Escolar Documentos
Profissional Documentos
Cultura Documentos
5NCP
Enviado por
Sara ThorntonDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
5NCP
Enviado por
Sara ThorntonDireitos autorais:
Formatos disponíveis
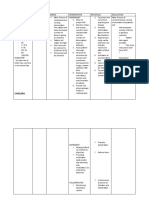
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective:
Sobrang sakit nitong
tahi ko. as verbalized
by the patient.
Objective:
>Pain scale of 8/10
>Teary eyed
>(+) guarding
behavior
>(+) facial grimace
>Irritable
>Pale palpebral
conjunctiva
>Skin warm to touch
V/S taken as follows:
T=
PR=
RR=
BP
Acute pain related to
disruption of skin and
tissue secondary to
cesarean section.
After 4hrs. of nursing
intervention, patient
will verbalize
decrease intensity of
pain from 8/10 to
3/10.
Independent:
>Established rapport.
>Monitored vital
signs.
>Assessed quality,
characteristics,
severity of pain.
>Provided
comfortable
environment-
changed bed linens
and turned on the
electric fan.
>Instructed to put
pillow on the
abdomen when
coughing or moving.
>Instructed patient to
do deep breathing
and coughing
>To have a good
nurse-client
relationship.
>To establish a
baseline data.
> To establish a
baseline data for
comparison in making
evaluation and to
assess for possible
internal bleeding.
>Calm environment
helps to decrease the
anxiety of the patient
and promote
likelihood of
decreasing pain.
>To check for
diastasis recti and
protect the area of
the incision to
improve comfort. And
to initiate
nonstressful muscle-
setting techniques
and progress as
tolerated, based on
the degree of
separation.
>For pulmonary
ventilation, specially
when exercising, and
After 4hrs. of nursing
intervention, the
patient verbalized
pain decreased from
a scale of 8/10 to
3/10 as evidenced by
(-) facial grimace
(-) guarding behavior.
Frequent small talks
with significant
others.
GOAL MET.
exercise.
>Provided
diversionary
activities. Initiate
ankle pumping, active
lower extremity ROM
and walking.
Collaborative:
>Administer analgesic
as per doctors order.
to relieve stress and
promote relaxation.
>To promote
circulation, prevent
venous stasis,
prevent pressure on
the operative site.
>Relieves pain felt by
the patient.
Subjective:
>none
Objective:
>dressing dry and
intact
V/S taken as follows:
T=
PR=
RR=
BP=
Risk for infection
related to inadequate
primary defenses
secondary to surgical
incision.
STG:
After 4hrs. of nursing
intervention, patient
will be able to
understand causative
factors, identify signs
of infection and
report them to health
care provider
accordingly.
LTG:
After 2-3 days of
nursing intervention,
patient will achieve
timely wound
healing, be free of
purulent drainage or
erythema, be afebrile
and be free of
infection.
Independent:
>Monitor vital signs.
>Inspect dressing and
perform wound care.
>Monitor WBC.
>Monitor
temperature,
redness, swelling,
increased pain, or
purulent drainage at
incisions.
>Wash hands and
teach other
caregivers to wash
hands before contact
with patient between
>To establish a
baseline data.
>Moist from drainage
can be a source of
infection.
>Rising WBC indicates
bodys efforts to
combat pathogens;
normal values: 4000-
11,000 mm
3
>These are signs of
infection.
>Friction and running
water effectively
remove
microorganisms from
hands. Washing
Patient is expected to
be free of infection,
as evidenced by
normal vital signs and
absence of purulent
drainage from
wounds, incisions,
and tubes.
procedures with
patient.
>Encourage fluid
intake of 2000ml to
3000ml per day.
>Encourage coughing
and deep breathing:
consider use of
incentive spirometer.
Collaborative:
>Administer
antibiotics as per
doctors order.
between procedures
reduces the risk of
transmitting
pathogens from one
area of the body to
another.
>Fluids promote
diluted urine and
frequent emptying of
bladder; reducing
stasis of urine, in
turn, reduces risk of
bladder infection or
UTI.
>These measures
reduce stasis of
secretions in the
lungs and bronchial
tree. When stasis
occurs, pathogens
can cause upper
respiratory infections,
including pneumonia.
>Antibiotics have
bactericidal effect
that combats
pathogens.
Objective Cues:
>Patient has not yet
eliminated since
delivery.
>Absence of bruit
sounds.
Risk for constipation
related to post
pregnancy secondary
to cesarean section.
STG:
Within 4hrs. of
nursing intervention,
the patient will be
able to demonstrate
behaviors or lifestyle
Independent:
>Ascertain normal
bowel functioning of
the patient, about
how many times a
day she defecate.
>This is to determine
the normal bowel
pattern.
After 4hrs. of nursing
interventions, the
patient was able to
identify measures to
prevent infection as
manifested by clients
>Normal pattern of
bowel has not yet
returned
changes to prevent
developing problem.
LTG:
Within 3 days of
nursing interventions,
the patient will be
able to maintain
usual pattern of
bowel functioning.
>Encourage intake of
foods rich in fiber
such as fruits.
>Promote adequate
fluid intake. Suggest
drinking of warm
fluids, especially in
the morning to
stimulate peristalsis.
>Encourage
stimulation such as
walking within
individual limits.
>However, since she
has had cesarean,
also encourage
adequate rest
periods.
Collaborative:
>Administer bulk-
forming agents or
stool softeners such
as laxatives as
indicated or
prescribed by the
physician.
>To increase the bulk
of the stool and
facilitate the passage
through the colon.
>To promote moist
soft stool.
>To stimulate
contractions of the
intestines and
prevent post
operative
complications.
>To avoid stress on
the cesarean
incision/wound.
>To promote
defecation.
verbalization of:
Iinom ako ng
maraming tubig at
kakain ng prutas para
makadumi ako.
Você também pode gostar
- ShiatsuDocumento148 páginasShiatsuPreto Misturado93% (14)
- Castration in The Horse: by Christina Cable, DVM, Dipl. ACVSDocumento5 páginasCastration in The Horse: by Christina Cable, DVM, Dipl. ACVSRavi KangAinda não há avaliações
- NCP CSDocumento9 páginasNCP CSFreida Marie PiczonAinda não há avaliações
- Fracture NCPDocumento3 páginasFracture NCPCandy Paraiso AgustinAinda não há avaliações
- CABGDocumento31 páginasCABGRiya PhilipAinda não há avaliações
- Healing Psoriasis by Dr. PaganoDocumento3 páginasHealing Psoriasis by Dr. PaganoXavier GuarchAinda não há avaliações
- Quality Control TFDocumento150 páginasQuality Control TFPrabhat Kumar100% (2)
- OcclusionDocumento14 páginasOcclusionpasser byAinda não há avaliações
- Mitral Stenosis PresentationDocumento84 páginasMitral Stenosis PresentationStawan Chougule100% (2)
- Pain Care PlanDocumento18 páginasPain Care Planjordanw0613Ainda não há avaliações
- Basic Life SupportDocumento3 páginasBasic Life SupportSarah EddiahAinda não há avaliações
- Imbalanced Nutrition Less Than Body RequirementsDocumento2 páginasImbalanced Nutrition Less Than Body RequirementsSundaraBharathiAinda não há avaliações
- Chorioamnionitis NCPDocumento8 páginasChorioamnionitis NCPjunard258067% (3)
- Tuano, Salma M. Bsn4-1 Acute PainDocumento2 páginasTuano, Salma M. Bsn4-1 Acute PainSALMA M. TUANOAinda não há avaliações
- Veterinary JournalDocumento96 páginasVeterinary JournalΝίκος Κριτσοταλάκης100% (1)
- NCP CholeDocumento8 páginasNCP CholeAndrewAlvinTemploAinda não há avaliações
- NCP On Decrease Cardiac OutputDocumento1 páginaNCP On Decrease Cardiac OutputHamayun KhanAinda não há avaliações
- AnxietyDocumento3 páginasAnxietyJenny Pearl Pasal100% (1)
- Discharge PlanDocumento4 páginasDischarge PlanPaul Loujin LeeAinda não há avaliações
- NCP Impaired ComfortDocumento2 páginasNCP Impaired ComfortGia P. de VeyraAinda não há avaliações
- NCP PainDocumento4 páginasNCP PainMark Allison BuenaventuraAinda não há avaliações
- Nursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy MalaiseDocumento1 páginaNursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy Malaise06eltianAinda não há avaliações
- Acute Pyelonephritis Nursing Care PlansDocumento2 páginasAcute Pyelonephritis Nursing Care PlansJoannah Marie Juloya Kiat-ong100% (1)
- Acute Pain Related To Frequent As Evidenced by Pain ScaleDocumento3 páginasAcute Pain Related To Frequent As Evidenced by Pain ScaledanaAinda não há avaliações
- Assessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationDocumento3 páginasAssessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationCrissa AngelAinda não há avaliações
- NCP For Insomnia PDFDocumento2 páginasNCP For Insomnia PDFEca0% (1)
- Lapkas HegDocumento1 páginaLapkas HegkurniaAinda não há avaliações
- NCP CSDocumento7 páginasNCP CSTwobee Kriz LeghidAinda não há avaliações
- NCP Pedia SleepapneaDocumento2 páginasNCP Pedia SleepapneaDavid Brillo100% (1)
- SOAPIEDocumento4 páginasSOAPIEdhianne_garcia2001Ainda não há avaliações
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeDocumento2 páginasTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Pre-OperativeMiar QuestAinda não há avaliações
- Health History Format BlankDocumento32 páginasHealth History Format BlankRich-Anne LagarasAinda não há avaliações
- COMMUNITY-MANUSCRIPT SampleDocumento84 páginasCOMMUNITY-MANUSCRIPT SampleCA SavageAinda não há avaliações
- Revised NCPDocumento8 páginasRevised NCPKryza Dale Bunado BaticanAinda não há avaliações
- Nursing Care Plan D-CDocumento2 páginasNursing Care Plan D-CGian MonillaAinda não há avaliações
- NCP Proper CholecystectomyDocumento2 páginasNCP Proper CholecystectomyGail Lian SantosAinda não há avaliações
- NCP of Endometrical CancerDocumento2 páginasNCP of Endometrical CancerFrando kennethAinda não há avaliações
- Reflective Journal 1Documento4 páginasReflective Journal 1api-365605511Ainda não há avaliações
- Deficient Knowledge: Nursing Diagnosis Nursing Care Plans (NCP)Documento3 páginasDeficient Knowledge: Nursing Diagnosis Nursing Care Plans (NCP)Vincent Paul SantosAinda não há avaliações
- Postpartal Thrombophlebitis: Client Assessment Data Base Activity/RestDocumento8 páginasPostpartal Thrombophlebitis: Client Assessment Data Base Activity/RestLei OrtegaAinda não há avaliações
- NCP Meningitis Sure NaniDocumento2 páginasNCP Meningitis Sure NaniARISAinda não há avaliações
- Subjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationDocumento2 páginasSubjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationAyra PunzalanAinda não há avaliações
- Nursing Care Plan: Provide Rest Periods To Promote Relief, Sleep, and RelaxationDocumento2 páginasNursing Care Plan: Provide Rest Periods To Promote Relief, Sleep, and RelaxationGrace MellaineAinda não há avaliações
- Activity IntoleranceDocumento2 páginasActivity IntoleranceDiane AbanillaAinda não há avaliações
- Imbalanced NutritionDocumento2 páginasImbalanced NutritionRizza 이 동해 Ocampo100% (1)
- Discharge Planning BurnsDocumento12 páginasDischarge Planning BurnsChaa Maii100% (1)
- NCPDocumento2 páginasNCPCamille VirayAinda não há avaliações
- Ineffective Peripheral Tissue Perfusion Related To Vasoconstriction Secondary To High Glucose Level.Documento6 páginasIneffective Peripheral Tissue Perfusion Related To Vasoconstriction Secondary To High Glucose Level.SAROL, RYAN CHRISTIAN B.Ainda não há avaliações
- NCP (Postpartum Hemmorhage)Documento3 páginasNCP (Postpartum Hemmorhage)Anne DyAinda não há avaliações
- Complications in PregnancyDocumento36 páginasComplications in PregnancyJADE PATEGAAinda não há avaliações
- Drug-Study NCPDocumento5 páginasDrug-Study NCPMURILLO, FRANK JOMARI C.Ainda não há avaliações
- Buergers Power PointDocumento16 páginasBuergers Power PointYan VencerAinda não há avaliações
- Assessment Diagnosis Outcomes Interventions Rationale Expected OutcomeDocumento1 páginaAssessment Diagnosis Outcomes Interventions Rationale Expected OutcomeMatelyn OargaAinda não há avaliações
- Nursing Care Plan Format Name: - Medical Diagnosis: - DateDocumento2 páginasNursing Care Plan Format Name: - Medical Diagnosis: - DateSheryl Ann Barit PedinesAinda não há avaliações
- Emj Cases : Questions For Case 1Documento8 páginasEmj Cases : Questions For Case 1Azmyza Azmy100% (1)
- Huntingtons Disease NCPDocumento4 páginasHuntingtons Disease NCPJerich Mark SalasAinda não há avaliações
- NCPDocumento3 páginasNCPJoevelyn LaynoAinda não há avaliações
- NSO - Adam's Forward Bend TestDocumento2 páginasNSO - Adam's Forward Bend TestMaha AmilAinda não há avaliações
- NCP RiskDocumento2 páginasNCP RiskNorries Jonell CaballarAinda não há avaliações
- APOLONIO, JC - Natural Theory - Thomas AquinasDocumento3 páginasAPOLONIO, JC - Natural Theory - Thomas AquinasJustin ApolonioAinda não há avaliações
- NCP MeningitisDocumento2 páginasNCP MeningitisARISAinda não há avaliações
- Physical Exam - AppendectomyDocumento8 páginasPhysical Exam - Appendectomyirish felixAinda não há avaliações
- Pedia Ward NCPDocumento2 páginasPedia Ward NCPChacha AllanaAinda não há avaliações
- NCPDocumento2 páginasNCPNichole Audrey SaavedraAinda não há avaliações
- NCP 2 LRDR For PrintDocumento2 páginasNCP 2 LRDR For PrintGeorge PandaAinda não há avaliações
- NCP Readiness RevisionDocumento3 páginasNCP Readiness RevisionimnasAinda não há avaliações
- Meckel's DiverticulumDocumento2 páginasMeckel's Diverticulumlorenz_gtlAinda não há avaliações
- Postoperative Nursing Care Plan For Cesarian Section Patient Case Pres orDocumento6 páginasPostoperative Nursing Care Plan For Cesarian Section Patient Case Pres orLoren EstefanAinda não há avaliações
- 2017 Spine Tango Annual Report Final 1Documento29 páginas2017 Spine Tango Annual Report Final 1BeckyAinda não há avaliações
- Burn Management All PhasesDocumento5 páginasBurn Management All PhasesDesslyn RafflyAinda não há avaliações
- Covid Covid Special Special Hospital Hospital: Santhu Maji 16SA20 SEM-9Documento5 páginasCovid Covid Special Special Hospital Hospital: Santhu Maji 16SA20 SEM-9santhu majiAinda não há avaliações
- 3.16.13-Letter To The Editor From Paul LiistroDocumento1 página3.16.13-Letter To The Editor From Paul LiistroLisa BousquetAinda não há avaliações
- Lung CancerDocumento4 páginasLung CancerjorgeacctAinda não há avaliações
- Dr. Alano vs. LagmaoDocumento2 páginasDr. Alano vs. LagmaoGigiRuizTicarAinda não há avaliações
- Adolescent PregnancyDocumento8 páginasAdolescent Pregnancyapi-281250888Ainda não há avaliações
- BronchiolitisDocumento4 páginasBronchiolitistingtingcrazyAinda não há avaliações
- 3 - Modalities of NursingDocumento6 páginas3 - Modalities of NursingMark Zedrix MediarioAinda não há avaliações
- Circulating SerotoninDocumento17 páginasCirculating Serotoninnihilx27374Ainda não há avaliações
- Effects of Corneal Scars and Their Treatment With Rigid Contact Lenses On Quality of VisionDocumento5 páginasEffects of Corneal Scars and Their Treatment With Rigid Contact Lenses On Quality of VisionJasmine EffendiAinda não há avaliações
- Blood Anatomy and Physiology ReviewDocumento20 páginasBlood Anatomy and Physiology ReviewStacey CamilleAinda não há avaliações
- Air Liquide 2012en4275308938748421437Documento63 páginasAir Liquide 2012en4275308938748421437Pushpa BaruaAinda não há avaliações
- Obsessive Compulsive DisorderDocumento13 páginasObsessive Compulsive Disorderapi-296998780Ainda não há avaliações
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocumento5 páginasEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyChennieWongAinda não há avaliações
- Legg-Calvé-Perthes Disease: Roberto E. Novo, DVM, DACVSDocumento2 páginasLegg-Calvé-Perthes Disease: Roberto E. Novo, DVM, DACVSEdi BackyAinda não há avaliações
- Nursing Care Plan: CirrhosisDocumento11 páginasNursing Care Plan: CirrhosisneuronurseAinda não há avaliações
- Ecology: Streptococcus Agalactiae, Also Known As Group B Streptococci, AreDocumento7 páginasEcology: Streptococcus Agalactiae, Also Known As Group B Streptococci, Are99nonameAinda não há avaliações
- Drugstudy Case StudyDocumento7 páginasDrugstudy Case StudyHerwincayeAinda não há avaliações
- Reliability and Validity of The Turkish Version of The Job Performance Scale InstrumentDocumento9 páginasReliability and Validity of The Turkish Version of The Job Performance Scale InstrumentsatmayaniAinda não há avaliações
- Hemiplegia Is Total Paralysis of The ArmDocumento3 páginasHemiplegia Is Total Paralysis of The ArmRaveen mayi100% (1)