Escolar Documentos
Profissional Documentos
Cultura Documentos
Esophagus and Stomach Notes
Enviado por
lizzy5960 notas0% acharam este documento útil (0 voto)
69 visualizações15 páginasSurgical Cases Review
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoSurgical Cases Review
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
69 visualizações15 páginasEsophagus and Stomach Notes
Enviado por
lizzy596Surgical Cases Review
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 15
B. Belingon Notes from case session & case session slides, Annas notes (Dr.
. Esterl), Beckys notes (Dr. Sideman)
Week 3 Esophagus & Stomach M 07.15.13
A 45 year old male presents to your office with a 4 month history of epigastric pain. There is no radiation of
pain. He often has a bad taste in the mouth. The pain worsens after he eats a big meal. The pain worsens
when he is in a supine position after a big meal. He denies frequent nausea or vomiting. He denies frequent
vomiting of undigested food. Alcohol, tobacco and caffeine worsen the pain. He has tried over the counter
antacids over the last 4 months but he has only slight improvement in symptoms. He has no previous cardiac
history. He occasional wakes from sleep with a coughing spell. He has gained 30 pounds over the last 4
month period because of a new stressful but sedentary job. The vital signs are stable. On physical
examination his abdomen is soft, obese and nondistended with normal bowel sounds. The rectal exam shows
no masses but is occult blood positive.
DDx: GERD, peptic ulcers can have hemoccult positive stools with both; also achalasia, Barretts,
diverticulum of esophagus, gastritis, hepatitis, pancreatitis, GB dz
Dx: GERD (primarily dx by good history)
o Gastric contents reflux into the esophagus
o Heartburn, regurgitation, dysphagia, waterbrash (:spontaneous appearance in the mouth of a
slightly sour or salty fluid)
o Atypical symptoms cough, wheezing, chest pain, hoarseness, dental erosions, pharyngitis (pulm
presentation)
o Affects more than 40% of U.S. population at least once per month, 20% once per week, 7% daily
o Contributing factors
Diminished LES function (primary factor)
Impaired esophageal clearance
Increased gastric acidity
Diminished gastric emptying
Hiatal hernia (high incidence of reflux dz pts w hiatal hernia)
o Worsens sx: tobacco, caffeine, alcohol, peppermint, chocolate, fatty foods
o Extra-esophageal manifestations Dental erosions, laryngeal (laryngitis, polyps, cancer,
hoarseness, stenosis), pulmonary (chronic cough, asthma, bronchitis, fibrosis), reactive airway dz,
recurrent pneumonia
KIDS failure to thrive
o Complications of GERD: reflux esophagitis, ulcers, strictures, Barretts disease, malignancy
Workup
o Trial of PPI
o Barium swallow (gastrografin or barium to look for mucosal abnormalitiesonly use
gastrografin when suspect an intra-abdominal perforation b/c barium has risk of adhesions
obstruction; barium is better for pulm b/c less inflammatory; gastrografin much more toxic to
lungs can cause chemical pneumonitis)
o Endoscopy (EGD = esophagogastroduodenoscopy): more useful for eval of GERD complications
Biopsy (ex. Barretts)
o 24 hr pH monitor: *gold standard* quantifies # and duration of reflux episodes, differentiates
upright & supine events; correlates events w subjective sx
o Manometry: assesses peristalsis AND LES pressure; helpful for dx of primary motility d/o
Treatment
o Lifestyle changes (avoid triggers, sleep w head elevated, wt loss, avoid meals 2-3 hrs prior to
sleep)
o Acid suppression (PPI) *gold standard*
LT S/E: change pH in stomach pna or carcinoid tumors
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
Omeprazole or protonics 40 mg/d & bring back in 4-6 wks (real world)
o Surgery
Does patient in this case need surgery? NO.
Indications
Lifelong PPI use (pt wishes to stop meds)
Failure of medical therapy
Complications of GERD not responding to
medical therapy (esophagitis, stricture, barretts)
Paraesophageal hernia assoc w GERD
Pedi indications: FTT, pulm compromise
Anti-reflux procedures: Lap Nissen fundoplication (take
greater curve behind esophagus to create a short, loose
wrap; goal = re-establish length of intra-abdominal esophagus by creating Nissen)
A 42 year old male with a long history of gastroesophageal reflux disease presents to your office with
persistent epigastric pain. He has been on OTC Zantacs for several months with little improvement in pain.
The vital signs are stable. On physical examination his abdomen is soft, obese and nondistended with normal
bowel sounds. The rectal exam shows no masses but is occult blood positive. You perform a barium swallow
which reveals gastroesophageal reflux. You perform 24 hour pH monitoring in the distal esophagus which
confirms gastroesophageal reflux disease. You perform esophagoduodenoscopy which shows long standing
esophagitis. You perform multiple biopsies in the distal esophagus which reveal mild intestinal dysplasia.
Dx: Barretts esophagus
o Change in esophageal mucosa with replacement of the squamous epithelium by columnar
epithelium. (METAPLASIA)
o Dysplasia - Histologic changes that occur before neoplastic Barretts cells become malignant
Classified as low grade dysplasia versus high grade dysplasia
o Can lead to ulcers and strictures; untreated adenocarcinoma of distal esophagus
o Cancer risk is significantly higher in patients with high grade dysplasia
Rate of cancer development for patients with high grade dysplasia in Barretts esophagus
is 4-6%
(Overall cancer risk in patient with Barretts esophagus is 0.5% per year)
Workup
o Mult biopsies along whole extent of esophagus results: mild esophageal dysplasia = Barretts
esophagitis (intestinal columnar metaplasia)
Treatment of high grade dysplasia
o Must confirm by 2 pathologists; esophagectomy if surgical candidate; if not good surgical
candidateq3 month surveillance until carcinoma identified (cancer dev in ~50% pts during f/u)
vs mucosal ablative techniques (can poss miss seeing adenocarcinoma)
Treatment of low grade dysplasia
o Q6-12 mo surveillance; tx w PPI +/- fundoplication
Double-dose PPI (omeprazole 40 mg x 2 per day) (H2 blockers dont have best response
for typical GERD or Barretts)
Repeat upper endoscopy & mult biopsies
Fundoplication (can do early in disease process) + max dose PPI therapy can halt or
reverse Barretts and prevent progression to adenocarcinoma
A 42 year old female describes a 2 month history of progressively worsening dysphagia. She denies any
previous medical or surgical history. She has no cardiac symptoms. She takes no OTC or prescription
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
medications. The vital signs are stable. The lungs are clear. The heart has a regular rate and rhythm with
no gallops, rubs or clicks. The abdomen is soft and nondistended with no masses or hernias. The bowel
sounds are normal.
Next step?
o Barium swallow (results = sigmoid-shaped esophagus that ends
in birds beak; air-fluid level can indicate sm bowel
obstruction)
Least invasive, least expensive
Potential for perforation if dont do barium swallow
first; use gastrografin
Dx: Achalasia
o Failure of the LES to relax
o Progressive esophageal dilation and dysphagia (liquids then solids)
o Typically middle-aged women w no other history
o Dx with manometry
Hypertensive LES, failure of LES to relax, esophageal aperistalsis, elevated lower
esophageal baseline pressure
o What infectious dz process can cause exact same pathology? Chagas (Trypanosoma cruzi)
Workup
o EGD
Goal to rule out cancer or pseudoachalasia, ensure no masses causing compression
Dont actually need endoscopy to rule in achlasia
Treatment
o Pneumatic dilation of LES (slight balloon through scope and inflate)
o Botox injection
o Heller myotomy *surgery of choice* - longitudinal incision thru muscle of L chest, tight O-
shaped circle, makes a C, cant contract as before; minimally invasive
o Medications dont usually work (nitrates, CCB)
A 55 year old male with a long history of alcohol disease presents to the Emergency Department with left
chest pain and upper abdominal pain after a severe episode of violent vomiting. The vital signs are temp 103,
P 130, RR 34 and BP 90/60. The neck and left chest wall have crepitus. The left chest is dull to percussion
with decreased breath sounds and vocal fremitus. The abdomen is soft, distended and slightly tender with
decreased bowel sounds.
Dx: Boerhaaves syndrome
o Spontaneous rupture of esophagus
o Present w acute onset chest pain, fevers,
usually after episode of retching/vomiting
o Physical exam finding: crepitus of chest or
neck (may be the only phys finding)
o Dx w CXR (pneumomediastinum or L
pleural effusion d/t disruption of
mediastinal pleura) or contrast
esophagram (use water sol contrast =
gastrografin =/= barium)
Can also give secondary findings
(atelectasis)
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
Patient is unstable: hypotension, tachycardia, fever
(indicates SIRS or early septic shock once have a
source can call septic shock); source? Ruptured
esophagus secondary to significant episode of
retching/vomiting
ABCs
o Listen to breath sounds (decr breath sounds,
vocal fremitus, dull to percussion), can get a
CXR but this is an acute setting, can put chest
tube in OR
o Resuscitate for shock (large bore IV, 1-2L
fluids for septic shock; can give pressors as
support but appropriate only if have enough
volume (preload!!!)
o How do you know when adequately
resuscitated? CVP (Nl 4-6)incr until about 7-
11 or so; can also put in Foley to monitor UOP
o Can also give early intervention (pre-op) w broad-spectrum Abx (shown to decr mortality) to
cover mouth flora feed thru jejunostomy
Labs: CBC chem, LFTs, amylase/lipase (alcoholic hx), T & C for blood
Treatment
o Surgical emergency!!!
15% mortality w/i 24 hrs, 45% mortality > 24 hrs
Die from mediastinitis d/t leakage into mediastinum
MCC of perforation? Iatrogenic; perforates in L chest b/c of esophageal
shift
After 24 hrs, tissue is too friable to handle sutures so divert (gastrostomy,
spit fistula, chest tube)
Mucosal injury may be larger than muscle injury primary closure of mucosal
injury; staple off cardia of stomach; esophagus doesnt seal well (b/c lacks serosa)
buttress w any tissue nearby; drain widely (if you think you need 1 chest tube, put
in 2; if you think you need 5 chest tubes, put in 10)
o Drainage, debridement (may have intense inflammatory response from contaminated saliva in
other organs in chest/stomach), repair, diversion
o If pt presents 48 hrs post perforation lots of inflammation unable to stent
Take to OR and resect distal esophagus, give spit fistula on neck for saliva; staple off
cardia of stomach; stabilize
Reconstruct esophagus in 1 yr using stomach or colon for reconstruction
A 27 year old otherwise healthy male presents to your clinic with a history of regurgitation of undigested
food. He sometimes wakes from sleep with uncontrollable coughing spells. His girlfriend states that he has
worsening bad breath. The vital signs are stable. The lungs are clear. The heart has a regular rate and
rhythm. The abdomen is soft, nondistended and nontender with normal bowel sounds.
Dx: Zenkers Diverticulum
o Dysfunction of the cricopharyngeus leads to mucosal herniation
o Sx: Dysphagia, regurgitation of undigested food, halitosis, possibly aspiration and pneumonia
o Food stasis in diverticulum w bacterial overgrowth
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
o Diagnosed with modified barium swallow
(anatomical study b/c anatomical problem!)
Diverticulum usually on L side
Dont need manometry or upper
endoscopy (scope may get stuck or
perforate)
Is this a typical Zenkers pt? No, usually theyre older
Treatment
o Diverticulectomy
o Cricopharyngotomy
o Proximal myotomy done on constrictors
separate distal muscle as far down as possible
Vs. achalasia distal myotomy
**Compare & contrast Zenkers w epiphrenic diverticulum
A 55 year old male with a history of 2 DUI offenses is required by the court to attend an outpatient alcoholic
support group for 1 year, to perform 40 hours of community service and to take antabuse to avoid alcohol
consumption. He relapses, consumes alcohol while on antabuse and develops acute violent emesis. With his
fourth episode of emesis he develops massive painless hematemesis. He has never had a previous history of
hematemesis. His vital signs include temp 100, P110, RR 22 and BP 110/70. He appears malnourished. The
lungs are clear. The heart shows mild tachycardia but no gallops, rubs or clicks. The abdomen is soft and
nondistended with no masses or hernias. The bowel sounds are normal. There are no signs and symptoms of
cirrhosis. You place supplemental oxygen and 2 large bore IV catheters into the upper extremities.
DDx (upper GI bleed): esophageal varices, perforated ulcer, stress
gastritis, submucosal vessel bleeding (Dieulafoys lesion), Boerhaaves
Dx: Mallory-Weiss Tear
o Mucosal tear after vomiting causes upper GI bleed
(disrupts blood vessels under mucosa vs. Boerhaavas full-
thickness tear)
o Tear usually almost always at GE junction
o Usually self-limited
o Painless hematemesis!
ABCs: resuscitate!!! w large bore IVs, T&C blood (dont need H&H)
Treatment
o Most bleeding stops w resuscitation (medical management)
o Inject w epi to vasoconstrict, or cauterize
o Can have PPI, ocreotide, or somatostatin drip
o Endoscopic treatment (for dx or to control bleeding)
o Rarely requires surgical treatment (explore stomach, can do blind figure 8 sutures around tears; get
vascular to embolize; or get interventional radiology angioembolization of any bleeders)
Massive upper GI bleeding from liver dz variceal hemorrhage need to intubate, marked resuscitation,
full laps, do upper endoscopy; tx = banding, PPI & ocreotide continuously for 12 days
o If still bleeding w marked hematemesis do another upper endoscopy, band where appropriate
o Still bleeding control acute hemorrhage w temporizing measures NG lavage to confirm
upper GI source (SB tube: tube w gastric balloon holding 500 cc w esophageal balloon holding 50
cc) put down nasogastric groove
KUB to make sure balloon below diaphragm to avoid perforation pressure stops
bleeding
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
NG tube proximal to esophageal tube to collect blood
Can do operative procedure (TIPS or porto-caal shunt) good for pts getting more
definitive procedure later (liver transplant)
o Best tx = liver transplant
A 45 year old male presents to your office with vague chest pressure. The pain is substernal in location and
dull in nature with no radiation to the back, neck or arms. He describes frequent early satiety. He describes
frequent gaseous eructations, nausea and vomiting. He denies cough. He denies history of gastroesophageal
reflux disease. He denies previous cardiopulmonary history. The vital signs are temp 98, P 90, RR 22 and BP
130/70. The lungs are clear to auscultation and percussion. The heart has a regular rate and rhythm with no
gallops, rubs or clicks. The abdomen is soft and nondistended but with slight epigastric tenderness. The
rectal exam shows no masses but is trace occult positive.
Dx: Paraesophageal hiatal hernia
o Types Confirm type w barium swallow (barium better to see
motility)
Type I: Sliding (most common, can move betw abd and
thorax; wont see on CXR)
Type II: Paraesophageal (esophagus in anatomical
position [GEJ in correct location] but part of stomach
herniates adjacent to esophagus; CXR shows large
gastric bubble in retrocardiac area/behind heart)
Type III: Combo I & II
o Sx: GERD, epigastric discomfort, post-prandial bloating, dysphagia
o Complications: ulceration anemia, strangulation (esp w paraesophageal)
Incarceration: something protrudes thru hernia & gets stuck; strangulation: compromised
blood flow
Workup
o Guaiac (+) = ischemia until proven otherwise
o Upper endoscopyto reveal degree of ischemia
o CT scan (look for other organs that herniated)
o Check blood flow w fluorescence or Doppler
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
Treatment
o Surgical emergency b/c complications include stomach becoming ischemic and perforating
o Indications: Symptomatic, or if stomach in chest
o Laparoscopic paraesophageal hernia repair +/- mesh
o Reduce stomach, repair hiatus, add fundoplication; empty stomach contents
o Put in G-tube, resect hernia sack, close crura behind stomach, secure diaphragm to prevent repeat
herniation
A 35 year old male attempts suicide by ingestion of the caustic alkaline liquid agent Drano. He presents to
the Emergency Department at University Hospital with drooling, and substernal chest pain. The vital signs
are temp 101, P 110, RR 28 and BP 116/60. He appears uncomfortable and diaphoretic. He has no
crepitance in the neck. The heart has tachycardia but no gallops, rubs or clicks. The breath sounds are equal
bilaterally. The abdomen is soft and nondistended with no masses. The rectal examination shows no masses
but is trace guaiac positive.
Dx: Caustic esophageal injury
o Alkalis: cause liquefactive necrosis, deep penetration & perforation (worse than acids)
o Acids: coagulation necrosis involving eschar formation, limited depth of injury
Escar formation shields deeper tissue from injury
o DO NOT induce vomiting (just re-exposes mucosa to caustic agent), dilute with water
o Degree
1
st
: mucosal hyperemia and edema
2
nd
: limited hemorrhage, exudate ulceration, pseudomembrane
3
rd
: deep ulcer, perforation, obstruction of lumen, massive bleeding
Workup
o EGD within 24 hrs admission if discover full thickness injury, pre-emptively go to surgery
o Gastrografin swallow (assess for perforation even if no clinical suspicion)
o Give Abx only if suspect esophageal perforation b/c of nature of injury, can progress to full
thickness involvement of esophagus
o
Treatment
o Supportive care
Assess airway do you need to intubate? Consider intubation if pt has lots of secretions
that cant clear
IV fluids
NG tube (radiologic guided)
Large volume resuscitation
TPN vs feeds
o Surgery for full thickness necrosis or perforation
Esophagogastrectomy
Esophagostomy
FJC
Prognosis: good for minor burns; chronic strictures for moderate ingestions (need surgery)
Different scenario: suicide attempt w Drano; presents w tachycardia, equal breath sounds, no crepitus,
mild epigastric pain could have liquefactive necrosis, looks like Boerhaaves
o Tx: resuscitation as much as possible, dont feed; if necessary, gently put down NG tube; do
gastrografin swallow; resection if perforation (happens w/i hrs); if no perforation gentle upper
endoscopy to see burns & stop when see first major burn (textbook) [real world: scope through to
2
nd
portion of duodenum)
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
o Can still progress to perforation perforation can lead to stricture
o Dx stricture w upper GI swallow; do upper endoscopy to look for tumor if see stricture (need to
r/o) tx stricture w dilation
A 5 year old male ingested pool cleaner hydrochloric acid accidently one month ago and developed a
corrosive esophageal injury that was treated nonoperatively. He now presents to the outpatient pediatric
surgery clinic with worsening dysphagia of liquid and solid foods. He has the impression that food gets
stuck in his chest. The vital signs are temp 99, P 100, RR 22 and BP 118/60. He appears comfortable. The
heart has a regular rate and rhythm with no gallops, rubs or clicks. The bilateral breath sounds are equal.
The abdomen is soft and nondistended with no masses. The rectal examination shows no masses and is
guaiac negative.
Workup
o Gastrografin swallow
Imaging shows long stricture
o EGD
Mucosa inflamed (chronically) not
a good salmon pink color
Dx: Chronic esophageal injury (stricture)
o Fibrotic scarring of esophagus from caustic
injury
Treatment
o Bougie dilation
o Surgical resection if:
Complete stenosis, marked irregularity on swallow study, severe reaction to dilation
(esophagitis/mediastinitis), fistula formation, unable to dilate
o Surgical resection w gastric or colonic interposition graft (1
st
choice stomach, 2
nd
choice colon, 3
rd
choice small bowel (jejunum)
A 65 year old male with a long history of cigarette and whisky use presents to your office with progressive
dysphagia for liquid and solid meals. He describes a 20 pound weight loss over 3 months. He describes
vague substernal chest pain. He has occasional nausea and vomiting. He denies previous medical or surgical
history. The vital signs are stable. He appears quite malnourished. The neck has several shotty
supraclavicular lymph nodes. The lungs are clear. The heart has a regular rate and rhythm with no gallops,
rubs or clicks. The abdomen is soft and nondistended with no masses or hernias. The bowel sounds are
normal. The rectal exam shows no masses but is trace occult positive.
Pts age, wt loss, RF of smoke/drink, progressive dysphagia (solid
then liquids) cancer until proven otherwise
Dx: Esophageal cancer
o Mostly during 5
th
-7
th
decade of life
o Men > women
o Smoker & drinker = most common contributing factors
o Progressive dysphagia (solids then liquids)
o Wt loss
Supraventricular LN probably indicates metastatic biopsy w FNA
o FNA (+) = metastatic cancer not resectable b/c its spread & stage its reached not a good
candidate for surgery d/t distal nodal spread tx w chemo/radiation
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
Staging
o Barium swallow then EGD + biopsy
Imaging shows irregular stricture
o Endoscopic ultrasound: determines T stage (depth of invasion)
o CT abdomen & chest for invasion of structures next to
esophagus/metastasis
o Bone scan if bony pain
Histologic types
o Squamous cell, adenocarcinoma
Treatment
o Neoadjuvant chemoradiation (shrink and downstage before surgery)
o Surgical resection
Ivory-Lewis esophagectomy (two stage procedure:
laparotomy for gastric mobilization and tubularization, followed by R thoracotomy for
esophageal resection & reconstruction)
Transhiatal esophagectomy (upper midline laparotomy incision and left neck incision,
pull stomach into the neck; gastric conduit anastomosed to remaining cervical esophagus
above level of clavicles)
Indication: no evidence of tumor spread (tracheobronchial tree, aorta, RLN), no distant
metastasis, patient fit from cardiopulmonary POV
Diff scenario: female w extra-mucosal obstruction (egg-shaped) in wall of esophagus (non-mucosal,
smooth, round lesion) leiomyoma (MC benign lesion) dont do upper endoscopy or biopsy b/c not a
mucosal lesion
o Tx: OR enuclate lesion (pops out like an egg), close lesion, dont biopsy
A 50 year old male presents to your outpatient clinic with a 6 month history of burning epigastric pain. The
patient takes over the counter antacids with some improvement in the epigastric pain. The pain is
occasionally aggravated by a meat laden diet. The vital signs are stable. The lungs are clear and the heart
has a regular rate and rhythm. The abdomen is soft and nondistended with mild epigastric pain on deep
palpation and decreased bowel sounds. There are no peritoneal signs. The liver and spleen are not palpable
and the liver span is 8 cm. The rectal exam shows no lesions but shows trace occult blood.
DDx: PUD, biliary rule out GB: timing of pain (GB typically after
fatty or spicy meals), type of pain (GB usually crampy, comes & goes,
lasts 20 mins to an hr then goes away)
Dx: Peptic ulcer disease (gastric)
o Imbalance between acid production and acid protection in the
stomach
o Spectrum of disease from gastritis to ulcer with perforation
o Risk factors: H pylori infection >> NSAIDs > stress,
smoking, alcohol use
H pylori infection: duodenal >> gastric
o MC complaint: burning epigastric pain
o Gastric ulcers irritated by high protein diet
o Types
I: gastric body, lesser curve; low acid secretion
II: gastric body & duodenal ulcer; high acid
secretion
III: prepyloric region; high acid secretion
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
IV: high on lesser curvature; low acid secretion
V: anywhere; NSAIDs
Workup
o Obstructive series (if see nonspecific bowel gas pattern do a swallow)
o EGD w biopsy (to r/o malignancy)
If just see chronic inflammation bring back in 6 wks to repeat upper endoscopy
o Test for H Pylori
Treatment
o Treat the assoc factors
Triple therapy for H pylori: PPI + amoxicillin + clarithromycin, can sub metronidazole
for amox in PCN-allergy
Remove risk factors (NSAIDs, ASA, smoking)
o Monitor H pylori eradication with breath test
o Confirm ulcer resolution w upper endoscopy (if still there distal gastrectomy)
Complications
o Bleeding, perforation, obstruction (esp > 3 cm size)
Diff scenario Duodenal ulcer work up is the same (obstructive series to r/o perforation or obstruction;
contrast study; EGD), have low likelihood to be cancer, high acid state
o Tx H pylori w triple therapy for 1 wk, put on PPI
Bring back in 6 wk to ensure sx improving; operate if complications (refractory to tx,
perforation, bleeding, inflammation, or inflammation stricture causing gastric outlet
obstruction)
A 75 year old obese diabetic male undergoes a difficult sigmoidectomy and colostomy for perforated sigmoid
diverticulitis. He past medical history is significant for coronary artery disease, for which he takes a beta
blocker and aspirin 325 mg po daily, and for degenerative joint disease, for which he takes ibuprofen 600 mg
po daily. He recovers in the surgical intensive care unit after his sigmoidectomy and colostomy. He is on the
ventilator and has a radial arterial catheter, a Swan Ganz catheter, a urinary catheter and a nasogastric
catheter in position. On the second postoperative day he develops bright red blood from the nasogastric
catheter. The vital signs are temp 100.5, P 68, RR 12 and BP 110/80. The lungs have scattered rhonchi
bilaterally. The heart has a regular rate and rhythm. The abdomen is soft and slightly distended with mild
epigastric tenderness on deep palpation and with decreased bowel sounds. The rectal exam shows no masses
but is occult positive.
Dx: Stress gastritis
o Likely a sequence of events in the critically ill with multiorgan failure
Inadequate blood flow to gastric mucosa
Poor formation of mucosal barriers
Mucosal breakdown
Bleeding
o ASA/NSAIDs set up for gastritis and/or type V gastric ulcers; can also have stress ulcers after
major surgery
Treatment
o PREVENT PREVENT PREVENT (PPI)
o NGT lavage
o If hemorrhagic stress gastritis angiographic embolization vs. endoscopic control of hemorrhage
o Surgical treatment vagotomy and drainage, oversewing of bleeders vs. subtotal gastrectomy
(RARELY GETS TO SURGICAL TREATMENT)
Read about stress gastritis!!
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
A 25 year old male medical student presents to the emergency room with epigastric pain. The pain began
approximately 4 hours ago as severe, persistent epigastric pain. The pain is now becoming more diffuse. The
patient describes some nausea but no emesis. He has never experienced such pain before. He took OTC
Tylenol but there was no relief of pain. He takes no prescribed medication. He smokes a rare cigarette on the
weekend and drinks approximately 6-12 beers every week. His past medical history is unremarkable but
describes his surgical history is significant for bilateral inguinal herniorraphy at age 2 years. The vital signs
are temp 101, P 120, RR 28 and BP 110/60. He looks very uncomfortable and lies motionless in bed. The
lungs are clear. The heart shows tachycardia but no gallops, rubs or clicks. The abdomen is rigid, board-like
with no bowel sounds. The rectal exam shows no masses but is trace occult positive.
Rigid board-like abdomen = peritoneal signs of peritonitis
ABCs resuscitate!
Dx: Perforated duodenal ulcer
o Classic presentation
o Sudden, severe upper abdominal pain (peritoneal signs)
o Onset can be recalled precisely (very sudden)
o Severely distressed patient
o Rigid abdominal muscles
o Duodenal ulcers more prone to perforation than gastric
(duodenal wall more thin than gastric); if gastric ulcer
perforation, suspicious of gastric cancer
Acute abdominal series (3 films)
o Upright CXR subdiaphragmatic air!!! NEED TO
OPERATE
o Flat and upright KUB
Emergent surgery
o Midline incision [exam will show hole in 2
nd
portion of duodenum w minimal contamination]
If unstable, omental (Graham) patch use patch of vascularized omentum, swing up and
position over perforation, then suture it down
o Laparoscopic vs. open repair of perforation (if large, may need to resect area)
o Omental patch (if small)
o High morbidity & mortality w/o surgery
Treatment
o Long term use of PPI
o Triple therapy against H pylori for 1 wk
o Historically, vagotomy and drainage or parietal cell vagotomy (antrectomy) used to be standard
surgical treatment refractory to medical treatment (addresses acid secretion stimulated by
gastrin, histamine, Ach)
Scenario: If pt is bleeding (duodenal ulcer w hemorrhage) pt presents w pale, clammy skin, melenic
bowel movements or hematochezia tx like shock pt (resuscitate, 2 IVs, T&C for blood); diagnostic test =
quick obstructive series to r/o perforation; dx intraluminal hemorrhage w NG tube
o Upper endoscopy (diagnostic and therapeutic) see arterial hemorrhage in second part of
duodenum, r/o intra-abdominal perforation, rule in intra-luminal bleeding
o Tx: triple therapy against H pylori, PPI, control hemorrhage w electrocautery, epinephrine
injection (can do through scope), evacute blood w NG tube
o If do electrocautery & bleed again try electrocautery one more time; after two attempts of
electrocautery or epi injection, then operate: pyloroplasty to access, visualize & control
hemorrhage; truncal vagotomy and antrectomy are larger, more definitive operations
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
Scenario: Obstruction N/V, stricture at duodenum, alkalotic from vomiting
o Dx: EGD to r/o cancer
o Tx for duodenal obstruction d/t ulcer disease = resuscitate, lots of fluid upfront w K+
supplementation
o High acid state pyloroplasty doesnt help stricture; do vagotomy, antrectomy & Billroth II
reconstruction (for retractability; highly selective vagotomy w vagus n still intact so rest of GI
tract works well); Billroth I reconstruction (connect duodenum back to distal stomach)
Scenario: Gastritis w type V gastric ulcer marked hemorrhage, vomiting blood, melenic stools, hx of
NSAID use
o Resuscitate!
o Gastritis: diffuse punctate bleeding all over stomach
o Tx: discontinue offending agent, r/o H pylori, put on PPI; if doesnt resolve total gastrectomy
o Do EGD to ensure not missing anything else
A 45 year old male with a long standing history of duodenal ulcer disease now presents with nausea and
vomiting with every meal. He vomits near totally undigested food. The vital signs are temp 100, P 102, RR 22
and BP 120/70. The abdomen shows some distension and tympany in the left upper quadrant with decreased
bowel sounds. There are no peritoneal signs. The laboratory evaluation shows a hyponatremic,
hypochloremic metabolic alkalosis. The obstructive series shows a dilated stomach with an air-fluid level.
Workup [Whats next?]
o Upper GI series w contrast confirms obstruction (delineated by contrast)
o NG to decompress
o IVF to correct electrolyte abnormality
o DDx for stricture at level of stomach = gastric cancer (r/o w EGD)
If stricture, then confirm no other assoc findings (on EGD)
Dx: Gastric outlet obstruction
o Chronic inflammation and recurrent bouts of acute inflammation leads to fibrosis of the pylorus
o Fibrotic pylorus limits gastric emptying leading to gastric outlet obstruction
o Antrum contains G cells which stimulate acid secretion from parietal cells (located in fundus)
Treatment
o Goal to relieve obstruction and dysphagia
o Endoscopic dilation
o Surgical resection (pylorus too scarred to function)
Vagotomy and antrectomy or highly selective vagotomy and gastrojejunostomy
A 42 year old female with morbid obesity comes to your office with complaints of hypertension, back pain,
joint aches and diabetes. She has tried multiple diets, exercise programs, biofeedback, psychological
counseling and yoga to try to lose weight. Her weight has decreased from 312 to 285 pounds in the last year
but her weight interferes with her employment and with her quality of life. She comes to your outpatient
clinic for advice.
Obesity Surgery
o Morbid obesity assoc illnesses: DJD, Low back pain, HTN, OSA, GERD, Gallstones, Diabetes,
Hyperlipidemia, Asthma, Fatal cardiac arrhythmias, Right sided heart failure, Migraines, Venous
stasis ulcers, DVTs, Stress urinary incontinence, Infertility, Dysmenorrhea, Depression, Increased
cancer risk (uterus, breast, colon, prostate)
o Indications
BMI > 35 w comorbidities, or BMI > 40
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
Must have attempted supervised wt loss programs & willing to change lifestyle
o BMI
Normal: 18.5-24.9
Overweight: 25.0-29.9
Obesity
Mild: 30.0-34.9
Moderate: 35.0-39.9
Severe: > 40
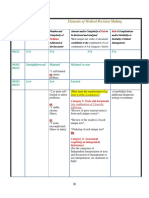
Superobese: > 50
o Types of surgery
Restrictive: Laparoscopic adjustable
gastric banding, sleeve gastrectomy,
vertical banded gastroplasty
Malabsorptive: Biliopancreatic diversion, jejunoileal bypass
Combo restrictive & malabsorptive: Roux-en-Y gastric bypass, BPD w duodenal
switch
A 55 year old male presents to your office with vague epigastric pain and fullness. He describes occasional
nausea and vomiting. He denies frank hematemesis, melena or hematochezia. He describes anorexia and a
15 pound weight loss over 4 months. The vital signs are stable and his current weight is 65 kg. He denies
cigarette or alcohol use. He takes no prescribed medications. He has taken extra strength Tylenol with
minimal improvement in epigastric pain. The lungs are clear and the heart has a regular rate and rhythm
with no gallops, rubs or clicks. The abdomen is soft and slightly distended with slight epigastric tenderness
and with an epigastric mass. The rectal exam shows no masses but is trace positive.
Even if pt had new-onset reflux sx & discomfort in absence of wt loss consider malignancy b/c of age,
could have an early gastric cancer which is not typically symptomatic until more advanced
Workup
o EGD w biopsy
o Endoscopic ultrasound (staging)
o CT scan
o PET scan
Dx: Gastric cancer
o Poor prognosis because usually diagnosed late
At diagnosis, ~ 50% have disease beyond locoregional confines.
Only half of them can undergo a potentially curative resection
o Symptoms Weight loss, persistent abdominal pain.
Dysphagia if proximal
Nausea, early satiety (mass effect or poor distensibility of stomach)
Gastric outlet obstruction
o More prevalent in Asian countries
o Must consider in cases of chronic gastric ulcer
Treatment
o Multimodality
o Surgical resection dictated by location
UNRESECTABLE
Distant metastasis
Invasion of major vascular structures - Aorta, encasement or occlusion of
hepatic artery, celiac trunk, proximal splenic artery
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
Involvement of distant lymph nodes (aorto-caval, pancreatic, mediastinal, portal
hepatis)
o Know who benefits from neoadjuvant chemo vs post-op chemo
A 45 year old male underwent a vagotomy and antrectomy with Bilroth II anastomosis for severe duodenal
ulcer 2 years ago. He presents to your office with severe epigastric pain and diarrhea. The pain is very
similar to his previous ulcer pain. He has taken OTC Zantacs with minimal improvement in pain. The pain
improves slightly with meals. The vital signs are stable. The lungs are clear and the heart shows regular
rate and rhythm with no gallops, rubs or clicks. The abdomen is soft and distended but has moderate
epigastric tenderness on deep palpation. The abdomen shows no hepatosplenomegaly and no hernias. The
bowel sounds are decreased. The rectal exam shows no masses but is trace occult positive. He undergoes an
upper gastrointestinal barium examination which reveals multiple mucosal ulcerations in the jejunal limbs.
DDx for numerous ulcerations in atypical location
o Zollinger-Ellison syndrome caused by gastrinoma
Endocrine tumor that secretes gastrin
Leads to acid hypersecretion and peptic ulcerations
Presenting sx: abd pain, PUD, severe esophagitis
Diagnosis
o Serum gastrin level (> 1000 pg/ml is diagnostic)
o Secretin stimulation test if gastrin level between 200 500
Localize lesion(s)
o CT scan
o If CT scan negative endoscopic ultrasound (more sensitive than CT)
o If EUS negative Octreotide scan detects tumors < 1cm [nuclear medicine]
o If scan negative exploratory laparotomy palpate for lesions, look in duodenum, can do intra-
op ultrasound on pancreas
Most of the time, gastrinoma located in Passaros triangle (gastrinoma triangle)
3 points that define triangle
o 1) confluence of cystic and common bile duct
o 2) junction of 2
nd
and 3
rd
portions of duodenum
o 3) junction of neck and body of pancreas
Treatment
o Take out proximal duodenum and antrum (location of most of acid-producing cells in stomach)
o Billroth II: gastrojejunostomy (stomach and sm bowel sewn together), major complications in
30% of pts Roux-en-Y more common
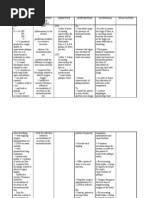
Post-gastrectomy complications of Billroth II (LIKELY TO SEE ON NBME!!!)
Dumping syndrome (Efferent loop syndrome)
o Immediately after eating have to use restroom d/t incr gastric motility
eat frequent, small meals, limit carb intake, meds
Afferent loop syndrome
o Afferent loop has bile; efferent loop from stomach to intestine; happens
w twist or scar that prevents bile from draining from afferent limb;
obstruction of afferent limb usually requires surgery to correct
Bile reflux gastritis (from bile washing back into stomach)
Margin ulceration (ulcer at anastomosis of mucosa)
o Billroth I: pull duodenum and sew onto stomach, doesnt work well, many times wont reach
Diff scenario: Diagnosis if high calcium + gastrinoma? Think PTH
B. Belingon Notes from case session & case session slides, Annas notes (Dr. Esterl), Beckys notes (Dr. Sideman)
MEN 1 Syndrome (pituitary, parathyroid, pancreas) (1
st
MCC parathyroid
adenoma)
MEN 2a: Calcitonin, calcium, catecholamines
Medullary carcinoma of thyroid, pheochromocytoma, hyperparathyroidism (2
nd
MCC)
3
rd
MCC: cancer (< 1% parathyroid carcinoma)
Você também pode gostar
- High Yield Surgery Compatible Version PDFDocumento20 páginasHigh Yield Surgery Compatible Version PDFSurgery CSC1Ainda não há avaliações
- Exam 4Documento10 páginasExam 4Hasan A AsFourAinda não há avaliações
- Surgery Handbook Class of 2017Documento16 páginasSurgery Handbook Class of 2017medstudentAinda não há avaliações
- Obstetrics Cases by Caroline de CostaDocumento9 páginasObstetrics Cases by Caroline de CostaJeffrey HingAinda não há avaliações
- Peds Lecture 3Documento19 páginasPeds Lecture 3Suraj Mukatira100% (1)
- Neurology Notes Syrian StudentDocumento5 páginasNeurology Notes Syrian StudentLiridon SopajAinda não há avaliações
- Divine Intervention Step 2CK Podcasts Notes - Read Only File - Docx (Dragged) 4Documento3 páginasDivine Intervention Step 2CK Podcasts Notes - Read Only File - Docx (Dragged) 4winston1234Ainda não há avaliações
- 3 Comments SHELF Practice Questions Surgery USMLE Step 2 HomeDocumento8 páginas3 Comments SHELF Practice Questions Surgery USMLE Step 2 HomeIndy PhangurehAinda não há avaliações
- MCQ Recall Paper - October 2001Documento33 páginasMCQ Recall Paper - October 2001dr_gentel19Ainda não há avaliações
- Jeopardy Questions OBGYNDocumento4 páginasJeopardy Questions OBGYNjkj;jjAinda não há avaliações
- Fast HugDocumento41 páginasFast HugBharti NaraAinda não há avaliações
- Hematology Oncology Notes Syrian StudentDocumento2 páginasHematology Oncology Notes Syrian StudentLoyla RoseAinda não há avaliações
- Shelf Questions From The CLIPP CasesDocumento54 páginasShelf Questions From The CLIPP CasesJoe Cone100% (1)
- Chapter 015Documento9 páginasChapter 015Christopher EndicottAinda não há avaliações
- Asthma That Disappears Between Ages 6-8 - Bronchioles Grew & Resolved The AsthmaDocumento27 páginasAsthma That Disappears Between Ages 6-8 - Bronchioles Grew & Resolved The Asthmasimonedarling100% (1)
- BluePrint 5th QuestionsDocumento25 páginasBluePrint 5th QuestionsAbuFreihAinda não há avaliações
- Surgery Pretest SummaryDocumento9 páginasSurgery Pretest SummaryPrince DuAinda não há avaliações
- Past QuestionsDocumento116 páginasPast QuestionsYhr YhAinda não há avaliações
- Answers To OB GYN Form 1Documento2 páginasAnswers To OB GYN Form 1b0% (1)
- Gyn QsDocumento198 páginasGyn QsA Fish100% (1)
- UntitledDocumento41 páginasUntitledvioletdeocaresAinda não há avaliações
- جراحه هام جدا PDFDocumento80 páginasجراحه هام جدا PDFAmir AttaAinda não há avaliações
- Assessment of The Acutely Ill PatientDocumento10 páginasAssessment of The Acutely Ill PatientZacmilo Dela TorreAinda não há avaliações
- Nclex ReviewDocumento5 páginasNclex ReviewOncologynAinda não há avaliações
- Peds NBME Form 1 Flashcards - QuizletDocumento14 páginasPeds NBME Form 1 Flashcards - Quizletparth515Ainda não há avaliações
- Apgo & World Study Guide - TPDocumento16 páginasApgo & World Study Guide - TPxx_caligurl_93xxAinda não há avaliações
- HHHHDocumento36 páginasHHHHdger11Ainda não há avaliações
- Aafp QuestionsDocumento6 páginasAafp QuestionsPrince DuAinda não há avaliações
- Obstetrics OverviewDocumento91 páginasObstetrics OverviewAbi TudAinda não há avaliações
- 2003 2008 MCQDocumento81 páginas2003 2008 MCQIshola Segun SamuelAinda não há avaliações
- PaperDocumento112 páginasPaperRight VentricleAinda não há avaliações
- OB OSCE ReviewerDocumento5 páginasOB OSCE ReviewerPao Ali100% (1)
- Group F GYNE MCQDocumento3 páginasGroup F GYNE MCQmarina_shawkyAinda não há avaliações
- Medical Surgical Nursing 4 BulletsDocumento5 páginasMedical Surgical Nursing 4 BulletsQueen ElizabethAinda não há avaliações
- Pharmacology Exam4 ReviewDocumento8 páginasPharmacology Exam4 ReviewNatalia BortellAinda não há avaliações
- Clinical Packet OBDocumento7 páginasClinical Packet OBLiza Jean BakerAinda não há avaliações
- EXAM CompiledDocumento19 páginasEXAM CompiledAhmad Fuad HasbollahAinda não há avaliações
- Absite 2011Documento19 páginasAbsite 2011Shawn Robinson0% (1)
- Gyne Past Papers Update 5Documento139 páginasGyne Past Papers Update 5Misbah KaleemAinda não há avaliações
- OBGYN Objective - Module Study GuideDocumento79 páginasOBGYN Objective - Module Study GuideHema LaughsalotAinda não há avaliações
- 19 Spinal CordDocumento8 páginas19 Spinal Cordkarar AhmedAinda não há avaliações
- ObGyn Secrets, 3rDocumento1 páginaObGyn Secrets, 3rCahyadi PangemananAinda não há avaliações
- Done By: Abdul Hakeem Hady. Gynecology SlidesDocumento16 páginasDone By: Abdul Hakeem Hady. Gynecology Slidesعمر احمد شاكرAinda não há avaliações
- Pain at GIDocumento74 páginasPain at GIdmtaponAinda não há avaliações
- Appleton - Obstetrics and GinecologyDocumento306 páginasAppleton - Obstetrics and GinecologyFajar Raharja50% (2)
- Neonate Module Pedia NotesDocumento23 páginasNeonate Module Pedia NotesAria Alysis100% (1)
- Clinical CasesDocumento12 páginasClinical CasesAndreea HanuAinda não há avaliações
- USMLEasy Psych Case01Documento10 páginasUSMLEasy Psych Case01Tanzeel Ur RehmanAinda não há avaliações
- Breast Disorder: by DR - Wael MetwalyDocumento7 páginasBreast Disorder: by DR - Wael MetwalyhasebeAinda não há avaliações
- U.S. Preventive Services Task Force (USPSTF) Recommendations - Stats - Medbullets Step 2 - 3Documento5 páginasU.S. Preventive Services Task Force (USPSTF) Recommendations - Stats - Medbullets Step 2 - 3mtataAinda não há avaliações
- 1 Bullets Pain & orDocumento7 páginas1 Bullets Pain & orAnne Mae PaculaAinda não há avaliações
- Cardiovascular Shoutouts: When She Says You SayDocumento7 páginasCardiovascular Shoutouts: When She Says You SayGbotemi AlaladeAinda não há avaliações
- Surgery Part 1, Tras ExamDocumento17 páginasSurgery Part 1, Tras ExamWaddah N. MohamedAinda não há avaliações
- Ethics Uworld NotesDocumento3 páginasEthics Uworld NotesActeen MyoseenAinda não há avaliações
- VA SICU Guide To An Organ Based PresentationDocumento4 páginasVA SICU Guide To An Organ Based Presentationseigfried13Ainda não há avaliações
- ID - 4282 - Physiological Duration of Pre - English - Sem - 8Documento43 páginasID - 4282 - Physiological Duration of Pre - English - Sem - 8ajal hamza100% (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsAinda não há avaliações
- Problem-based Approach to Gastroenterology and HepatologyNo EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisAinda não há avaliações
- 8 Steps To Solving Acid-Base ProblemsDocumento2 páginas8 Steps To Solving Acid-Base Problemslizzy596Ainda não há avaliações
- 2012-13 Psychiatry Board ReviewDocumento79 páginas2012-13 Psychiatry Board Reviewlizzy596100% (1)
- Uwise Gynecology and BreastDocumento24 páginasUwise Gynecology and Breastlizzy596Ainda não há avaliações
- Bladder CatheterizationDocumento1 páginaBladder Catheterizationlizzy596Ainda não há avaliações
- Nasogastric Tube InsertionDocumento1 páginaNasogastric Tube Insertionlizzy596Ainda não há avaliações
- Ventilation Cheat SheetDocumento1 páginaVentilation Cheat Sheetlizzy59683% (6)
- 2012 ECG HandoutDocumento40 páginas2012 ECG Handoutlizzy596Ainda não há avaliações
- Liver and Biliary NotesDocumento16 páginasLiver and Biliary Noteslizzy596Ainda não há avaliações
- Surgical Intensive CareDocumento95 páginasSurgical Intensive Carelizzy596Ainda não há avaliações
- Week 1 - Trauma (BB)Documento11 páginasWeek 1 - Trauma (BB)lizzy596Ainda não há avaliações
- B. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)Documento14 páginasB. Belingon - Notes From Case Session Slides, Becky's Notes (Dr. Nguyen)lizzy596Ainda não há avaliações
- B. Belingon - Notes From Case Session Slides, Anna's Notes (Dr. Esterl), Becky's Notes (Dr. Nguyen)Documento11 páginasB. Belingon - Notes From Case Session Slides, Anna's Notes (Dr. Esterl), Becky's Notes (Dr. Nguyen)lizzy596Ainda não há avaliações
- Musculoskeletal System ReviewDocumento6 páginasMusculoskeletal System Reviewlizzy596Ainda não há avaliações
- Classes of Neurotransmitters: Amino AcidsDocumento30 páginasClasses of Neurotransmitters: Amino Acidslizzy596Ainda não há avaliações
- Week 2 Critical CareDocumento8 páginasWeek 2 Critical Carelizzy596Ainda não há avaliações
- MBB2 NeurologyDocumento38 páginasMBB2 Neurologylizzy596Ainda não há avaliações
- E PortfolioDocumento3 páginasE Portfolioapi-337945337Ainda não há avaliações
- Myocarditis NCP 2Documento8 páginasMyocarditis NCP 2astro_aaron117375% (4)
- DS Clarithromycin GI ARLEDDocumento5 páginasDS Clarithromycin GI ARLEDvivi's eyebrowsAinda não há avaliações
- I Summary Family MedicineDocumento185 páginasI Summary Family MedicineModa ModyAinda não há avaliações
- Chap 1Documento27 páginasChap 1MownikaAinda não há avaliações
- Caraway Essential Oil InformationDocumento19 páginasCaraway Essential Oil InformationRahul SinghAinda não há avaliações
- Common - CardioDocumento91 páginasCommon - CardioHanadi UmhanayAinda não há avaliações
- Group 1,2,4 QuizDocumento221 páginasGroup 1,2,4 QuizPaulAinda não há avaliações
- Rebound Your Way To Lymphatic HealthDocumento7 páginasRebound Your Way To Lymphatic HealthMaxLev10100% (1)
- NURSING CARE PLAN - Liver CirrhosisDocumento2 páginasNURSING CARE PLAN - Liver Cirrhosisderic100% (27)
- 3-Level of MDMDocumento3 páginas3-Level of MDMmedical codingAinda não há avaliações
- Genetic Disorder Webquest ArtifactDocumento13 páginasGenetic Disorder Webquest Artifactapi-582653189Ainda não há avaliações
- Pcol 1 Sas 7Documento9 páginasPcol 1 Sas 7HaruhAinda não há avaliações
- Future Perfect and Cont TestDocumento2 páginasFuture Perfect and Cont TestEdit GöröcsAinda não há avaliações
- The Therapeutic Use of Centella AsiaticaDocumento6 páginasThe Therapeutic Use of Centella AsiaticaDr. Md. Shahab UddinAinda não há avaliações
- Neonatal Seizures : Types, Etiology and Long Term Neurodevelopmental Out-Come at A Tertiary Care HospitalDocumento7 páginasNeonatal Seizures : Types, Etiology and Long Term Neurodevelopmental Out-Come at A Tertiary Care HospitalAgung NohuAinda não há avaliações
- Antimycobacterial DrugsDocumento35 páginasAntimycobacterial DrugsJunah SeninaAinda não há avaliações
- NCP For Ineffective Airway ClearanceDocumento3 páginasNCP For Ineffective Airway ClearanceJennelyn BayleAinda não há avaliações
- The Antipsychiatry Movement: Dead, Diminishing, or Developing?Documento3 páginasThe Antipsychiatry Movement: Dead, Diminishing, or Developing?José Alberto Pacheco OsornioAinda não há avaliações
- Navales Vs Navales GR No 167523Documento11 páginasNavales Vs Navales GR No 167523Jonjon BeeAinda não há avaliações
- Notes From Beynon LectureDocumento6 páginasNotes From Beynon LecturearianAinda não há avaliações
- Age NCPDocumento3 páginasAge NCPMartin Allen ClaudioAinda não há avaliações
- Dr. Max Gerson Inducted Into Orthomolecular Medicine Hall of Fame - 2005Documento2 páginasDr. Max Gerson Inducted Into Orthomolecular Medicine Hall of Fame - 2005TUartistAinda não há avaliações
- Impaired Gas Exchange PneumoniaDocumento2 páginasImpaired Gas Exchange PneumoniaShanice BedecirAinda não há avaliações
- Medical CertificateDocumento1 páginaMedical Certificatetri rahmawatiAinda não há avaliações
- Letter To ACS CommissionerDocumento4 páginasLetter To ACS CommissionerCity Limits (New York)Ainda não há avaliações
- PTSD DBQ 21-0960P-4Documento5 páginasPTSD DBQ 21-0960P-4Christopher Reece100% (1)
- LG 2.7 Urinalysis Virtual LabDocumento115 páginasLG 2.7 Urinalysis Virtual LabLEANNE CLARISSE LOSANESAinda não há avaliações
- Krok 2 Medicine (EN) - Attempt Review 4Documento52 páginasKrok 2 Medicine (EN) - Attempt Review 4IS ZDAinda não há avaliações
- Alison Cooper QuestionDocumento3 páginasAlison Cooper QuestionSathiyaseelan Velayutham89% (18)