Escolar Documentos
Profissional Documentos
Cultura Documentos
Addison Disease: Diagnosis and Initial Management
Enviado por
Teguh RahTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Addison Disease: Diagnosis and Initial Management
Enviado por
Teguh RahDireitos autorais:
Formatos disponíveis
834 Reprinted from AUSTRALIAN FAMILY PHYSICIAN VOL. 39, NO.
11, NOVEMBER 2010
Background
Adrenal insufficiency is a rare disease caused by either
primary adrenal failure (Addison disease) or by impairment
of the hypothalamic-pituitary-adrenal axis. Steroid
replacement therapy normalises quality of life, however,
adherence can be problematic.
Objective
This article provides information on adrenal insufficiency
focusing on awareness of initial symptoms and on
risk scenarios, emergency management and baseline
investigations, complete investigations and long term
management.
Discussion
Early recognition of adrenal insufficiency is essential
to avoid associated morbidity and mortality. Initial
diagnosis and decision to treat are based on history and
physical examination. Appropriate management includes
emergency resuscitation and steroid administration. Initial
investigations can include sodium, potassium and blood
glucose levels. However, complete investigations can be
deferred. Specialist advice should be obtained and long
term management includes a Team Care Arrangement. For
patients, an emergency plan and emergency identification
are essential.
Keywords: Addison disease; diagnosis, differential;
fludrocortisone; hydrocortisone; patient care planning
Susan OConnell
Aris Siafarikas
Addison disease
Diagnosis and initial management
Primary adrenal insufficiency was first described
by the English physician Thomas Addison in 1855.
1
Addison disease is a rare condition with an estimated
prevalence of 411 per 100 000 and an incidence of 0.8
per 100 000 population/year.
2,3
In children, boys constitute
approximately 75% of patients in contrast to adults, where
the majority (70%) are women.
4
The underlying pathology is
a destruction of the cortex of the adrenal gland.
5
Secretion
of cortisol is reduced or absent, with or without associated
reduction or absence of aldosterone. Adrenocorticotrophic
hormone (ACTH) levels are increased.
2
Historically, tuberculosis was the most common cause of Addison
disease.
4,5
Today however, 7080% of all cases of Addison disease
in the Western world are due to autoimmune adrenalitis;
4,6
whereas
worldwide infectious diseases such as tuberculosis,
7
fungal
infections (histoplasmosis, cryptococcus), and cytomegalovirus are
still important causes. Acute haemorrhage (ie. in meningococcal
septicaemia) although uncommon, is also a cause of primary adrenal
insufficiency.
5
Overall, Addison disease in the paediatric population is most
commonly attributed to primary adrenal insufficiency, which occurs in
approximately one in 15 000 births and usually presents in the neonatal
period or early childhood.
8
Ninety-five percent of cases are due to
deficiency of an enzyme (21 hydroxylase) involved in the steroidogenesis
pathway, which also results in impaired aldosterone synthesis. In
contrast to Addison disease, the adrenal cortex is not destroyed and
hence increased ACTH stimulation causes adrenal hyperplasia.
5
Concomitant autoimmune disease is seen in 50% of patients with
Addison disease. These include thyroid disease, hypoparathyroidism
and type 1 diabetes mellitus.
5
More complex associations can be found
in two recognised polyglandular autoimmune syndromes (PGA).
5,8,9
Secondary forms of adrenal insufficiency, characterised by low
ACTH levels, are caused by hypopituitarism due to pituitary disease,
or suppression of the hypothalamo-pituitary-adrenal axis (HPA)
following steroid therapy or endogenous steroid excess (ie. tumour).
The role of inhaled steroids is controversial. It has been suggested
that therapy with more than 800 g/day over a prolonged period of
time might result in HPA suppression.
10
In secondary adrenal insufficiency, secretion of aldosterone is
not affected. However, with acute hypopituitarism, other hormone
Traps for the unwary
Reprinted from AUSTRALIAN FAMILY PHYSICIAN VOL. 39, NO. 11, NOVEMBER 2010 835
What should I do?
In every scenario the initial diagnosis of acute adrenal insufficiency
and decision to treat are based on history, physical examination, and
occasionally, laboratory findings (hyponatraemia, hyperkalaemia,
hypoglycaemia).
12
Delay in treatment while attempting to confirm
this diagnosis can result in poor outcomes and must be avoided
(Table 1).
13
Management of adrenal crisis
This is a medical emergency.
12,13
Acute management is based
on emergency resuscitation: restoring and maintaining circulation,
administration of IV hydrocortisone, detection and treatment of
hypoglycaemia, and identification and treatment of precipitating
causes. A specialist should be contacted early. In many cases
admission to an intensive care unit will be required.
12,13
Management of the subacute or chronic
presentation
In most cases patients are cardiovascularly stable. Electrolyte
imbalances and hypoglycaemia can be present. Therapy will focus
on steroid replacement and fluid resuscitation. Basic laboratory
investigations include sodium, potassium and blood glucose levels.
Urea, creatinine, calcium and full blood count can be added to
specify underlying causes. Referral to an endocrinologist for further
investigations will be required to confirm primary adrenal insufficiency.
Optional investigations are: serum cortisol, serum ACTH and
24 hour urinary cortisol. If considered necessary, a synacthen (ACTH
stimulation) test can be performed but this should never result in
delayed administration of steroids and should only be performed under
controlled circumstances in the hospital setting.
Education of the patient, and their family, on the diagnosis,
importance of adherence, and an emergency management plan must
be initiated.
Long term management
Long term management may include a Team Care Arrangement
involving a general practitioner, endocrinologist and clinical nurse
specialist. Assistance by social workers and psychologists can be
important. Medical management includes replacement of
cortisol aldosterone. Regular specialist reviews are needed to
optimise therapy.
12,1416
These include: assessment of growth
and pubertal development, looking for clinical signs of adrenal
insufficiency, biochemical analyses of electrolytes, cortisol levels and,
depending on the underlying pathology, ACTH, and monitoring for
other autoimmune conditions.
5
Emphasis will be on the importance
of adherence with medication and adjustments for illness and stress
situations to achieve a good quality of life.
11,13
As steroid replacement
therapy is associated with an increased risk of osteoporosis, further
investigations including dual energy X-ray absorptiometry scans and
preventive strategies such as adequate dietary calcium, exercise and
vitamin D/sun exposure should be considered.
deficiencies including growth hormone, thyroxine, oestradiol or
testosterone, must be identified and treated.
When should I consider an adrenal
crisis?
Adrenal crisis is a medical emergency and should be considered in any
patient presenting with one or more of the following symptoms:
altered consciousness
circulatory collapse
hypoglycaemia
hyponatraemia
hyperkalaemia
seizures
history of steroid use/withdrawal, or
any clinical features of Addison disease.
Adrenal crisis may be precipitated by stress, sepsis, dehydration or
trauma; clinical features may be modified accordingly. In patients with
known adrenal insufficiency, nonadherence with therapy, inappropriate
cortisol dose reduction or lack of stress related cortisol dose
adjustment can cause adrenal crisis.
11
When should I consider Addison
disease?
Addison disease can manifest with adrenal crisis. Chronic symptoms
result from cortisol deficiency, aldosterone deficiency and excess ACTH:
cortisol deficiency results in weakness (99%), fatigue, weight loss
(97%), anorexia progressing to nausea, vomiting, diarrhoea (20%),
constipation (19%), flank or abdominal pain (34%), low blood
glucose levels and hyperthermia.
2,4,5
Fasting hypoglycaemia is
common and occurs because of loss of the gluconeogenic effects of
cortisol.
5
In patients with pre-existing type 1 diabetes, deterioration
of glycaemic control with recurrent hypoglycaemia can be the
presenting sign of adrenal insufficiency
2
aldosterone deficiency causes hyponatraemia, hyperkalaemia,
acidosis, tachycardia and hypotension. Low voltage
electrocardiogram (ECG) and a small heart on chest X-ray are
not necessarily present.
4,5
Suggestive symptoms are postural
hypotension and salt cravings
2,11
excess ACTH is only present in primary adrenal insufficiency. It
causes increased melanin production resulting in generalised
hyperpigmentation.
4,5
Because this resembles a suntan, it is
essential to inspect areas not exposed to the sun for diffuse
hyperpigmentation which can be more obvious in recent scars
and in areas such as the axillae, nipples, pressure points,
palmar creases, and mucous membranes. Some patients with
autoimmune mediated adrenal insufficiency also present with
vitiligo.
2,5
Chronic unrecognised Addison disease can cause psychiatric symptoms
such as memory impairment, confusion, apathy, depression and
psychosis.
5
These features regress on treatment with replacement
corticosteroids.
FOCUS
836 Reprinted from AUSTRALIAN FAMILY PHYSICIAN VOL. 39, NO. 11, NOVEMBER 2010
Addison disease diagnosis and initial management
5.5 mmol/L. He was given a bolus of 10% dextrose followed
by normal saline. He then had a generalised tonic clonic
seizure, was treated with anticonvulsants and intubated,
ventilated and transferred to the intensive care unit.
In his background history he had an admission at 11 months
of age with profound hypoglycaemia (BGL 0.6 mmol/L)
following an episode of gastroenteritis. He had presented to
the ED unresponsive and pale following 18 hours of profuse,
watery diarrhoea and vomiting. At that time, sodium was
recorded at 126 mmol/L with potassium 4.3 mmol/L. He
became alert and interactive after 10% dextrose bolus.
On the second admission, the boy was noted to have
hyperpigmentation of the buccal mucosa (Figure 1) and
appeared diffusely suntanned.
Plasma cortisol was <30 mmol/L with a raised ACTH of
492 pmol/L (normal range 2.010). A diagnosis of acute
Addisonian crisis was made and he was treated with 50 mg
IV hydrocortisone 4 hourly. He made a full recovery.
He was discharged on oral maintenance hydrocortisone
with an emergency plan. A MedicAlert bracelet and
ambulance cover were organised. Further investigations
revealed normal aldosterone levels, negative adrenal
Emergency plan
An up-to-date emergency plan and practical teaching in administering
emergency medication are of paramount importance. At each
consultation the physician must ensure that the patient and carer(s)
are well versed in the emergency plan and that their ready-to-use vial
of emergency hydrocortisone is in-date and available for use at any
time.
11,14
In growing children, the dose may require adjustment and a
new appropriate prescription should be issued where indicated. It is
recommended that patients wear a MedicAlert bracelet or pendant and
have ambulance cover.
Case study 1 An acute presentation
Paramedics attended a boy, aged 21 months, at his home. His
Glasgow Coma Scale was 8/15. He was poorly perfused, with
Sp0
2
of 76% and capillary blood glucose <2 mmol/L. He had
been unwell at home with symptoms of an upper respiratory
tract infection for the previous 24 hours. He was given oral
glucose gel and IM glucagon with no effect. On arrival at
the hospital emergency department he had spontaneous
respirations with a heart rate of 126 bpm and cool peripheries.
Investigations showed a metabolic acidosis, blood glucose
level (BGL) of 1.6 mmol/L, sodium 134 mmol/L and potassium
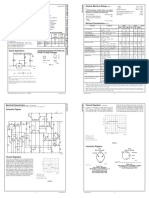
Table 1. Summary of the management and prevention of acute adrenal insufciency
5,11,14
Clinical findings
Cortisol deficiency: weakness, anorexia, nausea
and/or vomiting, hypoglycaemia, hypotension
(particularly postural) and shock
Aldosterone deficiency: dehydration, hyperkalaemia,
hyponatraemia, acidosis, low blood pressure
Investigations
Blood sugar level; serum glucose, urea, sodium and
potassium; blood gas analysis
Keep extra blood for analysis of ACTH and cortisol
if possible
Do not wait for results to start therapy
Intravenous fluids
Initial fluid resuscitation: NaCl 0.9% 20 mL/kg (severe
dehydration); 10 mL/kg (moderate dehydration)
repeat until circulation restored
Maintenance fluids: 510% dextrose
Steroid replacement (hydrocortisone)
If intravenous (IV) access is difficult, give
intramuscularly (IM) while establishing IV line
Neonates (1 year): 25 mg stat, then 1025 mg
46 hourly
Toddlers (13 years): 2550 mg stat, then 2550 mg
46 hourly
Children (412 years): 5075 mg stat, then 5075 mg
46 hourly
Adolescents and adults: 100150 mg stat, then 100 mg
46 hourly
Correction of hypoglycaemia
Neonates or infants: 10% dextrose 5 mL/kg (IV bolus)
Older children, adolescents and adults: 25% dextrose
2 mL/kg (IV bolus)
Correction of hyperkalaemia
Potassium usually normalises with fluid and electrolyte
replacement
If K+ >6 mmol/L perform ECG and apply cardiac monitor
as arrhythmias and cardiac arrest may occur
Identify and treat potential precipitating causes
Admit to appropriate inpatient facility
When patient tolerates oral intake
Reduce IV hyrocortisone dose, then switch to triple
dose oral hydrocortisone therapy, gradually reducing to
maintenance levels (1015 mg/m
2
/day)
Patients with aldosterone deficiency: start fludrocortisone
at maintenance doses (usually 0.1 mg/day)
11
Prevention
Emergency plan for susceptible patients, emergency
identification (MedicAlert)
Triple normal oral maintenance dose for 23 days during
stress (ie. fever, fracture)
Administer IM hydrocortisone if oral medication not
tolerated (eg. vomiting)
Increase parenteral hydrocortisone (12 mg/kg) before
anaesthesia, consider increased dose postoperatively
Ensure patients have ambulance cover and ready-to-use
IM hydrocortisone preparation (Act-o-vial
) for emergencies
FOCUS
Reprinted from AUSTRALIAN FAMILY PHYSICIAN VOL. 39, NO. 11, NOVEMBER 2010 837
Addison disease diagnosis and initial management
Why is Addison disease easily missed?
Addison disease is easily missed due to nonspecific symptoms and
presentations, rarity of the condition, and low index of suspicion.
The consequences of delayed diagnosis and treatment are increased
morbidity, mortality and medicolegal risk.
12,13
Outcomes may be
improved with a higher index of diagnostic suspicion, prompt emergency
management with IM or IV hydrocortisone as indicated, early referral,
and good patient education.
11,13
Key points in management
Physical findings are subtle and nonspecific; hyperpigmentation
may be seen, particularly in sun exposed areas or pressure points.
Circulatory compromise can range from mild signs of sodium and
volume depletion to shock.
If in doubt give oral/IM/IV hydrocortisone.
Dont delay treatment while awaiting laboratory results.
Authors
Susan OConnell MB, MRCPI, MD, is Fellow in Paediatric
Endocrinology, Princess Margaret Hospital for Children, Western
Australia. susanmary.oconnell@health.wa.gov.au
Aris Siafarikas MD, FRACP, is Consultant Paediatric Endocrinologist,
Princess Margaret Hospital for Children, Clinical Associate Professor,
Institute of Health and Rehabilitation Research, University of Notre
Dame, and Senior Clinical Lecturer, School of Paediatrics and Child
Health, University of Western Australia, Perth, Western Australia.
Conflict of interest: none declared.
References
1. Addison T, editor. On the constitutional and local effects of disease of the supra-
renal capsules. London: Highley, 1855.
2. Arlt W, Allolio B. Adrenal insufficiency. Lancet 2003;361:188193.
3. Laureti S, Vecchi L, Santeusanio F, et al. Is the prevalence of Addisons disease
underestimated? J Clin Endocrinol Metab 1999;84:1762.
4. Brook GD, Brown RS, editors. Handbook of clinical pediatric endocrinology. 1st
edn. Malden, Mass: Blackwell Publishing, 2008.
5. Kronenburg, editor. Williams textbook of endocrinology. 11th edn. Philadelphia:
Saunders Elsevier, 2008.
6. Oelkers W. Adrenal insufficiency. N Engl J Med 1996;335:120612.
7. Soule S. Addisons disease in Africa a teaching hospital experience. Clin
Endocrinol (Oxf) 1999;50:11520.
8. Perry R, Kecha O, Paquette J, et al. Primary adrenal insufficiency in children:
twenty years experience at the Sainte-Justine Hospital, Montreal. J Clin
Endocrinol Metab 2005;90:324350.
9. Ahonen P, Myllarniemi S, Sipila I, et al. Clinical variation of autoimmune
polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED) in a series of 68
patients. N Engl J Med 1990;322:182936.
10. Greenfield JR, Samaras K. Suppression of HPA axis in adults taking inhaled corti-
costeroids. Thorax 2006;61:2723.
11. Arlt W. The approach to the adult with newly diagnosed adrenal insufficiency. J
Clin Endocrinol Metab 2009;94:105967.
12. Klauer KM. Adrenal insufficiency and adrenal crisis: differential diagnoses and
workup, 2009. Available at http://emedicine.medscape.com/article/765753-
diagnosis [Accessed 21 October 2010].
13. Erichsen MM, Lovas K, Fougner KJ, et al. Normal overall mortality rate in
Addisons disease, but young patients are at risk of premature death. Eur J
Endocrinol 2009;160:2337.
14. The Royal Childrens Hospital Melbourne. Adrenal crisis. 2010. Available at
www.rch.org.au/clinicalguide/cpg.cfm?doc_id=5121 [Accessed 24 June 2010].
15. Nieman L. Patient information: adrenal insufficiency (Addisons disease).
UpToDate, (internet serial), 2010.
16. Grant DB, Barnes ND, Moncrieff MW, et al. Clinical presentation, growth, and
pubertal development in Addisons disease. Arch Dis Child 1985;60:9258.
antibodies and normal, very long chain fatty acids (to
exclude adrenoleukodystrophy). Investigations to exclude
other endocrinopathies were normal, and no cause for
Addison disease identified.
Ongoing management
Ongoing management in this boy includes oral
hydrocortisone maintenance treatment and growth
monitoring. An emergency plan with instructions to increase
his dose of hydrocortisone in the event of illness is in place.
In the event of unresponsiveness or persistent vomiting his
parents have been instructed on the administration of IM
hydrocortisone and to call the emergency numbers listed
on the emergency plan. The importance of adherence with
regular medications is reiterated and the boys emergency
plan reviewed at each clinic attendance.
Case study 2 Issues in management
A girl, 15 years of age, with a diagnosis of Addison disease
made 3 years previously (anti-adrenal antibodies positive)
attended her routine endocrinology clinic appointment with
her father. She had a history of poor adherence. Regular
medications were: prednisolone 4 mg morning and evening
and fludrocortisone 100 g/day. She denied missing her
medications. She had regular menses. She described fair
energy levels.
On examination she looked well but appeared diffusely
suntanned, not confined to, but more obvious in sun
exposed areas. Her BP was normal. Records showed that
she had not gained weight for the past year.
The patient was intermittently living between her parents
homes. On review of her emergency plan she was unsure
of what to do should she become unwell. Her father
appeared to be well informed in the management of any
illness, however it was revealed that the ready-to-use IM
hydrocortisone was only available at her mothers house.
New prescriptions for IM hydrocortisone were issued for
both homes and for school, and copies of the emergency
plan were also made. The importance of adherence with
regular medication was reiterated.
Figure 1. Hyperpigmentation of the buccal mucosa
Você também pode gostar
- Addison Disease: Diagnosis and Initial ManagementDocumento5 páginasAddison Disease: Diagnosis and Initial ManagementI Gede SubagiaAinda não há avaliações
- Adrenal InsufficiencyDocumento11 páginasAdrenal InsufficiencyAustine OsaweAinda não há avaliações
- Jurnal Krisis AdrenalDocumento4 páginasJurnal Krisis AdrenalMelda IndrawatiAinda não há avaliações
- Causes of Diffuse Hyperpigmentation EndocrinopathiesDocumento9 páginasCauses of Diffuse Hyperpigmentation EndocrinopathiesAbdul QuyyumAinda não há avaliações
- MRCPass Notes For MRCP 1 - EnDOCRINOLOGYDocumento12 páginasMRCPass Notes For MRCP 1 - EnDOCRINOLOGYsabdali100% (1)
- Your Online Nursing Notes : Addison'S Disease Basic InfoDocumento4 páginasYour Online Nursing Notes : Addison'S Disease Basic InfoseigelysticAinda não há avaliações
- Addison's DseDocumento9 páginasAddison's DseKath RubioAinda não há avaliações
- Adrenocortical DisordersDocumento73 páginasAdrenocortical DisordersReunita ConstantiaAinda não há avaliações
- Adrenal Insufficiency: DR - Abbas Mansour Senior Consultant Internal MedicineDocumento24 páginasAdrenal Insufficiency: DR - Abbas Mansour Senior Consultant Internal Medicineraed faisalAinda não há avaliações
- Adrenal Diseases: Types Aetiology Diagnosis Complications TreatmentDocumento29 páginasAdrenal Diseases: Types Aetiology Diagnosis Complications Treatmentgani7222Ainda não há avaliações
- Wernicke Encephalopathy: EtiologyDocumento6 páginasWernicke Encephalopathy: EtiologyDrhikmatullah SheraniAinda não há avaliações
- Adrenal Gland DisordersDocumento31 páginasAdrenal Gland DisordersThe AbyssinicansAinda não há avaliações
- Insuficiencia AdrenalDocumento5 páginasInsuficiencia AdrenalLuciana RafaelAinda não há avaliações
- Endocrinology NotesDocumento12 páginasEndocrinology Notesrandiey john abelleraAinda não há avaliações
- Adrenal Gland: Adrenal Insufficiency, Addison Disease, Cushing SyndromeDocumento46 páginasAdrenal Gland: Adrenal Insufficiency, Addison Disease, Cushing Syndromeyuyu tuptupAinda não há avaliações
- Addisons DiseaseDocumento12 páginasAddisons DiseaseChinju CyrilAinda não há avaliações
- AddisonsdiseaseDocumento5 páginasAddisonsdiseasenessimmounir1173Ainda não há avaliações
- 6 Mary Lou Sole, Deborah Goldenberg Klein, Marthe J. Moseley - EndokrinDocumento56 páginas6 Mary Lou Sole, Deborah Goldenberg Klein, Marthe J. Moseley - EndokrinyaminmuhAinda não há avaliações
- Thyroid Disorder NCPDocumento9 páginasThyroid Disorder NCPKen RegalaAinda não há avaliações
- Adrenal Crisis: Risk FactorsDocumento25 páginasAdrenal Crisis: Risk Factorspwinzizitah063Ainda não há avaliações
- Adrenal Insufficiency in The Intensive Care Unit: Samir El Ansary Icu Professor Ain Shams CairoDocumento49 páginasAdrenal Insufficiency in The Intensive Care Unit: Samir El Ansary Icu Professor Ain Shams CairoGebby MamuayaAinda não há avaliações
- Adrenal CrisisDocumento4 páginasAdrenal CrisisRichie Marie BajaAinda não há avaliações
- Cushings, Addisons and Acromegaly: DR J Storrow FY2Documento38 páginasCushings, Addisons and Acromegaly: DR J Storrow FY2abdalkhalidAinda não há avaliações
- ENDO - Adrenal CrisisDocumento8 páginasENDO - Adrenal CrisisHajime NakaegawaAinda não há avaliações
- Tanpa JudulDocumento14 páginasTanpa JudulAsrapia HubaisyingAinda não há avaliações
- Endocrinology Course Content: Semester (5) Clinical Pharmacy CourseDocumento91 páginasEndocrinology Course Content: Semester (5) Clinical Pharmacy CourseSadigMukhAinda não há avaliações
- Subclinical Hyperthyroidism Case ReportDocumento26 páginasSubclinical Hyperthyroidism Case ReportkapanjddokterAinda não há avaliações
- 22 MetabolicEncephalopathies FinalDocumento19 páginas22 MetabolicEncephalopathies FinalShravan BimanapalliAinda não há avaliações
- Autoimmune Polyglandular Syndrome ReviewDocumento3 páginasAutoimmune Polyglandular Syndrome ReviewIan AlvaradoAinda não há avaliações
- Adrenal Crisis FinalDocumento10 páginasAdrenal Crisis FinalAmanda Scarlet100% (1)
- REPORTDocumento13 páginasREPORTEarlou MagbanuaAinda não há avaliações
- Addison's DiseaseDocumento3 páginasAddison's Diseaseavinash dhameriyaAinda não há avaliações
- Endocrinology Teaching CasesDocumento47 páginasEndocrinology Teaching CasesBinta BaptisteAinda não há avaliações
- EndokrinDocumento27 páginasEndokrinSarah Putri AbellysaAinda não há avaliações
- Canine Hypoadrenocorticism Overvew Diagnosis and Treatment LolattiDocumento6 páginasCanine Hypoadrenocorticism Overvew Diagnosis and Treatment LolattiAna Clara SevasteAinda não há avaliações
- 20 Endocrine Disease and AnaesthesiaDocumento0 página20 Endocrine Disease and AnaesthesiajuniorebindaAinda não há avaliações
- 2 Bvab048.1976Documento1 página2 Bvab048.1976Anca LunguAinda não há avaliações
- Case Study: MYXEDEMATOUS COMADocumento5 páginasCase Study: MYXEDEMATOUS COMAjisooAinda não há avaliações
- Adrenal Senior 1Documento12 páginasAdrenal Senior 1mohammad saifuddinAinda não há avaliações
- Stunted Growth: Addison DiseaseDocumento32 páginasStunted Growth: Addison DiseaseAshim AbhiAinda não há avaliações
- ENDOCRINE DISORDERS (Autosaved)Documento81 páginasENDOCRINE DISORDERS (Autosaved)Princewill SeiyefaAinda não há avaliações
- Adrenal and Pitutary Disoreders Adigrat LecDocumento144 páginasAdrenal and Pitutary Disoreders Adigrat Lecbereket gashuAinda não há avaliações
- Addison's Disease:: Clinical IntelligenceDocumento3 páginasAddison's Disease:: Clinical Intelligencemira tianiAinda não há avaliações
- Adrenal InsufficiencyDocumento2 páginasAdrenal InsufficiencyTracy NwanneAinda não há avaliações
- Flashcards - QuizletDocumento7 páginasFlashcards - QuizletNEsreAinda não há avaliações
- Addison DiseaseDocumento23 páginasAddison DiseaseKompari EvansAinda não há avaliações
- Pituitary &thyroid NotesDocumento7 páginasPituitary &thyroid NotesAli salimAinda não há avaliações
- Addison's DiseaseDocumento15 páginasAddison's DiseaseRonald A. Ogania50% (4)
- NCMB316 Rle 2-10-7addison's DiseaseDocumento4 páginasNCMB316 Rle 2-10-7addison's DiseaseMaica LectanaAinda não há avaliações
- Parathyroid DisordersDocumento44 páginasParathyroid DisordersBIAN ALKHAZMARIAinda não há avaliações
- Research Paper On Addisons DiseaseDocumento8 páginasResearch Paper On Addisons Diseasetug0l0byh1g2100% (1)
- Geriatric Anesthesia & Analgesia: ComplicationsDocumento4 páginasGeriatric Anesthesia & Analgesia: ComplicationsWilly Victorio CisnerosAinda não há avaliações
- adrenal presentation - صیادیDocumento39 páginasadrenal presentation - صیادیRazyAinda não há avaliações
- Summary of Medical EmergenciesDocumento24 páginasSummary of Medical Emergenciesbasharswork99Ainda não há avaliações
- Addisonian Crisis: Manish K Medical Officer IgmhDocumento47 páginasAddisonian Crisis: Manish K Medical Officer IgmhNaaz Delhiwale100% (1)
- Reye'S Syndrome: Mrs. Smitha.M Associate Professor Vijaya College of Nursing KottarakkaraDocumento7 páginasReye'S Syndrome: Mrs. Smitha.M Associate Professor Vijaya College of Nursing KottarakkarakrishnasreeAinda não há avaliações
- Endocrine DiseasesDocumento64 páginasEndocrine DiseasesshobanaaaradhanaAinda não há avaliações
- Thyrotoxicosis Ischaemic Heart Disease Hypertension Alcohol Excess Lone Atrial FibrillationDocumento5 páginasThyrotoxicosis Ischaemic Heart Disease Hypertension Alcohol Excess Lone Atrial FibrillationZhao Xuan TanAinda não há avaliações
- 351 UN 1824 Sodium Hydroxide SolutionDocumento8 páginas351 UN 1824 Sodium Hydroxide SolutionCharls DeimoyAinda não há avaliações
- Celltac MEK 6500Documento3 páginasCelltac MEK 6500RiduanAinda não há avaliações
- Presentasi Evaluasi Manajemen Risiko - YLYDocumento16 páginasPresentasi Evaluasi Manajemen Risiko - YLYOPERASIONALAinda não há avaliações
- Withania DSC PDFDocumento6 páginasWithania DSC PDFEfsha KhanAinda não há avaliações
- Qualitative Tests Organic NotesDocumento5 páginasQualitative Tests Organic NotesAdorned. pearlAinda não há avaliações
- Ams - 4640-C63000 Aluminium Nickel MNDocumento3 páginasAms - 4640-C63000 Aluminium Nickel MNOrnella MancinelliAinda não há avaliações
- Sociology/Marriage PresentationDocumento31 páginasSociology/Marriage PresentationDoofSadAinda não há avaliações
- PMEGP Revised Projects (Mfg. & Service) Vol 1Documento260 páginasPMEGP Revised Projects (Mfg. & Service) Vol 1Santosh BasnetAinda não há avaliações
- (ISPS Book Series) Yrjö O. Alanen, Manuel González de Chávez, Ann-Louise S. Silver, Brian Martindale - Psychotherapeutic Approaches To Schizophrenic Psychoses - Past, Present and Future-Routledge (20Documento419 páginas(ISPS Book Series) Yrjö O. Alanen, Manuel González de Chávez, Ann-Louise S. Silver, Brian Martindale - Psychotherapeutic Approaches To Schizophrenic Psychoses - Past, Present and Future-Routledge (20Manuel100% (1)
- Women and International Human Rights Law PDFDocumento67 páginasWomen and International Human Rights Law PDFakilasriAinda não há avaliações
- GeoSS Event Seminar 12 July 2012 - SlidesDocumento15 páginasGeoSS Event Seminar 12 July 2012 - SlidesNurmanda RamadhaniAinda não há avaliações
- 2008 03 20 BDocumento8 páginas2008 03 20 BSouthern Maryland OnlineAinda não há avaliações
- Additional Activity 3 InsciDocumento3 páginasAdditional Activity 3 InsciZophia Bianca BaguioAinda não há avaliações
- Shoulder Joint Position Sense Improves With ElevationDocumento10 páginasShoulder Joint Position Sense Improves With ElevationpredragbozicAinda não há avaliações
- HDFC Life Insurance (HDFCLIFE) : 2. P/E 58 3. Book Value (RS) 23.57Documento5 páginasHDFC Life Insurance (HDFCLIFE) : 2. P/E 58 3. Book Value (RS) 23.57Srini VasanAinda não há avaliações
- Defects Lamellar TearingDocumento6 páginasDefects Lamellar Tearingguru_terexAinda não há avaliações
- Cataloge ICARDocumento66 páginasCataloge ICARAgoess Oetomo100% (1)
- Vocab PDFDocumento29 páginasVocab PDFShahab SaqibAinda não há avaliações
- LM 337Documento4 páginasLM 337matias robertAinda não há avaliações
- NASA ISS Expedition 2 Press KitDocumento27 páginasNASA ISS Expedition 2 Press KitOrion2015Ainda não há avaliações
- Ethnomedicinal Plants For Indigestion in Uthiramerur Taluk Kancheepuram District Tamilnadu IndiaDocumento8 páginasEthnomedicinal Plants For Indigestion in Uthiramerur Taluk Kancheepuram District Tamilnadu IndiaGladys DjeugaAinda não há avaliações
- Pescatarian Mediterranean Diet Cookbook 2 - Adele TylerDocumento98 páginasPescatarian Mediterranean Diet Cookbook 2 - Adele Tylerrabino_rojoAinda não há avaliações
- Allison Weech Final ResumeDocumento1 páginaAllison Weech Final Resumeapi-506177291Ainda não há avaliações
- Indirect Current Control of LCL Based Shunt Active Power FilterDocumento10 páginasIndirect Current Control of LCL Based Shunt Active Power FilterArsham5033Ainda não há avaliações
- Cisco - Level 45Documento1 páginaCisco - Level 45vithash shanAinda não há avaliações
- Leave of Absence Form (Rev. 02 072017)Documento1 páginaLeave of Absence Form (Rev. 02 072017)KIMBERLY BALISACANAinda não há avaliações
- Material: Safety Data SheetDocumento3 páginasMaterial: Safety Data SheetMichael JoudalAinda não há avaliações
- 1 Stra Bill FinalDocumento41 páginas1 Stra Bill FinalRajesh JhaAinda não há avaliações
- R. Nishanth K. VigneswaranDocumento20 páginasR. Nishanth K. VigneswaranAbishaTeslinAinda não há avaliações
- Ergo 1 - Workshop 3Documento3 páginasErgo 1 - Workshop 3Mugar GeillaAinda não há avaliações