Escolar Documentos
Profissional Documentos
Cultura Documentos
Ce Dent
Enviado por
vacharaDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Ce Dent
Enviado por
vacharaDireitos autorais:
Formatos disponíveis
Earn
2 CE credits
This course was
written for dentists,
dental hygienists,
and assistants.
Oral Health Care
During Chemotherapy
A Peer-Reviewed Publication
Written by Laurel Swartzentruber and Dr. Elena Bablenis Haveles, Bs Pharmacy, PharmD
Abstract
Oral side efects are commonplace with cancer chemo and
adjunctive therapies. Intravenous bisphosphonate therapy
can lead to osteonecrosis, especially after a tooth extraction
or oral surgery. Scheduled cleanings should be performed
every six months or quarterly, as well as compliance with
meticulous home oral hygiene, depending on risk factors
and the patients overall health. Chemotherapy can cause
a host of oral side efects including hypersensitivity due to
discomfort and pain, ulcerated gingival tissues, impaired
taste buds, erosion of tooth enamel due to vomiting, and
mucositis. The primary method of treating mucositis is
palliative therapy. Therapy includes home oral hygiene, pain
control, oral mouth rinses, and palliation of dry mouth. It
is important for dental hygienists to be aware of these side
efects and how to counsel their patients appropriately.
Educational Objectives
1. List the signs and symptoms of osteonecrosis associated
with bisphosphonate therapy.
2. Describe the oral health care that patients receiving
bisphosphonates should perform in order to minimize
the risk of developing osteonecrosis.
3. Describe the potential consequences of tooth extraction
in a patient receiving bisphosphonate therapy.
4. List and describe the treatments available for oral
mucositis.
5. List and describe the guidelines that the dental
hygienist should use when performing oral health care
on patients receiving chemotherapy.
6. List and describe the guidelines that the patient
receiving chemotherapy should follow to maintain
good oral health care.
Author Profile
Laurel Swartzentruber is a 2013 Bachelor of Science
Degree Candidate in the Gene W. Hirschfeld School of Dental
Hygiene, Old Dominion University, Norfolk, Virginia. This
paper was the result of Ms. Swartzentrubers research project
for the Universitys Honors Program. She plans on practicing
dental hygiene in the Virginia Beach area.
Dr. Elena Bablenis Haveles, Bs Pharmacy, PharmD is an
Adjunct Associate Professor of Pharmacology in the Gene
W. Hirschfeld School of Dental Hygiene, Old Dominion
University, Norfolk, Virginia. Dr. Haveles has taught at Old
Dominion University for almost 20 years. Please direct all
correspondence to Dr. Haveles. She can be contacted at
ehaveles@odu.edu
Author Disclosure
Laurel Swartzentruber and Dr. Elena Bblenis Haveles have
no potential conficts of interest to disclose.
Publication date: Apr. 2013
Expiration date: Mar. 2015
This educational activity was developed by PennWells Dental Group with no commercial support.
This course was written for dentists, dental hygienists and assistants, from novice to skilled.
Educational Methods: This course is a self-instructional journal and web activity.
Provider Disclosure: PennWell does not have a leadership position or a commercial interest in any products or
services discussed or shared in this educational activity nor with the commercial supporter. No manufacturer or
third party has had any input into the development of course content.
Requirements for Successful Completion: To obtain 2 CE credits for this educational activity you must pay the
required fee, review the material, complete the course evaluation and obtain a score of at least 70%.
CE Planner Disclosure: Heather Hodges, CE Coordinator does not have a leadership or commercial interest with
products or services discussed in this educational activity. Heather can be reached at hhodges@pennwell.com
Educational Disclaimer: Completing a single continuing education course does not provide enough information
to result in the participant being an expert in the field related to the course topic. It is a combination of many
educational courses and clinical experience that allows the participant to develop skills and expertise.
Scientific Integrity Statement: Information shared in this CE course is developed from clinical research and
represents the most current information available from evidence based dentistry.
Registration: The cost of this CE course is $49.00 for 2 CE credits.
Cancellation/Refund Policy: Any participant who is not 100% satisfied with this course can request a full
refund by contacting PennWell in writing.
Supplement to PennWell Publications
PennWelldesignatesthisactivityfor2ContinuingEducationalCreditsDentalBoardof
California: Provider 4527, course registration number CA#: 02-4527-13013
ThiscoursemeetstheDentalBoardofCalifornia srequirementsfor2unitsofcontinuingeducation.
ThePennWellCorporationisdesignatedasanApprovedPACEProgramProviderbythe
AcademyofGeneralDentistry.Theformalcontinuingdentaleducationprogramsofthis
programproviderareacceptedbytheAGDforFellowship,Mastershipandmembership
maintenancecredit.Approvaldoesnotimplyacceptancebyastateorprovincialboardof
dentistryorAGDendorsement. Thecurrenttermofapprovalextendsfrom(11/1/2011)to
(10/31/2015) Provider ID# 320452.
Go Green, Go Online to take your course
68 | rdhmag.com RDH | April 2013
Abstract
Oral side efects are commonplace with cancer chemo and
adjunctive therapies. Intravenous bisphosphonate therapy can
lead to osteonecrosis, especially after a tooth extraction or oral
surgery. Scheduled cleanings should be performed every six
months or quarterly, as well as compliance with meticulous home
oral hygiene, depending on risk factors and the patients health.
Chemotherapy can cause a host of oral side efects including
hypersensitivity due to discomfort and pain, ulcerated gingival
tissues, impaired taste buds, erosion of tooth enamel due to vom-
iting, and mucositis. The primary method of treating mucositis
is palliative therapy. Therapy includes home oral hygiene, pain
control, oral mouth rinses, and palliation of dry mouth. It is im-
portant for dental hygienists to be aware of these side efects and
how to counsel their patients appropriately.
Educational Objectives
1. List the signs and symptoms of osteonecrosis associated with
bisphosphonate therapy.
2. Describe the oral health care that patients receiving bisphos-
phonates should perform in order to minimize the risk of
developing osteonecrosis.
3. Describe the potential consequences of tooth extraction in a
patient receiving IV bisphosphonate therapy.
4. List and describe the treatments available for oral mucositis.
5. List and describe the guidelines that the dental hygienist
should use when performing oral health care on patients
receiving chemotherapy.
6. List and describe the guidelines that the patient receiving
chemotherapy should follow to maintain good oral health
care.
Introduction
Cancer is a devastating fact in society today. It is the second
leading cause of death in the United States, surpassed only by
heart disease.
1
According to the American Cancer Society, as
of January 1, 2008, it was estimated that there were 11,958,000
people in the United States alone who were living with some type
of invasive cancer.
2
Because so many people are being treated for
cancer, the dental hygienist should be knowledgeable of the many
drugs used to treat cancer and their side efects that afect oral
health care.
While there is no known cure for cancer, there are a number
of medications and treatments that kill cancer cells resulting
in a cancer-free state. Unfortunately, these treatments are not
without side efects (Table 1).
3
Oral health care providers are at
the forefront of providing the patient with the necessary tools for
treating and educating the patient about the oral implications of
these drugs. In many cases, it may be possible for the oral health
care provider to help lessen these side efects through the way
treatment is rendered.
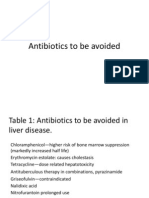
Table 1. Common Cancer Drugs and Their Side Effects
22
Common Cancer Drugs Gastrointestinal Side
Effects
Bone Marrow Side
Effects
Cyclophosphamide Nausea, vomiting,
abdominal pain, diar-
rhea, loss of appetite
Bone marrow sup-
pression
Doxorubicin Nausea, vomiting, ul-
ceration of the colon,
anorexia, abdominal
pain, diarrhea, dehy-
dration
Decreased func-
tion of bone mar-
row, low blood
counts
Anastrozole Nausea, vomiting,
diarrhea, abdominal
pain, constipation
Leukopenia
Exemestane Nausea, vomiting,
abdominal pain, dys-
pepsia (indigestion),
diarrhea, anorexia,
constipation, increase
in appetite
Lymphocytope-
nia (abnormally
low lymphocyte
levels)
Letrozole Nausea, vomit-
ing, constipation,
anorexia, abdominal
pain, dyspepsia,
diarrhea
None reported
Trastuzumab Nausea, vomiting,
diarrhea, anorexia
Neutropenia
Paclitaxel Nausea, vomiting,
diarrhea, mucositis
Bone marrow sup-
pression
Bisphosphonates
Bisphosphonates are frequently used in patients undergoing
chemotherapy to increase bone density and reduce the risk for
developing fractures.
4
Their beneft has been well established in
the treatment of hypercalcemia of malignancy and the prevention
of skeletal complications from bone metastasis.
5, 6, 7
Unfortunately, when given intravenously (IV), they can lead
to osteonecrosis of the jaw, which is an area of exposed bone in
either the maxilla or mandible that does not heal.
8
Clinical Presentation and Diagnosis of Osteonecrosis
Osteonecrosis can remain asymptomatic for weeks or even
months and is usually identifed by its unique clinical presenta-
tion of exposed bone in the oral cavity.
9
The lesions normally be-
come symptomatic when the site becomes secondarily infected or
there is trauma to the adjacent or healthy tissue from the irregular
surfaces of the exposed bone. Once symptomatic, the signs and
symptoms of osteonecrosis include localized pain, soft tissue
swelling and infammation, loosening of previously stable teeth,
drainage, and exposed bone. Normally, these symptoms occur
at the site of previous tooth extractions or other dental surgical
procedures. However, they can occur spontaneously.
It should be noted that some patients may present with atypi-
cal symptoms to include numbness, the feeling of a heavy
jaw, and various dysesthesias. Objective signs that may occur
RDH | April 2013 rdhmag.com | 69
before clinical oral symptoms include a sudden change in the
health of periodontal or mucosal tissue, failure of the oral mucosa
to heal, undiagnosed oral pain, loose teeth, and soft tissue infec-
tion.
9
If osteonecrosis does develop, it can lead to a host of other
oral side efects. The gingiva may have poor healing time and
may become infected and exudative. In addition, the jaw may
develop numbness, pain, or swelling.
8
Any patient who is receiv-
ing IV bisphosphonates should have their oral cavity examined
thoroughly for osteonecrosis. They should also practice very
meticulous oral hygiene, and should keep regularly scheduled
dental cleanings in order to help reduce the risk for developing
this condition. The frequency of scheduled cleanings is normally
every six months but, in this instance, may be scheduled every
three to four months depending on the number of risk factors
and the patients overall oral health. Also, removable dentures
should be examined for the potential to cause tissue injury and
be adjusted accordingly.
9
In instances where osteonecrosis does
develop, a removable appliance, such as a thin mouthguard, can
sometimes be used to protect the areas of exposed bone.
9
Patients who are receiving IV bisphosphonates have a high
risk of developing osteonecrosis after oral surgery or tooth extrac-
tion.
10
The dental hygienist needs to be very careful not to dam-
age any soft tissue. Also, the patient should check with an oral
surgeon and medical oncologist to see if it would be possible to
discontinue IV bisphosphonates prior to oral surgery. This would
give the patient the best chance of not developing osteonecrosis.
10
The patient could then resume the IV bisphosphonates once
the surgical site is completely healed. As another precautionary
measure, the oral surgeon could recommend that the patient start
a course of antibiotics before the surgery to fght of any pos-
sible infections.
10
These antibiotics should also continue after the
surgery for at least 10 days.
9
Research has shown that penicillin
generally stands the best chance at fghting of infections in these
patients.
9
The most important thing to remember is to always
check with the physician or oncologist before performing any
dental treatment or stopping any medications.
Oral Side Effects
Chemotherapeutic medications are the treatment of choice for
cancer therapy (Table 1). There are many diferent types of che-
motherapeutic drugs, so it is always wise to look up the specifc
one that the patient is taking in order to look out for any unique
side efects. Oral side efects occur often with chemotherapy, and
they include hypersensitivity due to discomfort and pain, ulcer-
ated gingival tissues, and impaired taste buds (Table 2).
3
Addi-
tionally, chemotherapy can cause vomiting, which leads to tooth
enamel erosion. The erosion can lead to tooth sensitivity. These
patients should be advised not to brush their teeth immedi-
ately after vomiting because brushing removes the outer layers of
enamel which has been softened by the acidic discharge. Instead,
the oral health care provider can suggest that these patients rinse
the mouth out very well with lukewarm water, with either baking
soda or salt, and then brush afterwards. Lastly, these medications
can cause xerostomia, which can lead to caries. Health care pro-
viders should educate patients on salivary substitutes and should
suggest that these patients begin a home fuoride regimen.
3
Table 2. Oral Side Effects of Common Cancer Chemotherapeutic
Agents
22
Common Cancer Drugs Oral Side Effects
Cyclophosphamide Ulceration of the oral mucosa
Doxorubicin Hyperpigmentation of the oral mucosa,
especially the tongue, mucositis
Anastrozole Dry mouth
Exemestane None reported
Letrozole Dry mouth, oral taste changes, metallic
taste
Trastuzumab Mouth sores
Paclitaxel Mouth sores
Mucositis
One of the most common oral side efects of chemotherapeutic
agents is mucositis, which is the ulceration of the mucosa lin-
ing the digestive tract, including the oral cavity.
11
Mucositis is a
common cause of morbidity in patients undergoing cancer che-
motherapy. According to the National Cancer Institute (NCI),
the incidence of NCI Grade 34 oral and gastrointestinal (GI)
mucositis is estimated between 5% and 15%.
12
Also, oral and
gastrointestinal mucositis can occur in up to 100% of patients
undergoing high-dose chemotherapy with hematopoietic stem
cell transplantation (HSCT).
13
From the patients perspective, it
is the HSCTs most debilitating side efect.
14
Oral mucositis is all encompassing and can range from mild
infammation and redness of the mucosa to severe ulceration.
Symptoms vary and include pain and discomfort to the complete
inability to tolerate food or drink. Mucositis may be so severe that
the patient may not be able to tolerate additional chemotherapy or
radiation therapy. In this case, treatment may be delayed, which
could limit the efectiveness of chemotherapy or radiation thera-
py. Also, patients with infamed mucosa and reduced immunity
due to chemotherapy and radiation therapy are at high risk for
opportunistic infections. Not only is the mucositis painful, but it
also increases the risk of developing infections and can sometimes
even lead to death. Furthermore, the patient will generally need
to prolong a hospital stay or delay additional chemotherapy in
order to manage this additional complication. Lastly, mucositis
can adversely afect the patients gums and teeth.
15
Many diferent treatment options are available to treat oral
mucositis. To date, the primary method of treating mucositis is
palliative therapy. This includes general oral care protocols, pain
control, oral mouth rinses, interventions to reduce the mucositis
associated with chemotherapy, and the palliation of dry mouth.
16
70 | rdhmag.com RDH | April 2013
The primary symptom of mucositis is pain, which can ad-
versely afect nutritional intake, oral health care, and quality of
life. Though they do not provide long-term relief, saline mouth
rinses, ice chips, and topical, alcohol-free mouth rinses with an
anesthetic provide short-term relief. More often than not, 2%
viscous lidocaine is used. Lidocaine is often mixed with equal
parts of diphenhydramine and a soothing agent such as Maalox
or Kaopectate
.
16
Other topical mucosal bioadherent agents
have been studied and include sucralfate chlorhexidine and
benzydamine topical rinse.
17
However, updated clinical prac-
tice guidelines for treating mucositis do not recommend their
use because their efectiveness has not been established.
18
The
current literature on nonopioid pain control includes the use of
a number of adjuvant treatments, including nonsteroidal anti-
infammatory drugs and gabapentin.
17
Cryotherapy or ice chips
appear to be efective in treating mucositis pain.
18
Current clinical
practice guidelines provide a Level I, Grade A recommendation
for patient-controlled analgesia (PCA) with morphine for those
patients undergoing HSCT.
17
Patients receiving chemotherapy are at high risk for devel-
oping mucositis so it is important that they maintain meticulous
oral hygiene. Unfortunately, there is not yet a defnite cure for
mucositis, so symptomatic treatment is the only option available
to cancer patients.
11
This symptomatic treatment includes main-
taining a very clean oral cavity through regular brushing, and also
avoiding any strong stimuli, such as spices, foods that are too hot,
and smoking.
15
If the mouth is uncomfortable, the patient can use
analgesics or topical anesthesia. Also, these patients should keep
their lips very well moisturized.
15
Hyposalivation or dry mouth associated with chemotherapy
can aggravate existing mucositis, which can put the patient at risk
for infection and make mastication difcult. Patients should be
advised to sip water as necessary to alleviate dry mouth. Artifcial
saliva substitutes can also be used. Patients can also rinse with a
solution of a teaspoonful of baking soda and/or a teaspoon-
ful of salt in 1 cup of warm water several times a day to alleviate
dry mouth symptoms. This will also clean and lubricate the oral
tissue and provide a protective barrier for the oral mucosa. Chew
tart, sugarless gum to enhance salivary fow and use cholinergic
agents (saliva substitutes) as necessary.
16
Guidelines for the Dental Hygienist
As health care providers, there are certain things that we need to
know about treating cancer patients. Chemotherapy treatments
are incredibly exhausting for the patient, so the best time to ad-
minister dental hygiene care is right before the next treatment.
19
When care is administered right before the next chemotherapy
appointment, patients wont be too weak to handle the dental
treatment and white blood cells should be at their highest lev-
els. Before any dental care is rendered, both the patient and the
hygienist should consult the oncologist in order to fnd out the
blood counts for the patient.
3
Platelet counts need to be greater
than 75,000 mm so that the blood can clot properly, and the
neutrophil count should be greater than 1,000 mm. Treatment
should be given whenever the patient has the highest possible
level of formed blood elements.
3
When the white blood cell count
is too low, there is an increased risk for infection, and so it is very
important to make sure that the blood counts are as high as pos-
sible.
20
During the actual appointment, the dental hygienist can have
the patient rinse with chlorhexidine mouth rinse to help avoid
any infections.
21
When performing the intraoral exam, the dental
hygienist should check for any lesions that could be cultured
in order to test for infection. Since chemotherapy inhibits the
salivary fow, some patients will probably have more bioflm and
caries than usual.
21
The dental professional should educate the
patient on how to avoid caries and practice proper oral hygiene.
Subsequent dental appointments for patients who experience
Brushing Mouth Rinses Flossing Other
Use an ultra soft toothbrush,
and rinse it with warm wa-
ter before brushing to avoid
damaging any tissues.
Rinsing with a solution of bak-
ing soda and saline will help
tender tissues to heal.
Floss at least once daily! Do not wear ill-fitting dentures. These
can increase the risk of a disease process
called osteonecrosis of the jaw.
Replace your toothbrush
either every 3 months OR
after any infection.
NEVER use a mouthwash that
contains alcohol! It will burn
the tissues.
If the gums are bleeding heavily,
do not floss those areas. Wait for
the tissues to heal.
Be aware of the side effects of any medi-
cations you are taking! Knowing what to
expect can help you to maintain healthy
teeth and gums.
Use mild toothpaste. Avoid
using strong flavors or
whitening agents.
Many chemotherapeutic agents
cause dry mouth, which may
lead to cavities. Topical fluoride
treatments can help to prevent
this.
Please consult your dental professionals
with any specific questions and concerns!
Use a chlorhexidine mouth
rinse to help prevent
infections. Ask your dental
professional for more infor-
mation.
Table 3. Oral Care Guidelines for Patients
15,21
RDH | April 2013 rdhmag.com | 71
more bioflm than normal should be scheduled for less than
six months. Typically, scheduling an appointment every four
months will sufce.
Oral Care Guidelines for the Patient
There are certain oral health care guidelines that dental hygien-
ists need to introduce to cancer patients (Table 3). Most impor-
tantly, the hygienist should emphasize that the patient needs to
maintain very good oral hygiene. Patients should be encouraged
to brush their teeth and gums after each meal and at bedtime.
When brushing, the patient should use an ultra soft toothbrush
and rinse it under warm water.
21
This helps to avoid damaging
any of the tissues. The toothbrush should be changed often, typi-
cally every three months or after any type of infection. Only mild
toothpastes should be used, and these patients should avoid using
any strong favors or whitening toothpastes, as these can irritate
the gingiva. The patient should swab their teeth and gums with a
gentle cloth if they cannot tolerate even a mild toothbrush.
21
The dental hygienist should also encourage the patient to foss
at least once daily, but the patient should never foss any areas that
are bleeding heavily. Baking soda rinsesare sometimes soothing
to the oral mucosa and may be pallative.
21
Topical fuoride can be
used to prevent the caries that are caused by the inhibited salivary
fow. The hygienist should make sure to tell the patient never to
use a mouthwash that contains alcohol.
21
This will cause a strong
burning sensation. Patients should be encouraged to report any
redness, tenderness or sores on their lips or mouth and to seek
prompt treatment for oral mucositis or infection.
Also, if the patient wears dentures, the hygienist should make
sure that they ft properly. Ill-ftting dentures greatly increase the
risk of developing osteonecrosis of the jaw.
21
The dentures should
be removed and cleaned every night, and the patient should not
wear their dentures while they are sleeping.
9
Conclusion
When people fnd out that they will be going through chemother-
apy for cancer treatment, they usually think of side efects such as
losing their hair, vomiting, or fatigue. They are much less likely
to think of the side efects that will take place in their mouths, al-
though these oral implications can be just as bad as the other side
efects. As dental professionals, it is our responsibility to supply
these patients with the necessary knowledge and tools to deal with
these oral side efects. In order to accomplish this task, we need to
be knowledgeable on the subject, and this will help us to provide
the best care possible to each and every one of our patients.
References
1. American Society for Radiation Oncology. Fast facts about
cancer. Available at: http://www.rtanswers.org/statistics/
aboutcancer.aspx. Accessed on November 31, 2012.
2. American Cancer Society. Cancer prevalence: how many
people have cancer? 2011. Available at: http://www.cancer.
org/Cancer/CancerBasics/cancer-prevalence. Accessed on
February 23, 2012.
3. Bablenis Haveles E. Antineoplastic Drugs. In Bablenis Haveles
E, ed. Applied Pharmacology for the Dental Hygienist. 6th ed.
St. Louis, MO: Mosby-Elsevier; 2011:269-275.
4. National Cancer Institute. Bisphosphonates may increase the
risk of jaw disease. 2007. Available at: http://www.cancer.gov/
cancertopics/coping/bisphosphonates. Accessed on February
25, 2012.
5. Rosen LS, Gordon D, Kaminski M, et al. Long-term efcacy
and safety of zoledronic acid compared with pamidronate
disodium in the treatment of skeletal complications in patients
with advanced multiple myeloma or breast carcinoma: A
randomized, double-blind, multicenter, comparative trial.
Cancer 2003;98:1735-1744.
6. Saad F, Gleason DM, Murray R, et al. Long-term efcacy of
zoledronic acid for the prevention of skeletal complications in
patients with metastatic hormone refractory prostate cancer. J
Natl Cancer Inst 2004;96:879-882.
7. Rosen LS, Gordon D, Tchekmedyian NS, et al. Long-term
efcacy and safety of zoledronic acid in the treatment of skeletal
metastases in patients with nonsmall cell lung carcinoma and
other solid tumors: A randomized, phase III, double-blind,
placebo-controlled trial. Cancer 2004;100:2613-2621.
8. Migliorati CA, Woo SB, Hewson I, Barasch A, Elting
LS, Spijkervet FK, Brennan MT. A systematic review of
bisphosphonate osteonecrosis (BON) in cancer. Supportive
Care in Cancer 2010;18:1099-1106.
9. Ruggiero S, Gralow J, Marx R, et al. Practical Guidelines for
the Prevention, Diagnosis, and Treatment of Osteonecrosis of
the Jaw in Patients with Cancer. American Society of Clinical
Oncology 2006; 2: 7-14. Available at: http://jop.ascopubs.org/
content/2/1/7.full. Accessed on October 3, 2012.
10. Osteogenesis Imperfecta Foundation. What is Osteonecrosis
of the Jaw? 2006. Available at: http://www.oif.org/site/
DocServer/Osteonecrosis_of_the_Jaw.pdf?docID=7218.
Accessed on February 24, 2012.
11. Clarkson J, Worthington H, and Eden O. Interventions for
treating oral mucositis for patients with cancer receiving
treatment. Australian Dental Journal 2008;53:363-5 Available at:
http://www.ncbi.nlm.nih.gov/pubmed/20687070. Accessed
on February October 4, 2012.
12. Elting SS, Cooksley C, Chambers M, Cantor SB, Manzullo
E, Rubenstein EB. The burdens of cancer therapy: Clinical
and economic outcomes of chemotherapy-induced mucositis.
Cancer 2003;98:1531-9.
13. Rubenstein EB, Peterson DE, Schubert M, et al. Clinical
practice guidelines for the prevention and treatment of cancer
therapyinduced oral and gastrointestinal mucositis. Cancer
2004;100 (suppl May 1):2026-2046.
14. Bellm LA, Epstein JB, Rose-Ped A, Martin P, Fuchs HJ. Patient
reports of complications of bone marrow transplantation.
Support Care Cancer. 2000;8:3339.
15. Oral Cancer Foundation. Prevention and treatment of oral
mucositis in cancer patients. Best Practice 1998;2:1-6., Available
at http://www.oralcancerfoundation.org/dental/pdf/
mucositis.pdf. Accessed on October 31, 2012.
16. Lalla RV, Sonis ST, Peterson DE. Management of oral mucositis
in patients with cancer. Dent Clin North Am 2008;52:61viii.
17. Harris DJ. Cancer treatment-induced mucositis pain: strategies
for assessment and management. Therapeutics and Clinical
Risk Management 2006;2:251258.
18. Kefe DM, Schubert MM, Elting LS, et al. Updated clinical
practice guidelines for the prevention and treatment of
mucositis. Cancer 2007;109:820-31.
19. Symonds N. Special Needs: Chemotherapy and Head and
Neck Radiation Patients. 1998. Available at: http://www.
learningplaceonline.com/nutrition/food/ca-during/mouth/
72 | rdhmag.com RDH | April 2013
special-needs.htm. Accessed on February 23, 2012.
20. WebMD. Complete Blood Count. 2010. Available at: http://
www.webmd.com/a-to-z-guides/complete-blood-count-cbc.
Accessed on March 4, 2012.
21. Anderson R. Oral Care for Cancer Patients. 2011. Available at:
http://www.slideshare.net/lreneeanderson87/oral-care-for-
cancer-patients-power-point. Accessed on February 24, 2012.
22. www.drugs.com Accessed on February 23, 2012
Author Profile
Laurel Swartzentruber is a 2013 Bachelor of Science Degree
Candidate in the Gene W. Hirschfeld School of Dental Hygiene,
Old Dominion University, Norfolk, Virginia. This paper was the
result of Ms. Swartzentrubers research project for the Univer-
sitys Honors Program. She plans on practicing dental hygiene in
the Virginia Beach area.
Dr. Elena Bablenis Haveles, Bs Pharmacy, PharmD is an
Adjunct Associate Professor of Pharmacology in the Gene W.
Hirschfeld School of Dental Hygiene, Old Dominion Univer-
sity, Norfolk, Virginia. Dr. Haveles has taught at Old Dominion
University for almost 20 years. Please direct all correspondence
to Dr. Haveles. She can be contacted at ehaveles@odu.edu
Disclaimer
The authors have no afliations with any company that would have a gained
interest in the material published in this course. There was no corporate spon-
sor in the making of this course and the authors are not employed by a company
that would stand to proft from the publication of this course. All the research is
presented in an unbiased manner.
Reader Feedback
We encourage your comments on this or any PennWell course. For your conve-
nience, an online feedback form is available at www.ineedce.com.
Notes
RDH | April 2013 rdhmag.com | 73
Online Completion
Use this page to review the questions and answers. Return to www.ineedce.com and sign in. If you have not previously purchased the program select it from the Online Courses listing and complete the online purchase.
Once purchased the exam will be added to your Archives page where a Take Exam link will be provided. Click on the Take Exam link, complete all the program questions and submit your answers. An immediate grade
report will be provided and upon receiving a passing grade your Verifcation Form will be provided immediately for viewing and/or printing. Verifcation Forms can be viewed and/or printed anytime in the future by
returning to the site, sign in and return to your Archives Page.
Questions
1. All of the following are oral care guidelines for
patients undergoing chemotherapy except one.
Which of the following is the exception?
a. Only use mild toothpastes.
b. Dont foss areas that are bleeding heavily.
c. Only use medium toothbrushes.
d. Use a chlorhexidine rinse to help prevent infections.
2. Which of the following is an oral side efect of
bisphosphonates?
a. Osteonecrosis of the jaw
b. Gingival hyperkeratosis
c. Gingival hyperplasia
d. Migratory glossitis
3. All of the following are symptomatic treat-
ments for mucositis except one. Which of the
following is the exception?
a. Avoid spicy foods.
b. Keep the lips well moisturized.
c. Use analgesics or topical anesthetics.
d. Rinse with an alcohol mouthwash.
4. Before dental care can be rendered for a
cancer patient, platelet counts should be above
_________________ mm.
a. 25,000
b. 50,000
c. 75,000
d. 100,000
5. All of the following are common oral fndings
in patients undergoing chemotherapy except
one. Which of the following is the exception?
a. Xerostomia
b. Actinic cheilitis
c. Excess bioflm
d. Mouth ulcers
6. The frequency of maintenance oral health
cleanings for patients with risk factors and
overall poor health that are receiving bisphos-
phonates is:
a. Every 6 months
b. Every 3-4 months
c. Monthly
d. Every 2 months
7. All of the following are risk factors for develop-
ing osteonecrosis except one. Which one is the
exception?
a. tooth extractions
b. oral surgery
c. ill-ftting dentures
d. xerostomia
8. Chemotherapy can cause nausea and vomiting,
which can lead to the erosion of tooth enamel.
The dental hygienist should instruct the patient
to perform which of the following oral health
care measures after vomiting:
a. Rinse with a alcohol-free mouth rinse
b. Brush with a soft-bristle toothbrush and a mild
toothpaste
c. Rinse with lukewarm water
d. Rinse with hot water
9. All of the following provide short-term
symptomatic relief for the treatment of the pain
associated with mucositis except one. Which
one is the exception?
a. alcohol-containing mouth rinses
b. ice chips
c. 2% viscous lidocaine
d. saline mouth rinses
10. Patients undergoing chemotherapy should be
encouraged to change their toothbrushes:
a. every 6 months
b. only after an infection
c. every 3-4 months or after any infection
d. every 6 months or after any infection
11. According to the American Cancer Society,
approximately how many people are living
with invasive cancer?
a. 5,000,000
b. 10,000,000
c. 12,000,000
d. 3,000,000
12. Which of the following classes of drugs is
associated with osteonecrosis of the jaw?
a. Aromatase inhibitors
b. Bisphosphonates
c. Vinca alkaloids
d. Taxanes
13. All of the following are typical signs and symp-
toms of osteonecrosis EXCEPT one. Which of
the following is the EXCEPTION?
a. Localized pain
b. Soft tissue swelling
c. Exposed bone
d. feeling of a heavy jaw
14. Once osteonecrosis develops, it can lead to
other oral side efects. Which of the following is
one of those side efects?
a. Poor healing time
b. Mouth sores
c. Dry mouth
d. Metallic taste
15. Which of the following can be used to protect
areas of exposed bone as a result of bisphospho-
nate therapy?
a. Oral antibiotics
b. A thin mouthguard or removable appliance
c. Topical antibiotics
d. A permanent appliance
16. According to current research, which of the
following is the drug of choice for avoiding
infections in patients with osteonecrosis as a
result of bisphosphonate therapy?
a. Metronidazole
b. Clarithromycin
c. Tetracycline
d. Penicillin
17. Patients that experience xerostomia as a result
of chemotherapy drugs are at higher risk for
developing caries. The dental hygienist should
recommend which of the following to help
reduce that risk?
a. Use of a home fuoride regimen
b. Use of alcohol-free mouth rinses
c. Use of standard alcohol rinses
d. Use of sour candies
18. According to the National Cancer Institute,
the incidence of Grade 3-4 oral and gastroin-
testinal mucositis is estimated at:
a. 15%-20%
b. 5%-10%
c. 5%-15%
d. 1%-5%
19. The incidence of oral and gastrointestinal
mucositis in patients undergoing high-dose
chemotherapy with hematopoietic stem cell
transplantation is:
a. 50%
b. 100%
c. 90%
d. 75%
20. The primary method of treating mucositis is
palliative therapy. All of the following are con-
sidered to be palliative EXCEPT one. Which of
the following is the EXCEPTION?
a. Pain control
b. Oral mouth rinses
c. Intravenous pain medication
d. Palliative treatment of dry mouth
21. Though they do not provide long-term relief
all of the following EXCEPT one provide short-
term relief for the pain associated with mucositis.
a. Ice chips
b. Saline mouth rinses
c. 2% viscous lidocaine with a topical, alcohol-free mouth rinse
d. 4% viscous lidocaine with a topical, alcohol-free mouth rinse
22. 2% Viscous lidocaine is an efective means of
controlling mucositis pain. It is often mixed
with all of the following EXCEPT one. Which
one is the EXCEPTION?
a. Sucralfate
b. Diphenhydramine
c. Maalox
d. Kaopectate
23. Which of the following is recommended for
patients undergoing hematopoietic stem cell
transplantation that experience mucositis?
a. Ibuprofen
b. Codeine
c. Morphine
d. Hydrocodone
24. All of the following are efective in treating
mucositis pain EXCEPT for one. Which of the
following is the EXCEPTION?
a. Cryotherapy
b. NSAIDS
c. Benzydamine topical rinse
d. Gabapentin
25. The Hyposalivation associated with che-
motherapy can aggravate existing mucositis.
Patients can be advised to rinse with which of
the following solutions?
a. teaspoonful of baking soda and/or teaspoonful of
salt in 2 cups lukewarm water several times a day.
b. teaspoonful of baking soda and/or teaspoonful of
salt in 1 cups lukewarm water several times a day.
c. teaspoonful of baking soda and/or teaspoonful of
salt in 2 cups lukewarm water several times a day.
d. teaspoonful of baking soda and/or teaspoonful of
salt in 1 cups lukewarm water several times a day.
26. All of the following can be used to treat the dry
mouth associated with chemotherapy EXCEPT for
one. Which of the following is the EXCEPTION?
a. Sip water
b. Chew tart, sugarless gum or candy
c. Use of anticholinergic drugs
d. Artifcial saliva substitutes
27. Cancer chemotherapeutic agents can cause
many diferent oral side efects. Which of the
following drugs can cause mouth sores?
a. Exemestane
b. Trastuzumab
c. Doxorubicin
d. Anastrozole
28. Which of the following cancer chemothera-
peutic agents can cause oral taste changes?
a. Anastrazole
b. Paclitaxel
c. Letrozole
d. Cyclophosphamide
29. Cancer chemotherapeutic drugs are known to
adversely afect the bone marrow. Which of the fol-
lowing drugs is an EXCEPTION to this statement?
a. Paclitaxel
b. Doxorubicin
c. Cyclophosphamide
d. Letrozole
30. Which of the following cancer chemothera-
peutic agents can cause Hyperpigmentation of
the oral mucosa?
a. Doxorubicin
b. Cyclophosphamide
c. Exemestane
d. Letrozole
Customer Service 216.398.7822
For IMMEDIATE results,
go to www.ineedce.com to take tests online.
Answer sheets can be faxed with credit card payment to
(440) 845-3447, (216) 398-7922, or (216) 255-6619.
Payment of $49.00 is enclosed.
(Checks and credit cards are accepted.)
If paying by credit card, please complete the
following: MC Visa AmEx Discover
Acct. Number: ______________________________
Exp. Date: _____________________
Charges on your statement will show up as PennWell
If not taking online, mail completed answer sheet to
Academy of Dental Therapeutics and Stomatology,
A Division of PennWell Corp.
P.O. Box 116, Chesterland, OH 44026
or fax to: (440) 845-3447
PLEASE PHOTOCOPY ANSWER SHEET FOR ADDITIONAL PARTICIPANTS.
ANSWER SHEET
Oral Health Care during Chemotherapy
Name: Title: Specialty:
Address: E-mail:
City: State: ZIP: Country:
Telephone: Home ( ) Ofce ( ) Lic. Renewal Date:
Requirements for successful completion of the course and to obtain dental continuing education credits: 1) Read the entire course. 2) Complete all
information above. 3) Complete answer sheets in either pen or pencil. 4) Mark only one answer for each question. 5) A score of 70% on this test will earn
you 2 CE credits. 6) Complete the Course Evaluation below. 7) Make check payable to PennWell Corp. For Questions Call 216.398.7822
CHEMO413RDH
COURSE EVALUATION and PARTICIPANT FEEDBACK
We encourage participant feedback pertaining to all courses. Please be sure to complete the survey included
with the course. Please e-mail all questions to: hhodges@pennwell.com.
INSTRUCTIONS
All questions should have only one answer. Grading of this examination is done manually. Participants will
receive confrmation of passing by receipt of a verifcation form. Verifcation of Participation forms will be
mailed within two weeks after taking an examination.
COURSE CREDITS/COST
All participants scoring at least 70% on the examination will receive a verifcation form verifying 2 CE
credits. The formal continuing education program of this sponsor is accepted by the AGD for Fellowship/
Mastership credit. Please contact PennWell for current term of acceptance. Participants are urged to contact
their state dental boards for continuing education requirements. PennWell is a California Provider. The
California Provider number is 4527. The cost for courses ranges from $20.00 to $110.00.
PROVIDER INFORMATION
PennWell is an ADA CERP Recognized Provider. ADA CERP is a service of the American Dental Association
to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP
does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours
by boards of dentistry.
Concerns or complaints about a CE Provider may be directed to the provider or to ADA CERP at www.ada.
org/cotocerp/.
The PennWell Corporation is designated as an Approved PACE Program Provider by the Academy of General
Dentistry. The formal continuing dental education programs of this program provider are accepted by the
AGD for Fellowship, Mastership and membership maintenance credit. Approval does not imply acceptance
by a state or provincial board of dentistry or AGD endorsement. The current term of approval extends from
(11/1/2011) to (10/31/2015) Provider ID# 320452.
RECORD KEEPING
PennWell maintains records of your successful completion of any exam for a minimum of six years. Please
contact our ofces for a copy of your continuing education credits report. This report, which will list all
credits earned to date, will be generated and mailed to you within fve business days of receipt.
Completing a single continuing education course does not provide enough information to give the
participant the feeling that s/he is an expert in the feld related to the course topic. It is a combination of
many educational courses and clinical experience that allows the participant to develop skills and expertise.
CANCELLATION/REFUND POLICY
Any participant who is not 100%satisfed with this course can request a full refund by contacting PennWell in writing.
IMAGE AUTHENTICITY
The images provided and included in this course have not been altered.
2013 by the Academy of Dental Therapeutics and Stomatology, a division of PennWell
Educational Objectives
1. List the signs and symptoms of osteonecrosis associated with bisphosphonate therapy.
2. Describetheoralhealthcarethatpatientsreceivingbisphosphonatesshouldperforminordertominimizetheriskof
developing osteonecrosis.
3. Describe the potential consequences of tooth extraction in a patient receiving bisphosphonate therapy.
4. List and describe the treatments available for oral mucositis.
5. Listanddescribetheguidelinesthatthedentalhygienistshouldusewhenperformingoralhealthcareonpatients
receiving chemotherapy.
6. Listanddescribetheguidelinesthatthepatientreceivingchemotherapyshouldfollowtomaintaingoodoralhealthcare.
Course Evaluation
1. Were the individual course objectives met? Objective #1: Yes No Obj ecti ve #3: Yes No
Objective #2: Yes No Objective#4: Yes No
Objective #5: Yes No Objective #6: Yes No
Please evaluate this course by responding to the following statements, using a scale of Excellent = 5 to Poor = 0.
2. To what extent were the course objectives accomplished overall? 5 4 3 2 1 0
3. Please rate your personal mastery of the course objectives. 5 4 3 2 1 0
4. How would you rate the objectives and educational methods? 5 4 3 2 1 0
5. How do you rate the authors grasp of the topic? 5 4 3 2 1 0
6. Please rate the instructors efectiveness. 5 4 3 2 1 0
7. Was the overall administration of the course efective? 5 4 3 2 1 0
8. Please rate the usefulness and clinical applicability of this course. 5 4 3 2 1 0
9. Please rate the usefulness of the supplemental webliography. 5 4 3 2 1 0
10. Do you feel that the references were adequate? Yes N o
11. Would you participate in a similar program on a different topic? Yes N o
12. If any of the continuing education questions were unclear or ambiguous, please list them.
___________________________________________________________________
13. Was there any subject matter you found confusing? Please describe.
___________________________________________________________________
___________________________________________________________________
14. How long did it take you to complete this course?
___________________________________________________________________
___________________________________________________________________
15. What additional continuing dental education topics would you like to see?
___________________________________________________________________
___________________________________________________________________
AGD Code 730
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- SyllabusDocumento12 páginasSyllabusvacharaAinda não há avaliações
- I PKDocumento81 páginasI PKvacharaAinda não há avaliações
- SensitivityDocumento11 páginasSensitivityvacharaAinda não há avaliações
- Dental SedationDocumento7 páginasDental SedationvacharaAinda não há avaliações
- Types of Outcome MeasuresDocumento91 páginasTypes of Outcome MeasuresvacharaAinda não há avaliações
- Table 1 Antibiotics To Be AvoidedDocumento2 páginasTable 1 Antibiotics To Be AvoidedvacharaAinda não há avaliações
- Table 236-2 Pharmacokinetic (PK) Steps Pertaining To Drug Metabolism and InteractionsDocumento2 páginasTable 236-2 Pharmacokinetic (PK) Steps Pertaining To Drug Metabolism and InteractionsvacharaAinda não há avaliações
- ' Interactions Before Administration ' Occur As A Result of Chemical Inactivation or Physical Incompatibility ' Harmful or TherapeuticDocumento6 páginas' Interactions Before Administration ' Occur As A Result of Chemical Inactivation or Physical Incompatibility ' Harmful or TherapeuticvacharaAinda não há avaliações
- Drug Action: +liver+diseasev2Documento23 páginasDrug Action: +liver+diseasev2vacharaAinda não há avaliações
- Drug InfoDocumento12 páginasDrug InfovacharaAinda não há avaliações
- Assessing PrescriptionDocumento1 páginaAssessing PrescriptionvacharaAinda não há avaliações
- Pharmacokinetics: Drug Absorption 1. Topic ObjectivesDocumento1 páginaPharmacokinetics: Drug Absorption 1. Topic ObjectivesvacharaAinda não há avaliações
- Antiseptics and DisinfectantsDocumento4 páginasAntiseptics and DisinfectantsvacharaAinda não há avaliações
- Warfarin DI ADocumento2 páginasWarfarin DI AvacharaAinda não há avaliações
- Met Form inDocumento16 páginasMet Form invacharaAinda não há avaliações
- Pharm Table 03Documento1 páginaPharm Table 03vacharaAinda não há avaliações
- The ChallengeDocumento9 páginasThe ChallengevacharaAinda não há avaliações
- Anti Fun GalsDocumento18 páginasAnti Fun GalsvacharaAinda não há avaliações
- Pines City Colleges: College of NursingDocumento1 páginaPines City Colleges: College of NursingJoy Erica LeoAinda não há avaliações
- Aconitum Ferox - Blue AconiteDocumento2 páginasAconitum Ferox - Blue Aconitejcoppala4476100% (1)
- Table of Specifications in Health 10Documento3 páginasTable of Specifications in Health 10Rowan ZheeAinda não há avaliações
- Physical Examination:-: Vital SignsDocumento4 páginasPhysical Examination:-: Vital SignspriyaAinda não há avaliações
- Yin FireDocumento4 páginasYin FireezraallenAinda não há avaliações
- GALLBLADDERDocumento16 páginasGALLBLADDERKadenceFreya-Charisse G PosadasBulintao100% (2)
- 6 01 11Documento36 páginas6 01 11grapevineAinda não há avaliações
- Diaper Decoder Poster v2Documento1 páginaDiaper Decoder Poster v2abhiAinda não há avaliações
- The Factories Act, 1948Documento14 páginasThe Factories Act, 1948Nirmalkumar NatarajanAinda não há avaliações
- Gynecology Reconstructive Surgery - Volume 2Documento318 páginasGynecology Reconstructive Surgery - Volume 2Bharti Pant GahtoriAinda não há avaliações
- Bartleby and Infantile AutismDocumento4 páginasBartleby and Infantile AutismAlyna Marya IoaneiAinda não há avaliações
- The Science Behind Holosync and Other NeurotechnologiesDocumento13 páginasThe Science Behind Holosync and Other NeurotechnologiesTheHiddenSoldiersAinda não há avaliações
- Anatomical Foundations of Chinese MedDocumento29 páginasAnatomical Foundations of Chinese Medanattā100% (1)
- TONSILLITIS AND TONSIL STONE EdittedDocumento5 páginasTONSILLITIS AND TONSIL STONE EdittedNineja NinejaAinda não há avaliações
- Acupuncture With Manual and Electrical Stimulation For Labour Pain: A Two Month Follow Up of Recollection of Pain and Birth ExperienceDocumento9 páginasAcupuncture With Manual and Electrical Stimulation For Labour Pain: A Two Month Follow Up of Recollection of Pain and Birth ExperiencejayaAinda não há avaliações
- The Tongue - Facts, Function & Diseases - Live SciencerDocumento12 páginasThe Tongue - Facts, Function & Diseases - Live SciencerImtiax LaghariAinda não há avaliações
- Swedish Group - ProgrammeDocumento3 páginasSwedish Group - Programmemarudo01Ainda não há avaliações
- Duyên H I 21 25Documento62 páginasDuyên H I 21 25Arina SakuraAinda não há avaliações
- Resilience in Nurses - An Integrative ReviewDocumento15 páginasResilience in Nurses - An Integrative ReviewBob SmithAinda não há avaliações
- A Guide To Radio Frequency Hazards With Electric DetonatorsDocumento37 páginasA Guide To Radio Frequency Hazards With Electric Detonatorszix013Ainda não há avaliações
- Evaluate Med TechDocumento35 páginasEvaluate Med TechWilly Pérez-Barreto MaturanaAinda não há avaliações
- c1 Mother Friendly Care NewDocumento20 páginasc1 Mother Friendly Care NewOng Teck Chong100% (1)
- The Independent 21 February 2016Documento60 páginasThe Independent 21 February 2016artedlcAinda não há avaliações
- 5SDocumento5 páginas5SKakek SugionoAinda não há avaliações
- MSC 1st Year RequirementsDocumento6 páginasMSC 1st Year RequirementsSilja Manoj100% (1)
- Programme Guide Certificate in Community Health (BPCCHN) - CompressedDocumento120 páginasProgramme Guide Certificate in Community Health (BPCCHN) - CompressedChakrapani ChaturvediAinda não há avaliações
- Lit Review Paper 1Documento7 páginasLit Review Paper 1api-679552755Ainda não há avaliações
- ONDANSENTRONDocumento2 páginasONDANSENTRONErza GenatrikaAinda não há avaliações
- Flexor Tendon Repairs Zones I III 05-13-2013Documento3 páginasFlexor Tendon Repairs Zones I III 05-13-2013Mihaela DoniciAinda não há avaliações
- Grand Strategy MatrixDocumento1 páginaGrand Strategy MatrixDominic SociaAinda não há avaliações