Escolar Documentos
Profissional Documentos
Cultura Documentos
Assignment #1 - PEDIA (GIT)
Enviado por
Kerima Danica Lising Gayo0 notas0% acharam este documento útil (0 voto)
245 visualizações1 páginaCharacteristic cough of laryngotracheobronchitis will be dry and hacking. Characteristic cough of spasmodic croup will be barking and "seal-like" pyloric stenosis is diagnosed in an infant with vomiting with increasing frequency.
Descrição original:
Título original
Assignment #1 - PEDIA(GIT)
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoCharacteristic cough of laryngotracheobronchitis will be dry and hacking. Characteristic cough of spasmodic croup will be barking and "seal-like" pyloric stenosis is diagnosed in an infant with vomiting with increasing frequency.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
245 visualizações1 páginaAssignment #1 - PEDIA (GIT)
Enviado por
Kerima Danica Lising GayoCharacteristic cough of laryngotracheobronchitis will be dry and hacking. Characteristic cough of spasmodic croup will be barking and "seal-like" pyloric stenosis is diagnosed in an infant with vomiting with increasing frequency.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 1
PEDIATRIC NURSING- HOMEWORK # 1
Name: Score: /25
1 of 1 | P a g e
1. A student nurse is caring for a 2-year-old child diagnosed with
croup. A nursing instructor asks the student about the clinical
manifestation associated with croup. Which statement by the
student indicates a need for further research?
a. Inspiratory stridor and a low-grade fever may be
present.
b. The cough is harsh and brassy.
c. Symptoms usually worsen at night and are better during
the day.
d. Symptoms usually worsen during the day and are
relieved during sleep.
2. The characteristic cough of laryngotracheobronchitis will be:
a. dry and hacking
b. moist and productive
c. barking and seal-like
d. spasmodic with wheezing
3. Two early symptoms that may occur in LTB or spasmodic croup are:
a. cough and inspiratory stridor
b. kussmaul breathing and bradycardia
c. elevated temperature and vomiting
d. flushed face and wheezing
4. A 4 week old infant is admitted with a tentative diagnosis of pyloric
stenosis. During the admission assessment, the nurse bicycles the
infants legs before palpating the abdomen. This enables the nurse
to:
a. Assess abdominal rebound
b. Palpate abdominal contour
c. Relax the abdominal muscle
d. Detect weak abdominal muscle
5. A 6 week old infant is brought to the clinic by her parents. They state
that their baby has been vomiting with increasing frequency and
force after feeding. Pyloric stenosis is diagnosed. The nurse is
aware that the manifestations of pyloric stenosis are:
a. Avid hunger and non bile stained vomitus
b. Severe abdominal pain and visible peristaltic waves
c. Vomiting several hours after a feeding and tarry
stools
d. Bile stained vomitus and generalized abdominal
distention
6. The mother of an infant with pyloric stenosis asks the nurse many
questions about the problem. When answering these questions the
nurse convey the idea that:
a. Surgery will be necessary
b. Chromosomal mutation is the cause
c. Slow feeding is necessary for a few months
d. Dietary restrictions will be required throughout
childhood
7. A 10 week old is diagnosed as having pyloric stenosis and is
scheduled for surgery. Oral feedings are usually initiated a few
hours after surgery. The nurse expects that initially the baby will
receive:
a. Clear liquids
b. Full strength formula
c. Half strength formula
d. Thickened formula with cereal
8. An infant who has surgery for pyloric stenosis is being fed by the
mother. To decrease the chance of vomiting after feedings, the
nurse teaches her that after a feeding the baby should be:
a. Rocked for 20 minutes
b. Placed in an infant seat
c. Positioned flat on the right side
d. Kept awake with sensory stimulation
9. An infant is to be discharged following surgery of pyloric stenosis.
The mother should be instructed to:
a. Give the baby creamy cereal at each feeing
followed by the regular formula
b. Continue the regular formula, hold the baby during
feedings, feed the baby slowly and burp frequently
c. Give the baby about 1 ounce of regular formula per
hour for the next two weeks; progressing slowly, as
tolerated, to larger amounts
d. Feed the regular formula while the baby is in the
crib positioned on the right side; handle the baby as
little as possible for two hours after each feeding
10. A newborn with a cleft lip is fed with a special nipple. To minimize
regurgitation of the feedings the nurse instructs the mother to:
a. Hold and burp the baby after feeding
b. Give the baby the thickened formula as ordered
c. Feed the baby while sitting the baby up in an infant
seat
d. Lay the baby on the side with the bottle firmly
propped
11. Immediate nursing care for a neonate born with a cleft lip is directed
primarily toward:
a. Modifying feeding methods
b. Keeping the baby from crying
c. Minimizing handling by parents
d. Preventing the occurrence of infection
12. During the initial post operative period after one month old infant has
had a cleft lip repair, the nurse should fed the infant using a:
a. Spoon
b. Nipple
c. 10mL syringe
d. Nasogastric tube
13. The first action by the nurse after each feeding of an infant with a
recent surgical repair of cleft lip should be:
a. Burp the infant several times
b. Place the infant on the abdomen
c. Cuddle the infant for a few minutes
d. Clean and rinse the suture line of the lip
14. A priority nursing measure for an infant during the immediate post
operative period following a surgical repair of a cleft lip is to:
a. Minimize the infants crying
b. Restraint the infant at all times
c. Oxygenate the infant frequently
d. Handle the infant as little as possible
15. To help the child retain tube feedings and avoid aspiration, the
nurse should place the child in the:
a. Prone position
b. Semi fowlers position
c. Left side lying position
d. Supine position with head turned
16. A mother asks why her 1 year old toddlers cleft palate was not
repaired at the time the cleft lip was repaired at 3 months of age.
The nurses best response would be:
a. Waiting leaves time for other birth defects to be
detected and corrected.
b. Cleft lip was so disfiguring that plastic surgery was
done as quickly as possible.
c. Your surgeon prefers to separate the operations to
minimize and prevent complications.
d. The palate is corrected after teething and before
your child talks so that correct speech may be
learned.
17. The physician orders arm restraints for a 1 year old who just had
surgery for a cleft palate. The nurse is aware that the reason for the
restraints is to prevent the child from:
a. Playing with unsterile toys
b. Rolling to a supine position
c. Putting fingers into the mouth
d. Pulling out the nasogastric tube
18. When a toddler with a cleft palate repair is able to tolerate fluids, the
nurse should administer the fluids with a:
a. Small cup
b. Bulb syringe
c. Lambs nipple
d. Teflon coated spoon
19. The nurse bases the care plan for an infant with celiac disease on
pathophysiology believe to cause this disorder, which would be an
inborn error of metabolism characterized by:
a. Excessive salt in the sweat glands
b. An absence of the enzyme peptidase
c. Excessive viscosity of the mucous glands
d. An absence of the enzyme phenylalanine
20. When obtaining history from the mother of an infant with celiac
disease, the nurse would expect the mother to say that he baby:
a. Is irritable at all times
b. Has bulky, foul, frothy stools
c. Drinks large amount of fluids
d. Voids strong, concentrated urine
21. The nurse recognizes that the diagnoses of celiac disease can be
performed when a jejunal biopsy reveals:
a. Small areas of fatty plaques
b. Atrophic changes in the mucosal wall
c. Irregular areas of superficial ulcerations
d. Diffuse degenerative fibrosis of the acini
22. Discharge planning for a toddler newly diagnosed with celiac
disease includes instructions related to dietary restrictions. The
nurse recognizes that the mother understands the instructions when
she states that the foods she will withhold from the diet:
a. Beef, pork, chicken
b. Eggs, milk, rice, krispies
c. Corn crisps, spinach, cheese
d. Chocolate milk, whole wheat toast, fruit
23. After being on a dietary regimen for celiac disease for six months,
the childs compliance to the diet can be evaluated by assessing
the:
a. Physical and emotional progress
b. Ability to handle stressful situations
c. Understanding of the disease process
d. Knowledge of foods allowed on the diet
24. In addition to teaching the mother of a toddler with celiac disease
the specific foods allowed on gluten restricted diet, the nurse should
help the mother understand that:
a. This diet will be discontinued in three to five years
b. She must read the labels of all prepared foods
carefully
c. All grains contain gluten; therefore non can be
include in the diet
d. The caloric intake will be adjusted to compensate
for the deficient protein intake
25. A homecare nurse instructs the mother about dietary measures for a
5-year-old child with lactose intolerance. The nurse tells the mother
that it is necessary to provide which dietary supplement in the childs
diet?
a. Fats
b. Calcium
c. Protein
d. Zinc
Você também pode gostar
- Pedia 1Documento4 páginasPedia 1Aijem Ryan100% (2)
- CHF RevisedDocumento74 páginasCHF RevisedAbigael Patricia GutierrezAinda não há avaliações
- Newborn Exam ChecklistDocumento4 páginasNewborn Exam ChecklistJJAinda não há avaliações
- Perioperative Nursing ManagementDocumento19 páginasPerioperative Nursing ManagementSarah SeverreAinda não há avaliações
- 100 Items Ob - CompressDocumento15 páginas100 Items Ob - CompressKirsten FeologAinda não há avaliações
- Harden vs Benguet | Mining Contract Dispute ResolvedDocumento3 páginasHarden vs Benguet | Mining Contract Dispute ResolvedNeil BorjaAinda não há avaliações
- Pediatric Checklist EditedDocumento72 páginasPediatric Checklist EditedJun Man100% (2)
- Maternal and Child HealthDocumento28 páginasMaternal and Child Health지창욱Ainda não há avaliações
- Chapter 17Documento11 páginasChapter 17missy23papAinda não há avaliações
- Pediatric Nursing Exam Review: Growth, Development and Common ConditionsDocumento21 páginasPediatric Nursing Exam Review: Growth, Development and Common ConditionsChristianmel JavierAinda não há avaliações
- Downloadfile 2Documento8 páginasDownloadfile 2Michael SilvaAinda não há avaliações
- Risk Factors and Nursing Care for Neurological ConditionsDocumento4 páginasRisk Factors and Nursing Care for Neurological ConditionsKrizia R. PingkeAinda não há avaliações
- 60 Item Pediatric Nursing Exam by JeddahDocumento10 páginas60 Item Pediatric Nursing Exam by Jeddahchelljynxie100% (1)
- Hirschprung's Disease, Celiac Disease, Hydrocephalus, Poisoning, Child Abuse, Anemia, Respiratory DisordersDocumento139 páginasHirschprung's Disease, Celiac Disease, Hydrocephalus, Poisoning, Child Abuse, Anemia, Respiratory DisordersJhoms Poja FeriaAinda não há avaliações
- PediaDocumento6 páginasPediaエニエルカム オレーバンAinda não há avaliações
- QuestionsDocumento6 páginasQuestionsLorvic Andrew Juanson UmaliAinda não há avaliações
- Nutritional Foundations and Clinical Applications 5th Edition Grodner Test BankDocumento10 páginasNutritional Foundations and Clinical Applications 5th Edition Grodner Test BankKareemAinda não há avaliações
- Electrolyte ImbalanceDocumento4 páginasElectrolyte ImbalanceDoneva Lyn MedinaAinda não há avaliações
- Pre-Test Maternal and Child Health NursingDocumento18 páginasPre-Test Maternal and Child Health NursingDefensor Pison GringgoAinda não há avaliações
- Pediatric Nursing - Respiratory DisordersDocumento9 páginasPediatric Nursing - Respiratory Disordershasan ahmdAinda não há avaliações
- Prof. Sandra M. Covarrubias - September 24, 2021: 5.2fluid & Electrolytes ImbalancesDocumento5 páginasProf. Sandra M. Covarrubias - September 24, 2021: 5.2fluid & Electrolytes ImbalancesIvy VillalobosAinda não há avaliações
- Labor Process and Nursing Care GuideDocumento9 páginasLabor Process and Nursing Care GuideMary Florence VelardeAinda não há avaliações
- Fabella NICUDocumento4 páginasFabella NICURoel Dominic BasilanAinda não há avaliações
- Peds Exam 3Documento61 páginasPeds Exam 3Katie Morgan EdwardsAinda não há avaliações
- Pulmonary Hypertension: Causes, Symptoms, Diagnosis and TreatmentDocumento10 páginasPulmonary Hypertension: Causes, Symptoms, Diagnosis and TreatmentCkaye GansubinAinda não há avaliações
- Febrile SeizuresDocumento11 páginasFebrile SeizuresLita Al AmudiAinda não há avaliações
- Oc Ob Set ADocumento10 páginasOc Ob Set AmatrixtrinityAinda não há avaliações
- Pharmacology Common Drugs and Its AntidotesDocumento6 páginasPharmacology Common Drugs and Its AntidotesKira86% (7)
- Tutorials On GenitourinaryDocumento15 páginasTutorials On Genitourinaryabangjojo123Ainda não há avaliações
- Physical AssessmentDocumento51 páginasPhysical AssessmentJasmin Jacob100% (2)
- Bowel EliminationDocumento4 páginasBowel Eliminationdlneisha61100% (3)
- QUIZ 8-Gen - PathDocumento27 páginasQUIZ 8-Gen - PathDrbee10Ainda não há avaliações
- GASTROINTESTINAL NURSING: NON-INVASIVE PROCEDURESDocumento14 páginasGASTROINTESTINAL NURSING: NON-INVASIVE PROCEDURESVoid LessAinda não há avaliações
- Pediatric Nursing Practice Test Part 1Documento15 páginasPediatric Nursing Practice Test Part 1Mikaela Angeles NazarAinda não há avaliações
- Low-residue diet and colonoscopy options for diverticular diseaseDocumento3 páginasLow-residue diet and colonoscopy options for diverticular diseaseTanya ViarsAinda não há avaliações
- BluePrint 5th QuestionsDocumento25 páginasBluePrint 5th QuestionsAbuFreihAinda não há avaliações
- Pediatric Nursing (Nomral) : Psychiatric (Sigmund Freud) Nursing Concept Range Extends To The 18 MonthDocumento6 páginasPediatric Nursing (Nomral) : Psychiatric (Sigmund Freud) Nursing Concept Range Extends To The 18 MonthVon R SemillaAinda não há avaliações
- Obstetric Case Study CesarianDocumento16 páginasObstetric Case Study CesarianRazan NasereddineAinda não há avaliações
- Cord CoilDocumento2 páginasCord CoilAlphine DalgoAinda não há avaliações
- NP2 Nursing Board Exam December 2006 Answer KeyDocumento16 páginasNP2 Nursing Board Exam December 2006 Answer KeyShine LynAinda não há avaliações
- Obstetric Nursing: Antepartum, Complications, Intrapartum, PostpartumDocumento7 páginasObstetric Nursing: Antepartum, Complications, Intrapartum, PostpartumMycz DoñaAinda não há avaliações
- Pedia-Reviewer CompleteDocumento36 páginasPedia-Reviewer CompletePotato BroAinda não há avaliações
- Individual Case PresentationDocumento20 páginasIndividual Case Presentationim. EliasAinda não há avaliações
- Ob FinalDocumento43 páginasOb FinalPrincess LotusAinda não há avaliações
- UtangDocumento11 páginasUtangmaimaiAinda não há avaliações
- Care of Clients with Genitourinary DisordersDocumento61 páginasCare of Clients with Genitourinary DisordersAngelica Kaye BuanAinda não há avaliações
- Lec 7 Care of Clients With Problems in Oxygenation Part 1Documento185 páginasLec 7 Care of Clients With Problems in Oxygenation Part 1Chucky VergaraAinda não há avaliações
- Obstetrics and GynecologyDocumento36 páginasObstetrics and GynecologyLeiAinda não há avaliações
- Jay ObDocumento6 páginasJay ObJenxAinda não há avaliações
- Pediatric Nursing CA Sir Archie Alviz 04-09-2022Documento3 páginasPediatric Nursing CA Sir Archie Alviz 04-09-2022Jonah MaasinAinda não há avaliações
- Croup SyndromeDocumento3 páginasCroup SyndromeMabesAinda não há avaliações
- Endo GI Extra QuestionsDocumento3 páginasEndo GI Extra QuestionsToni Marie Buenconsejo PunzalanAinda não há avaliações
- The Format: Case Study FormDocumento17 páginasThe Format: Case Study FormJane DyAinda não há avaliações
- MCQ On Heart DiseaseDocumento10 páginasMCQ On Heart DiseaseSucheta Ghosh ChowdhuriAinda não há avaliações
- MCN (Icons)Documento7 páginasMCN (Icons)Angelica Charisse BuliganAinda não há avaliações
- Types of LeadershipDocumento13 páginasTypes of LeadershipMary Roan RonatoAinda não há avaliações
- Pediatric Nursing PrioritiesDocumento6 páginasPediatric Nursing PrioritiesJavier Shields83% (6)
- Pedia Disorders Upgraded For Lnu CaDocumento6 páginasPedia Disorders Upgraded For Lnu Cashirlenedel cariñoAinda não há avaliações
- Understanding Child DevelopmentDocumento73 páginasUnderstanding Child DevelopmentPrince Jhessie L. AbellaAinda não há avaliações
- Pediatric Nursing Practice QuestionsDocumento10 páginasPediatric Nursing Practice QuestionsSurendra Momidi100% (2)
- Philippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFDocumento140 páginasPhilippine CPG On The Diagnosis and Management of Urinary Tract Infections in Adults-2015 Update - Part 2 PDFspringdingAinda não há avaliações
- World Water Day Celebration 201703092017114838Documento2 páginasWorld Water Day Celebration 201703092017114838Kerima Danica Lising GayoAinda não há avaliações
- Ho HohohohohoDocumento1 páginaHo HohohohohoKerima Danica Lising GayoAinda não há avaliações
- A Model of Burnout Process Gil MonteDocumento15 páginasA Model of Burnout Process Gil MonteEsmeralda TorresAinda não há avaliações
- Doctor ClassificationDocumento1 páginaDoctor ClassificationKerima Danica Lising GayoAinda não há avaliações
- Sources: 2014 Revision. Retrieved FromDocumento1 páginaSources: 2014 Revision. Retrieved FromKerima Danica Lising GayoAinda não há avaliações
- InterventionDocumento4 páginasInterventionKerima Danica Lising GayoAinda não há avaliações
- Community Health Nursing Board ExamDocumento15 páginasCommunity Health Nursing Board Examrhenier_ilado86% (14)
- Assignment #1 - PEDIA (GIT)Documento1 páginaAssignment #1 - PEDIA (GIT)Kerima Danica Lising GayoAinda não há avaliações
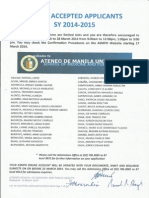
- Official Results For SY2014-2015Documento6 páginasOfficial Results For SY2014-2015Marguerite Alcazaren de LeonAinda não há avaliações
- St. LukesDocumento5 páginasSt. LukesKerima Danica Lising GayoAinda não há avaliações
- Raw Labs MayorDocumento1 páginaRaw Labs MayorKerima Danica Lising GayoAinda não há avaliações
- 1.) Title PageDocumento1 página1.) Title PageKerima Danica Lising GayoAinda não há avaliações
- MBA 290-Strategic AnalysisDocumento110 páginasMBA 290-Strategic AnalysisTammy252Ainda não há avaliações
- ECG Exercise, Insights, Ang HighlightsDocumento5 páginasECG Exercise, Insights, Ang HighlightsKerima Danica Lising GayoAinda não há avaliações
- EBP Suction Dan Dressing Pada Trachheostomy CareDocumento3 páginasEBP Suction Dan Dressing Pada Trachheostomy CareDani NurseAinda não há avaliações
- Magna Carta of Public Health Workers ActDocumento12 páginasMagna Carta of Public Health Workers ActKerima Danica Lising GayoAinda não há avaliações
- Philippine Patient's Bill of RightsDocumento6 páginasPhilippine Patient's Bill of Rightsplethoraldork98% (49)
- CiticolineDocumento2 páginasCiticolineKerima Danica Lising GayoAinda não há avaliações
- Amphothericin BDocumento2 páginasAmphothericin BKerima Danica Lising GayoAinda não há avaliações
- Magna Carta of Public Health Workers ActDocumento12 páginasMagna Carta of Public Health Workers ActKerima Danica Lising GayoAinda não há avaliações
- Pacu 09-08-13Documento3 páginasPacu 09-08-13Kerima Danica Lising GayoAinda não há avaliações
- Meropenem 220 MG q8h IVDocumento11 páginasMeropenem 220 MG q8h IVKerima Danica Lising GayoAinda não há avaliações
- Econ 11 HandoutsDocumento6 páginasEcon 11 HandoutsKerima Danica Lising GayoAinda não há avaliações
- 21 Day Muscle Part 2 The 21 AsdsadsadDocumento42 páginas21 Day Muscle Part 2 The 21 Asdsadsadbatista587Ainda não há avaliações
- CH 10 PPT LectureDocumento31 páginasCH 10 PPT Lecturexy manAinda não há avaliações
- IV antibiotics post-infusion phlebitis signsDocumento124 páginasIV antibiotics post-infusion phlebitis signsD and D Educators and Associates100% (2)
- Shapes Fitness CenterDocumento158 páginasShapes Fitness CentermaryumsarfrazAinda não há avaliações
- GD Sodium Silicate MSDS2012Documento5 páginasGD Sodium Silicate MSDS2012nit_xlriAinda não há avaliações
- Herbs Health & Happiness 10 Herbs For The Eyes - Herbs Health & HappinessDocumento3 páginasHerbs Health & Happiness 10 Herbs For The Eyes - Herbs Health & HappinessLinda PrideAinda não há avaliações
- CarbohydrateDocumento104 páginasCarbohydrateAdnan QureshiAinda não há avaliações
- Health Benefits of SquashDocumento9 páginasHealth Benefits of SquashBeth Bauzon100% (1)
- G10Mapeh Exam First QuaterDocumento8 páginasG10Mapeh Exam First QuaterJonas LamcisAinda não há avaliações
- Full Download Understanding Nutrition 13th Edition Whitney Solutions ManualDocumento35 páginasFull Download Understanding Nutrition 13th Edition Whitney Solutions Manualyettihonomi2100% (30)
- Oils, Fats and Waxes: Smoke PointDocumento7 páginasOils, Fats and Waxes: Smoke PointDyanne Jane Cid DuldulaoAinda não há avaliações
- Group 4Documento72 páginasGroup 4larasAinda não há avaliações
- Bahasa Inggeris T2Documento5 páginasBahasa Inggeris T2NajwaAbdullahAinda não há avaliações
- Drug Interaction MonitoringDocumento5 páginasDrug Interaction MonitoringAnonymousAinda não há avaliações
- Alana Pascal - Kombucha - How-To and What It's All AboutDocumento125 páginasAlana Pascal - Kombucha - How-To and What It's All Aboutjeesup9100% (4)
- PiXL Knowledge Test QUESTIONS - AQA B1 CORE Science - Legacy (2016 and 2017)Documento6 páginasPiXL Knowledge Test QUESTIONS - AQA B1 CORE Science - Legacy (2016 and 2017)Mrs S BakerAinda não há avaliações
- Vata PacifyDocumento17 páginasVata PacifySiyaa SinghAinda não há avaliações
- Vitamin KDocumento14 páginasVitamin KSafdar RasoolAinda não há avaliações
- AdimeDocumento4 páginasAdimeapi-340838547Ainda não há avaliações
- Vitamin Ebook DR Andrew SaulDocumento25 páginasVitamin Ebook DR Andrew Saulsilviapoli2100% (11)
- Biochemistry QuestionsDocumento7 páginasBiochemistry QuestionsCatherine JennensAinda não há avaliações
- Certificate of Analysis: Attention:Nancy Jo SeatonDocumento6 páginasCertificate of Analysis: Attention:Nancy Jo SeatonPeterborough ExaminerAinda não há avaliações
- Sesame in PakistanDocumento40 páginasSesame in PakistanHumayoon HanifAinda não há avaliações
- Gestational Diabetes Brochure ENGDocumento2 páginasGestational Diabetes Brochure ENGP Zamora100% (2)
- Barecuatro - BSN1 11L - Pre Finals ActivityDocumento12 páginasBarecuatro - BSN1 11L - Pre Finals ActivityAngelica Claire BarecuatroAinda não há avaliações
- 12th MCQDocumento88 páginas12th MCQRishik Kr. Sahu 'B'Ainda não há avaliações
- Health Benefits of DrumstickDocumento3 páginasHealth Benefits of Drumstickanasnasir9Ainda não há avaliações
- Food Worksheet SolutionsDocumento3 páginasFood Worksheet SolutionsPNG networksAinda não há avaliações
- hsns270 Assignment 1 Bhima Devi Poudel Adhikari CKD 220179000Documento12 páginashsns270 Assignment 1 Bhima Devi Poudel Adhikari CKD 220179000api-525310113Ainda não há avaliações
- 4 Sneaky Tricks To Lower Your Blood Sugar G1981Documento26 páginas4 Sneaky Tricks To Lower Your Blood Sugar G1981pipAinda não há avaliações