Escolar Documentos
Profissional Documentos
Cultura Documentos
Prostate Cancer Treatment: Unproven Proton Radiation Therapy Wastes Millions of Dollars
Enviado por
Center for American Progress0 notas0% acharam este documento útil (0 voto)
76 visualizações4 páginasNew proton therapy technology costs Medicare and seniors millions of dollars but offers zero improvement for prostate cancer patients.
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoNew proton therapy technology costs Medicare and seniors millions of dollars but offers zero improvement for prostate cancer patients.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
76 visualizações4 páginasProstate Cancer Treatment: Unproven Proton Radiation Therapy Wastes Millions of Dollars
Enviado por
Center for American ProgressNew proton therapy technology costs Medicare and seniors millions of dollars but offers zero improvement for prostate cancer patients.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 4
1 Center for American Progress | Prostate Cancer Treatment
Prostate Cancer Treatment:
Unproven Proton Radiation
Therapy Wastes Millions of Dollars
The High Price of Unnecessary Treatment
By Topher Spiro, Thomas Huelskoetter, and Gina Phillipi July 17, 2014
In this ongoing series, we analyze the recently released Medicare physician payment database
to identify wasteful spending by Medicare and seniors, including on treatments proven to be
inefective or in cases where equally efective alternatives to a high-priced treatment exist.
A growing controversy in medical circles concerns the treatment of prostate cancer with
proton beam radiation therapy. Tis relatively new treatment, used on a variety of cancers,
is provided in specially constructed facilities costing hundreds of millions of dollars.
1
In
order to recoup these hefy construction costs, proton therapy centers aggressively pro-
mote their services for a broad array of cancers, especially the relatively common prostate
cancer. However, there is currently zero evidence that proton radiation therapy is more
efective for treating prostate cancer than the alternative standard treatment, which is half
the cost.
2
With the number of proton therapy centers in the United States expected to
double in the next few years, Medicare and seniors face the prospect of rapidly increasing
prices for prostate cancer treatment, with no proven benefts for benefciaries.
3
Background
To date, studies have consistently shown proton radiation therapy, or PRT, to be no
more efective in treating prostate cancer than intensity-modulated radiation therapy,
or IMRT, the dominant treatment alternative that costs half what PRT does. IMRT is a
widely used, advanced version of radiation therapy.
4
PRT is a newer radiation technol-
ogy that uses positively charged particles known as protons.
5
In certain casesprimarily
for cancers in children and in sensitive regions such as the spinal cordPRT improves
safety by lowering the degree of toxicity to which the surrounding tissue is exposed.
6
However, for other cases, including prostate cancer, PRT ofers no improvement over
IMRT. Multiple studies have been unable to demonstrate any added clinical beneft
of PRT over IMRT for prostate cancer, and one recent study indicated no diference
2 Center for American Progress | Prostate Cancer Treatment
between the two in toxicity in prostate patients 12 months afer treatment.
7
Yet despite
this lack of apparent clinical beneft, almost 80 percent of Medicares spending on PRT
goes toward prostate cancer treatment.
8
Tis substantially increases the cost of treatment
for Medicare and seniors, since the median Medicare reimbursement for PRT is about
1.7 times higher than that for IMRT.
9
Despite these concerns, the United States currently
has 14 operational PRT centers, with at least 12
more under construction or in development.
10
Tese
facilities cost anywhere from $125 million to more
than $200 million to build and are roughly the size of
a football feld.
11
By 2017, they are expected to gar-
ner $1.17 billion in annual revenue.
12
Te question
relevant to taxpayers, Medicare, and seniors, then,
is where the PRT centers will fnd this revenue. By
one estimate, a $125 million center must treat 2,000
patients per year and generate more than $50 million
in annual revenue to turn a proft.
13
Although PRT is
recognized as a preferred option for treating chil-
dren and some specifc cancers, these cases are not
prevalent enough to fll the necessary spots in cen-
ters. Tus, proton therapy centers have aggressively
advertised their services for prostate cancer and
other more common forms of cancer to maximize
their revenue potential. Given these incentives, the
cost of PRT to Medicare will only grow over time,
even in cases where no medical basis for selecting PRT exists. Already, prostate patients
range from 10 percent to more than 50 percent of some proton therapy centers caseloads
and represent 79 percent of Medicares spending on proton therapy treatment.
14
Potential savings to Medicare and seniors
Medicare spent an estimated $22.4 million on proton beam radiation therapy for pros-
tate cancer in 2012. If IMRT had been used to treat all of these cases, Medicare would
have spent only $12.8 millionsaving $9.6 million.
15
Medicare benefciaries, meanwhile, would have saved an additional $2.4 million in out-
of-pocket costs such as co-insurance.
16
While the Medicare payment database does not
include patient data, it does indicate that 3,506 unique Medicare benefciaries received
proton beam radiation therapy. If all benefciaries received the same level of IMRT treat-
ment, savings would average $685 per senior. Te exact level of savings per senior would
depend on the doses received by each benefciary; while many seniors have supplemental
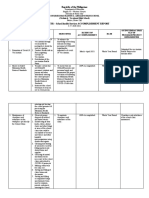
FIGURE 1
Proton radiation therapy versus intensity-modulated
radiation therapy
How much could we save by not using proton radiation therapy for
prostate cancer?
Sources: Center for American Progress analysis of Centers for Medicare & Medicaid Services, Medicare Provider
Utilization and Payment Data: Physician and Other Supplier (2012), available at http://www.cms.gov/Research-
Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-
Supplier.html; Stephanie Jarosek, Sean Elliott, and Beth Virnig, Proton beam radiotherapy in the U.S. Medicare
population: growth in use between 2006 and 2009 (Rockville, MD: Agency for Healthcare Research and Quality,
2012); James B. Yu and others, Proton Versus Intensity-Modulated Radiotherapy for Prostate Cancer: Patterns of
Care and Early Toxicity, Journal of the National Cancer Institute 105 (1) (2013): 2532.
Overall savings:
$12 million
Savings to Medicare $9.6 million
Savings to seniors
$2.4
million
Average per-beneciary
savings: $865
3 Center for American Progress | Prostate Cancer Treatment
coverage that covers co-insurance, premiums for this coverage would be
lower if it did not have to cover proton beam radiation therapy costs.
Savings to Medicare and benefciaries combined would have totaled
about $12 million in 2012.
17
Conclusion
Proton radiation therapy is a prime example of our health system
rushing headlong into an unproven, costly treatment. Medicare
wisely lowered its reimbursement amount for PRT in 2013 in order
to reduce the perverse incentives that have encouraged the prolif-
eration of PRT for cancers for which it ofers no added beneft.
20
Nevertheless, as the number of expensive proton therapy centers
remains on track to double in the next few years, PRT poses a growing
risk for a greater waste of taxpayer money.
Topher Spiro is the Vice President for Health Policy at the Center for
American Progress. Tomas Huelskoeter is the Special Assistant for
Health Policy at the Center. Gina Phillipi was formerly an intern on the
Health Policy team at the Center.
Te Center for American Progress thanks the Peter G. Peterson
Foundation for its support of our Health Policy programs and of this fact
sheet. Te views and opinions expressed in this fact sheet are those of the
Center for American Progress and the authors and do not necessarily
refect the position of the Peter G. Peterson Foundation. Te Center for
American Progress produces independent research and policy ideas driven
by solutions that we believe will create a more equitable and just world.
The Medicare payment database does not include
diagnosis information, so we used a Department of
Health and Human Services analysis to estimate the
percent of Medicares proton beam radiation spend-
ing that went toward prostate cancer treatment79
percent.
18
In addition, the Medicare databases billing
codes correspond to specic dose levels of both PRT
and IMRT that may not be directly comparable. To
work around this, we divided overall Medicare spend-
ing on PRT by the average Medicare payment amount
for the treatment, as calculated by a 2011 study.
IMRTs median reimbursement was $18,575, and PRTs
was $32,428.19 These prices include beneciary cost
sharingset at 20 percent of a treatments costso
we reduced these prices by 20 percent to isolate the
price paid by Medicare.
Dividing Medicare spending on PRT for prostate
cancer by the median price paid by Medicare gave
us an estimate of the number of treatments, which
we multiplied by the IMRT price to nd the cost of
treating these patients with IMRT. We subtracted
this cost from the proton beam radiation spending
for prostate cancer to estimate the potential savings
from switching to IMRT for these patients. Since this
only represented Medicare savings, we then calcu-
lated the value of the additional 20 percent to nd
beneciary savings.
Methodology
4 Center for American Progress | Prostate Cancer Treatment
Endnotes
1 Charlotte Huf, Catching the Proton Wave,The National
Association for Proton Therapy, available at, http://www.
proton-therapy.org/hhnarticle.htm (last accessed June
2014).
2 Ezekiel J. Emanuel and Steven D. Pearson, It Costs More, but
Is It Worth More?, The New York Times, January 2, 2012, avail-
able at http://opinionator.blogs.nytimes.com/2012/01/02/
it-costs-more-but-is-it-worth-more/.
3 Dan Browning, Mayos proton beam therapy adds to debate
over high-tech costs, Star Tribune, March 19, 2014, available
at http://www.startribune.com/lifestyle/health/250899661.
html#sH4HHfRlyoFcxlAW.97.
4 Palo Alto Medical Foundation, Intensity Modulated Radia-
tion Therapy (IMRT), available at http://www.pamf.org/
radonc/tech/imrt.html (last accessed May 2014).
5 Mayo Clinic Staf, Proton Therapy, Mayo Clinic, available
at http://www.mayoclinic.org/tests-procedures/proton-
therapy/basics/defnition/prc-20013308 (last accessed May
2014).
6 Daniela Schulz-Ertner and Hirohiko Tsujii, Particle Radiation
Therapy Using Proton and Heavier Ion Beams, Journal of
Clinical Oncology 25 (8) (2007): 953964.
7 Nathan Sheets and others, Intensity-Modulated Radiation
Therapy, Proton Therapy, or Conformal Radiation Therapy
and Morbidity and Disease Control in Localized Prostate
Cancer, Journal of the American Medical Association 307 (15)
(2012): 16111620; Bradford Hoppe and others, Compara-
tive efectiveness study of patient-reported outcomes after
proton therapy or intensity-modulated radiotherapy for
prostate cancer, Cancer 120 (7) (2014): 10761082; Aaron
Allen and others, An evidence based review of proton
beam therapy: The report of ASTROs emerging technology
committee, Radiotherapy & Oncology 103 (1) (2012): 811;
James B. Yu and others, Proton Versus Intensity-Modulated
Radiotherapy for Prostate Cancer: Patterns of Care and
Early Toxicity, Journal of the National Cancer Institute 105 (1)
(2013): 2532.
8 Stephanie Jarosek, Sean Elliot, and Beth Virnig, Proton
beam radiotherapy in the U.S. Medicare population: growth
in use between 2006 and 2009 (Rockville, MD: Agency for
Healthcare Research and Quality, 2012), available at http://
www.efectivehealthcare.ahrq.gov/ehc/products/439/1062/
Data-Points-10_20120529.pdf.
9 Roxanne Nelson, Uncertainty About Proton-Beam Radio-
therapy Lingers, Medscape, January 30, 2013, available at
http://www.medscape.com/viewarticle/778466.
10 Browning, Mayos proton beam therapy adds to debate
over high-tech costs.
11 Huf, Catching the Proton Wave.
12 Imaging Technology News, 27 U.S. Proton Therapy Centers
Expected by 2017, March 14, 2014, available at http://www.
itnonline.com/article/27-us-proton-therapy-centers-expect-
ed-2017.
13 Huf, Catching the Proton Wave.
14 Carolyn Y. Johnson, Proton beams vs. radiation: 5-year
MGH study seeks defnitive answers about costly prostate
cancer treatment, The Boston Globe, May 14, 2012,
available at http://www.boston.com/lifestyle/health/
articles/2012/05/14/is_proton_beam_therapy_a_bet-
ter_treatment_for_prostate_cancer_mass_general_trial_
to_answer_question/?page=full; Jarosek, Elliot, and Virnig,
Proton beam radiotherapy in the U.S. Medicare population.
15 CAP analysis of Centers for Medicare & Medicaid Services,
Medicare Provider Utilization and Payment Data: Physician
and Other Supplier (2012), available at http://www.cms.
gov/Research-Statistics-Data-and-Systems/Statistics-Trends-
and-Reports/Medicare-Provider-Charge-Data/Physician-
and-Other-Supplier.html.
16 Ibid.
17 Ibid.
18 Jarosek, Elliot, and Virnig, Proton beam radiotherapy in the
U.S. Medicare population.
19 Yu and others, Proton Versus Intensity-Modulated Radio-
therapy for Prostate Cancer.
20 Lauren Bonner, CMS wont budge on proton therapy cuts,
DOTmed, December 17, 2012, available at http://www.
dotmed.com/news/story/20140/.
Você também pode gostar
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Cognitive TherapyDocumento30 páginasCognitive TherapyDr. Jayesh Patidar100% (2)
- (PSYCH) 4.01 Forensic Psychiatry - Dr. Cruz PDFDocumento6 páginas(PSYCH) 4.01 Forensic Psychiatry - Dr. Cruz PDFMon Kristoper CastilloAinda não há avaliações
- Maternal & Child NotesDocumento19 páginasMaternal & Child NotesCailah Sofia SelausoAinda não há avaliações
- A Quality Alternative: A New Vision For Higher Education AccreditationDocumento25 páginasA Quality Alternative: A New Vision For Higher Education AccreditationCenter for American ProgressAinda não há avaliações
- Roles and Functions of Local Government UnitsDocumento3 páginasRoles and Functions of Local Government Unitsthepathfinderformercury100% (4)
- Incident Near Miss ReportingDocumento38 páginasIncident Near Miss ReportingKhaskheli Nusrat100% (3)
- An Infrastructure Plan For AmericaDocumento85 páginasAn Infrastructure Plan For AmericaCenter for American ProgressAinda não há avaliações
- Joy Wanjiru Midwifery Case StudyDocumento17 páginasJoy Wanjiru Midwifery Case StudyJimmy MainaAinda não há avaliações
- Leveraging U.S. Power in The Middle East: A Blueprint For Strengthening Regional PartnershipsDocumento60 páginasLeveraging U.S. Power in The Middle East: A Blueprint For Strengthening Regional PartnershipsCenter for American Progress0% (1)
- A Progressive Agenda For Inclusive and Diverse EntrepreneurshipDocumento45 páginasA Progressive Agenda For Inclusive and Diverse EntrepreneurshipCenter for American ProgressAinda não há avaliações
- Rhetoric vs. Reality: Child CareDocumento7 páginasRhetoric vs. Reality: Child CareCenter for American ProgressAinda não há avaliações
- Aging Dams and Clogged Rivers: An Infrastructure Plan For America's WaterwaysDocumento28 páginasAging Dams and Clogged Rivers: An Infrastructure Plan For America's WaterwaysCenter for American ProgressAinda não há avaliações
- Paid Leave Is Good For Small BusinessDocumento8 páginasPaid Leave Is Good For Small BusinessCenter for American ProgressAinda não há avaliações
- Housing The Extended FamilyDocumento57 páginasHousing The Extended FamilyCenter for American Progress100% (1)
- Preventing Problems at The Polls: North CarolinaDocumento8 páginasPreventing Problems at The Polls: North CarolinaCenter for American ProgressAinda não há avaliações
- Addressing Challenges To Progressive Religious Liberty in North CarolinaDocumento12 páginasAddressing Challenges To Progressive Religious Liberty in North CarolinaCenter for American ProgressAinda não há avaliações
- 3 Strategies For Building Equitable and Resilient CommunitiesDocumento11 páginas3 Strategies For Building Equitable and Resilient CommunitiesCenter for American ProgressAinda não há avaliações
- Closed Doors: Black and Latino Students Are Excluded From Top Public UniversitiesDocumento21 páginasClosed Doors: Black and Latino Students Are Excluded From Top Public UniversitiesCenter for American ProgressAinda não há avaliações
- Fast Facts: Economic Security For Arizona FamiliesDocumento4 páginasFast Facts: Economic Security For Arizona FamiliesCenter for American ProgressAinda não há avaliações
- Preventing Problems at The Polls: FloridaDocumento7 páginasPreventing Problems at The Polls: FloridaCenter for American ProgressAinda não há avaliações
- How Predatory Debt Traps Threaten Vulnerable FamiliesDocumento11 páginasHow Predatory Debt Traps Threaten Vulnerable FamiliesCenter for American ProgressAinda não há avaliações
- A Market-Based Fix For The Federal Coal ProgramDocumento12 páginasA Market-Based Fix For The Federal Coal ProgramCenter for American ProgressAinda não há avaliações
- Preventing Problems at The Polls: OhioDocumento8 páginasPreventing Problems at The Polls: OhioCenter for American ProgressAinda não há avaliações
- America Under Fire: An Analysis of Gun Violence in The United States and The Link To Weak Gun LawsDocumento46 páginasAmerica Under Fire: An Analysis of Gun Violence in The United States and The Link To Weak Gun LawsCenter for American Progress0% (1)
- Fast Facts: Economic Security For Illinois FamiliesDocumento4 páginasFast Facts: Economic Security For Illinois FamiliesCenter for American ProgressAinda não há avaliações
- The Path To 270 in 2016, RevisitedDocumento23 páginasThe Path To 270 in 2016, RevisitedCenter for American ProgressAinda não há avaliações
- Fast Facts: Economic Security For New Hampshire FamiliesDocumento4 páginasFast Facts: Economic Security For New Hampshire FamiliesCenter for American ProgressAinda não há avaliações
- Fast Facts: Economic Security For Virginia FamiliesDocumento4 páginasFast Facts: Economic Security For Virginia FamiliesCenter for American ProgressAinda não há avaliações
- Fast Facts: Economic Security For Wisconsin FamiliesDocumento4 páginasFast Facts: Economic Security For Wisconsin FamiliesCenter for American ProgressAinda não há avaliações
- The Missing Conversation About Work and FamilyDocumento31 páginasThe Missing Conversation About Work and FamilyCenter for American ProgressAinda não há avaliações
- Federal Regulations Should Drive More Money To Poor SchoolsDocumento4 páginasFederal Regulations Should Drive More Money To Poor SchoolsCenter for American ProgressAinda não há avaliações
- Opportunities For The Next Executive Director of The Green Climate FundDocumento7 páginasOpportunities For The Next Executive Director of The Green Climate FundCenter for American ProgressAinda não há avaliações
- Great Leaders For Great Schools: How Four Charter Networks Recruit, Develop, and Select PrincipalsDocumento45 páginasGreat Leaders For Great Schools: How Four Charter Networks Recruit, Develop, and Select PrincipalsCenter for American ProgressAinda não há avaliações
- A Clean Energy Action Plan For The United StatesDocumento49 páginasA Clean Energy Action Plan For The United StatesCenter for American ProgressAinda não há avaliações
- The Hyde Amendment Has Perpetuated Inequality in Abortion Access For 40 YearsDocumento10 páginasThe Hyde Amendment Has Perpetuated Inequality in Abortion Access For 40 YearsCenter for American ProgressAinda não há avaliações
- Workin' 9 To 5: How School Schedules Make Life Harder For Working ParentsDocumento91 páginasWorkin' 9 To 5: How School Schedules Make Life Harder For Working ParentsCenter for American ProgressAinda não há avaliações
- IND, NDA, ANDA IndiaDocumento51 páginasIND, NDA, ANDA IndiakbnarkhedeAinda não há avaliações
- Effectiveness of Gumamela (Hibiscus Rosa-Sinensis) : A ProposedDocumento8 páginasEffectiveness of Gumamela (Hibiscus Rosa-Sinensis) : A Proposedjani nakamotoAinda não há avaliações
- Ok Sa Deped Divmemo169 s.2018Documento19 páginasOk Sa Deped Divmemo169 s.2018Bella MelendresAinda não há avaliações
- NCP Post VaricocoelectomyDocumento4 páginasNCP Post VaricocoelectomyIris CaberteAinda não há avaliações
- SGO 2016 CPT Code RVUDocumento26 páginasSGO 2016 CPT Code RVUBrian SzenderAinda não há avaliações
- Vaccine Hesitancy Among Healthcare WorkersDocumento33 páginasVaccine Hesitancy Among Healthcare WorkersFitz Jaminit100% (1)
- PML Company Profile - Clinical TrialDocumento11 páginasPML Company Profile - Clinical Trialwisang geniAinda não há avaliações
- Timeline Presentation - 1940sDocumento10 páginasTimeline Presentation - 1940sapi-270879097Ainda não há avaliações
- Fda Abracair Air CleanerDocumento5 páginasFda Abracair Air Cleanerdecio ventura rodrigues miraAinda não há avaliações
- Required: Bharati Vidyapeeth (Deemed To Be University)Documento2 páginasRequired: Bharati Vidyapeeth (Deemed To Be University)Nitin KumarAinda não há avaliações
- Secretary List 30th November 2023Documento34 páginasSecretary List 30th November 2023Keshav KumarAinda não há avaliações
- Ebook Foundations of Mental Health Care PDF Full Chapter PDFDocumento67 páginasEbook Foundations of Mental Health Care PDF Full Chapter PDFronald.corlew644100% (23)
- Catherine Jenkins ReportDocumento60 páginasCatherine Jenkins Reportjupiter stationeryAinda não há avaliações
- 2nd Quarter - School Health Services Accomplishment ReportDocumento4 páginas2nd Quarter - School Health Services Accomplishment ReportJimmellee EllenAinda não há avaliações
- Medical Repricing-96105332Documento14 páginasMedical Repricing-96105332Mazlynn AmirAinda não há avaliações
- Quality of Postnatal Care ServicesDocumento10 páginasQuality of Postnatal Care Servicessaleha sultanaAinda não há avaliações
- Farmacoterapia en ObesidadDocumento29 páginasFarmacoterapia en ObesidadAnali Durán CorderoAinda não há avaliações
- Assessment: About Inflammatory Bowel Disease (IBD)Documento20 páginasAssessment: About Inflammatory Bowel Disease (IBD)NushurAinda não há avaliações
- IMDocumento5 páginasIMChimboy BartolomeAinda não há avaliações
- Triangle Insights - Should Antibiotics Enthusiasm Be TemperedDocumento8 páginasTriangle Insights - Should Antibiotics Enthusiasm Be TemperedJoya DelgadoAinda não há avaliações
- Sep 15 Final Cpsa LetterDocumento19 páginasSep 15 Final Cpsa LetterFatima Berriah CamposAinda não há avaliações
- SilgramDocumento6 páginasSilgramJacqueline SweetAinda não há avaliações
- Medical Leave FormatsDocumento1 páginaMedical Leave FormatsAdara deepAinda não há avaliações
- English 1301 Analysis WorksheetDocumento4 páginasEnglish 1301 Analysis Worksheetapi-709313609Ainda não há avaliações