Escolar Documentos
Profissional Documentos
Cultura Documentos
Postpartum Maternal Physical Assessment Summary
Enviado por
Alyanna EvangelistaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Postpartum Maternal Physical Assessment Summary
Enviado por
Alyanna EvangelistaDireitos autorais:
Formatos disponíveis
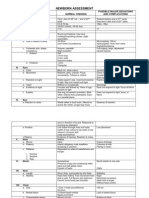
Postpartum Maternal Physical Assessment Summary- BUBBLE HE
Breasts:
inspect: size, symmetry, shape of breast and nipples taking note of erection, flatness, redness, bruising, open wounds, presence of
mastitis and colostrum
palpate: fullness, soft or engorged, firmness and lumps
pain assessment
Uterus (Fundus):
palpate: firmness/bogginess, location of the fundus in relation to the abdomen, determine the location of the fundus in relation to
the belly button to determine amount of fundal involution
inspect incision site
check policy: in some organizations, they may not assess fundal involution by palpation due to fear of dehiscence
Bladder:
void amount (~30ml/hr)
assess for distention, incontinence, urinary retention, urinary infection especially if the patient had a foley catheter
Bowel:
last bowel movement/flatus
assess for distention, abdominal pain
Lochia:
amount, color, odour
assess for postpartum hemorrhage
Episiotomy
level of laceration
number of stitches, redness, edema, bruisin, discharge, approximation of wound edges
assess perineal area
Homans Sign-for DVT
assess for pain with dorsiflexion
check policy: this is sometimes not done in organizations
Emotional State:
assess for signs and symptoms of postpartum depression and infant-maternal bonding
Postpartum physical adaptations
Uterus continued
Changes in Fundal Position
Immed after placenta expelled:
Uterus contracts to compress blood vessels
Size of large grapefruit
Fundus in midline, about half way to 2/3 way between umbilicus and symphysis pubis
Rises to level of navel about 6-12 hours after delivery changes in ligaments
Fundus above umbilicus and soft and spongy (boggy) associated with excess bleeding
If high and displaced to side (usually right), prob secondary to full bladder
Empty bladder and reassess
Postpartum physical adaptations
Uterus continued
Uterus remains at level of umbilicus about day
after birth
On first day following birth top of fundus about
1cm below umbilicus
Fundus descends about 1 fingerbreadth or 1 cm
daily
Descends into pelvis on 10
th
day, can no longer be
palpated
Returns to pre-preg size and location by 5-6 wks
If descends slower, called subinvolution
Postpartum physical adaptations
Lochia
Debris eliminated in discharge called lochia, is
classified according to appearance
Lochia rubra:
Dark red, first 2-3 days after delivery
Clotting result of pooling in vagina, nickel size
clots otherwise ok
Lochia serosa:
Pinkish to brownish
3-10 days pp
Lochia alba:
Yellowish-whitish
Duration varies
Postpartum physical adaptations
Lochia
When lochia stops, cervix is closed, less chance
of uterine infection
Total lochia blood loss volume is 225 mL
Volume decreases gradually, may increase with
nursing, exertion
Normal odor slightly musty, non-offensive
Foul odor to lochia suggests infection
Assessment of lochia necessary
Type, amt of lochia corresponds to involution &
healing of placental site
Failure of lochia to progress and decrease in
amount = subinvolution or PP hemorrhage
If continuous bright red seep with firm uterus
right after birth, must consider possibility of
laceration
Postpartum physical adaptations
Cervical Changes
Spongy and flabby, formless after birth
Reforms with in few hours & closes slowly, by
end of first week will only admit fingertip
Shape permanently changed
Vaginal Changes
May be edematous and bruised, no rugae
Size decreases and rugae returns in 3-4 wks,
normal by 6 wks
Can improve tone with Kegels exercises
If nursing may be dry, pale
Postpartum physical adaptations
Perineal Changes
Appears swollen and bruised
If episiotomy or laceration, should be well approx
Should be healed by 2-3 weeks after delivery
with complete healing by 4-6 months
May have some discomfort during this time
Recurrence of Ovulation and Menstruation
Generally 6-10 wks after birth if not nursing
If nursing, return is prolonged
Depends on length of breastfeeding and
supplements
Not reliable form of contraception
Postpartum physical adaptations
Abdomen
Appears loose and flabby
Responds to exercise with in 2-3 months
If abdomen over distended or poor muscle tone
pre-preg, may not regain tone, remains flabby
Diastasis recti abdominis
Is separation of abdominis muscles
Often occurs with preg, especially if poor abd
tone
Abdominal wall has no muscle support
Improvement depends on cond of mom, type and
amt of exercise, number of pregnancies and spacing
May result in pendulous abd
Striae
Results from rupture of elastic fibers of skin
Fade to silvery white if Caucasian
If dark skin, they stay darker than surrounding
skin
Postpartum physical adaptations
Gastrointestinal system
Hunger, thirst immediately after birth common
Bowels tend to be sluggish
d/t progesterone, decreased abdominal tone
If episiotomy scared will hurt or tear sutures
with BM
Nursing interventions may help prevent, relieve
If C/S, clear liq till bowel sounds, then solid food
Postpartum physical adaptations
Urinary system
At risk for over distention, incomplete emptying
with residual urine d/t
Increased bladder capacity
Swelling and bruising of tissues around urethra
Decreased sensation of full bladder (anesthetic
block)
Output first 12-24 hrs pp (PP diuresis)
Eliminate 2000-3000 mL preg fluid, more if PIH
Fills bladder quickly, watch closely for distention
Risk of UTI high
Full bladder will also uterine relaxation, bleeding
Postpartum physical adaptations
Vital signs Should be afebrile after 24 hrs
May have temp up to 100.4 F (38 C) for 24 hrs d/t
dehydration
May also have elevation of 100 to 102 F (37.8-39
C) when milk comes in
BP may spike immediately after delivery
Should have normal BP within few days
Orthostatic hypotension common first couple days
Decrease = hemorrhage versus normal?
Increase = preeclampsia, excess oxytocin use?
Decreased pulse common for first 6-10 days PP
Pulse > 100 related to hemorrhage, fear, pain,
infection
Postpartum physical adaptations
Blood values
Values return to normal by 6-8 wk after delivery
Increased coagulation factors continue for
variable time, increases risk for blood clot
Blood loss averages
H & H difficult to determine in first 2 days pp d/t
changing blood volume (diuresis)
200-500 cc with vag del
700-1000cc with C/S
Rule of thumb 2 point drop in Hct = 500 mL
blood lost
WBC increases in labor & early pp to 25,000-
30,000
Platelets return to normal by 6 weeks
Postpartum physical adaptations
Cardiovascular changes
Blood volume increases because no longer has
blood circulating to placenta
Works to protect mother against excess blood loss
Diuresis decreases extracellular fluid
If fails to happen, can lead to pulmonary edema
esp in mother with preeclampsia or existing cardiac
problems
Weight loss
10-12 # immediately after birth (infant, placenta,
amniotic fluid)
Diuresis additional 5# first wk
By 6-7 wks return to pre-preg wt if gained normal
amt
Postpartum physical adaptations
Afterpains
Are intermittent contrx of uterus
More common in multips, retained placenta or
with overdistention of uterus
Oxytocin & breastfeeding increases afterpains
Can use mild analgesic 1 hour before nursing
May be very uncomfortable for 2-3 days
Usually gone in 5 minutes
Postpartal Nursing Physical Assessment
Physical Assessment see guide pg 1001-1004
Explain to pt purposes
Record and report results
Avoid exposure to body fluids
Teach pt as assess use q opportunity since
limited time
Post Partum Nursing Assessment
Assessment necessary to identify individual needs
or potential problems
See page 1053-1055 for complete assessment
guide
Also see table on page 1052 about postpartal high
risk factors and their implications
Term BUBBLEHE can help remember
components
breast, uterus, bladder, bowel, lochia, episiotomy,
Homans/hemorrhoids, emotional
Principles in assessment of pp woman
Provide explanation of assessment to client
Perform procedures gently to avoid unnecessary
discomfort
Record and report results
Take appropriate precautions to prevent exposure
to body fluids
Provides excellent opportunity for client teaching
about physical changes of pp and common concerns
Post Partum Nursing Assessment
Vital signs
Alterations in VS can indicate complications
already discussed
Lung auscultation
Lungs should be clear
Women treated for PTL, PIH @ risk for
pulmonary edema
Post Partum Nursing Assessment
Breasts
Assess fit and support of bra
Helps maintain shape by limiting stretching of
ligaments and connective tissue
Bra for nursing mother
Non-elastic straps
Be one size larger than normal
Have cups that fold down for nursing
Breast assessment
Inspect for redness, engorgement
Palpate for warmth, firmness of filling or
engorgement, tenderness
In nursing women:
Assess nipples for cracks, bleeding, soreness,
fissures, inversion
Post Partum Nursing Assessment
Abdomen and Fundus pg 1057 -1058
Pt should void prior to checking fundus
Uterus positioned better
More comfortable to client
Position pt on back with legs flexed
Assess relationship of fundus to umbilicus,
midline
Assess firmness of uterus
Massage prn if not firm
Assess any blood discharged during massage
Assess gently, uterus slightly tender
Excessive pain with palpation clue to infection
If cesarean
Palpate fundus gently
Assess incision (REEDA, patency of staples)
Post Partum Nursing Assessment
If uterine atony (boggy):
Question patient about her bleeding, passage of
clots
Re-eval bladder
Babe to breast if nursing
Assess maternal BP, pulse
Notify MD since may need oxytocic med
Post Partum Nursing Assessment
Lochia pg 1059
Assess for character, amt, odor, clots
Should never be more than moderate amt with
non-offensive odor:
Partially saturate 4-8 pads, 6 average/day
Women with C/S bleed less first day than vag del
Also assess womans pad changing practices, her
type of pad
Assess chux pad
If pt reports heavy bleeding, change pad, reassess
in 1 hr
If need accurate assessment, can weigh pad; 1g =
1cc
Teach proper wiping, progression of lochia
Post Partum Nursing Assessment
Perineum pg 1061-1062
Inspect with pt in Sims position
Lift buttock to expose perineum, anus
If present, assess episiotomy or laceration for
REEDA
Should have minimal tenderness with gentle
palpation
No hardened areas or hematomas
Also assess hemorrhoids: size, pain
Evaluate effectiveness of any comfort measures
performed
Educate about suture absorption
Post Partum Nursing Assessment
Lower Extremities
PP woman at increased risk of thrombophlebitis,
thrombus formation; most likely site is legs
To screen, use Homans sign (not diagnostic)
Nurse grasps foot and dorsiflexes sharply
Should have no calf pain
If positive for pain notify MD
Check for edema, redness, tenderness, warmth of
leg
Prevention best
Early ambulation
Passive ROM for cesarean client till sensation
returns
Teach
Signs and symptoms to watch after discharge
Self care for prevention ambulate, leg exercises
in bed, avoid crossing legs and pressure behind
knees
Post Partum Nursing Assessment
Elimination
Urinary
Should void within 4 hours, then q 4-6 hours
Monitor bladder carefully first few hrs (diuresis)
Watch for distention
Misplaced or boggy uterus, palpable bladder signs
Check to see if empty first few times
Use techniques to encourage void
If cant void after 8 hours or voiding small (<100
mL) amounts frequently, then cath
Evaluate for fluid intake, ask if bladder feels
empty, UTI symptoms
Post Partum Nursing Assessment
Elimination
Bowels
Ask about concerns
Evaluate whether having stools since delivery
Constipation causes pressure on sutures, increases
discomfort
To avoid constipation:
Stool softeners
Encourage ambulation
Force fluids (>2000mL/day)
Fresh fruits and veggies
Post Partum Nursing Assessment
Rest status
Requires energy to make adjustments to
motherhood and infant
Fatigue often significant problem
Evaluate amount of rest mother is getting
Determine cause of not sleeping, use appropriate
interventions
Encourage daily rest period
Arrange activities in hospital
Post Partum Nursing Assessment
Nutritional status
Non-nursing
Decrease calories by 300/day
Return to pre-preg nutritional requirements
If nursing
Increases calories by 200 over preg level or 500
over pre-preg level
Refer to dietician if vegetarian, food allergies,
lactose intolerance or have specific food needs
related to culture/religion
Advise iron supplements, prenatal vitamins for 3
months esp if nursing
Postpartal Psychologic Adaptations
PP time of adjustment and adaptation to new
baby, pp discomfort, change in body, loss of
pregnancy
2 periods of adjustment:
Taking in period
First couple days, tends to be passive, dependent
Hesitates to make decisions, follows suggestions
Preoccupied with her needs
Must assimilate experience
Talks about labor, sorts out reality
Sleep, eat is major focus
Postpartal Psychologic Adaptations
Periods of adjustment
Taking hold period
By 2
nd
3
rd
day ready to resume control of body, mothering and her life
Needs reassurance needed shes doing well as mother
This theory 40 years old, slightly outdated as women more independent today
Adjust more rapidly in shorter time periods than these
Você também pode gostar
- Meditation ScriptDocumento9 páginasMeditation Scriptapi-361293242100% (1)
- Postpartum Teaching PlanDocumento3 páginasPostpartum Teaching Plan6bigstar991% (11)
- Maternal and Child NursingDocumento30 páginasMaternal and Child NursingJack Bisarra Sanchez0% (1)
- Incompetent CervixDocumento29 páginasIncompetent CervixCyrelle Jen TorresAinda não há avaliações
- Newborn AssessmentDocumento7 páginasNewborn AssessmentMJ Amarillo100% (6)
- Child Abuse Nursing Care PlanDocumento7 páginasChild Abuse Nursing Care PlanMAHESH KOUJALAGIAinda não há avaliações
- AntepartumDocumento32 páginasAntepartumphoenix180100% (1)
- Postpartum Nursing Care Fa 10 Nur 263Documento63 páginasPostpartum Nursing Care Fa 10 Nur 263EddogawaAinda não há avaliações
- Postpartum LectureDocumento21 páginasPostpartum LectureFelisa Lacsamana Gregorio0% (1)
- Newborn CarePlanDocumento8 páginasNewborn CarePlanXtin Buendia Cordero0% (1)
- Script - DefenseDocumento3 páginasScript - DefenseAlyanna Evangelista100% (3)
- Chapter 24: Nursing Care of A Family During A Surgical Intervention For BirthDocumento22 páginasChapter 24: Nursing Care of A Family During A Surgical Intervention For BirthAlyssaGrandeMontimorAinda não há avaliações
- Unang YakapDocumento3 páginasUnang YakapBernadeth Labrador100% (1)
- OB Nursing Care PlanDocumento4 páginasOB Nursing Care PlanJustin AncogAinda não há avaliações
- Handout On The Concept of Health and Health EducationDocumento5 páginasHandout On The Concept of Health and Health Educationmomo connorAinda não há avaliações
- BubbleDocumento12 páginasBubblekarloeguiareyesAinda não há avaliações
- NCM 109 Resource UnitDocumento51 páginasNCM 109 Resource UnitDaryl Adrian RecaidoAinda não há avaliações
- NCM 107 LecDocumento16 páginasNCM 107 LecSheila May SantosAinda não há avaliações
- Postpartum LectureDocumento64 páginasPostpartum LectureStephen Gabriel TitoAinda não há avaliações
- Postpartum CareDocumento13 páginasPostpartum CareChristian100% (11)
- Complications of PregnancyDocumento40 páginasComplications of PregnancyNatalie Pemberton100% (1)
- NSVD Case StudyDocumento11 páginasNSVD Case StudyMichael UrrutiaAinda não há avaliações
- Newborn AssessmentDocumento3 páginasNewborn AssessmentValerie Ybañez Peñalber100% (2)
- Essential Intrapartum and Newborn CareDocumento23 páginasEssential Intrapartum and Newborn CareEarl ReyesAinda não há avaliações
- Chapter 015 PSDocumento11 páginasChapter 015 PSJann ericka Jao100% (1)
- MCN QuizDocumento6 páginasMCN QuizMÖna Macaranas100% (5)
- Post PartumDocumento18 páginasPost PartumStefanie Kelly JimeneaAinda não há avaliações
- DischargeDocumento4 páginasDischargePatricia Franco100% (1)
- Occupational Health NursingDocumento1 páginaOccupational Health NursingAlyanna EvangelistaAinda não há avaliações
- Postpartum Physical AssessmentDocumento60 páginasPostpartum Physical Assessmentalmyr_rimandoAinda não há avaliações
- Perinatal Manual of Southwestern OntarioDocumento6 páginasPerinatal Manual of Southwestern OntarioƦя de GuzмѧN100% (1)
- Intrapartum CareDocumento14 páginasIntrapartum CareChristian80% (5)
- 8 Point Postpartum Assessment WorksheetDocumento2 páginas8 Point Postpartum Assessment WorksheetSoni Ali100% (2)
- Discharge Instructions For Your NewbornDocumento10 páginasDischarge Instructions For Your Newbornbeauty100% (1)
- Body Template 1998Documento7 páginasBody Template 1998itayAinda não há avaliações
- Labor and Delivery OB Concept MapDocumento2 páginasLabor and Delivery OB Concept MapMissy Johnson75% (4)
- Initial Newborn AssessmentDocumento14 páginasInitial Newborn Assessmentaclark831Ainda não há avaliações
- Maternity Case 1: Olivia Jones (Core) : Guided Reflection QuestionsDocumento3 páginasMaternity Case 1: Olivia Jones (Core) : Guided Reflection QuestionsDai Nguyen100% (1)
- Ob 1Documento13 páginasOb 1iandame100% (1)
- Care Plan PostpartumDocumento2 páginasCare Plan PostpartumSiwei Yang100% (1)
- Guidelines For Contemporary Air-Rotor StrippingDocumento6 páginasGuidelines For Contemporary Air-Rotor StrippingGerman Cabrera DiazAinda não há avaliações
- Newborn AssessmentDocumento17 páginasNewborn Assessmentryancohen1100% (1)
- Actual Nursing Care Plan 2Documento16 páginasActual Nursing Care Plan 2Alyanna Evangelista100% (2)
- MCN Prenatal AssessmentDocumento9 páginasMCN Prenatal Assessmentaibuty100% (1)
- Dela Rosa 2A MCN-Module 04Documento4 páginasDela Rosa 2A MCN-Module 04Atsu MiyaAinda não há avaliações
- Fetal DistressDocumento5 páginasFetal DistressRonnie Portillo Cruz100% (1)
- NSVDDocumento48 páginasNSVDchiqui14100% (2)
- Nursing Care Plan 3 Risk For Altered ParentingDocumento7 páginasNursing Care Plan 3 Risk For Altered Parentingdbryant010178% (9)
- Group 1 Interprofessional Care Map PDFDocumento1 páginaGroup 1 Interprofessional Care Map PDFanette katrin0% (1)
- Nursing Care PlanDocumento7 páginasNursing Care Planrockerespi1283Ainda não há avaliações
- Family Coping IndexDocumento54 páginasFamily Coping IndexdsenpenAinda não há avaliações
- MOPON MCNDocumento3 páginasMOPON MCNDannielle EvangelistaAinda não há avaliações
- ECOMAP Community Health Nursing CHNDocumento1 páginaECOMAP Community Health Nursing CHNmAinda não há avaliações
- Drugs - OBDocumento7 páginasDrugs - OBglennarthurAinda não há avaliações
- Nursing Care PlansDocumento5 páginasNursing Care PlansYannah Mae EspineliAinda não há avaliações
- Careplan NewBornDocumento2 páginasCareplan NewBornVic DangAinda não há avaliações
- How To Perform LeopoldDocumento5 páginasHow To Perform LeopoldChared Lumba100% (3)
- Sample Letter Templates (4th Year)Documento49 páginasSample Letter Templates (4th Year)Yna LafuenteAinda não há avaliações
- Newborn Careplan 9-15-2011Documento17 páginasNewborn Careplan 9-15-2011Brittany Wood100% (1)
- Family Caseload Presentation Barangay BalagbagDocumento6 páginasFamily Caseload Presentation Barangay BalagbagCharmae NaveaAinda não há avaliações
- Stages of Labor Nursing ConsiderationsDocumento5 páginasStages of Labor Nursing Considerationsneleh gray100% (2)
- Nursing Crib Com NURSING CARE PLAN Spontaneous AbortionDocumento2 páginasNursing Crib Com NURSING CARE PLAN Spontaneous AbortionJustin PasaronAinda não há avaliações
- Dysfunctional Labor As One of The Intrapartal ComplicationsDocumento23 páginasDysfunctional Labor As One of The Intrapartal ComplicationsKenje Kate AgripoAinda não há avaliações
- Normal Postpartum: Jodie Fuller, MSN, RN Jennie Hensley, CNM, EddDocumento69 páginasNormal Postpartum: Jodie Fuller, MSN, RN Jennie Hensley, CNM, EddmcneiljmAinda não há avaliações
- Postpartum - Physiology and NSG Care 15Documento33 páginasPostpartum - Physiology and NSG Care 15yuuki konnoAinda não há avaliações
- Postpartum Physical AssessmentDocumento60 páginasPostpartum Physical AssessmentJhgrace Mary Pacaña Gallo100% (1)
- Post Partum Nursing NotesDocumento35 páginasPost Partum Nursing NotesyolondanicAinda não há avaliações
- Basic VocabularyDocumento1 páginaBasic VocabularyAlyanna EvangelistaAinda não há avaliações
- Method 6 of 6: Other Basic VocabularyDocumento1 páginaMethod 6 of 6: Other Basic VocabularyAlyanna EvangelistaAinda não há avaliações
- 'Back-To-Basics' Grammar Tests For 11-Year-Olds Revealed: by Andrew Marszal, Digital Education EditorDocumento2 páginas'Back-To-Basics' Grammar Tests For 11-Year-Olds Revealed: by Andrew Marszal, Digital Education EditorAlyanna EvangelistaAinda não há avaliações
- ProjectDocumento6 páginasProjectAlyanna Evangelista100% (1)
- Attendance For ReportDocumento1 páginaAttendance For ReportAlyanna EvangelistaAinda não há avaliações
- AreaDocumento2 páginasAreaAlyanna EvangelistaAinda não há avaliações
- Compiled Labs Normal ValuesDocumento7 páginasCompiled Labs Normal ValuesAlyanna EvangelistaAinda não há avaliações
- Rehabilitation: Engracia, Angelie Chariz B. Evangelista, Alyanna F. Mombille, Anamie TDocumento19 páginasRehabilitation: Engracia, Angelie Chariz B. Evangelista, Alyanna F. Mombille, Anamie TAlyanna EvangelistaAinda não há avaliações
- SCRIPT On Our ProposalDocumento2 páginasSCRIPT On Our ProposalAlyanna EvangelistaAinda não há avaliações
- Pulse OximeterDocumento18 páginasPulse OximeterAlyanna Evangelista100% (1)
- Iii. Medical ManagementDocumento3 páginasIii. Medical ManagementAlyanna EvangelistaAinda não há avaliações
- My Narrative ReportDocumento3 páginasMy Narrative ReportAlyanna EvangelistaAinda não há avaliações
- NARQ40007-PROCESS - Beauty Parlor ManagementDocumento3 páginasNARQ40007-PROCESS - Beauty Parlor ManagementYogesh ThakurAinda não há avaliações
- Sample Massage Therapy Business Plan TemplateDocumento8 páginasSample Massage Therapy Business Plan Templatewealth nwaiwuAinda não há avaliações
- Marchand 2012Documento20 páginasMarchand 2012Elton MatsushimaAinda não há avaliações
- Eeh455 Assignment2b MaharpDocumento22 páginasEeh455 Assignment2b Maharpapi-267478292Ainda não há avaliações
- The Ethics of Helping Transgender Men and Women Have ChildrenDocumento16 páginasThe Ethics of Helping Transgender Men and Women Have ChildrenAnonymous 75M6uB3OwAinda não há avaliações
- F17 Reflection 383 FN - 15 Nov 17Documento7 páginasF17 Reflection 383 FN - 15 Nov 17jigsawAinda não há avaliações
- Treatment and Prognosis of Febrile Seizures - UpToDateDocumento14 páginasTreatment and Prognosis of Febrile Seizures - UpToDateDinointernosAinda não há avaliações
- 3 Colinet Dustsampling PDFDocumento21 páginas3 Colinet Dustsampling PDFom pandeyAinda não há avaliações
- JHU Press Fall 2013 CatalogDocumento99 páginasJHU Press Fall 2013 CatalogjhupressAinda não há avaliações
- SPS and TBT MeasuresDocumento4 páginasSPS and TBT MeasuresValentina Vasquez CasallasAinda não há avaliações
- BMI W HFA Validated (3!24!2017)Documento151 páginasBMI W HFA Validated (3!24!2017)jeffordillasAinda não há avaliações
- Cancer Treatment - Capsaicin - Oil RecipeDocumento4 páginasCancer Treatment - Capsaicin - Oil RecipeJESUS IS RETURNING DURING OUR GENERATIONAinda não há avaliações
- Block-D FinalDocumento47 páginasBlock-D FinalAnonymous 7IKdlmAinda não há avaliações
- Chapter I Related Literature Teenage PreDocumento12 páginasChapter I Related Literature Teenage PreWilkenn Tuazon100% (3)
- Validity and Reliability Study of The Turkish Version of Ego Identity Process QuestionairreDocumento6 páginasValidity and Reliability Study of The Turkish Version of Ego Identity Process QuestionairreSergio F. GonzalezAinda não há avaliações
- Advancements in The Bbutilization of Azolla Anabaena System in RelationDocumento17 páginasAdvancements in The Bbutilization of Azolla Anabaena System in Relationryana_soesantieAinda não há avaliações
- Break The Cycle Activity GuidesDocumento19 páginasBreak The Cycle Activity GuidesJuanmiguel Ocampo Dion SchpAinda não há avaliações
- Mental HealthDocumento14 páginasMental Healthapi-455779994100% (1)
- Effect of A Program of Physical Activity Motivated by Lipid Parameters of Patients With Obesity and or Overweight PDFDocumento6 páginasEffect of A Program of Physical Activity Motivated by Lipid Parameters of Patients With Obesity and or Overweight PDFMarlio Andres Vargas PolaniaAinda não há avaliações
- Lecture #3 - Carbohydrates & LipidsDocumento23 páginasLecture #3 - Carbohydrates & Lipidsogangurel100% (3)
- HCM 239Documento199 páginasHCM 239Mohit VermaAinda não há avaliações
- Networker PerelDocumento7 páginasNetworker PerelPaula JiménezAinda não há avaliações
- TNF-dental PulpDocumento3 páginasTNF-dental PulpNicolas PintoAinda não há avaliações
- Strengthening Health Emergency Management System Through The ILHZDocumento7 páginasStrengthening Health Emergency Management System Through The ILHZCliff GubatAinda não há avaliações
- TSS 30 - Application Form - SODocumento4 páginasTSS 30 - Application Form - SOkemvanAinda não há avaliações
- Clinical Practice Guidelines: High-Grade Glioma: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDocumento9 páginasClinical Practice Guidelines: High-Grade Glioma: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpSiva SubramaniamAinda não há avaliações