Escolar Documentos
Profissional Documentos
Cultura Documentos
Coronary Heart Disease Study
Enviado por
renasariDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Coronary Heart Disease Study
Enviado por
renasariDireitos autorais:
Formatos disponíveis
Periodontal Disease and Coronary
Heart Disease
Karen Geismar,* Kaj Stoltze,* Bjarne Sigurd,
Finn Gyntelberg,
and Palle Holmstrup*
Background: Several epidemiological studies have demon-
strated an association between periodontal disease and coro-
nary heart disease (CHD). The association could be a result of
confounding by mutual risk factors. The present study was
undertaken in a Danish population to reveal the signicance
of common risk factors.
Methods: The investigationwas conductedas acase-control
study comprising 250individuals: 110individuals with veried
CHD from a Department of Cardiovascular Medicine and 140
control individuals without CHD from the Copenhagen City
Heart Study. Information on diabetic status, smoking habits,
alcohol consumption, physical activity, school attendance,
household income, body weight and height, triglyceride, and
serum cholesterol was obtained. Full-mouth probing depth
(PD), clinical attachment loss (CAL), bleeding on probing
(BOP), and alveolar bone level (ABL) on radiographs were
registered. ABL was stratied into ABL1 = ABL 2 mm;
ABL2 = ABL >2 to 4 mm; and ABL3 = ABL >4 mm. Multiple
logistic regression models with stepwise backward elimination
were used allowing variables with P <0.15 to enter the multi-
variate analysis.
Results: The CHD group had a signicantly lower out-
come with respect to PD, BOP, CAL, and ABL. For participants
<60 years old, only risk factors such as smoking and diabetic
status entered the multivariate analysis. For the ABL3 group,
there was a signicant association with CHD for participants
<60 years old, the odds ratio being 6.6 (1.69 to 25.6). For par-
ticipants 60 years old, there was no association.
Conclusions: The present study showed a positive associa-
tion between periodontal disease and CHD in agreement with
several other studies. The association was highly age depen-
dent and could only be attributed to diabetes and smoking to
some extent. J Periodontol 2006;77:1547-1554.
KEY WORDS
Case-control study; coronary heart disease; periodontal
disease; risk factors.
W
ithin the past decade, epi-
demiological studies have re-
peatedly shown an association
between periodontal disease and coro-
nary heart disease (CHD). Periodontal
disease and CHD are widespread condi-
tions, and, therefore, an association be-
tween them is an important scientic
subject from a preventive point of view.
Several studies have been conducted
using cohort, cross-sectional, or case-
control designs with varying conclusions
on the strength of the association as re-
viewed by Holmstrup et al.
1
Most of the
results reporting a lack of association
between periodontal disease and CHD
are from prospective studies.
In earlier studies, the measurement of
periodontal disease has ranged fromself-
reported periodontal disease, partial
recording of attachment, the number of
teeth left, and the Russell plaque index
to clinical attachment loss (CAL) and al-
veolar bone level (ABL), but no studies
have been based on full-mouth registra-
tion of CAL and registration of ABL to
our knowledge.
It has been suggested that the spread
of bacteria and bacterial products from
the periodontal lesion to the bloodstream
may contribute to arteriosclerosis and
CHD.
2,3
However, whether an associa-
tion between periodontal disease and
CHD could be causal is still uncertain.
Another explanation for the observed as-
sociation could be that the two disease
entities share common risk factors.
For CHD, several modiable and
non-modiable factors, such as elevated
* Department of Periodontology, School of Dentistry, Faculty of Health Science, University
of Copenhagen, Denmark.
Department of Cardiovascular Medicine, Rehabilitation Unit, Bispebjerg University
Hospital, Copenhagen, Denmark.
Clinic of Environmental and Occupational Medicine, Bispebjerg University Hospital.
doi: 10.1902/jop.2006.050405
J Periodontol September 2006
1547
serum lipids, smoking, diabetes, age, male gender,
low socioeconomic status, hypertension, dyslipide-
mias, and alcohol consumption,
4,5
are generally ac-
cepted risk factors. Studies have also linked several
of these risk factors to periodontal disease, including
smoking, diabetes, age, male gender, and low socio-
economic status. Recently, studies have even shown
that dyslipidemias may be related to periodontal
disease,
6,7
and a few studies have shown that alco-
hol consumption resulted in increased periodontal
disease.
8
In this study, we aimed to test the hypothesis that a
high prevalence of periodontal disease among CHD
patients could be explained, at least in part, by mutual
risk factors.
MATERIALS AND METHODS
The Scientic Ethical Committee of Copenhagen and
Frederiksberg approved the study, and informed writ-
ten consent was obtained from all participants.
Study Population
The study was designed as a case-control study. It
involved 110 consecutive CHD patients (mean age:
65 years; 70% male) diagnosed at the Department
of Cardiology, Bispebjerg University Hospital. After
discharge, they were invited to participate in the
study. Fromthe CopenhagenCity Heart Study, Epide-
miologic Research Unit, Bispebjerg University Hospi-
tal, 140 people without CHD (mean age: 62.6 years;
60% male) were recruited consecutively to match
the age and gender distribution of CHD patients as
closely as possible. Enrollment started in May 2002
and ended in June 2003. Participants with chronic in-
ammatory disease, human immunodeciency virus
(HIV) infection, a history of organ transplant, or can-
cer treatment 6 months before examination were ex-
cluded during the selection period.
To conrm the diagnoses of individuals with CHD,
hospital case records were examined. Atotal of 42 in-
dividuals had clear ischemic changes on the electro-
cardiogram(ECG). Among the rest of the CHDcases,
17 had been subjected to coronary artery bypass graft
surgery, 34 to percutaneous transluminal coronary
angioplasty(PTCA), and17hadsignsof coronaryische-
miafromcoronaryangiography. SixtypatientswithCHD
had their rst CHD event a maximum of 12 months
prior to the examination. No ischemic changes were
observed on the ECG of control individuals.
Medical Examination
All 250 participants had a medical examination in the
Copenhagen City Heart Study involving a question-
naire concerning symptoms and diseases, familial
dispositions, education and socioeconomic status,
smoking and drinking habits, eating habits, physical
activity, medication, and previous contacts with the
health care system. Smoking was recorded as the
type of tobacco, amount used, and duration of smok-
ing period in years. Height and weight were measured.
A resting ECG was taken, and an echocardiography
was performed. Arm blood pressure was measured
with the subject seated, a blood sample was taken,
and total serum cholesterol, high-density lipoprotein
cholesterol (HDL-c), low-density lipoprotein choles-
terol (LDL-c), and triglyceride were measured. Any
use of medicine was registered. The methods have
been described in detail previously.
9
Oral Examination
A dentist (KG) performed the oral examination at a
dental unit intheDepartment of Cardiology, Bispebjerg
University Hospital. Periodontal registrations were
performed by a trained periodontist. Information on
dental hygiene procedures was registered, and a clin-
ical examination was carried out: probing depth (PD),
recession, and bleeding on probing (BOP) were regis-
tered by the use of a periodontal probe on six sites of
all existing teeth excluding third molars. An indirect
measurement of CAL was calculated on the basis of
PD and the level of the gingival margin. Six intraoral
radiographs were taken: two vertical bitewings on each
side and two periapical radiographs of the incisors of
both jaws.
The radiographs were scanned and digitized.
Two
blinded measurements of ABL were made on each
tooth present, excluding third molars. ABL was
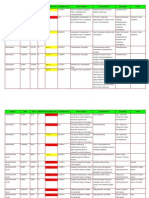
Table 1.
Univariate Association Between Coronary
Heart Disease and Oral Variables
Oral
Variable
CHD
(N = 110)
Non-CHD
(N = 140) P*
ABL (mm) 3.6 (1.8) 2.8 (1.4) <0.001
CAL (mm) 3.7 (1.5) 2.9 (1.3) <0.001
PD (mm) 2.9 (0.9) 2.5 (0.6) 0.002
BOP (%) 38.4 30.7 0.015
NUM 17.9 (9.6) 20.8 (8.7) 0.015
Edentulous (%) 11.6 7.3 0.236
ABL1 (%) 16.5 35.1
g
ABL2 (%) 52.5 46.9 0.003
ABL3 (%) 31.0 18.0
Values presented are mean (SD) or frequency in percent.
NUM = number of teeth.
* Student t and x
2
tests.
Epson expression 1680 pro, Hemel Hempstead, U.K.
Association Between Periodontal Disease and Coronary Heart Disease Volume 77 Number 9
1548
dened as the distance between the cemento-enamel
junction (CEJ) to the most apical level of the alveolar
crest or, incases of anevident infrabony pocket, tothe
bottom of the defect. If the point to mark the alveolar
crest could not be decided, the site of the tooth was
omitted.
If a crown or lling covered the CEJ, an estimated
placement of CEJ was marked using the CEJ level of
adjoining teeth. If no CEJ could be found, or if it was
covered by a neighboring tooth, the site of the tooth
was excluded. The measurement was carried out
blinded on the digitized radiograph with an image-
handling program
i
using a mouse-driven cursor. Prior
to the measurement of ABL, measures of agreement
were made by the use of k statistics. The simple k
values were 0.66, and the weighted values were
0.84, which were regarded as acceptable.
ABL was stratied into three groups: in the ABL1
group, the means were 2 mm; in the ABL2 group,
the means were >2 to 4 mm; and in the ABL3 group,
the means were >4 mm. The same stratication was
made for CAL. The means were
calculated based on all measured
sites from each individual.
Statistical Methods
Statistical analysis was performed
using statistical software.
The Student t test was used
for continuous variables, and the
Mann-Whitney rank sum test was
used if they did not meet the de-
mand for variance homogeneity
and normality. All oral variables
were tested using both parametric
and non-parametric analyses; all
analyses were in agreement. With
more thantwogroups, the Kruskal-
Wallis test was used. Differences
between groups for categorical
variables were analyzed using x
2
distribution. The Spearman cor-
relation for continuous variables
and the Kendall t B correlation
test for ordinal variables were
used when testing for a trend. A
two-sided 5% level of signicance
was used in statistical analyses.
Multiple logistic regression
models with stepwise backward
elimination were used allowing
variables with P <0.15 to enter
the multivariate analysis. Odds
ratios were calculated with a con-
dence interval of 95%.
RESULTS
Table 1 shows periodontal variables characteristic
within the CHD and non-CHD groups. The CHD
group had a signicantly poorer outcome with respect
to all periodontal variables (P <0.05) except for the
proportion of edentulous individuals (25 of all partic-
ipants) where the difference was insignicant.
A comparison of risk factors (Table 2) showed sig-
nicant differences in self-reported diabetes, physical
activity level, and years of school attendance be-
tween the CHDand non-CHDgroups. The distribution
of smoking (pack years) in the CHD and non-CHD
groups had an overall signicant difference at P =
0.025. The differences seen in HDL-c, LDL-c, and
blood pressure were found to be opposite to the ex-
pectedvalues, sothat the CHDgrouphadlower values
than the non-CHD group. HDL-c, LDL-c, triglyceride,
Table 2.
Univariate Association Between Coronary Heart Disease and
Cardiovascular Risk Factors
Risk Factors
CHD
(N = 110)
Non-CHD
(N = 140) P*
Diseases
Diabetes, self-reported (%) 17.3 3.6 <0.001
Lifestyle factors
Smoking >40 pack years (%) 20.6 14.1
g
Smoking >20 to 40 pack years (%) 34.0 20.3 0.025
Smoking >0 to 20 pack years (%) 20.6 29.7
Alcohol, daily consumption (%) 33.6 39.3 0.358
Physical activity, <2 hours weekly (%) 17.3 8.6 0.038
Socioeconomic factors
School attendance (years) 8.8 (1.9) 9.5 (2.0) 0.005
Household income, small
(%) 42.7 33.6 0.138
Other characteristics
Male (%) 70.0 60.0 0.101
Age (years) 65.2 (11.5) 62.6 (10.5) 0.070
Clinical and paraclinical measurements
BMI (kg/m
2
) 27.1 (4.7) 26.7 (4.2) 0.488
Blood pressure, systolic (mmHg) 134.9 (22.6) 141.1 (21.6) 0.027
Triglyceride (mmol) 1.7 (0.8) 1.5 (0.9) 0.131
HDL-c (mmol) 1.3 (0.5) 1.5 (0.4) 0.002
LDL-c (mmol) 2.8 (1.0) 3.6 (1.0) <0.001
Values presented are mean (SD) or frequency in percent.
BMI = body mass index.
* Compared to non-smoking group, using the Student t test for continuous variables and the x
2
test for
categorical variables.
Individuals with a household income less than <200,000 Danish kroner yearly.
i DP-soft, version 3.2 for Windows, Olympus, Hamborg, Germany.
SAS for PC, Statistical Analysis System, SAS Institute, Cary, NC.
J Periodontol September 2006 Geismar, Stoltze, Sigurd, Gyntelberg, Holmstrup
1549
and blood pressure were consequently left out of the
logistic regression model.
The participants grouped into ABL1, ABL2,
and ABL3 (Table 3) showed statistically signicant
differences in smoking dened as pack years. Socio-
economic factors, such as household income and
school attendance, showed a signicant difference
between ABL groups.
Table 4 shows a multiple logistic regression analy-
sis using a backward elimination procedure with the
cardiovascular risk factors. A 0.15 signicance level
was used for inclusion. Diabetes and smoking, strati-
ed into four groups on the basis of pack years, were
allowed to stay in all groups. Age was not a signicant
variable in the group of participants <60 years old and
was not allowed to stay in the model.
In the analysis of all study participants (Table 5),
neither ABL2 nor ABL3 remained signicant com-
pared to ABL1 after adjusting for the selected var-
iables from Table 4. However, in the age group
<60 years, the odds ratio between ABL1 and ABL3
stayed signicant after adjustment (odds ratio = 6.6
[1.69 to 25.6]). In the age group 60 years, the crude
and adjusted odds ratios were almost equal to 1.
When the same straticationwas made on the basis
of CAL for all age groups, the crude odds ratio was 8.2
(2.68 to 25.5) for CAL3 and 3.3 (1.19 to 9.17) for
CAL2 compared to CAL1. After adjustment for age,
diabetes, smoking, and school attendance, odds ra-
tios for CAL3 were signicant, i.e., 5.1 (1.41 to 18.6)
and insignicant for CAL2, i.e., 2.1 (0.68 to 6.40).
For participants <60 years old, the crude odds ratio
for CAL3 was 17.0 (3.93 to 73.5) and insignicant for
CAL2, i.e., 2.7 (0.77 to 9.29). After adjustment, the
odds ratio for CAL3 was 12.7 (2.54 to 63.7). The cor-
relation coefcient for ABL and CAL was r = 0.844
(Fig. 1).
There were no signicant differences between
groups of recently diagnosed CHDand the group with
a longer history of CHDin the association of periodon-
tal disease and CHD (results not shown). Therefore,
we used only one CHD group in the analyses.
DISCUSSION
In the present study, we found signicantly higher
odds (odds ratio = 6.6) for individuals <60 years old
of being CHD patients when having a mean ABL >4
mm based on measurements of radiographs. For
Table 3.
Univariate Association Between Alveolar Bone Level and Cardiovascular Risk Factors
Risk Factors ABL1 (N = 61) ABL2 (N = 111) ABL3 (N = 53) P* P
Diseases
Diabetes, self-reported (%) 3.3 10.8 7.5 0.217 0.3497
Lifestyle factors
Smoking >40 pack years (%) 6.6 19.7 37.7
g
Smoking >20 to 40 pack years (%) 15.3 24.3 22.5 <0.001 <0.001
Smoking >0 to 20 pack years (%) 37.7 22.5 18.9
Alcohol, daily consumption (%) 26.2 39.6 47.2 0.060 0.020
Physical activity, <2 hours weekly (%) 13.1 9.0 15.1 0.473 0.802
Socioeconomic factors
Household income, small (%) 24.6 30.6 49.1 0.015 0.007
School attendance (years) 10.2 (2.0) 9.3 (2.0) 8.6 (1.6) <0.001 <0.001
Other characteristics
Male (%) 54.1 69.4 69.8 0.097 0.067
Age (years) 55.0 (8.9) 65.4 (9.9) 65.7 (10.2) <0.001 <0.001
Clinical and paraclinical measurements
BMI (kg/m
2
) 26.1 (4.5) 26.7 (4.0) 26.7 (5.0) 0.412 0.458
Blood pressure, systolic (mmHg) 131.1 (22.2) 139.7 (22.2) 140.0 (20.0) 0.014 0.007
Triglyceride (mmol) 1.6 (1.0) 1.5 (0.8) 1.7 (1.0) 0.622 0.857
HDL-c (mmol) 1.4 (0.4) 1.4 (0.4) 1.4 (0.5) 0.550 0.616
LDL-c (mmol) 3.4 (1.1) 3.3 (1.1) 3.1 (1.2) 0.138 0.047
Values presented are mean (SD) or frequency in percent.
BMI = body mass index.
* The Kruskal-Wallis test was used for continuous variables, and the x
2
test was used for ordinal variables.
For the trend test, the Kendall test was used for ordinal variables, and the Spearman test was used for continuous variables.
Association Between Periodontal Disease and Coronary Heart Disease Volume 77 Number 9
1550
registered CAL, the association was stronger. To our
knowledge, this study is the rst to include both ABL
and full-mouth registration of CAL. A case-control
design is limited by the fact that exposure and disease
have occurred at the time of entry into the study, and
interpretation of the results must be cautious. Despite
these limitations, half of the increasedcrude riskcould
be explained by mutual risk factors for CHD and peri-
odontal disease: diabetes and smoking.
The CHDcases available for the study were lifetime
prevalence cases and not only recently diagnosed
cases as would have been preferred. To get an im-
pression of the signicance of the temporal asso-
ciation between periodontal disease and CHD, we
repeated all analyses on a subgroup of recently
diagnosedCHDpatients. For this group, it is likelythat
periodontal disease preceded the diagnosis of CHD,
especially when considering that it generally takes
time to develop a high loss of periodontal attachment.
Between the recently diagnosed subjects and the
other patients, there was no difference in the strength
of the association found.
We found poorer outcomes for all periodontal var-
iables among CHD patients compared to non-CHD
patients including PD and BOP.
For ABL, there was a highly sig-
nicant association for individ-
uals <60 years old. A positive
association between radiographi-
cally measured bone level and
CHD has been found previ-
ously.
10-12
WhenusingCALas aperiodon-
tal variable in this study, the asso-
ciation between CAL and CHDfor
all age groups remained signi-
cant after adjustment and was
even higher for individuals <60
years old. The fact that CAL is as-
sociated with CHD is in accor-
dance with previous studies.
13,14
In studies on the association
between periodontal disease and
CHD, different periodontal varia-
bles have been used. This may
explain the discrepancies in re-
sults obtained and why some
studies have failed to observe
any relationship.
15,16
It has been
debated which variable is the
most suitable periodontal vari-
able in statistical analysis. ABL
was recently found to be the peri-
odontal variable that had the
strongest association to CHD.
17
Furthermore, computerized mea-
surement of ABL may facilitate high reproducibility
and can be done in a blinded fashion.
18,19
We found
a good correlation between CAL and ABL (r =
0.844) and, regardless of a blinded registration of
ABL, we showed the same association with CHD for
CAL, although the strength of this association was
higher. This could be due to inammation of the peri-
odontal pocket. Inamed pockets may result in the
overestimation of CAL.
20
It could also reect the un-
intended bias by the examiner in the unblinded regis-
tration, although this is less likely.
The stronger associationof periodontal diseaseand
CHD in younger study populations has also been ob-
servedin other studies.
21-25
The fact that a decreasing
effect was observed among the age group >60 years
old could be due to a healthy survivor effect among
older ages, where a selection may have taken place
due to death from CHD. Also, age-dependent co-
inuence of other diseases and their treatment may
result in a weaker association between periodontal
disease and CHD.
One of the classical Bradford Hill criteria of causal-
ity is a strong dose-response relationship. The in-
creasing crude odds ratios from ABL1 to ABL2
Table 4.
Multiple Logistic Regression Analyses for CHD Covariates
Using Stepwise Backward Elimination
Factors Included in the Model
Group Variable Odds Ratio P
All Age 1.0 (1.00 to 1.05) 0.080
Diabetes versus not 10.1 (2.75 to 36.9) <0.001
Smoking >40 pack years 2.3 (0.99 to 5.34) 0.247
Smoking >20 to 40 pack years 3.0 (1.37 to 6.52) 0.018
Smoking >0 to 20 pack years 1.1 (0.50 to 2.41) 0.107
Non-smoking* 1 1.000
School attendance >10 years versus less 1.7 (0.86 to 3.39) 0.126
<60 years old Diabetes versus not 5.9 (1.03 to 33.9) 0.047
Smoking >40 pack years 6.5 (1.42 to 29.8) 0.016
Smoking >20 to 40 pack years 2.7 (0.87 to 8.88) 0.331
Smoking >0 to 20 pack years 0.8 (0.21 to 3.32) 0.053
Non-smoking* 1 1.000
60 years old Age 1.1 (1.00 to 1.12) 0.051
Diabetes versus not 17.7 (2.13 to 147) 0.008
Smoking >40 pack years 1.4 (0.50 to 4.15) 0.703
Smoking >20 to 40 pack years 4.2 (1.44 to 12.0) 0.011
Smoking >0 to 20 pack years 1.3 (0.48 to 3.30) 0.390
Non-smoking* 1 1.000
Odds ratios with 95% condence limits are presented for variables in the nal model (P <0.15). Covariates
in the full model were as follows: small household income; body mass index >25; alcohol daily
consumption; male gender; physical inactivity; <10 years of school attendance; diabetes; and smoking in
pack years.
* Reference category.
J Periodontol September 2006 Geismar, Stoltze, Sigurd, Gyntelberg, Holmstrup
1551
(Table 5) among participants <60 years old indicates
that a dose-response relationship between ABL and
CHD may exist.
The biologically plausible explanation of the ob-
served association between periodontal disease and
CHD has been that chronic infections and associated
inammatory processes may be involved in the initi-
ation and progression of atherosclerosis. Two path-
ways are suspected to be involved: a direct pathway
where the periodontal bacteria
invade the arterial wall
26,27
or an indirect pathway where
bacterial products from the
periodontal pocket exert a sys-
temic effect on atherosclerosis
development.
28,29
Chlamydia
pneumoniae has also been
linked with CHD, and it was
proposed that infection with
C. pneumoniae was a cause
of CHD. However, recent meta-
analysis rejects any strong as-
sociation between infections
with C. pneumoniae and CHD,
although a modest association
in a younger age group cannot
be excluded.
30
In our study, it is evident that
periodontal disease and CHD
share common risk factors,
and smoking and diabetes
could explain half of the ob-
served associations between
periodontal disease and CHD.
Smoking and diabetes are
known to induce changes in
the microvascular function af-
fecting the peripheral blood
circulation.
31,32
The functional impairment of the
microcirculation in smokers has been shown to affect
the gingival tissue.
33
Furthermore, smoking and dia-
betes are known to be associated with a greater sus-
ceptibility to infections.
34,35
This is in agreement
with the result of seroepidemiological studies showing
that C. pneumoniae infections are more common in
smokers.
36
With a poor adjustment for smoking, a study could
correlate periodontal disease to smoking-related dis-
eases like chronic obstructive lung disease, lung can-
cer, and CHD.
37
These associations disappeared after
relevant adjustment, including duration, amount, and
type of smoking.
38
In the present study, available data
on tobacco use enabled the calculation of pack years,
and this variable was found to be associated with ABL
and CHD (Tables 2 and 3). Despite the adjustment
with smoking recorded as pack years, the asso-
ciation in the present study remained statistically
signicant.
CONCLUSIONS
The present study has shown a positive association
between periodontal disease and CHD in agreement
with several other studies. The association was highly
age dependent and could only be attributed to diabe-
tes and smoking to some extent.
Table 5.
Odds Ratio (95% condence limits) for Coronary Heart
Disease According to ABL With Different Adjustment Criteria
Logistic Regression With Forced Entry of Variables
Group ABL1 ABL2 ABL3
All
Crude odds ratio 1 2.4 (1.21 to 4.73) 3.7 (1.67 to 8.07)
Adjusted for
1) Age 1 2.4 (1.13 to 4.97) 3.6 (1.57 to 8.44)
2) 1) + diabetes 1 2.1 (0.96 to 4.41) 3.4 (1.45 to 8.06)
3) 2) + smoking >0 pack years 1 1.7 (0.76 to 3.71) 2.2 (0.87 to 5.61)
4) 3) + school attendance >10 years 1 1.6 (0.71 to 3.51) 2.0 (0.77 to 5.08)
<60 years old
Crude odds ratio 1 3.8 (1.38 to 10.4) 9.8 (2.77 to 34.9)
Adjusted for
1) Smoking >0 pack years 1 3.1 (1.09 to 8.91) 6.9 (1.80 to 26.8)
2) 1) + diabetes 1 2.4 (0.82 to 7.41) 6.6 (1.69 to 25.6)
60 years old
Crude odds ratio 1 1.3 (0.46 to 4.72) 1.5 (0.44 to 3.56)
Adjusted for
1) Age 1 1.0 (0.34 to 3.83) 1.1 (0.34 to 3.00)
2) 1) + diabetes 1 0.9 (0.31 to 2.97) 1.1 (0.30 to 3.74)
3) 2) + smoking >0 pack years 1 0.7 (0.18 to 2.74) 0.8 (0.26 to 2.69)
Figure 1.
Correlation between ABL and CAL.
Association Between Periodontal Disease and Coronary Heart Disease Volume 77 Number 9
1552
ACKNOWLEDGMENTS
The authors thank the Velux Foundation, Fut/Calcin
Foundation, Danish Foundation for Mutual Efforts
in Dental Care, and Wedell-Wedellsborg Foundation,
Copenhagen, Denmark, for nancial support.
REFERENCES
1. Holmstrup P, Poulsen AH, Andersen L, Skuldbol T,
Fiehn NE. Oral infections and systemic diseases. Dent
Clin North Am 2003;47:575-598.
2. Cairo F, Gaeta C, Dorigo W, et al. Periodontal patho-
gens in atheromatous plaques. A controlled clinical and
laboratory trial. J Periodontal Res 2004;39:442-446.
3. Pussinen PJ, Jousilahti P, Alfthan G, Palosuo T,
Asikainen S, Salomaa V. Antibodies to periodontal
pathogens are associated with coronary heart disease.
Arterioscler Thromb Vasc Biol 2003;23:1250-1254.
4. Keil U. Coronary artery disease: The role of lipids,
hypertension and smoking. Basic Res Cardiol 2000;
95(Suppl. 1):I52-I58.
5. Wood D. Established and emerging cardiovascular
risk factors. Am Heart J 2001;141:S49-S57.
6. Katz J, Flugelman MY, Goldberg A, Heft M. Associa-
tion between periodontal pockets and elevated cho-
lesterol and low density lipoprotein cholesterol levels.
J Periodontol 2002;73:494-500.
7. Losche W, Karapetow F, Pohl A, Pohl C, Kocher T.
Plasma lipid and blood glucose levels in patients with
destructive periodontal disease. J Clin Periodontol
2000;27:537-541.
8. Tezal M, Grossi SG, Ho AW, Genco RJ. Alcohol
consumption and periodontal disease. The Third Na-
tional Health and Nutrition Examination Survey. J Clin
Periodontol 2004;31:484-488.
9. The Copenhagen City Heart Study. Osterbrounderso-
gelsen. A book of tables with data from the rst exam-
ination (1976-78) and a ve year follow-up (1981-83).
The Copenhagen City Heart Study Group. Scand J Soc
Med Suppl 1989;41:1-160.
10. Mendez MV, Scott T, LaMorte W, Vokonas P, Menzoian
JO, Garcia R. An association between periodontal
disease and peripheral vascular disease. Am J Surg
1998;176:153-157.
11. Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher
S. Periodontal disease and cardiovascular disease.
J Periodontol 1996;67(Suppl.):1123-1137.
12. Persson RE, Hollender LG, Powell VL, et al. Assess-
ment of periodontal conditions and systemic disease
in older subjects. II. Focus on cardiovascular diseases.
J Clin Periodontol 2002;29:803-810.
13. Arbes SJ Jr., Slade GD, Beck JD. Association be-
tween extent of periodontal attachment loss and
self-reported history of heart attack: An analysis of
NHANES III data. J Dent Res 1999;78:1777-1782.
14. Lopez R, Oyarzun M, Naranjo C, Cumsille F, Ortiz M,
Baelum V. Coronary heart disease and periodontitis
A case control study in Chilean adults. J Clin Peri-
odontol 2002;29:468-473.
15. Hujoel PP, Drangsholt MT, Spiekerman C, DeRouen
TA. Periodontal disease and risk of coronary heart
disease. JAMA 2001;285:40-41.
16. Howell TH, Ridker PM, Ajani UA, Hennekens CH,
Christen WG. Periodontal disease and risk of subse-
quent cardiovascular disease in U.S. male physicians.
J Am Coll Cardiol 2001;37:445-450.
17. Renvert S, Ohlsson O, Persson S, Lang NP, Persson
GR. Analysis of periodontal risk proles in adults with
or without a history of myocardial infarction. J Clin
Periodontol 2004;31:19-24.
18. Wolf B, von Bethlenfalvy E, Hassfeld S, Staehle HJ,
Eickholz P. Reliability of assessing interproximal bone
loss by digital radiography: Intrabony defects. J Clin
Periodontol 2001;28:869-878.
19. Kim TS, Benn DK, Eickholz P. Accuracy of computer-
assisted radiographic measurement of interproximal
bone loss in vertical bone defects. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod 2002;94:379-387.
20. Robinson PJ, Vitek RM. The relationship between gin-
gival inammation and resistance to probe penetra-
tion. J Periodontal Res 1979;14:239-243.
21. Jansson L, Lavstedt S, Frithiof L, Theobald H. Rela-
tionship between oral health and mortality in car-
diovascular diseases. J Clin Periodontol 2001;28:
762-768.
22. DeStefano F, Anda RF, Kahn HS, Williamson DF,
Russell CM. Dental disease and risk of coronary heart
disease and mortality. BMJ 1993;306:688-691.
23. Mattila KJ, Valle MS, Nieminen MS, Valtonen VV,
Hietaniemi KL. Dental infections and coronary athero-
sclerosis. Atherosclerosis 1993;103:205-211.
24. Morrison HI, Ellison LF, Taylor GW. Periodontal dis-
ease and risk of fatal coronary heart and cerebrovas-
cular diseases. J Cardiovasc Risk 1999;6:7-11.
25. Mattila KJ, Valtonen VV, Nieminen M, Huttunen JK.
Dental infection and the risk of new coronary events:
Prospective study of patients with documented coro-
nary artery disease. Clin Infect Dis 1995;20:588-592.
26. Chiu B. Multiple infections in carotid atherosclerotic
plaques. Am Heart J 1999;138:S534-S536.
27. Choi JI, Chung SW, Kang HS, Rhim BY, Kim SJ, Kim
SJ. Establishment of Porphyromonas gingivalis heat-
shock-protein-specic T-cell lines from atherosclero-
sis patients. J Dent Res 2002;81:344-348.
28. DAiuto F, Ready D, Tonetti MS. Periodontal disease
and C-reactive protein-associated cardiovascular risk.
J Periodontal Res 2004;39:236-241.
29. Slade GD, Offenbacher S, Beck JD, Heiss G, Pankow
JS. Acute-phase inammatory response to periodon-
tal disease in the US population. J Dent Res 2000;79:
49-57.
30. Danesh J, Whincup P, Lewington S, et al. Chlamydia
pneumoniae IgA titres and coronary heart disease;
prospective study and meta-analysis. Eur Heart J 2002;
23:371-375.
31. Stratton IM, Adler AI, Neil HA, et al. Association of
glycaemia with macrovascular and microvascular
complications of type 2 diabetes (UKPDS 35): Pro-
spective observational study. BMJ 2000;321:405-
412.
32. Ijzerman RG, Serne EH, van Weissenbruch MM, de
Jongh RT, Stehouwer CD. Cigarette smoking is associ-
ated with an acute impairment of microvascular func-
tion in humans. Clin Sci (Lond) 2003;104:247-252.
33. Hanioka T, Tanaka M, Ojima M, Takaya K, Matsumori
Y, Shizukuishi S. Oxygen sufciency in the gingiva of
smokers and non-smokers with periodontal disease.
J Periodontol 2000;71:1846-1851.
34. Ambrose JA, Barua RS. The pathophysiology of cig-
arette smoking and cardiovascular disease: An up-
date. J Am Coll Cardiol 2004;43:1731-1737.
35. Dandona P, Aljada A. A rational approach to patho-
genesis and treatment of type 2 diabetes mellitus,
J Periodontol September 2006 Geismar, Stoltze, Sigurd, Gyntelberg, Holmstrup
1553
insulin resistance, inammation, and atherosclerosis.
Am J Cardiol 2002;90:27G-33G.
36. Leinonen M. Chlamydia pneumoniae and other
risk factors for atherosclerosis. J Infect Dis 2000;
181(Suppl. 3):S414-S416.
37. Jansson L, Lavstedt S, Frithiof L. Relationship be-
tween oral health and mortality rate. J Clin Periodontol
2002;29:1029-1034.
38. Hujoel PP, Drangsholt M, Spiekerman C, DeRouen TA.
Periodontitis-systemic disease associations in the
presence of smoking causal or coincidental? Peri-
odontol 2000 2002;30:51-60.
Correspondence: Dr. Karen Geismar, Department of
Periodontology, School of Dentistry, Faculty of Health
Science, University of Copenhagen, Nrre Alle 20, 2200
Copenhagen, Denmark. Fax: 45-35326699; e-mail:
kgm@odont.ku.dk.
Accepted for publication April 21, 2006.
Association Between Periodontal Disease and Coronary Heart Disease Volume 77 Number 9
1554
Você também pode gostar
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Communicable and Non Communicable Diseases PDFDocumento96 páginasCommunicable and Non Communicable Diseases PDFhiabhijit2967% (3)
- Diets Modified in CompositionDocumento6 páginasDiets Modified in Compositionsy saludAinda não há avaliações
- Haematological Parameters and Lipid Profile AbnormDocumento10 páginasHaematological Parameters and Lipid Profile AbnormPhelix O DaniyanAinda não há avaliações
- Lipids - ReviewerDocumento7 páginasLipids - ReviewerIYA LABAOAinda não há avaliações
- Urden, Stacy, Lough: Critical Care Nursing, 6 Edition: Chapter 19: Cardiovascular Disorders Test Bank Multiple ChoiceDocumento13 páginasUrden, Stacy, Lough: Critical Care Nursing, 6 Edition: Chapter 19: Cardiovascular Disorders Test Bank Multiple ChoiceTara McNeillAinda não há avaliações
- Laboratory Report: HaematologyDocumento3 páginasLaboratory Report: HaematologyArundhathy KrishnaAinda não há avaliações
- Probiotic 13 Fr-2021-845 Wulandari Aprl 2023Documento11 páginasProbiotic 13 Fr-2021-845 Wulandari Aprl 2023wisnuadi UMBYAinda não há avaliações
- Jurnal HyperlipidemiaDocumento12 páginasJurnal HyperlipidemiaJo LenongAinda não há avaliações
- Management of HyperlipidemiaDocumento39 páginasManagement of HyperlipidemiaRajgopal100% (2)
- General Health Screen Lab ReportDocumento8 páginasGeneral Health Screen Lab ReportM.leela Vinotha KrishnanAinda não há avaliações
- CHAPTER I BASIC CONCEPT NUTRITION AND DIET THERAPY Questions01Documento30 páginasCHAPTER I BASIC CONCEPT NUTRITION AND DIET THERAPY Questions01Jeeyan DelgadoAinda não há avaliações
- Cholesterol Homeostasis Regulated by ABCA1 Is Critical For Retinal Ganglion Cell SurvivalDocumento15 páginasCholesterol Homeostasis Regulated by ABCA1 Is Critical For Retinal Ganglion Cell SurvivalAndrianna NastasyaAinda não há avaliações
- Effect of Lactobacillus Gasseri BNR17 On Overweight and Obese Adultts A Randomized, Double-Blind Clinical TrialDocumento10 páginasEffect of Lactobacillus Gasseri BNR17 On Overweight and Obese Adultts A Randomized, Double-Blind Clinical TrialAna Rosa Ortega CastilloAinda não há avaliações
- Efeitos Metab Licos Do Jejum Intermitente PDFDocumento197 páginasEfeitos Metab Licos Do Jejum Intermitente PDFLarisa JanušićAinda não há avaliações
- Hypolipidemic Activity of Caralluma Adscendens On Triton and Methimazole Induced Hyperlipidemic RatsDocumento4 páginasHypolipidemic Activity of Caralluma Adscendens On Triton and Methimazole Induced Hyperlipidemic RatsمحمدأميندماجAinda não há avaliações
- Amazing Health MagazineDocumento60 páginasAmazing Health MagazineAnjani KumarAinda não há avaliações
- Brochure-MakatiMed Health Packages 2015Documento2 páginasBrochure-MakatiMed Health Packages 2015Mikee FelipeAinda não há avaliações
- Metabolic Syndrome PDFDocumento6 páginasMetabolic Syndrome PDFVanessa HermioneAinda não há avaliações
- Super SlowDocumento9 páginasSuper SlowFabiano LacerdaAinda não há avaliações
- 7 Amazing Benefits of Black CuminDocumento4 páginas7 Amazing Benefits of Black CuminGary Pears100% (1)
- Chapter 33: Cardiovascular System Introduction Linton: Medical-Surgical Nursing, 7th EditionDocumento16 páginasChapter 33: Cardiovascular System Introduction Linton: Medical-Surgical Nursing, 7th EditionStaceyAinda não há avaliações
- Blood Vessels QuizDocumento28 páginasBlood Vessels Quiztatti999Ainda não há avaliações
- Hba1c (Ifcc - New Method) - 2023-08-29T00 - 00 - 00Documento1 páginaHba1c (Ifcc - New Method) - 2023-08-29T00 - 00 - 00Michamiel SerratoAinda não há avaliações
- Chem InvestigatoryDocumento18 páginasChem InvestigatoryNysa HajiraAinda não há avaliações
- Nejmoa 2210645Documento12 páginasNejmoa 2210645masah al haj aliAinda não há avaliações
- Research in Public Health by Prof DR Rwamakuba ZephanieDocumento120 páginasResearch in Public Health by Prof DR Rwamakuba ZephanieDr Zephanie RwamakubaAinda não há avaliações
- Lipid DisordersDocumento3 páginasLipid DisordersAhmed AssafAinda não há avaliações
- NutraHacker Complete SASDocumento9 páginasNutraHacker Complete SASJustin KellyAinda não há avaliações
- Pe 10 Q2Documento152 páginasPe 10 Q2Lanie Tamacio Baday85% (20)
- TriglyceridesDocumento7 páginasTriglyceridespandeypcAinda não há avaliações