Escolar Documentos
Profissional Documentos
Cultura Documentos
Acute Renal Failure
Enviado por
RohitKumarDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Acute Renal Failure
Enviado por
RohitKumarDireitos autorais:
Formatos disponíveis
Mayo Clin Proc, January 2001, Vol 76 Acute Renal Failure 67
Mayo Clin Proc. 2001;76:67-74 67 2001 Mayo Foundation for Medical Education and Research
Conci se Revi ew for Cl i ni ci ans
Acute Renal Failure: A Practical Update
ROBERT C. ALBRIGHT, JR, DO
From the Division of Nephrology and Internal Medicine and Division
of Pulmonary and Critical Care Medicine and Internal Medicine,
Mayo Clinic, Rochester, Minn.
A question-and-answer section appears at the end of this article.
Address reprint requests and correspondence to Robert C. Albright,
J r, DO, Division of Nephrology, Mayo Clinic, 200 First St SW,
Rochester, MN 55905 (e-mail: albright.robert@mayo.edu).
Acute renal failure (ARF) affects almost all medical spe-
cialties. Its occurrence seems to be increasing in hospital-
ized patients. A structured approach to the evaluation and
management of ARF would facilitate rapid diagnosis and
treatment in most patients. Appreciation for the multiple
drugs that affect renal function is especially important.
Exclusion of urinary outflow obstruction and administra-
tion of therapies that improve renal perfusion should be
given top priority with respect to managing ARF. Dialytic
intervention for ARF is required when otherwise irrevers-
A
cute renal failure (ARF) is a syndrome with multiple
causes; its associated consequences affect all organ
systems. Defined as a sudden loss of renal function (over
several hours to several days), ARF results in derange-
ments in extracellular fluid balance, acid base, electrolytes,
and divalent cation regulation. However, an increased se-
rum creatinine concentration, accumulation of other nitrog-
enous-based waste products, and often a decline in urinary
output are the hallmarks of ARF.
Although many advances in organ support technologies
have occurred during the past 2 decades, the absolute mortal-
ity rates for ARF acquired in the hospital and in the intensive
care unit (ICU) are approximately 45% and 70%, respec-
tively.
1
However, the demographics of ARF have changed
over the past 2 decades, with patients generally being older
and having a higher acuity of illness based on multiple
scoring systems. Fortunately, renal functional recovery
(ability to discontinue dialysis) over the past 20 years has
remained greater than 50% to 75% in survivors of ARF.
1
EPIDEMIOLOGY
Rigorous study of ARF is complicated by the lack of a
uniform definition. More than 20 definitions have been
published in both basic science and clinical trials. Despite
these difficulties, ARF occurs in approximately 1% of
hospitalized patients, in as many as 20% of patients treated
ACE = angiotensin-converting enzyme; ARF = acute renal
failure; ATN = acute tubular necrosis; ICU = intensive care
unit; NSAIDs = nonsteroidal anti-inflammatory drugs
ible pathophysiologic derangements of electrolyte homeo-
stasis, fluid balance, and uremic solute control are immi-
nent. This article provides a brief review and update on the
clinical evaluation and management of ARF.
Mayo Clin Proc. 2001;76:67-74
in ICUs, and as many as 4% to 15% of patients after
cardiovascular surgery.
1
Approximately 30% of patients
who experience ARF will require renal replacement ther-
apy.
1
Community-acquired ARF occurs in approximately
209 patients per 1 million population, and the frequency
of this syndrome appears to be increasing in hospitalized
patients.
2
ASSESSMENT OF THE PATIENT WITH ARF
Because of the various causes of ARF, effective use of
history and medical chart review, physical examination,
and laboratory testing are essential to recognize and correct
the factors quickly that cause ARF. Results of these evalu-
ations will help to classify patients into 1 of 3 major diag-
nostic categories of ARF: traditional prerenal, postrenal,
and intrinsic renal.
Medi cal Chart Revi ew and Physi cal Exami nat i on
A thorough review of the patients history often reveals
possible contributing factors of ARF, such as nephrotoxin
exposure, episodes of blood pressure swings, and predis-
posing conditions for renal damage (hypertension and dia-
betes). Determination of a familial history of renal disease
and a personal history of urolithiasis or urinary outlet
symptoms is often helpful in the evaluation of ARF.
Intravascular volume status is perhaps the most impor-
tant factor in the evaluation of ARF. Extracellular volume
depletion is often suggested by tachycardia, orthostatic
blood pressure changes, dry mucous membranes, or hy-
potension. However, obtaining serial weights of hospital-
ized patients often proves crucial in determining volume
status. Physical examination findings suggestive of con-
gestive heart failure or cirrhosis that leads to functional
renal hypoperfusion deserve special attention. Skin condi-
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
Acute Renal Failure Mayo Clin Proc, January 2001, Vol 76 68
tions such as cutaneous exanthems, purpura, livedo retic-
ularis, microinfarctions, stigma of endocarditis, and limb
ischemia often provide valuable clues in ascertaining
causes of ARF. A distended bladder, costovertebral angle
tenderness, or prostatic hypertrophy is suggestive of ob-
structive uropathy.
A decrease in urinary volume is often one of the initial
clinical findings in ARF. Categorization of renal failure
into oliguric or nonoliguric is of diagnostic importance. Ol-
iguria is defined as a urinary output of less than 400 mL/d.
Anuria (<50 mL of urinary output per day) suggests acute
cortical necrosis, obstructive uropathy, or a vascular catas-
trophe causing cessation of renal perfusion.
Laborat ory Test i ng
The diagnosis of ARF is primarily determined by in-
creasing levels of nitrogenous-based waste products, such
as creatinine or blood urea nitrogen, often along with a
decline in urinary production. Unfortunately, a well-ac-
cepted common definition of ARF does not exist. Gener-
ally, a decline in renal function occurring over hours to
days involving an increase in nitrogenous-based waste
products such as a serum creatinine level by more than 0.5
mg/dL, an increase of 50% or more in serum creatinine
over the baseline serum creatinine level, and a decline of
calculated or measured creatinine clearance by more than
25% are accepted as indicators of ARF. Pseudoacute renal
failure may occur when substances (ketoacids, cefoxitin)
are falsely analyzed as creatinine, when creatinine produc-
tion is increased (mild muscle protein breakdown), or when
a substance (trimethoprim, cimetidine) inhibits renal tubu-
lar creatinine secretion.
Determination of serum electrolytes offers valuable in-
formation, such as potassium levels, clues about volume
status (high bicarbonate, elevated blood urea nitrogen-
creatinine ratio, hypernatremia), acidosis, and anion gap.
Therefore, an electrolyte panel should be part of the re-
quired evaluation of all patients with ARF. Additionally,
determination of calcium, phosphorus, albumin, uric acid,
and creatine kinase levels as well as liver function tests
often add important information.
Arguably, the most important laboratory test for a pa-
tient with ARF is urinalysis. Both the urinary sediment and
the urinary indices in combination with serum values can
often be extremely helpful in determining the cause of
ARF. Conceptually, these indices are designed to deter-
mine whether tubular function is intact. A low fractional
excretion of sodium (<1%) suggests that oliguria (and per-
haps azotemia) is likely due to decreased renal perfusion,
and the nephron is responding appropriately by decreasing
the excretion of filtered sodium to improve plasma volume
and perfusion. The various serum and urinary findings
used in diagnosing the major causes of ARF are shown in
Table 1.
Discovery of an active urinary sediment should lead to a
focused set of serologic tests to determine whether an
autoimmune diathesis is present. Renal biopsy should be
considered when no apparent cause of ARF is found or to
achieve tissue diagnosis of a suspected glomerulonephritis
associated with ARF.
Radi ol ogi c Eval uat i on
A renal ultrasound study is key in the evaluation of
ARF. Valuable information about renal size, echotexture
(parenchymal density), and renal vascular status (with
Doppler evaluation) is obtained with this noninvasive test.
Specifically, renal ultrasonography is most often per-
formed to rule out obstructive uropathy as the cause of
ARF. Unfortunately, renal ultrasonography is neither
highly sensitive nor specific for obstructive uropathy (see
subsequent discussion), but accuracy increases with serial
examinations. Computed tomograms (without contrast)
and nuclear perfusion scans have a limited role in the
evaluation of ARF.
Cat egori zat i on of ARF
More than 50 identified pathophysiologic pathways are
responsible for ARF. Traditionally, the evaluation of ARF
has focused on the determination of whether the cause of
renal failure is prerenal (a condition resulting in decreased
effective renal perfusion), postrenal (an obstruction to
urinary outflow), or intrinsic renal (due to pathophysi-
ologic derangements in the renal tubules, interstitium, vas-
culature, or glomeruli). This designation has not yet been
improved.
PRERENAL CAUSES
Overall, 60% of cases of community-acquired ARF are due
to prerenal conditions.
2
Frequently, this disorder is caused
by excessive, nonreplaced fluid deficits due to gastrointes-
tinal, renal, or cutaneous losses. However, hospital-ac-
quired prerenal renal failure is primarily due to decreased
effective renal perfusion. Often, congestive heart failure,
cirrhosis, or sepsis (hyperdynamic vasodilated hypotensive
states with cytokinemia) is noted. A continuum exists be-
tween prerenal renal failure and ischemic acute tubular
necrosis (ATN); thus, prompt recognition and therapy for
prerenal conditions is necessary before irreversible is-
chemic tubular necrosis develops. Commonly, prerenal
conditions that otherwise would not progress to frank ATN
do so in the setting of acute multisystemic illness and
ongoing additional renal insults. Of importance, many
medications induce a functional prerenal state because of
alterations in glomerular hemodynamics.
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
Mayo Clin Proc, January 2001, Vol 76 Acute Renal Failure 69
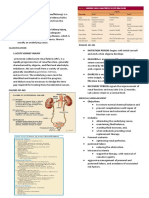
Table 1. Laboratory Evaluation of Acute Renal Failure*
Test Prerenal Intrinsic renal Postrenal
BUN/Cr ratio >20 10-20 10-20
Urine specific gravity >1.020 ~1.010 >1.010 early, <1.0101 late
Uosm (mOsm/kg) >350 ~300 >400 early, ~300 late
UNa (mEq/L) <20 >30 <20 early, >40 late
FeNa (%) <1 >2-3 <1 early, >3 late
UCr/PCr ratio 40 20 >40 early, 20 late
Urine microscopy Normal ATN: dark granular casts, Normal hyaline, granular
hyaline casts hyaline casts, renal epithelial casts
cells/casts
GN: RBCs, dysmorphic RBC
(>20%), RBC casts,
WBC/WBC casts, proteinuria
AIN: urine eosinophilia, WBC,
WBC casts, hyaline casts
(consider CES)
*AIN = acute interstitial nephritis; ATN = acute tubular necrosis; BUN = blood urea nitrogen; CES = cholesterol
emboli syndrome; Cr = creatinine; FeNa = fractional excretion of sodium (calculated as UNa/PNa PCr/UCr
100); GN = glomerulonephritis; PCr = plasma creatinine; PNa = plasma sodium; RBC = red blood cell; UCr =
urinary creatinine; UNa = urinary sodium; Uosm = urinary osmolality; WBC = white blood cell.
Falsely low FeNa seen occasionally with acute GN, radiocontrast-induced nephropathy, rhabdomyolysis.
Nonst eroi dal Ant i -i nfl ammat ory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit
prostaglandin-mediated afferent arteriolar vasodilation in
the glomerulus. These prostaglandins are essential for pa-
tients who rely on preglomerular capillary vasodilation to
maintain glomerular capillary pressure. Predisposing fac-
tors for NSAID-induced ARF include congestive heart fail-
ure, cirrhosis, nephrotic syndrome, chronic renal failure,
severe atherosclerotic disease of the renal arteries, and
hypovolemia. Additionally, NSAIDs have been implicated
in acute allergic interstitial nephritis, membranous nephri-
tis, and minimal change nephropathy; occasionally, they
cause hyperkalemia, hyponatremia, and sodium and water
retention.
Angi ot ensi n-Convert i ng Enzyme Inhi bi t ors
Angiotensin-converting enzyme (ACE) inhibitors were
recently shown to be particularly useful in the treatment of
chronic renal diseases. However, these agents continue to
be recognized for their ability to induce ARF. Primarily,
ACE inhibitors can cause ARF by inhibiting the ability of
the glomerular efferent arteriole to vasoconstrict to main-
tain a glomerular filtration rate constant within the auto-
regulatory range. The risk factors with ACE inhibitors
are similar to those with NSAIDs. Acute renal failure asso-
ciated with administration of ACE inhibitors should
prompt investigation to rule out bilateral renal artery steno-
sis or severe renal artery stenosis in a solitary functioning
kidney.
Cal ci neuri n Inhi bi t ors
Calcineurin inhibitors (tacrolimus and cyclosporine) are
used in an increasing number of solid organ transplant
recipients who are often treated by primary care clinicians.
These immunosuppressive agents may induce a prerenal
state due to preglomerular vasoconstriction. Hypovolemia,
a complication associated with calcineurin inhibitor use,
is an often-recognized cause of ARF in recipients of
solid organ transplants. Of importance, the interaction
between several antihypertensive and anti-infective agents
must be remembered in regard to the possibility of these
drug-drug interactions causing elevated levels of cal-
cineurin inhibitors, thereby inducing renal failure. Addi-
tionally, calcineurin inhibitors have occasionally been im-
plicated in inducing microangiopathic hemolytic anemia
causing ARF.
Amphot eri ci n B
Amphotericin B primarily causes distal tubular derange-
ments that lead to decreasing urinary concentration, distal
renal tubular acidosis, potassium wasting, magnesium
wasting, and occasionally profound renal vasoconstriction.
Patients of advanced age with a history of diuretic use
(when use induces hypovolemia or electrolyte imbalance),
high doses of amphotericin therapy, preexisting advanced
renal insufficiency, hypokalemia (due to induction of im-
paired renal concentration capacity), and decreased effec-
tive renal perfusion are particularly at risk for amphotericin
B nephrotoxicity. Prevention of amphotericin B nephrotox-
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
Acute Renal Failure Mayo Clin Proc, January 2001, Vol 76 70
icity is best accomplished by preadministration of intrave-
nous saline solution.
3
Liposomal preparations of ampho-
tericin B have been demonstrated to be less nephrotoxic in
patients with neutropenic fever.
4
However, widespread use
is limited because of expense.
Cont rast -Induced Nephropat hy
Contrast-induced nephropathy causes ARF predomi-
nantly via acute vasoconstriction. Additionally, after de-
creased renal perfusion, the sluggish flow of filtered con-
trast material often causes intratubular precipitation and
ongoing generation of free oxygen radicals.
5
Risk factors for contrast-induced nephropathy are gen-
erally accepted to be a glomerular filtration rate of less than
35 mL/min, diabetic nephropathy, severe heart failure, ad-
ministration of large amounts of contrast, or preexisting
hypokalemia or hypotension.
Despite multiple trials involving numerous therapeutics,
administration of crystalloid (1-1.5 mLkg
1
h
1
for 8-12
hours before a procedure) remains the safest, most effica-
cious, and cost-effective method of preventing contrast-
induced nephropathy. Recently, Tepel et al
6
showed pre-
vention of radiographic-contrastinduced nephrotoxicity
by administering acetylcysteine in two 600-mg doses the
day before along with saline infusion for patients with
stable chronic renal insufficiency (creatinine >2.0 mg/dL).
Immunost i mul ant Agent s
Immunostimulant agents (interleukin 2, tumor necrosis
factor receptor agonists) have rarely been implicated in
causing a capillary leak syndrome, which causes decreased
effective circulating volume similar to sepsis.
Cocai ne
Cocaine induces ARF via multiple pathways. Acute
vasoconstriction of both afferent and efferent arterioles has
been documented in experimental studies of cocaine neph-
rotoxicity. Additionally, cocaine has been implicated in
causing malignant hypertension, rhabdomyolysis, antiglo-
merular basement membrane nephropathy, thrombotic
microangiopathy, renal infarction, and multiple acid base
and electrolyte derangements (metabolic acidosis, respira-
tory alkalosis, hypokalemia, and hyperkalemia-rhabdo-
myolysis). In many urban centers, cocaine-induced nephro-
toxicity is the most common cause of ARF.
7
POSTRENAL CAUSES
Postrenal causes account for 5% to 15% of cases of com-
munity-acquired ARF.
1
A history of prostatism, urolithi-
asis, retroperitoneal disease, or use of medications known
to cause crystalluria should prompt a thorough evaluation
to rule out obstruction. Elderly and young patients are most
commonly affected. Renal ultrasonography is an essential
part of the work-up of any patient with ARF. However,
ultrasonography is neither highly sensitive nor specific
(sensitivity may be only 80%-85%); when the clinical situ-
ation suggests a high probability of postrenal ARF, serial
ultrasound studies may be necessary.
8
Alternatively, spiral
computed tomography (without contrast) may often be of
benefit in delineating obstructive uropathy due to urolithi-
asis.
8
A patent urinary catheter is obviously a required first
step in the work-up of any patient with ARF.
Medication-induced crystalluria causing tubular or ure-
teral obstruction has been known to occur with multiple
drugs. The most common agents that cause this phenom-
enon are acyclovir, the sulfonamides, methotrexate, and
protease inhibitors (indinavir).
RENAL CAUSES
Although the most common cause of ARF in the hospital-
ized patient is intrinsic renal failure due to ATN, the terms
acute tubular necrosis and intrinsic renal failure are not
synonymous. Delineating intrinsic ARF into the 4 distinct
anatomical compartments of the kidney facilitates the most
accurate categorization.
Vascul ar Causes of Int ri nsi c ARF
The incidence of renal failure due to vascular disease is
increasing. Epidemic atherosclerotic vascular disease in
the aging population, widespread use of vasoactive drugs,
and the increased frequency of invasive vascular proce-
dures have led to a general increase in the incidence of
vascular causes of intrinsic ARF.
6
Small-vessel vascular
diseases that cause renal failure, including atheroembolic
renal disease, scleroderma, malignant hypertension, hemo-
lytic uremic syndrome-thrombotic thrombocytopenic pur-
pura, and acute cortical necrosis, are being diagnosed with
much more frequency.
9
These disorders may lead to only
mild prerenal azotemia; however, frequently they lead to
frank tubular damage and necrosis resulting in ARF.
Atheroemboli may also be increasing in frequency.
Acute renal failure in the setting of recent intravascular
intervention or anticoagulation associated with livedo
reticularis, hypocomplementemia, eosinophilia (occasion-
ally with eosinophiluria), blue toe syndrome, or cutaneous
infarctions should prompt consideration of atheroem-
boli. Thrombotic or embolic disease and renal arterial dis-
section, which may present as anuria and flank pain, are
accurately diagnosed with nuclear perfusion scans and
angiography.
Renal Int erst i t i al Di seases
Polypharmacy is common among most patients with
chronic diseases and hospitalized patients. Allergic inter-
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
Mayo Clin Proc, January 2001, Vol 76 Acute Renal Failure 71
stitial nephritis should be strongly considered in all patients
with ARF. A nonexclusive list of agents that have been
firmly implicated in causing allergic interstitial nephritis
include the penicillins, cephalosporins, sulfonamides,
rifampin, ciprofloxacin, NSAIDs, thiazide diuretics, furo-
semide, cimetidine, phenytoin, and allopurinol. Recently,
Chinese herb nephropathy was recognized as an important
cause of fibrotic interstitial nephritis. Chinese herb ne-
phropathy often occurs in patients who use slimming
teas, often labeled Han Fang Ji or Quang Fang Ji. The
causative agent implicated in this disorder is aristolochic
acid. The syndrome of Chinese herb nephropathy is char-
acterized by progressive renal failure with a bland uri-
nary sediment, shrunken hyperechoic kidneys with low-
grade proteinuria, and an association with uroepithelial
cancers.
10
Often, the characteristic eosinophilia, rash, and urinary
eosinophilia are absent in allergic interstitial nephritis.
Therefore, a high index of suspicion is necessary to diag-
nose this disorder. Allergic interstitial nephritis is classi-
cally nonoliguric, which may aid in the diagnosis.
Gl omerul onephri t i s
Acute glomerulonephritis as a cause of ARF is rarely
subtle. Urinary findings including prominent moderate to
severe proteinuria (nephrotic category), hemoglobinuria,
erythrocytes, leukocytes, and erythrocyte casts with dys-
morphic erythrocytes (nephritic category) are character-
istic features. Often, constitutional signs and symptoms,
specifically an influenza-like syndrome, are noted. Fre-
quently, urine is smoky in color, and a rash accompanies
many syndromes of glomerulonephritis.
Acute glomerulonephritis often accompanies systemic
disorders such as lupus, hepatitis, vasculitis, and pulmo-
nary renal syndromes. Serologic assays (notably lupus se-
rologies, antineutrophil cytoplasmic antibodies, and
complement levels) and immunopathologic examination of
the kidneys will identify most causes of rapidly progressive
glomerulonephritis. Recognition of this syndrome is ex-
tremely important because it is often reversible with immu-
nosuppressive therapy.
Tubul ar Di sorders
The most common cause of hospital-acquired ARF is
ATN. As previously mentioned, prerenal azotemia and
ischemic ATN represent a continuum. Multiple pathways
and clinical conditions lead to renal ischemia. Numerous
factors commonly contribute to the occurrence of ischemic
ATN.
Dramatic advances were made recently in the under-
standing of the cellular mechanisms involved in glomerular
and renal tubular cell damage and death, interstitial fibro-
genesis, and apoptosis. Increased cytosolic calcium levels,
decreased adenosine triphosphate levels, derangements in
cytoskeletal functions, increased intracellular phospholi-
pase levels, increased generation of apoptotic signals, and
increased levels of intracellular reactive oxygen species
have all been experimentally well documented to contrib-
ute to ARF due to ATN.
1,11
Patients at risk for ATN include those with prolonged
systemic hypotension and those with decreased effec-
tive renal perfusion for prolonged periods. Additionally,
multiple medications and toxins may induce tubular dam-
age. Aminoglycoside antibiotics, cisplatin, cyclosporine,
tacrolimus, mannitol, amphotericin B, methotrexate,
foscarnet, pentamidine, organic solvents, heavy metals, co-
caine, intravenous immunoglobulin, and radiocontrast
agents are often implicated in tubular dysfunction and
damage. Intrinsic toxins such as heme pigments (as in
rhabdomyolysis), myeloma light chain proteins, and uric
acid crystals frequently cause tubular obstruction and
damage.
Rhabdomyolysis induced by combination antihyper-
lipidemic therapy or by antihyperlipidemic therapy in com-
bination with immunosuppressive agents (especially cal-
cineurin inhibitors) has been recognized. Additionally, the
epidemic of cocaine use has caused an increase in the
incidence of cocaine-induced rhabdomyolysis. Clinical
hallmarks of rhabdomyolysis are often present in patients
with ARF and include muscle tenderness, signs of extrem-
ity compartment syndrome, and characteristic elevation in
serum creatine kinase and urinary myoglobin levels.
ARF IN THE RENAL TRANSPLANT RECIPIENT
The assessment of patients with ARF who have a renal
allograft does not differ from that for the general popula-
tion. Serum, urine, and radiographic studies are indicated.
Therapeutic levels of immunosuppressive agents should be
determined at the trough period.
Obstructive uropathy due to trauma, ureteral stenosis, or
compression by lymphocoel is often seen; therefore, ul-
trasonography is a necessary first step in the evaluation.
Doppler flow studies of the transplants vascular supply are
easily performed because of the position of the graft.
The diagnosis and management of prerenal causes are
complicated by the known vasoconstrictive effects of the
calcineurin inhibitors (cyclosporine, tacrolimus), which are
often injurious in situations of volume depletion. Close
attention to possible drug-drug interactions, which may
potentiate calcineurin toxicity by inhibition of hepatic
metabolic pathway, is extremely important.
Rejection of the transplant is one of the renal parenchy-
mal causes of ARF. Again, a review of the medication
history to determine whether induction of the hepatic meta-
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
Acute Renal Failure Mayo Clin Proc, January 2001, Vol 76 72
bolic pathways has been stimulated by pharmacologic
agents (thereby decreasing immunosuppressive agent lev-
els) is necessary, as is an assessment of compliance with
the medication regimen. Transplant biopsy is frequently
performed to determine presence and/or extent of the rejec-
tion process.
THERAPY
The goal of any focused evaluation of ARF is immediate
correction of its reversible causes. Recognition and re-
lief of urinary outlet obstruction should be given the
highest priority, especially for patients with anuria.
Support of renal perfusion with either volume infusion
or therapeutics that improve renal oxygen delivery should
be considered before any attempt to improve urinary
flow. Urinary indices should be examined before diuretic
intervention.
Therapy to correct the pathophysiologic derangements
of ARF can be broadly categorized into nondialytic and
dialytic.
Nondi al yt i c Therapy
Paramount in the initial treatment of ARF is ensuring
that renal perfusion is maximized by volume infusion and/
or correction of the underlying pathophysiologic process
that has caused ARF. Additionally, a recent growth in the
understanding of the molecular biology of ARF has led to
several clinically based targeted therapeutic trials.
Growth Factors.As the most common cause of hos-
pital-acquired ARF is ATN, prompt recovery from ATN
requires tubular cell regeneration. Multiple animal studies
have shown promise in stimulating regrowth of the is-
chemic injured tubular cells by growth factors such as
insulin-like growth factor, hepatocyte growth factor, and
transforming growth factor . However, thus far, human
trials have been disappointing in their ability to document
any pronounced change in the course of ARF with directed
therapy with insulin-like growth factor or hepatocyte
growth factor.
Atrial Natriuretic Peptide.Atrial natriuretic peptide
has been shown in small studies to improve urinary flow.
Animal trials have suggested that, because of the vaso-
dilatory activities of atrial natriuretic peptides, the severity
of ARF may be attenuated with their use. However, a
recent randomized controlled multicenter trial of atrial
natriuretic peptide in oliguric ARF failed to show any
benefit with this agent.
12
Intracellular Adhesion Molecules.Recently, it was
well documented that intracellular adhesion molecules have
an essential role in leukocyte adhesion, rolling, and diape-
desis in the ongoing injury model. Inhibition of intracellular
adhesion molecules is the subject of current animal studies.
Antioxidant Therapy.Several indirect and direct
lines of evidence suggest that free oxygen radical dam-
age is a prominent etiologic factor in ongoing renal
parenchymal damage. Whether up-regulation of intrinsic
cellular protective antioxidant mechanisms may be stimu-
lated by previous ischemic insults and whether supple-
mentation of antioxidant compounds affords protection
from ARF are intriguing hypotheses. Studies of several
antioxidant compounds are currently under way to assess
their ability to decrease the severity and length of injury in
ARF.
Dopamine.Traditionally, dopamine has been a main-
stay of the therapeutic armamentarium in all patients with
ARF. This is primarily due to its putative ability to vaso-
dilate splanchnic vasculature selectively at renal doses
(1-3 gkg
1
min
1
). While dopamine has certainly been
proved in humans to be natriuretic and phosphaturic, no
evidence shows, despite many clinical trials, that dopamine
favorably affects the course of ARF.
13
Diuretics.In many clinical settings, there is little evi-
dence that use of diuretics to change a patients condi-
tion from oliguric to nonoliguric renal failure has any ef-
fect on clinical outcome. Use of diuretics for patients
with ARF complicated by volume overload or for patients
who need intravascular space for therapeutic parenteral
medications is certainly warranted. However, their use
specifically to affect the course and outcome of ARF has
not been shown to be advantageous. Therefore, diuretics
should be considered only after renal perfusion has been
maximized.
Certain clinical situations may warrant the use of di-
uretics early in the course of renal failure, such as in
volume-replete patients with endogenous heme pigment
injury; forced diuresis in the setting of renally excreted
toxins such as lithium, theophylline, and salicylates and
toxic alcohol ingestions; or in patients with tumor lysis
syndrome.
Adjuvant Measures.A nutrition program with an
energy prescription of 126 to 147 kJ/kg per day and re-
striction of potassium (60 mEq/d), sodium (90 mEq/d),
and phosphorus (800 mg/d) should be recommended for
most patients with ARF. Protein supplementation of 0.6
to 1.4 g/kg per day is required for most patients with
hospital-acquired ARF to minimize protein catabolism, de-
pending on whether dialysis is required. Severe protein
restriction, prescribed to avoid dialysis, is controversial at
best. A patients current medical regimen, especially medi-
cation doses, should be adjusted to their residual renal
function, and patients should be told to avoid further poten-
tial nephrotoxins.
Agents whose renally excreted metabolites may become
toxic must be closely monitored. Meperidines metabolite
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
Mayo Clin Proc, January 2001, Vol 76 Acute Renal Failure 73
normeperidine accumulates in ARF and has been linked to
seizure activity, as has the antibiotic imipenem. Digoxin
should be administered cautiously with close attention to
serum levels, as with nitroprusside and its metabolites.
NSAIDs should be avoided in the setting of ARF be-
cause of their previously described adverse effects on renal
perfusion.
Life-threatening hyperkalemia may complicate ARF.
Urgent measures to stabilize cardiac cellular membrane
repolarization with intravenous calcium gluconate or chlo-
ride for patients with electrocardiographic changes should
be the first priority. Until removal of potassium is possible,
induction of intracellular shifting of potassium is the next
priority. These shifts can be facilitated by intravenous insu-
lin and dextrose administration, as well as -agonist
therapy. However, the required dose of -agonist to effect
transcellular potassium shifting is about 10 to 20 times the
usual nebulized dose for reactive airway disease, and there-
fore -agonists are often impractical. Parenteral bicarbon-
ate therapy may be of use, although this has been ques-
tioned recently. Potassium removal may be achieved via
the kidneys, if oliguria is not present, with high-dose loop
diuretics. If oliguria occurs, enteric removal by administra-
tion of exchange resins (sodium polystyrene sulfonate)
may be considered. Recently, several case reports and se-
ries demonstrated colonic necrosis associated with the use
of sodium polystyrene sulfonate in critically ill and hemo-
dynamically unstable patients.
14
Therefore, many clinicians
think that sodium polystyrene sulfonate should be used
cautiously in the ICU. Hemodialysis after placement of
suitable vascular access allows rapid removal of potassium
and should be considered early in the presentation of life-
threatening hyperkalemia.
Di al ysi s
Initiation of renal replacement therapy (peritoneal dialy-
sis, intermittent hemodialysis, continuous dialysis-he-
mofiltration) has traditionally been recommended when
severe derangements in electrolyte concentrations (potas-
sium, sodium), volume overload, acid-base imbalance, pro-
nounced azotemia (blood urea nitrogen >100 mg/dL), or
florid symptoms of uremia (pericarditis, encephalopathy,
bleeding, nausea-vomiting, pruritus) are noted. Few pa-
tients with ARF are treated with peritoneal dialysis primar-
ily because of poor delivery of dialysis dose and difficulty
managing ultrafiltration. In the United States, most patients
with ARF who require renal replacement therapy are
treated with intermittent hemodialysis.
A link between the delivered dose of dialysis and out-
come has been firmly established in patients with end-stage
renal disease receiving outpatient maintenance dialysis.
Recent data have suggested a similar relationship in pa-
tients with ARF.
15,16
Furthermore, initiation of hemodialy-
sis before severe pathophysiologic derangements occur has
been suggested to benefit the patient with multiorgan fail-
ure and ARF.
17
The extracorporeal circuit obviously has an important
role in renal replacement therapies. Pivotal studies per-
formed in the mid-1990s documented improved mortality
and recovery of renal function with the use of biocom-
patible dialysis membranes.
18
Continuous renal replacement therapies likely offer
several potential benefits for critically ill patients with
ARF. These benefits are suggested by an increased he-
modynamic tolerance of dialysis, improved ability to
manage fluid and electrolyte balance, improved dialytic
dose delivery, and use of synthetic (more biocompatible)
membranes.
SUMMARY
Acute renal failure is a multisystemic disorder that affects
patients cared for by nearly all health care professionals. Its
occurrence seems to be increasing in hospitalized patients.
A structured approach to the evaluation of ARF will result
in a quick diagnosis of the cause and facilitate rapid effec-
tive therapy. The clinician should recognize the growing
list of medications and potential nephrotoxins that cause
ARF.
Although morbidity statistics remain unacceptably high
in patients with hospital-acquired ARF, ongoing efforts to
improve both dialytic and nondialytic therapies are being
explored.
REFERENCES
1. Thadhani R, Pascual M, Bonventre JV. Acute renal failure. N Engl
J Med. 1996;334:1448-1460.
2. Liano F, Pascual J, Madrid Acute Renal Failure Study Group.
Epidemiology of acute renal failure: a prospective, multicenter,
community-based study. Kidney Int. 1996;50:811-818.
3. Branch RA. Prevention of amphotericin B-induced renal impair-
ment: a review on the use of sodium supplementation. Arch Intern
Med. 1988;148:2389-2394.
4. Prentice HG, Hann IM, Herbrecht R, et al. A randomized compari-
son of liposomal versus conventional amphotericin B for the treat-
ment of pyrexia of unknown origin in neutropenic patients. Br J
Haematol. 1997;98:711-718.
5. Yoshioka T, Fogo A, Beckman JK. Reduced activity of antioxidant
enzymes underlies contrast media-induced renal injury in volume
depletion. Kidney Int. 1992;41:1008-1015.
6. Tepel M, van der Giet M, Schwarzfeld C, Laufer U, Liermann D,
Zidek W. Prevention of radiographic-contrast-agent-induced re-
ductions in renal function by acetylcysteine. N Engl J Med. 2000;
343:180-184.
7. Nzerue CM, Hewan-Lowe K, Riley LJ Jr. Cocaine and the kidney:
a synthesis of pathophysiologic and clinical perspectives. Am J
Kidney Dis. 2000;35:783-795.
8. Maillet PJ, Pelle-Francoz D, Laville M, Gay F, Pinet A. Nondilated
obstructive acute renal failure: diagnostic procedures and therapeu-
tic management. Radiology. 1986;160:659-662.
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
Acute Renal Failure Mayo Clin Proc, January 2001, Vol 76 74
9. Abuelo JG. Diagnosing vascular causes of renal failure [published
correction appears in Ann Intern Med. 1995;124(1, pt 1):78]. Ann
Intern Med. 1995;123:601-614.
10. Vanherweghem JL, Abramowicz D, Tielemans C, Depierreux M.
Effects of steroids on the progression of renal failure in chronic
interstitial renal fibrosis: a pilot study in Chinese herbs nephropa-
thy. Am J Kidney Dis. 1996;27:209-215.
11. Wagener OE, Lieske JC, Toback FG. Molecular and cell biology of
acute renal failure: new therapeutic strategies. New Horiz. 1995;3:
634-649.
12. Lewis J, Salem MM, Chertow GM, et al, Anaritide Acute Renal
Failure Study Group. Atrial natriuretic factor in oliguric acute renal
failure. Am J Kidney Dis. 2000;36:767-774.
13. Szerlip HM. Renal-dose dopamine: fact and fiction [editorial]. Ann
Intern Med. 1991;115:153-154.
14. Scott TR, Graham SM, Schweitzer EJ, Bartlett ST. Colonic necro-
sis following sodium polystyrene sulfonate (Kayexalate)-sorbitol
enema in a renal transplant patient: report of a case and review of
the literature. Dis Colon Rectum. 1993;36:607-609.
15. Paganini EP, Tapolyai M, Goormastic M, et al. Establishing a
dialysis therapy/patient outcome link in intensive care unit: acute
dialysis for patients with acute renal failure. Am J Kidney Dis.
1996;28(5, suppl 3):S81-S89.
16. Ronco C, Bellomo R, Homel D, et al. Effects of different doses in
continuous veno-venous haemofiltration on outcomes of acute re-
nal failure: a prospective randomised trial. Lancet. 2000;356:26-30.
17. DuBose TD Jr, Warnock DG, Mehta RL, et al. Acute renal failure
in the 21st century: recommendations for management and out-
comes assessment. Am J Kidney Dis. 1997;29:793-799.
18. Hakim RM, Wingard RL, Parker RA. Effect of the dialysis mem-
brane in the treatment of patients with acute renal failure. N Engl J
Med. 1994;331:1338-1342.
Questions About ARF
1. Which one of the following would not be associated
with an elevated serum creatinine level, which may
not reflect a decline in renal function?
a. Hypovolemia
b. Elevated serum ketone levels
c. Administration of select types of cephalosporin
antibiotics
d. Elevated serum creatine kinase levels
e. Administration of cimetidine
2. Which one of the following is not an indication for
urgent dialysis therapy?
a. Pericarditis associated with severe azotemia
b. Hyperkalemia
c. Oliguria
d. Volume overload (congestive heart failure)
e. Nausea, vomiting, mental status changes, and
bleeding associated with severe azotemia
3. Which one of the following urinary findings is
inconsistent with intrinsic renal causes of ARF?
a. Dysmorphic erythrocytes, erythrocyte casts
b. Fractional excretion of sodium, 0.58%
c. Fractional excretion of sodium, 5.8%
d. Urinary creatinine-plasma creatinine ratio, 15:1
e. Dark granular muddy brown casts
4. Which one of the following medications does not
cause a functional decrease in renal perfusion?
a. NSAIDs
b. Cyclosporine
c. Cocaine
d. Cisplatin
e. ACE inhibitors
5. Which one of the following strategies has been shown
in human clinical trials to prevent or ameliorate
ARF?
a. Dopamine at renal dose (1-4 gkg
1
min
1
)
b. Infusion of atrial natriuretic peptide
c. Infusion of saline before radiographic contrast
exposure (1 mLkg
1
min
1
12 hours before)
d. High-dose intravenous loop diuretics
e. Infusion of insulin-like growth factor
Correct answers:
1. a, 2. c, 3. b, 4. d, 5. c
For personal use. Mass reproduce only with permission from Mayo Clinic Proceedings.
Você também pode gostar
- Common Medical AbbreviationsDocumento4 páginasCommon Medical AbbreviationsJustine DicksonAinda não há avaliações
- Diabetes TeluguDocumento31 páginasDiabetes TeluguRamesh100% (1)
- Usmle World Ed ObjectiveDocumento16 páginasUsmle World Ed ObjectiveNisarg Patel100% (3)
- CCRN-PCCN Review RenalDocumento11 páginasCCRN-PCCN Review RenalGiovanni MictilAinda não há avaliações
- Acute Nephrology For The Critical Care Physician PDFDocumento280 páginasAcute Nephrology For The Critical Care Physician PDFMahtosurup GodavarthyAinda não há avaliações
- Acute Renal FailureDocumento4 páginasAcute Renal FailurePerrilyn PereyAinda não há avaliações
- Hepatorenal Syndrome: Causes, Tests, and Treatment OptionsNo EverandHepatorenal Syndrome: Causes, Tests, and Treatment OptionsNota: 4.5 de 5 estrelas4.5/5 (2)
- Marking of PACESDocumento2 páginasMarking of PACESRohitKumarAinda não há avaliações
- Acute Renal FailureDocumento17 páginasAcute Renal FailureDina Rasmita100% (1)
- Acute Kidney Injury: Causes, Stages, and ManagementDocumento62 páginasAcute Kidney Injury: Causes, Stages, and ManagementApidha KartinasariAinda não há avaliações
- cc4 PDFDocumento280 páginascc4 PDFSid DhayriAinda não há avaliações
- Vital Nephrology - $86.04Documento106 páginasVital Nephrology - $86.04Abdallah Bouleghraif100% (1)
- Acute Liver Failure Pathophysiologic Basis and The Current and Emerging TherapiesDocumento9 páginasAcute Liver Failure Pathophysiologic Basis and The Current and Emerging TherapiesIonut GrozavAinda não há avaliações
- Acute Renal FailureDocumento6 páginasAcute Renal Failurearif kurnia timurAinda não há avaliações
- Common Cases PacesDocumento3 páginasCommon Cases PacesRohitKumarAinda não há avaliações
- Acute Kidney InjuryDocumento8 páginasAcute Kidney InjuryRohitKumarAinda não há avaliações
- The Hepatorenal SyndromeDocumento26 páginasThe Hepatorenal SyndromeWaraBawanaAinda não há avaliações
- Acute Renal Failure in The Hospital: Diagnosis and ManagementDocumento8 páginasAcute Renal Failure in The Hospital: Diagnosis and ManagementJulio César Valdivieso AguirreAinda não há avaliações
- Coursematerial 136Documento13 páginasCoursematerial 136Nyj QuiñoAinda não há avaliações
- Acute Renal FailureDocumento18 páginasAcute Renal FailureMar DavidAinda não há avaliações
- Perioperative Care of The Patient With Renal FailureDocumento17 páginasPerioperative Care of The Patient With Renal FailureWhempyGawenAinda não há avaliações
- Step-By-Step Diagnostic Approach: History in Pre-Renal FailureDocumento4 páginasStep-By-Step Diagnostic Approach: History in Pre-Renal FailurewiggmanAinda não há avaliações
- Acute Renal Failure DXDocumento7 páginasAcute Renal Failure DXfarid akbarAinda não há avaliações
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsDocumento5 páginasEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriAinda não há avaliações
- Acute Renal FailureDocumento33 páginasAcute Renal FailureAqsa Akbar AliAinda não há avaliações
- Changes in Urine Volume and Serum Albumin in Incident Hemodialysis PatientsDocumento12 páginasChanges in Urine Volume and Serum Albumin in Incident Hemodialysis Patientsmelda lestari haidirAinda não há avaliações
- KIDNEY INJURY AND ACUTE RENAL FAILUREDocumento36 páginasKIDNEY INJURY AND ACUTE RENAL FAILUREMahfira AmaliaAinda não há avaliações
- Overview of Management of Acute Renal Failure andDocumento6 páginasOverview of Management of Acute Renal Failure andParhimpunan NasutionAinda não há avaliações
- Management: DiagnosisDocumento6 páginasManagement: DiagnosisAhmed El-MalkyAinda não há avaliações
- ARF in ElderlyDocumento7 páginasARF in ElderlySathya MoorthyAinda não há avaliações
- Science in medicine: Acute renal failure definitions and diagnosisDocumento10 páginasScience in medicine: Acute renal failure definitions and diagnosisSabila RosyidaAinda não há avaliações
- San Pedro College: A Case Study inDocumento15 páginasSan Pedro College: A Case Study inKyla ValenciaAinda não há avaliações
- Management of Oral and Maxillofacial Surgery Patients With End-Stage Renal DiseaseDocumento6 páginasManagement of Oral and Maxillofacial Surgery Patients With End-Stage Renal Diseasemehak malhotraAinda não há avaliações
- Ascitesandhepatorenal Syndrome: Danielle Adebayo,, Shuet Fong Neong,, Florence WongDocumento24 páginasAscitesandhepatorenal Syndrome: Danielle Adebayo,, Shuet Fong Neong,, Florence WongHernan GonzalezAinda não há avaliações
- Azotemia - StatPearls - NCBI BookshelfDocumento1 páginaAzotemia - StatPearls - NCBI Bookshelfmellinda anastasyaAinda não há avaliações
- Aki PDFDocumento18 páginasAki PDFFeyAinda não há avaliações
- Antiphospholipid Syndrome Nephropathy in Patients With Systemic Lupus Erythematosus and Antiphospholipid AntibodiesDocumento11 páginasAntiphospholipid Syndrome Nephropathy in Patients With Systemic Lupus Erythematosus and Antiphospholipid AntibodiesdhineyAinda não há avaliações
- AcuterenalfailureDocumento3 páginasAcuterenalfailureJessica JacksonAinda não há avaliações
- Acute Renal FailureDocumento29 páginasAcute Renal Failurelianrose448Ainda não há avaliações
- Renal Failure, Acute (Acute Kidney Injury) : Selected ReferencesDocumento10 páginasRenal Failure, Acute (Acute Kidney Injury) : Selected ReferencesputriarumAinda não há avaliações
- Acute Renal FailureDocumento12 páginasAcute Renal FailureRifa Aprillia CahyaniAinda não há avaliações
- Acute Renal FailureDocumento14 páginasAcute Renal FailureBianca EmanuellaAinda não há avaliações
- Acute Renal Failure in The ICU PulmCritDocumento27 páginasAcute Renal Failure in The ICU PulmCritchadchimaAinda não há avaliações
- CAC - Manejo Perioperatorio Del Paciente Con Falla RenalDocumento23 páginasCAC - Manejo Perioperatorio Del Paciente Con Falla RenalKarinita Campoverde SalasAinda não há avaliações
- Ascitis PDFDocumento17 páginasAscitis PDFLeonardo MagónAinda não há avaliações
- Acute Kidney InjuryDocumento2 páginasAcute Kidney InjuryMariel GamaloAinda não há avaliações
- Acute Renal Failure/ Gagal Ginjal Akut: Tunggul Adi P., M.SC., Apt. Lab Farmasi Klinik, Farmasi, FKIK, UNSOEDDocumento27 páginasAcute Renal Failure/ Gagal Ginjal Akut: Tunggul Adi P., M.SC., Apt. Lab Farmasi Klinik, Farmasi, FKIK, UNSOEDPramita Purbandari100% (1)
- Aki 6Documento12 páginasAki 6WindaAinda não há avaliações
- ANT 2 S20.fullDocumento13 páginasANT 2 S20.fulllguerreroAinda não há avaliações
- Diagnosis and Management of Hyponatremia in Acute Illness PDFDocumento13 páginasDiagnosis and Management of Hyponatremia in Acute Illness PDFMihaela MocanAinda não há avaliações
- Current Concepts: Cute LiguriaDocumento5 páginasCurrent Concepts: Cute Liguriakate blackAinda não há avaliações
- Aasld 2021 Ascite, Pbe e SHR PDFDocumento77 páginasAasld 2021 Ascite, Pbe e SHR PDFAna ClaudiaAinda não há avaliações
- Version of Record Doi: 10.1002/HEP.31884Documento84 páginasVersion of Record Doi: 10.1002/HEP.31884Thien Nhan MaiAinda não há avaliações
- Acute Renal Failure: Definitions, Diagnosis, Pathogenesis, and TherapyDocumento11 páginasAcute Renal Failure: Definitions, Diagnosis, Pathogenesis, and TherapyLuis Hernán Guerrero LoaizaAinda não há avaliações
- Sepsis y El Riñon CCC 2005Documento12 páginasSepsis y El Riñon CCC 2005Distribuidora IntegralAinda não há avaliações
- Some Clinical Features Liver Cell Failure: Appraisal: of of TheirDocumento6 páginasSome Clinical Features Liver Cell Failure: Appraisal: of of TheirSyAinda não há avaliações
- Renal Failure: Prepare by Mohammed Sahman Basees Alsharari - 391110030Documento31 páginasRenal Failure: Prepare by Mohammed Sahman Basees Alsharari - 391110030jsksAinda não há avaliações
- 2852-12054-3-PBDocumento4 páginas2852-12054-3-PBdewiAinda não há avaliações
- MINI ReviewDocumento10 páginasMINI ReviewShamila KaruthuAinda não há avaliações
- Renal IndicesDocumento6 páginasRenal IndicesSaravanan SridharanAinda não há avaliações
- Renalparenchymal hypertension causes and diagnosisDocumento4 páginasRenalparenchymal hypertension causes and diagnosisSanduni WickramaratneAinda não há avaliações
- Acute Vs Chronic Renal FailureDocumento7 páginasAcute Vs Chronic Renal FailurePellan Rhey CapuyanAinda não há avaliações
- Anesthetic Concerns in Renal FailureDocumento16 páginasAnesthetic Concerns in Renal FailureEdwin Gustavo Sandoval TorresAinda não há avaliações
- Acute Renal FailureDocumento15 páginasAcute Renal FailureFilip DadićAinda não há avaliações
- American College of Radiology ACR Appropriateness CriteriaDocumento12 páginasAmerican College of Radiology ACR Appropriateness CriteriasaidyanzAinda não há avaliações
- Managing Acute Liver Failure in Critical Care: A Structured ApproachDocumento9 páginasManaging Acute Liver Failure in Critical Care: A Structured ApproachMahen BoralessaAinda não há avaliações
- Acute: Renal Failure Management in The NeonateDocumento8 páginasAcute: Renal Failure Management in The NeonatejahangirealamAinda não há avaliações
- Ascites: Phillip S. Ge, MD, Carlos Guarner, MD, PHD, and Bruce A. Runyon, MDDocumento12 páginasAscites: Phillip S. Ge, MD, Carlos Guarner, MD, PHD, and Bruce A. Runyon, MDTere DelgadoAinda não há avaliações
- 1271 HSP .FullDocumento8 páginas1271 HSP .FulldonkeyendutAinda não há avaliações
- Diagnostic Pathology of Hematopoietic Disorders of Spleen and LiverNo EverandDiagnostic Pathology of Hematopoietic Disorders of Spleen and LiverAinda não há avaliações
- WWW - Healthcare.gov/sbc-Glossary: Important Questions Answers Why This MattersDocumento10 páginasWWW - Healthcare.gov/sbc-Glossary: Important Questions Answers Why This MattersRohitKumarAinda não há avaliações
- Cardiogenic ShockDocumento9 páginasCardiogenic ShockRohitKumar100% (1)
- Guide To Resumes & Curricula VitaeDocumento18 páginasGuide To Resumes & Curricula VitaeRohitKumarAinda não há avaliações
- McCombe Et Al. Brain 1987 (CIDP)Documento14 páginasMcCombe Et Al. Brain 1987 (CIDP)RohitKumarAinda não há avaliações
- Terapi AntiretroviralDocumento13 páginasTerapi AntiretroviralthiamuthiaAinda não há avaliações
- Case of Temporal Arteritis...Documento14 páginasCase of Temporal Arteritis...RohitKumarAinda não há avaliações
- History Taking and Physical Exam Checklist: Introduction To Clinical Medicine IIDocumento16 páginasHistory Taking and Physical Exam Checklist: Introduction To Clinical Medicine IIYukiMaedaAinda não há avaliações
- LymphadenopathyDocumento4 páginasLymphadenopathyRohitKumarAinda não há avaliações
- Epilepsy and SeizuresDocumento37 páginasEpilepsy and SeizuresRohitKumarAinda não há avaliações
- Infectious Diseases Consultation ReportDocumento5 páginasInfectious Diseases Consultation ReportRohitKumar100% (1)
- Cardiogenic ShockDocumento9 páginasCardiogenic ShockRohitKumar100% (1)
- Bronchial AsthmaDocumento28 páginasBronchial AsthmaRohitKumarAinda não há avaliações
- ART guidelines for HIV-Infected Adults and AdolescentsDocumento122 páginasART guidelines for HIV-Infected Adults and AdolescentsRohitKumarAinda não há avaliações
- Dengue JournalDocumento4 páginasDengue JournalRohitKumarAinda não há avaliações
- ReproductiveDocumento45 páginasReproductiveRohitKumarAinda não há avaliações
- Nejm Journal Alcoholic HepatitisDocumento10 páginasNejm Journal Alcoholic HepatitisRohitKumarAinda não há avaliações
- Emergency Medicine Residents Perception About Patient Safety CultureDocumento4 páginasEmergency Medicine Residents Perception About Patient Safety CultureRohitKumarAinda não há avaliações
- Patient Satisfaction - ACEPDocumento8 páginasPatient Satisfaction - ACEPRohitKumarAinda não há avaliações
- ACG Guideline AcutePancreatitis September 2013Documento16 páginasACG Guideline AcutePancreatitis September 2013gorditomaloAinda não há avaliações
- HematologyDocumento119 páginasHematologyRohitKumarAinda não há avaliações
- Curs IRA 2021Documento114 páginasCurs IRA 2021plaiul mioriticAinda não há avaliações
- Acute Kidney InjuryDocumento3 páginasAcute Kidney InjuryHarkirat AtwalAinda não há avaliações
- Nej Mo A 2310307Documento11 páginasNej Mo A 2310307Víctor C. ValverdeAinda não há avaliações
- Medicine Admitting Conference: University of Santo Tomas Faculty of Medicine and SurgeryDocumento70 páginasMedicine Admitting Conference: University of Santo Tomas Faculty of Medicine and SurgerySTEPHANIE TANAinda não há avaliações
- Acute Renal Failure Comprehensive Case AnalysisDocumento7 páginasAcute Renal Failure Comprehensive Case Analysisate NarsAinda não há avaliações
- HFHS CKD V6Documento76 páginasHFHS CKD V6medicalAinda não há avaliações
- Renal MedsurgDocumento14 páginasRenal MedsurgCliff Lois ╭∩╮⎷⎛⎝⎲⏝⏝⎲⎠⎷⎛╭∩╮ Ouano100% (1)
- QuesDocumento26 páginasQuesJoyce LauAinda não há avaliações
- NC Fauzi ERIADocumento21 páginasNC Fauzi ERIADodi DiAinda não há avaliações
- Brown 2020Documento21 páginasBrown 2020dega230989Ainda não há avaliações
- Nursing Care Plan 1Documento20 páginasNursing Care Plan 1Mary Beth Smyrl Stalnaker100% (1)
- Clinical Chemistry Lecture NPNDocumento5 páginasClinical Chemistry Lecture NPNmizunoAinda não há avaliações
- 664717ku PDFDocumento19 páginas664717ku PDFShankar Sex boyAinda não há avaliações
- Journal of Critical Care: Clinical PotpourriDocumento9 páginasJournal of Critical Care: Clinical PotpourriMas koAinda não há avaliações
- Apport de Lhemodialyse Dans Linsuffisance Renale Aigue Obstructive: Benefices Et RisquesDocumento8 páginasApport de Lhemodialyse Dans Linsuffisance Renale Aigue Obstructive: Benefices Et RisquesIJAR JOURNALAinda não há avaliações
- Renal Failure in ChildrenDocumento43 páginasRenal Failure in Childrendennyyy175Ainda não há avaliações
- IV Fluid Therapy in Adults: National Clinical Guideline CentreDocumento270 páginasIV Fluid Therapy in Adults: National Clinical Guideline CentreYanti YantiAinda não há avaliações
- MS Kidney DisDocumento10 páginasMS Kidney DisMartin T Manuel100% (1)
- 1.acute Kidney InjuryDocumento3 páginas1.acute Kidney InjuryIan CruzAinda não há avaliações
- Urea Nitrogen (BUN) Test GuideDocumento2 páginasUrea Nitrogen (BUN) Test GuideMarianAinda não há avaliações
- Acute Kidney Injury: Sarah Abigail C. Ong Siu Second Year ResidentDocumento41 páginasAcute Kidney Injury: Sarah Abigail C. Ong Siu Second Year ResidentSarah Ong SiuAinda não há avaliações
- Name: Aisyah Amalyah Putri NIM: 21114030Documento2 páginasName: Aisyah Amalyah Putri NIM: 21114030Dedikaka CoyAinda não há avaliações
- AKIDocumento23 páginasAKInadddAinda não há avaliações
- Aki App ContentDocumento6 páginasAki App ContentmimoAinda não há avaliações