Escolar Documentos
Profissional Documentos
Cultura Documentos
NCP and DS
Enviado por
franzcatchie100%(1)100% acharam este documento útil (1 voto)
636 visualizações6 páginasbsn
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
DOCX, PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentobsn
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
100%(1)100% acharam este documento útil (1 voto)
636 visualizações6 páginasNCP and DS
Enviado por
franzcatchiebsn
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato DOCX, PDF, TXT ou leia online no Scribd
Você está na página 1de 6
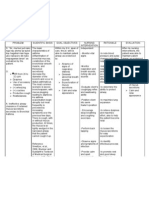
NURSING CARE PLAN: Elevated Blood Pressure
Assessment Nursing Diagnosis Planning Interventions Rationale Evaluation
Subjective:
Mataas po ang
presyon ng dugo ko
kaya ako nahihilo at
madaling
mapagod, as
verbalized by the
patient.
Objective:
BP: 180/100
mmHg
RR: 29 brpm
PR: 85 bpm
Family History of
Hypertension
Decreased urine
output 180 cc
during PM shift
BUN: 9.2
mmol/L
Creatinine:193
umol/L
Easy fatigability
Dizziness
Decreased cardiac
output: increased
blood pressure r/t
increased vascular
pressure secondary
to RAAS activation
Rationale:
Hypertension
damages the kidney
arterioles, causing
them to thicken,
which narrows the
lumen; because the
blood supply to the
kidneys is thereby
reduced, this
increases vascular
volume and
elevation of
peripheral vascular
resistance, the
kidneys will now
secrete more rennin,
which elevates the
pressure even more.
(Tortora, 2008, p.
798)
Short-Term
Goal:
After 2 hours
of nursing
intervention,
the patients
blood
pressure will
lower down
from 180/100
mmHg to
140/80
mmHg.
Long-Term
Goal:
After 8 hours
of nursing
intervention,
the patient will
maintain
blood
pressure of
90-140/60-80
mmHg and
verbalize
understanding
of disease
process and
treatment
regimen.
Independent:
Assessed and
recorded blood
pressure every
hour.
Monitored vital
signs and
notified
physician for
any changes.
Assessed
respiratory
status at least
every 2 hours
and reported
complaints of
dyspnea.
Inspected skin
for pallor,
cyanosis and
temperature.
Assessed
apical and
radial pulse
every 2 to 4
hours.
Reported
complaints of
dizziness and
syncope
promptly.
Provided for
adequate rest
periods.
Provided quiet
and restful
environment.
Maintained
dietary
restrictions,
low-fat, low-
salt, renal diet
as ordered.
Limited fluid
volume to
Provides baseline data
and evaluate response to
treatment and
therapeutic regimen
(Smeltzer; 2008 p.1536).
To monitor patients
hypertensive status
(Doenges; 2002, p.533).
Adventitious breath
sounds or dyspnea may
indicate fluid buildup in
lungs and pulmonary
capillary bed (Sparks and
Taylor; 2008, p.49).
Pallor is indicative of
diminished peripheral
perfusion secondary to
inadequate cardiac
output, vasoconstriction
and anemia. (Sparks and
Taylor; 2008, p. 49)
To monitor for
arrhythmias, impending
cardiac arrest or shock.
(Sparks and Taylor;
2008, p. 657)
May indicate decreased
cerebral blood flow due to
slow carotid sinus reflex
and rhythm disturbance.
(Sparks & Taylor; p. 49)
Conserves energy,
reduces cardiac workload
(Doenges, 2002, p. 65.
Psychological rest helps
reduce emotional stress,
(Doenges, 2002, p.49)
To reduce risk of cardiac
disease. (Sparks and
Taylor; 2008, p. 53)
Restricting fluid intake
can assist in decreasing
Short-Term
Goal:
Partially Met.
After two hours
of nursing
intervention,
patients blood
pressure
lowered down
from 180/100
mmHg to 160/90
mmHg.
Long-Term
Goal:
Goal Met.
After 8 hours of
nursing
intervention, the
patients blood
pressure was
maintained
within normal
limits with blood
pressure of
140/90 mmHg
and verbalized
understanding
of disease
process and
treatment
regimen as
evidenced by
patients
verbalization of:
Naiintindihan
ko na naman po
na kaya
tumataas ang
presyon ko
gawa may sakit
ako sa bato
kaya kailangan
ko sundin yung
payo ng doctor.
1L/day or by
doctors order.
Reinforced the
importance of
adhering to
treatment
regimen.
Dependent:
Administered
Furosemide
40mg via slow
IV push stat as
ordered.
Administered
Losartan
hydrochlorothia
zide 50mg
tablet now then
once a day.
Administered
Catapres
(Clonidine)
75mcg
sublingually
stat then PRN
for BP160/90.
Placed on O2
inhalation via
nasal cannula
regulated at 4
liters per
minute.
circulating volume
thereby decreasing
cardiac workload and
fluid retention (Rodgers;
2007, p. 473).
Lack of cooperation is a
reason for failure of
antihypertensive therapy.
To decrease blood
pressure by promoting
fluid loss and it helps
relieve possible
pulmonary congestion.
For the management of
hypertension.
For immediate treatment
of elevated BP.
Promotes oxygenation
and prevents hypoxia of
body cells.
NOC:
Vital signs
o Extent to which temperature, pulse, respiration, and blood pressure are within normal range
Circulation status
o Unobstructed, unidirectional blood flow at an appropriate pressure through large vessels of the systemic and
pulmonary circuits
Cardiac pump effectiveness
o Adequacy of blood volume ejected from the left ventricle to support systemic perfusion pressure
NIC:
Hemodynamic regulation
o Optimization of heart rate; preload, afterload and contractility
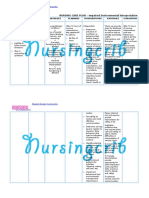
DRUG STUDY: FUROSEMIDE
Drug: Furosemide (Lasix) 40mg IV
Classification: Loop Diuretic
Indication: For the treatment and management of edema and congestion
Mechanism of Action:
Inhibits the reabsorption of sodium and chloride from the loop of Henle and distal renal tubule.
Increase renal excretion of water, sodium, chloride, magnesium, hydrogen and calcium.
Diereses and subsequent mobilization of excess fluid.
Contraindications:
Hypersensitivity
Cross-sensitivity with thiazides and sulfonamides may occur.
Pre-existing electrolyte imbalance, hepatic coma, or anuria
Nursing Considerations:
Assess fluid status during therapy.
Monitor daily weight, intake and output ratio.
Monitor blood pressure and pulse before and during administration.
Assess for allergy to sulfonamides.
Observe the ten rights in giving each medicine by Joyce Kee
DRUG STUDY: FERROUS SULFATE
Drug: Ferrous sulfate 1 capsule OD
Classification: Iron Preparation
Mechanism of Action:
Elevates the serum iron concentration which then helps to form High or trapped in the reticuloendothelial cells for storage and
eventual conversion to a usable form of iron.
Indications:
Prevention and treatment of iron deficiency anemias.
Contraindications:
Hypersensitivity and Severe hypotension.
Adverse Effect:
Dizziness, N & V, Nasal Congestion, Dyspnea, Hypotension, Flushing
Nursing Responsibilities:
Advise patient to take medicine as prescribed.
Caution patient to make position changes slowly to minimize orthostatic hypotension.
Instruct patient to avoid concurrent use of alcohol or OTC medicine without consulting the physician.
Advise patient to consult physician if irregular heartbeat, dyspnea, swelling of hands and feet and hypotension occurs.
Inform patient that angina attacks may occur 30 min. after administration due reflex tachycardia.
DRUG STUDY: LOSARTAN HTCZ
Generic Name: Losartan hydrochlorothiazide
Brand Name: Cozaar
Classification: Cardiovascular agent /Antihypertensive
Mechanism of Action:
Losartan (more specifically, the chemical formed when the liver converts the inactive losartan into an active chemical) blocks the
angiotensin receptor. By blocking the action of angiotensin, losartan dilates blood vessels and thereby reduces blood pressure
Indications:
Used for treating hypertension, left ventricular hypertrophy (increase in muscle) and diabetic nephropathy (kidney disease)
Adverse Reactions and Side Effects:
Diarrhea, muscle cramps, dizziness, insomnia, and nasal congestion. Losartan also may cause a persistent cough, increase
serum potassium, and angioedema
Contraindications:
Hypersensitivity to losartan
Pregnancy[category C (first trimester), category D (second and third trimesters)]
Lactation
Nursing Considerations:
Monitor BP at drug trough (prior to a scheduled dose).
Monitor drug effectiveness when losartan is used as monotherapy.
Inadequate response may be improved by splitting the daily dose into twice-daily dose.
DRUG STUDY: SODIUM BICARBONATE
Generic Name: Sodium Bicarbonate
Brand Name: Rhea Sodium (Oral 325 mg/tab 2 tabs QID)
Classification: Antacids, Antireflux Agents & Antiulcerants
Mechanism of Action:
Neutralizes gastric acid and decreases pepsin activity
Indications:Hyperacidity, Peptic ulcer, Hyperkalemia, Reflux esophagitis
Adverse Reactions and Side Effects:
Fluid and GI: Gastric distention, belching, flatulence.
Metabolic: alkalosis, hypernatremia, hypokalemia, hyperosmolarity
Contraindications:
Patients with alkalosis; Patients taking diuretics known to produce hypochloremia alkalosis; and patients with hypocalcemia. Oral
sodium bicarbonate is contraindicated in patients with acute ingestion of strong mineral acids.
Nursing Considerations:
Monitor urinary pH, calcium, electrolytes and phosphate levels.
Record amount and consistency of stools.
Clients on low-sodium diets should evaluate sodium contents of antacids.
DRUG STUDY: CEFUROXIME
Drug Name: Cefuroxime IV 750mg q6
Classification: Antiinfective; Antibiotic; Second-generation Cephalosporin
Indications: Treatment of penicillinase-producing Neisseria gonorrhoea (PPNG). Effectively treats bone and joint infections,
bronchitis, meningitis, gonorrhea, otitis media, lower respiratory tract infections, skin and soft tissue infections, urinary tract
infections, and is used for surgical prophylaxis
Adverse Reactions and Side Effects:
Body as a Whole: Thrombophlebitis (IV site); pain, burning, cellulitis (IM site); superinfections, positive Coombs' test.
GI: Diarrhea, nausea, antibiotic-associated colitis.
Skin: Rash, pruritus, urticaria.
Urogenital: Increased serum creatinine and BUN, decreased creatinine clearance.
Contraindications:
Hypersensitivity to cephalosporins and related antibiotics;
Pregnancy (category B),
Lactation.
Nursing Considerations:
Determine history of hypersensitivity reactions to cephalosporins, penicillins, and history of allergies, particularly to
drugs, before therapy is initiated.
Inspect IM and IV injection sites frequently for signs of phlebitis.
Report onset of loose stools or diarrhea.
Monitor I&O rates and pattern: Especially important in severely ill patients receiving high doses.
Report any significant changes.
DRUG STUDY: RANITIDINE
Generic: Ranitidine IV 50mg OD
Brand: Zantac
Classification: Anti-ulcer
Mechanism of Action:
Inhibits the action of histamine at the H2 receptor site located primarily in gastric parietal cells, resulting in inhibition of
gastric acid secretion.
Has some antibacterial action against H. pylori
Indications:
Treatment and prevention of heartburn, acid indigestion, and sour stomach.
Prophylaxis of GI hemorrhage from stress ulceration
Contraindications:
Pregnancy
Lactation (excreted in breast milk)
Geriatric patients (more susceptible to adverse CNS reactions)
Renal impairments
Cirrhosis
Adverse Reactions or Side Effects:
Hypersensitivity, Cross-sensitivity may occur; some oral liquids contain alcohol and should be avoided in patients with known
intolerance
Nursing Considerations:
Instruct patient not to take new medication w/o consulting physician
Instruct patient to take as directed and do not increase dose
Allow 1 hour between any other antacid and ranitidine
Avoid excessive alcohol
Assess patient for epigastric or abdominal pain and frank or occult blood in the stool, emesis, or gastric aspirate
Nurse should know that it may cause false-positive results for urine protein; test with sulfosalicylic acid
Inform patient that it may cause drowsiness or dizziness
Inform patient that increased fluid and fiber intake may minimize constipation
Advise patient to report onset of black, tarry stools; fever, sore throat; diarrhea; dizziness; rash; confusion; or
hallucinations to health car professional promptly
Inform patient that medication may temporarily cause stools and tongue to appear gray black
Instruct patients to monitor for and report occurrence of drug-induced adverse reaction
DRUG STUDY: CLONIDINE
Name of Drug: Clonidine (Catapres) 75 mcg tab OD
Classification: Centrally- acting drugs, Antihypertensive
Mechanism of Action:
Stimulates Central alpha-adrenergic receptors to inhibit sympathetic cardio accelerator and vasoconstrictor centers.
Indications: Management of all grades of hypertension.
Contraindications:
Hypersensitivity to clonidine and Sick sinus syndrome
Side Effects/Adverse Reactions:
Local skin irritation, allergic contact dermatitis, hypopigmentation and hyperpigmentation of the skin. Constipation, depression,
anxiety, fatigue, nausea, anorexia, parotid pain, sleep disturbances, impotence, urinary retention, itching sensation of the eye.
Nursing Considerations:
Assess blood pressure and apical pulse before initial dose. If systolic blood pressure is <90 mmhg or pulse is <60 bpm,
with hold drug and notify physician.
Check for edema in feet, legs daily,
Monitor input-output ratio: check for decreasing output.
Note allergic reactions: fever, rash, pruritus, urticaria, and edema.
DRUG STUDY: COMBIVENT
Generic Name: Ipratropium Bromide- Salbutamol Sulfate (Combivent)
Dosage: 1 nebule
Route: via nebulization
Frequency: q6
Pharmacologic action:
Combivent Inhalation Solution is a combination of the anticholinergic bronchodilator, ipratropium bromide, and the beta2-
adrenergic bronchodilator, salbutamol sulfate. Ipratropium bromide is a quaternary ammonium derivative of atropine and is an
anticholinergic drug which has bronchodilator properties. Salbutamol produces bronchodilation through stimulation of beta2-
adrenergic receptors in bronchial smooth muscle, thereby causing relaxation of muscle fibres. This action is manifested by an
increase in pulmonary function as demonstrated by spirometric measurements.
Indications:
For the management of bronchospasm in patients suffering from chronic obstructive pulmonary disease (COPD) who requires
regular treatment with both ipratropium and salbutamol.
Contraindications:
Patients with cardiac tachyarrhythmias, hypertrophic obstructive cardiomyopathy and patients with a history of hypersensitivity to
any of its components or to atropine or its derivatives.
Adverse Effects of the Drug:
Fatigue, abdominal pain, hypertension, dyspepsia, tachycardia, sinusitis, dysuria, blurred vision, taste perversion, dry mouth,
paradoxical bronchospasm, gastrointestinal distress, vomiting, diarrhea, edema, constipation and urinary difficulty
Nursing Responsibilities/ Precautions:
Monitor respiratory status; auscultate lungs before and after inhalation
Report treatment failure (exacerbation of respiratory symptoms) to physician
Do not allow the solution/ mist to enter the eyes
Consult a doctor immediately in the event of acute, rapidly worsening dyspnea. In addition, the patient should be
warned to seek medical advice should a reduced response become apparent.
The concomitant use of Combivent with other sympathomimetic agents is not recommended since such combined
use may lead to deleterious cardiovascular effects.
Eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from conjunctival
and corneal congestion may be signs of acute narrow-angle glaucoma. Should any combination of these symptoms
develop, treatment with miotic drops should be initiated and specialist advice sought immediately.
Allow 30-60 sec between puffs for optimum results.
Wait 5 min between this and other inhaled medications.
Rinse mouth after medication puffs to reduce bitter taste.
Você também pode gostar
- NCP Ineffective Cardiopulmonary PerfusionDocumento3 páginasNCP Ineffective Cardiopulmonary PerfusionjamiemapanaoAinda não há avaliações
- Aminogen Drug StudyDocumento2 páginasAminogen Drug Studymilesmin100% (1)
- 13 Areas of AssessmentDocumento10 páginas13 Areas of Assessmentobietobi50% (2)
- Nursing Care Plan for Hypertension and Knee PainDocumento3 páginasNursing Care Plan for Hypertension and Knee PainEzron Kendrick Duran50% (2)
- Actual NCPDocumento2 páginasActual NCPbaki0146Ainda não há avaliações
- NCP DiarrheaDocumento2 páginasNCP DiarrheaBracel GarciaAinda não há avaliações
- NCP Activity Intolerance Related To Decreased in Oxygen SupplyDocumento3 páginasNCP Activity Intolerance Related To Decreased in Oxygen SupplyKyle Stephen TancioAinda não há avaliações
- NCP 1Documento1 páginaNCP 1hsiriaAinda não há avaliações
- NafarinDocumento2 páginasNafarinianecunar100% (2)
- Managing hypertension with bisoprololDocumento2 páginasManaging hypertension with bisoprololNovi YulianaAinda não há avaliações
- Drug StudyDocumento8 páginasDrug StudyzenAinda não há avaliações
- Case Study: Gastrointestinal System of Older People Case Scenario: LapayDocumento1 páginaCase Study: Gastrointestinal System of Older People Case Scenario: LapayAriaAinda não há avaliações
- Risk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.Documento2 páginasRisk For Aspiration Related To Esophageal Compromise Affecting The Lower Esophageal Sphincter As Evidenced by Heart Burn.eleinsamAinda não há avaliações
- NCP For CHF 3 Activity IntoleranceDocumento2 páginasNCP For CHF 3 Activity IntoleranceAngelyn ArdinesAinda não há avaliações
- SNU49Documento2 páginasSNU49Nora BacolAinda não há avaliações
- Pedia Care Study - Appendix B - Drug StudyDocumento8 páginasPedia Care Study - Appendix B - Drug Studyryan100% (1)
- Impaired Tissue Perfusion Related To The Weakening / Decreased Blood Flow To The Area of Gangrene Due To Obstruction of Blood VesselsDocumento3 páginasImpaired Tissue Perfusion Related To The Weakening / Decreased Blood Flow To The Area of Gangrene Due To Obstruction of Blood VesselsKat AlaAinda não há avaliações
- "Nagtatae Siya 4 Days Na" As Verbalized by The Mother. Inatake of Causative Agents Irritation of The Stomach Inflammation of The Stomach Increase GI Motility DiarrrheaDocumento4 páginas"Nagtatae Siya 4 Days Na" As Verbalized by The Mother. Inatake of Causative Agents Irritation of The Stomach Inflammation of The Stomach Increase GI Motility DiarrrheaMelissa MhelAinda não há avaliações
- Nursing Care PlanDocumento11 páginasNursing Care Planaycee0316100% (1)
- Nursing Care Plan for Rheumatoid ArthritisDocumento3 páginasNursing Care Plan for Rheumatoid ArthritisJashAnia MarIe EvArdo FloresAinda não há avaliações
- BSN 3e Duropan Ncp-Knowledge DeficitDocumento12 páginasBSN 3e Duropan Ncp-Knowledge DeficitJane DuropanAinda não há avaliações
- NCP & Discharge PlanningDocumento12 páginasNCP & Discharge PlanningStephanie Mae Amoylen OdchigueAinda não há avaliações
- NCP RiskDocumento3 páginasNCP RiskMaricar Azolae MascualAinda não há avaliações
- Week 10 Drug Card - Hydrochlorothiazide (HCTZ)Documento2 páginasWeek 10 Drug Card - Hydrochlorothiazide (HCTZ)RCurry09Ainda não há avaliações
- Decrease Cardiac OutputDocumento6 páginasDecrease Cardiac OutputGerardeanne ReposarAinda não há avaliações
- Drug StudyDocumento2 páginasDrug StudyLorina Lynne ApelacioAinda não há avaliações
- Hypertension NCPDocumento1 páginaHypertension NCPj4royce100% (1)
- Patient Risk for Self-Directed ViolenceDocumento2 páginasPatient Risk for Self-Directed ViolenceGrape JuiceAinda não há avaliações
- Ncp'sDocumento8 páginasNcp'sDuchess Kleine RafananAinda não há avaliações
- This Study Resource Was: AssignmentDocumento2 páginasThis Study Resource Was: AssignmentJOEY MEAD ARUGAYAinda não há avaliações
- Ineffective Airway ClearanceDocumento1 páginaIneffective Airway ClearancejomerdalonaAinda não há avaliações
- Drug StudyDocumento18 páginasDrug StudyAntonethe DemdamAinda não há avaliações
- Drug Study MMMCDocumento14 páginasDrug Study MMMCKathleen Pagulayan Intalan-GloriosoAinda não há avaliações
- Nursing Care Plan For Impaired Environmental Interpretaion NCPDocumento4 páginasNursing Care Plan For Impaired Environmental Interpretaion NCPderic100% (2)
- NCP - FeverDocumento2 páginasNCP - FeverJoeven HilarioAinda não há avaliações
- Ineffective Airway ClearanceDocumento2 páginasIneffective Airway ClearancePatrick Arvin Ballesteros BarcarseAinda não há avaliações
- NCP Systemic Viral Infection SVIDocumento4 páginasNCP Systemic Viral Infection SVIPavel Kolesnikov100% (1)
- Nursing care plan for cardiomyopathyDocumento7 páginasNursing care plan for cardiomyopathyKym RonquilloAinda não há avaliações
- Critical Thinking ExerciseDocumento1 páginaCritical Thinking ExerciseMaye ArugayAinda não há avaliações
- Emj Cases : Questions For Case 1Documento8 páginasEmj Cases : Questions For Case 1Azmyza Azmy100% (1)
- SLCN Gazette Magazine, Volume 1, Issue 1, 2019Documento20 páginasSLCN Gazette Magazine, Volume 1, Issue 1, 2019Mayzelle RizAinda não há avaliações
- ANDAYA, Kristine Alexis L. BSN218 Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocumento3 páginasANDAYA, Kristine Alexis L. BSN218 Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAlexis TineAinda não há avaliações
- ASPIRIN Drug Study ERDocumento1 páginaASPIRIN Drug Study ERMargueretti Delos ReyesAinda não há avaliações
- Acute Pain NCPDocumento1 páginaAcute Pain NCPJed AvesAinda não há avaliações
- Afinidad, Jiezl A: Davao Doctors College Nursing ProgramDocumento4 páginasAfinidad, Jiezl A: Davao Doctors College Nursing ProgramJiezl Abellano AfinidadAinda não há avaliações
- Drug StudyDocumento9 páginasDrug StudyJonica CamposAinda não há avaliações
- Impaired Urinary EliminationDocumento3 páginasImpaired Urinary EliminationAgcopra MtchAinda não há avaliações
- 13 Areas of AssessmentDocumento6 páginas13 Areas of Assessmentdanna christine g. paguntalanAinda não há avaliações
- NCP DobDocumento3 páginasNCP DobLester BuhayAinda não há avaliações
- Nursing Care PlanDocumento3 páginasNursing Care Planjnx_anonymousAinda não há avaliações
- NCP - Hyperthermia - FEUNRMFDocumento5 páginasNCP - Hyperthermia - FEUNRMFJk SalvadorAinda não há avaliações
- Renea Joy Arruejo - Activity For LectureDocumento2 páginasRenea Joy Arruejo - Activity For LectureRenea Joy Arruejo100% (1)
- Hypertension: Pathophysiology, Diagnostic Test, Medical Management, and Nursing Care PlanDocumento12 páginasHypertension: Pathophysiology, Diagnostic Test, Medical Management, and Nursing Care PlanMaulidyaFadilahAinda não há avaliações
- Drug StudyDocumento8 páginasDrug StudyJheryck SabadaoAinda não há avaliações
- Drug Indication Action Side Effects and Adverse Reaction Nursing ConsiderationDocumento8 páginasDrug Indication Action Side Effects and Adverse Reaction Nursing Considerationkier khierAinda não há avaliações
- CHF Simulation PreparationDocumento5 páginasCHF Simulation Preparation5Dragoon5Ainda não há avaliações
- Hypertensive CrisisDocumento7 páginasHypertensive Crisisalul847474Ainda não há avaliações
- DBP: Diastolic Blood Pressure SBP: Systolic Blood PressureDocumento7 páginasDBP: Diastolic Blood Pressure SBP: Systolic Blood PressureM. JoyceAinda não há avaliações
- 3 Drugs Study Updates Issues HemodialysisDocumento7 páginas3 Drugs Study Updates Issues HemodialysisKim GalamgamAinda não há avaliações
- Drug StudyDocumento2 páginasDrug StudyAjay SupanAinda não há avaliações
- Diabetes and Pregnancy Review ArticleDocumento9 páginasDiabetes and Pregnancy Review ArticleGabyliz Gonzalez CastilloAinda não há avaliações
- Rodriguez - Diagnostico Clinico Del Autista PDFDocumento6 páginasRodriguez - Diagnostico Clinico Del Autista PDFLuz Dianeth ZapataAinda não há avaliações
- Patofisiologi BPHDocumento31 páginasPatofisiologi BPHHendry Cleodora RomeoAinda não há avaliações
- Association of Serum Uric Acid Level with Coronary Artery DiseaseDocumento25 páginasAssociation of Serum Uric Acid Level with Coronary Artery Diseasedr.jkAinda não há avaliações
- The Natural History of Human Papillomavirus InfectionDocumento12 páginasThe Natural History of Human Papillomavirus InfectionValentina GarciaAinda não há avaliações
- Et Antiparalytic IJNRD2202025Documento13 páginasEt Antiparalytic IJNRD2202025GOMTIAinda não há avaliações
- REVIEW Cell Adaptation, Injury and DeathDocumento101 páginasREVIEW Cell Adaptation, Injury and DeathandiariansyahAinda não há avaliações
- Typhoid Fever: By, Arathy DarvinDocumento35 páginasTyphoid Fever: By, Arathy DarvinJaina JoseAinda não há avaliações
- .Au Files Dysbiosis ScoreDocumento2 páginas.Au Files Dysbiosis ScorekenetmartinAinda não há avaliações
- Characteristics of hospitalized liver cirrhosis patients in Medan Haji Hospital 2016-2018Documento10 páginasCharacteristics of hospitalized liver cirrhosis patients in Medan Haji Hospital 2016-2018Jamilah Sinaga100% (1)
- Tugas Bahasa Inggris "Roleplay Ambulation": OlehDocumento3 páginasTugas Bahasa Inggris "Roleplay Ambulation": Olehnono NonoAinda não há avaliações
- Health Assessment 21Documento4 páginasHealth Assessment 21shannon c. lewisAinda não há avaliações
- Feline Scabies, Case Report Pramodh Bernard 17BVM89Documento10 páginasFeline Scabies, Case Report Pramodh Bernard 17BVM89pramodh bernardAinda não há avaliações
- Pott DiseaseDocumento36 páginasPott DiseaseGiovanna Algu100% (1)
- DUTY SDH + CKDDocumento6 páginasDUTY SDH + CKDadelia putri wirandaniAinda não há avaliações
- Management For PancreatolithiasisDocumento13 páginasManagement For PancreatolithiasisAhmad Fakhrozi HelmiAinda não há avaliações
- Medication SheetDocumento4 páginasMedication SheetJasleen AilenAinda não há avaliações
- 3.4 Balroga - Kaumarbhritya (Ayurvedic Pediatrics)Documento4 páginas3.4 Balroga - Kaumarbhritya (Ayurvedic Pediatrics)Dr Thushar T.SAinda não há avaliações
- Adime Note Allison 2Documento3 páginasAdime Note Allison 2api-457873289Ainda não há avaliações
- Overview of The Evaluation of Stroke - UpToDateDocumento57 páginasOverview of The Evaluation of Stroke - UpToDateclarissa suryaAinda não há avaliações
- Unit-6 New Born IgnouDocumento26 páginasUnit-6 New Born IgnouVijay MgAinda não há avaliações
- Ketoasidosis DiabetikDocumento6 páginasKetoasidosis DiabetikSahril RamadhanAinda não há avaliações
- Ultraformer Flyer Proof PDFDocumento2 páginasUltraformer Flyer Proof PDFreception7122Ainda não há avaliações
- Case StudyDocumento5 páginasCase StudyJhosua RoldanAinda não há avaliações
- PE and HealthDocumento3 páginasPE and HealthRia Ellaine Cornelio LachicaAinda não há avaliações
- Tog 12685Documento3 páginasTog 12685saeed hasan saeedAinda não há avaliações
- Extubation Criteria FinalizedDocumento12 páginasExtubation Criteria FinalizedaryamanishAinda não há avaliações
- Final NCP PediaDocumento2 páginasFinal NCP PediaKuro HanabusaAinda não há avaliações
- Colette Scrimger StatementDocumento2 páginasColette Scrimger StatementWWMTAinda não há avaliações
- ASALEXU-Volume 25-Issue 3 - Page 115-127Documento13 páginasASALEXU-Volume 25-Issue 3 - Page 115-127asmaa elnabawy1Ainda não há avaliações