Escolar Documentos
Profissional Documentos
Cultura Documentos
Herbal Photoprotective Formulation and Their Evaluation - Chanchal & Swarnlata 2009
Enviado por
Desy M WenasTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Herbal Photoprotective Formulation and Their Evaluation - Chanchal & Swarnlata 2009
Enviado por
Desy M WenasDireitos autorais:
Formatos disponíveis
The Open Natural Products Journal, 2009, 2, 71-76 71
1874-8481/09 2009 Bentham Open
Open Access
Herbal Photoprotective Formulations and their Evaluation
Deep Chanchal and Saraf Swarnlata*
Institute of Pharmacy, Pt. Ravishankar Shukla University, Raipur., C.G. 492001, India
Abstract: Photochemoprevention has become an important armamentarium in the fight against ultraviolet radiation in-
duced damage to the skin. UV irradiation to skin results in erythema, edema, sunburn cells, hyperplasia, immunosuppres-
sion, photoaging and photocarcinogenesis. Various synthetic agents have been used as photoprotectives but they have lim-
ited use because of their potential toxicity in humans and their ability to interfere only in selected pathways of multistage
process of carcinogenesis. Several botanical compounds have been shown to be antimutagenic, anticarcinogenic and non-
toxic and have ability to exert striking inhibitory effects on a plethora of cellular events at various stages of carcinogene-
sis. Since multiple pathways are involved in photocarcinogenesis so mixture of several botanical antioxidants working
through various mechanisms, in conjunction with the use of sunscreens could also be an effective approach for reducing
photoaging and skin cancer in humans. The performance of sunscreen substances could be improved by modification of
their chemical, physical and technological properties or by the use of novel carriers like liposomes, nanoparticles, phyto-
somes, transferosomes, nanospheres etc. The application of novel approaches can also improve its efficacy regarding con-
tinuous action of herbs on the human body. This review will focus on list of herbs, formulations and evaluation parame-
ters of photoprotective herbs.
Keywords: Photoprotectives, evaluation, herbs, photoaging, herbal formulations.
INTRODUCTION
Long exposure of UV radiation increases the risk of skin
cancer including basal cell and squamous cell carcinoma as
well as malignant melanoma. There are also many specific
diseases like phototoxic or photoallergic reactions, autoim-
mune diseases including lupus erythematous, idiopathic pho-
todermatosis and varieties of skin cancers which are trig-
gered or exacerbated by UV radiation exposure. Solar UVR
is divided into three categories UV-C (200-280 nm), UV-B
(280-320 nm ) and UV-A (320-400 nm ). UV-C is most bio-
logically damaging but it is filtered out by ozone layer. Cur-
rently UV-B radiation and to a lesser extent UV-A are re-
sponsible for inducing skin cancer [1]. Among many UV-R
damages, skin cancer is of greatest concern as its rates have
been increasing. Ultraviolet radiation increases oxidative
stress in skin cells by causing excessive generation of reac-
tive oxygen species (ROS), leading to cancer initiation and
promotion. The main histological features of photoaging
include dermal damage with marked elastotic degenerative
change, loss of collagen, reduction in number and size of
fibroblasts, an increase in proteoglycans and a moderate
mononuclear inflammatory cell infiltrate. Irregular epidermal
thickening progressing in the later stages leads to dysplasia
and cytological atypia [2]. Development of novel strategies
to reduce the occurrence of skin cancer and delay the process
of photoaging are highly desirable goals. Photoprotection
could be achieved by the use of sunscreens, moisturizers,
keratolytics and antioxidants.
There are so many synthetic sunscreen agents (Octaben-
zone, Octyl methoxyciinnan~ate, Benzophenone-3, Pro-
*Address correspondence to this author at the Institute of Pharmacy, Pt.
Ravishankar Shukla University, Raipur., C.G. 492001, India; Tel/Fax: +91
771 2262832; E-mail: swarnlata_saraf@rediffmail.com
vatene, 2-Ethoxy Ethyl P-Methoxycinnamate, Sulisoben-
zone, Mexenone, Avobenzone, Dioxybenzone, 4-Dimethyl
Amino Benzoic acid etc.) are available in form of photopro-
tectives with certain limitation, which restrict their use at cel-
lular level. They have limited use because of their potential
toxicity in humans and their ability to interfere only in selected
pathways of the multistage process of carcinogenesis [3]. Bo-
tanical agents may work in various ways by stimulating the
immune response, by inducing gene suppression, by detoxify-
ing carcinogens, by blocking oxidative damage to DNA, by
initiating selected signaling pathways or by other mechanisms.
Thus many of these agents play multiple roles in ameliorating
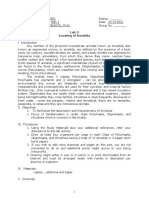
the process of carcinogenesis [3]. (Fig. 1) Few examples in-
clude tea polyphenols, curcumin, silymarin, garlic compounds,
apigenin, resveratrol, ginkgo biloba, beta- carotenoids, ascor-
bic acid etc. Compounds that can protect against UV- A and
UV- B radiations both could be ideal photochemoprotective
agents [3].
The active synthetic molecules are being used since
years, but the research shows that these active molecules
adversely affects on human skin via self inducing reactive
oxygen species. Thus, to overcome such serious side effects
of synthetic molecules, the research is now diverted towards
natural biomaterials [4]. Naturally occurring antioxidants
like alpha carotene, ascorbic acids, flavones, flavanone, have
ability to donate electrons and stops free radical chain reac-
tions and also showed broad spectrum UV absorption [5,6] It
was reported that association of botanical extracts (biofla-
vonoids) and vitamins produce synergistic photoprotective
effects in preventing increased erythema, transepidermal
water loss and sunburn cell formation [7].
The herbs as biological additives in form of extracts are
utilizing since long period of time in the cosmetic formula-
tion and now scientific evidences proven that many plant
72 The Open Natural Products Journal, 2009, Volume 2 Chanchal and Swarnlata
extracts showed their photo protective activity with signifi-
cant improvement in enzymes like superoxidedismutase,
catalase and total protein and ascorbic acid level [8]. Extracts
of many plants, citrus fruits and leafy vegetables as source of
ascorbic acid, vitamin E and phenolics compounds and en-
zymes possess the ability to reduce the oxidative damage.
These oxidative damages ultimately reduce the protective
enzyme level and imbalances the level of total protein and
ascorbic acid and other antioxidants level in cells. The
creams comprises such extracts could be utilized for the pro-
tection of photo induced intrinsic oxidative stress as well as
structural alteration in skin [9].
In the series of natural photo protective agents, enzymes
like superoxide dismutase (SOD), peroxidase and proteolytic
enzymes have opened up new avenues to photoprotective
reaction occurring within the cell. These chemical entities
were first discovered in 19th century, where as use of en-
zymes in cosmetics have been advocated for many years [10].
Proteolytic enzymes like bromelaine, papain etc. has been
used for skin peeling and smoothing [11]. These are utilized
as efficient tool to reduce UV-induced erythema, which can
also be thought of as free radical scavenging ability [12].
Naturally occurring herbal compounds such as phenolic
acids, flavonoids and high molecular weight polyphenols are
very useful for prevention of the adverse effects of UV radia-
tion on the skin and evaluation of their clinical efficacy is
awaited [13]. Adequate UV A protection and an appropriate
testing method of UV A efficacy are the most pressing un-
met needs [14]. Most commonly used herbal photoprotec-
tives are listed in Table 1, this table will be helpful in the
selection of herbal constituent for formulation of photopro-
tective dosage form.
HISTOPATHOLOGICAL CHANGES OF PHO-
TOAGING
In skin aging two independent processes occur simulta-
neously (i) Chronological or intrinsic aging which affects the
skin by slow and irreversible tissue degeneration and (ii)
extrinsic aging or photoaging, which results from exposure to
environmental factors including primarily ultraviolet (UV)
radiation. In chronological aging skin becomes thin, dry, pale
and exhibits fine wrinkles while, photoaging leads to marked
cutaneous alterations characterized clinically by deep wrin-
kles, roughness, sallowness, mottled dyspigmentation, te-
langiectasia and a variety of benign and malignant neoplasms.
In chronologically aged skin, the different characteristic steps
of epidermal differentiation are preserved, however, based on
a reduced keratinocyte proliferation, epidermal thinning is
observed histologically. The dermis is also thin in aged skin,
resulting from a reduction in the amount and organization of
connective tissue. The extracellular matrix in the dermis is
composed primarily of type I collagen, associated with type III
collagen, elastin, proteoglycans and fibronectin. Sun-exposed
sites usually display a reduction in mature type I collagen and
an increase in collagen III-tocollagen I ratio. The histopa-
thological hall-mark of photoaging is a massive accumulation
of elastotic material in the upper and mid dermis also known
as solar elastosis. Elastosis is due to accumulation of dam-
aged elastin, the main component of elastic fibers, and is asso-
ciated with degeneration of the surrounding collagen mesh-
work [15]. The histological effects can be well studied by
Table 2, it helps to decide the evaluation parameter (Table 3).
Fig. (1). Multiple pathway mechanism of botanical photoprotectives [3].
Sunscreen (1
st
line) Redox regulation of
signal transduction
pathway (3
rd
line)
Prevention of
damage
Suppresses inflammation
Suppresses proliferation
Transformation specific
apoptosis in transformed cells
UVB
Antioxidant (2
nd
line)
Radical scavenger
Reduces oxidative stress
Reduces DNA damage
Gene
Inactivation
p53
DNA excission repair
Prevention Correction
Skin
Botanical Antioxidants Act As
Herbal Photoprotective Formulations and their Evaluation The Open Natural Products Journal, 2009, Volume 2 73
Table 1. Herbal Constituents Used as Photoprotectives [2, 13]
Natural Photoprotective
Agents
Source/Family Components Action/Uses
Tea Green, black and oolong teas Catechin, gallocatechin, gallic acid,
kaempferol, myricintin
Potent antioxidant and can scavenge
ROS
Curcumin Root of Curcuma longa Zingiberacea Curcumin (diferuloylmethane) Antioxidant, anti-inflammatory
Silymarin Milk thistle( Silybum marianum) Silybin, silibinin, silidianin, silychris-
tin, isosylibin
Antioxidant and anticarcinogenic
Genistein Soy, red clover, ginkgo biloba, Greek
oregano and Greek sage
Genistein Antioxidant and anticarcinogenic
Garlic compounds Allium sativum Garlic sulphur compounds Antioxidant and photochemopreventive
Apigenin Vascular plants 5,7,4 trihydroxyflavone Anticarcinogenic
Resveratrol Grapes, nuts, fruits Trans-345-trihydroxystilbine Potent antioxidant, anti-inflammatory
and antiproliferative.
Ginkgo biloba Ginkgoacea Quercetin,epicatechin, rutin,apigenin Antioxidant, anti-inflammatory and
anticarcinogenic
Carotenoids Green plants, carrots,tomatoes etc. carotene, lycopenes Photoprotective
- tocopherol Plant oils - tocopherol Photochemoprotective
L-ascorbic acid Most fruits and vegetables L-ascorbic acid Antioxidant
Caffeic and ferulic acids Vegetables, olives, olive oil Caffeic and ferulic acids Photochemoprotective
Table 2. Histopathological Effects of Photoaging [16]
Parameters Changes in Photoaged Skin
Number of keratinocytes Reduces
Number of fibroblasts Reduces
Epidermal cells Get flattened
Number of Langerhans cells and melanocytes Decreases
Lymphatic channels of dermis Dilates
Collagen and Elastic fibers Reduces
Fat content Loses and redistributes
Pigmented cells Overactive causing blotches of hyperpigmentation
PHOTOPROTECTIVE FORMULATIONS
Commonly used cosmetics have low affinity to the skin
and have little percutaneous absorption. The conventional
cosmetics show little efficiency as a cosmetic. Novel tech-
nology has shown great potential for improving the effec-
tiveness and efficiency of delivery of nutraceuticals and bio-
active compounds. Recent advances in nanotechnology show
their promise as potential cosmetics for poorly soluble,
poorly absorbed and labile herbal extracts and phytochemi-
cals. An innovative approach can improve both the aesthetics
and performance of a cosmetic product. The application of
novel approaches can also improve its efficacy regarding
continuous action of herbs on the human body [17]. The
formulation and selection of approach to be used for herbal
cosmetics will depend upon purpose of preparation that is for
topical or systemic effect, inherent properties of drug or herb
extract such as hydrophilic or hydrophobic; surface charac-
teristics of a system like permeability and charges; degree of
biodegradability, biocompatibility, toxicity; release profile,
size of the product required and antigenicity of the final
product [18].
The novel approaches that could be used include Micro-
emulsions [19-21], multiple emulsions [22-24], liposomes
[25, 26], phytosomes [27-32], transfersomes [33-39] noe-
74 The Open Natural Products Journal, 2009, Volume 2 Chanchal and Swarnlata
mulsions [40] multiple nanoemulsions [41], nanocrystals
[42], cubosomes [43] and transdermal Delivery System [44].
EVALUATION PARAMETERS OF PHOTOPROTEC-
TIVES
Erythema Determination
Erythema can be determined by investigating the his-
tological , ultrastructural, biochemical and immunological
effects of UV radiation on skin and its relationship to photo-
damage and skin cancer.
Method
Hairless mouse model could be used for photo protection
studies. Prior to experimentation four hairless mice are anes-
thetized (using ketamine) and a rectangular area approxi-
mately 2.5 cm x 4 cm is marked off on the dorsal area of
each animal. Then sunscreen formulations are applied and
one mice is left as control mice which is untreated. After 15
min drying period, ultraviolet radiation are produced by a
planar array of two UV- A 340 fluorescent lamps which
stimulate UV radiation present in sunlight from wavelength
295 nm to 365 nm. Irradiance could be measured using
Erythema UV A and UV B Intensity meter and minimal
erythemal dose (MED) is calculated. One MED is defined as
the amount of UV radiation necessary to cause a slight red-
dening of the skin 24 hr after exposure. For hairless mouse
one MED is approximately 140 m J / cm
2
[45].
Lipid Damage Determination
UV radiation induces the formation of reactive oxygen
species resulting in damage to various components of skin
like lipid damage which is oxidative degradation of unsatu-
rated free fatty acids and cholesterol. It is observed that UV
exposure decreases lipid melting temperature of the mouse
skin and that application of sunscreens prior to UV radiation
would reduce this epidermal damage.
Method
Immediately following UV exposure, mice are sacrificed
by carbondioxide asphyxiation and full thickness, dorsal skin
is removed by blunt dissection. The epidermis is separated
from the full thickness skin by placing the skin dermis side
down on filter paper saturated with 2.5 % (w/v) trypsin solu-
tion. After storage at 37 C for 4 hr, epidermal sheets are
gently lifted from the skin using forceps and then covered
with fresh trypsin solution and stored at 37 C for 1 hr. Re-
move trypsin from epidermal sheets with gentle rinsing using
deionized water. Epidermal samples are stored at room tem-
perature and 75 % relative humidity overnight. Then 10 mg
samples of epidermis are sealed in aluminium pans and ana-
lyzed using Differential scanning colorimeter. Scan the sam-
ples at a heating rate of 5 C per min from 10 C to 80 C
with a temperature modulation of 0.759 C per min and de-
termine the lipid melting temperatures [45].
Edema Determination
Inflammation is acute biological response to UV radia-
tion. The vasodilatation of cutaneous blood vessels results in
erythema (reddening) and edema (swelling). The treatment
reduces this edema thus it is also an evaluation parameter for
photoprotectives.
Method
Immediately prior to irradiation, the thickness of skin
folds, at the back of the neck of two sedated mice are meas-
ured using a spring loaded pocket thickness gauge. Three
measurements are taken for each mouse and these data are
used as the baseline. Twenty four hours post- UV exposure,
mice are sacrificed by carbondioxide asphyxiation and skin
fold thickness is measured. Edema is calculated by the dif-
ference in skin fold thickness between the baseline and post-
UV exposure data [45].
Sunburn Cell Count
Objective
Sunburn cells are apoprotic keratinocytes that have ab-
sorbed a lethal dose of UV radiation and have been observed
in humans, mice, rabbits and guinea pigs. They are indica-
tion of acute photodamage.
Method
After measurement of postexposure edema , UV exposed
dorsal skin of each mouse is removed and fixed in 10 %
formalin solution. two nonsequential sections of the skin are
removed and mounted to a slide and Hematoxylin and Eosin
stained. The stained samples are then subjected to micro-
scopic examination (600X) and the number of sunburn cells
per linear centimeter are calculated. Counts are done on 1.5
cm sections of interfollicular epidermis [45].
SPF Determination
SPF by definition is determined in vivo as the increase in
exposure time required to induce erythema. Ratio of UV
doses protected to unprotected gives the SPF. The in vitro
method measures the reduction of the irradiation by measur-
ing the transmittance after passing through a film of product
[46].
Method
The most common invitro technique involves measuring
the spectral transmittance at UV wavelengths from 280 nm
to 400 nm. The invitro SPF is calculated as follows:
400 nm
SPF =
E
. S
. d
200 nm
-------------------
400 nm
E
. S
. T
200 nm
where,
E = CIE erythemal spectral effectiveness
S = solar spectral iradiance
T = spectral transmittance of the sample
Quantification of UV Induced DNA Damage
To estimate whether the application of the test formula-
tion exhibits a protective effect on DNA lesions.
Herbal Photoprotective Formulations and their Evaluation The Open Natural Products Journal, 2009, Volume 2 75
Method
The test formulations are applied to volunteers twice
daily. After a two week treatment three test areas are estab-
lished on the inner forearms of every volunteer and marked
with a stencil. Five and 24 hr prior to isolation of suction
blister epidermis, two areas on every forearm are irradiated
with 1.2 minimal erythemal dose solar simulated radiation.
The third area is not irradiated and used as a control. One
forearm is treated as described above; the colateral forearm
is left untreated. To assess DNA damage by single-cell gel
electrophoresis (Comet assay), epidermal keratinocytes are
isolated fromsuction blister epidermis and embedded in low
gelling agarose gels [47].
Skin Viscoelasticity Determination
To determine effects of a treatment with the test formula-
tion on skin firmness.
Method
Two test areas are marked on the forearms of the volun-
teers. One test area is treated twice daily with the test formu-
lation; the second is left untreated and used as a control. At
the baseline visit and after 1, 2, and 4 weeks of regular use,
skin viscoelasticity is determined using a cutometer. As an ad-
ditional means of control for volunteer compliance, skin mois-
ture is examined using a corneometer [47, 48].
Wrinkle Volume Determination
To determine a decrease in wrinkle volume after treat-
ment with the test formulation.
Method
Volunteers treated the assigned side of the face for 4
weeks twice daily with the test formulation. At the baseline
visit and after 4 weeks of treatment, facial wrinkles in the
crows feet area are evaluated by means of i n vivo topome-
try using phase shift rapid in vivo measuring of human skin
phase induction PRIMOS. The PRIMOS system represents
an established and widely used method to quantify effects on
skin wrinkles [47].
Epidermal Cell Turnover Determination
Thedecrease in corneocyte size is correlated with accel-
erated epidermal turnover.
Method
Three test areas are established on the inner forearms of
each volunteer, and a stencil is used to mark these test areas.
Two areas are treated with the test formulations, and one area
is left untreated and served as additional control. Volunteers
apply the test formulations twice daily (morning and evening)
for 6 weeks. The size of single corneocytes is determined at
the baseline visit and after 4, 5, and 6 weeks of treatment.
Ten to 20 h after application of test samples, measurements
are performed. The determination is carried out by image
analysis of D-Squame
sheets [47].
CONCLUSION
The photoprotective formulation must be such that it is
stable pharmaceutically and is able to reverse some of the
characteristic signs of the chronological aging and pho-
toaging in both skin compartments after topical applications.
Various chemical photoprotectives are available but re-
searches are going for use of more herbal constituents as
photoprotectives and there is need of better evaluation pa-
rameters for those formulations. We have studied above
evaluation parameters but more researches have to be carried
out to validate simple, economic and rapid methods to carry
out efficacy studies of herbal photoprotective formulations.
According to the present scenario there is need for adoption
of new alternative methods to ensure the safety of cosmetic
preparations without or minimum use of animals.
ACKNOWLEDGEMENTS
One of the author wishes to thank AICTE (RPS scheme)
and UGC (Major project), New Delhi for financial support
for this work.
REFERENCES
[1] Afaq, F.; Mukhtar, H. Botanical antioxidants in the prevention of
photocarcinogenesis and photoaging. Exp. Dermatol., 2006, 15,
678-684.
[2] Griffiths, C.E.M.; Maddin, S.; Weidow, O.; Marks, R.; Donald,
A.E.; Kahlon, G. Treatment of photoaged skin with a cream
containing 0.05% isotretinoin and sunscreens. J. Dermatol. Treat.,
2005, 16, 79-86.
[3] Guyer, S.F.; Afaq, F.; Mukhtar, H. Photochemoprotection of skin
cancer by botanical agents. Photodermatol. Photoimmunol.
Photomed., 2003, 19, 56-72.
[4] Ashawat, M.S.; Saraf, S.; Saraf, S. Antisolar activity of R. damne-
sia and T. errecta. Planta Indica, 2005, 2, 26-28 .
Table 3. Bioengineering Methods of Evaluation [47]
S.No. Parameter of Evaluation Instrument Used
1 Skin hydration Corneometer
2 Skin color Chromameter
3 Skin Elasticity Cutometer
4 Barrier Function Assessment Evaporimeter
5 Skin surface lipid measurement Sebumeter
6 Skin roughness and wrinkle Skin visiometer
7 Transepidermal water loss (TEWL) Tewameter
8 Erythema index Reflectance Spectrophotometry using Mexameter
76 The Open Natural Products Journal, 2009, Volume 2 Chanchal and Swarnlata
[5] Bajpai, M.; Parade, A.; Tiwari, S.K.; Prashad, D. Phenolic content
and antioxidant activity of some food and medicinal plants. Int. J.
Food Sci. Nut., 2005, 4, 287-291.
[6] Ashawat, M.S.; Saraf, S.; Saraf, S. Cosmetic potentiality of plant
extracts and natural oils. Biosci. Biotechnol. Res. Asia, 2006, 3,
181-188.
[7] Campos, P.M.B.G.M.; Gianeti, M.D.; Kanashiro, A.; Lucisano,
V.Y.M.; Gaspar, L.R. In vitro antioxidant and in vivo photoprotec-
tive effects of an association of bioflavonoids with liposoluble vi-
tamins. Photochem. Photobiol., 2006, 82, 683-688.
[8] Ashawat, M.S.; Saraf, S.; Saraf, S. Biochemical and histopathological
studies of herbal cream against UV radiation induced damage.
Trends Med. Res., 2007a, 2(3), 135-141.
[9] Ashawat, M.S.; Saraf, S.; Saraf, S. In vitro antioxidant activity of
ethanolic extracts of Centella asiatica, Punica granatum, Glycyr-
rhiza glabra and Areca catechu. Res. J. Med. Plants, 2007b, 1, 13-
16.
[10] Cleaver, J . Defective repair replication of DNA in xeroderma pig-
mentosum. Nature, 1968, 372, 773-775.
[11] Yarosh, D.J .; Klein, A.; Connor, J .; Hawk, E.; Rafel, P.W. The
xeroderma pegmentosum study group: Effect of topically applied
T4 endonuclease V in liposomes on skin cancer in Xeroderma pig-
mentosum: a randomized study. Lancet, 2001, 357, 926-929.
[12] Lods, L.M.; Dress, C.; J hhonson, C.; Scholz, D.B.; Brooks, G.J .
The future of enzymes in cosmetics. Int. J. Cosmet. Sci., 2000, 22,
85-94.
[13] Svobova, A.; Psotova, J .; Walterova, D. Natural phenolics in the
prevention of UV induced skin damage. A Review. Biomed. Pa-
pers, 2003, 147(2), 137-145.
[14] Gasparro, F.P. Sunscreens, skin photobiology and skin cancer: the
need for UVA protection and evaluation of efficacy. Environ.
Health Perspect., 2000, 108(1), 71-78.
[15] Seite, S.; Bredoux, C.; Compan, D.; Zucchi, H.; Lombard,
D; Medaisko, C; Fourtainer, A. Histological evaluation of
atopically applied retinol- vitamin C combination. Skin
Pharmacol. Physiol., 2005, 18, 81-87.
[16] Silva, M.R.; Carneiro, S.C.D.S. Elderly skin and its rejuvenation:
products and procedures for the aging skin. J. Cosmet. Dermatol.,
2007, 6, 40-50.
[17] Deep, C.; Saraf, S. Novel approaches in herbal cosmetics. J. Cos-
met. Dermatol., 2008, 7, 89-95.
[18] Hoet P.H.M.; Irene, B.H.; Oleg, V.S. Nanoparticles- known and
unknown health risks. J. Nanobiotechnol., 2006, 2, 12-27.
[19] Chen, H.; Weiss, J .; Shahidi, F. Nanotechnology in nutraceuticals
and functional foods. Inodtechnology, 2006, 30.06, 30-36. Avilable
from: http://www.ift.org
[20] Carlotti, M.E.; Gallarate, M.; Rossatto, V. O/W microemulsion as a
vehicle for sunscreens. J. Cosmet. Sci., 2003, 54(5), 451-462.
[21] Gallarate, M.; Carlotti, M.E.; Trotta, M.; Bovo, S. On the stability
of ascorbic acid in emulsified systems for topical and cosmetic use.
Int. J. Pharm., 1999, 188(2), 233-241.
[22] Khan, A.Y.; Talegaonkar, S.; Iqbal, Z.; Ahmed, F.J .; Khar, R.K.
Multiple emulsions: an overview. Curr. Drug Deliv., 2006, 3(4),
429-443.
[23] Okochi, H.; Nakano, M. Preparation and evaluation of w/o/w type
emulsions containing vancomycin. Adv. Drug Deliv. Rev., 2000,
45, 5-26.
[24] Raynal, S.; Grossiord, J .L.; Seiller, M.; Clausse, D. A topical
w/o/w multiple emulsion containing several active substances:
formulation, characterization and study of release. J. Cont. Rel.,
1993, 26, 129-140.
[25] Niemiec, S.M.; Ramachandran, C.; Weiner, N. Influence of non-
ionic liposomal composition on topical delivery of peptide drugs
into pilosebaceous units: an in vivo study using the hamster ear
model. Pharm Res., 1995, 12(8), 1184-1188.
[26] Cevc, G. Lipid vesicles and other colloids as drug carriers on the
skin. Adv. Drug Deliv. Rev., 2004, 56(5), 675-711.
[27] Bombardelli, E.; Cristoni, A.; Morazzoni, P. Phytosomes in func-
tional cosmetics. Fitoterpia. LXV, 1994, 5, 387-389.
[28] Bombardelli, E.; Cum, S.B.; Loggia, R.; Della, N.; Del, P.; Tubaro,
A.; Gariboldi, P. Complexes between phospholipids and vegetal
derivatives of biological interest. Fitoterpia, 1989, 60, 1-9.
[29] Loggia, R.D.; Sosa, S.; Tubaro, A.; Morazzoni, P.; Bombardelli, E.;
Griffin, A. Anti-Inflammatory activity of some Gingko biloba con-
stituents and of their phospholipids- complexes. Fitoterapia, 1996,
3, 257-273.
[30] Yanyu, X.; Yunmei, S.; Zhipeng, C.; Qineng, P. The preparation of
silybin- phospholipid complex and the study on its pharmacokinet-
ics in rats. Int. J. Pharma., 2006, 307, 77-82.
[31] Franco, P.G.; Bombardelli, E. Complex compound of bioflavonoids
with phospholipids, their preparation and use and pharmaceutical
and cosmetic composition containing them. US Patent, EPTO no.
EP0275005, 1988, 6-14.
[32] Gupta, A.; Ashawat, M.S.; Saraf, S.; Saraf, S. Phytosome: a novel
approach towards functional cosmetics. J. Plant Sci., 2007, 2(6),
644- 649.
[33] Benson, H.A. Transferosomes for transdermal drug delivery.
Expert Opin. Drug Deliv., 2006, 3(6), 727-737.
[34] Cevc, G. Drug delivery across the skin. Expert Opin. Investig.
Drugs, 1997, 6(12), 1887-1937.
[35] Schmid, D.; Zulli, F. Role of beta endorphin in the skin. Int. J.
Appl. Sci., 2005, 4, 131-134.
[36] Pople, P.V.; Singh, K.K. Development and evaluation of topical
formulation containing solid lipid nanoparticles of vitamin A.
AAPS Pharm. Sci. Tech., 2006, 7(4), Article 91, E1-E7.
[37] Wissing, S.A.; Muller, R.H. The influence of solid lipid nanoparti-
cles on skin hydration and viscoelasticity in vivo study. Eur. J.
Pharm., 2003, 56(1), 67-72.
[38] Souto, E.B.; Muller, R.H.; Gohla, S. A novel approach based on
lipid nanoparticles (SLN) for topical delivery of alpha- lipoic acid.
J. Microencapsul., 2005, 22(6), 581-592.
[39] Wissing, S.A.; Muller, R.H. Cosmetic applications of solid lipid
nanoparticles. Int. J. Pharm., 2003, 254(1), 65-68.
[40] Zulli, F. Preparation and properties of Coenzyme Q10 nanoemul-
sions. Cosmet. Sci. Technol., 2006, 1, 1-7.
[41] Merisko, L.E.; Liversidge, G.G.; Cooper, E.R. Nanosizing: a for-
mulation approach for poorly-water-soluble compounds. Eur. J.
Pharm. Sci., 2003, 18(2), 113-120.
[42] Da, Y.; Bruce, A.; Seth, R.M. Cubic liquid-crystalline nanoparti-
cles. J. Nanoparticle Res., 2002, 4(4), 297-311.
[43] Embil, K.; Nacht, S. The microsponge delivery system(MDS): a
topical delivery systemwith reduced irritancy incorporating multi-
ple triggering mechanisms for the release of actives. J. Microen-
capsul., 1996, 13(5), 575-588.
[44] Chadawar, V.; Shaji, J . Microsponge delivery system. Curr. Drug
Deliv., 2007, 4(2), 123-129.
[45] Felton, L.A.; Wiley, C.J .; Godwin, D. Influence of cyclodextrin
complexation on the in vivo photoprotective effects of oxybenzone.
Drug Dev. Indust. Pharm., 2004, 30, 95-102.
[46] Pissawini, M.; Ferrero, L. In vitro determination of Sun protection
Factor. Bus. Brief. Glob. Cosmet. Manuf., 2004, 2, 1-5.
[47] Knott, A.; Koop, U.; Mielke, H.; Reuschlein, K.; Peters, N.; Muhr,
G.M.; Lenz, H.; Wensorra, U.; J aspers, S.; Kolbe, L.; Raschke, T.;
Stb, F.; Wenck, H.; Gallinat, S. A novel treatment option for
photoaged skin. J. Cosmetic Dermatol., 2008, 7, 15-22.
[48] Ashawat, M.S.; Saraf, S.; Saraf, S. Preparation and characterization
of herbal creams for improvement of skin viscoelastic properties.
Int. J. Cosmet. Sci., 2008, 30(3), 183-193.
Received: December 31, 2008 Revised: March 07, 2009 Accepted: March 12, 2009
Chanchal and Swarnlata; Licensee Bentham Open.
This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License
(http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the
work is properly cited.
Você também pode gostar
- Compendium of Medicinal and Aromatic Plants Volume 1Documento129 páginasCompendium of Medicinal and Aromatic Plants Volume 1Pasha Urr90% (10)
- Riches of The Forest - For Health Life and Spirit in AfricaDocumento128 páginasRiches of The Forest - For Health Life and Spirit in AfricaDesy M WenasAinda não há avaliações
- Terpene Biosynthesis PDFDocumento42 páginasTerpene Biosynthesis PDFDella AprilaAinda não há avaliações
- Green TeaDocumento2 páginasGreen TeaDesy M WenasAinda não há avaliações
- Traditional MedicineDocumento22 páginasTraditional MedicineDesy M WenasAinda não há avaliações
- Bisht Et Al 2011 - Amomum Subulatum - Tradisional Phytochemical ActivityDocumento5 páginasBisht Et Al 2011 - Amomum Subulatum - Tradisional Phytochemical ActivityDesy M WenasAinda não há avaliações
- Green Tea and Mouth OdourDocumento6 páginasGreen Tea and Mouth OdourDesy M WenasAinda não há avaliações
- Glycyrrhiza GlabraDocumento8 páginasGlycyrrhiza GlabrarmaganAinda não há avaliações
- Hiora Shinetoothpaste 001Documento5 páginasHiora Shinetoothpaste 001Desy M WenasAinda não há avaliações
- Development and Biological Evaluation of Herbal Anti Acne GelqDocumento4 páginasDevelopment and Biological Evaluation of Herbal Anti Acne GelqWendy FXAinda não há avaliações
- Gabungan Tumbuhan Buat GgiDocumento8 páginasGabungan Tumbuhan Buat GgiDesy M WenasAinda não há avaliações
- The Skin Microbiome: Elizabeth A. Grice and Julia A. SegreDocumento10 páginasThe Skin Microbiome: Elizabeth A. Grice and Julia A. SegreElisa Chaves100% (1)
- Developm Peacock Flower - Anti Wrinkle Formulation - Soisuwan Et Al 2010Documento6 páginasDevelopm Peacock Flower - Anti Wrinkle Formulation - Soisuwan Et Al 2010Desy M WenasAinda não há avaliações
- Gel MangisDocumento6 páginasGel MangisAry SukmaAinda não há avaliações
- 4 EBC0 D 01Documento3 páginas4 EBC0 D 01windiniaAinda não há avaliações
- Skin Microbiome - Looking Back To Move Forward - Kong & SegreDocumento7 páginasSkin Microbiome - Looking Back To Move Forward - Kong & SegreDesy M WenasAinda não há avaliações
- Permeation of Topical Caffeine - Trauer 2009Documento6 páginasPermeation of Topical Caffeine - Trauer 2009Desy M WenasAinda não há avaliações
- Elderly Skin and Its Rejuvenation - Products and Procedures For The Aging Skin - Ramos e Silva Et Al 2006Documento11 páginasElderly Skin and Its Rejuvenation - Products and Procedures For The Aging Skin - Ramos e Silva Et Al 2006Desy M WenasAinda não há avaliações
- Overcoming Stratum Corneum - Modulation of Skin PENETRATION - Trommer & NeubertDocumento16 páginasOvercoming Stratum Corneum - Modulation of Skin PENETRATION - Trommer & NeubertDesy M WenasAinda não há avaliações
- Diffusion Testing Fundamentals - DefinisiDocumento8 páginasDiffusion Testing Fundamentals - DefinisiDesy M WenasAinda não há avaliações
- Alfa Mangostin - Cardiac ProtectionDocumento5 páginasAlfa Mangostin - Cardiac ProtectionDesy M WenasAinda não há avaliações
- TOXICITY STUDYDocumento10 páginasTOXICITY STUDYDesy M WenasAinda não há avaliações
- Photo-Aging - A Literature Review - Limpiangkanan 2010Documento5 páginasPhoto-Aging - A Literature Review - Limpiangkanan 2010Desy M WenasAinda não há avaliações
- Efk Carica Papaya On Healing Burn WoundDocumento9 páginasEfk Carica Papaya On Healing Burn WoundDesy M WenasAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Gps Vehicle Tracking System ProjectDocumento3 páginasGps Vehicle Tracking System ProjectKathrynAinda não há avaliações
- Shapes FlashcardsDocumento5 páginasShapes FlashcardsHome Organising by JRAinda não há avaliações
- GSM Modernization Poster2Documento1 páginaGSM Modernization Poster2leonardomarinAinda não há avaliações
- Enviroclean 25 LTRDocumento1 páginaEnviroclean 25 LTRMaziyarAinda não há avaliações
- Lesson 1 - Simple StressDocumento5 páginasLesson 1 - Simple StressJohn Philip NadalAinda não há avaliações
- Three Bucket Method & Food ServiceDocumento4 páginasThree Bucket Method & Food Servicerose zandrea demasisAinda não há avaliações
- Cars Ger Eu PCDocumento157 páginasCars Ger Eu PCsergeyAinda não há avaliações
- Fajar Secondary Sec 3 E Math EOY 2021Documento16 páginasFajar Secondary Sec 3 E Math EOY 2021Jayden ChuaAinda não há avaliações
- IIT2019 RIT-1-CPM Chemistry TestDocumento15 páginasIIT2019 RIT-1-CPM Chemistry TestPRAKHAR GUPTAAinda não há avaliações
- BMW Mini COoper Installation InstructionsDocumento1 páginaBMW Mini COoper Installation InstructionsEdiJonAinda não há avaliações
- Causes and Effects of PollutionDocumento6 páginasCauses and Effects of PollutionNhư NgọcAinda não há avaliações
- Appendix C: Time Value of MoneyDocumento15 páginasAppendix C: Time Value of MoneyrockerAinda não há avaliações
- BELL B40C - 872071-01 Section 2 EngineDocumento38 páginasBELL B40C - 872071-01 Section 2 EngineALI AKBAR100% (1)
- Knowing Annelida: Earthworms, Leeches and Marine WormsDocumento4 páginasKnowing Annelida: Earthworms, Leeches and Marine WormsCherry Mae AdlawonAinda não há avaliações
- 4 Ideal Models of Engine CyclesDocumento23 páginas4 Ideal Models of Engine CyclesSyedAinda não há avaliações
- Print Date:: Container No NO Size Seal No Seal Party Supplier Status Movement TypeDocumento3 páginasPrint Date:: Container No NO Size Seal No Seal Party Supplier Status Movement TypeYudha PermanaAinda não há avaliações
- MPC-006 DDocumento14 páginasMPC-006 DRIYA SINGHAinda não há avaliações
- Uji Deteksi Biofilm Dari Isolat Klinik Kateter Urin Bakteri Entercoccus Dibandingkan Dengan Tube MethodDocumento27 páginasUji Deteksi Biofilm Dari Isolat Klinik Kateter Urin Bakteri Entercoccus Dibandingkan Dengan Tube MethodIyannyanAinda não há avaliações
- IITG MA101 Endsem Question PaperDocumento12 páginasIITG MA101 Endsem Question PaperNarravula Harshavardhan100% (2)
- Termites and Microbial Biological Control StrategiesDocumento30 páginasTermites and Microbial Biological Control StrategiesMuhammad QasimAinda não há avaliações
- Tyfo SDocumento2 páginasTyfo SAndi AsAinda não há avaliações
- II Unit - End EffectorsDocumento49 páginasII Unit - End EffectorsGnanasekarAinda não há avaliações
- كونكت بلس - 2 ابتدائي - ترم 1 - مذكرة 2Documento86 páginasكونكت بلس - 2 ابتدائي - ترم 1 - مذكرة 2cafubodoAinda não há avaliações
- Function and Euqations - Quantitative Aptitude Questions MCQDocumento4 páginasFunction and Euqations - Quantitative Aptitude Questions MCQAnonymous v5QjDW2eHxAinda não há avaliações
- Director's Report Highlights Record Wheat Production in IndiaDocumento80 páginasDirector's Report Highlights Record Wheat Production in Indiakamlesh tiwariAinda não há avaliações
- Myths of Greece and Rome PDFDocumento247 páginasMyths of Greece and Rome PDFratheesh1981Ainda não há avaliações
- Navmesh Plus: How ToDocumento7 páginasNavmesh Plus: How TobladimirAinda não há avaliações
- ARES SC4 Service Manual (HP-300UA)Documento20 páginasARES SC4 Service Manual (HP-300UA)mike_net8903Ainda não há avaliações
- Electrical EngineerDocumento3 páginasElectrical Engineer12343567890Ainda não há avaliações
- Vrio Analysis Slide Template 16x9 1Documento8 páginasVrio Analysis Slide Template 16x9 1Alt HrishiAinda não há avaliações