Escolar Documentos
Profissional Documentos
Cultura Documentos
Animal Toxins
Enviado por
ShaziaAshraf0 notas0% acharam este documento útil (0 voto)
27 visualizações13 páginasProject on Animal Toxins
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoProject on Animal Toxins
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
27 visualizações13 páginasAnimal Toxins
Enviado por
ShaziaAshrafProject on Animal Toxins
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 13
NATIONAL UNIVERSITY OF
ADVANCED LEGAL STUDIES
Medical Jurisprudence Project
ANIMAL TOXINS
Shazia Bint Ashraf
Roll no. 624
8
th
Semester
SNAKE BITE
Snake bite is common life-threatening in many countries. Farmers, hunters, rice-
pickers are at particular risk. Prompt medical treatment is vital. 3-5 million victims
/year, 50 000 deaths, 400 000 amputations. 40% of bites do not produce signs of
envenoming. It is difficult to predict which bites will produce symptoms or the
clinical outcome; all victims should be brought under medical care as quickly as
possible. Poisonous species of snake fall into the families. Snake venoms are
complex mixtures of proteins & small polypeptides with enzymatic activity. Snake
venoms are neurotoxins, haematotoxins (haemorrhagic or coagulopathic) or
cardiotoxins etc.
Characteristic Poisonous Non-poisonous
a. Shape of head triangular round
b. Pit (+) (-)
c. Pupils elliptical Round
d. Bite marks Fang marks 2 rows of teeth
e. Caudal plates Single row Double row
f. Color body
Red ring next to yellow
(coral snakes)
Alternating color
The venom is detected from a dry swab of the bite site using monoclonal antibody
techniques. The 20-minute whole blood-clotting test is a useful bedside tool in
remote areas; a 2-3 ml sample of venous blood from the victim is left undisturbed at
ambient temperature for at least 20 minutes. The vessel containing the blood is then
tipped once & may be compared with a normal control. If it has not clotted, there is
haemostatic disturbance from systemic envenoming. All patients should have a full
blood count, urea/electrolytes, liver function tests, creatine kinase, troponins, ECG.
EFFECTS OF DIFFERENT TYPES OF TOXINS
MANAGEMENT OF SNAKE BITES
Reassuring the patient
Immobilizing the bitten area to minimize venom spread
Identifying the snake.
Application of a firm bandage to occlude lymphatic drainage is appropriate,
but tourniquets are unhelpful since they do not prevent the spread of venom &
frequently applied incorrectly.
Incisions at the bite site &attempts to suck out the venom by mouth should
not be made.
A large-bore IV cannula inserted on an unaffected limb.
BP, coagulation, renal, neurological, cardio respiratory status must be
monitored, as hypotension, anaphylactic shock, renal failure, respiratory
distress may develop rapidly.
All patients with suspected envenoming should be observed for 12-24 hours,
as the initial manifestations may be delayed, especially with elapid bites.
Pain/vomiting should be managed symptomatically.
Aspirin should not be used, it may aggravate bleeding.
In severe coagulopathy with thrombocytopenia causing DIC, large quantities
of fresh frozen plasma, cryoprecipitate , platelets are required if the response
to antivenin is poor.
The most appropriate therapy is timely administration of the species-
appropriate antivenin when indications.
Before starting antivenin, ask about history of allergy & intradermal sensitivity
test performed by injecting 0.02 ml of saline-diluted antiserum at a site
distant from the bite.
The injured site is observed for at least 10 minutes for the redness, hives,
pruritus or other adverse effects.
The shorter the interval between injured & reaction, the greater the degree of
sensitivity.
0.5 ml 1:1000 adrenaline must be available when antivenin given
A negative skin test does not rule out a reaction following administration of
the full antivenin dose.
The rate antivenin should be based on the severity of the case& the patient's
tolerance to the antivenin.
The entire initial dose should be given as soon as possible within 4 hours of
the bite.
In severe envenoming, antivenin given up to 24 hours after the bite has been
shown to reverse coagulation deficits.
SPIDER BITES
I. Lactrodectus spiders (Black Widow)
Worldwide
female: black color w/ a distinctive red ventral marking w/ hourglass
shape
Nocturnal spider; bites defensively
Has neurotoxin venom
Act at presynaptic terminal
Enhance neurotransmitter release
Acetylcholine = neuromuscular junction (muscle spasm)
Norepinephrine = produces adrenergic stimulation
Manifestation:
Erythema & pain at bite site
Neuromuscular symptoms (30mins)
Severe pain & spasm of large muscle group
1. Abdominal cramps
2. Dyspnea (chest tightness)
Adrenergic stimulation:
1. HPN / diaphoresis / tachycardia
2. Fasciculation / Nausea/vomiting
3. Headache / paresthesia / fatigue / salivation
Acute symptoms peak several hours & resolve in 1-2 days
Death unusual
Treatment:
a. Mild envenomation
Local wound care:
Clean the site
Apply ice to alleviate pain
tetanus prophylaxis
b. Severe envenomation
- IV calcium gluconate (transient effect)
- Narcotic & benzodiazepine - relieve muscle pain
- Antivenin (horse serum) reserve for severe envenomation due
to anaphylaxis & serum sickness (side effect)
- Antivenum is recommended:
Pregnant women
Children under 16 yrs
Patients w/ severe reaction:
a. Uncontrolled HPN
b. Respiratory distress
c. Seizures
- Skin testing = if (+) should. Receive pretx w/ diphenhydramine.
- Recommended antivenin dose = 1 vial, repeated as necessary
SCORPION STINGS
Scorpions are the most important venomous animals after snakes. Most scorpion
species produce venom which causes only minor local reactions in humans, but in
Mexico, Tunisia, Algeria, Morocco, Libya scorpion stings are a serious health hazard.
Scorpions do not attack humans & escape when disturbed. Stings occur after a
person accidentally steps on or involuntarily presses the scorpion (when it is trapped
inside shoes or clothes) or when reaching under dead wood or stones. Clothes / shoes
need to be inspected closely & shaken& sitting or sleeping places checked when
camping in rural districts where scorpions are common.
Some scorpions have neurotoxins that prevent sodium channel closure. Cranial
nerves & neuromuscular dysfunction are caused which result in respiratory distress
in the bite victim.
Treatment:
Local:
Ice pack therapy / analgesic -> for pain
Tetanus prophylaxis
Systemic:
Monitor closely cardiovascular & respiratory status in ICU
Antivenin can reverses cranial nerve & neuromuscular symptoms but can
cause anaphylaxis & delayed serum sickness
BEE STINGS
The term bee here, includes Honeybee, bumble bee, black hornet etc. their
venom is administered drop by drop similar to a rattle snake. The bees have a barb-
shaped stinger.
Venom: Histamine/serotonin (local reaction & pain)
Causes tissue necrosis, Phospholipase/hyaluronidase, destroys collagen and is also
an allergen.
Manifestation
Local reaction:
Sting produced localize pain, wheal which results in a pustule.
20% produced large local reaction as erythematous, edematous, and painful and
pruritic areas larger than 10cm. This may last for up to 2-5 days.
Represents combination of IgE mediated, cell mediated problems.
Systemic reaction:
Multiple stings can produce toxic reactions.
1. Vomiting, diarrhea, generalized edema
2. Cardiovascular collapse
3. Hemolysis
3% causes death due to anaphylaxis w/in 1 hr.
Starts as urticaria then proceeds to angioedema, respiratory arrest 2
nd
to airway
edema and cardiovascular collapse.
Treatment:
Local therapy:
Removal of sting (gentle scraping)
Clean the site
Pain: - apply ice
- Vinegar
- Topical or injected lidocaine
Pruritus: - antihistamine
Larger area: elevate the site
- Analgesia
- Prednisone (1mg/k/day)
Systemic therapy:
Mild anaphylaxis:
Epinephrine
Oral or IV antihistamine
Severe anaphylaxis:
IV - endotracheal intubation
Vasopressor - steroid
Bronchodilator - ICU monitoring
Venomous Aquatic Animals
Invertebrates
1. Coelenterates: (Jelly fish)
Venomous stinging cells called nematocyte
Mild envenomation:
- Sting produces skin irritation
1. Pruritus, paresthesia & throbbing pain
2. Edema and erythema ----> blisters & petechia ----> local
infection & ulceration.
Treatment:
Clean the wound w/ sea water
Apply diluted 5% acetic acid (vinegar) or baking soda; it can
inactivate the toxin; applied for 30 minutes or until the pain is relieved
After wound irrigation ---> remaining nematocyst are removed by
applying shaving cream and shave the area w/ razor
Local anesthesia, antihistamine or steroids can relieve pain after the
toxin is inactivated.
Prophylactic antibiotic are usually unnecessary
2. Echinodermata (sea urchins & sea cucumber)
Causes contact dermatitis
Sea cucumbers feeds on coelenterates and secrete nematocytes hence
local therapy for coelenterates should be done
Sea urchins venomous spines causing local & systemic reaction like
coelenterates
Treatment:
Soak w/ hot water
Spines of the organism located w/ x-ray or MRI and should be removed
Swelling alleviated w/ steroids
3. Mollusks (octopus):
Can bite & inject tetrodoxine (paralytic agent)
pressure & immobilize to contain venom
Systemic complication --- supportive
Vertebrates
1. Stingrays:
Whiplike appendages with spines at its end that can produce puncture
wounds & lacerations
Venom = vasoconstrictions causing cyanosis of wound ---->
myonecrosis
Systemic reaction:
1. Cardiac arrhythmia
2. Respiratory arrest
3. seizures
Treatment:
Wound irrigated and soaked w/water for an hour
Debridement, exploration and removal of spines
Wound is elevated, dressed and not closed primarily
Pain relieved locally and systemically
2. Sea Snakes: (Hydrophiidae)
Neurologic sign and symptoms
Death is due to paralysis and resp. arrest
Toxin similar to coral snake
Pressure, immobilize technique
Antivenin administration 1 ampule initially then repeated as
needed
Você também pode gostar
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Parathyroid Glands: Presented By: Dr. Mohammed Alshehri Pgy2Documento28 páginasParathyroid Glands: Presented By: Dr. Mohammed Alshehri Pgy2Omar Alruwaili100% (1)
- Patho AsthmaDocumento1 páginaPatho AsthmaAyel JimenezAinda não há avaliações
- 07 - Sudden Plays A Hand (1950)Documento206 páginas07 - Sudden Plays A Hand (1950)ShaziaAshrafAinda não há avaliações
- 01 - Sudden - Outlawed (1935)Documento223 páginas01 - Sudden - Outlawed (1935)ShaziaAshrafAinda não há avaliações
- 02 - Sudden (1933)Documento339 páginas02 - Sudden (1933)ShaziaAshrafAinda não há avaliações
- History and Admiralty Jurisdiction of The High Court in IndiaDocumento9 páginasHistory and Admiralty Jurisdiction of The High Court in IndiaShaziaAshrafAinda não há avaliações
- ITLOS - Admiralty JurisdictionDocumento13 páginasITLOS - Admiralty JurisdictionShaziaAshrafAinda não há avaliações
- The Immunity of State Owned Vessels From Maritime ArrestsDocumento7 páginasThe Immunity of State Owned Vessels From Maritime ArrestsShaziaAshrafAinda não há avaliações
- Compensation Claims Under WorkmenDocumento10 páginasCompensation Claims Under WorkmenBijay Krishna DasAinda não há avaliações
- Role of Non-Governmental Organizations in Environment Conservation - The Indian ScenarioDocumento18 páginasRole of Non-Governmental Organizations in Environment Conservation - The Indian ScenarioShaziaAshrafAinda não há avaliações
- Deletion Od Article 32 Is UnconstituionalDocumento2 páginasDeletion Od Article 32 Is UnconstituionalShaziaAshrafAinda não há avaliações
- Combination Hyperbaric Oxygen and Temozolomide Therapy in c6 Rat Glioma ModelDocumento5 páginasCombination Hyperbaric Oxygen and Temozolomide Therapy in c6 Rat Glioma ModelDICKY PANDUWINATAAinda não há avaliações
- Land of NodDocumento7 páginasLand of NodMaltesers1976Ainda não há avaliações
- Department of Obstetrics and Gynecology FinalDocumento42 páginasDepartment of Obstetrics and Gynecology Finalkremlin23455Ainda não há avaliações
- Paedia - Dr. RehabDocumento173 páginasPaedia - Dr. RehabMohammed Saad NabhanAinda não há avaliações
- Nursing Care Plan Placenta PreviaDocumento2 páginasNursing Care Plan Placenta PreviaApril Ann HortilanoAinda não há avaliações
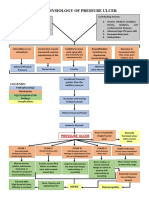
- Pathophysiology of Pressure UlcerDocumento1 páginaPathophysiology of Pressure UlcerSTORAGE FILEAinda não há avaliações
- Proton Pump Inhibitors, Adverse Events and Increased Risk of MortalityDocumento36 páginasProton Pump Inhibitors, Adverse Events and Increased Risk of MortalityMohammad Mahmudur RahmanAinda não há avaliações
- Annals of Thyroid ResearchDocumento2 páginasAnnals of Thyroid ResearchAustin Publishing GroupAinda não há avaliações
- Aches and Pains in The ElderlyDocumento34 páginasAches and Pains in The ElderlyAna CampeanuAinda não há avaliações
- What Is An Obstetric Fistula?Documento5 páginasWhat Is An Obstetric Fistula?abyAinda não há avaliações
- NCP PryllDocumento6 páginasNCP PryllpjcolitaAinda não há avaliações
- JACC Volume 78, Issue 11 SeptemberDocumento122 páginasJACC Volume 78, Issue 11 SeptemberFareesha KhanAinda não há avaliações
- Ã'Tia' Fiakdkdhl Úohd, H - FLD U 07: D.S. Senanayake College - Colombo 07Documento12 páginasÃ'Tia' Fiakdkdhl Úohd, H - FLD U 07: D.S. Senanayake College - Colombo 07joker boyAinda não há avaliações
- Acetylcholine Esterase AntibodyDocumento2 páginasAcetylcholine Esterase AntibodySrinivasanAinda não há avaliações
- Treatment of Portal HypertensionDocumento10 páginasTreatment of Portal HypertensionLourianne NcAinda não há avaliações
- Child Abuse Nursing Care PlansDocumento7 páginasChild Abuse Nursing Care PlansMAHESH KOUJALAGIAinda não há avaliações
- Syphilis Symptoms, Causes, and DiagnosisDocumento3 páginasSyphilis Symptoms, Causes, and DiagnosisIndra FahleviAinda não há avaliações
- Thyroid Hormone Profile in Chronic Kidney DiseaseDocumento6 páginasThyroid Hormone Profile in Chronic Kidney DiseaserefaAinda não há avaliações
- Annotated-Research 20paperDocumento7 páginasAnnotated-Research 20paperapi-667261947Ainda não há avaliações
- NCM 104 RLE Module 3 FinalsDocumento22 páginasNCM 104 RLE Module 3 FinalsAlexander DontonAinda não há avaliações
- Colon Large Intestine: ColorectalDocumento3 páginasColon Large Intestine: ColorectalAlina AldeaAinda não há avaliações
- Acute Suppurative Parotitis: Related SummariesDocumento7 páginasAcute Suppurative Parotitis: Related SummariesFarida Dwi IrnawatiAinda não há avaliações
- Rickettsia eDocumento10 páginasRickettsia eDeep Iyaz100% (1)
- Lapp Jan2020Documento88 páginasLapp Jan2020Siti RojanahAinda não há avaliações
- C-Reactive Protein in Serum by NephelometryDocumento12 páginasC-Reactive Protein in Serum by NephelometryTrajceAinda não há avaliações
- Midterm Activity ScitechDocumento3 páginasMidterm Activity ScitechKean KaiAinda não há avaliações
- Drug Study FINALDocumento32 páginasDrug Study FINALhomeworkping1Ainda não há avaliações
- Pathophys RespDocumento38 páginasPathophys RespSabrina LavegaAinda não há avaliações