Escolar Documentos
Profissional Documentos
Cultura Documentos
Pocket Guide June2013 PDF
Enviado por
SergeyGruntovDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Pocket Guide June2013 PDF
Enviado por
SergeyGruntovDireitos autorais:
Formatos disponíveis
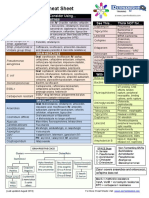
Adul t Pocket Anti mi crobi al Gui de
Infection
Acute osteomyelitis
Microbiologic diagnosis is essential. If blood cultures negative, need culture of bone.
If risk of MRSA
Septic Arthritis:
Open Fractures:
Prosthetic Joint
Native joint
Microbiologic diagnosis is essential. If blood cultures negative, need culture of bone.
Previously MRSA +ve
If gonococcal septic
arthritis suspected
First Line
Flucloxacillin 2g IV 4 Hourly
Vancomycin IV (See page 11 for dose)
+ Rifampicin 450mg PO BD
Total course length 6 weeks
Benzylpenicillin
if heavy soil / farm/ faecal
+
for 72 hours or 24 hours after
until C+S available
wound adequately covered
then amend on
Cefuroxime
Vancomycin
1.2g IV QDS
1.5g IV TDS
IV
Flucloxacillin 2g IV QDS
Vancomycin IV
Add
(See page 11 for dose)
Contact medical microbiology
for advice
Total course length: 14-28 days
Penicillin Allergic / Alternative
Clindamycin 600mg IV QDS
As for 1st Line treatment
Clindamycin
Clindamycin
for 72 hours or 24 hours after
As for 1st line treatment
600mg IV QDS
600mg IV QDS
As for 1st Line treatment
Contact medical microbiology
for advice
Bone & Joint
3rd EDITION
Patient Age
<50 years of age
>50 years of age or
immunosuppressed
(including alcoholics,
diabetics)
First Line
Ceftriaxone 2g IV BD
Ceftriaxone 2g IV BD
+ Amoxicillin 2g IV QDS
(to treat possible listeria)
Penicillin Allergic / Alternative
Contact medical microbiology
for advice
Contact medical microbiology
for advice
Bacterial Meningitis
Total duration of antibiotic therapy (all IV)
Unknown: 7 days
Neisseria meningitides (meningococcus): 7 days
Streptococcus pneumoniae (pneumococcus): 10 - 14 days
Haemophilus influenzae: 7 days
Group B streptococcus: 10 - 14 days
Listeria monocytogenes: 2 - 3 weeks
If (suspected) encephalitis add in
AciclovirR 10mg/kg IV TDS
Oral NOT recommended.
Viral Encephalitis
Central Nervous System Clostridium difficile
Actions where Clostridium difficile diarrhoea suspected or confirmed:
Adequate replacement of fluid and electrolytes
Ensure the patient is accommodated in a single roomwith clinical hand washing sink and
either en-suite facilities or a designated toilet/commode
All HCWs must remove PPE (gloves/aprons) immediately after contact with patient and
their environment
The patient's immediate environment and patient care equipment must be cleaned with
HCWs must performhand hygiene with liquid soap and water for 15-20 seconds
immediately after removal of PPE. Alcohol hand gel/rub not suitable for hand hygiene
Test the stool for toxin
Do full blood count, stool chart, temperature, abdominal X-Ray (if abdo distended), CRP, U&Es
Discontinue unnecessary PPIs and anti-motility agents
Notify Infection Prevention and Control Nurse
a neutral detergent and disinfected with a hypochlorite solution
Severity Assessment (the following are indicators of severe infection):
Age>60, Temp>38oC, albuminlevel <25g/L, GFR<40ml/min, WBCcount of >15,000cells/mm3, elevatedcreatinine,
endoscopic evidenceof pseudomembranous colitis or needfor ITUcarebecauseof C.diff complications.
Disease Severity
Mild-Moderate
Severe / pregnancy
Fulminant disease
(pulse >100 AND abdo distension/
tenderness, dilatation on X-ray,
stool >10x / day)
Recurrence/Relapse
First Recurrence
Second recurrence
Contact Gastroenterology Registrar
Third recurrence
Treatment
Metronidazole 400mg TDS PO/NGT
Vancomycin 125mg PO/NGT QDS
Vancomycin 500mg PO/NGT QDS
+/- Metronidazole 500mg IV TDS
+ refer to Gastroenterology and surgical registrar
Treat as per initial therapy
Vancomycin 500mg PO QDS for 7 days
Vancomycin 125mg PO BD for 7 days
Vancomycin 125mg PO ODfor 7 days
Vancomycin 125mgAlternate days PO for 7 days
Vancomycin 125mg every 3 days PO for 7 days
Then STOP
Contact medical microbiology for further advice
Total Course length: 10 - 14 days
If patient is worsening at 48hrs step up therapy to next regimen.
Reassess patient at Day 5 of treatment:
if responding - continue for further 5 - 9 days
if NOT responding - step therapy up to next regimen and repeat process
Vancomycin injection can be used orally
For 125mg dose: Dissolve 500mgvancomycin injection in 10ml water for injection and administer 125mg (2.5ml) orally.
Mark date and time of preparation on the vial. The reconstituted vial can be used for up to 24 hours if kept in the fridge.
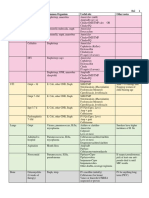
Gastro-intestinal Empiric Antibiotic Management of CAP,
Infection
Healthcare Acquired
Pneumonia (HAP)
<5 days sinceadmission
Evidenceof consolidation
on CXR
>5 days sinceadmission
or after ventilation
If requiring ICU
care or MRSA
Aspiration pneumonia
First Line
Treat as per CAP regime
for 7 days
Mild HAP:
Co - amoxiclav 625 mg POTDS
for 7 days
Moderate - Severe HAP:
Piperacillin/tazobactam
4.5g IV TDS for 7 days
+ Vancomycin IV (see page 11 for dose)
Co - amoxiclav 1.2g IV TDS
When tolerating oral consider
switch to: Co - amoxiclav
625mg POTDS (tablets) or
20mls TDS of paediatric 125/31.25 liquid for 5 - 7 days
Penicillin Allergic / Alternative
Treat as per CAP regime
for 7 days
Contact Medical Microbiology
Contact Medical Microbiology
for advice
for advice
Respiratory
Infection
Human/Dog/Cat Bites
Consider IV for first 24hrs
Diabetic Foot Ulcers
(mild/moderate)
(severe)
Necrotising Fasciitis
Urgent Gram-stain on
debrided tissue
Send blood culture
Discuss with a
Shingles
Grossly
Normal host
Contaminated
Immunocompromised
Wounds
(not severe)
(e.g. Road Traffic
Immunocompromised
Accidents)
First Line
Co-amoxiclav 625mg PO TDS
for 5 days
Co-amoxiclav 625mg PO TDS
Piperacillin/Tazobactam
4.5g IV TDS
Vancomycin IV (see page 11) +
Benzylpenicillin 2.4g IV 4 hourly
+ Clindamycin 900mg IV QDS
ValaciclovirR 1g PO
Wound debridement:
TDS for 7 days
Co-amoxiclav 625mg PO TDS
Severe:
Flucloxacillin 2g IV QDS
+
AciclovirR
Metronidazole
10mg/kg
400mg PO TDS
IV TDS for 10 - 14 days
+ Ciprofloxacin 500mg PO BD
reviewafter 5 days
Penicillin Allergic / Alternative
Co-trimoxazole 960mg PO BD
+ Clindamycin 300mg PO QDS
for 5 days
Clindamycin 300mg PO QDS
Clindamycin 900mg IV QDS
Clindamycin 450mg PO QDS
+ Ciprofloxacin 500mg PO BD
as for 1st line treatment
reviewafter 5 days
Skin & Wound
Dr. Cathal O'Sullivan, Consultant Microbiologist: (086) 0404894or viaswitch
MariePhilbin, Antimicrobial Pharmacist: Bleep312(MRHTonly);
JaneMartin, Antimicrobial Pharmacist: Bleep143(MRHPonly).
Microbiologist
Ear Nose & Throat
Infection
Acute Pharyngitis
Acute Epiglottitis
Acute Sinusitis
Post-tonsillectomy
Peritonsillar
(most casesare
mild- moderate
viral inaetiology)
severe
First Line
Benzylpenicillin 1.2g IV QDS
Ceftriaxone 2g IV BD
Amoxicillin 500mg-1g PO TDS
Co-amoxiclav 1.2g IV TDS
Benzylpenicillin 1.2g IV QDS
ReviewIVdaily&consider
for 5-7 days
5 - 7 days
500mg IV TDS
switch to 500mg Penicillin V
10 - 14 days
for 10 days
PO QDS for 10 days in total.
Penicillin Allergic / Alternative
Clarithromycin 500mg IV BD
Contact Medical Microbiology
Clarithromycin PO 500mg BD
Clindamycin 600mg IV QDS
ReviewIV daily and consider
for advice
or PO 200mg STAT Doxycycline
switch to PO Clarithromycin
then 100mg OD
for 3 - 5 days
500mg BDfor 10 days in total.
5 - 7 days
10 - 14 days
following care/contact.
NOTE: Not all cases
require antibiotics
If monospot positive
consider stopping
antibiotics
For further advice contact:
contamination
450mg PO BD
wound adequately covered
Administer antibiotic
Infection
ASAP after injury,
Obtain cultures before
ideally within 3 hours
starting antibiotics
Rifampicin
microbiology advice
Total course length: hip - 3 Months; Knee - 6 Months
+ Vancomycin IV
+ Vancomycin IV
(HSV / VZV)
Medical emergency antibiotics should be given
Take blood cultures using blood culture Prophylaxis: SeeAntibiotic Prophylaxis
packs and aseptic technique. Seek guidelines on information onAntimicrobials
assistance fromnursing staff. intranet page or BNF
Do LP if no contradictions Isolate patient
If LP or blood culture delayed, first dose of Notify Public Health: (057) 935 9891
bleed for 3 - 5 days
abscess + Metronidazole
Clindamycin 600mg IV QDS
for 10 days
Reviewpatient's antibiotic regime - stop all offending antibiotics if possible
Reviewdaily for clinical response
OR
Rifaximin 400mg PO TDS for 20 days
followed by:
Vancomycin 125mg PO QDS for 10 days
Infection
Appendicitis / Diverticulitis
(mild - moderate)
Acute Cholangitis
Peritonitis (severe)
Primary Peritonitis (SBP)
Consider 2 weeks
of treatment if blood
cultures positive
Secondary Peritonitis
(bowel perforation, ruptured appendix, ruptured diverticula)
(without necrosis)
(Idiopathic)
Pancreatitis Acute alcoholic
Pancreatic abscess,
pseudocyst, post-necrotising
pancreatitis
Antimicrobial prophylaxis
necrotising pancreatitis
First Line
Co-amoxiclav 1.2g IV TDS
ReviewIV at 48hrs and consider
switch to:
Co-amoxiclav 625mg PO TDS
for a total course of 7 days
Piperacillin/tazobactam
4.5g IV TDS
+ Gentamicin IV(seepage12for dose)
for 7 - 10 days
Co-amoxiclav 1.2g IV TDS
ReviewIV at 48hrs and consider
switch to:
Co-amoxiclav 625mg PO TDS
No antimicrobials
No necrosis on CT
Observe for pancreatic abscesses or necrosis which require therapy
Need culture of abscess/infected pseudocyst to direct therapy.
Can often get specimen by fine-needle aspiration.
Use of antimicrobials is controversial
Penicillin Allergic / Alternative
Cefuroxime 750mg IV TDS
+ Metronidazole 500mg IV TDS
ReviewIV at 48hrs and consider
switch to:
Ciprofloxacin 500mg PO BD
+ Metronidazole 400mg PO TDS
for a total course of 7 days
Ciprofloxacin 400mg IV BD
+ Metronidazole 500mg IV TDS
+ Vancomycin 1g IV BD
for 7 - 10 days
Ceftriaxone 1g IV OD
Cholecystitis
Diverticulitis (severe)
Contact Medical Microbiology
for advice
Urgent Surgical Debridement
Strep or Clostridia
MeropenemR 2g IV TDS
+ Gentamicin IV STAT
as for 1st line treatment Polymicrobial
IV STAT
(see page 12 for dose)
IV + Vancomycin as for 1st line treatment If risk of MRSA
(see page 11 for dose)
Periorbital Cellulitis Ceftriaxone IV 2g OD as for 1st line treatment
IV + Vancomycin
(see page 11 for dose)
IV 500mg TDS + Metronidazole
If risk of MRSA
as for 1st line treatment
(severe)
Infective Exacerbation of COPD & LRTI
History & Examination: The patient has, without other obvious cause, acute illness
with cough & other respiratory tract symptoms, features of systemic infection
(pyrexia, rigors, etc.)
Investigations; CXR, Oxygen saturations (+/- ABG), FBC, U&E, CRP and ECG. Sputum
sample if purulent sputumand blood cultures if pyrexial. Consider need to out-rule TB and
viral source of infection (influenza PCR).
IF LIFE THREATENING DISEASE: Give STAT IV Abx before CXR
New focal consolidation on CXR?
YES NO Does the patient have
a history of COPD?
Calculate & Record
severity score +1 for each of
onfusion
rea > 7mmol/L
espiratory Rate 30/min
(SBP) < 90/DBP<60mmHg)
Age yrs
CURB-65
C
U
R
BP
65
YES NO
CURB-65 1st Line Alternative Comments
0-1
(Mild)
MONO-
THERAPY
0-1
2
(with co-
morbidity)
(Moder-
ate)
3-5
(severe)
Amoxicillin
500mgPO
TDS
Amoxicillin
500mg- 1g
POtds+
500mgPO
bd
Clarithro-
mycin
Co-
amoxiclav
1.2gIVtds+
500mgIVbd
Clarithro-
mycin
Clarithromycin
Doxycycline
500mgPOBD
or
200mgSTAT
POthen
100mgOD
Doxycycline
Levofloxacin
200mgPOOD
day1then
100mgPOOD
or
500mgPOOD
R
LevofloxacinR
500mgIVBD.
ReviewIV
dailyand
consider
switchtoPO
Maybe
suitablefor
discharge
Duration
5-7days
Duration
7days
Send
pneumoc-
occal &
legionella
urinary
antigen.
Dur. 7days
Acute Infective
Exacerbation of COPD
if associatedwith 2
increased;
Breathlessness
Sputumcolour/purulence
Sputumvolume
ABX MONOTHERAPY
x5 days
Amoxicillin
500mg IV/PO tds
OR
500mg IV/PO bd
OR
200mg PO Day 1
then 100mg PO OD
Clarithromycin
Doxycycline
Non-pneumonic LRTI
manycasesareviral, this
is
But if signsof severity:
[raisedrespiratoryrate
(>30/min), lowBP
(SBP<90mmHg+/- DBP
<60mmHg), new
confusion, tachycardia
(>100/min), pyrexia] or if
significant co-morbid
diseasecommence
antibiotics.
not an indication for
antibiotics.
*CURB-65scoreshouldalwaysbeinterpretedinconjunctionwithclinical judgement andre-assessedwithin24hrs.
QueriesREpenicillinanaphylaxis, severeCAP, ICUrefer toConsultant Microbiologist.
Prescribing in Penicillin Allergic Patients
Drugs in RED are contra-indicated
Drugs in ORANGE should be prescribed with caution
Drugs in GREEN are considered safe
Caution =Avoid if allergy history suggests anaphylaxis or erythroderma unless benefit
outweighs the risk.
NB: there is up to 10% cross reactivity with cephalosporins in true penicillin allergic patients.
Allergy
PAGE 01 PAGE 02 PAGE 03 PAGE 04 PAGE 05 PAGE 06 PAGE 07
All doses stated assume 'normal' renal function.
Please note: Elderly patients may have renal impairment
despite a 'normal' serum creatinine
Dosing of Vancomycin, Gentamicin and Amikacin in renal impairment is
included as a separate section in this guide (pages 11 & 12).
Some antimicrobials require dose adjustment in all degrees of renal
impairment (aciclovir, levofloxacin, meropenem, valaciclovir).
R
These are highlighted throughout the guide by
For dosing of these and all other agents in renal impairment consult
BNF at www.medicinescomplete.com or www.medicines.ie
.
.
Revised J uly 2013. Approved by Pharmacy &Therapeutics Committee and Clinical Directors
(See page 11 for dose)
(See page 11 for dose)
(See page 11 for dose)
Determine presence of sepsis - if present refer to systemic sepsis section of guideline
>
>
>
Infection
Urinary Tract
Infection
Female,
non complicated
Pregnant women
Male
Pyelonephritis /
Urosepsis
Prostatitis (Acute)
Mild / Moderate
Severe
Epididymo-orchitis
NO risk of
N.gonorrhoeae /
C.trachomatis:
RISK of
N.gonorrhoeae /
C.trachomatis:
First Line
If GFR >50ml/min:
Nitrofurantoin 50 - 100mg PO QDS
for 3 days
If GFR <50ml/min or GFR unknown:
Trimethoprim 200mg PO BD
for 3 days
Cefalexin 500mg PO TDS
for 7 days
If GFR >50ml/min:
Nitrofurantoin 50 - 100mg PO QDS
for 7 days
If GFR <50ml/min or GFR unknown:
Trimethoprim 200mg PO BD
for 7 days
Or
Co-amoxiclav 625mg PO TDS
for 7 days
Co-amoxiclav 1.2g IV TDS
+ Gentamicin IV (seepage12for dose)
for 1 - 2 doses
ReviewIV at 48hrs and
consider switch to oral:
Co-amoxiclav 625mg PO TDS
for a total of 10 - 14 days
Ciprofloxacin 500mg PO BD
for 28 days
If IV required, treat as
urosepsis for 24 hrs then
Ciprofloxacin 500mg PO BD
for 28 days
Ciprofloxacin 500mg PO BD
for 14 days
Cefixime 400mg PO STAT
(Or Ceftriaxone 250mg IM STAT)
+ Doxycycline 100mg PO BD
for 10 - 14 days
Penicillin Allergic / Alternative
Cefalexin 500mg PO TDS
for 3 days
Or
Ciprofloxacin 500mg PO BD
for 3 days
Contact Medical Microbiology
for advice
Ciprofloxacin 500mg PO BD
for 7 days
Gentamicin IV
ReviewIV at 48hrs and
consider switch to oral:
Ciprofloxacin 500mg PO BD
for a total of 10 - 14 days
Trimethoprim 200mg PO BD
for 28 days
Ciprofloxacin 400mg IV BD
for 24 hrs then,
Ciprofloxacin 500mg PO BD
to complete a 28 day course
Contact Medical Microbiology
for advice
Urinary Tract & Uro-genital
Infection
Unknown source
Neutropenic sepsis
First Line
Piperacillin/tazobactam
4.5g IV TDS
MeropenemR IV 1g TDS
+
Amikacin
Gentamicin
15mg/kg IV STAT
IV STAT
If risk of MRSA:
+ Vancomycin IV (see page 11 for dose)
Piperacillin/tazobactam
4.5g IV QDS
+ Gentamicin IV
If suspected central line /
MRSA infection:
+ Vancomycin IV (see page 11 for dose)
Penicillin Allergic / Alternative
Contact Medical Microbiology
for advice
MeropenemR 1g IV TDS
+ Vancomycin IV
Systemic sepsis Empiric Antibiotic Management
Infection
Native valve or
First Line Penicillin Allergic / Alternative
Vancomycin IV
+ Gentamicin 1mg/kg
+ Rifampicin 450mg PO 12-hrly
Cardiac (Endocarditis)
Before starting antibiotics, ALWAYS take 3 sets of blood cultures
(from3 separate venopuncture sites) at the same time using blood culture
For each set send samples in aerobic and anaerobic bottles
Discuss with a Microbiologist &a Cardiologist
IV to Oral Switch Criteria
Switching a patient from IV to Oral may decrease their length of stay (LOS)
Considerations for switching a patient from IV to Oral therapy:
Absence of Specific indication / deep seated infection (see exclusions below)
Oral Route is not compromised - able to swallowand tolerate oral fluids,
normal GI absorption (no diarrhoea / vomiting) and an oral equivalent is available O O
Labs showa trend towards normal.
The patient should be apyrexial (Temp >36 and <38C) for at least 24hrs AND
meet the majority of the following:
- Respiratory rate <20 breaths/min
- Heart rate <100 beats/min for last 12hrs
- Systolic blood pressure >100 mmHg
- Roomair oxygen saturation >90%
- White cell count >4x109/L or <11x109/L
- Improving CRP
L L
S S
Intravenous Vancomycin
*Obese patients require a lower dose; ask pharmacy or use the dosing weight calculation in the box
Administration and monitoring for toxicity
Only give >48 hrs under direction frommedical microbiology
Take a pre-dose level immediately before the third dose
Wait for the result.
If the pre-dose level <5 mg/L, the third dose can be given at current dosing interval
dosing interval extended for subsequent doses
If the pre-dose level >5 mg/L, the third dose should be omitted and the level repeated in 12 hours
The next dose of amikacin should not be given until the level falls below5 mg/L and the
dosing interval extended for subsequent doses
IV infusion in 100 ml sodiumchloride 0.9%or glucose 5%given over 30 minutes
Creatinine clearance (CrCl)
The eGFR can be used as a quick estimate for calculating initial doses.
Amore accurate estimate can be obtained using the Cockcroft-Gault equation
(N=1.23 males, 1.04 females)
CrCl (ml/min) = N x [140 - age (years)] x Wt#(kg)
Serumcreatinine (micromol/L)
#Ideal Body Weight (IBW)
Use IBWif actual weight >120 %IBW
IBW(kg) =50 kg (male) or 45 kg (female) +1 kg per cmover 152 cm
Dose Determining Weight (DDW)
Use DDWfor Gentamicin andAmikacin prescriptions if actual body weight >120%IBW
DDW(kg) =IBW+0.4 (Actual weight - IBW)
Renal function (CrCl) Dosage Regime
>60 ml/min 5 mg/kg* OD (max 400mg)
30-60 ml/min 3 mg/kg* OD (max 200mg)
<30 ml/min 1.5 mg/kg* STAT
Gentamicin
*Obese patients require a lower dose; ask pharmacy or use the dosing weight calculation in the box
Administration and monitoring for toxicity
Writeastopdateattimeof initial prescribing. Onlygive>48hrs underdirectionfrommedical microbiology
Level required at least 18hrs after first gentamicin dose. Then aimfor pre-dose level <1mg/L
Wait for result before administering second dose
IV infusion in 100 ml sodiumchloride 0.9%or glucose 5%given over 30 minutes
Adjust dose/frequency of gentamicin using table below
CrCl (mL/min) Starting dose (slow infusion) Interval
>100 1.5 grams 12 hours
65-100 1 gram 12 hours
55-65 750mg 12 hours
45-55 1 gram 24 hours
35-45 750mg 24 hours
25-35 500mg 24 hours
<25 1 gramstat Wait for levels
Where possible prescribe bd regimes at 10am and 10pm, and once daily regimes at 10am.
Document time at which level taken
Thereis aseparateguidelinefor dosing, administration&monitoringof Vancomycininhaemodialysis patients
Administration and monitoring for toxicity and efficacy
Take first pre-dose level before 4th or 5th DOSE after start of therapy or following a change in
dosing / renal function (whichever is before the morning dose)
Aimfor pre-dose levels of 10-15 mg/L or 15-20mg/L for bone/joint infections, epidural abscess,
If level and renal function stable, repeat levels once weekly
Unless CrCl <25ml/min do not routinely wait for levels before administration of subsequent dose
Adjust dose/frequency of vancomycin using table below
Trough level (mg/L) If target pre-dose = 10-15 action:
>20 Omit one dose and move down one stage in dosing regime
16-20 Move down one stage in dosing regime
10-15 ON TARGET repeat pre-dose level once weekly
<10 Move up one stage in dosing regime
Trough level (mg/L) If target pre-dose = 15-20 action:
>20 Move down one stage in dosing regime
16-20 On Target repeat pre-dose level once weekly
<15 Move up one stage in dosing regime
Intermittent IV infusion in 250 ml sodiumchloride 0.9%or glucose 5%
The infusion must be given at a rate no greater than 10 mg/min to prevent infusion related adverse
effects. 1g must be administered over 100 minutes; 750 mg over 75 minutes; 2g over 200 minutes.
Aminoglycoside - Once Daily Dosing
If the patient has renal impairment, consideration should be given to increasing the interval between doses.
Exclusions: Endocarditis, Pregnancy, Children, Patients with ascites, Major burns patients,
Cystic fibrosis patients.
Dose at 12 noon if possible (Pre-dose level at 9.30am)
Exclusion criteria:
Patients with neutropenic sepsis or immunosuppression
CNS infection (meningitis, encephalitis, brain abscess)
Necrotising fasciitis or severe cellulitis
Endocarditis
Central line infections (line in-situ)
Multi resistant infections
Deep abscess, lung abscess, empyema
Ascending cholangitis
Osteomyelitis, septic arthritis - not absolute exclusions.
Level
(microgram/ml)
<1.0
1.1 to 2.0
2.1 to 3.0
> 3.0
Action
Necessary
Continue with same dose
Reduce dose by 1mg/kg
Omit next dose
Increase dose interval to 48 hours
Stop gentamicin
When to
re-check level
3 days
Next day
Before next dose
Repeat level next day
and seek pharmacy advice
Total duration of antibiotic therapy:
Staphylococcus aureus bacteraemia: 28 days (14 days if removable focus e.g. IV line)
GramNegative Bacteraemia: 10 - 14 days
Total duration of antibiotic therapy:
2 - 6 weeks depending on the type of Endocarditis
Renal function (CrCl) Dosage Regime
>60 ml/min 15 mg/kg* once a day
40-60 ml/min 15 mg/kg* 36 hourly
20-40 ml/min 15 mg/kg* 48 hourly
<20 ml/min Discuss with pharmacy
Amikacin
Bioavailability
Use oral route whenever possible
Ciprofloxacin, Clindamycin, Co-trimoxazole, Levofloxacin, Linezolid, Metronidazole,
Rifampicin, Sodium Fusidate & Fluconazole all have excellent oral bioavailability and have
excellent tissue and cell penetration. Unless patient cannot absorb orally, there is no advantage
using the IV route.
MRSA Eradication Policy
Treatment for colonisation
Treatment protocol for 5 days:
During normal working hours the Infection Prevention and Control Nurses (IPCN) will advise
when decolonisation is applicable, as per Infection Prevention and Control guideline no.12. Out
of hours consult this guideline when required.
There are pre-printed labels available on all wards for decolonisation treatments. These labels
are located in Infection Prevention and Control guideline no.12.
Your 5 moments for hand hygiene
1. Before touching a patient
2. Before Clean / Aseptic procedure
3. After body fluid exposure risk
4. After touching a patient
5. After touching patient surroundings
packs and aseptic technique. Seek assistance fromnursing staff.
Give a stat loading dose of 20mg/kg to a max of 2g at an infusion rate of 10mg/min. i.e. 2g over 200mins.
of Cellulitis
Cellulitis is an infection affecting the skin and subcutaneous fat. It is usually caused
by Streptococcus pyogenes. On occasion it can be caused by other organisms
including Staphylococcus aureus (usually when there is an ulcer or abscess).
Day 1
Day 2
Day 3
Benzylpenicillin Flucloxacillin 1.2g IV QDS + 1g IV QDS
Penicillin allergic: Stable 500mg PO/IV BDor
450mg PO QDS or 600mg IV TDS
Penicillin allergic: Unstable IV (see page 11 for dose)
Clarithromycin
Clindamycin
Vancomycin
Pt Improved?
Pt Improved?
Yes
Yes
No
No
Continue Antibiotic
regimen as above
Continue Antibiotic
regimen as above
1.
2.
3.
4.
Do an MRSA Screen
Increase dose to
2.4g QDS
Stop
Start 600mg IV TDS
Benzylpenicillin
Flucloxacillin
Clindamycin
1.
2.
3.
Discuss with microbiologist
Stop
Start
Benzylpenicillin
Linezolid
+
600mg PO/IV BD
(same bioavailabliity Oral &IV.
On Discharge: needs hi-tech Rx
+contact community pharmacy)
Clindamycin
Note: Clindamycin & Linezolid have same bioavailability oral & IV
- change to oral ASAP
Avoid Clindamycin if previous history of C diff
or if an elderly nursing home patient
(see page 12 for dose)
(see page 12 for dose)
For critically ill patients
If prostate biopsy in
discuss with consultant
previous 2 weeks + signs
microbiologist
of sepsis +
haemodynamically unstable
as for 1st line treatment
(see page 12 for dose)
(see page 11 for dose)
Prosthetic valve
(max 80mg) IV 12-hourly
as for 1st line treatment
Once culture +sensitivity results are available amend antibiotic therapy accordingly.
UTI antibiotic prophylaxis is not recommended.
Its use results in antimicrobial resistance +adverse drug effects
(see page 12 for dose)
endocarditis or ICU patient.
(max 120mg)
Indication
Stop Date
Draw line for
end of course
in addition to
documenting
stop date
Start Smart, Then Focus
An Care Bundle for Hospitals Antibiotic
Day 1: Start Smart... ...then Focus (Day 2 onwards)
1.
2.
3.
4.
Start antibiotics only if there is clinical
evidence of bacterial infection. -If there
is evidence of bacterial infection,
prescribe in accordance with your local
antibiotic guidelines and appropriately
for the individual patient (see notes
below).
Obtain appropriate cultures before
starting antibiotics.
Document in both the drug chart and
medical notes:
- Treatment indication
- Drug name, dose, frequency and route
- Treatment duration (or reviewdate)
Ensure antibiotics are given within four
hours of prescription - within 1 hour for
severe sepsis or neutropenic sepsis.
At 24-48 hours after starting antibiotics,
make an Antimicrobial Prescribing
Decision
- Reviewthe clinical diagnosis
- Reviewlaboratory/radiology results
- Choose one of the five options below
- Document this decision
Options
1.
2.
3.
4.
5.
Stop antibiotics
- no evidence of bacterial infection, or
infection resolved
Switch fromintravenous to oral
antibiotic(s) - if patient meets criteria for
oral switch
Change antibiotic(s)
- narrower spectrum, if possible;
broader spectrum, if indicated
Continue current antibiotic(s)
- reviewagain after further 24 hours
Outpatient parentral antibiotic therapy
- consult with local OPAT team
Whendecidingonthemost appropriateantibiotic(s) to Someantibioticsareconsideredunsafeinpregnancy
prescribe, consider thefollowingfactors: or youngchildren
Historyof drugallergy(document allergytype: Doseadjustment mayberequiredfor renal or
minor [rashonly] or major [anaphylaxisangioedema]) hepaticfailure
Recent cultureresults(e.g. ispatient colonised
Consider removal of anyforeignbody/indwellingdevice,
withamultiple-resistant bacteria?)
drainageof pus, or other surgical intervention
Recent antibiotictreatment
Potential druginteractions For adviceonappropriateinvestigationand
Potential adverseeffects(e.g. C. difficileinfection management of infections, consult your local infection
ismorelikelywithbroadspectrumantibiotics) specialist(s) (microbiologist, infectiousdisease
physicianand/or antimicrobial pharmacist)
Restricted
Antimicrobials
Onlytobeprescribedwithmicrobiology
approval if outsideof guidelines
Quinolones(Ciprofloxacin&Levofloxacin)
SecondgenerationCephalosporinsonmedical wards
ThirdgenerationCephalosporins
Teicoplanin, Vancomycin, Linezolid, Rifampicin
Gentamicin, Amikacin
Meropenem, Ertapenem
Ambisome , Caspofungin
Co-trimoxazole
Aztreonam
ALL antimicrobial
Prescriptions
MUST state:
INDICATION for treatment
DURATION of therapy
PAGE 08 PAGE 09 PAGE 10 PAGE 11 PAGE 12 PAGE 13 PAGE 14
Total course length: 7 - 14 days
Administer antibiotics within 1 hour
Check lactate
(see page 11 for dose)
If prosthetic:
At time of initial prescribing of Vancomycin, Gentamicin, Amikacin
request eGFR from biochemistry lab to calculate initial dose.
Request appropriate pre-level in blood book.
Write stop date.
Seek medical microbiology advice
Você também pode gostar
- Lab ValuesDocumento3 páginasLab Valuesashdmb217100% (49)
- Antibiotic Study Cheat Sheet August 2019Documento1 páginaAntibiotic Study Cheat Sheet August 2019Ryan TurnerAinda não há avaliações
- Medication Cheat Sheet For ClinicalDocumento4 páginasMedication Cheat Sheet For Clinicalanny100% (2)
- Antibiotic Study Cheat Sheet October 2018Documento1 páginaAntibiotic Study Cheat Sheet October 2018Nourhan100% (3)
- ICU Nursing Report SheetDocumento2 páginasICU Nursing Report Sheetthenekoling100% (2)
- Top 300 Drugs Pocket Reference Guide (2021 Edition)No EverandTop 300 Drugs Pocket Reference Guide (2021 Edition)Nota: 5 de 5 estrelas5/5 (1)
- The Mindfulness Workbook For Addiction Sample PagesDocumento30 páginasThe Mindfulness Workbook For Addiction Sample PagesAntonio Navarro100% (6)
- Antibiotics Summary - Flattened PDFDocumento3 páginasAntibiotics Summary - Flattened PDFmicheal1960100% (6)
- Pharmacology Complete Drug TableDocumento6 páginasPharmacology Complete Drug Tableninja-2001100% (4)
- Research Vegetable SiomaiDocumento23 páginasResearch Vegetable SiomaiPas Pas93% (14)
- Central Line Cheat SheetDocumento1 páginaCentral Line Cheat SheetLara Mae100% (1)
- Patho Physiology Bible: Over 70 Concept MapsDocumento139 páginasPatho Physiology Bible: Over 70 Concept Mapslauramphs79100% (5)
- Empirical Prescribing Chart GlasgowDocumento1 páginaEmpirical Prescribing Chart GlasgowHariharan Narendran75% (4)
- Drug Cheat SheetDocumento2 páginasDrug Cheat SheetThomas Hart IIIAinda não há avaliações
- Med Geeks Clinical Lab GuideDocumento17 páginasMed Geeks Clinical Lab GuideHuy Hoang100% (1)
- Med Surg Cheat Sheet 1Documento1 páginaMed Surg Cheat Sheet 1Figmentum FigmentumAinda não há avaliações
- Acid Base Handout (Student)Documento29 páginasAcid Base Handout (Student)Joel Topf100% (8)
- Risk For Diseases Cheat SheetDocumento1 páginaRisk For Diseases Cheat SheetRick Frea100% (5)
- Covid Test-PositiveDocumento2 páginasCovid Test-PositiveSuresh VarmaAinda não há avaliações
- Guidelines For First-Line Empirical Antibiotic Therapy in AdultsDocumento1 páginaGuidelines For First-Line Empirical Antibiotic Therapy in AdultsAnonymous s4yarxAinda não há avaliações
- Pharmacology Drug Chart: Drug Name Receptor Therapeutic Uses Adverse EffectsDocumento18 páginasPharmacology Drug Chart: Drug Name Receptor Therapeutic Uses Adverse EffectsPadmavathy Naidu Chokkapu100% (2)
- Soap TemplateDocumento3 páginasSoap TemplaterohitAinda não há avaliações
- Normal Lab ValuesDocumento3 páginasNormal Lab ValuesHAinda não há avaliações
- Pharm I - Abx ChartDocumento4 páginasPharm I - Abx ChartNicole BerryAinda não há avaliações
- Drug Interactions 2 Paper PDFDocumento2 páginasDrug Interactions 2 Paper PDFAzima AbdelrhamanAinda não há avaliações
- Antiinfectives Drug TableDocumento5 páginasAntiinfectives Drug Tablecdp1587100% (3)
- Admitting OrdersDocumento4 páginasAdmitting OrdersRommel OliverasAinda não há avaliações
- Brain Sheet - Nursing Brain Sheet ExampleDocumento1 páginaBrain Sheet - Nursing Brain Sheet ExampleShari KvidahlAinda não há avaliações
- BED12 - Antibiotics PharmacologyDocumento2 páginasBED12 - Antibiotics PharmacologyAmir AmirulAinda não há avaliações
- Ccu Survival GuideDocumento10 páginasCcu Survival Guideomegasauron0gmailcom100% (1)
- Antibiotics ChartDocumento10 páginasAntibiotics Chartadom09Ainda não há avaliações
- Commonly Used Lab Values at A Glance Chem 7 1Documento9 páginasCommonly Used Lab Values at A Glance Chem 7 1annatw100% (10)
- The Principles of Antibiotic Therapy: S. Aureus Streptococcus PneumoniaeDocumento16 páginasThe Principles of Antibiotic Therapy: S. Aureus Streptococcus PneumoniaeDianne Chua100% (7)
- Anti Infective Drug ChartDocumento1 páginaAnti Infective Drug ChartJessica100% (1)
- Diabetes Medications Chart PDFDocumento1 páginaDiabetes Medications Chart PDFRachel Lalaine Marie SialanaAinda não há avaliações
- Lab Values Flash CardDocumento24 páginasLab Values Flash CardEyySiEffVeeAinda não há avaliações
- Nursing SheetDocumento1 páginaNursing Sheetseaturtles505100% (1)
- Common Medical NotationsDocumento3 páginasCommon Medical NotationssaltarisAinda não há avaliações
- Critical Care Drug Reference SheetDocumento12 páginasCritical Care Drug Reference SheetYanina CoxAinda não há avaliações
- Diabetes Mellitus Drug ChartDocumento3 páginasDiabetes Mellitus Drug Chartlui.stephanie1751100% (1)
- The Intern Pocket Card Surviving GraysDocumento2 páginasThe Intern Pocket Card Surviving GraysKathleen Grace ManiagoAinda não há avaliações
- Lile Bai 1: Area/Site Common Organism Useful Abx Other NotesDocumento3 páginasLile Bai 1: Area/Site Common Organism Useful Abx Other NotesNicole BerryAinda não há avaliações
- Classification of Antibiotics For PrintingDocumento4 páginasClassification of Antibiotics For PrintingMuthu Kumar100% (2)
- Drug ChartDocumento8 páginasDrug Chartstudentalwaysstudy100% (1)
- Blood Gas AnalysisDocumento3 páginasBlood Gas AnalysisChameera Bandara100% (2)
- Cardiology Step 2 CK NotesDocumento5 páginasCardiology Step 2 CK NotesVidur S SinghAinda não há avaliações
- Antibacterial Drugs SummaryDocumento13 páginasAntibacterial Drugs SummaryNeo Ramagaga100% (1)
- Respiratory DrugsDocumento2 páginasRespiratory Drugsmed testAinda não há avaliações
- Antibiotics Chart 1Documento7 páginasAntibiotics Chart 1Vee MendAinda não há avaliações
- Anemia ChartDocumento1 páginaAnemia ChartBetsy Brown ByersmithAinda não há avaliações
- GI Drugs PDFDocumento6 páginasGI Drugs PDFErica Hyeyeon Lee100% (1)
- Fluids and Electrolytes Pathophysiology NursingDocumento16 páginasFluids and Electrolytes Pathophysiology Nursinggrad_nurse_2015100% (3)
- Clinical KardexDocumento2 páginasClinical KardexJackie Frey100% (2)
- Medgeeks: Pharmacology Cheat SheetsDocumento13 páginasMedgeeks: Pharmacology Cheat SheetsJuan Jose CastroAinda não há avaliações
- Overview of by Mechanism 2Documento16 páginasOverview of by Mechanism 2daven100% (1)
- Drugs WorksheetDocumento16 páginasDrugs Worksheetninja-2001Ainda não há avaliações
- C DiffDocumento2 páginasC Difftheseus5Ainda não há avaliações
- Icu Antibiotic GuidelinesDocumento4 páginasIcu Antibiotic GuidelinesTia MonitaAinda não há avaliações
- Antibiotic Policy 2014Documento32 páginasAntibiotic Policy 2014shah007zaadAinda não há avaliações
- Vancomycin & Vancomycin Resistant Enterococci: Abdullah M. Kharbosh, B.SC., PharmDocumento78 páginasVancomycin & Vancomycin Resistant Enterococci: Abdullah M. Kharbosh, B.SC., Pharmkharbosham100% (1)
- NAG Urinary Tract InfectionsDocumento14 páginasNAG Urinary Tract InfectionsJun JimenezAinda não há avaliações
- Was King Tut Murdered?Documento4 páginasWas King Tut Murdered?mauricio760Ainda não há avaliações
- Nursepreneurs Essay by J. BacarisasDocumento17 páginasNursepreneurs Essay by J. BacarisasCris GalendezAinda não há avaliações
- ROICAM7 BookletDocumento99 páginasROICAM7 BookletPopy HalifahAinda não há avaliações
- Tinnitus Today September 1986 Vol 11, No 3Documento8 páginasTinnitus Today September 1986 Vol 11, No 3American Tinnitus AssociationAinda não há avaliações
- Interstitial Cystitis (Painful Bladder Syndrome) - Causes & TreatmentDocumento12 páginasInterstitial Cystitis (Painful Bladder Syndrome) - Causes & TreatmentJimmy GillAinda não há avaliações
- MoH - Uganda RBF Program Hospital Quartely Quality Assessment Tool - Jan 2019Documento31 páginasMoH - Uganda RBF Program Hospital Quartely Quality Assessment Tool - Jan 2019Steven SsemwangaAinda não há avaliações
- TDR Business Plan 2008-2013: Robert RidleyDocumento43 páginasTDR Business Plan 2008-2013: Robert RidleySripal JainAinda não há avaliações
- MSDS Dross AluminiumDocumento18 páginasMSDS Dross AluminiumNurul muzayyanahAinda não há avaliações
- BW Health-5Documento2 páginasBW Health-5Michael JaballasAinda não há avaliações
- Bethesda Thyroid 2017Documento6 páginasBethesda Thyroid 2017Ladipo Temitope AyodejiAinda não há avaliações
- Employee Benefits India PDFDocumento2 páginasEmployee Benefits India PDFshahidki31100% (1)
- Birthday Party - Character SketchesDocumento2 páginasBirthday Party - Character SketchesDhivyaAinda não há avaliações
- Liver UpdateDocumento16 páginasLiver UpdateyaniAinda não há avaliações
- Konika 7045 Service Manual PDFDocumento313 páginasKonika 7045 Service Manual PDFleo visaAinda não há avaliações
- VACCP Template Checklist - SafetyCultureDocumento7 páginasVACCP Template Checklist - SafetyCulturepattysaborio520Ainda não há avaliações
- 27 ASL For Teacher S BookDocumento28 páginas27 ASL For Teacher S BookNur Syazwani KhamisAinda não há avaliações
- Medical Supplies - English VocabularyDocumento4 páginasMedical Supplies - English Vocabularyfatimageraldinep2564Ainda não há avaliações
- Holistic WellnessDocumento541 páginasHolistic WellnessSeba FounderAinda não há avaliações
- C0mponents of A Logic ModelDocumento2 páginasC0mponents of A Logic Modelsameer mohamudallyAinda não há avaliações
- Reflective Journal 1 2 and 3Documento11 páginasReflective Journal 1 2 and 3api-321980896Ainda não há avaliações
- Psychometric Properties of The Consensus Sleep Diary in Those With Insomnia DisorderDocumento19 páginasPsychometric Properties of The Consensus Sleep Diary in Those With Insomnia DisorderMondlTAinda não há avaliações
- Rigging TechniquesDocumento27 páginasRigging TechniquesDeepak ShettyAinda não há avaliações
- 2021 A Guide To The African Human Rights System Celebrating 40 YearsDocumento115 páginas2021 A Guide To The African Human Rights System Celebrating 40 YearsChala Yuye KemerAinda não há avaliações
- Progressive Addition Lens Design and The Short of Stature (Shan-Yu, S.)Documento3 páginasProgressive Addition Lens Design and The Short of Stature (Shan-Yu, S.)Valentina PereaAinda não há avaliações
- Capnography Application in Acute and Critical Care: Tom Ahrens, DNS, RN, CCRN, CS Carrie Sona, MSN, RN, CCRN, CSDocumento10 páginasCapnography Application in Acute and Critical Care: Tom Ahrens, DNS, RN, CCRN, CS Carrie Sona, MSN, RN, CCRN, CSJavier Enrique Barrera PachecoAinda não há avaliações
- BT RA 01 WeldingDocumento6 páginasBT RA 01 Weldingnandha gopalAinda não há avaliações
- Raven Rock - Internal Counterintelligence Program (ICIP)Documento38 páginasRaven Rock - Internal Counterintelligence Program (ICIP)Bill GeerhartAinda não há avaliações