Escolar Documentos
Profissional Documentos
Cultura Documentos
Pedia 2.1a Bacterial Infections - Dra Carlos
Enviado por
Dia Dimayuga0 notas0% acharam este documento útil (0 voto)
41 visualizações4 páginaspediatrics
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentopediatrics
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
41 visualizações4 páginasPedia 2.1a Bacterial Infections - Dra Carlos
Enviado por
Dia Dimayugapediatrics
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 4
Page 1 of 4
Group 7 PR: Dia
2014-2015
Dra. Carlos | Date July 25 2014
Pediatrics II
2.1 Bacterial Infections
1st
2014 PEDIATRIC INFECTIOUS DISEASES HIGHLIGHTS
A. Plague
Caused by gram negative coccobacillus Yersinia pestis
Usually through bite of an infected rodent flea
Less common exposures include handling of infected animal
tissues, inhalation of infectious droplets from infected
animals and direct contact
Endemic in rural areas in central and southern Africa, central
Asia and the Indian subcontinent, the northeastern part of
South America, and parts of the southwestern United States.
Best known for the Black Death which killed millions in
Europe during the Middle Ages
July 2014 Yumen, China 30,000 people locked down and
151 placed in quarantine after the death of a 38 year old
victim
Incubation period: 1-6 days. S/Sx of 3 clinical presentations:
Bubonic (most common) rapid onset of fever; bubo (rapid
onset, extremely tender, swollen painful lymph gland)
usually inguinal
Pneumonic (most serious) high fever, pneumonia, bloody
sputum, chills
Septicemic fever, prostration, hemorrhage,
thrombocytopenia, acral gangrene
Y. pestis can be isolated from bubo aspirates, blood cultures,
or sputum culture if pneumonic. With Waysons stain:
bipolar safety pin appearance. Serologic test: F1 antigen.
1
st
line treatment: Parenteral Streptomycin
Alternate: IV Gentamicin; Oral Doxycycline
Typical Scenario
A 17 year old boy who has been camping in Africa complains of fever and swelling in
his groin area. PE shows an enlarged, tender inguinal lymph node and signs of flea
bites on his legs and feet. There are no penile lesions or discharge. Culture of
isolates reveals growing gram-negative rods with a safety pin appearance.
B. MERS-CoV (Middle East Respiratory Syndrome Corona Virus)
Caused by coronavirus called MERS-CoV
Spread by close person-to-person contact
Transmitted by respiratory droplet spread, fomites with
droplets and airborne spread
Incubation period: 2-14 days. S/Sx: viral prodrome - high
fever, chills, headache, feeling of discomfort and body aches
which progresses to severe acure respiratory illness - dry
nonproductive cough, shortness of breath, hypoxia
2
nd
most common cause of respiratory viral infections, next
to rhinovirus
First identified in the Arabian Peninsula from a 60 year old
man who died of severe pneumonia and renal failure
Have been found in camels
Proposed explanation: increased mixing between different
animal species and humans, climate change, intense
international travel, expansion of the immune suppressed
population, and changes in the virus itself to adapt to other
species.
PCR tests with respiratory samples and serology testing
using blood samples is used for identification of MERS-CoV
No specific antiviral treatment
No vaccine to prevent infection
Typical Scenario
A patient develops fever, cough and shortness of breath within 14 days of being in
Saudi Arabia.
C. Vaccine Preventable Diseases
Measles
Goal: eradication. At 9 mos, the cohort is set at 95%. At 15
mos, cohort for MMR is also set at 95%. The Philippines is
only at 88% leaving a 7% gap in our population.
Routine immunization of measles is at 9 mos. Vaccine
efficacy at 6 mos is 50%, at 9 mos is 85 % while at 1 year old
is 95 %. However, we cannot delay giving the vaccine at 1
year old because the attack rate of the measles virus is
higher when the child is less than a year old.
Pneumonia complication of measles which is the most
common cause of death in young children
Subacute Sclerosing Panencephalitis (SSPE) rare
postinfectious neurologic complication of measles
characterized by regressive changes in intellect and
personality. Within months, psychologic symptoms are
compounded by neurologic ones myoclonic jerks, mental
and motor deterioration culminating in extreme neurologic
dysfunction and death.
Pertussis
No pertussis-only vaccine is available. It is available as DTaP.
Waning immunity - getting sick with pertussis or getting
pertussis vaccines doesn't provide lifelong protection
Booster: DTaP
Poliomyelitis
Philippines is a Polio-free country but an evidence below
10% is needed to maintain our polio free status.
Regular submission of 2 stool samples with an interval of
2 weeks after the onset for all patients ages 0-15 years old
who present with weakness, regardless of the cause.
LEADING CAUSE OF MORTALITY WORLDWIDE UNDER 5
YEARS OLD
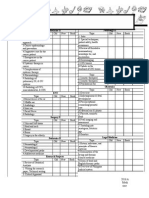
Figure 1. Distribution of causes of mortality in childern under 5yo.
Under 5 years old Mortality (infant and neonatal) is a good
indicator of the health system of the country.
Infant and neonatal mortalities are the most numerous and
major cause of mortalities. These are tied up with maternal
health.
Pneumonia is the major cause of deaths globally which is
vaccine preventable.
By 2015, the Millennium Developmental Goal 4 is to reduce
Under 5 Mortality to 18,000. According to the National
Statistical Board, the Philippines is on track from the
baseline of 57,000 (1990) to 25,000 (2008). However, MDG
has been extended to 2020.
Page 2 of 4
SUBJECT Lec#
LEADING CAUSES OF VACCINE PREVENTABLE DISEASES
WORLDWIDE (2004)
1. Pneumococcal diseases
2. Diarrhea (rotavirus)
3. Measles
4. Haemophilus influenza type B
5. Pertussis
6. Tetanus (neonatal and non-neonatal)
13 Filipino children die every year due to diarrhea
TOP 10 CAUSES OF DEATHS IN THE PHILIPPINES FOR ALL
AGE GROUPS (2009)
1. Diseases of the heart
2. Cerebro-vascular diseases
3. Malignant neoplasm
4. Pneumonia
5. Tuberculosis
6. COPD
7. Diabetes
8. Nephritis/Nephrotic syndrome
9. Assault
10. Perinatal conditions
Pneumonia and tuberculosis are the top infections that can
cause death. The rest are secondary to lifestyle.
TOP 10 CAUSES OF ILLNESSES IN THE PHILIPPINES FOR
ALL AGE GROUPS (2010)
1. ACUTE RESPIRATORY INFECTION
2. ACUTE LOWER RESPIRATORY INFECTION AND PNEUMONIA
3. BRONCHITIS
4. Hypertension
5. ACUTE WATERY DIARRHEA
6. INFLUENZA
7. UTI
8. TB
9. Accidents
10. Injuries
7 out of 10 are caused by infectious diseases.
S. pnemoniae is your gram (+) diplococci with a very thick
capsule and this is the one that renders the organism
virulent. Its thick capsule resists phagocytosis.
IMCI GENERAL DANGER SIGNS
IMCI = Integrated Management of Childhood Illnesses
1. Is the child able to feed, drink or breastfeed?
2. Does the child vomit everything?
3. Does the child have convulsions during the present illness or has
convulsions now?
4. Is the child lethargic or unconscious?
A child with a general danger sign has a serious problem.
URGENT referral to a hospital!!!
Upon initial meeting of the baby, one can already check his
demeanor and ability to ambulate.
ASSESS MAIN SYMPTOM
Cough or difficulty of breathing - check Respiratory Rate for
a full 1 minute
Diarrhea - usually caused by enteric virus such as rotavirus
Ear problem/discharge
Undernutrition and anemia - check for pallor of conjuctiva
and palms
Convulsions - meningeal irritation, meningitis, encephalitis
Check immunization status
Assess other problems.
This is a good opportunity to remind the parents to update
immunizations and to assess for anemia and undernutrition.
When immunization targets fall short, at risk population
increases and accumulates. When someone or a few acquire
the disease, it can affect a whole lot of people causing an
outbreak.
When patients are seen in the ER, they are required to
follow up the next day at the OPD for completion of missed
out data, to chek if diagnosis was right or if the patient
needs to be admitted.
THE CHILD WITH FEVER
In children 4 weeks to 5 years, body temperature should be measured
using either:
rectal thermometer
electronic thermometer in the axilla
infrared tympanic thermometer (best > 3 months)
Fever Requiring Tests
Temp > 38C in infants < 3 months
Temp 39C in infants > 3 months
Fever is a very important symptom for a child.
usually admitted due to fever
common causes of absenteeism: fever, cough, diarrhea
If a patient < 3 months old comes with fever, it is considered severe.
< 3 months is near the neonatal period (some would even
say that 3 months is extended neonatal period)
neonates and patients until 3 months old have the same
pathogens.
age when etiologic agents change (remember that etiologic
agents can be based on age)
Neonates have an immature thermoregulatory center.
Even if a neonate doesnt present with fever, it doesnt
mean that he is well. There are times when the patient is
seriously ill but has no fever immune system if the patient
has not been fully developed yet.
Infants < 3 months with fever who appear generally well;
who have been previously healthy; who have no evidence of
skin, soft tissue, bone, joint, or ear infection; and who have a
total white blood cell (WBC) count of 5,000-15,000 cells/L,
an absolute band count of less than 1,500 cells/L, and
normal urinalysis results are unlikely to have a serious
bacterial infection.
Mothers tend to bring their child early but if you know the
family of the patient and you examine him from time to
time, you may opt not to require tests.
Body Temperature
regulated by thermosensitive neurons located in the
preoptic or anterior hypothalamus that respond to changes
in blood temperature as well as to direct neural connections
with cold and warm receptors located in skin and muscle.
Diurnal Circadian Temperature Rhythm lower body
temperatures in the early morning and temperatures
approximately 1C higher in the late afternoon or early
evening.
Fever
defined as rectal temperature of 38C
a controlled increase in body temperature over the normal
values
Hyperpyrexia temperature of 40 C
Fever patterns per se are NOT often helpful in determining a
specific diagnosis but observing the clinical characteristics of
fever can provide useful information.
Page 3 of 4
SUBJECT Lec#
Single isolated fever spike is not associated with an
infectious disease. May be due to the following:
infusion of blood products
drugs procedures
manipulation of a catheter on a colonized or
infected body surface
Temperatures in excess of 41C are most often associated
with a non-infectious cause. Causes of very high
temperatures (>41C) include:
central fever (CNS dysfunction)
malignant hyperthermia
malignant neuroleptic syndrome o drug fever
heat stroke
Temperatures that are lower than normal (<36C) can be
associated with:
overwhelming sepsis
cold exposure
hypothyroidism
overuse of antipyretics
SERIOUS ILLNESS RISK CLASSIFICATION
Low Intermediate High
Color Normal Pallor Pale, mottled,
ashen, blue
Activity -Responds normally
to caretakers
-Is content and
smiles
-Stays awake or
awakens quickly
when aroused -
Strong, normal cry
Decreased activity -Unresponsive,
appears ill, and
barely rousable
-Weak high pitched
or continuous cry
Breathing -Regular
-Unlabored
Signs of
respiratory
distress
-Grunting
-Severe distress
Hydration Normal -Signs of
dehydration
-Poor feeding
-Decreased urine
output
-Capillary refill
time > 3 sec
Reduced skin
turgor
Others -Well- appearing -No
fever at time of
examination
-Fever > 5 days
-Swelling of limb
or joint
-Non-weight
bearing or not
using an extremity
-A new lump >
2cm
-Non- blanching
rash
-Fever at time of
examination
-Bulging fontanelle
-Neck stiffness
-Seizures or focal
neurologic
abnormality
-Bilious vomiting
Table 1. serious illness risk classification
A. LOW RISK OF SERIOUS ILLNESS
Color: Normal color of skin, lips and tongue
Activity:
o Responds normally to caretakers
o Is content and smiles
o Stays awake or awakens quickly weh aroused
o Strong, normal cry
Breathing: Regular, unlabored
Hydration: Normal
Others: well-appearing , no fever at time of examination
Management: Home management (give water and
Paracetamol)
B. INTERMEDIATE RISK OF SERIOUS ILLNESS
Color: Pallor (reported by parents/ caregivers)
Activity: Decreased activity
Breathing: signs of respiratory distress chest retractions
(subcostal, intercostal, suprasternal), nasal flaring
Hydration:
o Signs of dehydration (sunken eyes, decreased capillary refil
time, poor skin turgor, depressed fontanelles, dry mucosa,
decreased tear production.
o Poor feeding
o Decreased urine output (Ask for LAST URINE VOIDING)
o Capillary refill > 3 seconds
Others: Fever >/= 5 days, swelling of limb or joint, non- weight
bearing or not using an extremity, a new lump >/= 2cm
If intermediate to high risk, may warrant hospital admission
C. HIGH RISK OF SERIOUS ILLNESS
Color: Pale, mottled, ashen, blue
Activity: Unresponsive, appears ill, and barely rousable; weak
high pitched or continuous cry
Breathing: Grunting, severe distress
Hydration: Reduced skin turgor
Others: Non-blanching rash (= glass tumbler test), fever at time
of examination, bulging fontanelle, neck stiffness, seizures or
focal neurologic bnormality, bilious vomiting (green from bile,
there is an obstruction prior to ampula of Vater)
Management may have to be started at the ER
FEVER MANAGEMENT
Know the causative agent!
Bacteremia would present with non-specific manifestation
(ex. fever) versus sepsis which would present with clinical
manifestations.
Dont miss possible viral exantems.
Non-blanching rash - a rash that doesnt disappear when
pressing a glass. (+) glass tumbler test.
When there is no apparent source of infection, request for:
Blood: CBC, CRP, ESR, blood culture
Urine: Urinalysis, urine culture
CSF: Analysis, culture
Chest X-ray: if with pulmonary s/sx or high WBC
Check CBC for the predominant cellular action: is it
leukocytosis predominant lymphocytes? Or is it leukocytosis
predominant neutrophilic? Is there high stabs?
Leukocytopenia? Thrombocytopenia and thrombocytosis
can both be associated with infection.
CRP (C-Reactive Protein) and ESR (Erythrocyte
Sedimentation Rate) are on-specific, acute phare reactants.
They are indicative of infection, collagen disease or
inflammation.
In UTI, presence of gram negative organisms on blood
culture can be devastating as it can be associated with
shock.
A normal urinalysis does not rule out UTI, only culture will
do.
Meningitis is an emergency in pediatrics.
During the first 3 days of life, viral infections can present
with leukocytosis (WBC up to 50,000). But after the third day
or going to the fourth day, if it is viral, the true picture will
show that WBC becomes normal or leukopenic
predominantly lymphocytic.
If its bacterial, WBC will persistently go up.
Page 4 of 4
SUBJECT Lec#
If its serious (especially gram negative infection), it can
present with leukopenia because the infection can be
inhibitory to your WBC.
Management
CBC with differential WBC count and urinalysis should be part of the
initial laboratory evaluation.
ANC < 5,000/L - evidence against indolent bacterial
infection other than typhoid fever.
PMN greater than 10,000/mL or nonsegmented PMN
leukocytes > 500/mL - high likelihood of having a severe
bacterial infection.
Direct examination of the blood smear with Giemsa or Wright stain
may reveal organisms of malaria, trypanosomiasis, babesiosis, or
relapsing fever.
Acute Phase Specific Reactants
ESR > 30mm/hr indicates inflammation and needs further
evaluation for infectious, autoimmune, or malignant
diseases.
ESR > 100 mm/hr suggests tuberculosis, Kawasaki disease,
malignancy, or autoimmune disease.
A low ESR does not eliminate the possibility of infection or
JRA.
CRP also becomes elevated and returns to normal more
rapidly than the ESR.
Aspirin has been associated with Reye syndrome in children and
adolescents, its use is not recommended for the treatment of fever.
ANTIBIOTICS FOR MANAGEMENT OF SERIOUSLY ILL
CHILDREN WITH FEVER OF UNKNOWN ORIGIN
A. Immediate Treatment
3
rd
Generation Cephalosporins (Cefotaxime or Ceftriaxone)
provides coverage for both gram (+) and gram (-) organisms
can traverse the blood brain barrier
Given to patients with:
Signs of shock or coma
Meningococcal disease
Age < 1 month
Age 1-3 months and unwell with WBC < 5 or >15 x
10 to the 9
th
/ L
On the 3
rd
to 4
th
day, one can differentiate between viral and
bacterial cause in WBC count.
B. Treatment for Suspected Bacterial Infection
3
rd
Generation Cephalosporins
Given if any of the following are suspected:
Neisseria meningitidis
Streptococcus pnemonia
E. coli
E. coli- most common cause of neonatal sepsis in the
Philippines
Pneumococcus sepsis/meningitis Case Fatality Rate is 33%
(2010)
Staphylococcus aureus infection
DOC: Methicillin
DOC for MRSA: Vancomycin
Community-acquired methicilin resistant Staphylococcus
aureus (CA-MRSA) is gaining prevalence, 58% national.
Haemophilus influenzae type B infection
DOC: Oxacillin / Vancomycin
Seldomly seen in children > 5 year old
Usually seen among 3 mos 5 years.
Neonates are at high risk for infections due to their
underdeveloped immune systems.
Bacteroides fragilis most common normal flora in the large intestine;
anaerobic
Small intestines gram (-) aerobic
Large intestines gram (-) anaerobic
Você também pode gostar
- 01 Jan IncompleteDocumento123 páginas01 Jan IncompleteDia DimayugaAinda não há avaliações
- Pharmcheatsheets PDFDocumento13 páginasPharmcheatsheets PDFDia DimayugaAinda não há avaliações
- 1 MED II 6 - Systemic Therapy in Cancer PDFDocumento14 páginas1 MED II 6 - Systemic Therapy in Cancer PDFDia DimayugaAinda não há avaliações
- Pedia 2.2b Dengue - Dra BiberaDocumento10 páginasPedia 2.2b Dengue - Dra BiberaDia DimayugaAinda não há avaliações
- 1st LE MedicineDocumento11 páginas1st LE MedicineDia DimayugaAinda não há avaliações
- 1st LE Ophthalmology (2 Files Merged)Documento16 páginas1st LE Ophthalmology (2 Files Merged)Dia DimayugaAinda não há avaliações
- 1st LE ChecklistDocumento2 páginas1st LE ChecklistDia DimayugaAinda não há avaliações
- 5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDocumento2 páginas5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDia DimayugaAinda não há avaliações
- Day 1 April 27 SundayDocumento1 páginaDay 1 April 27 SundayDia DimayugaAinda não há avaliações
- Autonomous Growth-Remote EffectsDocumento4 páginasAutonomous Growth-Remote EffectsDia DimayugaAinda não há avaliações
- Glomerular DiseasesDocumento7 páginasGlomerular DiseasesDia DimayugaAinda não há avaliações
- 5: Diarrhea and Constipation: MedicineDocumento7 páginas5: Diarrhea and Constipation: MedicineDia DimayugaAinda não há avaliações
- Pharma NotesDocumento6 páginasPharma NotesDia DimayugaAinda não há avaliações
- BallardScore ScoresheetDocumento1 páginaBallardScore ScoresheetIsabel BarradasAinda não há avaliações
- Formal Laboratory ReportDocumento2 páginasFormal Laboratory ReportDia DimayugaAinda não há avaliações
- 5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDocumento2 páginas5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDia DimayugaAinda não há avaliações
- 5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDocumento2 páginas5 PSYCH 1 - Behavioral and Psychological Reactions To Illness - Dr. SundiangDia DimayugaAinda não há avaliações
- DEFINITION AND NATURE OF SOCIOLOGY IntroDocumento2 páginasDEFINITION AND NATURE OF SOCIOLOGY IntroDia Dimayuga100% (3)
- FYI InvitationDocumento1 páginaFYI InvitationDia DimayugaAinda não há avaliações
- A Young Lasallian Is US Environmental ScholarDocumento1 páginaA Young Lasallian Is US Environmental ScholarDia DimayugaAinda não há avaliações
- Chemical Bonds - Ionic or CovalentDocumento4 páginasChemical Bonds - Ionic or CovalentDia DimayugaAinda não há avaliações
- Nubel 1997 PCR Primers To Amplify 16S rRNA Genes From CyanobacteriaDocumento6 páginasNubel 1997 PCR Primers To Amplify 16S rRNA Genes From CyanobacteriaHoballahAinda não há avaliações
- IM WW Case 2Documento10 páginasIM WW Case 2Dia DimayugaAinda não há avaliações
- SharksDocumento2 páginasSharksDia DimayugaAinda não há avaliações
- Activity 2Documento3 páginasActivity 2Dia DimayugaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Preterm LaborDocumento29 páginasPreterm LaborBer AnneAinda não há avaliações
- The Insulin Receptor and Mechanism of ActionDocumento5 páginasThe Insulin Receptor and Mechanism of ActionMonica AbabeiAinda não há avaliações
- Esophageal Cancer NewDocumento52 páginasEsophageal Cancer Newapi-282115150Ainda não há avaliações
- Lakshmi V Paed KIMSB 2013Documento155 páginasLakshmi V Paed KIMSB 2013Kari RichardsonAinda não há avaliações
- Medicine Cupboard Keys Part BDocumento6 páginasMedicine Cupboard Keys Part BSojiAinda não há avaliações
- Reproduction and Heredity NotesDocumento63 páginasReproduction and Heredity NotesmceldowneaAinda não há avaliações
- Customizing Anaphylaxis Guidelines For Emergency MedicineDocumento8 páginasCustomizing Anaphylaxis Guidelines For Emergency MedicineCAMILA FERNANDA ROMERO GODOYAinda não há avaliações
- Gen Bio1 - Q1 - Module1 - WK1Documento19 páginasGen Bio1 - Q1 - Module1 - WK1Teacher Charlyn VlogAinda não há avaliações
- Sirshasana: Sirsasana 001 Sirsasana 002 Sirsasana 003 Sirsasana 004Documento2 páginasSirshasana: Sirsasana 001 Sirsasana 002 Sirsasana 003 Sirsasana 004Karisma SenapatiAinda não há avaliações
- TrajectoryDocumento29 páginasTrajectoryDithaALkunaAinda não há avaliações
- Compilation of Reviewer For Fundamentals of Nursing PDF FreeDocumento49 páginasCompilation of Reviewer For Fundamentals of Nursing PDF FreeTyler VintAinda não há avaliações
- Including Proper Education in Every Student's BackpackDocumento1 páginaIncluding Proper Education in Every Student's BackpackBlesshy Feb Melecio VisitacionAinda não há avaliações
- Quick Guide For BS200Documento16 páginasQuick Guide For BS200Diego Manuel TernidaAinda não há avaliações
- Asada 2Documento33 páginasAsada 2Anonymous iNLNBVtpoAinda não há avaliações
- Older AdultsDocumento21 páginasOlder AdultsGildred Rada BerjaAinda não há avaliações
- Fallen Angels - Walter Dean MyersDocumento815 páginasFallen Angels - Walter Dean MyersTache_Georgescu60% (5)
- Main PDFDocumento3 páginasMain PDFAlmira RahmaAinda não há avaliações
- Discrimination Resource Dec. 2020Documento33 páginasDiscrimination Resource Dec. 2020Fiorella CastilloAinda não há avaliações
- 10 Healthiest Fermented FoodsDocumento5 páginas10 Healthiest Fermented FoodsbateriameaAinda não há avaliações
- Surgical EndodonticsDocumento28 páginasSurgical Endodonticstomboy997Ainda não há avaliações
- Reading - Age With Moderate DehydrationDocumento8 páginasReading - Age With Moderate DehydrationSophia IbuyanAinda não há avaliações
- Another 365 Things That People Believe That Aren't TrueDocumento85 páginasAnother 365 Things That People Believe That Aren't TrueMohaideen SubaireAinda não há avaliações
- Army Life - Your Guide To The Medical ServicesDocumento15 páginasArmy Life - Your Guide To The Medical Servicesdemarchi2330Ainda não há avaliações
- File 7165Documento111 páginasFile 7165Riley ScherrAinda não há avaliações
- CHAPTER 2 Pharmacologic PrinciplesDocumento59 páginasCHAPTER 2 Pharmacologic PrinciplesASLY LUCIANA MARQUEZ GALLARDOAinda não há avaliações
- Pill CameraDocumento21 páginasPill CameraAnil DsouzaAinda não há avaliações
- 130248-Gc1 Immulite Global Menu Final-01971879Documento2 páginas130248-Gc1 Immulite Global Menu Final-01971879Jano GarciaAinda não há avaliações
- Accurate Diagnosis Is Difficult, Specially in The Latent PhaseDocumento4 páginasAccurate Diagnosis Is Difficult, Specially in The Latent Phasev_vijayakanth7656Ainda não há avaliações
- Bioactive and Functional Ingredients From Dairy Products: March 2019Documento41 páginasBioactive and Functional Ingredients From Dairy Products: March 2019Fandy RoevAinda não há avaliações
- Kidney StonesDocumento65 páginasKidney StonesnazmiAinda não há avaliações