Escolar Documentos
Profissional Documentos
Cultura Documentos
2012 Article 164
Enviado por
ursula_ursula0 notas0% acharam este documento útil (0 voto)
16 visualizações4 páginasstd article
Título original
13224_2012_Article_164
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentostd article
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
16 visualizações4 páginas2012 Article 164
Enviado por
ursula_ursulastd article
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 4
ORI GI NAL ARTI CLE
Prevalence of Sexually Transmitted Infections (HIV, Hepatitis B,
Herpes Simplex Type 2 and Syphilis) Among Asymptomatic
Pregnant Women
Jindal Neerja
Arora Usha
Singh Sukhwinder
Devi Bimla
Received: 20 January 2009 / Accepted: 2 April 2012 / Published online: 1 June 2012
Federation of Obstetric & Gynecological Societies of India 2012
Abstract
Objectives To determine the current prevalence of four
major sexually transmitted infections (STIs: HIV, Hepatitis
B, Herpes simplex virus 2, and Syphilis) in asymptomatic
pregnant women.
Methods This is a prospective study of 500 consecutive,
apparently healthy asymptomatic pregnant women who
were attending the antenatal clinic. The information
regarding their socio-demographic and behavioral charac-
teristics and obstetric performance was recorded. The
blood samples was collected after obtaining their informed
written consent from those who were tested for the HIV
antibodies (NACO guidelines), HBsAg (ELISA test),
HSV2-IgM (ELISA test), and Syphilis (VDRL and TPHA
tests).
Results The overall prevalence of one or the other four
STIs studied was 4.8 % with the highest prevalence of
HBV (2.4 %), followed by HSV-2 (2 %), and HIV (0.4 %).
No woman tested positive for syphilis and multiple infec-
tions. All the infections were more common in illiterate,
multigravida, monogamous women of low socio-economic
status. High-risk sexual behavior of the husbands, history
of STIs in husbands, and blood transfusions were the other
factors associated with the prevalence of these infections.
Conclusions The relatively high prevalence of HBV and
HSV-2 infections in asymptomatic pregnant women sug-
gests that there is need of screening for HBV and HSV-2
infections along with the pre-existing screening for HIV
and Syphilis and universal immunization of HBV high-risk
infants.
Keywords Asymptomatic pregnant women HSV-2
HBV HIV Syphilis
Introduction
The prevalence of sexually transmitted infections (STIs) in
India is estimated to be 6 %, and about 40 % of women
have STIs at any given point of time. Among pregnant
women, STIs are associated with a number of adverse
pregnancy outcomes including spontaneous abortions,
stillbirth, prematurity, low birth weight, postpartum endo-
metritis, and various sequelae in surviving neonates [1].
The management of a signicant proportion of these
infections is difcult and complicated because they run a
long, latent, and insidious course, remain inapparent or
asymptomatic, and cannot be initially detected clinically.
There are no screening programmes for the detection of
STIs in asymptomatic pregnant women even in our tertiary
level hospitals [2]. As there is paucity of data on the
prevalence of these infections in these women which may
differ in geographically disperate regions and is important
for designing STI/HIV control programs, the present study
Jindal N. (&), Professor Arora U., Professor & Head
Singh S., Jr. Resident Devi B., Associate Professor
Government Medical College Amritsar (Pb),
113-Race Course Road, Amritsar 143001, Punjab, India
e-mail: neerjarajender@hotmail.com
The Journal of Obstetrics and Gynecology of India (MarchApril 2012) 62(2):158161
DOI 10.1007/s13224-012-0164-6
1 3
was undertaken to determine the current prevalence of
some of the important STIs (HIV, Hepatitis B, herpes
simplex virus type 2 (HSV-2), and Syphilis) in asymp-
tomatic pregnant women of Amritsar (Punjab).
Materials and Methods
A total of 500 consecutive apparently healthy, asymp-
tomatic pregnant women, who had history of normal
obstetric performance and were attending the antenatal
clinic of the Obstetrics and Gynecology Department from
October 2004 to February 2006, were screened for HIV,
Hepatitis B Virus (HBV), herpes simplex virus type 2, and
Syphilis infections. Information regarding demographic,
social, and behavioral characteristics, and obstetric per-
formance was recorded, and blood samples were collected
after obtaining their informed written consent. Screening
for HIV antibodies was performed as per NACO guide-
lines; HBV infection was diagnosed by detecting Hepatitis
B surface antigen (HbsAg) by ELISA (Hepalis; J. Mitra &
Co. Ltd); and seroreactivity was performred for HSV2-IgM
using ELISA test kit ( ENZYWELL-Herpes Simplex2
IgM; DIESSE. Italy). Serological diagnosis of syphilis was
done using VDRL and TPHA tests. The v
2
test was used
for statistical analysis.
Results
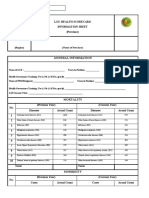
Table 1 shows that, of the 500 women included in the
study, 80.8 % were in the age group of 2130 years,
65.2 % had urban background, and 76 % had education up
to the 5th grade or more. Majority of them (59.2 %)
belonged to low socio-economic status and were house-
wives (61.2 %). Multigravida was more (58.2 %) than
primigravida (41.8 %). No woman gave history of pro-
miscuous sexual behavior or intravenous drug abuse by
herself. However, 7 % (35/500) reported the presence of
such behavior and STIs in their husbands 2 % (10/500).
On the whole, 24 of 500 (4.8 %) women were found to
be positive for one or other of these four infections with no
case of multiple infections. The highest prevalence was
that of Hepatitis B (2.4 %) followed by HSV-2 (2 %) and
HIV (0.4 %). No woman tested positive for Syphilis.
Study of the various factors in relation to HBV infection
showed that the infection was signicantly more prevalent
in women having low literacy rate (p = 0.0015) than those
having education up to the 5th grade or more (Table 1).
Other high-risk factors observed in HbsAg-positive women
were history of blood transfusion (6/12; 50 %) and high-
risk sexual behavior of the husband (8/12; 66.6 %). No one
was immunized against HBV infection. Presence of IgM
antibodies to HSV-2 in 10 of the 500 (2 %) women
Table 1 Prevalence in relation to various socio-demographic factors
S. No Socio-demographic
factors
No of
women 500
HIV ?ve
cases 2(0.4)
Hepatitis B ?ve
cases 12(2.4)
HSV-2 ?ve
cases 10(2)
Syphilis ?ve
cases Nil
1 Age (years)
\20 61 (122) 2 (3.3)
2130 404 (80.8) 2 (0.5) 10 (2.5) 9 (2.2)
[30 35 (7) 1 (2.9)
2 Geographic distribution
Urban 326 (65.2) 2 (0.6) 5 (1.5) 7 (2.14)
Rural 174 (34.8) 7 (4.02) 3 (1.7)
3 Education
\5th Grade 120 (24) 2 (1.7) 8 (6.7) 5 (4.2)
C5th Grade 380 (76) 4 (1.05)* 5 (1.3)
4 Socio-economic status
Low 296 (592) 2 (0.67) 8 (2.7) 5 (1.7)
Middle 165 (33.4) 3 (1.8) 4 (2.4)
Upper 37 (7.4) 1 (2.7) 1 (2.5)
5 Gravida
Multi 291 (58.2) 2 (07) 8 (2.7) 8 (2.7)
Primi 209 (418) 4 (1.9) 2 (0.9)
Figures in parenthesis represent percentage
* p = 0.0015 (Signicant)
1 3
The Journal of Obstetrics and Gynecology of India (MarchApril 2012) 62(2):158161 Prevalence of Sexually Transmitted Infections
159
demonstrated that these women had primary/rst episode
of HSV-2 infection during pregnancy and it was asymp-
tomatic. There was no statistically signicant association of
the IgM HSV-2 positivity to the various socio-demographic
factors. Both the HIV positive women of our study were in
the age group of 2130 years, urban, illiterate, had low
socio-economic status, and were monogamous and multi-
gravida. Husbands of both of them were laborers, and they
also tested positive for HIV. These women were neither
aware of their own HIV status nor that of their husbands.
Discussion
Most of the published data on STIs among pregnant
women is related to those having symptoms of STIs and/or
bad obstetrical history [2, 3]. In our series, 500 asymp-
tomatic pregnant women were studied, and overall preva-
lence of any one of the four infections (HIV, HBV, HSV-2,
and Syphilis) was 4.8 %. A multicentric study reported
prevalence of 7.4 % in any one of the ve infections (HIV,
HBV, Syphilis, Chlamydia, and Gonorrhea), and only half
of them had clinical signs and/or symptoms [2]. This
implies that syndromic approach which is used to manage
STIs in pregnancy in our country is notoriously poor in
identifying high proportions of infections in asymptomatic
pregnant women as observed by other workers too [2, 3].
In the present study, positivity for HBV (2.4 %) was the
highest. This is in agreement with the 2.6 % carrier rate of
HBsAg reported in a follow-up study of asymptomatic
mothers from South India [4]. In a recent study from Delhi,
4.25 % mothers were found to be carriers [5]. These
prevalence rates conform to Indias status as an interme-
diate endemicity area, and in an endemic population, ver-
tical transmission is responsible for majority of HBV
infections. The presence of HBsAg in the pregnant women
does not pose an additional risk for pregnancy, but the
infected infants became reservoir of infection, and as
adults, they are at risk of developing chronic hepatitis, liver
cirrhosis, and hepatocellular carcinoma [6]. Therefore, all
the infants born to HBsAg seropositive women need to be
given universal infant immunization.
Ten of the 500(2 %) women of our series tested positive
for the presence of IgM antibodies to HSV-2. Other authors
have reported asymptomatic infection in 0.58 % of
women depending upon the populations studied [7, 8]. In a
study of 779 women attending a STI clinic, 47 % had
serological evidence of HSV-2 infection, but only 22 %
presented with symptoms of genital herpes. It is critical to
recognize that the majority of mothers of infants with
neonatal HSV do not have a history of HSV [6]. Detection
of HSV-2 infections would facilitate counseling of the
pregnant women regarding therapy, risk of recurrences, and
appropriate measures to reduce HSV-2 infection to their
offsprings and contacts [8].
The HIV prevalence in antenatal women attending
public hospitals in different states of India varies from 0 to
2 %, and Punjab is an area of low level epidemic (preva-
lence rate \1 %) [9]. Our result of 0.4 % seropositivity is
in accordance with the same and almost similar to the
nding from Chandigarh where no woman was found to be
HIV positive [2]. Pregnancy does not have any adverse
impact on the course of HIV infection, and cases of AIDS
represent only a fraction of population infected with HIV.
However, asymptomatic HIV-infected women transmit the
infection to their offsprings, and mother-to-child trans-
mission is by far the most signicant route of transmission
of HIV infection in children below the age of 15 years.
With more and more pregnant women testing positive for
HIV and perinatal transmission rate of 1540 %, pediatric
AIDS is becoming a major public health problem in India
[10]. Timely detection of HIV infection and use of anti-
retroviral therapy along with the knowledge to avoid con-
tracting the infection could help in curtailing this problem.
In the present series, no woman tested positive for
Syphilis. In the study of Datey et al., the overall prevalence
of Syphilis from ve different centers of study was 1 %,
and the prevalence was the lowest (0.3 %) at Chandigarh
and Calcutta [2]. Although the seroprevalence of syphilis in
pregnancy is low, it is a recognized cause of fetal loss.
Proper treatment and antenatal care of the VDRL-reactive
women would help in achieving successful pregnancy
outcome.
Among the various STIs, the prevalence pattern of
Syphilis and herpes genitalis is pivotal. This is because
HSV-2 infection has an important role in the spread of HIV
infection, and in a pregnant, HIV-infected women, it may
be a risk factor for perinatal HIV transmission [11]. A
number of studies in the recent past have demonstrated a
strong association between HSV-2 seropositivity and
positive HIV and syphilis serology [3, 8]. However, no
such association was observed in the present study. This
could be because of a very different set of population
(asymptomatic pregnant women) studied, which showed
relatively low prevalence of these infections and the sam-
ple size studied was also small.
Similar to the studies conducted in other parts of our
country, low literacy status, high-risk sexual behavior,
history of STIs in husbands, and blood transfusions were
found to be associated with increased prevalence of STIs in
our study [2, 5, 9]. In the present study, STIs including
HIV/AIDS were more common among married monoga-
mous women. This is similar to another report from North
India (Punjab) [12]. Women in monogamous relationship
are placed at the risk for infection when their husbands
engage in high-risk sexual activity. The vulnerability of
1 3
Jindal et al. The Journal of Obstetrics and Gynecology of India (MarchApril 2012) 62(2):158161
160
women is also due to inadequate knowledge about STIs,
insufcient access to prevention services, inability to
negotiate safer sex, and lack of female-controlled preven-
tion method.
The present study thus concludes that along with ante-
natal screening of syphilis and HIV, there is an urgent need
for developing suitable screening strategies for HBV and
HSV-2 infections for asymptomatic pregnant women and
universal immunization of HBV high-risk infants. In
addition, greater emphasis should be laid on targeted
interventions of prevention services through information,
education, and promotion of womens right. This would go
a long way in reducing the spread of STIs in pregnant
women and its associated perinatal mortality and morbid.
References
1. National Guidelines on Prevention, Management and control of
Reproductive tract-infections including Sexually Transmitted
Infections: National AIDS Control Organisation, MOHFW, Govt.
of India. 2006.
2. Datey S, Bedi N, Gaur IN, et al. Sexually transmitted infections
(STIS) among antenatal women at ve tertiary level hospitals in
India. (An ICMR Task Force Study). J Obstet Gynecol India.
2003;53:538.
3. Mullick S, Watson Jones D, Beksinka M, et al. Sexually trans-
mitted infections in pregnancy: prevalence, impact on pregnancy
outcomes; and approach to treatment in developing countries. Sex
Transm Infect. 2005;81:294302.
4. Shanmugam J, Nair SR. A three and half year follow up study of
HBSAg carrier state in asymptomatic mothers. Indian J Pathol
Microbiol. 1982;25:2738.
5. Chakravarti A, Rawal D, Jain M. Study on the perinatal trans-
mission of the hepatitis B virus Indian. J Med Microbiol.
2005;23:12830.
6. Cloherty JP, Eichenwald EC, Stark AR. Manual of Neonatal
Care, 5th Ed. Philadelphia: Lippincott William S & Wilkins;
2004. p. 2757.
7. Vontver LA, Hickok DE, Brown Z, et al. Recurrent genital herpes
simplex virus infection in pregnancy: infant outcome and fre-
quency of asymptomatic recurrences. Am J Obstel Gynaecol.
1982;143:7584.
8. Peter BP, Rastogi VL, Monica, et al. Co-infection of HSV with
other sexually transmitted diseases of HSV with other sexually
transmitted diseases. Indian J Med Microbiol. 2005;23:1434.
9. HIV/AIDS Epidemiological Surveillance & Estimation report for
the year 2005. National AIDS control Organisation Ministry of
Health & Family Welfare Government of India. 2006.
10. Guideline for prevention of mother to child transmission
(PMTCT): Mumbai District AIDS Control Society, UNICEF.
2002.
11. Chen KT, Segu M, Kuhu L, et al. Genital herpes simplex virus
infection and perinatal transmission of human immunodeciency
virus. Obstet Gynecol. 2005;106:13418.
12. Kumar M. AIDS: Greater threat to women The Tribune 2007.
1 3
The Journal of Obstetrics and Gynecology of India (MarchApril 2012) 62(2):158161 Prevalence of Sexually Transmitted Infections
161
Você também pode gostar
- Prevalence and Risk Factors of Hepatitis B Virus Among Pregnant Women in Jazan Region - Kingdom of Saudi ArabiaDocumento6 páginasPrevalence and Risk Factors of Hepatitis B Virus Among Pregnant Women in Jazan Region - Kingdom of Saudi ArabiaAlexander DeckerAinda não há avaliações
- 10965-Article Text-70987-1-10-20081022 PDFDocumento6 páginas10965-Article Text-70987-1-10-20081022 PDFHumphrey MisiriAinda não há avaliações
- Pregnancy and HIV Disease Progression: A Systematic Review and Meta-AnalysisDocumento24 páginasPregnancy and HIV Disease Progression: A Systematic Review and Meta-AnalysisZulfahmi MusllimAinda não há avaliações
- Clin Infect Dis. 2007 Gupta 241 9Documento9 páginasClin Infect Dis. 2007 Gupta 241 9Handy SaputraAinda não há avaliações
- Aids Introduction Related To ObstetricsDocumento28 páginasAids Introduction Related To ObstetricsRoselineTigga100% (1)
- Socio-Demographic Characteristics Associated With HIV and Syphilis Seroreactivity Among Pregnant Women in Blantyre, Malawi, 2000-2004Documento2 páginasSocio-Demographic Characteristics Associated With HIV and Syphilis Seroreactivity Among Pregnant Women in Blantyre, Malawi, 2000-2004Humphrey MisiriAinda não há avaliações
- STI's HIV and AIDSDocumento509 páginasSTI's HIV and AIDSMaya ArianiAinda não há avaliações
- The Burden of HIV Infection Among Women Attending Antenatal Clinic in A Semi-Urban Nigerian TownDocumento6 páginasThe Burden of HIV Infection Among Women Attending Antenatal Clinic in A Semi-Urban Nigerian TownDavid MorgAinda não há avaliações
- Unrecognized Sexually Transmitted Infections in Rural South African Women: A Hidden EpidemicDocumento7 páginasUnrecognized Sexually Transmitted Infections in Rural South African Women: A Hidden EpidemicsehlabakmnsnrAinda não há avaliações
- 45 90 1 SM PDFDocumento16 páginas45 90 1 SM PDFMirza RisqaAinda não há avaliações
- Incident HIV During Pregnancy and Postpartum and Risk of Mother-to-Child HIV Transmission: A Systematic Review and Meta-AnalysisDocumento16 páginasIncident HIV During Pregnancy and Postpartum and Risk of Mother-to-Child HIV Transmission: A Systematic Review and Meta-Analysisursula_ursulaAinda não há avaliações
- Five-Year Trends in Epidemiology and Prevention of Mother-To-Child HIV Transmission, St. Petersburg, Russia: Results From Perinatal HIV SurveillanceDocumento11 páginasFive-Year Trends in Epidemiology and Prevention of Mother-To-Child HIV Transmission, St. Petersburg, Russia: Results From Perinatal HIV SurveillanceManuela Martín-Bejarano GarcíaAinda não há avaliações
- Medicine - IJGMP - HUMAN IMMUNO DEFFICIENCY - Adetunji Oladeni Adeniji - NigeriaDocumento10 páginasMedicine - IJGMP - HUMAN IMMUNO DEFFICIENCY - Adetunji Oladeni Adeniji - Nigeriaiaset123Ainda não há avaliações
- Hiv/Aids Prevalence in Surabaya, Indonesia: Nasronudin, Yayuk Susilawati, AtikaDocumento5 páginasHiv/Aids Prevalence in Surabaya, Indonesia: Nasronudin, Yayuk Susilawati, AtikaHervi LaksariAinda não há avaliações
- Impact of Maternal Hiv Infection On Pregnancy Outcomes in Southwestern China A Hospital Registry Based StudyDocumento9 páginasImpact of Maternal Hiv Infection On Pregnancy Outcomes in Southwestern China A Hospital Registry Based StudyKezia SoplanitAinda não há avaliações
- Medicine - Ijmps - Hiv Sero Discordance - Kola Musliudin OwonikokoDocumento10 páginasMedicine - Ijmps - Hiv Sero Discordance - Kola Musliudin OwonikokoTJPRC PublicationsAinda não há avaliações
- Journal DermatologyDocumento8 páginasJournal DermatologyImelva GirsangAinda não há avaliações
- Jurnal 6 Kelompok 12Documento9 páginasJurnal 6 Kelompok 12Rista HernidawatiAinda não há avaliações
- 35-1404729796 JurnalDocumento3 páginas35-1404729796 JurnalNancy ZhangAinda não há avaliações
- 299 ArabicDocumento9 páginas299 ArabicTinkhaniMbichilaAinda não há avaliações
- 1742 4755 6 4 PDFDocumento8 páginas1742 4755 6 4 PDFAbdirahmanAinda não há avaliações
- 2279 17564 3 PBDocumento10 páginas2279 17564 3 PBGabriella EugeniaAinda não há avaliações
- WS Nihms448407Documento11 páginasWS Nihms448407ayubahriAinda não há avaliações
- Simpore2006-Toxoplasma Gondii, HCV, and HBV SeroprevalenceDocumento4 páginasSimpore2006-Toxoplasma Gondii, HCV, and HBV Seroprevalenceizvery.badAinda não há avaliações
- Efecto de Hiv1 en Mujeres Embarazadas de RwandaDocumento8 páginasEfecto de Hiv1 en Mujeres Embarazadas de RwandaIsmaelJoséGonzálezGuzmánAinda não há avaliações
- 2 6 1 PBDocumento7 páginas2 6 1 PBkumala dewiAinda não há avaliações
- Jurnal Ibu Hamil Dan HIVDocumento6 páginasJurnal Ibu Hamil Dan HIVJacobus Lee-sHa67% (3)
- Sande's HIV - AIDS Medicine (PDFDrive)Documento562 páginasSande's HIV - AIDS Medicine (PDFDrive)angel muñozAinda não há avaliações
- HIV-AIDS-Learning Notes Lesson 1Documento49 páginasHIV-AIDS-Learning Notes Lesson 1Ssentongo NazilAinda não há avaliações
- BMC Infectious DiseasesDocumento10 páginasBMC Infectious DiseasesDomenico BevilacquaAinda não há avaliações
- Case Study GonorrheaDocumento37 páginasCase Study GonorrheaAnge MinguitoAinda não há avaliações
- (Kakalang, Masloman, & Manoppo, 2016) PDFDocumento6 páginas(Kakalang, Masloman, & Manoppo, 2016) PDFnedya asnuriantiAinda não há avaliações
- 192 Prevalence of Hepatitis B Surface AntigeDocumento2 páginas192 Prevalence of Hepatitis B Surface AntigeLazwardy_Perda_718Ainda não há avaliações
- Sexual Habits and Clinico-Etiological Profile of Sexually Transmitted Diseases in NepalDocumento7 páginasSexual Habits and Clinico-Etiological Profile of Sexually Transmitted Diseases in NepalMuhammad TariqAinda não há avaliações
- HIV Associated High-Risk HPV Infection Among Nigerian Women: Researcharticle Open AccessDocumento6 páginasHIV Associated High-Risk HPV Infection Among Nigerian Women: Researcharticle Open AccessMay MaghdalenaAinda não há avaliações
- Jurnal LeukoreaDocumento6 páginasJurnal LeukoreaLystiani Puspita DewiAinda não há avaliações
- Jalalpur Jattan Case StudyDocumento8 páginasJalalpur Jattan Case Studyduracell19Ainda não há avaliações
- HIV Transmission and Prevention: Mother-to-Child (Perinatal)Documento5 páginasHIV Transmission and Prevention: Mother-to-Child (Perinatal)Wahyu Wijasena AdhiAinda não há avaliações
- Case Series of Infertility Amongst Young Women With Peri - 2019 - Journal of VirDocumento3 páginasCase Series of Infertility Amongst Young Women With Peri - 2019 - Journal of VirSansa LauraAinda não há avaliações
- Gestante y VihDocumento9 páginasGestante y VihJacobo IbañezAinda não há avaliações
- Jurnal Tentang WPSDocumento8 páginasJurnal Tentang WPSAdzamAinda não há avaliações
- Hiv and Aids AssDocumento9 páginasHiv and Aids AssquarozAinda não há avaliações
- Chlamydia TrachomatisDocumento46 páginasChlamydia TrachomatisJulius Togo TeodorusAinda não há avaliações
- Paper On HIV Widows FinalDocumento5 páginasPaper On HIV Widows FinalAntriya DevarajAinda não há avaliações
- Knowledge On Sexually Transmitted Infections (STI) Among Women in Bangladesh: A Short ReviewDocumento13 páginasKnowledge On Sexually Transmitted Infections (STI) Among Women in Bangladesh: A Short ReviewAhmad Kabir MaikanoAinda não há avaliações
- 2017ponee175166 PDFDocumento16 páginas2017ponee175166 PDFAbdirahmanAinda não há avaliações
- High Rates of Late HIV Diagnosis Among People Who Inject Drugs Compared To Men Who Have Sex With Men and Heterosexual Men and Women in AustraliaDocumento7 páginasHigh Rates of Late HIV Diagnosis Among People Who Inject Drugs Compared To Men Who Have Sex With Men and Heterosexual Men and Women in AustraliaDANIAinda não há avaliações
- Human Papillomavirus Infection in Shenyang City, People's Republic of China: A Population-Based StudyDocumento5 páginasHuman Papillomavirus Infection in Shenyang City, People's Republic of China: A Population-Based StudyyoggihermawanAinda não há avaliações
- VIH/SIDA - RevelacaoDocumento7 páginasVIH/SIDA - Revelacaovanessa waltersAinda não há avaliações
- Maternal Mortality: A Retrospective StudyDocumento4 páginasMaternal Mortality: A Retrospective StudyIOSRjournalAinda não há avaliações
- CandidaDocumento9 páginasCandidahilmysyarifahAinda não há avaliações
- Journal Reading Bacterial VaginosisDocumento21 páginasJournal Reading Bacterial Vaginosisnurul hidayatiAinda não há avaliações
- IGNOU Block 3 Unit 4 Communicable Diseases 3 - Zoonotic DiseasesDocumento17 páginasIGNOU Block 3 Unit 4 Communicable Diseases 3 - Zoonotic Diseaseserice.researchAinda não há avaliações
- 17akinbolaji EtalDocumento5 páginas17akinbolaji EtaleditorijmrhsAinda não há avaliações
- Russi Et Al - 2003Documento5 páginasRussi Et Al - 2003Javier ReyAinda não há avaliações
- Prevalence and Incidence of Genital Warts and Cervical Human Papillomavirus Infections in Nigerian WomenDocumento10 páginasPrevalence and Incidence of Genital Warts and Cervical Human Papillomavirus Infections in Nigerian WomenRiszki_03Ainda não há avaliações
- The Complete Guide to HPV: Symptoms, Risks, Diagnosis & TreatmentsNo EverandThe Complete Guide to HPV: Symptoms, Risks, Diagnosis & TreatmentsAinda não há avaliações
- The Complete Guide to Genital Herpes: Symptoms, Risks, Diagnosis & TreatmentsNo EverandThe Complete Guide to Genital Herpes: Symptoms, Risks, Diagnosis & TreatmentsAinda não há avaliações
- DM Guidelines CCPDocumento87 páginasDM Guidelines CCPfuad20Ainda não há avaliações
- HHS Public Access: Early Chronic Kidney Disease: Diagnosis, Management and Models of CareDocumento27 páginasHHS Public Access: Early Chronic Kidney Disease: Diagnosis, Management and Models of Careursula_ursulaAinda não há avaliações
- NIH Public Access: Hypertensive Chronic Kidney Disease in African Americans: Strategies For Improving CareDocumento14 páginasNIH Public Access: Hypertensive Chronic Kidney Disease in African Americans: Strategies For Improving Careursula_ursulaAinda não há avaliações
- Nephrology: World Journal ofDocumento18 páginasNephrology: World Journal ofursula_ursulaAinda não há avaliações
- Internal Medicine Clinical Treatment Guidelines 9-10-2012 1Documento264 páginasInternal Medicine Clinical Treatment Guidelines 9-10-2012 1ursula_ursulaAinda não há avaliações
- 1635 FullDocumento77 páginas1635 Fullursula_ursula100% (1)
- Helicobacter PyloriDocumento3 páginasHelicobacter Pyloriursula_ursulaAinda não há avaliações
- Incident HIV During Pregnancy and Postpartum and Risk of Mother-to-Child HIV Transmission: A Systematic Review and Meta-AnalysisDocumento16 páginasIncident HIV During Pregnancy and Postpartum and Risk of Mother-to-Child HIV Transmission: A Systematic Review and Meta-Analysisursula_ursulaAinda não há avaliações
- Preventing Sexually Transmitted Infections: Back To Basics: Review Series IntroductionDocumento4 páginasPreventing Sexually Transmitted Infections: Back To Basics: Review Series Introductionursula_ursulaAinda não há avaliações
- Evidence of Human Papillomavirus in The Placenta: BriefreportDocumento3 páginasEvidence of Human Papillomavirus in The Placenta: Briefreportursula_ursulaAinda não há avaliações
- Goetz CG, Et Al - The Unified Parkinson's Disease Rating Scale (UPDRS) Status and RecommendationsDocumento13 páginasGoetz CG, Et Al - The Unified Parkinson's Disease Rating Scale (UPDRS) Status and Recommendationsursula_ursulaAinda não há avaliações
- Interventions To Prevent Sexually Transmitted Infections, Including HIV InfectionDocumento15 páginasInterventions To Prevent Sexually Transmitted Infections, Including HIV Infectionursula_ursulaAinda não há avaliações
- Zigmond MJ, Burke RE - Pathophysiology of Parkinson's DiseaseDocumento14 páginasZigmond MJ, Burke RE - Pathophysiology of Parkinson's Diseaseursula_ursula100% (1)
- Food Biopreservation (2014)Documento121 páginasFood Biopreservation (2014)reader1453100% (1)
- Medical Microbiology SyllabusDocumento7 páginasMedical Microbiology Syllabusapi-237835375Ainda não há avaliações
- ScienceDocumento20 páginasScienceAntriksh kingAinda não há avaliações
- Respiratory Tract Infection Act MP PDFDocumento3 páginasRespiratory Tract Infection Act MP PDFJessa mae CabredoAinda não há avaliações
- Secondary Bacterial Infections in CovidDocumento4 páginasSecondary Bacterial Infections in Covidnanang hidayatullohAinda não há avaliações
- Antibiotics BrochureDocumento2 páginasAntibiotics Brochureidno1008Ainda não há avaliações
- Dental PLAQUE: by Dr. Nitika Jain Post Graduate StudentDocumento70 páginasDental PLAQUE: by Dr. Nitika Jain Post Graduate StudentJee ArceoAinda não há avaliações
- CD Respi 30 ADocumento3 páginasCD Respi 30 ANae OrdanozoAinda não há avaliações
- 09-07-2020 HMB English PDFDocumento90 páginas09-07-2020 HMB English PDFdhaneesh22Ainda não há avaliações
- Malassezia Furfur An-An Ap-Ap Naturally Found On The SkinDocumento48 páginasMalassezia Furfur An-An Ap-Ap Naturally Found On The SkinNikki ValerioAinda não há avaliações
- Fish Diseases and Disorders Vol 1 - Protozoan and Metazoan InfectionsDocumento801 páginasFish Diseases and Disorders Vol 1 - Protozoan and Metazoan Infectionsclaudiousdecastro100% (1)
- CAFL - The Consolidated Annotated Frequency ListDocumento53 páginasCAFL - The Consolidated Annotated Frequency Listpressotti100% (1)
- Lymphatic Filariasis / Elephantiasis: Wuchereria Bancrofti & Brugia MalayiDocumento21 páginasLymphatic Filariasis / Elephantiasis: Wuchereria Bancrofti & Brugia Malayisujit555556677Ainda não há avaliações
- Taenia SagitaDocumento3 páginasTaenia SagitaNur LiyanaAinda não há avaliações
- Infectiuos Disease PDFDocumento248 páginasInfectiuos Disease PDFntnquynhpro0% (1)
- National AIDS Control Organization (NACO) : Care, Support & Treatment ServicesDocumento3 páginasNational AIDS Control Organization (NACO) : Care, Support & Treatment ServicesRewan ShindeAinda não há avaliações
- I. Education: Curriculum Vitae, Bayeh AberaDocumento2 páginasI. Education: Curriculum Vitae, Bayeh AberaHaile KassaAinda não há avaliações
- Protocolo BovigamDocumento2 páginasProtocolo BovigamMauro GonzalezAinda não há avaliações
- Kepositifan Induksi Sputum NaCl 3 Dan Teknik BroncDocumento7 páginasKepositifan Induksi Sputum NaCl 3 Dan Teknik Broncvovinda rujianaAinda não há avaliações
- Micro Lab Mans LsuDocumento38 páginasMicro Lab Mans LsuCarol Ann Baliad100% (1)
- Evaluation of Microbiological Hazards in BarbershopsDocumento3 páginasEvaluation of Microbiological Hazards in BarbershopshifzilAinda não há avaliações
- ANNEX B - LGU Information SheetDocumento2 páginasANNEX B - LGU Information SheetToni Quitalig GamezAinda não há avaliações
- Using Antimicrobial Agents To Control Mirobial Growth in VivoDocumento39 páginasUsing Antimicrobial Agents To Control Mirobial Growth in VivoHannah BuquironAinda não há avaliações
- Antibacterial Activity of Santol (Erscel)Documento4 páginasAntibacterial Activity of Santol (Erscel)Irsai ZiseeAinda não há avaliações
- Immunization: DR Shahbaz Ahmad Professor Community Medicine Independent Medical College FaisalabadDocumento67 páginasImmunization: DR Shahbaz Ahmad Professor Community Medicine Independent Medical College FaisalabadPriya bhattiAinda não há avaliações
- Sterilization in Microbiology WorksheetDocumento4 páginasSterilization in Microbiology WorksheetKrisha Mae VillanuevaAinda não há avaliações
- Microbiology Part 3Documento74 páginasMicrobiology Part 3Authentic IdiotAinda não há avaliações
- FYP Proposal DraftDocumento17 páginasFYP Proposal DraftKristen TeeAinda não há avaliações
- Tle9 Nailcare Q1 M14Documento8 páginasTle9 Nailcare Q1 M14Rheanna AbanillaAinda não há avaliações
- Melkamu MSC 1Documento60 páginasMelkamu MSC 1melkamu meleseAinda não há avaliações