cardiac deficit. In PSP, the
small differences in heart rate responses to var-
ious tests (29,30), which were attributed to
central autonomic involvement, have not been
confirmed in a larger study (18).
Cardiac arrhythmias have been reported in
parkinsonian patients and may result from fac-
tors that include age, the effect of drugs, or an
intrinsic propensity to the development of ar-
rhythmias. A prolonged Q-T interval may iden-
tify patients at risk of developing ventricular
fibrillation and sudden cardiac death. In MSA
the Q-T interval is prolonged but Q-T disper-
sion, which may provide a better measure of
tendency to arrhythmias, is unaffected (31).
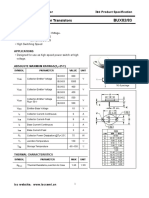
Studies on cardiac sympathetic innervation
in parkinsonian patients have revealed unex-
pected differences. These studies include use of
1 2 3
meta-idobenzylguanadine (I-MIBG), which
is dependent on active transport into sympa-
thetic nerve terminals by a noradrenaline trans-
porter; gamma scintiscanning of heart and me-
diastinum provide a measure of cardiac uptake
and thus sympathetic innervation. In MSA with
a pre-ganglionic lesion, such transport is pre-
served, with results similar to those seen in
normal subjects; this is in contrast to PD,
where there is impaired uptake, even in pa-
tients without autonomic failure, suggesting
cardiac sympathetic denervation or dysfunction
C.J. Mathias
262 FUNCTIONAL NEUROLOGY (16)3 2001
Table IV - Outline of non-pharmacological and pharma-
cological measures used in the management of postural
hypotension due to neurogenic failure.
To be avoided
Sudden head-up postural change (especially on
waking)
Prolonged recumbency
Straining during micturition and defaecation
High environmental temperature (including hot baths)
Severe exertion
Large meals (especially when these contain refined
carbohydrate)
Alcohol
Drugs with vasodepressor properties
To be introduced
Head-up tilt during sleep
Small, frequent meals
High salt intake
Increased water intake
Sensible/moderate exercise (including swimming)
Body positions and maneouvres
To be considered
Elastic stockings
Abdominal binders
Pharmacological measures
Starter drug: fludrocortisone
Sympathomimetics: ephedrine, midodrine
Specific targeting: octreotide, desmopressin,
erythropoietin
It should be emphasised that non-neurogenic factors such as flu-
id loss due to vomiting or diarrhoea may substantially worsen
neurogenic postural hypotension and will need to be rectified.
(Modified from ref.s 17, 22)
(33-35) (Fig. 5). In PD, dopaminergic drug
therapy does not appear to be the cause of the
abnormality and such patients differ from other
parkinsonian disorders such as vascular parkin-
sonism and PSP (34). These findings are simi-
lar to those described using 18F fluo-
rodopamine and positron emission tomography
scanning (36), which indicate minimal uptake
in PD with AF, but normal uptake in MSA.
Overall, the data suggest that apparently selec-
tive cardiac sympathetic denervation occurs at
an early stage in PD; the reason for this abnor-
mality and its implications in relation to heart
rate control and cardiac arrhythmias remain to
be resolved.
CONCLUDING REMARKS
In parkinsonian disorders, a variety of car-
diovascular abnormalities affecting blood pres-
sure control and heart rate variability occur, a
prime example being MSA where autonomic
failure is an integral component of the disease.
The abnormalities reported in PD may have
other causes and explanations; thus, evaluation
of cardiovascular autonomic dysfunction in
these disorders is important. It aids diagnosis,
in MSA where such abnormalities are charac-
teristic, and in PSP where cardiovascular auto-
nomic abnormalities are an exclusionary fea-
ture. Furthermore, such evaluation is necessary
for appropriate overall management in parkin-
sonian disorders.
REFERENCES
11. Mathias CJ. Autonomic disorders and their
recognition. N Eng J Med 1997;10:721-
724
12. Schatz IJ, Bannister R, Freeman RL et al.
Consensus statement on the definition of
orthostatic hypotension, pure autonomic
failure and multiple system atrophy. Clin
Auton Res 1996;6:125-126
13. Mathias CJ, Bannister R. Investigation of
autonomic disorders. In: Mathias CJ, Ban-
nister R eds Autonomic Failure: A Te x t-
book of Clinical Disorders of the Auto-
nomic Nervous System. 4th Edition. Ox-
ford; Oxford University Press 1999:169-
195
14. Mathias CJ. Orthostatic hypotension -
causes, mechanisms and influencing fac-
tors. Neurology 1995;45:s6-11
15. Mathias CJ, Mallipeddi R, Bleasdale-Barr
K. Symptoms associated with orthostatic
hypotension. J Neurol 1999;246:893-898
16. Mathias CJ. Autonomic dysfunction. In:
Grimley-Evans J, Franklin Williams T,
Lynn Beattie B, Michel J-P, Wilcock GK
eds Oxford Textbook of Geriatric Medi-
cine. Second Edition. Oxford; Oxford Uni-
versity Press 2000:833-852
17. Mathias CJ. Disorders affecting autonomic
function in Parkinsonian patients. In: Bat-
tistin L, Scarlato G, Caraceni T, Ruggieri
FUNCTIONAL NEUROLOGY (16)3 2001 263
Cardiovascular dysfunction in Parkinsonian disorders
F i g . 5 - Comparison of the early phase, heart/medi-
astinum ratio (H/M), using
131
meta-iodo-benzylguanadine
scintigraphic scanning in different neurological disorders
and in controls. Open circles show normal and filled cir-
cles abnormal H/M ratios. PD = Parkinsons disease, VP
= vascular parkinsonism, MSA = multiple system atro-
phy, ET = essential tremor, DC = disease controls, C =
healthy controls. (From ref. 34).
S. eds Parkinsons Disease. New Yo r k ;
Raven Press 1996; ch. 69:383-391
18. Mathias CJ. Cardiovascular autonomic
dysfunction in parkinsonian patients. Clin
Neurosci 1998;5:153-166
19. Sandroni P, Ahlskog JE, Fealey RD, Low
PA. Autonomic involvement in extrapyra-
midal and cerebellar disorders. Clin Auton
Res 1991;1:147-155
10. Senard J-M, Rai S, Lapeyre-Mestre M et
al. Prevalence of orthostatic hypotension
in Parkinsons disease. J Neurol Neurosurg
Psychiatry 1997;63:578-589
11 . Wenning GK, Scherfler C, Granata R et al.
Time course of symptomatic orthostatic hy-
potension and urinary incontinence in pa-
tients with postmortem confirmed parkin-
sonian syndromes: a clinicopathological
s t u d y. J Neurol Neurosurg Psychiatry 1999;
6 7 : 6 2 0 - 6 2 3
12. Mathias CJ. Can the early presence of au-
tonomic dysfunction aid diagnosis in
parkinsonism? J Neurol Neurosurg Psychi-
atry 1999;67:566 (editorial)
13. Senard JM, Valet P, Durrieu G et al.
A d r e n e rgic supersensitivity in parkinsoni-
ans with orthostatic hypotension. Eur J
Clin Invest 1990;20:613-619
14. Senard J-M, Rascol O, Durrieu G et al. Ef-
fects of Yohimbine on plasma cate-
cholamine levels in orthostatic hypoten-
sion related to Parkinsons disease or mul-
tiple system atrophy. Clin Neuropharmacol
1993;16:70-76
15. Daniel S. The neuropathology and neuro-
chemistry of multiple system atrophy. In:
Mathias CJ, Bannister R eds Autonomic
Failure: A Textbook of Clinical Disorders
of the Autonomic Nervous System. 4th
Edition. Oxford University Press, Oxford
1999;321-328
16. Matthews MR. Autonomic ganglia and
preganglionic neurones in autonomic fail-
ure In: Mathias CJ, Bannister R eds Auto-
nomic Failure: A Textbook of Clinical
Disorders of the Autonomic Nervous Sys-
tem. 4th Edition. Oxford; Oxford Univer-
sity Press 1999:329-339
17. Mathias CJ, Kimber JR. Treatment of pos-
tural hypotension. J Neurol Neurosurg
Psychiatry 1998;65:285-289
18. Kimber JR, Watson L, Mathias CJ. Physi-
ological, pharmacological and neurohor-
monal assessment of autonomic function
in progressive supranuclear palsy. Brain
2000;123:1422-1430
19. Hishikawa N, Hashizume Y, Hirayama M
et al. Brainstem-type Lewy body disease
presenting with progressive autonomic
failure and lethargy. Clin Auton Res 2000;
10:139-143
20. Larner AJ, Mathias CJ, Rossor MN. Auto-
nomic failure preceding dementia with
Lewy bodies. J Neurol 2000;247:229-231
21. Kosaka K. Diffuse Lewy body disease in
Japan. J Neurol 1990;237:197-204
22. Mathias CJ, Kimber JR. Postural hypoten-
sion - causes, clinical features, investiga-
tion and management. Annu Rev Med
1999;50:317-336
23. Jordan J, Shannon JR, Grogan E, Biag-
gioni I, Robertson D. A potent pressor re-
sponse elicited by drinking water. Lancet
1999;353:723 (letter)
24. Cariga P, Mathias CJ. Continuous hemo-
dynamic responses to distilled water inges-
tion in pure autonomic failure. Clin Auton
Res 2000;10:89-90
25. Senard J-M, Brefel C, Carel C, Tran M-A,
Montastruc J-L. Water drinking and the
heart. Lancet 1999;353:1971-1978
26. Cotzias GC, Papvasilou PS, Gellene R.
Modification of parkinsonism chronic
treatment with l-dopa. N Engl J Med
1969;280:337-334
27. Baratti M, Calzetti S. Fluctuation of arteri-
al blood pressure during end-of-dose aki-
nesia in Parkinsons disease. J Neurol
Neurosurg Psychiatry 1984;47:1241-1243
2 8 . Ghika J, Bogousslavsky J. Presympto-
C.J. Mathias
264 FUNCTIONAL NEUROLOGY (16)3 2001
matic hypertension is a major feature in
the diagnosis of progressive supranu-
clear palsy. Arch Neurol 1997;54:11 0 4 -
11 0 8
29. Gutrecht JA. Autonomic cardiovascular
reflexes in progressive supranuclear palsy.
J Auton Nerv Syst 1992;39:29-35
30. van Dijk J, Haan J, Koenderink M, Ray-
mund A, Roos C. Autonomic nervous
function in progressive supranuclear palsy.
Arch Neurol 1991;48:1083-1084
3 1 . Lo SS, Mathias CJ, St John Sutton M. QT
interval and dispersion in primary auto-
nomic failure. Heart 1996;75:498-501
32. Hakusui S, Yasuda T, Yanagi T et al. A ra-
diological analysis of heart sympathetic
functions with meta-(
1 2 3
I) iodobenzylgua-
nadine in neurological patients with auto-
nomic failure. J Auton Nerv Syst 1994;49:
81-84
3 3 . Yoshita M. Differentiation of idiopathic
P a r k i n s o n s disease from striatonigral de-
generation and progressive supranuclear
palsy using iodine-123 and metaiodoben-
zylguanadine myocardial scintigraphy. J
Neurol Sci 1998;155:60-67
34. Orimo S, Ozawa E, Nakade S, Sugimoto
T, Mizusawa H. 123I-metaiodobenzyl-
guanidine myocardial scintigraphy in
P a r k i n s o n s disease. J Neurol Neurosurg
Psychiatry 1999;67:189-194
35. Braune S, Reinhardt M, Schnitzer R,
Riedel A, Lucking CH. Cardiac uptake of
(
1 2 3
I) MIBG separates Parkinsons disease
from multiple system atrophy. Neurology
1999;53:1020-1025
36. Goldstein DS, Holmes C, Cannon RO III,
Eisenhofer G, Kopin IJ. Sympathetic car-
dioneuropathy in dysautonomias. N Engl J
Med 1997;336:696-702
FUNCTIONAL NEUROLOGY (16)3 2001 265
Cardiovascular dysfunction in Parkinsonian disorders
Você também pode gostar
- Hipotensi Orthostatik NeurogenikDocumento8 páginasHipotensi Orthostatik NeurogenikayuniputriAinda não há avaliações
- Mechanisms, Causes, and Evaluation of Orthostatic Hypotension - UpToDateDocumento20 páginasMechanisms, Causes, and Evaluation of Orthostatic Hypotension - UpToDateCipriano Di MauroAinda não há avaliações
- A Review of The Etiology, Asssociated Comorbidities, andDocumento13 páginasA Review of The Etiology, Asssociated Comorbidities, andFrancis RomanosAinda não há avaliações
- Hipotensi PDFDocumento6 páginasHipotensi PDFimahAinda não há avaliações
- PRIN PBL Week 11 Tutorial 1Documento3 páginasPRIN PBL Week 11 Tutorial 1jonx225Ainda não há avaliações
- Pathophysiology of Heart FailureDocumento2 páginasPathophysiology of Heart Failurewayanesa9Ainda não há avaliações
- АГ, атеросклероз удDocumento74 páginasАГ, атеросклероз удsoumyajitchakraborty0238Ainda não há avaliações
- Hypertensive Encephalopathy: Presentation DDX Workup Treatment MedicationDocumento8 páginasHypertensive Encephalopathy: Presentation DDX Workup Treatment MedicationMoh SuriyawalAinda não há avaliações
- Pathophysiology Diagnosis and Treatment of Orthostatic Hypotension and Vasovagal Syncope1Documento17 páginasPathophysiology Diagnosis and Treatment of Orthostatic Hypotension and Vasovagal Syncope1Idha AAinda não há avaliações
- Neurohormonal Hypothesis in Heart FailureDocumento11 páginasNeurohormonal Hypothesis in Heart FailureCypress Trixia Mananquil MacapagalAinda não há avaliações
- Cardiovascular Autonomic Dysfunction in Parkinson's DiseaseDocumento7 páginasCardiovascular Autonomic Dysfunction in Parkinson's DiseaseCocosul Cocosului CocosaruluiAinda não há avaliações
- CH27 FinalDocumento8 páginasCH27 FinalDiogoBeirãoAinda não há avaliações
- Cardiovascular Dysfunction in Spinal Cord DisordersDocumento12 páginasCardiovascular Dysfunction in Spinal Cord DisordersGerardo SilvaAinda não há avaliações
- Disautonomia en Adulto Mayor 2018Documento13 páginasDisautonomia en Adulto Mayor 2018Carlos BucaraAinda não há avaliações
- Heart Failure Pathophysiology ExplainedDocumento42 páginasHeart Failure Pathophysiology ExplainedParsa EbrahimpourAinda não há avaliações
- POTS Current Concepts Trends in CVMDocumento5 páginasPOTS Current Concepts Trends in CVMmperlethAinda não há avaliações
- J Neurol Neurosurg Psychiatry 2013 Asahina 674 80Documento8 páginasJ Neurol Neurosurg Psychiatry 2013 Asahina 674 80doraemonraniAinda não há avaliações
- Congestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications For Respiratory CareDocumento10 páginasCongestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications For Respiratory CareKevinDilianSugandaAinda não há avaliações
- Malignant Hypertension: Hypertensive EmergenciesDocumento7 páginasMalignant Hypertension: Hypertensive EmergenciesAbdul QuyyumAinda não há avaliações
- Peer Review Process: Author: Section Editor: Deputy EditorDocumento14 páginasPeer Review Process: Author: Section Editor: Deputy EditorLuis Enrique Caceres AlavrezAinda não há avaliações
- Is Postural Orthostatic Tachycardia Syndrome (POTS) A Central Nervous System Disorder?Documento8 páginasIs Postural Orthostatic Tachycardia Syndrome (POTS) A Central Nervous System Disorder?LinaConejomutanterosaAinda não há avaliações
- Treatment OptionsDocumento17 páginasTreatment OptionsAnonymous bbeAZHxZAinda não há avaliações
- Inappropriate Sinus TachycardiaDocumento23 páginasInappropriate Sinus TachycardiaOnon EssayedAinda não há avaliações
- Neurologic Manifestations of Hyperthyroidism and GravesDocumento3 páginasNeurologic Manifestations of Hyperthyroidism and GravesAde YonataAinda não há avaliações
- Medical Guide to Postural Tachycardia Syndrome (PoTSDocumento12 páginasMedical Guide to Postural Tachycardia Syndrome (PoTSAttis PhrygiaAinda não há avaliações
- Diff DS AH - Eh. TreatmentDocumento80 páginasDiff DS AH - Eh. TreatmentCastleKGAinda não há avaliações
- Abnormalities of Angiotensin Regulation in PotsDocumento14 páginasAbnormalities of Angiotensin Regulation in Potsiri_balAinda não há avaliações
- MJMHS 0626Documento7 páginasMJMHS 0626lilydariniAinda não há avaliações
- Jurnal FisioDocumento8 páginasJurnal Fisiorizkya amanahAinda não há avaliações
- 4ea7cdc044aebf27f87d94a2 PDFDocumento7 páginas4ea7cdc044aebf27f87d94a2 PDFTaufiqur Rohman ChimeraAinda não há avaliações
- Pharmacotherapy of Heart FailureDocumento17 páginasPharmacotherapy of Heart FailurelisaAinda não há avaliações
- Signs and SymptomsDocumento16 páginasSigns and SymptomsRose AnnAinda não há avaliações
- Syncope - Electrocardiographic and Clinical CorrelationDocumento16 páginasSyncope - Electrocardiographic and Clinical CorrelationNANDY LUZ FERIA DIAZAinda não há avaliações
- Heart Failure - AhaDocumento77 páginasHeart Failure - AhaChendy Endriansa100% (1)
- How To Manage A Patient With OrthostaticDocumento18 páginasHow To Manage A Patient With OrthostaticReza Oktarizal100% (2)
- 1-s2.0-S003537872301144X-mainDocumento12 páginas1-s2.0-S003537872301144X-mainSergioAinda não há avaliações
- The Effect of Cilostazol On Right Heart FunctionDocumento43 páginasThe Effect of Cilostazol On Right Heart FunctionGunawan YogaAinda não há avaliações
- Parkinson's & Movement Disorders-Harrison's NeurologyDocumento23 páginasParkinson's & Movement Disorders-Harrison's Neurologyindia2puppyAinda não há avaliações
- Neuromodulation in Treatment of Hypertension by Acupuncture: A Neurophysiological ProspectiveDocumento8 páginasNeuromodulation in Treatment of Hypertension by Acupuncture: A Neurophysiological Prospectivewillv4Ainda não há avaliações
- Molecular Neurobiology of DepressionDocumento9 páginasMolecular Neurobiology of DepressionFlyefs AttikosAinda não há avaliações
- Materi English 1Documento11 páginasMateri English 1WINARDIAinda não há avaliações
- Stupor and Coma in Adults: Author: Section Editors: Deputy EditorDocumento30 páginasStupor and Coma in Adults: Author: Section Editors: Deputy EditorYessenia BarrantesAinda não há avaliações
- Role of Sleep-Wake Cycle On Blood Pressure Circadian Rhythms and HypertensionDocumento13 páginasRole of Sleep-Wake Cycle On Blood Pressure Circadian Rhythms and HypertensionFarah AhmadAinda não há avaliações
- Drugs Used in Heart Failure: Pharmacology (2) PHAR 342Documento19 páginasDrugs Used in Heart Failure: Pharmacology (2) PHAR 342Dana HamarshehAinda não há avaliações
- Peripheral Autoregulatory ComponentsDocumento2 páginasPeripheral Autoregulatory ComponentsDebbyNovriozaAinda não há avaliações
- PRES (Posterior Reversible Encephalopathy Syndrome) and Eclampsia-ReviewDocumento5 páginasPRES (Posterior Reversible Encephalopathy Syndrome) and Eclampsia-ReviewAvicena M IqbalAinda não há avaliações
- Chronic Baroreflex Activation Restores Spontaneous Baroreflex Control and Variability of Heart Rate in Obesity-Induced HypertensionDocumento10 páginasChronic Baroreflex Activation Restores Spontaneous Baroreflex Control and Variability of Heart Rate in Obesity-Induced HypertensionCaesar Catalin CaratasuAinda não há avaliações
- Fatigue: Normal and Abnormal FatigueDocumento8 páginasFatigue: Normal and Abnormal FatigueMt. ZulfiqorAinda não há avaliações
- Proyecto de Investigación Del Sistema CardiovascularDocumento3 páginasProyecto de Investigación Del Sistema CardiovascularNatalia quirogaAinda não há avaliações
- Fisiopatologia de La Falla CardiacaDocumento28 páginasFisiopatologia de La Falla CardiacaDANIELA ANDREA MARTINEZ FUENTESAinda não há avaliações
- Screen for Secondary Causes of HypertensionDocumento12 páginasScreen for Secondary Causes of HypertensionMelissaHuayapaAAinda não há avaliações
- Clinical Autonomic and Mitochondrial Disorders: Diagnosis, Prevention, and Treatment for Mind-Body WellnessNo EverandClinical Autonomic and Mitochondrial Disorders: Diagnosis, Prevention, and Treatment for Mind-Body WellnessAinda não há avaliações
- Unit 2 Heart Failure: StructureDocumento29 páginasUnit 2 Heart Failure: StructurebtaleraAinda não há avaliações
- Anti Hypertensive ThesisDocumento85 páginasAnti Hypertensive Thesiskartik369Ainda não há avaliações
- Heart Failure TodayDocumento54 páginasHeart Failure TodaypoolchagoAinda não há avaliações
- Search Termsearch Database: Limits Advanced Journal List HelpDocumento21 páginasSearch Termsearch Database: Limits Advanced Journal List Helpحسام جبار مجيدAinda não há avaliações
- The Human Sympathetic Nervous System: Its Relevance in Hypertension and Heart FailureDocumento10 páginasThe Human Sympathetic Nervous System: Its Relevance in Hypertension and Heart FailureadeAinda não há avaliações
- Uncontrolled Blood Pressure: Recognizing and Treating Hypertensive EmergenciesDocumento2 páginasUncontrolled Blood Pressure: Recognizing and Treating Hypertensive Emergenciesmhassan8154Ainda não há avaliações
- Hipertensi: A. Hypertension A.1 Definition of HypertensionDocumento12 páginasHipertensi: A. Hypertension A.1 Definition of HypertensionIrwan SyahputraAinda não há avaliações
- Pathophysiology of Heart Failure - Neurohumoral Adaptations PDFDocumento10 páginasPathophysiology of Heart Failure - Neurohumoral Adaptations PDFcristianamihailaAinda não há avaliações
- Cell Transport RevisionDocumento32 páginasCell Transport RevisionramadanAinda não há avaliações
- 6 - Hemodynamic Disorders PDFDocumento66 páginas6 - Hemodynamic Disorders PDFNogra CarlAinda não há avaliações
- Membrane Transport Mechanisms and HomeostasisDocumento29 páginasMembrane Transport Mechanisms and Homeostasisramadan100% (1)
- 357 Man 07Documento28 páginas357 Man 07ramadanAinda não há avaliações
- Ijms 15 03989Documento18 páginasIjms 15 03989ramadanAinda não há avaliações
- DR Ramadan ObjectivesDocumento3 páginasDR Ramadan ObjectivesramadanAinda não há avaliações
- 1Documento7 páginas1ramadanAinda não há avaliações
- 04a CartilageDocumento22 páginas04a CartilageramadanAinda não há avaliações
- Renal Physiology RevisionDocumento6 páginasRenal Physiology RevisionramadanAinda não há avaliações
- Endocrine QuestionsDocumento4 páginasEndocrine QuestionsramadanAinda não há avaliações
- NBME Physio QsDocumento7 páginasNBME Physio QsramadanAinda não há avaliações
- Human Anatomy: The CellDocumento33 páginasHuman Anatomy: The CellramadanAinda não há avaliações
- Preparation of The Mitochondrial FractionDocumento1 páginaPreparation of The Mitochondrial FractionramadanAinda não há avaliações
- Exercise Cardio Topic 9Documento2 páginasExercise Cardio Topic 9ramadanAinda não há avaliações
- Study of The Possible Cardioprotective Effects of Insulin, ATP, and - Arginine Against Isoproterenol-Induced Myocardial InfarctionDocumento7 páginasStudy of The Possible Cardioprotective Effects of Insulin, ATP, and - Arginine Against Isoproterenol-Induced Myocardial InfarctionramadanAinda não há avaliações
- Management of Poisoning and Drug Overdose - 2 PDFDocumento24 páginasManagement of Poisoning and Drug Overdose - 2 PDFramadanAinda não há avaliações
- Exercise Digestive Topic 2Documento6 páginasExercise Digestive Topic 2ramadan0% (1)
- Exam2 98Documento8 páginasExam2 98ramadanAinda não há avaliações
- Biochem SpecificationDocumento2 páginasBiochem SpecificationramadanAinda não há avaliações
- Changes of Ghrelin and Leptin Levels in Plasma by Cigarette Smoke in RatsDocumento8 páginasChanges of Ghrelin and Leptin Levels in Plasma by Cigarette Smoke in RatsramadanAinda não há avaliações
- 274 Renal Physiology - Part 2Documento11 páginas274 Renal Physiology - Part 2ramadanAinda não há avaliações
- Intestine Krebs-Ringer's Buffer Solution CompositionDocumento1 páginaIntestine Krebs-Ringer's Buffer Solution CompositionramadanAinda não há avaliações
- Renal PhysiologyDocumento37 páginasRenal PhysiologyramadanAinda não há avaliações
- Respiratory PhysiologyDocumento38 páginasRespiratory Physiologyramadan100% (3)
- The Respiratory System Part 2Documento25 páginasThe Respiratory System Part 2ramadanAinda não há avaliações
- Thorax00105 0035 PDFDocumento4 páginasThorax00105 0035 PDFramadanAinda não há avaliações
- EMG IntroductionDocumento6 páginasEMG IntroductionramadanAinda não há avaliações
- Respiratory and Gastrointestinal Complications of Caustic Ingestion in ChildrenDocumento3 páginasRespiratory and Gastrointestinal Complications of Caustic Ingestion in ChildrenramadanAinda não há avaliações
- Corrosive Acid Ingestion in Clinical and Endoscopic Study: Man ADocumento5 páginasCorrosive Acid Ingestion in Clinical and Endoscopic Study: Man AramadanAinda não há avaliações
- Child Development: Resilience & Risk, A Course SyllabusDocumento17 páginasChild Development: Resilience & Risk, A Course SyllabusJane GilgunAinda não há avaliações
- Isc BUX82/83: Isc Silicon NPN Power TransistorsDocumento2 páginasIsc BUX82/83: Isc Silicon NPN Power TransistorsCarlos HCAinda não há avaliações
- Molecular Biology: Robert F. WeaverDocumento60 páginasMolecular Biology: Robert F. WeaverSidharth KhannaAinda não há avaliações
- CHAPTER 6 Maintenance Management: Introduction, Importance, Types & ReliabilityDocumento29 páginasCHAPTER 6 Maintenance Management: Introduction, Importance, Types & Reliabilitynur aidaAinda não há avaliações
- Processing Cacao Pod Husk into Low-Methoxyl PectinDocumento9 páginasProcessing Cacao Pod Husk into Low-Methoxyl PectinEmmanuel PlazaAinda não há avaliações
- MHWirth PileTopDrillRigs Brochure Web2Documento12 páginasMHWirth PileTopDrillRigs Brochure Web2geobyun100% (1)
- General Biology 1: Quarter 1 - Module - : Title: Cell CycleDocumento27 páginasGeneral Biology 1: Quarter 1 - Module - : Title: Cell CycleRea A. Bilan0% (1)
- Experi Men 22Documento7 páginasExperi Men 22bernardAinda não há avaliações
- Environmental Pollution Control (ET ZC362 - WILP Course) : BITS PilaniDocumento41 páginasEnvironmental Pollution Control (ET ZC362 - WILP Course) : BITS Pilanisa_arunkumarAinda não há avaliações
- Public Safety BriefingDocumento23 páginasPublic Safety BriefingHNNAinda não há avaliações
- 5090 w11 Ms 62Documento3 páginas5090 w11 Ms 62mstudy123456Ainda não há avaliações
- Rotex Brochure PDFDocumento4 páginasRotex Brochure PDFestramilsolutionAinda não há avaliações
- Effects of Air and Noise PollutionDocumento6 páginasEffects of Air and Noise Pollutionhaiqa malikAinda não há avaliações
- Indian Economy On The Eve of IndependenceDocumento5 páginasIndian Economy On The Eve of IndependenceAshiga RajendaranAinda não há avaliações
- Methyldopa Drug DataDocumento3 páginasMethyldopa Drug DataLaurel Joshua Reyes DauzAinda não há avaliações
- Level I Questions Thermal and Infrared Testing Method: Southern Inspection ServicesDocumento8 páginasLevel I Questions Thermal and Infrared Testing Method: Southern Inspection Servicesprabhakaran.SAinda não há avaliações
- ANGLICISMSDocumento14 páginasANGLICISMSManuel Jorquera100% (1)
- C9880046 Signed OfferLetterDocumento8 páginasC9880046 Signed OfferLetterẞhûpâthi RëddyAinda não há avaliações
- Crude Palm Oil MSDS Provides Safety InformationDocumento3 páginasCrude Palm Oil MSDS Provides Safety InformationCarlos MontanoAinda não há avaliações
- Bearing From Copper AlloyDocumento7 páginasBearing From Copper AlloyPhung Tuan AnhAinda não há avaliações
- Uco Bank Final (Simple Charts)Documento40 páginasUco Bank Final (Simple Charts)gopal8726Ainda não há avaliações
- Eastern RlyDocumento25 páginasEastern Rlyshivam.jhawar95Ainda não há avaliações
- Charles LawDocumento12 páginasCharles LawLerr Real RelleAinda não há avaliações
- RPH Finals Quiz BeeDocumento29 páginasRPH Finals Quiz BeeJoshua Liann EscalanteAinda não há avaliações
- Harmonized "Cluster" Document: For Electrical Connectors Conductive Plated CoatingsDocumento22 páginasHarmonized "Cluster" Document: For Electrical Connectors Conductive Plated CoatingsFrederico CésarAinda não há avaliações
- Thermocold AWC PROZONE Tech PDFDocumento44 páginasThermocold AWC PROZONE Tech PDFAlexAinda não há avaliações
- SWOT Analysis AuchanDocumento2 páginasSWOT Analysis AuchanDaniela DogaruAinda não há avaliações
- 17 Quarter 1 Module 17-ANAEROBICDocumento20 páginas17 Quarter 1 Module 17-ANAEROBICMah Jane DivinaAinda não há avaliações
- Cell Membrane TransportDocumento37 páginasCell Membrane TransportMaya AwadAinda não há avaliações
- Fever With Rash in Table Form.Documento4 páginasFever With Rash in Table Form.Azizan HannyAinda não há avaliações