Escolar Documentos
Profissional Documentos
Cultura Documentos
Tube Ileostomy
Enviado por
abhishekbmcDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Tube Ileostomy
Enviado por
abhishekbmcDireitos autorais:
Formatos disponíveis
International Scholarly Research Network
ISRN Surgery
Volume 2012, Article ID 547523, 5 pages
doi:10.5402/2012/547523
Clinical Study
Comparison between Tube Ileostomy and Loop Ileostomy as
a Diversion Procedure
Vijayraj Patil, Abhishek Vijayakumar, M. B. Ajitha, and Sharath Kumar L
Department of General Surgery, Victoria Hospital, Bangalore Medical College and Research Institute, Bangalore 560002, India
Correspondence should be addressed to Abhishek Vijayakumar, abhishekbmc@yahoo.co.in
Received 3 November 2012; Accepted 27 November 2012
Academic Editors: R. W. Hsu and K.-E. Kahnberg
Copyright 2012 Vijayraj Patil et al. This is an open access article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Aim. Loop ileostomy has high complication rates and causes much patient inconvenience. This study was performed to compare
the outcome of tube versus loop ileostomy in management of ileal perforations. Patients and Methods. From July 2008 to July
2011, all patients with ileal perforation on laparotomy where a defunctioning proximal protective loop ileostomy was considered
advisable were chosen for study. Patients were randomly assigned to undergo either tube ileostomy or classical loop ileostomy as the
diversion procedure. Tube ileostomy was constructed in the fashion of feeding jejunostomy, with postoperative saline irrigation.
Results. A total of 60 diversion procedures were performed over the period with 30 for each of tube and loop ileostomy. Typhoid
and tuberculosis formed the most common etiology for ileal perforation. The complication rate of tube ileostomy was 33%. Main
complications related to tube ileostomy were peritubal leak, tube blockage. In patients with loop, overall complications in 53%
majority were peristomal skin irritation and wound infection following ileostomy closure. Two patients developed obstruction
following ileostomy closure which needed reoperation. Conclusions. Tube ileostomy is eective and feasible as a diversion procedure
and has reduced morbidity. It can be used as an alternative to loop ileostomy.
1. Introduction
Emergency laparotomy for intestinal perforation and ob-
struction surgeons are faced with dicult decision to per-
form stoma for fecal diversion; an even more dicult task
is explaining the need for stoma to patient. Creation of a
diverting stoma has its own set of complications including
stomal retraction, prolapse, or necrosis; para-ileostomy
infection/abscess and stula; intestinal obstruction; skin
irritation/excoriation; mucosal ulceration; oensive odors;
prestomal ileitis; diarrhea; and hemorrhage [1]. The need for
frequent change of the costly ileostomy appliance because
of the leakage following loss of seal imposes great nancial
burden, especially in developing countries. Aneed for second
surgery for closure of stoma adds on to nancial burden and
unnecessary delays due to nonprioritization of stoma closure
due to high case volume. The closure of the intestinal stoma
is also frequently followed by complications in 17%27% of
patients [2, 3].
These complications include fever, wound infection,
abdominal septic complications, leak fromileostomy closure,
intestinal obstruction, incisional hernia, and death.
We designed this prospective study to assess the feasibility
and outcome of proximal catheter ileostomy in place of a
defunctioning proximal loop ileostomy in patients treated by
primary repair and/or resection-anastomosis of small bowel.
The construction of catheter ileostomy was based on the
concept of the currently well-accepted catheter jejunostomy.
A comparison was made between tube ileostomy and loop
ileostomy in terms of complications and outcome.
2. Material and Methods
The present study was conducted at Bangalore Medical
College and Research Institute (BMCRI), Bangalore, India,
from July 2008 to July 2011. Patients who underwent explo-
rative laparotomy for small bowel perforation or obstruction
and in whom a decision to perform a proximal diversion
stoma on the basis of any of the following intraoperative
ndings: multiple perforations, edematous and inamed
bowel, adherent loops of bowel, and insecure anastomosis,
were chosen for the study. Patients were randomly assigned
to undergo either a tube ileostomy or classical loop ileostomy
as a diversion procedure.
2 ISRN Surgery
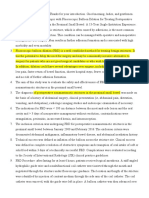
Figure 1: Steps of tube ileostomy. (1) Tube selection abdominal drain or Foleys catheter. (2) Selection of healthy segment of bowel proximal
to repair. (3) Tube insertion and anchoring with purse string suture. (4) Fixation to anterior abdominal wall. (5) Fixation of tube to skin.
Patients who died within 5 days of surgery unrelated
to anastomotic complication and patients who were lost to
followup were excluded from the study.
3. Technique of Tube Ileostomy Construction
At laparotomy after dealing with primary pathology and per-
forming necessary procedure, patients underwent either tube
ileostomy or open ileostomy. A 28 French abdomen drain
tube was brought into peritoneal cavity through stab incision
on abdomen wall. Tube was inserted 10 cm proximal in
diseased bowel in case of ileal perforation with tube tip
directed proximally (Figure 1). Tube was secured to bowel
wall by 2-0 polyglactin by purse string suture. Segment of
bowel 5 cm proximal and 5 cm distal to the site of inser-
tion of tube was xed to parietal wall with interrupted 2-0
polyglactin. Tube was xed to skin with 2-0 Mersilk and con-
nected to drainage bag. Another tube was inserted through
ank and placed in pelvis.
In patients with no evidence of anastomotic, leak tube
was clamped after second week and nally removed after
third week of surgery to have a controlled stula in place.
Clinical suspicion of leak prompted the tube ileostomy to be
maintained till the leak would seal.
A detailed record of day on which tube ileostomy started
functioning, tube drainage, peritubal leak, tube blockade,
any feature suggestive of anastomotic leak, or any other com-
plication was maintained. The day when tube was clamped
and removed was recorded. Time to closure of the controlled
stula was also noted. All the patients were regularly followed
in the outpatient department for any complications.
ISRN Surgery 3
4. Results
Over a period of three years from July 2008 to July 2011 a
total of 60 diversion procedure were performed. Out of the
diversion procedures 30 were conventional loop ileostomy
and 30 were tube ileostomy as described above.
Patients ranged from 16 to 63 years with mean age 32.6
years. Majority of patients were male (70%).
Preoperative diagnosis was perforation (n = 46), ob-
struction (n = 15), and penetrating abdominal injury (n =
1). Duration of symptoms ranged from 1 to 5 days. The
most common symptoms were pain abdomen (n = 53),
abdominal distension (n = 45), and absolute constipation
(n = 22). Among presented signs all patients had tachy-
cardia, signs of peritonitis were present in 47 patients with
masked liver dullness (n = 23), free uid in abdomen
(n = 42), and seven patients presented with severe dehydra-
tion and shock.
Erect X-ray showed air under diaphragm in 36 cases,
dilated bowel loop in 24 cases, and ground glass appearance
in 7 cases. Abdominal ultrasound showed moderate free uid
in 54 of the cases and dilated loops in 28 cases. Widal test
was positive in 38 cases with high O titers in 22 cases, and
tuberculin test was positive in 16 cases with 9 cases showing
high Adenosine deaminase levels.
During the period of study 13 patients died in immediate
postoperative period, unrelated procedure, and related com-
plications, 9 were due to septicemia and multiorgan failure
and 2 each as a result of massive pulmonary embolism and
myocardial infarction. These cases were excluded from the
study.
In majority of patients (64%) tube ileostomy started
functioning on rst postoperative day while in rest from sec-
ond day. Tube ileostomy output ranged from 50700 mL/day
with mean of 300 mL. Once a day irrigation was sucient
to keep the tube patent in 25 patients; 5 patients developed
tube blockade of whom 4 resolved with thrice daily irrigation
of tube with saline. One patient who had persistent blockade
and developed signs of peritonitis was reoperated and found
to have a kinking of tube and anastomotic leak. Three
patients developed peritubal leak which was managed with
regular dressing.
The tube ileostomy was removed on postoperative day
21; the drain site managed with daily dressing in whom the
wound discharge was minimum. Two patients had increased
wound discharge which was managed with application of
colostomy bag for 2 weeks which later resolved, and wound
closure was achieved. The wound-closure time ranged from
4 to 9 days (mean 7 days). None of the patients required
formal closure of the wound. All patients were followed for
an average of 6 months and showed no complications.
In loop ileostomy group the main complication was peri-
stomal skin excoriation (n = 4) which required prolonged
regular dressing. Two patients developed severe dehydration
following high output from stoma and required hospitaliza-
tion for electrolyte abnormalities and were managed with
intravenous uid. There was one case of early necrosis of
stoma and retraction which required operation and stoma
revision. Anastomotic leak occurred in two cases one of
Table 1: Characteristics of cases.
Characteristics
Tube ileostomy Loop ileostomy
N % N %
Age in years
<20 2 6.6 0 0
2030 11 36.6 10 33.3
3040 12 40.0 15 50.0
4050 4 13.3 3 10.0
>50 1 3.3 2 6.6
Sex
Male 22 73.3 19 63.3
Female 8 26.6 11 36.6
Etiology
Typhoid 20 66.6 18 60.0
Tubercular 6 20.0 4 13.3
Traumatic 1 3.3 0 0
Nonspecic 3 10.0 8 26.6
Table 2: Complications following tube and loop ileostomy.
N %
Tube ileostomy
Peritubal leak 3 10.0
Tube block 5 16.6
Distal anastomotic leak 1 3.3
Tube migration 1 3.3
Loop ileostomy
Peristomal skin irritation 4 13.3
Electrolyte imbalance 2 6.6
Necrosis 1 3.3
Retraction 1 3.3
Post ileostomy closure obstruction 2 6.6
Wound infection 6 20.0
which required reoperation due to clinical deterioration.
The patients underwent ileostomy closure between 2 to 4
months (mean 10 weeks). The main complication following
ileostomy closure was wound infection (n = 6) which
resolved with regular dressing and antibiotics. Two patients
developed obstruction following closure one of whom
required reoperation. Patients were followed up for a period
of 6 months with one patient presenting with obstruction
which required reoperation and adhesion release (Tables 1
and 2).
5. Discussion
In the rst report of loop ileostomy by Turnbull and Weakley
[4] in 1966 it has gained popularity as a method of fecal
diversion to protect distal anastomosis. The routine use of
loop ileostomy to protect the distal anastomosis is much
debated, and the literature supports all arguments both in
favour and against. Therefore presently no conclusive evi-
dence or guidelines supports the use or avoidance of such
4 ISRN Surgery
ileostomies. Proponents of routine use argue that though the
ileostomy does not prevent leakage, it does however decrease
the detrimental eects of a leak [5] with less major leaks and
less reoperation rates [6].
In cases of intestinal perforation or obstruction with fea-
tures of peritonitis a defunctioning proximal protective loop
ileostomy is considered advisable due to presence of one or
more of the following intraoperative ndings: insecure repair
or anastomosis, multiple perforations, matted bowel loops,
and grossly unhealthy bowel due to severe edema and inam-
mation [7, 8].
On the other hand, the routine use of ileostomy adds to
the morbidity and mortality besides longer hospital stay and
costs. Furthermore because ileostomy closure is not a high
priority in this era of stringent nancial budgeting, it is often
postponed or delayed [9]. During this period stoma-related
complications have been reported to range from 974% [10
12].
Even minor complications with the ileostomy signi-
cantly hamper the quality of life of these patients. Tube ileo-
stomy as an alternative to loop ileostomy is an attempt to
protect the distal anastomosis and at the same time decrease
the ileostomy complications and totally avoid the morbidity
and mortality associated with stoma takedown.
The rst reported use of T-tube ileostomy was at Texas
Childrens Hospital in 1959 for proximal fecal diversion;
several investigators have reported successful outcomes fol-
lowing laparotomy with T-tube enterostomy with irrigation
in neonates with unresolved uncomplicated meconium ileus
unrelieved by contrast enema [13]. In 1981, Lizarralde [14]
used lateral tube ileostomy in 23 of 59 children operated
upon for typhoid ileal perforation and reported a success
rate of 43.5%. Rygl et al. [15] found T-tube ileostomy to
be an eective and safe primary repair technique in ve
extremely low-birth-weight children with localized intestinal
damage/perforation.
Use of tube ileostomy in adults is only sparingly reported.
With rst reported case by Hojo [16] who used tube ileo-
stomy along with total colectomy and ileoanal anastomosis
for familial polyposis coli in seven young patients and had
successful outcomes in all. He found that the simple tube
ileostomy is as eective as the loop ileostomy and recom-
mended the procedure.
In our study we noted complications with tube ileostomy
in 33% of patients; this was signicantly less than the com-
plication rate after the loop ileostomy of 53%. The peristomal
complications like skin breakdown, dermatitis, and erythema
with loop ileostomy were 16%, in accordance to that reported
in the literature ranging from 336% [17]. These problems
can be transient but recurrent till ileostomy is closed and
usually hamper the proper application of ileostomy appli-
ance making management of ileostomy euent dicult [18].
In our study local skin problems in tube ileostomy were
noted in only three patients due to peritubal leakage; how-
ever this problem is transient and easily treatable or pre-
ventable by maintaining tube patency by regular ushings.
Dehydration requiring frequent hospital admissions is a
well-known problem after ileostomy due to high ileostomy
output. Reported incidence of dehydration ranges from 2.2
20% [19]. These patients have to be on astringent diet
and antidiarrheal medication often [20]. Some recommend
such measures only if urinary sodium concentration is low
(010 meq/L), and delay discharge till euent is less than
1 L/day. Two of our patients on loop ileostomy presented
with dehydration and electrolyte disturbances requiring
readmission.
The other major complications associated with conven-
tional loop ileostomy include prolapsed and retractions. Of
these retraction is more worrisome as it results in skin exco-
riation and incomplete defunctionalization of the distal anas-
tomosis. This problem is reported to occur in up to 15.9%
of patients [21]. In our study only one patient developed
retraction of loop ileostomy which required reoperation.
Incomplete defunctionalization using tube ileostomy
occurs if the tube gets blocked and does not drain freely.
Tubal blockage was found in ve of our patients; it was
observed that in patients in whomthe tube was placed within
25 cm of ileocecal junction developed block. This could
probably be due to increased consistency of feces distally.
All tube blocks were managed with saline irrigation thrice
daily. In one patient who developed peritonitis and was reo-
perated there was kinking of the tube which had caused
circumferential tear at tube. A resection anastomosis was
done followed by a proximal loop ileostomy.
Early bowel obstruction before loop ileostomy reversal
has been reported to be due to adhesions, retraction of loop
ileostomy, and herniation of proximal bowel lateral to the
ileostomy. Stoma-related obstruction occurred in 6.4% with
loop ileostomy in the study reported by Metcalf et al. None
of the patients with tube ileostomy developed obstruction.
Two patients developed obstruction following closure of
loop ileostomy of whom one required reoperation. There
have been reports that the risk of obstruction is less if the
ileostomy site is resected and anastomosis performed by
stapler [22]. However others have not found any signicant
dierence between the various techniques of closure [20].
Leakage from distal anastomotic site with pelvic sepsis
despite proximal loop ileostomy is well known. Garca-
Botello et al. [20] reported 10.24% anastomotic leak in
series of 127 patients despite proximal loop ileostomy. Four
patients (3.15%) had to be reoperated due to generalized
peritonitis, worsening clinical signs, or evidence of sepsis
despite conservative management. Feinberg et al. reported
a 13.6% leak rate in their series of 117 patients [18]. Two
patients with loop ileostomy developed anastamostic leak
which was initially managed conservatively; one patient
required reoperation due to worsening clinical signs.
Other complications have been frequently reported with
delay in the ileostomy closure or the takedown itself. Gall-
stones occur with gallstone pancreatitis especially if the ileo-
stomy closure is delayed [18]. Anastomotic leaks from ileo-
stomy reversal site in up to 8.3% are mentioned in the lit-
erature [17, 19]. The incidence of wound infection has been
reported from 1.3%18.3% while incisional hernia occurs in
up to 11.9% of patients after ileostomy closure [17]. All these
morbidities are avoided with the use of tube ileostomy.
ISRN Surgery 5
In a study by Rondelli et al. [23] comparing loop ileo-
stomy to percutaneous tube ileostomy in patients undergo-
ing laparoscopic anterior resection for adenocarcinoma, a
balloon catheter was used for tube ileostomy and ination
of balloon to achieve complete defunctioning ileostomy. We
feel a complete defunctioning ileostomy is not necessary for
anastomosis healing and an adequate decrease in ow across
the anastomosis using tube ileostomy is enough. Also for suc-
cessful tube ileostomy care must be taken to place the tube
in healthy segment of bowel. Very proximal placement of
tube leads to high volume ileostomy output. And when tube
is placed in distal ileum a larger lumen tube must be used
to prevent tube blockade. Further large scale well-designed,
randomized control trials are needed to compare tube
ileostomy as an alternative to conventional loop ileostomy as
a diversion procedure.
6. Conclusion
Tube ileostomy was found to be an alternate diversion pro-
cedure with few complications and was easy to construct
and manage as compared to conventional ileostomy. It ee-
ctively diverts the bowel contents and avoids the need for a
second surgery and its related complications. Further larger
randomized studies need to be undertaken before tube ileo-
stomy could be recommended as an alternative to loop ileo-
stomy as a diversion procedure.
References
[1] J. C. Duchesne, Y. Z. Wang, S. L. Weintraub, M. Boyle, and J. P.
Hunt, Stoma complications: a multivariate analysis, Ameri-
can Surgeon, vol. 68, no. 11, pp. 961966, 2002.
[2] K. P. Riesener, W. Lehnen, M. H ofer, R. Kasperk, J. C. Braun,
and V. Schumpelick, Morbidity of ileostomy and colostomy
closure: impact of surgical technique and perioperative treat-
ment, World Journal of Surgery, vol. 21, no. 1, pp. 103108,
1997.
[3] L. J. Mann, P. J. Stewart, R. J. Goodwin, P. H. Chapuis, and E.
L. Bokey, Complications following closure of loop ileostomy,
Australian and New Zealand Journal of Surgery, vol. 61, no. 7,
pp. 493496, 1991.
[4] R. B. Turnbull Jr. and F. L. Weakley, Ileostomy technics and
indications for surgery, Review of Surgery, vol. 23, no. 5, pp.
310314, 1966.
[5] E. Carlsen and A. B. Bergan, Loop ileostomy: technical
aspects and complications, European Journal of Surgery, vol.
165, no. 2, pp. 140144, 1999.
[6] D. F. Altomare, O. C. Pannarale, L. Lupo, N. Palasciano, V.
Memeo, and M. Rubino, Protective colostomy closure: the
hazards of a minor operation, International Journal of Col-
orectal Disease, vol. 5, no. 2, pp. 7378, 1990.
[7] K. P. Singh, K. Singh, and J. S. Kohli, Choice of surgical pro-
cedure in typhoid perforation: experience in 42 cases, Journal
of the Indian Medical Association, vol. 89, no. 9, pp. 255256,
1991.
[8] H. N. Ahmed, M. P. Niaz, M. A. Amin, M. H. Khan, and A. B.
Parhar, Typhoid perforation still a common problem: situa-
tion in Pakistan in comparison to other countries of Low
Human Development, Journal of the Pakistan Medical Asso-
ciation, vol. 56, no. 5, pp. 230232, 2006.
[9] M. Kairaluoma, H. Rissanen, V. Kultti, J. P. Mecklin, and I.
Kellokumpu, Outcome of temporary stomas: a prospective
study of temporary intestinal stomas constructed between
1989 and 1996, Digestive Surgery, vol. 19, no. 1, pp. 4551,
2002.
[10] J. H. Saghir, F. D. McKenzie, D. M. Leckie et al., Factors that
predict complications after construction of a stoma: a retro-
spective study, European Journal of Surgery, vol. 167, no. 7,
pp. 531534, 2001.
[11] J. J. Park, A. Del Pino, C. P. Orsay et al., Stoma complications:
the Cook County Hospital experience, Diseases of the Colon
and Rectum, vol. 42, no. 12, pp. 15751580, 1999.
[12] G. C. OToole, J. M. P. Hyland, D. C. Grant, and M. K. Barry,
Defunctioning loop ileostomy: a prospective audit, Journal
of the American College of Surgeons, vol. 188, no. 1, pp. 69,
1999.
[13] G. Z. Mak, F. J. Harberg, P. Hiatt, A. Deaton, R. Calhoon,
and M. L. Brandt, T-tube ileostomy for meconium ileus: four
decades of experience, Journal of Pediatric Surgery, vol. 35, no.
2, pp. 349352, 2000.
[14] E. A. Lizarralde, Typhoid perforation of the ileum in child-
ren, Journal of Pediatric Surgery, vol. 16, no. 6, pp. 10121016,
1981.
[15] M. Rygl, K. Pycha, Z. Stranak et al., T-tube ileostomy for
intestinal perforation in extremely low birth weight neonates,
Pediatric Surgery International, vol. 23, no. 7, pp. 685688,
2007.
[16] K. Hojo, Total colectomy, rectal mucosectomy and ileoanal
anastomosis for familial polyposis coli - use of tube ileostomy,
Japanese Journal of Clinical Oncology, vol. 15, no. 4, pp. 661
669, 1985.
[17] H. D. W. M. Van De Pavoordt, V. W. Fazio, D. G. Jagelman, I.
C. Lavery, and F. L. Weakley, The oucome of loop ileostomy
closure in 293 cases, International Journal of Colorectal Dis-
ease, vol. 2, no. 4, pp. 214217, 1987.
[18] S. M. Feinberg, R. S. McLeod, and Z. Cohen, Complications
of loop ileostomy, American Journal of Surgery, vol. 153, no.
1, pp. 102107, 1987.
[19] S. D. Wexner, D. A. Taranow, O. B. Johansen et al., Loop
ileostomy is a safe option for fecal diversion, Diseases of the
Colon and Rectum, vol. 36, no. 4, pp. 349354, 1993.
[20] S. A. Garca-Botello, J. Garca-Armengol, E. Garca-Granero et
al., Aprospective audit of the complications of loop ileostomy
construction and takedown, Digestive Surgery, vol. 21, no. 5-
6, pp. 440446, 2004.
[21] A. M. Metcalf, R. R. Dozois, and R. W. Beart Jr., Temporary
ileostomy for ileal pouch-anal anastomosis: function and
complications, Diseases of the Colon and Rectum, vol. 29, no.
5, pp. 300303, 1986.
[22] H. Hasegawa, S. Radley, D. G. Morton, and M. R. B. Keighley,
Stapled versus sutured closure of loop ileostomy. A rando-
mized controlled trial, Annals of Surgery, vol. 231, no. 2, pp.
202204, 2000.
[23] F. Rondelli, R. Balzarotti, W. Bugiantella, L. Mariani, R.
Pugliese, and E. Mariani, Temporary percutaneous ileostomy
versus conventional loop ileostomy in mechanical extraperi-
toneal colorectal anastomosis: a retrospective study, European
Journal of Surgical Oncology, vol. 38, no. 11, pp. 10651070,
2012.
Você também pode gostar
- Presentation Sheets Zhang Dong-Yang Feb.22nd的副本Documento3 páginasPresentation Sheets Zhang Dong-Yang Feb.22nd的副本YangAinda não há avaliações
- Complicated AppendicitisDocumento4 páginasComplicated AppendicitisMedardo ApoloAinda não há avaliações
- Transanal Endorectal PullthroughDocumento8 páginasTransanal Endorectal PullthroughMuhammad Harmen Reza SiregarAinda não há avaliações
- Striktur UretraDocumento4 páginasStriktur UretramariamunsriAinda não há avaliações
- Transanal Extrusion of Ventriculoperitoneal Shunt in AdultDocumento7 páginasTransanal Extrusion of Ventriculoperitoneal Shunt in AdultMochi SaturnussAinda não há avaliações
- Pi Is 2213576614000049Documento3 páginasPi Is 2213576614000049Ditha FadhilaAinda não há avaliações
- perbaikan anastomosisDocumento6 páginasperbaikan anastomosisReagen DeAinda não há avaliações
- Laparoscopic Repair of Vesicovaginal FistulaDocumento4 páginasLaparoscopic Repair of Vesicovaginal FistulaGloria AteAinda não há avaliações
- Iatrogenic Injury To The Common Bile Duct: Case ReportDocumento3 páginasIatrogenic Injury To The Common Bile Duct: Case ReportGianfranco MuntoniAinda não há avaliações
- Togasj 6 25Documento6 páginasTogasj 6 25Prabowo SuryaningtyasAinda não há avaliações
- Article. Loop Ileostomy Closure After Restorative Proctocolectomy. Outcome in 1504 Patients. 2005Documento8 páginasArticle. Loop Ileostomy Closure After Restorative Proctocolectomy. Outcome in 1504 Patients. 2005Trí Cương NguyễnAinda não há avaliações
- 1 s2.0 S174391910700129X MainDocumento6 páginas1 s2.0 S174391910700129X MainGiorgio André Gabino GonzalezAinda não há avaliações
- Original Research ArticleDocumento9 páginasOriginal Research ArticleAnand ShanmugaiahAinda não há avaliações
- Anatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFDocumento10 páginasAnatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFannisa ussalihahAinda não há avaliações
- AchalasiaDocumento6 páginasAchalasiagabriel martinezAinda não há avaliações
- Main PDFDocumento4 páginasMain PDFhhAinda não há avaliações
- Laparoscopic Cholecystectomy:An Experience of 200 Cases: Original ArticleDocumento4 páginasLaparoscopic Cholecystectomy:An Experience of 200 Cases: Original ArticleAndrei GheorghitaAinda não há avaliações
- Indications and Complications of Intestinal Stomas - A Tertiary Care Hospital ExperienceDocumento4 páginasIndications and Complications of Intestinal Stomas - A Tertiary Care Hospital ExperienceOliviaAinda não há avaliações
- RectopexyDocumento7 páginasRectopexyInzamam Ul HaqAinda não há avaliações
- Open Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective StudyDocumento3 páginasOpen Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective Study'Adil MuhammadAinda não há avaliações
- Sotelo Et Al, Laparoscopic Rectovesical Fistula RepairDocumento5 páginasSotelo Et Al, Laparoscopic Rectovesical Fistula RepairjordynixnAinda não há avaliações
- Tau 06 03 510Documento7 páginasTau 06 03 510Eko NoviantiAinda não há avaliações
- Omentum overlay in laparoscopic treatment of umbilical and incisional herniasDocumento10 páginasOmentum overlay in laparoscopic treatment of umbilical and incisional herniasAlin MihetiuAinda não há avaliações
- Review StrikturDocumento13 páginasReview StrikturFryda 'buona' YantiAinda não há avaliações
- Case Report On Spontaneous Restoration of Bowel ContinuityDocumento5 páginasCase Report On Spontaneous Restoration of Bowel Continuityofficial.drjainAinda não há avaliações
- Complete Penile DisassemblyDocumento2 páginasComplete Penile DisassemblyGunduz AgaAinda não há avaliações
- Ms AJCRS 99757Documento6 páginasMs AJCRS 99757Cesar DominguezAinda não há avaliações
- Finally Ileal Ureter Corrected (1) (1) IbjuDocumento11 páginasFinally Ileal Ureter Corrected (1) (1) IbjuSheshang KamathAinda não há avaliações
- Laparoscopic Umbilical Hernia Repair Technique PapDocumento6 páginasLaparoscopic Umbilical Hernia Repair Technique PapEremeev SpiridonAinda não há avaliações
- Fundus First Laparoscopic Cholecystectomy Technique Reduces ComplicationsDocumento5 páginasFundus First Laparoscopic Cholecystectomy Technique Reduces ComplicationsRony RonyAinda não há avaliações
- Repair of Bowel Perforation Endoscopic State of The ArtDocumento6 páginasRepair of Bowel Perforation Endoscopic State of The ArtAthenaeum Scientific PublishersAinda não há avaliações
- Advanced Endoscopy Techniques: Jayant P.Talreja, M.D. Gastrointestinal Specialists, Inc. Bon Secours St. Mary's HospitalDocumento25 páginasAdvanced Endoscopy Techniques: Jayant P.Talreja, M.D. Gastrointestinal Specialists, Inc. Bon Secours St. Mary's HospitaldrelvAinda não há avaliações
- Perbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterDocumento7 páginasPerbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterAfiani JannahAinda não há avaliações
- Post Aua ReconstructivaDocumento14 páginasPost Aua ReconstructivaIndhira Sierra SanchezAinda não há avaliações
- Postoperative Management After Loop Ileostomy Closure: Are We Keeping Patients in Hospital Too Long?Documento5 páginasPostoperative Management After Loop Ileostomy Closure: Are We Keeping Patients in Hospital Too Long?shah hassaanAinda não há avaliações
- NeurogenicbladdermanagementwithcompleteurethraldistructionDocumento11 páginasNeurogenicbladdermanagementwithcompleteurethraldistructionPutri Rizky AmaliaAinda não há avaliações
- STL Approach for Small Bowel Atresia Repair: A ReviewDocumento5 páginasSTL Approach for Small Bowel Atresia Repair: A ReviewFebri Nick Daniel SihombingAinda não há avaliações
- Oesophagocoloplasty Outcomes for Corrosive StricturesDocumento12 páginasOesophagocoloplasty Outcomes for Corrosive StricturesSpandan KadamAinda não há avaliações
- Jurnal 1 PDFDocumento5 páginasJurnal 1 PDFsabila_chaAinda não há avaliações
- Pattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?Documento4 páginasPattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?neildamiAinda não há avaliações
- Wind2007 PDFDocumento5 páginasWind2007 PDFanatolioAinda não há avaliações
- Revision 2 32838Documento12 páginasRevision 2 32838chatarina anugrahAinda não há avaliações
- VVF RepairDocumento4 páginasVVF RepairAdil KhurshidAinda não há avaliações
- Incisional Hernia Mesh RepairDocumento5 páginasIncisional Hernia Mesh Repaireka henny suryaniAinda não há avaliações
- Mithun Journal-1 4Documento27 páginasMithun Journal-1 4Tanuja LAinda não há avaliações
- Hosseini2009 PDFDocumento6 páginasHosseini2009 PDFCeesar Nilthom Aguilar GuevaraAinda não há avaliações
- 30740632: Ileostomy Versus Fecal Diversion Device To Protect Anastomosis After Rectal Surgery A Randomized Clinical TrialDocumento9 páginas30740632: Ileostomy Versus Fecal Diversion Device To Protect Anastomosis After Rectal Surgery A Randomized Clinical TrialRicovially DavyaAinda não há avaliações
- Pattern of Acute Intestinal Obstruction Is There A PDFDocumento3 páginasPattern of Acute Intestinal Obstruction Is There A PDFMaría José Díaz RojasAinda não há avaliações
- 1 s2.0 S0022480423002895 MainDocumento7 páginas1 s2.0 S0022480423002895 Mainlucabarbato23Ainda não há avaliações
- Cutaneous Needle Aspirations in Liver DiseaseDocumento6 páginasCutaneous Needle Aspirations in Liver DiseaseRhian BrimbleAinda não há avaliações
- Endosponge Treatment Anaspomotis LeakageDocumento5 páginasEndosponge Treatment Anaspomotis LeakagepalfiataAinda não há avaliações
- Trans-Fistulary Endoscopic Drainage For Post-Bariatric Abdominal Collections Communicating With The Upper Gastrointestinal TractDocumento8 páginasTrans-Fistulary Endoscopic Drainage For Post-Bariatric Abdominal Collections Communicating With The Upper Gastrointestinal TractAlexandra JichituAinda não há avaliações
- Closure of Loop Ileostomy Potentially ADocumento7 páginasClosure of Loop Ileostomy Potentially Ashah hassaanAinda não há avaliações
- Palliative Management of Malignant Rectosigmoidal Obstruction. Colostomy vs. Endoscopic Stenting. A Randomized Prospective TrialDocumento4 páginasPalliative Management of Malignant Rectosigmoidal Obstruction. Colostomy vs. Endoscopic Stenting. A Randomized Prospective TrialMadokaDeigoAinda não há avaliações
- Complications of Enterocystoplastycase SeriesDocumento5 páginasComplications of Enterocystoplastycase SeriesIJAR JOURNALAinda não há avaliações
- Management of Anastomotic Leaks After Esophagectomy and Gastric Pull-UpDocumento9 páginasManagement of Anastomotic Leaks After Esophagectomy and Gastric Pull-UpSergio Sitta TarquiniAinda não há avaliações
- 2014 172 0 Retroperitoneal and Retrograde Total Laparoscopic Hysterectomy As A Standard Treatment in A Community Hospital 97 101 1Documento5 páginas2014 172 0 Retroperitoneal and Retrograde Total Laparoscopic Hysterectomy As A Standard Treatment in A Community Hospital 97 101 1Sarah MuharomahAinda não há avaliações
- 1 Salim TahirhvDocumento4 páginas1 Salim TahirhvTajudin SuryaAinda não há avaliações
- Post-cholecystectomy Bile Duct InjuryNo EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorAinda não há avaliações
- Percutaneous Surgery of the Upper Urinary Tract: Handbook of EndourologyNo EverandPercutaneous Surgery of the Upper Urinary Tract: Handbook of EndourologyPetrisor Aurelian GeavleteNota: 5 de 5 estrelas5/5 (1)
- Maxillary FX Pic MDocumento58 páginasMaxillary FX Pic MabhishekbmcAinda não há avaliações
- Delfi Spec LimbProtectionSleeveDocumento2 páginasDelfi Spec LimbProtectionSleeveabhishekbmcAinda não há avaliações
- Z Plasty - VariationsDocumento7 páginasZ Plasty - VariationsabhishekbmcAinda não há avaliações
- Burnout Syndrome Among Dental Students: A Short Version of The "Burnout Clinical Subtype Questionnaire " Adapted For Students (BCSQ-12-SS)Documento11 páginasBurnout Syndrome Among Dental Students: A Short Version of The "Burnout Clinical Subtype Questionnaire " Adapted For Students (BCSQ-12-SS)abhishekbmcAinda não há avaliações
- 3M Donor SiteDocumento6 páginas3M Donor SiteabhishekbmcAinda não há avaliações
- Hand Burns Treatment Goals and UnknownsDocumento42 páginasHand Burns Treatment Goals and UnknownsabhishekbmcAinda não há avaliações
- Cuadra AlvaroDocumento7 páginasCuadra AlvaroabhishekbmcAinda não há avaliações
- View Doc 635470672036959908Documento6 páginasView Doc 635470672036959908abhishekbmcAinda não há avaliações
- Burns Free Flap Systematic ReviewDocumento12 páginasBurns Free Flap Systematic ReviewabhishekbmcAinda não há avaliações
- Gall Stone SpillageDocumento6 páginasGall Stone SpillageabhishekbmcAinda não há avaliações
- POSASv2 0 ObserverScale EN1Documento1 páginaPOSASv2 0 ObserverScale EN1abhishekbmcAinda não há avaliações
- Silk DressingDocumento13 páginasSilk DressingabhishekbmcAinda não há avaliações
- 3ftfbsdi "Sujdmf $pnqbsjtpo PG) JQQPDBNQBM 7Pmvnf Jo %fnfoujb 4vcuzqftDocumento5 páginas3ftfbsdi "Sujdmf $pnqbsjtpo PG) JQQPDBNQBM 7Pmvnf Jo %fnfoujb 4vcuzqftabhishekbmcAinda não há avaliações
- Aps 39 397Documento7 páginasAps 39 397abhishekbmcAinda não há avaliações
- 440 FullDocumento8 páginas440 FullabhishekbmcAinda não há avaliações
- Wo ArticleDocumento13 páginasWo ArticleabhishekbmcAinda não há avaliações
- 220 228Documento9 páginas220 228abhishekbmcAinda não há avaliações
- ReviewDocumento8 páginasReviewabhishekbmcAinda não há avaliações
- Blunt Trauma PancreasDocumento5 páginasBlunt Trauma PancreasabhishekbmcAinda não há avaliações
- 3Fwjfx "Sujdmf &BSMZ %jbhoptjt PG (Bmmcmbeefs $bsdjopnb "O "Mhpsjuin "QqspbdiDocumento6 páginas3Fwjfx "Sujdmf &BSMZ %jbhoptjt PG (Bmmcmbeefs $bsdjopnb "O "Mhpsjuin "QqspbdiabhishekbmcAinda não há avaliações
- Cystic ThyroidDocumento4 páginasCystic ThyroidabhishekbmcAinda não há avaliações
- Obg Extra EdgeDocumento201 páginasObg Extra EdgeabhishekbmcAinda não há avaliações
- Fournier S GangreneDocumento8 páginasFournier S GangreneabhishekbmcAinda não há avaliações
- 2005 Jaime NNDocumento10 páginas2005 Jaime NNabhishekbmcAinda não há avaliações
- Abdominal X RayDocumento64 páginasAbdominal X RayabhishekbmcAinda não há avaliações
- All India Post Graduate Medical Entrance Exam ForumsDocumento57 páginasAll India Post Graduate Medical Entrance Exam ForumsabhishekbmcAinda não há avaliações
- Abdominal X RayDocumento64 páginasAbdominal X RayabhishekbmcAinda não há avaliações
- Fluid and Electrolyte Management PDFDocumento10 páginasFluid and Electrolyte Management PDFbalab2311Ainda não há avaliações
- 300Documento36 páginas300abhishekbmc100% (1)
- PHYSIOLOGY OF THYROID GLANDDocumento9 páginasPHYSIOLOGY OF THYROID GLANDAbby EvangelistaAinda não há avaliações
- DengueDocumento5 páginasDengueSam Angelo EstrellaAinda não há avaliações
- Research PaperDocumento5 páginasResearch PaperLyn Niño100% (1)
- Hygiene Code of PracticeDocumento4 páginasHygiene Code of PracticeLouis ManaloAinda não há avaliações
- Family Nursing Care PlanDocumento27 páginasFamily Nursing Care Planshayne_peroAinda não há avaliações
- Human Rabies in The PhilippinesDocumento2 páginasHuman Rabies in The PhilippinesAngeli SoabasAinda não há avaliações
- Alice in Wonderland SyndromeDocumento6 páginasAlice in Wonderland SyndromeNilly NagyAinda não há avaliações
- Test Your Knowledge About Pneumonia - ProProfs QuizDocumento8 páginasTest Your Knowledge About Pneumonia - ProProfs QuizNaresh Kumar SoniAinda não há avaliações
- GF 689 Poverty and HealthDocumento4 páginasGF 689 Poverty and HealthTowardinho14Ainda não há avaliações
- A 25yr Old Male Presented With Skin Rash Involving Both Hands and Feet For 2 DaysDocumento234 páginasA 25yr Old Male Presented With Skin Rash Involving Both Hands and Feet For 2 DaysAli LashhabAinda não há avaliações
- Pigeon Disease - The Eight Most Common Health Problems in PigeonsDocumento2 páginasPigeon Disease - The Eight Most Common Health Problems in Pigeonscc_lawrence100% (1)
- Chapter 20 HomeworkDocumento9 páginasChapter 20 HomeworkKvn4N6Ainda não há avaliações
- An Overview of Therapeutic Plasma ExchangeDocumento65 páginasAn Overview of Therapeutic Plasma ExchangesayednourAinda não há avaliações
- 61 - SPIN - JRP Full Proposal Incl Projects 1-5Documento117 páginas61 - SPIN - JRP Full Proposal Incl Projects 1-5KiranaR.RirihAinda não há avaliações
- Definition of Death and DyingDocumento3 páginasDefinition of Death and DyingacelestscribdAinda não há avaliações
- Long Test 10Documento2 páginasLong Test 10Jerome ManabatAinda não há avaliações
- Facial Nerve Paralysis 2Documento44 páginasFacial Nerve Paralysis 2Omowole GbengaAinda não há avaliações
- Carbapenamses in Antibiotic ResistanceDocumento53 páginasCarbapenamses in Antibiotic Resistancetummalapalli venkateswara raoAinda não há avaliações
- Cavernous Sinus Thrombosis ..Documento4 páginasCavernous Sinus Thrombosis ..DReKA2010Ainda não há avaliações
- Industry Paper On The Activities of Amusement Parks and Theme Parks in The PhilippinesDocumento14 páginasIndustry Paper On The Activities of Amusement Parks and Theme Parks in The PhilippinesHeina LyllanAinda não há avaliações
- Roll Back MalariaDocumento2 páginasRoll Back Malariaapi-3705046Ainda não há avaliações
- St. Scholastica’s Academy – Tabunok Case Study on GonorrheaDocumento19 páginasSt. Scholastica’s Academy – Tabunok Case Study on GonorrheaErika ThereseAinda não há avaliações
- Tarika Clinical Trial For ACNEDocumento5 páginasTarika Clinical Trial For ACNEnsin536Ainda não há avaliações
- The Magic of Honey and It's Many UsesDocumento8 páginasThe Magic of Honey and It's Many UsesSShaAinda não há avaliações
- MSH/TML Parasitology Manual ProceduresDocumento147 páginasMSH/TML Parasitology Manual Proceduresvachhanikapil100% (1)
- 2 Comparacion BD Phoenix Vitek MicroscanDocumento10 páginas2 Comparacion BD Phoenix Vitek MicroscanBenjamin MendozaAinda não há avaliações
- @MedicalBooksStore 2012 (ERS Monograph) TuberculosisDocumento271 páginas@MedicalBooksStore 2012 (ERS Monograph) TuberculosisHeri GunawanAinda não há avaliações
- Congenital Ptosis - GenetikaDocumento28 páginasCongenital Ptosis - GenetikaJohanes Arie SetiawanAinda não há avaliações
- Scabies by DR Najeeb Memon PakistanDocumento39 páginasScabies by DR Najeeb Memon Pakistanmnajeeb807196Ainda não há avaliações
- Eur Heart J 2016 Roffi 267 315Documento59 páginasEur Heart J 2016 Roffi 267 315Putu Reza Sandhya PratamaAinda não há avaliações