Escolar Documentos
Profissional Documentos
Cultura Documentos
OS 206 Renal Physiology
Enviado por
alphius_mendozaDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
OS 206 Renal Physiology
Enviado por
alphius_mendozaDireitos autorais:
Formatos disponíveis
Dr. Elizabeth S.
Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
2. Calcitriol (an active metabolite of vitamin D)
Lecture Outline:
o Recall: Previtamin D in skin (through sun
I. Functional Renal Anatomy
A. Major Functions of the Kidney exposure), also from diet (milk), deep sea
B. The Nephron fish (salmon) is converted to:
C. Renal Vasculature 25(OH)D (calcidiol) in the liver and
D. Basic Renal Processes processed by the prostate gland,
II. Renal Blood Flow
breast, colon, lungs, immune cells to
III. Glomerular Filtration
A. Filtration Membrane
1,25(OH)2D used for regulation of cell
B. Glomerular Filtration Rate growth or immune function.
C. Autoregulation 1,25(OH)2D (calcitriol) in the
V. Clearance Principle mitochondria of the convoluted &
VI. Appendix straight proximal tubules of the
kidney. It increases GI Ca absorption,
stimulates osteoclastic Ca resorption
FUNCTIONAL RENAL ANATOMY from bone, facilitates the effect
parathyroid hormone (PTH) has on
A. MAJOR FUNCTIONS OF THE KIDNEYS bone resorption, & increases renal
tubular absorption of Ca. It is
Regulation of body fluid osmolality and volumes
essential for muscle and bone health
Regulation of electrolyte balance
and aids in the regulation of blood
Regulation of acid-base balance
pressure.
Excretion of metabolic end-products (urea, uric acid
3. Erythropoietin
& creatinine) & foreign substances (drugs,
o Produced by the by the peritubular
xenobiotics, etc.)
capillary endothelial cells in the kidney to
Production and secretion of hormones. The kidneys
stimulate RBC production in the erythroid
function as endocrine glands that produce and
marrow
secrete renin, calcitriol and erythropoietin.
o As the pluripotential stem cell differentiates,
1. Renin
it begins to produce receptors for
o manufactured, produced and secreted by
erythropoietin.
granular cells in juxtaglomerular apparatus. o In the presence of erythropoietin, the
o activates the Renin-angiotensin-
differentiated/dedicated stem cells become
aldosterone system
progenitor cells.
i. The kidney produces renin, w/c o In the absence of erythropoietin, a dedicated
converts angiotensinogen (from liver)
stem cell will undergo apoptosis.
into angiotensin I. This is the first step o As they differentiate into precursor cells,
and the rate-limiting step of the renin-
erythropoietin receptors are lost & depend
angiotensin-aldosterone system
on other substrates for further differentiation.
ii. Angiotensin I is converted into o Feedback mechanism:
angiotensin II by ACE (angiotensin
Hypoxia is the most potent stimulator of
converting enzyme)
erythropoietin. In hypoxic conditions,
iii. Angiotensin II produces the following
erythropoietin is secreted stimulating the
effects:
marrow to produce RBCs. Increase in RBC
formation of aldosterone
production leads to increase in O2 circulation
(important in Na and fluid retention,
and removal of hypoxic stimulus.
more importantly enhances Na
o Decreased RBC production is a cause of
retention, w/c leads to an increase
in blood volume and pressure)
anemia seen in chronic renal failure.
Direct systemic vasoconstriction
w/c can lead to hypertension
B. THE NEPHRON
Cardiac and vascular basic structural and functional unit of the kidney
hypertrophy Each human kidney contains approx. 1 Million
Indirect increase of blood volume nephrons, w/c consists of specialized tubular structure
through stimulation of the thirst & closely associated blood vessels.
mechanism. Number of nephrons at birth remains constant through
Stimulation of ADH (antiduiretic adulthood. Implication: premature babies who are born
hormone) secretion by the posterior with less nephrons are at greater risk for end-stage
lobe of the pituitary gland w/c also renal disease
leads water conservation The nephron consists of:
a. Renal corpuscle:
o Generally, it affects the adrenal cortex,
a. Glomerulus
kidney, intestine, CNS, PNS, vascular
a tuft of capillaries supplied by the
smooth muscle and the heart to maintain or
afferent arteriole and drained by the
increase extracellular volume (ECV), total
efferent arteriole
peripheral resistance and cardiac output.
covered by epithelial cells - podocytes
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 1 of 9
Mark | Marvin | Mau |Schubert
Dr. Elizabeth S. Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
b. Bowman’s capsule
visceral layer – formed by podocytes
parietal layer
Bowman’s space – capsular space
bet. the visceral and parietal layer;
lumen of the proximal tubule (at the
urinary pole)
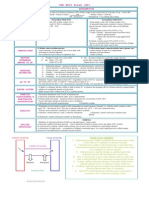
Figure 2. Tubular Segments of a [Juxtaglomerular] Nephron
There are two types of nephrons:
1. Cortical or superficial (~85%) – glomeruli are
near the periphery of cortex and nephron loops
in the outer medulla; characterized by a short
loop of Henle and an almost absent thin
Figure 1. Cellular Features of Renal Corpuscle ascending limb
2. Juxtamedullary – glomeruli are near the
b. Renal tubule corticomedullary junction and have relatively
a. Proximal convoluted tubule (PCT) long nephron loops that extend deep into the
several coils that descends toward the medulla.
medulla The efferent arteriole of juxamedullary
PCT cells nephron forms not only a network of peritubular
extensively amplified apical capillaries, but also a series of vascular loops
membrane (urine side) – brush called the vasa recta.
border
*** Vasa recta
highly invaginated basolateral
series of vascular loops that descends into
membrane (blood side) – many
medulla, form capillary networks
mitochondria
surrounding collecting ducts and
b. Loop of Henle
ascending limbs of Henle’s loop
Straight part of the proximal tubule
blood returns to the cortex in the
Descending thin limb, DTL (ending in
ascending vasa recta
hairpin turn)
receives < 0.7% of renal blood flow
Ascending thin limb, ATL (in
Functions: 1) conveys oxygen and
nephrons w/ long loops of Henle)
important nutrients to nephron segments;
DTL and ATL – poorly developed
2) delivers substances to the nephron for
apical and basolateral
secretion; 3) serves as a pathway for the
membrane; few mitochondria
return of reabsorbed water and solutes to
Thick ascending limb
the circulatory system, & 4) concentrates
abundant mitochondria; extensive
and dilutes urine
infoldings of the basolateral
membrane ***The renal medulla (pyramid) consists of two zones:
Macula densa (portion of the thick Outer zone
ascending limb passing between a. Outer stripe
afferent and efferent arterioles) b. Inner stripe
c. Distal Convoluted Tubule Inner zone
d. Collecting Duct (cortical CD J outer All segments of Henle’s Loop end at the same area of
medullary CD J inner medullary CD); the medulla, i.e. for a juxtamedullary nephron, the
2 types of cells straight part of the proximal tubule nephron will always
i. Principal cells – moderately end at the junction between the inner and outer
invaginated basolateral medullary stripe.
membrane; few mitochondria
ii. Intercalated cells – high
density of mitochondria `xÜÜç V{Ü|áàÅtá tÇw [tÑÑç
inner medullary CD – poorly
developed apical and basolateral axã lxtÜ ECDG4
surfaces; few mitochondria
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 2 of 9
Mark | Marvin | Mau |Schubert
Dr. Elizabeth S. Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
C. BASIC RENAL PROCESSES
The coordinated actions of the nephron’s various
segments determine the amount of substance that
appears in the urine. This represents 3 general
processes:
1. Glomerular Filtration - Filtration of plasma in the
glomerulus, ultrafiltrate then collects in the
urinary space of Bowman's capsule and flows
downstream to the tubular lumen
2. Tubular Reabsorption - Transport of
substances out of tubular lumen which are
returned to the systemic circulation via the
peritubular capillaries
3. Tubular Secretion - Transport of substances
from the peritubular capillaries into the tubular
lumen.
Figure 3. Two Types of Nephrons. Schematic of relations
between blood vessels and tubular structures and differences ***In Focus: Glomerular filtration
between cortical and juxtamedullary nephrons. See Netter (4e),
plate 336 for another depiction. RENAL BLOOD FLOW
C. VASCULAR SUPPLY Average renal blood flow of 1800 L/day urine flow of
Extrarenal vasculature: arteriole JcapillaryJvenule 2L/day
Renal vasculature: In resting subjects, the blood flow to the kidneys ≈ 1.25
arteriole J capillary J arteriole J capillary L/min ≈ 25% of cardiac output received by an organ less
Main renal artery (from abdominal aorta) J segmental than 0.5% of total body weight.
arteries (3-5;in the renal sinus ) J interlobar arteries Cortex receives bulk of the blood flow (82%) while the rest
(pass through the renal columns) J arcuate artery goes to the medulla and the papilla. The papilla is the
(traverses the base of the medullary pyramids) J most hypoperfused part of kidney, making it more prone to
interlobular arteries (important because this is where necrosis; however, it still gets more perfusion than the
the arterioles come from) J afferent arterioles J heart, brain and lungs.
glomerular capillary J efferent arterioles J
o In cortical nephrons, these send branches to Table 1. Comparison of the distribution of blood flow to the different
organs
peritubular capillaries (formed within the
Organs Blood Flow, mL/(g*min)
cortical area, forming a complex system in Kidney 4.0
the tubules) J interlobular vein J arcuate Heart 0.9
vein J interlobar vein J renal vein J IVC Brain 0.6
Liver 0.2
o In juxtamedullary nephrons,
Resting muscle 0.1
peritubular capillaries J vasa recta J
Roles served by renal blood flow (from the lecture)
interlobular vein J …. J IVC
Sustains filtration and excretion of end-products
***the vessels of the venous system, run parallel to the
such as urea and creatinine
arterial vessels.
Achieves rapid changes in body fluid
volumes and composition through
changes in renal excretion of water and
solutes
Serves a hemodynamic reserve function in
case if extreme emergency (shock) by
redistributing blood to other organs. That
is, RBF can be reduced to very low levels
to help sustain the blood flow in other
organs (brain, heart, etc)
Delivers sufficient oxygen and nutrients to
the kidneys.
Roles served by renal blood flow (more from
Berne)
Deliver sufficient oxygen, nutrients and
hormones to the cells of the nephron and
returning carbon dioxide and reabsorbed fluid
and solutes to the general circulation
Indirectly determines the GFR
Modifies the rate of solute and water reabsorption by the
Figure 4. Vascular Supply of the Kidney. Please take note that
proximal tubule.
the renal artery normally lies posterior to the renal vein. This
is not shown in the figure above. The figure highlights the course Participates in the concentration and dilution of urine
of blood as it is supplied to and drained from the kidney. Delivers substrates for excretion in the urine
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 3 of 9
Mark | Marvin | Mau |Schubert
Dr. Elizabeth S. Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
The blood flow through any organ may be represented by
GLOMERULAR FILTRATION
Q = ∆P / R
where:
A. FILTRATION MEMBRANE
Q = blood flow ≈ RBF
∆P = mean arterial pressure – mean venous pressure “making urine is just like making coffee”
R = total renal vascular resistance essentials:
filtration membrane
Accordingly, renal blood flow, RBF is equal to the
solid parts and large molecules suspended in
pressure difference between the renal artery and the plasma or blood
renal vein (VP) divided by the total renal vascular ultrafiltrate
resistance
||> GLOMERULAR FILTRATION
KVenous Pressure LRBF and KR L RBF
Ultrafiltration of plasma
Consider the forces that determine overall renal blood flow.
performed because the Glomerular Filtration
The basic equation demonstrates that virtually all factors
that influence total renal blood flow must do so by altering
Membrane is an extremely fine molecular sieve
either the arterial blood pressure or the renal vascular ||> GLOMERULUS
resistance. Pathway of fluid: ECL → BM → SM
Glomerular Filtration Membrane has three
layers for filtration:
1.) Endothelial Cell Layer (ECL)
contains blood vessels and capillaries
has sieve-like fenestrations (500-1000
Å) that allow the passage of small
molecules whilst restraining the
passage of large molecules
most permeable
2.) Basement Membrane (BM)
least permeable
two layers:
Figure 5. Pressure changes across renal vasculature. The a. Lamina Densa - central dense
generally accepted pressure gradient through the renal vascular layer
system. Areas of large pressure drops are main points of
b. Lamina Rara Interna & Externa -
autoregulation.
thinner and more electrolucent
The following notes come from 2013 trans. Those that outermost and innermost layers
were mentioned/emphasized in the lecture are in bold. 3.) Slit Membrane (SM)
There is a wide range of pressure in the kidneys the “diaphragm” of the glomerulus
because it reflects systemic pressure. lies in between the podocytes of
Main point of resistance: afferent arteriole endothelial cells (“interdigitations”)
provides dissipation of pressure moderately permeable because of the
very high venous resistance to blood flow presence of slit pores (250 Å)
Hydrostatic pressure drops dramatically Table 2. Filterability of some substances
between the beginning of the afferent Substance MW Molecular [ Filtrate/
arteriole & glomerular capillary. radius (Å) Plasma ]
Afferent arteriole has great influence on Water (H2O) 18 0.1 1.0
glomerular capillary by increasing or Glucose 180 0.36 1.0
Inulin 5000 1.4 1.0
reducing resistance
Hemoglobin 17000 2.0 0.03
Second drop at the efferent arteriole; 2nd point
Serum Albumin 69000 3.6 0.001
of resistance. Cationic Dextran (+) 3.6 0.42
Most active segments are the afferent and efferent Neutral Dextran 3.6 0.15
arterioles: segments that regulate blood flow Anionic Dextran (-) 3.6 0.01
Pressure at the glomerular and peritubular ↑ molecular size, the harder it is for the molecule to
capillaries are constant. Initial pressure of efferent pass thru the filtration membrane
arteriole is the same as final pressure of afferent ↑ filtrate to plasma ratio of a substance, the better
arteriole. it is filtered
Each of the capillary networks is exquisitely
||> FACTORS AFFECTING FILTERABILITY
designed to serve the functional needs of the
kidney. 1.) Size (most important factor)
Every day 180 liters of fluid pass through the substances of MW up to 5000 and radius
glomerular capillaries as filtrate. less than 15 Å are freely filtered
About 99% is recovered from the tubules ↑ size, ↓ filterability
and carried back into the general circulation
2.) Shape
via the peritubular capillaries.
slender and flexible = ↑ filterability
Remaining 1% continues on to its final
spherical and non-deformable = ↓ filterability
presentation as urine.
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 4 of 9
Mark | Marvin | Mau |Schubert
Dr. Elizabeth S. Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
3.) Electrical Charge
(+) charge = ↑ filterability
(-) charge = ↓ filterability
***the glomerular filtration membrane bears
negative charges due tah glycosaminoglycans,
e.g. heparan sulfate [recall: like charges repel]
B. GLOMERULAR FILTRATION RATE
total amount of filtrate formed by the Kidneys per
unit time (normally in minutes).
This is not how much blood passes through the
glomerulus each minute, but instead; it is how much
filtrate is removed from the blood each minute.
Figure 6. Glomerular Filtration is promoted by Capillary
unit = mL/min.
mL hydrostatic pressure and opposed by capsular hydrostatic
normal value = 125 /min. pressure and blood colloid osmotic pressure.
a test for Kidney Function
Key:
||> STARLING HYPOTHESIS PH = Pcap = Capillary hydrostatic pressure
the net movement of fluid out of a capillary is given π = πcap = Capillary [colloid] oncotic (or osmotic) pressure
by (equation from Berne): gradient due to proteins in plasma but not in
Bowman’s capsule
Jv = Kf [(Pcap – Pif) – σ(πcap – πif)] Pfluid = Pif = Fluid pressure created by fluid in Bowman’s capsule
πif = Interstitial [colloid] oncotic pressure gradient due to
where proteins in in Bowman’s capsule. w/c promotes
1.) Jv = Net fluid movement between compartments filtration. Under normal conditions, the
≈ GFR concentration of protein in the glomerular filtrate is so
low that the πif ~ zero.
2.) Kf = Coefficient of [Ultra]Filtration
NFR = Net Filtration Rate: Effective driving force for
= a constant of proportionality filtration.
= two components: = (Pcap – Pif) – σ(πcap – πif)
a.) capillary surface area = Normally, 10 mm Hg (assuming σ ≈ 1)
b.) capillary hydraulic conductance
= area x hydraulic conductance GFR = Kf × net filtration pressure
= ↑Kf, more water-permeable capillary Since normal value of GFR is 125
mL
/min, the normal Kf is
= ↓Kf, less water-permeable capillary ml
calculated to be about 12.5 /min·mmHg of filtration pressure
3.) σ = Reflection Coefficient Nice to know: when Kf is expressed per 100 g of kidney wt., it’s
= a correction factor about 4.2 ml/min/mm Hg, a value about 400 times as high as the Kf
= can have a value from 0 to 1 of most other capillary systems of the body; the average Kf of many
***Dr. Montemayor didn’t really expound nor gave much other tissues in the body is only about 0.01 ml/min/mm Hg per 100
attention to this. Anyway, glomerular capillaries have a σ grams. This high Kf for the glomerular capillaries contributes
value very close to 1
tremendously to their rapid rate of fluid filtration. However, changes
4.) Pcap = Capillary Hydrostatic Pressure in Kf probably do not provide a primary mechanism for the normal
= pressure brought about by water within day-to-day regulation of GFR. (Guyton&Hall, 11e)
capillaries directing water OUT of the
||> PRESSURE PROFILE
capillary
in a SKELETAL MUSCLE capillary:
5.) Pif = Interstitial Hydrostatic Pressure
hydrostatic pressure is high at the arterial end
= pressure brought about by water within
and low at the venous end; oncotic pressure is
the interstitium directing water INTO the
constant.
capillary
filtration occurs at arterial end; absorption
6.) πcap = Capillary Oncotic (or Osmotic) Pressure occurs at venous end
= pressure brought about by the presence initial hydrostatic pressure is 35 mmHg
of proteins within the capillaries directing in a GLOMERULAR capillary:
water INTO the capillary (recall the hydrostatic pressure profile is higher (> 55 mm
concept of gradients…water flows from
Hg, initially) and declines only very little with
higher concentration to lower concentration)
distance, Hydrostatic pressure remains
7.) πif = Interstitial Oncotic (or Osmotic) Pressure essentially constant from afferent arteriole to
= pressure brought about by the presence efferent arteriole (see Fig 5)
of proteins within the interstitium directing oncotic pressure increases due to filtration of
water OUT of the capillary (again…recall protein-free fluid (↑ protein content inside
thuh concept of gradients…water flows from capillary)
higher concentration to lower concentration)
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 5 of 9
Mark | Marvin | Mau |Schubert
Dr. Elizabeth S. Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
||> DETERMINANTS OF GLOMERULAR FILTRATION RATE 3.) (πcap – πif) as determined primarily by plasma oncotic
1.) Kf or permeability characteristic of glomerulus pressure. Low plasma oncotic pressure increases
depends on: the amount of filtrate.
a. Surface area available for filtration ↑ πcap ↓GFR. ↑ πcap is brought about by
– ↑ surface area, ↑ Kf, ↑GFR dehydration (↑ osmolarity), multiple myeloma and
b. Mesangial cell activity* hyperviscosity syndrome.
c. change in porosity of filtration membrane ||> SUBSTANCESWHICH AFFECT GLOMERULAR
– ↑ holes or pores, ↑ fluid mov’t, ↑GFR FILTRATION RATE
– inflammation (e.g. insect bites)
increases porosity 1.) Angiotensin
vasoconstrictor
*MESANGIAL CELLS preferentially constricts the efferent arteriole;
o another type of cell in the glomerulus but not making it the preferred inhibitor for renal disease
located within the capillaries at higher plasma levels:
o provide support for the glomerular capsule contracts all mesangial cells
o secrete extracellular matrix generalized vasoconstriction (afferent and
o regulate blood flow efferent)
o alter capillary surface area (w/c affects Kf & GFR) maintains central arterial pressure in
o secrete prostaglandins and cytokines; expense of RBF and filtration
o with phagocytic activity 2.) Endothelin – vasoconstrictor
2.) (Pcap – Pif) or the hydrostatic pressure difference 3.) Arginine Vasopressin (AVP) – vasoconstrictor
two kinds: 4.) Prostaglandins – vasodilator*
a. Capillary Hydrostatic Pressure 5.) Nitric Oxide (NO) – vasodilator
determined by aortic pressure or 6.) Natriuretic Peptides – vasodilator
changes in the resistance at the *2 & 3 lower RBF while 4, 5, 6 counteract the effects of
afferent and/or efferent arteriole vasoconstrictors
b. Hydrostatic Pressure at the Bowman’s
||> FILTRATION FRACTION and RENAL PLASMA FLOW
Capsule [space]
a.k.a. Interstitial Hydrostatic ♣ FILTRATION FRACTION (FF)
Pressure (Pif). ↑ Pif. ↓ GFR ratio of Glomerular Filtration Rate (GFR) to
↑ Pif is observed in patients w/ kidney Renal Plasma Flow (RPF)*
stones (nephrolithiasis). portion of the Renal Plasma Flow filtered in the
Changes in tubular hydrostatic kidneys
pressure: obstruction will increase represents the portion of the fluid reaching the
tubular pressure to as high as kidneys which passes into the renal tubules
capillary pressure and therefore no normal value: 0.15 to 0.20 (e.g. only ~20% of the
filtration can occur (GFR is zero). plasma that enters the glomerulus is actually
filtered.
♣ EFFECTS OF AFFERENT/EFFERENT
DILATION/CONSTRICTION ON DIFFERENT
FF = GFR / RPF
VARIABLES ♣ RENAL PLASMA FLOW (RPF)
– This is the subject of the take-home volume of blood plasma delivered to the kidneys
simulated laboratory experiment. per unit time
the kidneys are hyperfiltrating units
Table 3. Effects of afferent and efferent dilation on RBF, RPF = RBF x (1 – Hct);
HP, GFR, and FF
Blood consists of about 55% plasma and about
RBF ∆HP GFR FF 45% cellular components (mostly RBCs ≈
Afferent Dilation ↑ ↑ ↑ ↔ hematocrit, Hct)
mL
Efferent Dilation ↑ ↓ ↓ ↓ normal value: 650 /min
Afferent ↓ ↓ ↓ ↔ For “higher learning” : The following outlines the computation
Constriction of FF from the following “normal” values… Note the
Efferent ↓ ↑ ↑ ↑ relationship of the different variables.
Constriction*
a. Cardiac output (CO) = 6 L/min
* to compensate for the loss of nephrons, efferent
L
arterioles constrict. b. Renal blood flow (RBF) 20-25% of CO = 1.25 /min
c. Renal plasma flow (RPF) =RBF x (1 – Hct);
Variables: RBF = Renal Blood Flow
∆HP = Difference in Hydrostatic Pressure If the Hct level of the person is 45%.
GFR = Glomerular Filtration Rate RPF = (1250 mL/min)(1 – 0.45) = 687.5 mL/min
FF = Filtration Fraction d. Glomerular filtration rate (GFR) = 125 mL/min
Legend: ↑= increase, ↓ decrease, ↔ = same
e. FF = GFR / RPF = 125/687.5 = 0.182
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 6 of 9
Mark | Marvin | Mau |Schubert
Dr. Elizabeth S. Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
Effector Mechanism: Adenosine
C. AUTOREGULATION + +
with increased uptake of Na , K , Cl
-
ability of the kidneys to maintain constancy of a.) increased generation of Adenosine
Renal Blood Flow (RBF) and Glomerular Filtration b.) Adenosine activates Adenosine1
Rate (GFR) over a wide range of Renal Perfusion receptors triggering an increase in
Pressure or Blood Pressure cytosolic Ca2+ in the extraglomerular
Mechanisms: mesangial cells
c.) intensive coupling between
1.) Myogenic Reflex (universal, i.e. peripheral and
juxtaglomerular granular cells
renal)
containing renin and extraglomerular
T=PxR mesangial cells occurs, resulting in
where, afferent arteriole constriction and
T = vascular wall tension renin inhibition
P = transmural pressure gradient
R = inner radius of vessel **the reverse occurs w/ decreased uptake
of Na+, K+, Cl-
In order for T to remain constant: R is forced
to increase when P decreases and vice versa. ♣ JUXTAGLOMERULAR APPARATUS
Mechanism: – layers:
– vascular smooth muscles reflexively a.) Juxtaglomerular Granular Cells
contract (decreasing afferent arteriole • located at the walls of afferent
diameter) when stretched, reducing arterioles
blood flow. • contains specific granules
– vascular smooth muscles reflexively which produce renin
relax and dilate when not stretched, b.) Extraglomerular Mesangium
thereby increasing blood flow. • functional link between Macula
2.) Tubuloglomerular Feedback Mechanism Densa and Glomerular
due to the sensitivity of the macula densa Arterioles
cells of the juxtaglomerular apparatus to the • contains the Extraglomerular
filtrate osmolarity and/or rate of filtrate flow Mesangial Cells
in the terminal portion of the ascending loop c.) Macula Densa
of Henle • specific region of the thick
increase in GFR = increase in filtration = ascending limb which acts as a
increase in delivery of solutes to the tubules sensor arm
to the macula densa • where the cuboidal cells of the
thick ascending limb become
columnar
3.) Sympathetic Control
Sympathetic nerve fibers innervate all blood
vessels of the kidney as an intrinsic regulation
activity.
Minimal influence during normal daily activity
In extreme stress or blood loss, sympathetic
stimulation overrides the autoregulatory
mechanisms of the kidney.
Increased sympathetic discharge causes
intense constriction of all renal blood vessels
w/c has the following results:
The activity of the kidney is temporarily
lessened or suspended as blood is
shunted to other vital organs.
GFR reduction causes minimal fluid
loss from the blood maintaining higher
blood volume and blood pressure for
other vital functions.
Reduction in filtration cannot go indefinitely,
as waste products build up and metabolic
Figure 7. Tubulo-glomerular feedback mechanism. 1)GFR ↑ imbalances increase in the blood.
2) Flow through tubule ↑ 3) Flow past macula densa ↑ 4) IV fluid must soon be administered to
Paracrine from macula densa to afferent arteriole 5) Afferent increase blood volume and pressure
arteriole constricts; Resistance in afferent arteriole ↑; Hydrostatic and to decrease sympathetic discharge
pressure in glomerulus ↓; GFR ↓ and restore normal arteriole diameters
and normalize GFR and filtrate flow.
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 7 of 9
Mark | Marvin | Mau |Schubert
Dr. Elizabeth S. Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
Substituting equations (2) and (3) on equation (1) and
CLEARANCE PRINCIPLE
rearranging for Cw
•
Clearance is a term used to describe the rate of • U ×V
removal or clearing of a substance from the blood; Cw × Pw = U w × V ⇒ Cw = w
The principle of renal clearance emphasizes the Pw
excretory function of the kidney. Thus, it is used to
evaluate renal function.
The definition of clearance as a volume of plasma
The clearance principle is based on the Fick principle
from which all the substance has been removed and
(mass balance or conservation of mass).
excreted into the urine per unit time is somewhat
misleading since for most substances cleared by the
kidneys, only a portion is actually removed and excreted
in a single pass through the kidneys. The volume of
plasma in the above equation is an idealized volume.
Nevertheless, the concept of clearance is important
because it can be used to measure the GFR and renal
plasma flow and to determine whether a substance is
reabsorbed or secreted along the nephron.
Exercise: Compute for the subject's GFR using inulin*
clearance in mL/min
*inulin (from 2013 trans)
o Prototype drug (Considered to be the first pure compound to have been discovered
Figure 8. The Principle of Renal Clearnace. The renal artery in any series of chemically or developmentally related therapeutic agents.)
is the single input source to the kidney, whereas the renal vein o Polymer of fructose (MW=5000) non-toxic to humans
o Administered intravenously, not produced by the body
and ureter constitute the two output routes. o used to help measure kidney function by determining the GFR
o Freely filtered across the glomerulus into Bowman’s space
The following equation define the mass-balance o Neither reabsorbed, secreted, nor metabolized by nephrons
relationship (input = output): o Amount of inulin excreted in the urine per minute equals the amount
of inulin filtered at the glomerulus each minute
•
Pxa × RPF a = ( Pxv × RPF v ) + (U x × V ) Given: Plasma inulin conc = 4 mg/L
Urine collected in 10 hrs = 1 L
where mg
Urine inulin concentration = 300 /L
mass of inulin filtered mass of inulin excreted
=
time time
•
U inulin × V
GFR =
Pinulin ×
300 mg L × 1 L
= 10 h
The equation above is valid for any substance that is 4 mg L
1. freely filterable at the renal corpuscle (small and 300 mg L × 1000 mL
not bound to a protein), across the glomerulus = 600 min
into the Bowman’s space
4 mg L
2. Neither secreted nor reabsorbed by the tubule = 125 mL min
3. Not synthesized nor broken down by the Comparing the clearances of other substances
tubules For a certain substance, like inulin filtered
Useful derivations: Assume there is a susbtance (W) through glomeruli and not reabsorbed or
that meets the above criteria. secreted by tubules, Clearance of inulin equals
Glomerular Filtration Rate:
mass of W filtered mass of W excreted
= eqn (1) Cx = Ci = GFR
time time For a certain substance, x, that is filtered
mass of W filtered through glomeruli and reabsorbed by tubules,
= Pw × Cw eqn (2)
time Clearance of x equals GFR minus Tubular
mass of W excreted • Reabosorption Rate
=U w ×V eqn (3)
time Cx = GFR – Tax
Cx < Ci
Note:
Pw = concentration of substance w in plasma For a certain substance, x, that is filtered
Cw = “removal rate” or “clearance”; volume of through glomeruli and secreted by tubules,
plasma cleared of substance w per unit time Clearance of x equals GFR plus Tubular
(usually in mL/min)
Reabosorption Rate
≈ GFR (for substances that meet the above criteria)
Cx = GFR + TSx
Uw = concentration of substance w in the urine
. Cx > Ci
V = volume of urine per unit time (urine flow rate)
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 8 of 9
Mark | Marvin | Mau |Schubert
Dr. Elizabeth S. Montemayor
3
OS206 Abdomen and Pelvis
Lec 2: Overview of Renal Physiology
For a certain substance, x, that is filtered ZÜxxà|Çzá
through glomeruli and reaborbed and secreted Bry‐o‐chem: Woohoo! tis time fo greetin' 'gain!! this'd be a long one since
along the tubules, Clearance of x equals GFR thuh last one i did wuz real short..well..here it goes! Hello tah thuh whole
minus net reabsorption plus secretion rate of 2014! our effin openin' number wuz amazin! go europe! special thanks
tah nico 'course..galing! tah those who helped me wit' thuh voiceovers,
Cx = GFR – Tax + TSx
thanks a bunch! still owe ye guys a lil sumthin sumthin..:P congrats din
Cx > Ci sa'tin fo doin' a good job sa chorale competition! anne, dane, ate jana,
without y'all..wala..haha! go tenor 2's! A hello tah mah feedin' program
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐End ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
din..na on‐hiatus sa ngayon (parang glee na sa april pa ang balik..)..haha!
REFERENCES: we should have sumthin' befo' thuh break guys, yea? hello 'course tah
MPS: k‐ab, k‐flo, jb, tin, sam, alex, roland, therese, jason, marcus, karla! go
1. Dra. Montemayor’s lecture notes transcribed by Marivic and Bryan easy on me sa summer initiations! haha! hello tah mah fellow mss apps!
2. Physiology 5e by Berne, et al 'course, would i forget tah say hi tah iMed!! ano, kelan party? nga pala,
3. 2013 Transcription
hello tah mah roommates: poch, kuya renzo and phantom! now fo thuh
3. Textbook of Medical Physiology 5e by Guyton and Hall
single greetings: Hello tah: patrick ang sumasayaw na conductor at LO na
nanonoxic, aa, christelle and mairre (di makasayaw si christelle nung mss
APPENDIX victory party..wala daw kasi si mairre..haha!), ma‐e..spleen!, nic!, jonas
and his sausage marvyn!, mommy carla that i always greet :D, fellow mpl
Table 4. baby ko na si bossing!, sa bon‐casti duo, coy‐tincee‐ricky‐leeann quartet,
dalvie!, franco and camille, migz and ate abby (ate abby..'yung tanong ko,
di mo pa sinasagot..:P), lance G!, ching‐lennie couple (wahaha!), southbro
carlos!, carlo‐glaiza pair, dana na kaya nang mag‐stay awake sa class fo' up
tah 20 minutes!!, david!, lolo aidz!, robert!, hun shayne!, chesca na nililink
ko kay cons..haha!, faye!, rr‐joreb‐luigi wutta great drinkin' night we
had..til next time!, anna clau, april, mervyn na nagpapabati..may bonding
pa tayo bago mag‐break!, lau, jesha..sisiw!, yhan na namimiss ko
na..awww, marivic, alphius, dragons and virgins, zane, jam!, janna,
kimongkimongki! peace!, scott!, roni‐jaypang dance pair!, tonch a.k.a. sid
ng ice age/donatello ng tmnt, romeo and julieeeeee!, edge!, ado!, kay!,
karl babe na mahilig kumain sa class, godfrey & bea na magkamukha, jere
& roger na miss na ang isa't isa, zie!, grace v.!, marvie na miss na miss ko
na at sure na miss na rin niya'ko..2 months‐advanced happy birthday!
haha! overnight ulit tayo! :P, pito..still owe ye sumthin' effin long
overdue..lol..oyea, belated hb! chill sometime, yea?, peace&bounce! and
lastly hi tah jhing..thanx a lot! ;)
Woah! Haba pala nun! :| ohwell..haha! Merry Christmas and Happy New
Year 2014!! Enjoy thuh break!! Chillax lang..sa January na mag‐aral! haha
b.i.!
o eto..game: sa trans na 'to (not includin' thuh greetin' part)..there're two
words (only two!) that are part of mah text/e‐mail/ym language..find 'em and
show 'em tah me..may libreng dilly bar fro' dq ang pinakaunang makakahanap!
(trans group ko..di kayo kasama..haha!) guess that's it! Happy Holidays y'all!
Out!!
Marivic: Happy Holidays! ☺☺☺
Waaahh may space pa kaya naman babatiin ko
ang Class 2014 para sa matagumpay na TRP
opening number, stage design at chorale number
ngayong taon. Syempre special greetings sa mga
kapwa ko aprikano, na binigay ang lahat sa maiksi
ngunit di‐malilimutang parte sa opening number!
Inaantok na ako para isa‐isahing batiin ang mga
tao na patuloy na nagbibigay ng kakaibang saya at
inspirasyon sa akin. Mahaba pa ang ating
pagsasamahan at sana sa mga darating pang
panahon ay mas makilala natin ang isa’t isa. Ayun!
Sa mga nakakasama, nakakausap, nakakatrabaho,
nakaka‐chat at nakakabiruan ko sa araw‐araw
(kilala nyo na kung sino kayo) inaalay ko ang trans
na ito sa inyo… At sa iyo ____ hangad namin* ang
iyong kasiyahan at kapayapaan ng loob.
Ayun. Sa mga naki‐kidney o nababato ngayong
bakasyon, sana ay matuwa kayo sa trans namin.
Sana palampasin na ang mga pagkukulang tutal
maayos naman naming nagawa ito. Sana ay
makatulong nang lubos sa inyong pag‐aaral.
Maraming salamat kay Bryan at Marivic na gaya
ko ay binuno ang trans na ito.
Maligayang Pasko at Masaganang Bagong Taon sa
inyong lahat =) Labing‐apat! Walang katapat!
Nagpapasalamat para sa makabuluhang taon,
Figure 9. Renal blood flow and GFR Alphius
Alphius | Bryan| Jean | Marivic Thurs., Dec. 10, 2009 Page 9 of 9
Mark | Marvin | Mau |Schubert
Você também pode gostar
- PATHOMADocumento232 páginasPATHOMANicole Juliette CCAinda não há avaliações
- Pharmacology Step 1 For USMLEDocumento3 páginasPharmacology Step 1 For USMLEraj_1041100% (1)
- High-Yield Physiology Notes-Points For USMLE Step 1 & FCPS Part 1Documento11 páginasHigh-Yield Physiology Notes-Points For USMLE Step 1 & FCPS Part 1SHAKEEL1991Ainda não há avaliações
- Endocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologyDocumento3 páginasEndocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologySamuelAinda não há avaliações
- Pathology Mnemonics - Medical Students Wonder - Medical Powerpoint Presentations Videos Ebooks and OthersDocumento7 páginasPathology Mnemonics - Medical Students Wonder - Medical Powerpoint Presentations Videos Ebooks and OthersBhopesh KadianAinda não há avaliações
- UW (Step 1) Renal - Educational Objectives PDFDocumento50 páginasUW (Step 1) Renal - Educational Objectives PDFDrbee10Ainda não há avaliações
- Micro para - CompiledDocumento94 páginasMicro para - CompiledJanie-Vi GorospeAinda não há avaliações
- Autonomic Nervous System AgentsDocumento120 páginasAutonomic Nervous System Agentscoosa liquors100% (1)
- Acid Base StudyGuide PDFDocumento25 páginasAcid Base StudyGuide PDFMalik Ata Ur RehmanAinda não há avaliações
- USMLE Step 1 NotesDocumento5 páginasUSMLE Step 1 NotesvillarexAinda não há avaliações
- DR NajeebDocumento3 páginasDR NajeebByeongsu Park100% (1)
- Renal SystemDocumento76 páginasRenal SystemDaNy ChiriacAinda não há avaliações
- Renal Physiology IDocumento16 páginasRenal Physiology IJubilee Christiene AngAinda não há avaliações
- DR Kumar Ponnusamy Biochemistry-Genetics USMLE Preparatory Course BIOGEN Reusable On-Line Resources For Large Group Teaching-Learning in Relatively Short TimeDocumento1 páginaDR Kumar Ponnusamy Biochemistry-Genetics USMLE Preparatory Course BIOGEN Reusable On-Line Resources For Large Group Teaching-Learning in Relatively Short TimeDr Kumar Ponnusamy100% (1)
- TOPNOTCH Patho Supplement Handout For Sept 2018 UPDATED May 2018Documento25 páginasTOPNOTCH Patho Supplement Handout For Sept 2018 UPDATED May 2018Waiwit KritayakiranaAinda não há avaliações
- Platelets and Coagulation SystemDocumento5 páginasPlatelets and Coagulation Systemfaithfabulous1_06100% (1)
- CardiovascularDocumento18 páginasCardiovascularMedSchoolStuff100% (1)
- Disorders of Primary Hemostasis Quantitative Disorders of Secondary HemostasisDocumento23 páginasDisorders of Primary Hemostasis Quantitative Disorders of Secondary Hemostasisasda201487100% (1)
- Biochem High YieldDocumento106 páginasBiochem High YieldEvelyn Lee Russell100% (1)
- Qworld USMLE Step1 Course 2019Documento91 páginasQworld USMLE Step1 Course 2019Qworld0% (1)
- Renal Physiology NotesDocumento6 páginasRenal Physiology Notescipa920% (1)
- Mnemonic Lysosomal Storage Disorders....Documento3 páginasMnemonic Lysosomal Storage Disorders....Gurmeet Singh100% (1)
- Ion Channels in Health and DiseaseNo EverandIon Channels in Health and DiseaseGeoffrey S. PittAinda não há avaliações
- Clinical SignsDocumento26 páginasClinical SignswiraandiniAinda não há avaliações
- PhysiologyWorkbook7 5Documento267 páginasPhysiologyWorkbook7 5SophiaAinda não há avaliações
- SURVIVOR’S GUIDE Quick Reviews and Test Taking Skills for USMLE STEP 1No EverandSURVIVOR’S GUIDE Quick Reviews and Test Taking Skills for USMLE STEP 1Nota: 5 de 5 estrelas5/5 (2)
- FA MenominicsDocumento43 páginasFA MenominicssarahAinda não há avaliações
- General Pathology: Growth AdaptationsDocumento93 páginasGeneral Pathology: Growth AdaptationsPrarthanaAinda não há avaliações
- My Notes For USMLEDocumento1 páginaMy Notes For USMLEmonica ortizAinda não há avaliações
- USMLE Flashcards: Biochemistry - Side by SideDocumento137 páginasUSMLE Flashcards: Biochemistry - Side by SideMedSchoolStuffAinda não há avaliações
- Kirchers Pathoma AddendumDocumento70 páginasKirchers Pathoma AddendumJameson87Ainda não há avaliações
- Kaplan Powerpoint Pharm Review Usmle Step 1-: - Flash Cards by Cueflash PDFDocumento6 páginasKaplan Powerpoint Pharm Review Usmle Step 1-: - Flash Cards by Cueflash PDFAnonymous OAmXUJFRRR100% (1)
- Physiology: Guevara, Henaku-Larbi, Inciong, JutizDocumento3 páginasPhysiology: Guevara, Henaku-Larbi, Inciong, JutizMavic VillanuevaAinda não há avaliações
- Glomerulonephritis Cheat Sheet PDFDocumento1 páginaGlomerulonephritis Cheat Sheet PDFAnonymous aA9Ol6239Ainda não há avaliações
- 2 Renal Buzzword ChartDocumento6 páginas2 Renal Buzzword ChartTyler KingAinda não há avaliações
- PLM AbdomenDocumento11 páginasPLM AbdomenClaudine Victoria Taracatac100% (1)
- Haematology II Past Papers 3rd YearDocumento11 páginasHaematology II Past Papers 3rd YearSyed Muhammad HameemAinda não há avaliações
- USMLE Step 1 Study PlannerDocumento6 páginasUSMLE Step 1 Study Plannertmtb04Ainda não há avaliações
- Respiratory Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo EverandRespiratory Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsAinda não há avaliações
- GOLJAN - Special Pathology (Resp)Documento21 páginasGOLJAN - Special Pathology (Resp)bobiomeAinda não há avaliações
- Diseases - BiochemDocumento4 páginasDiseases - BiochemJay FeldmanAinda não há avaliações
- USMLE Step 1 JournalDocumento167 páginasUSMLE Step 1 Journalmed studentAinda não há avaliações
- 3 Physiology Notes PDFDocumento119 páginas3 Physiology Notes PDFshiningdream100% (1)
- 2 BiochemWorkbook 5.5Documento168 páginas2 BiochemWorkbook 5.5step wonAinda não há avaliações
- St. Luke's College of Medicine - William H. Quasha MemorialDocumento3 páginasSt. Luke's College of Medicine - William H. Quasha MemorialMavic VillanuevaAinda não há avaliações
- Biochemistry PDFDocumento1.193 páginasBiochemistry PDFAmna ShahAinda não há avaliações
- St. Luke's College of Medicine - William H. Quasha Memorial: PhysiologyDocumento6 páginasSt. Luke's College of Medicine - William H. Quasha Memorial: PhysiologyMavic Villanueva100% (1)
- UW 2021 Notes - Lungs UsmleDocumento422 páginasUW 2021 Notes - Lungs Usmlekathi raja sekhar100% (1)
- Goljan Blue NotesDocumento1 páginaGoljan Blue NotesCarl NieweldAinda não há avaliações
- Step 1 ShartzDocumento333 páginasStep 1 ShartzDaniella Vazquez100% (1)
- 'Aliah's Physio NotesDocumento30 páginas'Aliah's Physio NotesLuqman Al-Bashir FauziAinda não há avaliações
- Microbiology PDFDocumento237 páginasMicrobiology PDFchioAinda não há avaliações
- Pregnancy and Lactation Flashcards - Guyton Physiology Chapter 82Documento19 páginasPregnancy and Lactation Flashcards - Guyton Physiology Chapter 82MedSchoolStuffAinda não há avaliações
- Renal CastsDocumento1 páginaRenal Castsgregoryvo100% (4)
- UW (Step 1) Biochemistry - Educational ObjectivesDocumento41 páginasUW (Step 1) Biochemistry - Educational ObjectivesUsama BilalAinda não há avaliações
- Assignment MicrobioDocumento7 páginasAssignment MicrobioHariz BukhariAinda não há avaliações
- Biosphere Clinical Research Profile - 2020Documento18 páginasBiosphere Clinical Research Profile - 2020UK BiosphereCROAinda não há avaliações
- Daftar Pustaka: Head and Neck Surgery 3Rd Edition. Mcgraw-Hill, San Francisco (HalDocumento3 páginasDaftar Pustaka: Head and Neck Surgery 3Rd Edition. Mcgraw-Hill, San Francisco (HalBhisma SuryamanggalaAinda não há avaliações
- Position PaperDocumento2 páginasPosition PaperEunice Pasana100% (1)
- Cardiac OutputDocumento37 páginasCardiac OutputIndrashish Chakravorty100% (1)
- Dent Clin N Am 50 (2006) 547-562Documento16 páginasDent Clin N Am 50 (2006) 547-562lalajanAinda não há avaliações
- JONAM16000170Documento14 páginasJONAM16000170R.G.ManikarajanAinda não há avaliações
- The Ketogenic Diet - A Detailed Beginner's Guide To KetoDocumento19 páginasThe Ketogenic Diet - A Detailed Beginner's Guide To Ketoradhika1992Ainda não há avaliações
- Pathology 2 TND LiveDocumento38 páginasPathology 2 TND Livepavan kumarAinda não há avaliações
- HandoutDocumento3 páginasHandoutapi-336657051Ainda não há avaliações
- A Clinical Study in The Management of Bahya Arsha External Haemorrhoids, Piles With Suvarchikadi Lepa Study ReviewDocumento7 páginasA Clinical Study in The Management of Bahya Arsha External Haemorrhoids, Piles With Suvarchikadi Lepa Study ReviewEditor IJTSRDAinda não há avaliações
- Prisma Med - Schneider Electric - or SwitchboardDocumento20 páginasPrisma Med - Schneider Electric - or SwitchboardAna RuxandraAinda não há avaliações
- Cues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationDocumento3 páginasCues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationVher SisonAinda não há avaliações
- Unit 5-Heart QuestionsDocumento37 páginasUnit 5-Heart Questionsareyouthere92100% (1)
- CL Head Lice - Diagnosis and TherapyDocumento7 páginasCL Head Lice - Diagnosis and TherapyMaya Asharie HarahapAinda não há avaliações
- Clinical and Etiological Profile of Acute Febrile Encephalopathy in Eastern NepalDocumento3 páginasClinical and Etiological Profile of Acute Febrile Encephalopathy in Eastern NepalNeha OberoiAinda não há avaliações
- M Airt TDocumento6 páginasM Airt TLeticia GallardoAinda não há avaliações
- Fcps IMMDocumento22 páginasFcps IMMHaseeb Rasool0% (1)
- Pi Is 0016508506600139Documento328 páginasPi Is 0016508506600139AsmaerAinda não há avaliações
- An Insight Into The Quality Assurance of Ayurvedic, Siddha and Unani DrugsDocumento10 páginasAn Insight Into The Quality Assurance of Ayurvedic, Siddha and Unani DrugsHomoeopathic PulseAinda não há avaliações
- Combination of Microneedling and 10% Trichloroacetic Acid Peels in The Management of Infraorbital Dark CirclesDocumento16 páginasCombination of Microneedling and 10% Trichloroacetic Acid Peels in The Management of Infraorbital Dark CirclesAna Claudia Kordelos DinizAinda não há avaliações
- JetoptimusDocumento7 páginasJetoptimusShubh YouTubeAinda não há avaliações
- Nosocomial InfectionDocumento7 páginasNosocomial InfectionSachin ParamashettiAinda não há avaliações
- Forbidden Cures E Book DR SircusDocumento381 páginasForbidden Cures E Book DR Sircusvitaolga7100% (18)
- AR 2009-2010 WebDocumento36 páginasAR 2009-2010 WebOsu OphthalmologyAinda não há avaliações
- Autism Assessment New Referral Form PDFDocumento3 páginasAutism Assessment New Referral Form PDFshalina0% (1)
- Sputum ExaminationDocumento9 páginasSputum ExaminationDr. Ashish JawarkarAinda não há avaliações
- Therapeutic Communication in Psychiatric NursingDocumento21 páginasTherapeutic Communication in Psychiatric NursingElisha Gine AndalesAinda não há avaliações
- Harga OpthaDocumento1 páginaHarga Opthaalifudinalifudin51Ainda não há avaliações
- Consumos Medicamentos 2020Documento568 páginasConsumos Medicamentos 2020LUCERO LOPEZAinda não há avaliações