Escolar Documentos
Profissional Documentos
Cultura Documentos
A Case Study of Client That Undergo Appendectomy Post Operative
Enviado por
Rio Bonifacio0 notas0% acharam este documento útil (0 voto)
383 visualizações49 páginasff
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoff
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
383 visualizações49 páginasA Case Study of Client That Undergo Appendectomy Post Operative
Enviado por
Rio Bonifacioff
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 49
A CASE STUDY OF CLIENT WITH ACUTE APPENDICITIS
THAT UNDERGONE APPENDECTOMY
Submitted by:
BSN 3A-Group 1
Aguilar, Divine Grace P.
Angeles, Sharmaine I.
Arojo, Dhianne Joye C.
Azul, Kizsia Mae
Bagay, Maria Fatima C.
Batac, Joice M.
Bernardo, Jamaica Ezza
Bonifacio, Ann Rio S.
Bulanadi, Krisna Jane D.
Carlos, Jenikka Mhae
Submitted to Clinical Instructor:
Narcisa Cruz RN, MAN
Mylene Fajardo RN, MAN
Jesusa Capispisan RN
Abigail Ramos RN, MAN
Maribel Valencia RN, MAN
Jose Florante C. Nabong RN, MAN
Marlon Robles RN
October 03, 2013
I. INTRODUCTION
Our client is Mr.N.C, a 12-year old client from Tigbe, Norzagaray, Bulacan, admitted at Bulacan Medical Center on August 25, 2013 with an initial
diagnosis of Acute Appendicitis with chief complain of an abdominal pain.
According to US National Library of Medicine, Appendicitis is considered to be a serious illness and the most efficient treatment at the time being involves
medical surgery. Appendicitis is therefore a surgical emergency and it can be efficiently overcome only by removing the diseased appendix from the body. The
vermiform appendix is a tubular extension of the large intestine (colon) and it is considered to have a role in the process of digestion. The actual function of the
appendix is not exactly known, but its absence doesn't cause any changes inside the organism. Appendicitis occurs due to strangulation or obstruction of the
vermiform appendix.
The appendix can either be blocked by feces or it can be pressed against by swollen lymph nodes. The appendix gradually stops receiving blood and it
eventually dies. Bacteria accumulate inside the appendix and cause inflammation and swelling. Acute appendicitis may lead to complications such as perforation of
the appendix and sepsis (severe bacterial infection). In rare cases, abdominal traumatic injuries can also lead to the development of appendicitis. In some people,
genetic predispositions to appendicitis can also facilitate the occurrence of the illness.
Appendicitis can be either acute or chronic. Acute appendicitis develops faster and the presence of the illness is easier to detect. Chronic appendicitis is
slower to evolve and it is more difficult to diagnose. The most common symptoms of appendicitis are intense, continuous abdominal pain, nausea, vomiting,
constipation or diarrhea and fever. The pain usually begins in the umbilical region of the abdomen and later shifts to the right lower side. The abdominal pain
characteristic to acute appendicitis intensifies with physical effort.
An interesting aspect of appendicitis is that it can be very difficult to detect and diagnose correctly, due to the unspecific character of its symptoms. In some
cases, the patients might not have any symptoms at all (elderly people, people that have previously suffered surgical interventions, people with HIV, people with
diabetes and overweight people). The form of appendicitis that generates no specific symptoms is called a typical appendicitis. The rate of mortality among patients
with atypical appendicitis is very high.
Anyone can develop appendicitis, regardless of age and sex. However, the illness has a higher incidence in men. Also, children with ages between 3-15 are
exposed the most to developing acute appendicitis. Elderly people and patients with special conditions usually develop atypical acute appendicitis. If appendicitis is
discovered in time and treated appropriately; the patients fully recover within weeks.
However, if the illness is discovered late, it may lead to serious complications (perforation, gangrene, sepsis).Although appendicitis can't be effectively
prevented, it is thought that a diet rich in fibers may reduce the chances of developing the illness.
Incidence extrapolations for USA for Acute Appendicitis: 680,000 per year, 56,666 per month, 13,076 per week, 1,863 per day, 77 per hour, 1 per minute, 0
per second. Note: this extrapolation calculation uses the incidence statistic: 25 per 10,000 (age 10-17), 1-2 per 10,000 (under 4) Death rate extrapolations for USA
for Acute Appendicitis: 389 per year, 32 per month, 7 per week, 1 per day, 0 per hour, 0 per minute, 0 per second. Note: this extrapolation calculation uses the
deaths statistic: 390 deaths reported in USA 2010 for appendix conditions (NVSR Sep 2010). According to Department of Health, as of September 2012, statistics
in the Philippines shows that about 215,604 of the 86,241,697 Filipinos had an incident of appendicitis. Incidence (annual) of Acute Appendicitis: 25 per 10,000
(age 10-17), 1-2 per 10,000 (under 4). Lifetime risk for Acute Appendicitis: 8.6% risk for males, 6.7% for females.
OBJECTIVES
GENERAL OBJECTIVE:
After 3-4 hours of Case Presentation, we nursing students will be able to gain knowledge about Appendicitis.
STUDENT-CENTERED:
I. Knowledge
Define what Appendicitis is
Enumerate signs and symptoms of Appendicitis.
Identify nursing interventions to be done when handling patient with Appendicitis.
II. Skills
Properly assess the patient.
Perform proper nursing care to patient.
Present a liable case study to clinical instructors about the patient handled at the hospital.
III. Attitude
Observe discipline while in the field of duty.
Manage own emotions while in the field of duty.
Establish self-confidence when giving nursing care into the client.
CLIENT-CENTERED:
I. Knowledge
Enumerate some causes of Appendicitis
Enumerate signs and symptoms.
Identify some foods to eat and to avoid when suffering from Appendicitis.
II. Skills
Practice and enhance improvement a good communication skills through interviews.
Conduct a comprehensive assessment of patient who had appendicitis and undergone appendectomy.
Develop a critical thinking and analytical skills through frequent brainstorming sessions.
III. Attitude
Establish rapport with patient
Develop a warm environment between the student and the patient fora better working relationship towards improvement of health.
Provide health teachings with the client
II. NURSING ASSESSMENT
A. PERSONAL HISTORY
Name: N.C.
Permanent Address: Tigbe, Norzagaray, Bulacan
Birthday: September 23, 2000
Age: 12 years old
Gender: Male
Occupation: None
Race: Asian
Marital Status: Single
Religious Orientation: Roman Catholic
Educational Attainment: Elementary level
Source of Healthcare Financing: Fathers Income
Healthcare Insurance: Phil Health
Date of Admission: August 25, 2013 at 12:39 pm
Date of discharge: September 03, 2013
Initial diagnosis: Acute appendicitis
Final diagnosis: supperative appendicitis
B. CHIEF COMPLAINT
Abdominal Pain
C. HISTORY OF THE PRESENT CONDITION
According to the father of our client, his son having an abdominal pain for 3 days on August 21, 2013. On August 17, 2013 they go in the center in
Norzagaray, and they gave 1 capsule of 10 mg of Buscopan when the abdominal cramps. Then, August 23, 2013 he admitted at Norzagaray Hospital. The
diagnosis of the doctor in Norzagaray Hospital is appendix and the appendix might blow. He was transferred at Bulacan Medical Center at 12:39 pm of
August 25, 2013 and the operations do. N.C. is a 12 years old.
According to the father of our client, his son feels the symptoms of having abdominal pain and vomiting. And he never goes in the hospital or having
a checkup. According to N.C., he is having an acute appendicitis, because when he done eating he is playing immediately.
He ignores the pain on that day and sleep but on the second day morning he suffers again the pain and he tell to his father about his feeling. His father
brought him to the Health center near there barangay and was checked up by the rural health doctor prescribed medication such as Buscopan 10 mg 1tablet a
day when his abdomen cramps.
In this 7 days onset of severe pain and symptoms his father brought him in the Norzagaray Hospital at August 23, 2013 and confined him.
Then the doctor diagnosed that the client had Acute Appendicitis with positive anorexia and vomiting in which referral for another hospital admitted
in Bulacan Medical Center, August 25, 2013 time of 12:39:19 pm for surgery.
D. HISTORY OF THE PAST CONDITION/ ILLNESS
The father of our client told us that his son didnt undergo any operations, aside from he is under go before in the appendectomy cause by acute
appendicitis. His childhood or previous diseases are fever, cough, colds, diarrhea, measles, sore eyes, and mumps. According to his father, during his
childhood he has the complete immunization like BCG, DPT, OPV, HEPA A, B, and C. He has no allergies, accidents, injuries this past years, and
hospitalization aside from the present.
F. FUNCTIONAL HEALTH PATTERN
PRIOR TO HOSPITALIZATION DURING HOSPITALIZATION
A. Health
Perception and
Health
Management
Pattern
The client perceives himself unhealthy. He suffers abdominal pain around
the epigastric area, which may have an sudden onset and become
increasingly severe pain, started August 16, 2013. He also suffers
vomiting, diarrhea and body malaise. He rate his pain for about 8/10 in
pain scale. Kasi kung minsan hindi siya palakain inuuna pa ang laro kesa
sa kain yan siguro dahilan ng pagkakasakit ng tiyan niya as verbalized by
his father.
After Surgery the client feels calm and quiet with IVF which is
0.9 NaCL 500cc @ 450 cc level regulated at 16 gtts/min. He
has incision on right lower quadrant for about 2 inches
transverse and sutures. Masakit yung tahi ko as verbalized by
the client. He rates the pain scale 5. He also add Kumakati ang
tahi ko as he stated
B. Nutritional
Metabolic
Pattern
-72 HOURS DIET RECALL
The client usually drink 2-3 glasses of soft drink a day, 3fruit guava and
eat flavored snack. He doesnt want to consume his full meal as stated by
his father. He would go with his friend and play with them. His weight
was 23 kilograms and a height of 3 feet and 9 inches with a Body Mass
Index of 17.6 which is classified as underweight. There's no difficulty in
swallowing and no known allergy to foods His wounds dont heal easily
as stated by his father. In fact there are many scars in his legs caused by
stumbling and lack of balance in playing like basketball and hide n' seek.
He has twenty six permanent teeth with no third molars yet.
August 24, 2013 August 25, 2013 August26,2013
Breakfast
Lunch
Dinner
NPO
NPO
NPO
-72 HOURS DIET RECALL
August 27,
2013
August 28, 2013 August 29,
2013
Breakfast 1 glass of
water
(250ml)
1 piece of bread
1 glass of water
(250 ml)
2 piece of
bread
1 glass of
water (250 ml)
Lunch 20 grams of
noodles soup
1 glass of
water (250 ml)
1 glass of water
(250 ml)
40 grams of
Nissan cup
noodles
1 serving of
kare-kare
1 half rice
1 glass of
water (250 ml)
Dinner None 1 bottled mineral
water
None
On august 27, 2013 the doctor ordered General liquid diet And
August 28-29, 2013 the doctor ordered Diet As Tolerated.
"Pipilitin ko na talaga siya kumain ngayon sa ayaw at sa gusto
niya" as verbalized by his father.
C. Elimination
Pattern
Color Frequency Amount Character Discomfort
Urine yellowis
h
4x a day 480 ml hazy None
Color Frequency Amount Character Discomfort
Urine yellowis
h
6x a day 720 ml hazy none
Stool brownish 0-1x a day Not
applicable
floating Slightly
Theres no excessive perspiration but he sweat immediately while playing
basketball with his friend as stated by his father. Minsan amoy
pagpapawis niya na parang mgangasim asim lalo na ka kili-kili as
verbalized by his father.
Stool brownish 1-2x a day Not
applicable
loose none
Post op the client doesnt feel any discomfort in urinating and
defecating.
D. Activity
Exercise
Pattern
Meron siyang sapat na enerhiya para maglaro pero pag uutusan sa bahay
walang nagagawa as verbalized by the father. The client tells that he
exercise everyday by walking to school. The school which he entered
grade 6 was just walking distance as the client states. He does some
recreation like basketball, hide n seek, playing some activities with his
friends either morning or in the afternoon. If he has free time he just
sleeps or watches television every morning especially his favorite shows
like Dragon Ball Z and Doraemon
Perceive ability for (code level):
0 Feeding
0 Dressing
0 Bathing
0 Grooming
0 Toileting
0 General Mobility
0 Bed Mobility
On August 27, 2013, 8 am, the doctor orders the father of my
client for ambulation. And for not carrying any heavy materials
or objects. Being hospitalized interfered with Activities of daily
living especially in his school attendance.
Perceive ability for (code level):
0Feeding
0 Dressing
0 Bathing
0 Grooming
0 Toileting
0 General Mobility
0 Bed Mobility
E. Sleep- Rest
Pattern
The sleeping hours of my client starts from 8pm to 9am in the morning for
a total of 10 hours in week days. But in school days it is 8pm to 6am for a
total of 7hours. He has no nap time because he spent this time for
recreational activities. He doesn't have any sleeping problems and no
sleeping medications. He has continuous sleep but interrupts when he felt
pain on the abdomen. He only rest when he feel exhausted from playing
Start of Sleep 8: 00 pm
End of Sleep 9: 00 am
Nap time none
Total no. of Hours 10 hours
The hours of sleep during are intermittent sleep for about 10:30
pm to 7 am. Then he sleeps at the afternoon for nap time of 15
mins. Nahihirapan akong akong matulog dito as verbalized
by the client.
Start of Sleep 10: 30 pm
End of Sleep 7: 00 am
Nap time 15 mins
Total no. of Hours
(Code Level)
Level 0 - Full Self care
Level 1 - Requires use of equipment or
device
Level 2- Requires assistance or supervision
from another person
Level 3- Requires assistance or supervision
from another person or device
Level 4- Is dependent and does not
participate
(Code Level)
Level 0 - Full Self care
Level 1 - Requires use of equipment or
device
Level 2- Requires assistance or supervision
from another person
Level 3- Requires assistance or supervision
from another person or device
Level 4- Is dependent and does not
participate
sport.
F. Cognitive-
Perceptual
Pattern
He doesnt have any hearing difficulties and not using hearing aid. No
blurred vision and also not using eye glasses. No consultation of doctor
about vision. Doesnt have any changes in the memory lately. His easiest
way to learn things is to have time by his mother to teach him.
The client only suffers a bit of achiness and ichiness in his
incision. No changes in the 5 senses.
G. Self-
Perception
Pattern and
Self- Concept
Pattern
He said hes healthy before his condition as my client stated. As he grows
up in the age of 12 years old there so many thing changes specifically his
physical appearance. He grows more having an Adams apple and his
voice gets deeper. He starts to clean by himself in hygienic purposes.
Kapag pinapagalitan ako ni papa dun ako naiinis o kaya nalulungkot
kaya dinadaan ko na lang sa laro ito as verbalized by the client.
He stated that his healthy now though he can still feel a little
pain. He also state that he has impaired skin integrity due to
surgical incision.
H. Role-
Relationship
Pattern
He has parents and with 3 siblings not living alone. He lives in Tigbe,
Norzagaray, Bulacan and has a nuclear family as stated by his father. He
thinks that his father was worrying about his status. He also has friends
that join also in playing basketball. Opo, minsan kulang ang aking baon
sa pang araw-araw kong pangngangailangan as verbalized by the client.
He said that his neighbor was kind and frequently going outside the house
to talk with my neighbor.
The client was able to listen and follow on his fathers
instruction. He felt uneasy with other patient. Maayos ang mga
nurse at doctor dito as verbalized by the father.
I. Sexuality
Reproductive
Pattern
He was circumcised last April 13, 2010. This Elective surgery was done
in their barangay where in they have free circumcision on that day.
He grows physically as hes father stated. He had an Adams
apple and with deep voice and underarm hair.
J. Coping Stress
Tolerance
Pattern
He doesnt take any drugs to cope stress neither drinks alcoholic
beverages. He usually goes to the computer shop to refresh his mind. He
doesnt change any in the past 1-2 years ago with the problems.
Theres stress now as the client stated. He was uncomfortable
when sleeping. He was disturbed by his surroundings like noise
at night. The client also shared that he is easily bored at bed so
he usually wonder around the hospital ward.
K. Value- Belief
Pattern
He doesnt like being yelled by his father. For him, family is very
important and he values his studies. He's a roman catholic and religion is
very important to him especially when he has problems. Hindi
nakakahadlang sa relihiyon ko ang kalagayan ko ngaun as verbalized by
the client.
He prayed to God for successful surgery and for better
recovery.
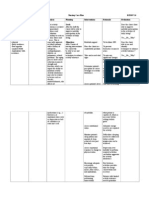
G. GROWTH AND DEVELOPMENT
THEORY ERICKSONs PSYCHOSOCIAL
DEVELOPMENT THEORY
PIAGETs
COGNITIVE
DEVELOPMENT
THEORY
FREUDs
PSYCOSEXUAL
DEVELOPMENT
THEORY
KOHLBERGs MORAL
THEORY
FOWLERS
STAGES OF FAITH
STAGE Industry vs. Inferiority Formal Operational
Stage
Latency Stage Conventional Morality Synthetic-
Conventional Faith
and the Interpersonal
Self
DEFINITION Children are at the stage where they
will be learning to read and write, to
do sums, to make things on their own.
Teachers begin to take an important
role in the childs life as they teach the
child specific skills.
It is at this stage that the childs peer
group will gain greater significance
and will become a major source of the
childs self esteem. The child now
feels the need to win approval by
demonstrating specific competencies
that are valued by society, and begin
to develop a sense of pride in their
accomplishments.
If children are encouraged and
reinforced for their initiative, they
begin to feel industrious and feel
confident in their ability to achieve
goals. If this initiative is not
encouraged, if it is restricted by
parents or teacher, then the child
begins to feel inferior, doubting his
As adolescents enter
this stage, they gain
the ability to think in
an abstract manner,
the ability to
combine and classify
items in a more
sophisticated way,
and the capacity for
higher-order
reasoning.
At about age 11+
years, the child
begins to manipulate
ideas in its head,
without any
dependence on
concrete
manipulation; it has
entered the formal
operational stage. It
can do mathematical
calculations, think
No further
psychosexual
development takes
place during this
stage (latent means
hidden). The libido
is dormant. Freud
thought that most
sexual impulses are
repressed during
the latent stage and
sexual energy can
be sublimated (re:
defense
mechanism)
towards school
work, hobbies and
friendships. Much
of the child's
energies are
channeled into
developing new
skills and acquiring
Conventional morality as
defined in Kohlberg's stages of
morality is the concept of
acceptable behavior that
mirror's the values of certain
political or social context.
Stage 3 - Interpersonal
Relationships
Often referred to as the
"good boy-good girl"
orientation, this stage of
moral development is
focused on living up to
social expectations and
roles. There is an emphasis
on conformity, being
"nice," and consideration
of how choices influence
relationships.
Stage 4 - Maintaining
Social Order
At this stage of moral
development, people begin
This was a watershed
in faith development
for Fowler: young
person uses logic and
hypothetical thinking
to construct and
evaluate ideas. New
cognitive abilities
make mutual
perspective-taking
possible and enable
one to integrate
diverse self-images
into a coherent
identity. A persona
and largely
unreflective synthesis
of beliefs and values
evolves to support
identity and to unite
one in emotional
solidarity with others.
own abilities and therefore may not
reach his or her potential.
If the child cannot develop the specific
skill they feel society is demanding
(e.g. being athletic) then they may
develop a sense of inferiority. Some
failure may be necessary so that the
child can develop some modesty. Yet
again, a balance between competence
and modesty is necessary. Success in
this stage will lead to the virtue
of competence.
creatively, use
abstract reasoning,
and imagine the
outcome of
particular actions.
new knowledge and
play becomes
largely confined to
other children of
the same gender.
to consider society as a
whole when making
judgments. The focus is on
maintaining law and order
by following the rules,
doing ones duty and
respecting authority.
FINDING/
ANALYSIS
The client has the ability to read and
write which is primarily needed by a
child develop his full potential.
The client speaks
accordingly with
appropriate
thoughts.
The client has a
social life for he
plays with his
childhood friends.
The client obeyed his father
when we asked for a
permission to see the site of
operation.
The patient grimaced
when we palpated the
side of the incision
site.
REMARKS Positive Positive Positive Positive Positive
III. ANATOMY AND PHYSIOLOGY
Small intestine- completes digestion. Mucus protects gut wall. It absorbs nutrients, mostly water. Peptidase digests proteins. Sucrases digest sugars. Amylase
digests polysaccharides.
Large intestine- reabsorbs some water and ions. It also forms and stores feces.
Appendix- is a tube-shaped organ with a length of approximately 10 cm and the stem on the cecum. It sits at the junction of the small intestine and large intestine.
Sometimes the position of the appendix in the abdomen may vary. Most of the time the appendix is in the right lower abdomen, but the appendix, like other parts of
the intestine has a mesentery. This mesentery is a sheet-like membrane that attaches the appendix to other structures within the abdomen. If the mesentery is large it
allows the appendix to move around.
In addition, the appendix may be longer than normal. The combination of a large mesentery and a long appendix allows the appendix to dip down into the pelvis
(among the pelvic organs in women) it also may allow the appendix to move behind the colon (a retrocolic appendix).
In infants, the appendix is a conical diverticulum at the apex of the cecum, but with differential growth and distention of the cecum, the appendix ultimately arises
on the left and dorsally approximately 2.5 cm below the ileocecal valve. The taeniae of the colon converge at the base of the appendix, an arrangement that helps in
locating this structure at operation.
The appendix in youth is characterized by a large concentration of lymphoid follicles that appear 2 weeks after birth and number about 200 or more at age 15.
Thereafter, progressive atrophy of lymphoid tissue proceeds concomitantly with fibrosis of the wall and partial or total obliteration of the lumen.
Appendix is blooded by apendicular artery which is a branch of the artery ileocolica. Arterial appendix is end arteries. Appendix has more than 6 mesoapendiks
obstruct lymph channels leading to lymph nodes ileocaecal. Although the appendix has less functionality, but the appendix can function like any other organ.
Appendix produces mucus 1-2ml per day. The mucus poured into the caecum. If there is resistance there will be a pathogenesis of acute appendicitis. GALT (Gut
Associated Lymphoid Tissue) in the appendix produce Ig-A. However, if the appendix removed, none affect the immune body system.
Ascending colon- watery stool
Transverse colon- mushy stool
Descending colon- semi-formed stool
Sigmoid colon- feces are formed
Rectum- stores and expels feces.
IV. PATIENT AND HIS CONDITION / ILLNESS
A. PHYSICAL ASSESSMENT
NAME: NARC
AGE: 12 years old
DATE: August 26, 2013
8 AM 12 PM
VITAL SIGNS: PR= 90 bpm PR= 84 bpm
TEMPERATURE= 35.3 C TEMPERATURE= 36.3 C
RR= 26 cpm RR= 26 cpm
BP=100/80mmHg BP=100/80mmHg
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
GENERAL SURVEY
1. Body built, height & weight
in relation to clients age,
lifestyle & health
Inspection
Proportionate and varies with
lifestyle.
Height: 23 kg
Weight : 39 inches
BMI: 17.6
Deviation from normal due to
malnourishment
3. Clients overall hygiene &
grooming
Inspection Clean, neat Client is clean and neat. NORMAL
4. Body & breath odor Inspection
No body odor or minor body
odor relative to work or
Neither body odor nor breath
odor was observed.
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
exercise, no breath odor.
5. Signs of distress in posture
or facial expression
Inspection No distress noted. No distress noted. NORMAL
6. Obvious signs of health or
illness
Inspection Healthy appearance.
Obvious sign of illness such as
pallor
NORMAL
SKI N
1. Skin color & uniformity Inspection and Palpation
Color- varies from light to
deep brown; from ruddy pink
to light pink; from yellow
overtones to olive.
Uniformity- generally uniform
except in areas exposed to
sunlight; areas of lighter
pigmentation (palms, lips, nail
beds) in dark skinned people.
The client has a light brown
complexion, uniformity in
color except those with
clothes,and have scars in the
both legs and feet.
Deviation from normal due to
insect bites.
2. Presence of edema Inspection No edema. No edema noted.
NORMAL
3. Skin lesions Inspection
Freckles, some birthmarks,
some flat and raised nevi; no
abrasions or other lesions.
Skin lesion located at the left
hand due to IV insertion
Deviation from normal due to
IV insertion.
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
4. Skin moisture Palpation
Moisture in skin folds and
axillae (varies with
environmental temperature
and humidity, body
temperature and activity.)
Moistened skin especially in
the skin folds.
NORMAL
5. Skin temperature Palpation Uniform; within normal range Uniform in temperature. NORMAL
6. Skin turgor Palpation
When pinched, skin springs
back to previous state.
\
Skin returns back to previous
state in less than 2 seconds.
NORMAL
NAI LS
1. Fingernails plate shape to
determine its curvature &
angle
Inspection
Convex curvature, angle of
nail plate about 160 degrees.
Nails are in convex curvature; NORMAL
2. Fingernail & toenail bed
color
Inspection
Highly vascular and pink in
light skinned clients; dark-
skinned clients may have
brown or black pigmentation
in longitudinal streaks.
Fingernails and toe nails color
are pinkish.
NORMAL
3. Tissues surroundings nails Inspection Intact epidermis. Intact epidermis, pale in color NORMAL
4. Fingernail & toenail texture Palpation Smooth texture.
Clients nails are smooth in
texture
NORMAL
5. Blanch test of capillary
Palpation
Prompt return of pink or usual Prompt return of pink or usual
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
refill color (generally less than 4
seconds.)
color (generally less than 4
seconds.)
HAI R & SCALP
1. Evenness of growth over the
scalp
Inspection Evenly distributed hair. Hairs are evenly distributed. NORMAL
2. Hair thickness & thinness Palpation Thick/thin hair.
The client has thick hair on
head.
NORMAL
3. Presence of infections or
infestations
Inspection Not present. No infestations noted NORMAL
4. Texture & oiliness over the
scalp
Palpation Silky, resilient hair. Oily, thick, resilient hair NORMAL
SKULL
1. Size, shape & symmetry Palpation
Rounded (normocephalic and
symmetrical, with frontal,
parietal, and occipital
prominences); smooth skull
contour.
Head is symmetrically round. NORMAL
2. Nodules or masses &
depressions
Palpation
Smooth, uniform consistency;
absence of nodules or masses.
No mass or nodules noted NORMAL
FACE
1. Facial features Inspection
Symmetric or slightly
asymmetric facial features;
palpebral fissures equal in
Symmetrical facial features;
palpebral fissures equal in
size; nasolabial folds are
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
size; symmetric nasolabial
folds.
symmetrical
2. Symmetry of the facial
movements
Inspection
Symmetrical facial
movements.
Facial movements are all
symmetrical
NORMAL
EYEBROWS & EYELASHES
1. Evenness of distribution &
direction of curl
Inspection
Hair evenly distributed; skin
intact. Eyebrows
asymmetrically aligned equal
movement. Eyelashes curl
slightly outward.
Eyebrows and eyelashes are
both evenly distributed,
symmetrical aligned.
Eyelashes curl slightly
outward.
NORMAL
EYELI DS
1. Surface characteristics &
ability to blink
Inspection and Palpation
Skin intact, no discharge, no
discoloration. Lids close
symmetrically approximately
15-20 involuntary blinks per
minute; bilateral blinking.
When lids open, no open, no
visible sclera above corneas,
and upper and lower borders
of cornea are slightly covered.
Eyelids skin are intact, no
noted discharge, and no noted
discoloration. Lids close
symmetrically. Client
exhibited 15 involuntary
blinks per minute.
NORMAL
CONJ UNCTI VA
1. Bulbar conjunctivas color,
texture & presence of lesions
Inspection
Transparent; capillaries
sometimes evident.
Transparent, capillaries
evident, no discharge was
noted.
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
2. Palpebral conjunctivas
color, texture & presence of
lesions
Inspection
Shiny, smooth, pink or red in
color.
Shiny, smooth and pale in
color
NORMAL
SCLERA
1. Color & clarity Inspection
Sclera appears white
(yellowish in dark- skinned
clients).
Sclera appears white NORMAL
CORNEA
1.Clarity & color Inspection
Transparent, shiny and
smooth; details of the iris are
visible. In older people, a thin
grayish white ring around the
margin, called arcus senilis,
may be evident.
Details of iris are visible.
Transparent, shiny and
smooth.
NORMAL
I RI S
1. Shape & color Inspection Flat and round
Flat and round and uniform in
color.
NORMAL
PUPI LS
1. Color, shape & symmetry of
size
Inspection
Black in color; equal in size;
normally 3-7 mm in diameter;
round, smooth border.
Black, equal in size, about 3
mm in diameter; round,
smooth & symmetrical.
NORMAL
2. Pupil light reaction &
accommodation
Inspection
Illuminate pupil constricts
(direct response)
Illuminated pupil constricts NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
3. Pupils direct & consensual
reaction to light
Inspection
Nonillluminated pupil
constricts (consensual
response)
Pupils constrict when looking
at near object; pupil dilates
when looking at far object;
pupils converge when object is
moved towards the nose.
Non-illuminated pupil
constricts too. Pupils dilated
when ask to look on distant
objects, constricts when pen
was placed near eyes; when
pen is moved towards the
nose
NORMAL
LACRI MAL GLAND, LACRI MAL SAC & NASOLACRI MAL DUCT
1. Presence of edema Inspection
No edema or tenderness over
lacrimal gland.
No edema noted NORMAL
VI SUAL FI ELDS
1. Test for peripheral visual
fields
Inspection
When looking straight ahead,
the client can see objects in the
periphery.
Client can see objects in the
periphery.
NORMAL
EARS AURICLE
1. Color & symmetry of size &
position
Inspection
Color same as facial skin,
symmetrical, auricle aligned
with outer canthus of eye,
about 10cm from vertical.
Color is same with facial skin,
symmetrical with each other,
auricle aligned with outer
canthus of eye,
NORMAL
2. Texture & elasticity & areas
of tenderness
Palpation
Mobile, firm and not tender,
pinna recoils after it is folded.
Both pinna recoils after being
folded. Mobile, firm and not
tender.
NORMAL
EXTERNAL EAR CANAL
1. Cerumen, skin lesions, pus
Inspection
Distal third contains hair
follicles and glands. Dry
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
& blood cerumen in various shades of
brown
No noted pus, blood and odor.
Minimal cerumen noted.
NOSE
1. Shape, size or color &
flaring or discharge from the
nares
Inspection
Symmetric and straight
No discharge or flaring
Uniform color
No discharge and/or flaring
noted. Symmetrical on both
sides. Also uniform in color.
NORMAL
2. Presence of redness,
swelling, growths & discharge
or nares using the flashlight
Inspection
Mucosa pink
Clear, watery discharge
No lesions.
Mucosa is intact and pinkish;
minimal moist noted inside; no
swelling or nodules found.
NORMAL
3. Position of nasal septum Inspection
Nasal septum intact and in
midline, intact
Nasal septum is intact and in
midline
NORMAL
4. Test patency of both nasal
septum
Inspection
Air moves freely as the client
breathes through the nares
Air moves freely as the client
breathes through each nares
NORMAL
5. Tenderness, masses &
displacement of bone &
cartilage
Palpation Not tender; no lesions
No tenderness, no lesions
noted. No displacement of
bone & cartilage.
NORMAL
SI NUSES
1. Presence of tenderness Palpation Not tender
Not tenderness noted.
NORMAL
LI PS
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
1. Symmetry of contour color
& texture
Inspection and Palpation
Uniform pink color (darker,
e.g., bluish hue, in
Mediterranean groups and
dark-skinned clients)
Soft, moist, smooth texture
Symmetry of contour
Ability to purse lips
Uniform pink color, smooth,
soft and symmetrical. Client is
able to purse lips.
NORMAL
BUCCAL MUCOSA
1. Color, moisture, texture &
presence of lesions
Inspection and Palpation
Uniform pink color (freckled
brown pigmentation in dark-
skinned clients)Moist, smooth,
soft, glistening, and elastic
texture (drier oral mucosa in
elderly due to decreased
salivation)
Uniform pink color. Moist,
smooth, glistening and elastic
texture.
NORMAL
TEETH
1. Inspect for color, number &
condition & presence of
dentures
Inspection
32 adult teeth
Smooth, white, shiny tooth
enamel
2Loss Molar tooth,
1Tooth Decay at the molar
Deviation from normal due to
improper mouth care.
GUMS
1. Color & condition Inspection
Pink gums (bluish or dark
patches in dark-skinned
clients)
Pink gums, moist, firm, no
noted lesions and nodules
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
Moist, firm texture to gums
TONGUE/FLOOR OF THE MOUTH
1. Color & texture of the
mouth floor & frenulum
Inspection and Palpation
Smooth tongue base with
prominent veins
Smooth tongue base with
prominent veins
NORMAL
2. Position, color & texture,
movement & base of the
tongue
Inspection and Palpation
Central in position
Pink in color (some brown
pigmentation on tongue
borders in dark-skinned
clients); moist; slightly rough;
thin white coating
Smooth, lateral margins, no
lesions
Raised papillae (taste buds)
Moves freely, no tenderness
Centered; slightly pink in
color, moist, slightly rough,
has thin white coating,
smooth, no lesions; moves
freely.
NORMAL
PALATES & UVULA
1. Color & shape, texture &
presence of bony prominences
Inspection and Palpation
Soft palate- light pink, smooth,
no lesions, moist.
Hard palate- lighter pink, more
irregular texture/ridges no
lesions
Light pink, smooth and moist
soft palate.
Light pink, irregular textured
and moist hard palate.
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
No noted nodules or masses
2. Position of the uvula &
mobility
Inspection
Positioned in midline of soft
palate.
Midline of soft palate NORMAL
OROPHARYNX & TONSI LS
1. Color & texture Inspection and Palpation
Pink and smooth posterior
wall.
Smooth and pinkish posterior
wall
NORMAL
2. Size of the tonsils, color &
discharge
Inspection
Tonsils are of normal size or
not visible, pink in color and
smooth. No discharge.
Tonsils are normal size or not
visible, smooth and pink in
color. No discharge noted.
NORMAL
3. Gag reflex Inspection Present Present NORMAL
NECK & LYMPH NODES
1. Symmetry & visible mass in
the thyroid gland
Inspection Not visible on inspection
Symmetric and not visible
upon inspection.
NORMAL
2. Presence of tenderness or
nodules in the lymph nodes
Inspection and Palpation Not palpable. No nodules were palpated NORMAL
3. Placement of the trachea Inspection
Central placement in midline
of neck, spaces are equal on
both sides.
Trachea is placed at the center.
Spaces are equal on both sides.
NORMAL
4. Smoothness & areas of
enlargement, masses or
nodules in the thyroid gland
Inspection
Lobes may not be palpitated.
If palpitated, lobes are small,
smooth, centrally located,
painless, and rise freely with
swallowing.
Lobes were not palpated. Rise
freely when swallowing.
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
BREAST
1. Symmetry and visible
mass in the breast.
Inspection
Symmetrical, no visible
masses upon inspection.
Symmetrical, no visible
masses upon inspection.
NORMAL
1. Color, moisture,
texture and presence of
lesion
Inspection and Palpation
Uniformity in color, moisture
and texture. No presence of
lesion.
Uniform in color, no lesion
was noted
NORMAL
POSTERI OR THORAX
1. Shape, symmetry &
compare the diameter of
antero posterior thorax to
transverse diameter
Inspection
Anteroposterior to transverse
diameter ratio of 1:2, chest is
symmetric.
1:2 ratio of the anteroposterior
to transverse diameter is
symmetric.
NORMAL
2. Spinal alignment Inspection Spine vertically aligned. Spine is vertically aligned. NORMAL
3. Breathing excursion Inspection No adventitious breath sounds.
NoAdventitious breathing was
inspected.
NORMAL
5. Temperature, tenderness,
masses
Palpation
Uniform skin temperature, no
masses or tenderness.
No mass were palpated and
uniform skin temperature.
NORMAL
7. Percuss the posterior thorax Percussion
Percussion notes resonate,
except over scapula.
Lowest point of resonance is at
the diaphragm.
Resonant sound was heard at
the upper portion and dull
sound was heard over the
scapula.
NORMAL
8. Auscultate the posterior
thorax
Auscultation
Vesicular and
bronchovesicular breathe
sounds.
Bronchovesicular sound was
heard at the upper portion and
vesicular sound was heard at
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
the lower portion of the
thorax.
ANTERI OR THORAX
1. Breathing pattern Inspection
Quiet, rhythmic, and effortless
respirations.
Wheezing sounds
2. Temperature, tenderness,
masses
Inspection and Palpation
Uniform skin temperature, no
masses or tenderness.
Uniform skin temperature,
neither masses nor tenderness
was palpated.
NORMAL
5. Percuss the anterior thorax Percussion
Percussion notes resonate
down to the sixth rib at the
level of the diaphragm but are
flat over areas of heavy muscle
and bone, dull on areas over
the heart and the liver, and
tympanic over the underlying
stomach.
Resonant sound was heard
down to the sixth rib at the
level of the diaphragm. On the
other hand, flat sound was
heard over heavy muscles, and
dull on the areas of the heart
and liver.
NORMAL
6. Auscultate the trachea Auscultation
Bronchial and tubular breath
sounds.
Bronchial and tubular breath
sounds were heard
NORMAL
7. Auscultate the anterior
thorax
Auscultation
Bronchovesicular and
vesicular breath sounds.
Bronchovesicular and
vesicular breath sounds were
heard.
NORMAL
CAROTI D ARTERI ES
1. Pulsation of carotid arteries Palpation No pulsations, lifts or heaves.
No pulsations and lifts
observed.
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
2. Auscultation of the carotid
arteries
Auscultation
No sound heard on
auscultation.
No sound was heard upon
auscultation.
NORMAL
J UGULAR VEI N
1. Visibility of jugular vein Inspection Veins not visible.
Veins were not visible upon
inspection.
NORMAL
ABDOMEN
1. Skin integrity Inspection
Unblemished skin, uniform in
color, silver white striae
(stretch marks) or surgical
scars.
Uniform in color.
Surgical Incision at the right
Lower quadrant(RLQ)
Deviation from normal due to
surgical incision.
2. Abdominal contour Inspection
Flat, rounded (convex) or
scaphoid(concave)
Convex in shape. NORMAL
3. Enlarge liver or spleen Palpation
No evidence of enlargement of
liver or spleen.
No enlargement was observed. NORMAL
4. Symmetry of contour Inspection Symmetric contour. Symmetric contour. NORMAL
5. Abdominal movements Inspection
Symmetric movements caused
by respiration. Visible
peristalsis in very lean people.
Aortic pulsations in thin
persons at epigastric area.
Symmetric movement due to
respiration. Peristalsis not
visible.
NORMAL
6. Vascular patterns Inspection No visible vascular pattern.
No visible vascular pattern.
NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
7. Bowel sounds, vascular
sound & peritoneal sounds
Auscultation
Audible bowel sounds,
absence of arterial bruit and
friction rubs.
No arterial bruit was heard.
Audible bowel sound.
NORMAL
8. Percuss abdominal
quadrants
Percussion
Tympanic sound over the
stomach and gas-filled bowels;
dullness, especially over the
liver and spleen or in full
bladder.
Uncomfortable for the client
to percuss because of the
surgical incision in the
abdomen.
9. Light palpation of
abdominal quadrants
Palpation
Tenderness may be present
near xiphoid process, over
cecum, and over sigmoid
colon.
Uncomfortable for the client
to palpate because of the
surgical incision in the
abdomen
MUSCOLOSKELETAL SYSTEM
1. Muscle size compare the
muscles on one side of the
body (arm, thigh, calf) to the
same muscle on the other side
Inspection
Equal size on both sides of
body.
Equal on both sides of the
body.
NORMAL
2. Constructures (shortening)
of the muscles & tendons
Inspection No contractures. No contractures. NORMAL
3. Muscle fasciculations &
tremors. Presence of tremors
of the hands & arms when
stretched in front of the body
Inspection No tremors. No tremors. NORMAL
4. Muscle tonicity Inspection Normally firm. Firm. NORMAL
PARTS TO BE ASSESSED TECHNIQUE NORMAL FINDINGS ACTUAL FINDINGS REMARKS
5. Muscle strength Inspection
Equal strength on each body
side.
Equal strength on each body
side.
NORMAL
BONES
1. Normal structure Inspection No deformities. No deformities NORMAL
2. Edema & tenderness Inspection No tenderness or swelling. No tenderness. NORMAL
J OI NTS
1. Swelling Inspection No swelling. No swelling. NORMAL
2. Presence of tenderness,
smoothness of movement,
swelling, crepitation &
presence of nodules
Inspection
No tenderness, swelling,
crepitation or nodules. Joints
move smoothly.
Joints move smoothly. No
tenderness was observed.
NORMAL
RANGE OF MOTI ON
1. Upper extremities Inspection
Uniform in color, veins are
visible in face, neck and
dorsum of the hands, average
muscles size, fingers are
complete
No lesions, no edema.
Uniform in color, veins are
visible in face, neck and
dorsum of the hands, average
muscles size, fingers are
complete.Skin Lesions due to
IV insertion, no edema.
NORMAL
2. Lower extremities Inspection
Uniform in color, no
deformities, complete fingers
in both feet.
Uniform in color, no
deformities, complete fingers
in both feet.
NORMAL
B. DIAGNOSTIC PROCEDURE / LABORATORY
LABORATORY
PROCEDURE
DATE
ORDERED/DATE
RESULT
INDICATION/PURPOSES NORMAL
VALUES
ACTUAL
VALUES
NURSING
RESPONSIBILITY
ANALYSIS /
INTERPRETATION
URINALYSIS
08/23/13
Performed to check for
urinary tract infection
occassionaly the urine screen
may pick up other
abnormalities of renal
functions such as excess
sugar or protein.
Color:yello
w
Ph: 7.0
SP Gravity:
1.005
Macroscopic
Color:yellow
Character:haz
y
Protein: (-)
Sugar: (-)
Ph: 7.0
SP Gravity:
1.020
Microscopic
Pus cells: 0-1
hpf
RBC:
Epithelial
cells:
Bacteria-(-)
Mucous
thread:
Casts:
Crystals:
All materials should
be clean for urine
analysis, gather only
midstream urine.
NORMAL
COMPLETE
BLOOD COUNT
08/23/13 It is used to check
for blood diseases
and disorders
,infections in the
blood ,oxygen levels
in the blood
,diabetes, kisner and
liver diseases and
host of ailments
WBC: 4.0-12.0
LYM: 0.8-7.0
MIDSIZED CELL:
0.1-1.5
GRAN: 2.0-8.0
LYM%:20.0-60.0
MIDSIZED
CELL%:3.0-15.0
GRAN%: 40.0-70.0
RBC: 4.00-6.00
HGB: 110-160
HCT:35.0-49.0
MCV:80.0-100.0
MCH:27.0-34.0
MCHC:310-370
RDW-CV:11.0-16.0
RDW-SD:35.0-56.0
PLATELET:150-400
WBC: 12.5
LYM: 1.4
MIDSIZED CELL:
0.7
GRAN: 9.6
LYM%:12.2
MIDSIZED
CELL%:5.9
GRAN%: 81.9
RBC: 5.46
HGB: 141
HCT:43.9
MCV:80.5
MCH:25.8
MCHC:321
RDW-CV:13.5
RDW-SD:41.0
PLATELET:465
Explain the
procedure to the
client
WBC indicates the
presence of an
infection
granulocytes
indicates a reaction
to an infection
lymphocytes count
indicates increased
rates of infection
after surgery or
trauma
platelets indicates
inflammation
CREATININE 08/23/13 It is used to find out
if the client has
signs of renal failure
44.2-150.3
Na: 135-148
K: 3.5-5.3
C: 1.1-1.3
Cl: 96-107
52.2 umo/l
133.5mmol/l
3.74
99.2
Explain the
procedure to the
client
normal
V. THE PATIENT AND HIS CARE
A. MEDICAL MANAGEMENT
I. INTRAVENOUS FLUID
MEDICAL MANAGEMENT DATE ORDERED/DATE
GIVEN/CHANGED/DISCONTINUED
GENERAL DESCRIPTION NURSING RESPONSIBILITY
D50.9 NaCl
21-22 gtts/min
08/23/13 Dextrose and Sodium
Chloride Injection, is a sterile,
nonpyrogenic solution for
fluid
and electrolyte replenishment
and caloric supply in single
dose containers
for intravenous administration.
Prior:
-Check the physicians order in thrice check
-Explain to the client the antibiotics and IV that the
patient will encounter
-Monitor the vital signs
-Determine the allergies to th antibiotics
-Prepare the client for the surgery
During:
-Check for the physicians order of doses
-Check for the gtts/min
-Check for the time management of the medicines
-Monitor the clients response
-Assess the vital signs
After:
-Monitor the vital signs and the clients
reaction/response
-Check for the physicians order
-Monitor the ugtts/min
-Time of the medication
-Report and document the procedure
D5 WATER Dextrose provides a source of calories. Prior:
Dextrose is readily metabolized, may
decrease losses of body protein and
nitrogen, promotes glycogen deposition
and decreases or prevents ketosis if
sufficient doses are provided
-Check the physicians order in thrice
check
-Explain to the client the antibiotics and
IV that the patient will encounter
-Monitor the vital signs
-Determine the allergies to th antibiotics
-Prepare the client for the surgery
During:
-Check for the physicians order of doses
-Check for the gtts/min
-Check for the time management of the
medicines
-Monitor the clients response
-Assess the vital signs
After:
-Monitor the vital signs and the clients
reaction/response
-Check for the physicians order
-Monitor the ugtts/min
-Time of the medication
-Report and document the procedure
II. DRUGS
NAME MECHANISM OF
ACTION
INDICATION CONTRAINDICATION SIDE EFFECTS NURSING
RESPONSIBILITIES
Generic Name:
Cefuroxime
Frequency:
TID
Dosage:
1tab 500mg q8
Route:
OP
Second-generation
cephalosporin that
inhibits cell wall
synthesis, promoting
osmotic instability,
usually bactericidal.
It is used for surgical
prophylaxis, reducing or
eliminating infection.
Hypersensitivity to
cephalosporin and related
antibiotics.
GI:
Diarrhea, nausea,
antibiotic-associated
colitis.
SKIN:
rashes, pruritus, urticaria
Determine history
of
hypersensitivity
reactions to
cephalosporins,
penicillins, and
history of
allergies,
particularly to
drugs before
therapy is
initiated.
Inspect IM and IV
injection sites
frequency for
signs of phlebitis.
Report of loose
stools or diarrhea.
Monitor I&O
rates and pattern.
NAME MECHANISM OF
ACTION
INDICATION CONTRINDICATION SIDE EFFECTS NURSING
RESPONSIBILITIES
Generic Name:
Cefuroxime
Frequency:
TID
Dosage:
750mg q8
Route:
IV
Second-generation
cephalosporin that
inhibits cell wall
synthesis, promoting
osmotic instability,
usually bactericidal
It is used for surgical
prophylaxis, reducing or
eliminating infection.
Hypersensitivity to
cephalosporins and
related antibiotics
GI:
Diarrhea, nausea,
antibiotic-associated
colitis.
SKIN:
rashes, pruritus, urticaria
Determine
history of
hypersensitivity
reactions to
cephalosporins,
penicillins, and
history of
allergies,
particularly to
drugs before
therapy is
initiated.
Inspect IM and
IV injection sites
frequency for
signs of phlebitis.
Report of loose
stools or diarrhea.
Monitor I&O
rates and pattern.
NAME MECHANISM OF
ACTION
INDICATION CONTRAINDICATION SIDE EFFECTS NURSING
RESPONSIBILITIES
Generic Name:
Ketorolac
Frequency:
TIV
Dosage:
10mg q8 (-) anst
Route:
IV
Anti-inflammatory and
analgesics activity,
inhibits prostaglandins
and leukotriene
synthesis.
Short term management
of pain.
Contraindicated with
significant renal
impairment,
hypersensitivity to Non-
Steroidal Anti
Inflammatory Drugs.
rash
ringing in the
ears
headache
dizziness
drowsiness
abdominal pain
nausea
diarrhea
constipation
heartburn
fluid retention
Pain as well as
inflammation and
its signs and
symptoms
redness, swelling,
fever and pain as
reduced.
Instruct client to
report any
adverse reaction
to the physician
or nurse. Tell the
patient that
adverse reaction
can occur with
overuse.
NAME MECHANISM OF
ACTION
INDICATION CONTRAINDICATION SIDE EFFECTS NURSING
RESPONSIBILITIES
Generic Name:
Ranitidine
Frequency:
TID
Dosage:
25mg q8
Route:
IV
Inhibits the action of
histamine at the H2
receptor site located
primarily in gastric
parietal cell. resulting in
inhibition of gastric acid
secretion.
Used prevent ulcer while
patient is on NPO.
Hypersensitivity to
ranitidine or any
component of the
formulation.
constipation
diarrhea
fatigue
headache
insomnia
muscle pain
nausea
vomiting
agitation
depression
bleeding
C- Gastrointestinal
agent, antisecretory (H2
receptor antagonist)
H- Reduced amount of
acid in the stomach that
may result to prevented
ulcer incidence.
E- Every 8hrs while
patient is on NPO.
C- Instruct client to
report any adverse
reaction to the physician
or nurse. Tell patient
antacids may decrease
the absorption of
ranitidine.
K- Ranitidine can
interfere with the
metabolism of alcohol.
NAME MECHANISM OF
ACTION
INDICATION CONTRINDICATION SIDE EFFECTS NURSING
RESPONSIBILITIES
Generic Name:
Mefenamic acid
Frequency:
TID
Dosage:
250mg 1cap
Route:
PO
Anti-inflammatory and
analgesic activity.
For relief of mild to
moderate pain in patients
12yrs 0ld and above.
Active ulceration or
chronic inflammation of
either the upper or lower
GI tract, preexisting renal
desease.
rash
ringing of ears
nausea
heartburn
It comes as a
capsule to be
taken by mouth.
It is usually taken
every 4 to 6 hours
on a schedule or
as needed for
pain.
III. DIET
Type of Date Ordered, General Description Indication/Purposes Specific Food Clients Nursing Responsibilities
Diet Date Changed Taken Response
Prior During After
NPO August 23-25,
2013
NPO dietary state in which patient is
force to take nothing by mouth over a
given period of time.
Normally instructed to pre- op patient
and patient that have to undergo a
certain laboratory examination.
Ex. serum electrolyte.
Cleanse the GI
tract from any
impurities and
maintains
immobility of the
tract.
During OR
procedure.
Nothing Per
orem
Feeling
weak,
restlessnes
s noted
Check for
doctors
order
Explain to
the client
what is
NPO and its
purpose
Make sure
that patient
followed
doctors
order
Document
date and
time. Noted
positive
gastric
motility.
General
Liquid
August 27,
2013
Diet contains only liquids or foods
turn to liquid at body temperture
Liquid diets are
ordered after
surgery to reduce
the nausea and
vomiting that
sometimes result
from the
anesthetic,
medications or the
surgery itself.
Liquids are
tolerated better
than solids and
allow the
gastrointestinal
tract to ease its
way back into
40 gms
Nissan soup
3 glass of
water
Feeling
weak
Check for
doctors
order
Explain to
the client
what is
General
Liquid and
its purpose
Make sure
that patient
followed
doctors
order
Document
date and
time. Noted
positive
gastric
motility.
operation.
DAT
with
SAP
Diet as
tolerated
with
Strict
aspiratio
n
precauti
on
August 28, 13 Aspiration precautions are measures
taken to prevent a person from
aspirating, or choking. Aspiration can
occur in debilitated patients who have
a diminished swallowing reflex, and
the condition can even cause a type
of pneumonia called aspiration
pneumonia. Typically, when a person
swallows, the contents pass through
the esophagus and into the stomach.
Aspiration occurs when the
swallowed contents do not pass
through the esophagus, but go
directly into the lungs.
To prevent
aspiration.
72 Diet Recall
No signs
of
aspiration
Check
physicians
order
Monitor
vital signs
Monitor
intake
& output
Check Vital
signs
IV. ACTIVITY EXERCISE
TYPE OF
EXERCISE
DATE
ORDERED,DATE
TAKEN/GIVEN,DATE
OF CHANGE,DATE
OF DISCONTINUE
GENERAL
DESCRIPTION
INDICATION/PURPOSES
CLIENTS
RESPONSE
NURSING RESPONSIBILITIES
(prior,during,after)
Ambulation
Started: August 27, 2013
- The act of
traveling by
foot ; walking
is healthy for
exercise
- It can help prepare and
condition the body for
the stress that the suture
will cause
- Improves muscle tone in
legs
- To stimulate the lower
extremities circulation
after the appendectomy
with the ambulation
- The patient
can
facilitate to
walk with a
slow
movement
Prior :
- Assess the client if he can walk dependently
- Explain to the client the purpose of
ambulation
During :
- Encourage the patient to walk dependently
with minimal movement for atleast 30 mins.
After :
- Instruct the client to take a rest
V. SURGICAL MANAGEMENT
I. Brief Description of the Procedure
An appendectomy is surgery to remove the appendix. An appendectomy is done using Spinal anesthesia. Medicine is put into your back to make you numb below
your waist. You will also get medicine to make you sleepy.
The surgeon makes a small cut in the lower right side of your belly area and removes the appendix.
If the appendix broke open or a pocket of infection (abscess) formed, your abdomen will be washed out during surgery. A small tube may be left in the belly area to
help drain out fluids or pus.
II. Patients response to Procedure
After the appendectomy, the client stays in the hospital for about Eight days. According to the client he can feel discomfort and slight pain in surgical site because of
the suture. But when we interviewing the client, he is calm. And he is always asleep.
III. Nursing Responsibilities
Prior:
- Check the doctors order.
- Monitor the vital signs
- Medicines for fever.
- If fever, must be lowered before anesthesia.
During:
- Check for the doctors order
- Check for the time management of the medicines
- Monitor the clients response
- Assess the vital signs
After:
- Monitor the vital signs and the clients reaction/response
- Check for the doctors order
- One day after surgery patients are encouraged to sit up in bed for 2 30 minutes.
- On the second day the patient can stand and sit outside the room.
- Report and document the procedure
VI. NURSING PROBLEM PRIORITIZATION
Date Identified Cues Problem/ Nursing Diagnosis Justification
August 27, 2013 Due to surgical incision. Acute Pain Because he underwent appendectomy.
August 27, 2013 Due to surgical incision. Impaired skin integrity. Because of the presence of incision site at the right
lower quadrant of the abdomen.
August 27, 2013 Due to unfamiliar environment and
frequent interruptions.
Disturbed sleeping pattern. Because the client has been admitted for __ days at
the hospital.
August 27, 2013 Due to his lack of interest in food
and poor muscle tone.
Imbalanced nutrition: Less
than body requirement
Because he underwent appendectomy.
August 27, 2013 Due to inadequate primary defense. Risk for infection. Because of the presence of incision site at the right
lower quadrant of the abdomen.
VII. NURSING CARE PLAN No. 1
Assessment
Nursing
Diagnosis
Planning Intervention Rationale Evaluation
Subjective:
Masakit yung
tahi ko ,as
verbalized
by the client.
Objective:
Facial Grimace
Pain scale of
5/10.
Guarding
behavior
Acute pain related
to distention of
intestinal
tissues by
inflammation
as manifested
by facial
grimace,
muscle
guarding and a
pain scale of
5/10.
Short term goal:
After 30 minutes of
nursing
intervention, the
client will be
able to verbalize
alleviation of
pain, from a pain
scale of 5/10 to
2/10.
Long term goal:
Within 2 hours, the
client will be
able to report
that pain is
relieved/controll
ed
Within 2 hours, the
client will be
able to follow
prescribed
pharmacological
regimen.
Independent
Encourage use of
relaxation
techniques such
as focus,
breathing,
imaging, CDs or
tapes
Encourage
verbalization of
feelings about
the pain.
Encourage
adequate rest
period.
Keep in rest in
Semi Fowlers
Position.
To distract attention and reduce
tension
To serve as baseline data.
To prevent fatigue.
Gravity localize inflammatory
exudates into lower abdomen
or pelvis, relieving abdominal
pain, which is accentuated by
supine position.
Long term goal:
GOAL MET
Short term goal:
GOAL MET
NURSING CARE PLAN No. 2
Within 2 hours, the
client will be
able to
demonstrate use
of relaxation
skills and
diversional
activities are
indicated for
individual
situation.
Dependent
Take medicines as
prescribed
To alleviate the pain that the
client is experiencing.
Assessment
Nursing
Diagnosis
Planning Intervention Rationale Evaluation
Subjective:
Kumakati
yung tahi
koas
verbalized
by the client.
Objective:
Facial Grimace
Surgical
incision at the RLQ
of the abdomen.
Impaired skin
integrity related
to disruption of
skin surface as
manifested by
presence of
surgical
incision.
Short term goal:
After 30 minutes of
nursing
intervention, the
client and
significant others
will be able to
gain knowledge
and information
about treatment
needs and
potential
complications.
Independent
Instruct proper
handwashing.
Inspet incision
site/dressing.
Note for
fever,chills,
diaphoresis, and
increasing
abdominal pain.
Reduces risk of spread of
bacteria.
Provides early detection of
developing infectious process.
Suggestive of presence of
infection/developing sepsis,
abscess, peritonitis.
Long term goal:
GOAL MET
Short term goal:
GOAL MET
NURSING CARE PLAN No. 3
Long term goal:
Within 2 hours, the
client will be
able to achieve
timely wound
healing and be
free of signs of
infection and
inflammation,
purulent
drainage and
fever.
Dependent
Take medicines as
prescribed
To alleviate the pain that the
client is experiencing.
Assessment
Nursing
Diagnosis
Planning Intervention Rationale Evaluation
Subjective:
Nahihirapan
akong
makatulog
dito ,as
verbalized
by the client.
Objective:
Facial Grimace
# or more
times nighttime
awakenings.
Disturbed
sleeping pattern
related to
environmental
noise,
unfamiliar
furnishings, and
interruptions
for
therapeutics,
monitoring and
lab tests.
Short term goal:
After 30 minutes of
nursing
intervention, the
client will be
able to verbalize
plans to
implement
bedtime routines.
Long term goal:
Within 2 hours, the
client will be
Independent
Assess client's sleep
patterns and usual bedtime
rituals and incorporate these
into the plan of care.
Observe client's medication,
diet, and caffeine intake.
Look for hidden sources of
caffeine, such as over-the-
counter medications.
To provide baseline
information.
Difficulty sleeping
can be a side effect of
medications such as
bronchodilators;
caffeine can also
interfere with sleep.
Long term goal:
GOAL MET
Short term goal:
GOAL MET
able to awaken
refreshed and not
fatigued during
the day.
.
Provide pain relief shortly
before bedtime and position
client comfortably for sleep.
Clients have reported
that uncomfortable
positions and pain are
common factors of
sleep disturbance
VI. DISCHARGE PLANNING
I. M-MEDICATION TO TAKE
Instruct and explain to the patients mother that the medication is very important to continue depending on the duration that the doctor ordered for the total recovery
of the patient.
II. E-EXERCISE
Instruct the mother to let her child for early ambulation
III. T-TREATMENT
Client undergone Appendectomy
IV. H-HEALTH TEACHING
Encourage and explain to the patients mother that it is important to maintain proper hygiene to prevent further infection. Instruct the patients mother to bath the
child every day.
V. O-OUT PATIENT FOLLOW-UP
Hes follow up check will be on September 03, 2013 and regular consultation to the physician can be a factor for recovery and assess and monitor the patients
condition.
VI. D-DIET
Diet as tolerated
VII. S- Sex/ Spiritual
The client is a boy needs to focus on Gods wisdom with his parents.
VII. CONCLUSION
We therefore conclude that after case presentation we nursing students will gain knowledge about Appendicitis, Enumerate signs and symptoms of
Appendicitis, Identify nursing interventions to be done when handling patient with Appendicitis, Perform proper nursing care to patient.
VIII. BIBLIOGRAPHY
http://www.webmd.com/digestive-disorders/digestive-diseases-appendicitis
http://www.medicinenet.com/appendicitis/article.htm
http://www.nlm.nih.gov/medlineplus/ency/article/000256.htm
Medical Surgical .. Brunner and Sudhhart
Você também pode gostar
- Dyspepsia (Gastritis) Case StudiesDocumento9 páginasDyspepsia (Gastritis) Case StudiesJessica Nurin Graman100% (1)
- CYSTOCLYSIS3Documento9 páginasCYSTOCLYSIS3Alvin OccianoAinda não há avaliações
- Nursing Care Plan For Breast Cancer NCP PDFDocumento2 páginasNursing Care Plan For Breast Cancer NCP PDFMaina BarmanAinda não há avaliações
- 2 Teaching Plan For AppendicictisDocumento1 página2 Teaching Plan For AppendicictisHarris CacanindinAinda não há avaliações
- CASE STUDY - Community Acquired Pneumonia With Pleural Effusion & UTIDocumento73 páginasCASE STUDY - Community Acquired Pneumonia With Pleural Effusion & UTIFrancis AdrianAinda não há avaliações
- HernioplastyDocumento6 páginasHernioplastyCherry Delos ReyesAinda não há avaliações
- Ongoing AppraisalDocumento2 páginasOngoing AppraisalLouisa Marie MirandaAinda não há avaliações
- Case Study ReportDocumento23 páginasCase Study Reportapi-290866384Ainda não há avaliações
- Velez College of Nursing F. Ramos Street, Cebu CityDocumento57 páginasVelez College of Nursing F. Ramos Street, Cebu Cityinah krizia lagueAinda não há avaliações
- Case Study Pleural EffusionDocumento4 páginasCase Study Pleural EffusionKhristine Anne FabayAinda não há avaliações
- Pulmonary Tuberculosis: A Case Study ofDocumento28 páginasPulmonary Tuberculosis: A Case Study ofDyanne BautistaAinda não há avaliações
- DM & DI ExamsDocumento11 páginasDM & DI ExamsTomzki CornelioAinda não há avaliações
- NCP Micu Hascvd Cad - RioDocumento5 páginasNCP Micu Hascvd Cad - RioRio BonifacioAinda não há avaliações
- Discharge Plan For Pneumonia PatientsDocumento2 páginasDischarge Plan For Pneumonia PatientsClark David PanganibanAinda não há avaliações
- NCP Icu-CcuDocumento6 páginasNCP Icu-CcuJohn CenasAinda não há avaliações
- Learning Feedback DiaryDocumento1 páginaLearning Feedback DiaryVhince PiscoAinda não há avaliações
- Nursing Care PlanDocumento5 páginasNursing Care PlanPaola Marie VenusAinda não há avaliações
- Upon Admission (15 PTS) in The Intensive Care Unit (15 PTS) : ? (5 Pts Each Parameter A Total of 15 Points)Documento5 páginasUpon Admission (15 PTS) in The Intensive Care Unit (15 PTS) : ? (5 Pts Each Parameter A Total of 15 Points)Janelle Cabida SupnadAinda não há avaliações
- Appendectomy Case StudyDocumento16 páginasAppendectomy Case StudyMahmoud Al Abed100% (1)
- IDocumento6 páginasInoronisa talusobAinda não há avaliações
- Discharge Care PlanDocumento2 páginasDischarge Care PlanLaurinda Angelica Dimaiwat PrestadoAinda não há avaliações
- Individual Case Study Acute GlomerulonephritisDocumento26 páginasIndividual Case Study Acute GlomerulonephritisBatrisyia HalimsAinda não há avaliações
- Tuberculosis Case StudyDocumento43 páginasTuberculosis Case StudyAJIgama100% (1)
- Hyperthermia and Risk For AspirationDocumento3 páginasHyperthermia and Risk For AspirationAlmyr RimandoAinda não há avaliações
- Cholelithiasis GRAND CASE PRESDocumento52 páginasCholelithiasis GRAND CASE PRESKyle Cholo CholoAinda não há avaliações
- Learning Feedback DiaryDocumento10 páginasLearning Feedback DiaryLoids IgnacioAinda não há avaliações
- PYOMYOSITISDocumento12 páginasPYOMYOSITISPaolo VillaAinda não há avaliações
- NCP For CKDDocumento4 páginasNCP For CKDMinhwa KimAinda não há avaliações
- A Case Study In:: Hirschsprung DiseaseDocumento18 páginasA Case Study In:: Hirschsprung DiseaseJaimie La PenaAinda não há avaliações
- Charting CraniotomyDocumento1 páginaCharting CraniotomyJrBong SemaneroAinda não há avaliações
- NCP - Acute PainDocumento1 páginaNCP - Acute PainjsthrAinda não há avaliações
- NURSING CARE PLAN For TB 2003Documento6 páginasNURSING CARE PLAN For TB 2003Princess Andrea Bulatao100% (1)
- CASE Study PTB 2Documento53 páginasCASE Study PTB 2Hedda Xyza PascuaAinda não há avaliações
- Appendectomy Appendicitis Case Study1Documento18 páginasAppendectomy Appendicitis Case Study1Los Devio100% (1)
- ARTHROCENTESISDocumento2 páginasARTHROCENTESISJairene Dave Martinez CambalonAinda não há avaliações
- DP For Acute Respiratory FailureDocumento1 páginaDP For Acute Respiratory FailurePauline SalgadoAinda não há avaliações
- HoplessnessDocumento16 páginasHoplessnessHamza IshtiaqAinda não há avaliações
- DMDocumento24 páginasDMJudeLaxAinda não há avaliações
- Related Learning Experience: Learning Outcomes Day ProceduresDocumento2 páginasRelated Learning Experience: Learning Outcomes Day ProceduresGee RidadAinda não há avaliações
- Care of The Client With Pulmonary Tuberculosis Utilizing Orem's TheoryDocumento13 páginasCare of The Client With Pulmonary Tuberculosis Utilizing Orem's TheoryRazel Kinette AzotesAinda não há avaliações
- In Partial Fulfillment of The Requirements in Surgical Ward RotationDocumento3 páginasIn Partial Fulfillment of The Requirements in Surgical Ward RotationEdgie FabreAinda não há avaliações
- NCA2 PosttestsDocumento20 páginasNCA2 PosttestsCzarena Ysabelle PayotAinda não há avaliações
- BSN 215 Reflection Essay - LagoDocumento2 páginasBSN 215 Reflection Essay - LagoAlliahkherzteen LagoAinda não há avaliações
- USC Case 04 - SinusitisDocumento9 páginasUSC Case 04 - SinusitisDisti Damelia SebayangAinda não há avaliações
- Developmental DataDocumento3 páginasDevelopmental DataRia ArcaneAinda não há avaliações
- Pulmonary Tuberculosis Health TeachingDocumento3 páginasPulmonary Tuberculosis Health Teachinggenellemaarte100% (1)
- CASE Study PTBDocumento52 páginasCASE Study PTBbennettchuaAinda não há avaliações
- Family Case Study-BibliographyDocumento1 páginaFamily Case Study-BibliographyKatherine 'Chingboo' Leonico LaudAinda não há avaliações
- Case Presentation CsDocumento18 páginasCase Presentation CsgenzpogiiAinda não há avaliações
- Case Study 18Documento4 páginasCase Study 18api-271284613Ainda não há avaliações
- Chronic Renal Failure - Case Study (Group)Documento35 páginasChronic Renal Failure - Case Study (Group)Coleen Mae CamaristaAinda não há avaliações
- AcknowledgementDocumento9 páginasAcknowledgementjhzenAinda não há avaliações
- Health Care Delivery System & COPARDocumento52 páginasHealth Care Delivery System & COPARDharylle Cariño100% (1)
- Word Ncp.......... TetanusDocumento3 páginasWord Ncp.......... TetanusYvounne Ananias Bautista RNAinda não há avaliações
- Meniere's Disease - Case StudyDocumento3 páginasMeniere's Disease - Case StudyZORANASNAinda não há avaliações
- Acute Tonsil Lo PharyngitisDocumento27 páginasAcute Tonsil Lo PharyngitisCheysser Alagao50% (2)
- Posterior Mold: PurposeDocumento3 páginasPosterior Mold: PurposeSheryl Ann Barit PedinesAinda não há avaliações
- NCP ModsDocumento6 páginasNCP ModsNickos Andrew Magno Asanza Jr.Ainda não há avaliações
- AcuteAppendicitis-BSN 4ADocumento28 páginasAcuteAppendicitis-BSN 4ALynetteCantosAinda não há avaliações
- Pancreatitis Case StudyDocumento48 páginasPancreatitis Case StudyHanna Joyce100% (6)
- Review NleDocumento6 páginasReview NleRio Bonifacio100% (3)
- Nle ReviewDocumento7 páginasNle ReviewRio BonifacioAinda não há avaliações
- Functional Health Pattern Prior To Hospitalization During Hospitalization A. Health - Perception and Health - Management PatternDocumento4 páginasFunctional Health Pattern Prior To Hospitalization During Hospitalization A. Health - Perception and Health - Management PatternRio BonifacioAinda não há avaliações
- NCP PCAP CDocumento4 páginasNCP PCAP CRio Bonifacio100% (2)
- NCP Micu Hascvd Cad - RioDocumento5 páginasNCP Micu Hascvd Cad - RioRio BonifacioAinda não há avaliações
- Pancreatitis Aguda: Erik Rauch Sánchez Médico Gastroenterólogo Febrero 2016. / 999 290 697Documento30 páginasPancreatitis Aguda: Erik Rauch Sánchez Médico Gastroenterólogo Febrero 2016. / 999 290 697NickAinda não há avaliações
- As NZS 3824-1998 Guidelines For Radiotherapy Treatment Rooms DesignDocumento10 páginasAs NZS 3824-1998 Guidelines For Radiotherapy Treatment Rooms DesignSAI Global - APACAinda não há avaliações
- Psychiatric Nursing Mastery Test Part 2Documento16 páginasPsychiatric Nursing Mastery Test Part 2Rika MaeAinda não há avaliações
- Everyone Knows That Joining A Gym Is A QuoteDocumento2 páginasEveryone Knows That Joining A Gym Is A Quotejigar shahAinda não há avaliações
- Alcohol and Drug Abuse Flow ChartDocumento1 páginaAlcohol and Drug Abuse Flow Chartboen jaymeAinda não há avaliações
- ADHD Parent Questionnaire PDFDocumento4 páginasADHD Parent Questionnaire PDFklichtAinda não há avaliações
- TrandolaprilDocumento28 páginasTrandolaprilYeyenJaejoongAinda não há avaliações
- Hyperthermia in Cancer Treatment: Cabuy E. Reliable Cancer Therapies. Energy-Based Therapies. 2011 1 (2) :1-48Documento48 páginasHyperthermia in Cancer Treatment: Cabuy E. Reliable Cancer Therapies. Energy-Based Therapies. 2011 1 (2) :1-48Eliza LlenzaAinda não há avaliações
- Cardiac Surgery in The Adult - 24-41Documento18 páginasCardiac Surgery in The Adult - 24-41Nicola AlkhorayAinda não há avaliações
- ENLS V4.0 ME Manuscript FINALDocumento17 páginasENLS V4.0 ME Manuscript FINALkoko komarudinAinda não há avaliações
- Action Plan For Rejuvenation of River Tunga 1Documento11 páginasAction Plan For Rejuvenation of River Tunga 1anitha_mathanAinda não há avaliações
- Hydra FacialDocumento34 páginasHydra FacialDrAmit Gaba MdsAinda não há avaliações
- HIV Policy MemoDocumento3 páginasHIV Policy MemoZhihong XuAinda não há avaliações
- Passmedicine MRCP Notes-Palliative Medicine and End of Life CareDocumento5 páginasPassmedicine MRCP Notes-Palliative Medicine and End of Life CareMayar WaelAinda não há avaliações
- B PharmacyDocumento26 páginasB PharmacyAkankshaAinda não há avaliações
- JCI-Sentinel Event AlertDocumento3 páginasJCI-Sentinel Event AlertDewi Ratna SariAinda não há avaliações
- Bio Medical Waste Management PPT 25-06-2019Documento47 páginasBio Medical Waste Management PPT 25-06-2019Dark InvaderAinda não há avaliações
- Biochemistry LaboratoryDocumento6 páginasBiochemistry LaboratoryMark Benedict MontalboAinda não há avaliações
- JIAP July 2011 - Guided Tissue Regeneration - A Decision-Making ModelDocumento8 páginasJIAP July 2011 - Guided Tissue Regeneration - A Decision-Making ModelLouis HutahaeanAinda não há avaliações
- NCP DM Group 6Documento4 páginasNCP DM Group 6Jeffrey Calicdan BucalaAinda não há avaliações
- ACLS Study Guide NewDocumento35 páginasACLS Study Guide NewNIRANJANA SHALINIAinda não há avaliações
- Therapeutic Modalities: Prepared By: John Patrick B. de JesusDocumento22 páginasTherapeutic Modalities: Prepared By: John Patrick B. de JesusChiee A. CentinoAinda não há avaliações
- Basic EKG Dysrhythmia IdentificationDocumento40 páginasBasic EKG Dysrhythmia IdentificationIlda Dhe Devis Spaho100% (1)
- Congenital DiseaseDocumento39 páginasCongenital DiseaseRavi SharmaAinda não há avaliações
- JONES Criteria: Rheumatic FeverDocumento5 páginasJONES Criteria: Rheumatic FeverChristopher GarrettAinda não há avaliações
- West Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityDocumento7 páginasWest Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityRegine Marie EspañaAinda não há avaliações
- Storgard Channing WP2Documento6 páginasStorgard Channing WP2Channing StorgardAinda não há avaliações
- Cayman Islands National Youth Policy September 2000Documento111 páginasCayman Islands National Youth Policy September 2000Kyler GreenwayAinda não há avaliações
- Helen K. Sneller: Program, 1996Documento2 páginasHelen K. Sneller: Program, 1996Siddharth NelsonAinda não há avaliações