Escolar Documentos
Profissional Documentos
Cultura Documentos
Oral Hydration Management Guideline Final
Enviado por
api-253451161Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Oral Hydration Management Guideline Final
Enviado por
api-253451161Direitos autorais:
Formatos disponíveis
University of Colorado Hospital Nursing Practice Guideline
12
th
Floor Medicine/AC Unit! "ral Hydration Manage#ent
$elated Policies and Procedures!
Assessment of Adult Patients at Risk for Aspiration
Approved %y!
Acute Care of the Elderly Leadership Team
Acute Care of the Elderly Nurse Manager
Acute Care for the Elderly Service Medical irector
!eriatric Leadership Committee
N"C#E Committee
Nursing Practice !uidelines Su$committee
ffective! %&'(%)*
&escription! This guideline provides detailed information on hydration
management for the geriatric population+ "t identifies potential complications, risk
factors, ho- to assess for dehydration, and nursing interventions+ This guideline -as
developed to help nurses and nursing assistants provide geriatric sensitive care to prevent
dehydration+
Accounta%ility! The clinical nursing staff involved -ith the care of patients is
responsi$le for the management of the patient.s hydration status+
&efinitions!
ACP! Advanced Care Partner
'M(! /ody Mass "nde0
'UN! /lood 1rea Nitrogen
CNA! Certified Nursing Assistant
&ehydration! depletion of total $ody -ater of more than 23 due to pathologic fluid
losses, reduced -ater intake, or a com$ination of $oth+
H$! Electronic #ealth Record
()"! "ntake and 4utput
NP"! Nil Per 4s, nothing $y mouth
*'+! Total /ody 5ater accounts for a percent of an adult.s $ody -eight and consists of
intracellular and e0tracellular fluid compartments+
$N! Registered Nurse
Practice Guidelines!
A, Co#plications
)+ ehydration presents an increased risk for renal failure, decu$itus ulcers,
constipation, urinary tract infections, medication to0icity, deep vein
throm$osis, myocardial ischemia, respiratory infections, acute confusion,
diminished muscle strength, and falls+
', $is- Factors
)+ Age6related physiological changes
a+ ecrease in T/5, altered thirst sensation, effectiveness of
vasopressin, impaired kidney function 7conservation of -ater, urine
concentration8
(+ emographics
a+ Age 9 :; or female, /M" <() or =(&
2+ Medications
a+ >our or more medications, medications that increase fluid loss
7diuretics, la0ative8, sedating medications that decrease a$ility to
o$tain fluid, medications that dull the thirst response 7antipsychotics8
*+ Medical conditions
a+ Cognitive deficits 7such as, dementia, delirium, Al?heimer.s8,
depression, thrush or oral mucositis, infection, hyperglycemia, four or
more chronic conditions, malnutrition, history of dehydration, nausea
and vomiting, increased diaphoresis, prolonged NP4 status prior to
procedure or test
;+ >unction
a+ ependencies in eating and drinking, immo$ility, refusal to drink due
to concern a$out incontinence, s-allo-ing disorders, ill6fitting
dentures, poor dentation
C, Assess#ent
)+ Recommended tools
a+ ehydration Risk Appraisal Checklist
i+ This tool calculates risk for dehydration $y looking at personal
factors, health conditions, medications, oral intake $ehaviors,
and la$oratory indicators+ Risk level is determined $y the
num$er of characteristics that apply+
ii+ See Appendi0 )
$+ Types of hydration pro$lems and suggested strategies
i+ This ta$le identifies different oral hydration ha$its -ith a point
system and strategies to prevent dehydration+ There are four
main categories and under the main categories are
su$categories@ Can rink 7"ndependent, >orgets8, Can.t rink
7ysphagia, Physically ependent8, 5on.t rink 7Sipper,
>ears "ncontinence8 and End of Life+
ii+ See Appendi0 (
(+ #ealth history
a+ Assess patients medical history of disease that put patient at risk for
dehydration, num$er of prescription drugs, past history of dehydration
or repeated infections
2+ Physical
a+ Aital signs@ hypotension, orthostatic hypotension, tachycardia, fever,
-eak Bthready. pulse, increased respirations
$+ 5eight@ acute -eight loss
c+ Neurological@ altered mental status, speech difficulties, lethargy,
muscle -eakness
d+ Skin@ dry and tenting sternal skin turgor, increased capillary refill time,
cool peripheries
e+ Eyes, Mouth@ dry and pale mucous mem$ranes, decreased saliva,
longitudinal furro-s on tongue, sunken eyes
f+ !astrointestinal '!enitourinary@ vomiting, diarrhea, decreased urine
output, urine color, net "C4
*+ iagnostic
a+ La$s@ 5hen revie-ing la$s look for an increase in urine6specific
gravity, /1N, creatinine, hematocrit, serum sodium, /1N'creatinine
ratio, serum osmolality, and changes in electrolytes+
&, Nursing Care .trategies
)+ ocument
a+ "ntake and output as directed per order 7D:#, D*#, Strict, Accurate8
$+ "ntake
i+ Record patient.s intake in E#R+ Calculate fluid intake $y the
e0act volume of container+ Refer to nutrition room -here three
different cups have measured volume+ Record food intake $y
percentage eaten+
ii+ ocument amount of intake volume upon completion of
container
iii+ "dentify patient.s a$ility to eat'drink and record in E#R for
feeding assistance under intake as either independent, moderate
assist, total assist, or )@) supervision+
c+ 4utput
i+ Continent'rains@ 1se hat in toilets or commode to accurately
measure outputE use cylinder to measure drain'foley output+
ii+ "ncontinent@ 1se prompted voiding to prevent incontinence+
>or incontinent episodes record in E#R as an occurrence+
iii+ Assess and document urine color, appearance and odor+
ocument stool assistance, appearance, color, amount, and
source+
(+ Communicate and educate
a+ Report to CNAs'ACPs patient.s feeding and drinking function and
needs, orders for "C4s freFuency, types of hydration pro$lems and
strategies+ Revie- CNA report sheet to ensure accurate "C4 status
$+ Reinforce need for oral care especially for patients -ith dysphagia and
NP4 status
c+ ocument intake of fluids upon completion of container
d+ Educate patients and families of current diet order, the importance of
hydration, the risk associated -ith increased age, and daily intake goal+
"nvolve family mem$ers'friends in encouraging the patient to drink
and eat+ Suggest the family mem$ers leave a list of $everages and
foods the patient likes to eat and drink if patient is una$le to do so+
e+ Contact doctor if patient.s diet order is NP4 to clarify -hen test is and
if it is necessary+
f+ 1sing the 1C# !eriatric Medicine Admission order set encourage
doctor include order Gminimum liFuids (;%mL P4 routine * times
dailyH
2+ "ncrease fluids
a+ "f no fluid restrictions are ordered on a patient, calculate recommended
daily fluid intake $y using recommended tool -hich is for older adults
-ho are hospitali?ed+
$+ Assess patient.s capacity for independent feeding@ conduct RN
$edside s-allo- screening, o$serve patient eating different types of
food and drinks using different modalities 7e+g+ stra-s, mugs, lids8+
c+ 1se modified fluid containers $ased on assessment of patient.s
capacity to hold cup and s-allo-+
d+ Assess need for change in diet consistency $ased upon patient.s
dentation, denture use, or patient.s preference
e+ Encourage fluid rich foods
f+ Suggest nutrition consult for patients needing supplements -ith or
$et-een meals or calorie count+
g+ "f appropriate for patient order room service -ith assistance so a
nutrition assistant can help patient order meals
h+ uring medication administration encourage patient to drink fluids+
i+ Make drinks availa$le+ o fluid rounds in mid6morning and late
afternoon to provide additional fluid in $et-een meals+ 4ffer a variety
of drinks+ Assess -hat patient prefers to drink and temperature+
Replenish and refresh drinks
I+ CNA fluid rounds at $eginning of shift 7%J2%, ):2%8 to remove and
record multiple or empty cups+ Replace -ith fresh -ater+
k+ Ensure patient is a$le to reach food and $everage
l+ "ncorporate s-allo-ing e0ercises if appropriate
m+ 1se visual reminders such as poster or note on patient -hite$oard to
encourage fluid intake
n+ Assess patients. diet and encourage GTea TimeH to increase fluid
intake+ 4n days that GTea TimeH is not offered provide patient -ith
options of $everages and snack in the afternoon+
Calculation
1//#l//-g for first 1/-g of 0eight
1/#l/-g for ne2t 1/-g of 0eight
11#l/-g for the re#aining 0eight
2a#ple
Patient weighting 73 kg
)%%ml')%kg6 )%%%
;%ml')%kg6 ;%%
);ml';2kg6 &K;
Calculated recommended daily fluid intakeL ((K;ml
Appendi2 1
&ehydration $is- Appraisal Chec-list
3 =:; years 3 /M" <() or =(&
3 >emale M/M"L -eight 7kg8'height 7m8
(
N
.ignificant Health Conditions/.ituations
3 ementia' Oscreen for cognitive impairment 3 Renal isease
3 epression' Oscreen for depression 3 Cardiac Arrhythmias
3 CAA 3 Malnutrition
3 ia$etes 3 #istory of dehydration
3 1rinary "ncontinence 3 #istory of repeated infections
3 MaIor Psychiatric isorders 3 9 * chronic health conditions
3 Aomiting 3 >ever
3 NP4 status 3 iarrhea
Medications
3 4* medications 3 iuretics
3 La0atives 3 Psychotropics@ Antipsychotics,
3 Steroids Antidepressants, An0iolytics
3 ACE inhi$itors
(nta-e 'ehaviors
3 ReFuires assistance to drink 3 Semi6dependent -ith feeding
3 #as difficulty s-allo-ing' Chokes 3 >luid intake of <);%%ml'day
3 Can drink independently $ut forgets 3 Spills
3 Poor eater 7eats <;%3 of food8 3 Receives tu$e feedings
3 Receiving "A fluid therapy 3 #olds food'fluid in mouth
3 rools 3 Spits out food'fluid
5a%oratory (ndicators
3 1rine specific gravity =)+%(% 3 Serum sodium =);%meF'L
3 1rine color dark yello- =* 3 Serum osmolality =2%%mmol'Pg
3 /1N'Creatinine = (%@) 3 #ematocrit = normal
ate of Assessment@ QQQQQQQQQQQQQQQQQQQQQQQQQQQ Assessor@QQQQQQQQQQQQQQQQQQQQQQ
(nstructions!
The information on this form may $e collected from direct
o$servation, from chart revie-, or from MS information that has
$een collected+ Many of the items on this checklist have MS
identifiers ne0t to them reflecting that information from MS can $e
used to complete this checklist+ The total num$er of risk factors should
$e totaled+ The higher the num$er of risk factors checked, the higher
the risk for hydration pro$lems+ Please check all that apply+
Addressograph
References@
Mentes, R+C+ C The "o-a Aeterans Affairs Nursing Research Consortium 7(%%*8 Evidence-Based Practice Guideline: Hydration
management."o-a City, "A@ The 1niversity of "o-a !erontological Nursing "nterventions Research Center Research Translation
and issemination Core+
Mentes, R+C+ C The "o-a Aeterans Affairs Nursing Research Consortium+ 7(%%%8+ #ydration management+ Journal o
Gerontological !ursing" J6);+
(ndependent
7n L &8
l
Educate@
#o- much
l
1se
graduated
cup
l
Provide
preferred
$everages
Forgets
&8 n L 7
l
>reFuent
offers
l
>luid during
activities
l
Teatime'
happy
hours
l
/everage
cart
&ysphagic
7n L &8
l
S-allo-ing
e0ercises
l
>oods rich
in fluid,
smoothies
l
4ral care
l
Educate
family to
help
Physically
&ependent
7n L J8
l
Sports cup
-ith stra-
l
Physical
aids to
assist -ith
drinking
Fears
(ncontinence
7n L (8
l
Educate
a$out
maintaining
fluid intake
l
Pegels, urge
inhi$ition
l
Medication
as last resort
.ipper
7n L ;8
l
>reFuent
small
amounts
at each
contact
l
>luid -ith
activities
l
Provide
preferred
$everages
l
Resident
and family
preference
l
Advance
directive
*ypes of hydration pro%le#s
#an $rink
n L )*
%on&t $rink
n L &
#an&t $rink
n L )2
End o 'ie
n L )
Appendi2 2
$eferences!
Collins, M+, C Claros, E+ 7(%))8+ Recogni?ing the face of dehydration+ !ursing, ()7:8, (J62)+
L4E &
!odfrey, #+, Cloete, R+, ymond, E+, C Long, A+ 7(%)(8+ An e0ploration of the hydration care of
older people@ A Fualitative study+ *nternational Journal o !ursing +tudies, (,, )(%%6)())+ L4E
J
Mentes, R+, C Culp, P+ 7(%%28+ Reducing hydration6linked events in nursing home residents+
#linical !ursing -esearch, ).728, ()%6((;+ L4E 2
Mentes, R+, C Pang, S+ 7(%)28+ Evidence6$ased practice guideline@ #ydration management+
Journal o Gerontological !ursing, 3,7(8, ))6)K+ L4E &
Ru0ton, C+ 7(%)(8+ Promoting and maintaining healthy hydration in patients+ !ursing +tandards,
./72)8, ;%6;J+ L4E :
5otton, P+, Crannitch, P+, C Munt, R+ 7(%%:8+ Prevalence, risk factors and strategies to prevent
dehydration in older adults+ #ontem0orary !urse, 3)7)8, **6;J+ L4E :
Você também pode gostar
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (120)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
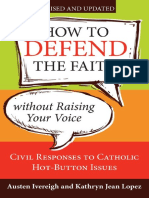
- How To Defend The Faith Without Raising Your VoiceDocumento139 páginasHow To Defend The Faith Without Raising Your VoiceCleber De Souza Cunha100% (2)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Mil-Std-1949a NoticeDocumento3 páginasMil-Std-1949a NoticeGökhan ÇiçekAinda não há avaliações
- Mpez-6 Installation Manual - Inline 201007Documento8 páginasMpez-6 Installation Manual - Inline 201007api-244989438Ainda não há avaliações
- Deductions From Gross IncomeDocumento2 páginasDeductions From Gross Incomericamae saladagaAinda não há avaliações
- Hotel Transportation and Discount Information Chart - February 2013Documento29 páginasHotel Transportation and Discount Information Chart - February 2013scfp4091Ainda não há avaliações
- Mock Test MCQ 2017Documento18 páginasMock Test MCQ 2017Alisha ChopraAinda não há avaliações
- Transdermal Nano BookDocumento44 páginasTransdermal Nano BookMuhammad Azam TahirAinda não há avaliações
- Bonding and Adhesives in DentistryDocumento39 páginasBonding and Adhesives in DentistryZahn ÄrztinAinda não há avaliações
- Group Interative Art TherapyDocumento225 páginasGroup Interative Art TherapyRibeiro CatarinaAinda não há avaliações
- Time Sheets CraneDocumento1 páginaTime Sheets CraneBillie Davidson100% (1)
- Letter of Rec - Melissa MDocumento2 páginasLetter of Rec - Melissa Mapi-253451161Ainda não há avaliações
- Level III Clinical NarrativeDocumento5 páginasLevel III Clinical Narrativeapi-253451161Ainda não há avaliações
- Level III Resume - FinalDocumento2 páginasLevel III Resume - Finalapi-253451161Ainda não há avaliações
- Jan - Letter of RecDocumento2 páginasJan - Letter of Recapi-253451161Ainda não há avaliações
- Recognition - Ed EmailDocumento2 páginasRecognition - Ed Emailapi-253451161Ainda não há avaliações
- NgnamembershipcardDocumento1 páginaNgnamembershipcardapi-253451161Ainda não há avaliações
- Pall Care AttendanceDocumento2 páginasPall Care Attendanceapi-253451161Ainda não há avaliações
- Communication With KatieDocumento2 páginasCommunication With Katieapi-253451161Ainda não há avaliações
- Niche Conference CeDocumento1 páginaNiche Conference Ceapi-253451161Ainda não há avaliações
- 1 Patient Questionnaire - CleanDocumento2 páginas1 Patient Questionnaire - Cleanapi-253451161Ainda não há avaliações
- StaffDocumento1 páginaStaffapi-253451161Ainda não há avaliações
- Thank You - DesiDocumento1 páginaThank You - Desiapi-253451161Ainda não há avaliações
- Palliative Care CommunicationDocumento5 páginasPalliative Care Communicationapi-253451161Ainda não há avaliações
- Prepost Sleep PPDocumento31 páginasPrepost Sleep PPapi-253451161Ainda não há avaliações
- Quality of Sleep Patients Get in The Hospital - PP Pre Autosaved AutosavedDocumento20 páginasQuality of Sleep Patients Get in The Hospital - PP Pre Autosaved Autosavedapi-253451161Ainda não há avaliações
- Quiet at Night - Implementing A Nightingale PrincipleDocumento9 páginasQuiet at Night - Implementing A Nightingale Principleapi-253451161Ainda não há avaliações
- Employee Ce RecordDocumento1 páginaEmployee Ce Recordapi-253451161Ainda não há avaliações
- 1 24 14 1 30 13 Car - Live FlyerDocumento1 página1 24 14 1 30 13 Car - Live Flyerapi-253451161Ainda não há avaliações
- Focus Pdca Revised 3Documento2 páginasFocus Pdca Revised 3api-253451161Ainda não há avaliações
- MCQ Cell InjuryDocumento19 páginasMCQ Cell InjuryMoaz EbrahimAinda não há avaliações
- App Guide EntelliGuard - G 09 - 2020 AplicacionDocumento100 páginasApp Guide EntelliGuard - G 09 - 2020 AplicacionjeorginagAinda não há avaliações
- Chapter 3.2 Futures HedgingDocumento19 páginasChapter 3.2 Futures HedginglelouchAinda não há avaliações
- Purpose in Life Is A Robust Protective Factor of Reported Cognitive Decline Among Late Middle-Aged Adults: The Emory Healthy Aging StudyDocumento8 páginasPurpose in Life Is A Robust Protective Factor of Reported Cognitive Decline Among Late Middle-Aged Adults: The Emory Healthy Aging StudyRaúl AñariAinda não há avaliações
- Sialoree BotoxDocumento5 páginasSialoree BotoxJocul DivinAinda não há avaliações
- Theoretical Background: Theories Relevance To The Study SourcesDocumento3 páginasTheoretical Background: Theories Relevance To The Study SourcesAdelfa Mae BerdonAinda não há avaliações
- TextDocumento3 páginasTextKristineAinda não há avaliações
- Pentacon Six-02Documento28 páginasPentacon Six-02Melissa Moreira TYAinda não há avaliações
- Quotation: Kentex CargoDocumento2 páginasQuotation: Kentex CargoMalueth AnguiAinda não há avaliações
- Differential Partitioning of Betacyanins and Betaxanthins Employing Aqueous Two Phase ExtractionDocumento8 páginasDifferential Partitioning of Betacyanins and Betaxanthins Employing Aqueous Two Phase ExtractionPaul Jefferson Flores HurtadoAinda não há avaliações
- Ppr.1 Circ.5 Gesamp Ehs ListDocumento93 páginasPpr.1 Circ.5 Gesamp Ehs ListTRANAinda não há avaliações
- Paes 406Documento12 páginasPaes 406Denver LangahinAinda não há avaliações
- ត្នោត (Borassus flabellifer L.)Documento11 páginasត្នោត (Borassus flabellifer L.)yeangdonalAinda não há avaliações
- What Is An Engineering Change OrderDocumento3 páginasWhat Is An Engineering Change OrderKundan Kumar MishraAinda não há avaliações
- Case Study of Flixborough UK DisasterDocumento52 páginasCase Study of Flixborough UK Disasteraman shaikhAinda não há avaliações
- 3M Window Film PR SeriesDocumento3 páginas3M Window Film PR SeriesPhan CrisAinda não há avaliações
- Protein Metabolism and Urea Recycling in Rodent HibernatorsDocumento5 páginasProtein Metabolism and Urea Recycling in Rodent HibernatorsBud Marvin LeRoy RiedeselAinda não há avaliações
- Review Dynamic Earth CoreScienceDocumento3 páginasReview Dynamic Earth CoreScienceVikram BologaneshAinda não há avaliações
- Public Speaking ScriptDocumento2 páginasPublic Speaking ScriptDhia MizaAinda não há avaliações
- Lpalmer ResumeDocumento4 páginasLpalmer Resumeapi-216019096Ainda não há avaliações