Escolar Documentos
Profissional Documentos
Cultura Documentos
06
Enviado por
biotech_vidhyaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
06
Enviado por
biotech_vidhyaDireitos autorais:
Formatos disponíveis
Hong Kong Dermatology & Venereology Bulletin 172
Case Reports
Eruptive Xanthoma
Dr. W. K. Tang
CASE SUMMARY
History
A two-month-old girl with unremarkable birth
history presented with sudden onset of erythematous
papules on the limbs and face for one week. There was
no systemic upset, and she remained asymptomatic. Her
sister had a history of hypertriglyceridaemia under
treatment. The patient's other family members enjoyed
good physical health and there was no family history of
premature coronary heart disease.
Physical examination
There were multiple discrete erythematous,
yellowish papules over the limbs, anterior trunk and
face, more on the extensor surface, and some lesions
coalesced together to form small plaques (Figure 1).
The liver and spleen were slightly enlarged at two
centimetres below the costal margin. No mucosal
involvement or lipaemia retinalis was found. There was
no dysmorphism nor other congenital abnormality
detected. Darier's sign was negative.
Differential diagnosis
In view of the morphology and distribution of the
cutaneous lesions, eruptive xanthoma was strongly
suspected. However, papular xanthoma and xanthoma
disseminatum might at some stage of the disease share
comparable clinical features. Non-Langerhans' cell
histiocytosis especially juvenile xanthogranuloma and
generalized eruptive histiocytosis should also be
considered in the differential diagnosis. Although
Darier's sign was negative, mastocytosis could not be
excluded clinically.
Date: 14 March, 2001
Venue: Yaumatei Dermatology Clinic
Organizer: Social Hygiene Service, DH;
Clinico-pathological Seminar
Investigations
The patient was found to have raised fasting blood
sugar and lipid levels. The whole blood was milky on
st andi ng, whi ch si gni fi ed markedl y el evat ed
chylomicrons in the blood. Urine protein, sugar and
ketones were negative and the amylase level was not
raised. Complete blood picture with differential count
was normal. The renal and liver functions were also
unremarkable.
The patient's parents and elder sister were asked for
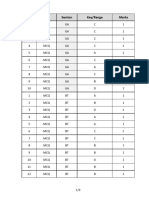
blood screening and the results were stated in Table 1.
Skin biopsy showed scattered foci of a few foam
cells in the superficial dermis, admixed with
lymphocytes, histiocytes and eosinophils. The overlying
epidermis was unremarkable. The features were
suggestive of eruptive xanthoma. Since the patient's
plasma lipoprotein lipase level was normal, abnormal
or deficient apoprotein C-II cofactor was suspected. It
was later confirmed by dramatic lowering of plasma
triglycerides after infusion of plasma from a normal
control.
Diagnosis
Based on the "sky-high" hypertriglyceridaemia and
histological findings, the diagnosis of eruptive xanthoma
Figure 1: Multiple yellowish papules over the right thigh
extensor surface
Vol.9 No.4, December 2001 173
Case Reports
was made. The early presentation, positive family
history of hypertriglyceridaemia and apoprotein C-II
deficiency point towards an underlying Type-I familial
hyperlipidaemia (Fredrickson classification).
Management
The patient was put on a low fat formula with a fat
content of 93% medium chain fatty acid and 7% long
chain fatty acid. Her fasting lipid and sugar improved
dramatically and returned towards normal (cholesterol
5.4 mmol/l, triglycerides 3.57 mmol/l and sugar 5.0
mmol/l). All skin eruption subsided about a month after
the dietary control.
REVIEW ON ERUPTIVE XANTHOMA
Eruptive xanthoma is characterized by small,
yellowish, cutaneous papules measuring 1-4 mm with
an erythematous halo. The lesions tend to arise abruptly
in crops and merge into patches on the extensor surface
of arms, legs, and buttocks, but may be more
generalized. This skin lesion can be found in patients
with a completely normal lipid level or those with an
underlying hypertriglyceridaemia, which is further
subdivided into familial and acquired forms.
1
These two
big categories will be discussed briefly below.
Hypertriglyceridaemia xanthomatosis
Familial
Fredrickson type I, IV and V familial hyper-
lipidaemia account for most of the familial hyper-
triglyceridaemia.
2
Type I and V are autosomal recessive
with absent lipoprotein lipase or its activator, apoprotein
C-II. Whereas type IV is autosomal dominant and the
catabolism of triglycerides rich lipoprotein is reduced
with overproduction of very low-density lipoproteins
(VLDL).
Other inherited metabolic diseases such as
lysosomal storage diseases and type I glycogen storage
disease (Von Gierke's) may also give rise to elevated
triglycerides and results in eruptive xanthoma.
Acquired
Causes commonly lead to eruptive xanthoma
include diabetes mellitus, alcohol ingestion, obesity,
chronic renal failure, nephrotic syndrome, pancreatitis,
hypothyroidism and biliary cirrhosis.
3
Medications
including estrogens, corticosteroids, miconazole,
isotretinoin, and etretinate
4
can lead to elevated lipid
level and cutaneous xanthoma.
Normolipaemic xanthomatosis
Development of xanthomas in the absence of
hyperlipoproteinaemia is not uncommon and was
described in detail by Parker.
5
Altered lipoprotein
content or structure, the presence of paraproteinaemia,
haematopoietic diseases such as histiocytosis,
myelomas and local trauma can cause eruptive
xanthoma despite the normal plasma lipid level. Other
caus es may i ncl ude t r auma or oedema.
6, 7
Normolipaemic eruptive xanthomas have also been
reported during pregnancy and in acquired total
lipodystrophy.
8
Pathogenesis
The high plasma concentration of lipoproteins
facilitates its permeation through dermal capillaries.
However, any conditions that increase the relative
vascular permeability to lipoproteins such as local
Table 1. The fasting lipids and blood sugars of the index patient and her family members. The high-density lipoprotein
(HDL) and low-density lipoprotein (LDL) levels in the patient and her sister could not be performed because of very high
triglycerides
Cholesterol mmol/l HDL mmol/l LDL mmol/l Triglycerides mmol/l Glucose mmol/l
Normal Range 3.5-6.5 0.70-2.1 (male) 1.55-4.4 0.70-2.1 (male)
(ideal <5.2) 0.50-1.70 (female) 0.50-1.70 (female) 4.5-5.6
Index Patient 13.0 83.2 20.7
Mother 6.7 1.17 4.84 1.51 5.0
Father 4.5 2.76 4.2
Sister 6.0 28.48 5.4
Hong Kong Dermatology & Venereology Bulletin 174
Case Reports
injury, oedema, altered lipoprotein structure or
paraproteins in the plasma, can also lead to lipoprotein
leakage into the dermis. Direct phagocytosis of
lipoproteins by dermal histiocytes or a reactive process
involving in-situ lipid synthesis in the histiocytes will
then evolve into foam cells.
9
Differential diagnosis
Clinically eruptive xanthoma may sometimes be
confused with other xanthomatosis or non-Langerhanss'
cell histiocytosis (Table 2).
10,11
Rarely the cutaneous
lesions may mimic Sweet's syndrome.
12
Most of the time
a skin biopsy can reliably differentiate eruptive
xanthoma from other xanthomatoses and non-
Langerhans' cell histiocytosis (Table 3).
Treatment
Treatment of eruptive xanthoma is directed to the
underlying causes. Since eruptive xanthoma secondary
to hypertriglyceridaemia typically responds well to
dietary control, a dietician's advice should be sought
first. In general, a low carbohydrates and saturated fat
diet is the first treatment of choice. Anti-hyperlipidaemic
agents should be considered when dietary control fails.
13
Prognosis
Unless the underlying causes can be corrected, the
patient should be put on life-long dietary control and
regular follow-up is needed. However patients can be
reassured that the cutaneous lesions and lipoprotein
abnormalities can revert to normal, in terms of weeks,
with appropriate treatment.
13
Table 2. Clinical features of the common differential diagnosis of eruptive xanthoma
Eruptive Papular Juvenile Xanthoma Generalized eruptive
xanthoma xanthoma xanthogranuloma disseminatum histiocytosis
Age Children, adult Mainly adult 80% <2year 60%<25year Mainly adult
Skin lesions Red-yellow Discrete yellowish Discrete orange Red-brown Red-brown papules
papules in crops papules -yellow nodule
Number of Multiple Multiple Solitary or Numerous Numerous
lesions numerous
Location Buttocks & thighs Face and trunk Head & upper Face, trunk, Trunk and limbs
& extensors, larger, do not tend trunk folds, proximal
tends to merge to merge extremities
Mucous Rare Uncommon Uncommon Characteristic Uncommon
membrane
Visceral Nil Nil Sometimes Characteristic Nil
involvement
Course Resolve over Self-limiting, Resolve in Resolve after Resolve during
several weeks come & go months/years several years childhood
Hyperlipidaemia + - - - -
Table 3. Brief summary of histological differences between eruptive xanthoma and its common differential diagnosis
Eruptive xanthoma Papular xanthoma/ Juvenile xanthogranuloma/
Other xanthoma Xanthoma disseminatum/
Monotonous infiltrate of foamy histiocytes Generalised eruptive histocytosis
Few foamy histiocytes in the Diffuse or nodular foamy Heterogeneous infiltrate of histiocytes with
early lesions, pattern is similar histiocytes with scanty variable composition of inflammatory
to interstitial granuloma inflammatory cells cells
annulare
Perivascular infiltration of
inflammatory cells, neutrophil
prominent
Vol.9 No.4, December 2001 175
Case Reports
Learning points:
Development of eruptive xanthoma is indicative
of an underlying hyper-triglyceridaemia.
Appropriate dietary changes, correction of
secondary factors along with antihyper-
lipidaemic agents, if needed, will lower plasma
triglycerides and allow the xanthomatous lesions
to resolve.
References
1. Ruggero C, Marcello M, Emilio B, Giovanni G. Normolipaemic
eruptive cutaneous xanthomatosis. Arch Dermatol 1986;12:
1294-7.
2. Antonio M, Gotto J. Clinical diagnosis of hyperlipoproteinaemia.
Am J Med 1983;74:5-9.
3. Parker F. Xanthomas and hyperlipidaemias. J Am Acad
Dermatol 1985;13:1-30.
4. Dicken CH, Connolly SM. Eruptive xanthomas associated
with isotretinoin (13-cis-retinoic acid). Arch Dermatol 1980;
116:951-2.
5. Parker F. Normocholesterolaemic xanthomatosis. Arch
Dermatol 1986;122:1253-6.
6. Goldstein GD. The Koebner phenomenon with eruptive
xanthomas. J Am Acad Dermatol 1984;10:1064-5.
7. Eeckhout I, Vogelaers D, Gleerts ML, Naeyaert JM. Xanthomas
due to generalized edema. Br J Dermatol 1997;136:601-3.
8. Mahmoud SF Lawrence. Seip Syndrome: Report of a case from
Egypt. Cutis 1997;60:91-3.
9. Ghislaine R, Marianne X, Jean D. Eruptive and tubero-eruptive
xanthomas of the skin arising on sited of prior injury; two case
reports. JAMA 1988;260:1282-3.
10. Ferrando J, Campo-Voegeli A, Soler-Carrillo J, et al. Systemic
xanthohistiocytoma: a variant of xanthoma disseminatum? Br
J Dermatol 1998;138:155-60.
11. Zelger BW, Sidoroff A, Orchard G, Cerio R. Non-Langerhans
cell histiocytoses. A new unifying concept. Am J Dermatopathol
1996;18:490-504.
12. Ahn SJ, Choi JH, Sung KJ, Moon KC, Koh JK. Sweet's
syndrome presenting with lesions resembling eruptive
xanthoma. Br J Dermatol 2000;143:449-50.
13. Archer CB, Macdonald DM. Eruptive xanthoma in type V
hyperlipoprotaeinemia associated with diabetes mellitus. Clin
Exp Dermatol 1984;9:312-6.
Você também pode gostar
- Facs ProtocolDocumento7 páginasFacs ProtocolmisterxAinda não há avaliações
- Whole Cell ExtractDocumento1 páginaWhole Cell Extractbiotech_vidhyaAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- Q.No. Type Section Key/Range MarksDocumento3 páginasQ.No. Type Section Key/Range Marksbiotech_vidhyaAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- BT 2019Documento13 páginasBT 2019biotech_vidhyaAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- TNPSC Group 1 Prelim Book List PDFDocumento2 páginasTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaAinda não há avaliações
- Polymerasen GuideDocumento16 páginasPolymerasen Guidebiotech_vidhyaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Stripping For ReprobingDocumento2 páginasStripping For ReprobingStella SalvatoreAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Stripping For ReprobingDocumento2 páginasStripping For ReprobingStella SalvatoreAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Troubleshooting SDS-PAGE 1Documento3 páginasTroubleshooting SDS-PAGE 1biotech_vidhyaAinda não há avaliações
- Polymerase Chain Reaction (PCR)Documento3 páginasPolymerase Chain Reaction (PCR)biotech_vidhyaAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Brad FordDocumento12 páginasBrad FordQi ChaoAinda não há avaliações
- TNPSC Group 1 Prelim Book List PDFDocumento2 páginasTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- SDS PageDocumento2 páginasSDS Pagebiotech_vidhyaAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Components Reaction MixtureDocumento3 páginasComponents Reaction Mixturebiotech_vidhyaAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Buffer Preparation Guide for DNA/Protein Work (Shi LabDocumento6 páginasBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Buffer Preparation Guide for DNA/Protein Work (Shi LabDocumento6 páginasBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Qpaper PondyDocumento21 páginasQpaper Pondybiotech_vidhyaAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- Nuclear ExtractsDocumento2 páginasNuclear Extractsbiotech_vidhyaAinda não há avaliações
- TDC 41597 A (Mechanical Engg.) - 2012Documento20 páginasTDC 41597 A (Mechanical Engg.) - 2012biotech_vidhyaAinda não há avaliações
- Img Word-To PDFDocumento3 páginasImg Word-To PDFbiotech_vidhyaAinda não há avaliações
- Ies 17 Set A Me Q ADocumento67 páginasIes 17 Set A Me Q Abiotech_vidhyaAinda não há avaliações
- TNPSC Group 1 Prelim Book List PDFDocumento2 páginasTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaAinda não há avaliações
- ESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionDocumento52 páginasESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionpataAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Mechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010Documento20 páginasMechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010biotech_vidhyaAinda não há avaliações
- Befcv List PDFDocumento22 páginasBefcv List PDFbiotech_vidhyaAinda não há avaliações
- A.E. (Mechanical Engineering I) 2007Documento24 páginasA.E. (Mechanical Engineering I) 2007Mukesh KumarAinda não há avaliações
- Qpaper PondyDocumento21 páginasQpaper Pondybiotech_vidhyaAinda não há avaliações
- 1 TolerancesDocumento1 página1 Tolerancesbiotech_vidhyaAinda não há avaliações
- Recruitment RulesDocumento5 páginasRecruitment Rulesbiotech_vidhyaAinda não há avaliações
- Part and Mold Design GuideDocumento170 páginasPart and Mold Design GuideminhtintinAinda não há avaliações
- CBSE Class 4 Social Studies Worksheet - Means of TransportDocumento4 páginasCBSE Class 4 Social Studies Worksheet - Means of TransportNancy Amelia RosaAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Bleeding DisorderDocumento3 páginasBleeding DisorderyanzwinerAinda não há avaliações
- Publications On Multimorbidity 01 PDFDocumento146 páginasPublications On Multimorbidity 01 PDFWalter MendozaAinda não há avaliações
- 3D CD Technique Completes Dentures in 3 Days for ElderlyDocumento5 páginas3D CD Technique Completes Dentures in 3 Days for ElderlyMaulida Dara HarjantiAinda não há avaliações
- Merck Veterinary ManualDocumento264 páginasMerck Veterinary Manualschmooshie91% (11)
- ProjectDocumento64 páginasProjectPradip DindaAinda não há avaliações
- Retinopathy of Prematurity Handout FormatDocumento31 páginasRetinopathy of Prematurity Handout FormatkaznielsAinda não há avaliações
- Scott-Sinema Medicare Advantage LetterDocumento2 páginasScott-Sinema Medicare Advantage LetterRachel CohrsAinda não há avaliações
- UTI in PregnancyDocumento47 páginasUTI in PregnancyAli MahmoudAinda não há avaliações
- Good Medical Practice Nov12 - 2019Documento13 páginasGood Medical Practice Nov12 - 2019Fransiscus RivaldyAinda não há avaliações
- Health Information SystemDocumento14 páginasHealth Information SystemRoberto MendozaAinda não há avaliações
- Brazilian Sanitary Guide For Cruise ShipsDocumento82 páginasBrazilian Sanitary Guide For Cruise ShipsStanislav KozhuharovAinda não há avaliações
- Interpretation: L63 - Ankit Jain Sagar Cc-3 I/F HDFC Bank Parkota Ward Goughat SAGAR-470002 M.PDocumento2 páginasInterpretation: L63 - Ankit Jain Sagar Cc-3 I/F HDFC Bank Parkota Ward Goughat SAGAR-470002 M.PAviral SinghAinda não há avaliações
- The Lancet, 2018Documento70 páginasThe Lancet, 2018dessyAinda não há avaliações
- Froelich Syndrome and HomoeopathyDocumento13 páginasFroelich Syndrome and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- LECTURE 4 Introduction To MicrobiologyDocumento36 páginasLECTURE 4 Introduction To MicrobiologyArcee Feb Dela PazAinda não há avaliações
- Gross Pathology SpringerDocumento2 páginasGross Pathology SpringerThalia ChristabelAinda não há avaliações
- Cdi Reviewer MidtermDocumento8 páginasCdi Reviewer MidtermKIMBERLY MARGARETTE REDAinda não há avaliações
- Pulmonary Embolism: Presented By: Miss. M.K.Kaku Nursing TutorDocumento9 páginasPulmonary Embolism: Presented By: Miss. M.K.Kaku Nursing TutorKaku ManishaAinda não há avaliações
- Dr. Khalid - S Explanation of 1700 MCQ1Documento683 páginasDr. Khalid - S Explanation of 1700 MCQ1heba100% (1)
- Form 3 - Patient Care Report (PCR) FormDocumento2 páginasForm 3 - Patient Care Report (PCR) FormMdrrmo Pamplona Camarines SurAinda não há avaliações
- Database Management SystemDocumento12 páginasDatabase Management Systemaklesh parteAinda não há avaliações
- TubercolosisDocumento8 páginasTubercolosisNitesh Bhura100% (1)
- MCQ Exam 2Documento13 páginasMCQ Exam 2Anwaar YousafAinda não há avaliações
- Daftar Max - Min Obat / Barang di ApotekDocumento38 páginasDaftar Max - Min Obat / Barang di ApotekMeta JuliaAinda não há avaliações
- Herbalage Products KnowledgeDocumento25 páginasHerbalage Products Knowledgemail9246Ainda não há avaliações
- Test Bank of Neurocognitive DisordersDocumento27 páginasTest Bank of Neurocognitive DisordersmAinda não há avaliações
- Đề Cương Môn Tiếng Anh Chuyên Ngành Ngành: DượcDocumento11 páginasĐề Cương Môn Tiếng Anh Chuyên Ngành Ngành: DượcNguyễn Thị Hương75% (8)
- Work in Team EnvironmentDocumento50 páginasWork in Team EnvironmentMercy Dadulla - ElvinaAinda não há avaliações
- Endophthalmitis 1Documento42 páginasEndophthalmitis 1Nasrin sultana rmcAinda não há avaliações
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNo EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionNota: 4 de 5 estrelas4/5 (402)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNo EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingNota: 5 de 5 estrelas5/5 (4)
- The Age of Magical Overthinking: Notes on Modern IrrationalityNo EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityNota: 4 de 5 estrelas4/5 (13)
- The Happiness Trap: How to Stop Struggling and Start LivingNo EverandThe Happiness Trap: How to Stop Struggling and Start LivingNota: 4 de 5 estrelas4/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeAinda não há avaliações
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNo EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsNota: 3.5 de 5 estrelas3.5/5 (3)