Escolar Documentos
Profissional Documentos
Cultura Documentos
Omega-3 Polyunsaturated Fatty Acids in The Treatment of Schizophrenia
Enviado por
Pedro PriorDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Omega-3 Polyunsaturated Fatty Acids in The Treatment of Schizophrenia
Enviado por
Pedro PriorDireitos autorais:
Formatos disponíveis
Omega-3 Polyunsaturated Fatty Acids inthe Treatment of
Schizophrenia
Malcolm Peet, MB, ChB, FRCPsych
Swallownest Court Hospital, Sheffield, Great Britain.
Abstract: Most studies have shown reduced levels of polyunsaturated fatty acids, particularly docosahexaenoic acid
and arachidonic acid, in the cell membranes of red blood cells fromschizophrenic patients. This has led to research in-
terest in the possible therapeutic benefits of omega-3 fatty acids in schizophrenia. There is evidence fromdouble-blind
placebo-controlled trials that omega-3 fatty acids might prevent conversion from a prodromal state into first episode
psychosis, and reduce the antipsychotic drug requirement in first episode patients. Results in chronic and acutely re-
lapsing schizophrenia have been mixed. The problems associated with single nutrient studies are discussed. Nutrients
are normally ingested in complex combinations, and they interact with each other in their normal metabolic and phys-
iological functions. It is likely that optimal nutritional treatment will involve complex combinations of nutrients, pref-
erably as part of a healthy balanced diet rather than by using supplements. However, such approaches have been little
evaluated in mental health.
Introduction
The phospholipid hypothesis of schizophrenia, orig-
inally developed by David Horrobin and his col-
leagues (1, 2), proposed that a variety of mental
health problems could result from abnormalities of
the phospholipid structure of neuronal membranes.
Since polyunsaturated fatty acids (PUFA) are major
structural components of cel l membrane
phospholipid, a great deal of research interest has
been focussed on the possible role of these fatty acids
in mental health. This review will focus on the avail-
able evidence relating to the role of omega-3 fatty
acids in schizophrenia.
The Role of Omega-3 Fatty Acids
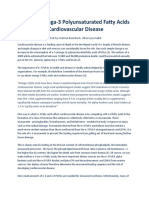
Omega-3 fatty acids are primarily obtained from di-
etary sources. An outline of the metabolism of
omega-3 fatty acids is shown in Figure 1. The parent
of this class of fatty acids is A-linolenic acid (ALA).
This fatty acid cannot be synthesized by humans, so
it is termed an essential fatty acid. The omega-3 fatty
acids which have been investigated most in relation
to mental health are eicosapentaenoic acid (EPA)
and docosahexaenoic acid (DHA). Although these
fatty acids can be synthesized from ALA, the meta-
Isr J Psychiatry Relat Sci Vol 45 No. 1 (2008) 1925
-linolenic acid
(18:3n-3)
Eicosapentaenoic acid
(20:5n-3)
Docosahexaenoic acid
(22:6n-3)
Tetrahexaenoic acid (24:6n-3)
Acyl coenzyme-A desaturase
-oxidation
-6-Desaturase
Elongase
-5-Desaturase
Elongase
Elongase
-6-Desaturase
Figure 1. An outline
of the metabolic
pathway for omega-3
fatty acids.
Address for Correspondence: Address for correspondence: MalcolmPeet, MB, ChB, FRCPsych, Swallownest Court Hos-
pital, Sheffield, S26 4TH, Great Britain. E-mail: malcolmpeet@yahoo.com
bolic pathway is not very efficient (3) so that in prac-
tice most EPAand DHAcomes fromdietary sources,
particularly fish.
DHA is a major omega-3 polyunsaturated fatty
acid in the phospholipid of neuronal cell membranes
(4). EPA, in contrast, is not present in neuronal cell
membranes. Because of this, DHAand EPAhave dif-
ferent physiological effects on neuronal function.
Thus, there is good evidence that changing the DHA
content of neuronal cell membranes can alter densi-
ties of dopamine, serotonin and muscarinic recep-
tors in brain (5). EPA can affect neuronal function
because it is an important precursor of eicosanoids
and modulator of cytokines which have neurotrans-
mitter and neuromodulatory effects (6). Omega-3
fatty acids can also modify the expression of genes,
including several genes which are important for
brain function (7). It has been shown that maternal
omega-3 fatty acid deficiency leads to long termover
expression of dopamine receptor genes in the off-
spring (8).
Omega-3 Fatty Acids in Schizophrenia
It has been shown repeatedly that schizophrenic pa-
tients have reduced cell membrane levels of polyun-
saturated fatty acids, particul arly DHA and
arachidonic acid (AA) (9). Most studies were con-
ducted on cell membranes from red blood cells
(RBC). RBC membrane levels of PUFA are regarded
as a reflection of brain levels; it has been shown that
the two correlate significantly in adult humans (10).
Some of the early studies may have been confounded
by extraneous factors. For example, there is evidence
that smoking leads to reduced levels of PUFAin RBC
membranes and it is well known that a higher pro-
portion of schizophrenic patients smoke relative to
the general population (11). Also, there is a tendency
for RBC membrane levels of DHA and AA to dimin-
ish during storage, and this happens more rapidly in
samples from schizophrenic patients than in those
from healthy controls (12), possibly because the
blood of schizophrenic patients is under increased
oxidative stress. Because of that, samples need to be
stored at -80C rather than the standard -20C (13).
Some recent studies, taking account of these con-
founders, have still reported low levels of DHA and
AAin RBCmembranes fromschizophrenic patients.
However, a recent study found no reduction of either
DHA or AA in large groups of unmedicated schizo-
phrenic patients from India and from Malaysia (9).
Therefore, reduced RBClevels of DHAare not a nec-
essary or inevitable association with schizophrenia
but perhaps may modify the presentation and course
of the illness.
Omega-3 PUFAin the Treatment of
Schizophrenia
An early open-label study of omega-3 PUFA in
schizophrenia reported significant improvement in
both schizophrenic symptoms and tardive dyskinesia
(TD) (14). These beneficial effects were confirmed
in early double blind placebo controlled trials (15).
There was also an indication from these early studies
that EPA was more effective than DHA, and as a re-
sult subsequent studies have focussed on EPA.
The results of all double blind placebo controlled
studies of omega-3 fatty acids treatment in schizo-
phrenia are summarized in Table 1. It has been di-
vided into studies including young people at ultra-
high risk of developing psychosis, those who have
developed a first episode of psychosis, and those pa-
tients who have established chronic schizophrenia.
The only placebo controlled trial in ultra-high risk
subjects provided evidence that an EPA rich omega-
3 preparation can reduce the risk of these subjects
developing overt psychosis (16). Two studies have
been conducted in first episode patients. In the first
study (15) EPA enriched oil or corn oil placebo was
given to unmedicated patients for three months. The
primary outcome measure was whether or not the
patients required treatment with antipsychotic
drugs. All 12 patients on placebo, but only eight out
of 14 on EPA, required these drugs during the three
months study period. The patients in this study were
older than a usual first episode group (mean 33
years) and the duration of psychosis averaged
around six years. Some had been treated previously.
Therefore, this was not a representative first episode
group. Arecent study (17) used EPAor placebo as an
add-on to existing treatment with risperidone. Al-
though the primary analysis based on symptom rat-
ings showed no difference between EPA or placebo
treated patients, secondary analysis showed that the
EPA treated patients were on a lower dose of
20 OMEGA-3 POLYUNSATURATED FATTY ACIDS IN THE TREATMENT OF SCHIZOPHRENIA
risperidone by the end of the study. Thus, both these
studies can be interpreted as showing an
antipsychotic-sparing effect of omega-3 fatty acid
treatment. Studies in chronic schizophrenia have
given much more mixed results, with three studies
reporting benefits from EPA enriched oil in either
the primary or secondary analysis of data, two
studies showing no benefit from EPA over placebo,
and one study in acutely relapsing schizophrenia
showing that EPA alone led to a significantly worse
outcome than placebo treatment. In all of these
studies, EPArich oil was given in addition to existing
antipsychotic medication. In the study by Bentsen
(18), the apparently detrimental effect of the EPA
was reversed when antioxidant medication was
given in addition. One study (19) showed a marked
benefit for EPAtreatment in the subgroup of patients
who were already being treated with clozapine.
MALCOLM PEET 21
Table 1. Double-Blind Placebo-Controlled Studies of Omega-3 PUFA in Schizophrenia
Authors Study Design Primary analysis Secondary analysis
High Risk
Amminger & Schafer (16) Mono; EPA rich oil vs pla-
cebo
EPA > placebo
First Episode
Peet et al. (15) Mono; 2g: EPA vs placebo EPA > placebo for anti-
psychotic drug requirement
Berger et al. (17) Add-on; 2g: EPA vs placebo EPA = placebo EPA > placebo for
antipsychotic dose
Chronic Schizophrenia
Peet et al. (15) Add-on; 2g: EPA vs DHA vs
placebo
EPA > placebo EPA > DHA
Fenton et al. (20) Add-on; 3g: EPA vs placebo EPA = placebo
Peet & Horrobin (19) Add-on; 1, 2 & 4g: EPA vs
placebo
EPA = placebo EPA(2g) > placebo in
clozapine subgroup
Emsley et al. (21) Add-on; 3g: EPA vs placebo EPA > placebo
Bentsen (18) Add-on; 2g: EPA vs antioxi-
dants vs combination vs pla-
cebo
EPA < placebo EPA + antioxidants
= placebo
Emsley et al. (22) Add-on; 2g: EPA vs placebo N/A
(Primary analysis for effect
on tardive dyskinesia)
EPA = placebo
Explanation of abbreviations: Add-on is the addition of omega-3 PUFA to current antipsychotic medication; mono is sin-
gle therapy with omega-3 fatty acids. Primary analysis is the statistical analysis for the hypothesized main effect; secondary
analysis relates to secondary hypotheses or post-hoc statistical analysis.
The Problemof Single Nutrient Studies
When treating schizophrenia, psychiatrists are ac-
customed to the idea that it is better to use a single
drug rather than polypharmacy. The same approach
is taken when investigating potential new treat-
ments. Nutritional treatments are different. Nutri-
ents are normally ingested in complex combinations,
and in normal physiology they act synergistically. Ei-
ther deficiency, or excess, of a particular nutrient can
have harmful effects (23). In schizophrenia, there is
evidence for benefits, not only from omega-3 PUFA,
but also from other nutrients. These include the
homocysteine-lowering vitamins (folate, B
6
, B
12
)
(24), and the antioxidant vitamins (25).
There is good evidence that the homocysteine-
lowering vitamins are important for omega-3 PUFA
metabolism. Vitamin B
6
is a co-factor for enzymes in
the metabolic chain shown in Figure 1. Rats fed high
quantities of ALA (the parent omega-3 fatty acid)
but low levels of vitamin B
6
showed significantly
higher levels of ALA but lower levels of EPA and
DHA than control animals which were not vitamin
B
6
deficient (26). This was associated with a marked
reduction in the activity of
6
-desaturase and the
first enzyme of the -oxidation pathway (acyl-CoA
oxidase), both of which are involved in the metabolic
pathway of omega-3 PUFA (Figure 1). Rats which
are deficient in folic acid have significantly reduced
plasma and platelet membrane levels of omega-3
PUFA (27), and the administration of folic acid leads
to an increase in omega-3 PUFAlevels in plasma and
in RBC and platelet membranes, relative to control
animals (28). There is also evidence that omega-3
fatty acids can influence homocysteine levels. While
short-term studies of the effects of omega-3 fatty
acids supplementation on homocysteine levels have
given mixed results (29), a more recent long-term
study showed that homocysteine levels are signifi-
cantly reduced after one year of omega-3 PUFA
treatment relative to the effects of corn oil in patients
who have suffered an acute myocardial infarction
(30). Li et al. (31) found a significant inverse rela-
tionship between plasma homocysteine levels and
phospholipid DHA levels in healthy male subjects.
Antioxidant vitamins may also be important with
regard to omega-3 PUFA levels. It is well recognized
that oxidative stress will reduce cell membrane levels
of DHA and other PUFA (32), and there is evidence
that vitamin E supplementation can increase RBC
membrane levels of DHA and other PUFA (33).
The possible importance for mental health of
these synergistic effects of micronutrients is demon-
strated by preliminary and as yet unpublished find-
ings from placebo controlled trials. A recent study
(34) reported that the apparently detrimental effects
of EPA on the symptoms of chronic schizophrenia
were reversed when the EPA was given together with
antioxidant vitamins. In depression, there is evi-
dence that EPAis effective only in those patients who
have an adequate folic acid status (Horrobin, unpub-
lished). Nutritional practitioners commonly use
combinations of homocysteine-lowering and antiox-
idant vitamins, omega-3 fatty acids and other micro-
nutrients in the supplementary treatment of
schizophrenia. However, the efficacy of these combi-
nations has been very little researched.
Research in the area is further compromised by
the ethical requirement to administer nutritional
treatment in addition to an established treatment
such as an antidepressant, rather than using an un-
proven nutritional supplement as the sole treatment.
However, now that we have increasing efficacy data
from add-on studies, it is becoming ethically ac-
ceptable to conduct nutrient-only studies under
some circumstances.
The Nutritional Status of Schizophrenic
Patients
There have been several studies showing that people
with a diagnosis of schizophrenia eat a diet which is
even worse than that of the general population.
Their diet is high in saturated fat and sugar, and low
in polyunsaturated fats and in fresh fruit and vegeta-
bles. Therefore, they consume low levels of omega-3
fatty acids, folic acid and antioxidant vitamins, and
excessive quantities of unhealthy foods (3538). This
may explain the common biochemical findings of
high homocysteine levels, low omega-3 fatty acid
levels, and high oxidative stress (39) in these pa-
tients. A recent study showed a positive correlation
between dietary fish fat intake and levels of folate
and vitamin B
12
in a group of schizophrenic patients,
which confirms that many patients suffer from mul-
tiple nutritional deficiencies (40).
22 OMEGA-3 POLYUNSATURATED FATTY ACIDS IN THE TREATMENT OF SCHIZOPHRENIA
Implications
Given what we knowabout nutrient interactions and
the multiple deficiencies which occur in schizo-
phrenic patients, it is not surprising that single nutri-
ent studies have given mixed results. It is likely that
the optimal nutritional treatment for schizophrenia
will involve increasing the intake of multiple nutri-
ents. It is also significant that schizophrenic patients
are known to suffer from increased risks of cardio-
vascular disease (41) and diabetes (42). It is likely
that both genetic and lifestyle factors play a role in
this increased physical morbidity, but nutritional
factors including lack of omega-3 fatty acids are
probably of particular importance (43, 44). The
same nutrients that have been implicated in mental
health including omega-3 fatty acids, homocysteine-
lowering vitamins and antioxidants, have also been
highlighted as essential to physical well-being (45,
46). We contend that nutritional management
should be an integral part of the treatment of people
suffering their first episode of psychosis, with the
aim of reducing subsequent physical morbidity and
mortality and the likelihood that the mental state
will also benefit from good nutrition. Our own prac-
tice is to carry out a full nutritional assessment on
every patient who presents with first episode psy-
chosis. This is conducted by a nutritionist using a
diet diary, and the dietary information is analyzed
using the WISP software package version 3.0
(Tinuvel software, Warrington, U.K.). This is fol-
lowed by detailed nutritional feedback aimed at in-
creasing dietary intake of nutrients which are
important for mental and physical health, and re-
ducing the dietary intake of harmful nutrients in-
cluding saturated fat and sugar. In the initial phases
of treatment, we use supplements which include
omega-3 fatty acids and multivitamin and mineral
combinations which include homocysteine-lower-
ing and antioxidant vitamins. These are given as
commercially available prescribed supplements
which contain 1g of omega-3-acid esters (EPA
460mg, DHA 380mg), folic acid 400 micrograms,
cyanocobalamin 3 micrograms, pyridoxine 2mg,
ascorbic acid 60mg, vitamin E 10mg, as well as a va-
riety of other vitamins, minerals and trace elements.
However, the main aim of nutritional therapy is to
encourage patients to eat a more balanced, healthy
diet as part of their normal lifestyle.
References
1. Horrobin DF. The membrane phospholipid hypothesis
as a biochemical basis for the neurodevelopmental
concept of schizophrenia. Schizophr Res 1998;30:193
208.
2. Peet M, Glen I, Horrobin DF, editors. Phospholipid
spectrum disorder in psychiatry and neurology. 2nd
ed. Carnforth: Marius, 2003.
3. Burdge G. Alpha-linolenic acid metabolism in men
and women: Nutritional and biological implications.
Curr Opin Clin Nutr Metab Care 2004;7:137144.
4. Horrobin DF, Manku MS, Hillman H, Glen AIM. Fatty
acid levels in the brains of schizophrenics and normal
controls. Biol Psychiatry 1991;30:795805.
5. Du Bois TM, Deng C, Huang XF. Membrane
phospholipid composition, alterations in neurotrans-
mitter systems and schizophrenia. Prog Neuro-
psycopharmacol Biol Psychiatry 2005;29:878888.
6. Fenton WS, Hibbeln J, Knable M. Essential fatty acids,
lipid membrane abnormalities and the diagnosis and
treatment of schizophrenia. Biol Psychiatry 2000;47:8
21.
7. Kitajka K, Sinclair AJ, Weisinger RS, Weisinger HS,
Mathai M, Jayasooriya AP, Halver JE, Puskas LG. Ef-
fects of dietary omega-3 polyunsaturated fatty acids on
brain gene expression. Proc Natl Acad Sci USA 2004;
101:1093110936.
8. Kuperstein F, Yakubov E, Dinerman P, Gil S, Eylam R,
Salem N Jr., Yavin E. Over expression of dopamine re-
ceptor genes and their products in the postnatal rat
brain following maternal n-3 fatty acid dietary defi-
ciency. J Neurochem 2005;95:15501562.
9. Peet M, Shah S, Selvam K, Ramchand CN. Polyunsatu-
rated fatty acid levels in red cell membranes of unmedi-
cated schizophrenic patients. World J Biol Psychiatry
2004;5:9299.
10. Carver JD, Benford VJ, Han B, Cantor AB. The rela-
tionship between age and the fatty acid composition of
cerebral cortex and erythrocytes in human subjects.
Brain Research Bull 2001;56:7985.
11. Hibbeln J, Makino KK, Martin CE, Dickerson F,
Boronow J, Fenton W S. Smoking, gender and di-
etary influences on erythrocyte essential fatty acid
composition among patients with schizophrenia and
schizoaffective disorders. Biol Psychiatry 2003;53:431
441.
12. Fox H, Ross BM, Tocher D, Horrobin D, Glen I, St Clair
D. Degradation of specific polyunsaturated fatty acids
in red blood cells stored at -20 degrees C proceeds
faster in patients with schizophrenia when compared
MALCOLM PEET 23
with healthy controls. Prostaglandins Leukot Essent
Fatty Acids 2003;69:291297.
13. Hodson L, Skeaff CM, Wallace A J, Arribas F L. Stabil-
ity of plasma and erythrocyte fatty acid composition
during cold storage. Clin Chim Acta 2002;321:6367.
14. Mellor J, Laugharne JDE, Peet M. Omega-3 fatty acid
supplementation in schizophrenic patients. Human
Psychopharmacol 1996;11:3946.
15. Peet M, Brind J, Ramchand CN, Shah S, Vankar GK.
Two double-blind placebo-controlled pilot studies of
eicosapentaenoic acid in the treatment of schizophre-
nia. Schizophr Res 2001;49:243251.
16. Amminger GP, Schafer MR. Indicated prevention with
omega-3 fatty acids in adolescents at ultra-high risk for
psychosis rationale, methods, and 3 months out-
come. Schiz Res 86; 2006: S978. Presented at 5
th
Inter-
national Conference on Early Psychosis, Birmingham,
Oct. 2006.
17. Berger GE. Ethyl-eicosapentaenoic acid (E-EPA)
supplementation in early psychosis: A double-blind
randomised placebo-controlled add on study in 80
drug-nave first episode psychosis patients [abstract].
Int J Neuropsychopharmacol 2004; 8 Suppl. 1: S422.
18. Bentsen H. The Norwegian study on the treatment of
schizophrenia and schizoaffective disorder with ethyl-
EPA and antioxidants. Presented at second conference
on Brain Phospholipids, Aviemore, Scotland, March,
2006.
19. Peet M, Horrobin DF. A dose-ranging exploratory
study of the effects of ethyl-eicosapentaenoate in pa-
tients with persistent schizophrenic symptoms. J
Psychiatr Res 2002;36:718.
20. Fenton WS, Dickenson FM, Boronow J, Hibbeln JR,
Knable M. A placebo-controlled trial of omega-3 fatty
acid (ethyl eicosapentaenoic acid) supplementation for
residual symptoms and cognitive impairment in
schizophrenia. Am J Psychiatry 2001;258:20712074.
21. Emsley R, Myburgh C, Ousthuizen P, van Rensburg SJ.
Randomised, placebo-controlled study of ethyl-
eicosapentaenoic acid as supplemental treatment in
schizophrenia. Am J Psychiatry 2002;159:15961598.
22. Emsley R, Niehaus DJH, Koen L. The effects of
eicosapentaenoic acid in tardive dyskinesia: A ran-
domised, placebo controlled trial. Schizophr Res 2006;
84:112120.
23. Mularski RA, Grazer RE, Santoni L, Strither JS, Bizovi
KE. Treatment advice on the internet leads to a life-
threatening adverse reaction: Hypotension associated
with niacin overdose. Clin Toxicol (Phil) 2006;44:81
84.
24. Levine J, Stahl Z, Sela BA, Ruderman V, Shumaico O,
Babushkin I, Osher Y, Bersudsky Y, Belmaker RH.
Homocysteine-lowering strategies improve symptoms
in chronic schizophrenic patients with hyper-
homocysteinaemia. Biol Psychiatry 2006;60:265269.
25. Dakhale GN, Khanzode SD, Khanzode SS, Saoji A.
Supplementation of vitamin C with atypical anti-
psychotics reduces oxidative stress and improves the
outcome of schizophrenia. Psychopharmacology
(Berl) 2005;182:494498.
26. Tsuge H, Hotta N, Hayakawa T. Effects of vitamin B-6
on (n-3) polyunsaturated fatty acid metabolism. J Nutr
2000;130:33353345.
27. Durand P, Prost M, Blache D. Pro-thrombotic effects
of a folic acid deficient diet in rat platelets and
macrophages related to elevated homocysteine and de-
creased n-3 polyunsaturated fatty acids. Atherosclero-
sis 1996;121:231243.
28. Pita M-L, Delgado M-J. Folate administration in-
creases n-3 polyunsaturated fatty acids in rat plasma
and tissue lipids. Thromb Haemostat 2000;84:420423.
29. De Bree A, Mennen LI, Hercberg S, Galan P. Evidence
for a protective (synergistic?) effect of B-vitamins and
omega-3 fatty acids on cardiovascular diseases. Eur J
Clin Nutr 2004;58:732744.
30. Grundt H, Nilsen DW, Mansoor MA, Hetland O,
Nordoy A. Reduction in homocysteine by n-3 polyun-
saturated fatty acids after one year in a randomised
double-blind study following an acute myocardial in-
farction: No effect on endothelial adhesion properties.
Pathophysiol Haemost Thromb 2003;33:8895.
31. Li D, Mann NJ, Sinclair AJ. A significant inverse
relationship between concentrations of plasma
homocysteine and phospholipid docosahexaenoic acid
in healthy male subjects. Lipids 2006;41:8589.
32. Clemens MR, Waller HD. Lipid peroxidation in eryth-
rocytes. Chem Phys Lipids 1987;45:251268.
33. Ota Y, Sasaqawa T, Suzuki K, Tomioka K, Nagai A,
Niiyana G, Kawakana M, Yamada G, Okita M. Vitamin
E supplementation increasing polyunsaturated fatty
acids of RBCmembrane in HCV-infected patients. Nu-
trition 2004;20:358363.
34. McCreadie R, Macdonald E, Blacklock C, Tilak-Singh
D, Wiles D, Halliday J, Paterson J. Dietary intake of
schizophrenic patients in Nithsdale, Scotland: Case-
control study. Br Med J 1998;317:784785.
35. Brown S, Birtwistle J, Roe L, Thompson C. The un-
healthy lifestyle of people with schizophrenia. Psychol
Med 1999;29:697701.
36. Ryan MCM, Collins P, Thakore J H. Impaired fasting
glucose tolerance in first-episode, drug-nave patients
with schizophrenia. Am J Psychiatry 2003;160:284
289.
37. Stokes C, Peet M. Dietary sugar and polyunsaturated
fatty acid consumption as predictors of severity of
schizophrenia symptoms. Nutr Neurosci 2004;7:247
249.
24 OMEGA-3 POLYUNSATURATED FATTY ACIDS IN THE TREATMENT OF SCHIZOPHRENIA
38. Khan MM, Evans DR, Gunna V, Scheffer RE, Parikh
VV, Mahadik SP. Reduced erythrocyte membrane es-
sential fatty acids and increased lipid peroxides in
schizophrenia at the never-medicated first-episode of
psychosis and after years of treatment with anti-
psychotics. Schizophr Res 2002;58:110.
39. Kemperman RFJ, Veurink M, van der Wal T,
Knegtering H, Bruggeman R, Fokkema M R, Kema IP,
Korf J, Muskiet FA. Low essential fatty acid and B-vita-
min status in a subgroup of patients with schizophrenia
and its response to dietary suppl ementation.
Prostaglandins Leukot Essent Fatty Acids 2006;74:75
85.
40. Hennekens CH, Hennekens AR, Hollar D, Casey DE.
Schizophrenia and increased risks of cardiovascular
disease. Am Heart J 2005;150:11151121.
41. De Hert M, van Winkel R, van Eyck D, Hanssens L,
Wampers M, Scheen A, Peuskens J. Prevalence of dia-
betes, metabolic syndrome and metabolic abnormali-
ties in schizophrenia over the course of the illness: A
cross-sectional study. Clin Pract Epidemiol Ment
Health 2006;2:14.
42. Hu FB, Willett WC. Optimal diets for the prevention
of coronary heart disease. JAMA 2002; 288: 2569
2578.
43. Peet M. The metabolic syndrome, omega-3 fatty acids
and inflammatory processes in relation to schizophre-
nia. Prostaglandins Leukot Essent Fatty Acids 2006;75:
323327.
44. Peet M. Diet, diabetes and schizophrenia: Review and
hypothesis. Br J Psychiatry 2004;184:102105.
45. Haag M, Dippenaar NG. Dietary fats, fatty acids and
insulin resistance: A short review of a multifaceted
connection. Med Sci Monit 2005; 11: RA359367.
46. Donaldson M S. Nutrition and cancer: A review of the
evidence for an anti-cancer diet. Nutr J 2004;3:19.
MALCOLM PEET 25
Você também pode gostar
- Omega-3 Oils: Applications in Functional FoodsNo EverandOmega-3 Oils: Applications in Functional FoodsErnesto HernandezNota: 3.5 de 5 estrelas3.5/5 (3)
- Nutricion y EsquizofreniaDocumento13 páginasNutricion y EsquizofreniacelliasttAinda não há avaliações
- Supplementation With Omega-3 Fatty Acids in Psychiatric Disorders: A Review of Literature DataDocumento26 páginasSupplementation With Omega-3 Fatty Acids in Psychiatric Disorders: A Review of Literature Datadaniel serraniAinda não há avaliações
- Kolagen 2Documento21 páginasKolagen 2OktageliaAinda não há avaliações
- Difference Between Vegetable and Animal Omega 3 Fatty AcidsDocumento3 páginasDifference Between Vegetable and Animal Omega 3 Fatty AcidsnicodipietroAinda não há avaliações
- The Role of Omega-3 Fatty Acids in Mood DisordersDocumento9 páginasThe Role of Omega-3 Fatty Acids in Mood DisordersARESS RIPAinda não há avaliações
- PEC 2020 AGOSTONI OMEGA3 Autism Early Psychosis ADHD PLANTILLA PDFDocumento25 páginasPEC 2020 AGOSTONI OMEGA3 Autism Early Psychosis ADHD PLANTILLA PDFCorreo DraftAinda não há avaliações
- Fotuhi 2009Documento13 páginasFotuhi 2009peri umardianaAinda não há avaliações
- Omega-6/Omega-3 Ratio and Brain-Related Functions: Shlomo YehudaDocumento20 páginasOmega-6/Omega-3 Ratio and Brain-Related Functions: Shlomo YehudaJonas SkadbergAinda não há avaliações
- Neuromedicterranea Omega 3 y Salud MentalDocumento13 páginasNeuromedicterranea Omega 3 y Salud MentalDORIS JANETHAinda não há avaliações
- Omega-3 Literature ReviewDocumento8 páginasOmega-3 Literature Reviewn1dihagavun2100% (1)
- Food For MoodDocumento15 páginasFood For MoodDaniele LimaAinda não há avaliações
- 2020 Article 1337Documento17 páginas2020 Article 1337Ubada Aqid Al-jabarAinda não há avaliações
- Biocatalysis and Agricultural BiotechnologyDocumento8 páginasBiocatalysis and Agricultural BiotechnologyWemdi Priya PrasetyaAinda não há avaliações
- Nihms 1034069Documento36 páginasNihms 1034069Ubada Aqid Al-jabarAinda não há avaliações
- Fish Oil's Effects on Rheumatic DiseasesDocumento8 páginasFish Oil's Effects on Rheumatic DiseasesJosé Isaac Lamas GarcíaAinda não há avaliações
- Effects of Omega-3 Polyunsaturated Fatty Acids and Their Metabolites On Haemostasis-Current Perspectives in Cardiovascular DiseaseDocumento13 páginasEffects of Omega-3 Polyunsaturated Fatty Acids and Their Metabolites On Haemostasis-Current Perspectives in Cardiovascular DiseaseIgor BaltaAinda não há avaliações
- CVD ArticleDocumento2 páginasCVD ArticleiacubaAinda não há avaliações
- Role of Omega-3 Fatty Acids and Their Metabolites - 1Documento8 páginasRole of Omega-3 Fatty Acids and Their Metabolites - 1Alif RahmanAinda não há avaliações
- Balancing Omega-6 and Omega-3 Fatty AcidsDocumento4 páginasBalancing Omega-6 and Omega-3 Fatty AcidsUsman AliAinda não há avaliações
- Increased dietary α-linolenic acid has sex-specific effects upon eicosapentaenoic acid status in humans: re-examination of data from a randomised, placebo-controlled, parallel studyDocumento5 páginasIncreased dietary α-linolenic acid has sex-specific effects upon eicosapentaenoic acid status in humans: re-examination of data from a randomised, placebo-controlled, parallel studyAlfina RahmaAinda não há avaliações
- LEUCOSELECT PHYTOSOME MODULATES SERUMDocumento16 páginasLEUCOSELECT PHYTOSOME MODULATES SERUMgiziklinikfkudayanaAinda não há avaliações
- Early Intervention Psych - 2021 - Susai - Omega 3 Fatty Acid in Ultra High Risk Psychosis A Systematic Review Based OnDocumento14 páginasEarly Intervention Psych - 2021 - Susai - Omega 3 Fatty Acid in Ultra High Risk Psychosis A Systematic Review Based OnMitchel Cordova LoaizaAinda não há avaliações
- Essential Fatty Acids v2Documento8 páginasEssential Fatty Acids v2SyamsulAinda não há avaliações
- Jurnal Nutri3Documento11 páginasJurnal Nutri3Winda SariAinda não há avaliações
- The Effect of Camelina Sativa OilDocumento11 páginasThe Effect of Camelina Sativa OilLau ToAinda não há avaliações
- Hierba de San JUanDocumento3 páginasHierba de San JUanBiol. Miguel Angel Gutiérrez DomínguezAinda não há avaliações
- Effects of n–3Documento9 páginasEffects of n–3Nilay CoşkunAinda não há avaliações
- Effects of Omega-3 Fatty Acids On Markers of Inflammation in Patients With Chronic Kidney DiseaseDocumento9 páginasEffects of Omega-3 Fatty Acids On Markers of Inflammation in Patients With Chronic Kidney DiseaseStefanie SuwitaAinda não há avaliações
- Omega 3 Fatty Acids Research PapersDocumento8 páginasOmega 3 Fatty Acids Research Papersvevuf1zad1w2100% (1)
- Kagan 2013Documento10 páginasKagan 2013punith kumarAinda não há avaliações
- Achieving a Healthy Omega BalanceDocumento19 páginasAchieving a Healthy Omega Balancemorasaki003Ainda não há avaliações
- Review Article: Omega-3 Fatty Acids and Depression: Scientific Evidence and Biological MechanismsDocumento17 páginasReview Article: Omega-3 Fatty Acids and Depression: Scientific Evidence and Biological MechanismsAna Paula Oliveira - NutricionistaAinda não há avaliações
- Depressive Symptoms, 3 Fatty Acids, and Inflammation inDocumento8 páginasDepressive Symptoms, 3 Fatty Acids, and Inflammation inSoulyogaAinda não há avaliações
- Protein Kinase Inhibition By: - 3 Fatty AcidsDocumento9 páginasProtein Kinase Inhibition By: - 3 Fatty AcidsStepss StepsAinda não há avaliações
- Nutritional Supplements in PT of ADHD - 2014Documento15 páginasNutritional Supplements in PT of ADHD - 2014GOLDFINCHAinda não há avaliações
- Artigo 15Documento8 páginasArtigo 15Maria Clara SalgadoAinda não há avaliações
- Is Low Dietary Intake of Omega-3 Fatty Acids Associated With Depression?Documento3 páginasIs Low Dietary Intake of Omega-3 Fatty Acids Associated With Depression?Sharon AdeleAinda não há avaliações
- Tryptophan Appetite Healthy: DepletionDocumento6 páginasTryptophan Appetite Healthy: DepletionRifqi Hamdani PasaribuAinda não há avaliações
- Omega-3 Supplements and Cardiovascular Diseases: TanaffosDocumento9 páginasOmega-3 Supplements and Cardiovascular Diseases: TanaffosNatalia LeeAinda não há avaliações
- Omega 3 Fatty Acid Supplementation in Advanced Kidney DiseaseDocumento5 páginasOmega 3 Fatty Acid Supplementation in Advanced Kidney DiseaseUriel FurlongAinda não há avaliações
- 135 - Possible MecanismsDocumento19 páginas135 - Possible MecanismsEduardo BacelarAinda não há avaliações
- Am J Cardiol Deha EpaDocumento10 páginasAm J Cardiol Deha EpajoremeAinda não há avaliações
- Badr Et Al, 2020Documento10 páginasBadr Et Al, 2020UrwaTariqAinda não há avaliações
- Increased Lipide Peroxidation During Long-Term Intervention With Hoght Doses of N-3 Fatty Acids (PUFAs) Following and Acute Myocardial InfactrionDocumento8 páginasIncreased Lipide Peroxidation During Long-Term Intervention With Hoght Doses of N-3 Fatty Acids (PUFAs) Following and Acute Myocardial InfactrionandresgarciafAinda não há avaliações
- Docosahexaenoic Acid (DHA) : MonographDocumento9 páginasDocosahexaenoic Acid (DHA) : MonographBen ClarkeAinda não há avaliações
- Dysphrenia 2012 3 1 01 Editorial Nutrition and Mental HealthDocumento4 páginasDysphrenia 2012 3 1 01 Editorial Nutrition and Mental HealthHaitry SamayoaAinda não há avaliações
- Deleterious Effect of N 3 Polyunsaturated Fatty Acids I - 2017 - Clinical NutritDocumento13 páginasDeleterious Effect of N 3 Polyunsaturated Fatty Acids I - 2017 - Clinical NutritRafaela MirandaAinda não há avaliações
- Ni Hms 485703Documento28 páginasNi Hms 485703Natalia LeeAinda não há avaliações
- Aplicações Óleo de Peixe Nos Cuidados Saúde PrimáriaDocumento9 páginasAplicações Óleo de Peixe Nos Cuidados Saúde PrimáriaVanessa Gama GalassoAinda não há avaliações
- Understanding the Cardioprotective Effects of Omega-3 Fatty AcidsDocumento7 páginasUnderstanding the Cardioprotective Effects of Omega-3 Fatty AcidskikevasquezAinda não há avaliações
- Omega 3 Fatty Acids: An In-Depth LookDocumento10 páginasOmega 3 Fatty Acids: An In-Depth LookSozdar ArgoshiAinda não há avaliações
- Brain Atrophy in Cognitively Impaired Elderly: The Importance of Long-Chain v-3 Fatty Acids and B Vitamin Status in A Randomized Controlled TrialDocumento8 páginasBrain Atrophy in Cognitively Impaired Elderly: The Importance of Long-Chain v-3 Fatty Acids and B Vitamin Status in A Randomized Controlled TriallauraAinda não há avaliações
- Research Digest: Exclusive Sneak PeekDocumento9 páginasResearch Digest: Exclusive Sneak PeekStashaAinda não há avaliações
- Nutrients-06-04058 - OMEGA 3Documento16 páginasNutrients-06-04058 - OMEGA 3Vanessa BarrosAinda não há avaliações
- Pufa PDFDocumento18 páginasPufa PDFChicinaș AlexandraAinda não há avaliações
- Polyunsaturated Fatty Acids, Specialized Pro-Resolving Mediators, and Targeting Inflammation Resolution in The Age of Precision NutritionDocumento8 páginasPolyunsaturated Fatty Acids, Specialized Pro-Resolving Mediators, and Targeting Inflammation Resolution in The Age of Precision NutritionAndrés Felipe Gutiérrez RodríguezAinda não há avaliações
- PHT3 AssignmentDocumento2 páginasPHT3 AssignmentJericho Basmayor SajulanAinda não há avaliações
- Nutrients: Maternal Docosahexaenoic Acid Status During Pregnancy and Its Impact On Infant NeurodevelopmentDocumento25 páginasNutrients: Maternal Docosahexaenoic Acid Status During Pregnancy and Its Impact On Infant NeurodevelopmentBeatrice Cynthia WalterAinda não há avaliações
- PIIS0022316622026001Documento9 páginasPIIS0022316622026001asagdaevAinda não há avaliações
- Chapter 136 - Watermelon (Citrullus Lanatus (Thunb.) Matsumura and Nakai) Seed Oils Pages 1149-1157Documento9 páginasChapter 136 - Watermelon (Citrullus Lanatus (Thunb.) Matsumura and Nakai) Seed Oils Pages 1149-1157Cassidy EnglishAinda não há avaliações
- Mustard Greens: What's New and Beneficial About Mustard GreensDocumento10 páginasMustard Greens: What's New and Beneficial About Mustard GreensShiv7_som784Ainda não há avaliações
- Ferain Et Al, 2016 - The Fatty Acid Profile of Rainbow Trout Liver Cells Modulates Their Tolerance To Methylmercury and CadmiumDocumento12 páginasFerain Et Al, 2016 - The Fatty Acid Profile of Rainbow Trout Liver Cells Modulates Their Tolerance To Methylmercury and Cadmiumarthur5927Ainda não há avaliações
- DFT Calculation and Raman Spectroscopy Studies ofDocumento7 páginasDFT Calculation and Raman Spectroscopy Studies ofyousif husseinAinda não há avaliações
- An008979 PDFDocumento20 páginasAn008979 PDFAisAinda não há avaliações
- Lipid Chemistry Functions and ClassificationsDocumento11 páginasLipid Chemistry Functions and Classificationsbero beroAinda não há avaliações
- ADM Feed Ingredients CatalogDocumento36 páginasADM Feed Ingredients CatalogHITESHAinda não há avaliações
- Position of The Academy of Nutrition and Dietetics: Vegetarian DietsDocumento10 páginasPosition of The Academy of Nutrition and Dietetics: Vegetarian DietsdialexeisAinda não há avaliações
- Fish Quality: Tuna Handling GuideDocumento30 páginasFish Quality: Tuna Handling GuideWinna Belinda MaulidinaAinda não há avaliações
- Nutrition Concerns and Health Effects of Vegetarian Diets: Winston John Craig, PHD, RDDocumento8 páginasNutrition Concerns and Health Effects of Vegetarian Diets: Winston John Craig, PHD, RDSarbu AndraAinda não há avaliações
- FAPAS 2022 2023 Lab Proficiency Testing Programme Price List GBPDocumento88 páginasFAPAS 2022 2023 Lab Proficiency Testing Programme Price List GBPOvianto DadangAinda não há avaliações
- About EPA and DHADocumento7 páginasAbout EPA and DHASha ShaAinda não há avaliações
- Linseed and Linseed Oil: Health Benefits-A Review: Vijaya Tripathi, A.B.Abidi, S. Marker, S.BilalDocumento9 páginasLinseed and Linseed Oil: Health Benefits-A Review: Vijaya Tripathi, A.B.Abidi, S. Marker, S.BilalKrissa sunastiAinda não há avaliações
- Effect of Vegan Diet VD On Sports Performance A Mechanistic Review of Metabolic CascadesDocumento23 páginasEffect of Vegan Diet VD On Sports Performance A Mechanistic Review of Metabolic Cascadeshaziq akmalAinda não há avaliações
- AwalMart Catalogue2Documento146 páginasAwalMart Catalogue2zulmalc100% (3)
- Introduction Too Leo ChemicalsDocumento67 páginasIntroduction Too Leo ChemicalsLeni Widiarti LenwidAinda não há avaliações
- Benefits of TurmericDocumento10 páginasBenefits of TurmericNorway Alinea MedinaAinda não há avaliações
- Canadian Encyclopedia of Natural MedicineDocumento455 páginasCanadian Encyclopedia of Natural MedicineNISAR_786Ainda não há avaliações
- Superfood PleasuresDocumento57 páginasSuperfood Pleasuresmmaidana2001100% (1)
- Nutrition Guide by Calisthenics FamilyDocumento25 páginasNutrition Guide by Calisthenics FamilyTommy MartelAinda não há avaliações
- Vasquez 2004 Part1 Diet FattyacidDocumento7 páginasVasquez 2004 Part1 Diet FattyacidAlex VasquezAinda não há avaliações
- Micronutrient DeficienciesDocumento71 páginasMicronutrient DeficienciesGelo Libelo100% (1)
- Chia Seed Benefits PDFDocumento8 páginasChia Seed Benefits PDFSellappan MuthusamyAinda não há avaliações
- Student Copy True Lipids TrueDocumento113 páginasStudent Copy True Lipids TrueSree Balaji Srinivas KatakamAinda não há avaliações
- Essential Fatty Acid Flax EPA ALADocumento7 páginasEssential Fatty Acid Flax EPA ALAlakshmibava100% (1)
- The Hidden Story of CancerDocumento74 páginasThe Hidden Story of CancerNasir Khan88% (8)
- 242 Vivinal Milk Fat Brochure PDFDocumento11 páginas242 Vivinal Milk Fat Brochure PDFCarlos MedinaAinda não há avaliações
- Natural Beauty Alchemy - Make Your Own Organic Cleansers, Creams, Serums, Shampoos, Balms, and More (PDFDrive)Documento326 páginasNatural Beauty Alchemy - Make Your Own Organic Cleansers, Creams, Serums, Shampoos, Balms, and More (PDFDrive)Stanislava Kirilova100% (2)
- Omega-3-6-9 Fatty Acids - A Complete Overview PDFDocumento1 páginaOmega-3-6-9 Fatty Acids - A Complete Overview PDFMunachande KanondoAinda não há avaliações
- Lipid Derived Flavor and Off Flavor of Traditional and Functional FoodsDocumento12 páginasLipid Derived Flavor and Off Flavor of Traditional and Functional FoodslangeldiazAinda não há avaliações