Escolar Documentos
Profissional Documentos
Cultura Documentos
tmpC73A TMP
Enviado por
FrontiersDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
tmpC73A TMP
Enviado por
FrontiersDireitos autorais:
Formatos disponíveis
1 3
International Ophthalmology
The International Journal of Clinical
Ophthalmology and Visual Sciences
ISSN 0165-5701
Int Ophthalmol
DOI 10.1007/s10792-013-9797-4
The study of etiological and demographic
characteristics of pterygium recurrence: a
consecutive case series study from Pakistan
P.Salim Mahar & Nabeel Manzar
1 3
Your article is protected by copyright and all
rights are held exclusively by Springer Science
+Business Media Dordrecht. This e-offprint
is for personal use only and shall not be self-
archived in electronic repositories. If you wish
to self-archive your article, please use the
accepted manuscript version for posting on
your own website. You may further deposit
the accepted manuscript version in any
repository, provided it is only made publicly
available 12 months after official publication
or later and provided acknowledgement is
given to the original source of publication
and a link is inserted to the published article
on Springer's website. The link must be
accompanied by the following text: "The final
publication is available at link.springer.com.
ORI GI NAL ARTI CLE
The study of etiological and demographic characteristics
of pterygium recurrence: a consecutive case series study
from Pakistan
P. Salim Mahar
Nabeel Manzar
Received: 5 June 2011 / Accepted: 13 February 2013
Springer Science+Business Media Dordrecht 2013
Abstract To determine the agents of recurrence, the
demographic features, and the management and out-
comes of pterygium cases treated at Aga Khan Univer-
sity Hospital (AKUH), Karachi. This hospital-based
descriptive study included 147 patients with pterygium
(147 eyes) from both sexes, who presented at the
Ophthalmology Department at AKUH between January
1, 2002 and December 31, 2010. Data regarding their
demographic prole and other factors were collected in a
well-structured proforma. Data were analyzed using
frequencies, proportions, group means, standard devia-
tions, and Pearsons chi squared test. The male to female
ratio in our study was 2:1, with factors such as younger
age (\50 years) at presentation(P = 0.04, Pearsons chi
squared test) and the presence of secondary pterygium
(P = 0.050) correlated signicantly with the recurrence
of pterygium. There was a denite trend of decreased
recurrence seen with lower grade of pterygium
(P = 0.06). The recurrence rate in our study was
8.8 %. These results suggest that a younger age coupled
with a higher grade of pterygium as well as a history of
multiple recurrences leads to increased susceptibility of
recurrence after surgical excision. Early diagnosis and
appropriate management will lead to a better prognosis.
Keywords Pterygium Recurrence Pterygium
grade Etiologic factors Age
Introduction
Pterygium is one of the most common conjunctival
surface degenerative disorders [13]. This brovas-
cular expansion of bulbar conjunctiva over the limbus
leads to chronic irritation, impaired cosmesis, irregu-
lar astigmatism and decreased vision secondary to the
development of pupillary axis blockage by the
increased growth [2]. A number of different surgical
approaches have been proposed for the treatment of
pterygium. The most common method has been the
bare scleral excision technique, rst described by
DOmbrain [4]. However, the major limitation to
simple excision is the high rate of postoperative
recurrence [5]. Therefore adjunctive therapies have
been advocated along with excision to varying levels
of success during the last three decades. A relatively
new method being used, but relatively less in devel-
oping countries, is the conjunctival autograft method.
The recurrence rates are comparable between the two
techniques (239 %) [6, 7]. However, the widely used
method to date is the use of topical mitomycin
C(MMC) as an adjunct therapy to the bare sclera
P. S. Mahar
Section of Ophthalmology, Department of Surgery,
Aga Khan University Hospital, Stadium Road,
Karachi 74800, Pakistan
e-mail: salim.mahar@aku.edu
N. Manzar (&)
Dow University of Health Sciences, Karachi, Pakistan
e-mail: nmanzar2003@hotmail.com
1 3
Int Ophthalmol
DOI 10.1007/s10792-013-9797-4
Author's personal copy
technique to prevent pterygium recurrence. It was rst
introduced by Kunitomo and Mori [8] of Japan and its
subsequent usage in the USA by Singh et al. [9] led to
its widespread use in Asia.
Since its inception, MMChas been used successfully
for treating various ocular disorders ranging from
pterygium to glaucoma [10, 11]. MMC was rst
developed in 1955 from Streptomyces caespitosus by
Hata et al. [12]. Since then much data and research
about pterygiumtreatment with MMCis available from
developed countries; however, there is a paucity of data
with regards to the etiology and demographics of
pterygium recurrence from developing countries such
as Pakistan because there is neither a national database
nor anyrelevant authoritythat follows recurrence cases.
A number of research studies have been carried out to
document the appropriate dosage and efcacy of MMC
in treating pterygium and preventing its recurrence.
However, relatively fewstudies have evaluated the role
of other factors such as age, gender, MMC exposure
time, as well as the size and extent of pterygium
encroaching on the cornea [1315], especially in the
context of the local population of Asia where there is
high prevalence of pterygium. The magnitude of the
problem, as well as signicant ocular morbidity and the
cost of the recurrent treatment expenditure incurred by
the state, motivated us to carry out our research. Factors
such as age, gender, type of pterygium, presenting
grade of pterygium, treatment, and outcome in terms of
recurrence of pterygium were taken into consideration.
The main purpose of our study was to determine the
agents of recurrence, the demographic features, the
management and outcomes of pterygium cases treated
at Aga Khan University Hospital (AKUH), Karachi and
to examine the factors associated with it.
Methods
This hospital-based retrospective, case series study was
carried out in the Ophthalmology Department, AKUH,
Karachi, Pakistan. Patient data les were analyzed
starting from January 1, 2002 to December 31, 2010.
One hundred and forty-seven patients (147 eyes)
diagnosed with pterygium and who fullled the inclu-
sion criteria were included in the study. The study
protocol was reviewed and approved by the ethics
committee at the study center (AKUH Ethical Review
Board), and the study was carriedout inaccordance with
the declaration of Helsinki of 1975, revised in 1983.
Patients fullling the following study criteria were
enrolled in the study:
Participants of all ages and gender as determined by
the completed proforma with established diagnosis
of unilateral progressive pterygia of different grades;
Surgical excision by the same surgeon (PSM)
using bare scleral technique along with topical
MMC administration with a minimum follow-up
period of 24 months; and
Informed consent from subjects or family for
participating in the study.
Patients with the following conditions were
excluded from the study:
Any suspicious growth other than pterygia and
corneal scarring;
Undergone pterygium excision by any other tech-
nique; or
Lost-to-follow-up during the study period.
The study was carried out in two parts. First, patient
data including detailed medical history along with
complete ocular examination were collected on a well-
structured proforma. This included best-corrected
visual acuity (BCVA), bio-microscopic examination
of anterior segment with Goldman applanation to-
nometery and fundus examination with ?90 DS lens.
This was followed by extraction of data regarding
social and demographic characteristics from the
patient archives. Pterygia were classied either as
primary or secondary (recurrent) pterygium on the
basis of rst-time episode or recurrence, respectively.
Pterygia were graded depending on the extent of
corneal involvement [3] by the principal investigator
(PSM) preoperatively to minimize any bias due to
inter-rater variability.
Grade 1, between limbus and a point midway
between limbus and pupillary margin;
Grade 2, head of the pterygium reaching the
pupillary margin (nasal papillary margin in case of
nasal pterygium and temporal margin in case of
temporal pterygium), and
Grade 3, crossing the pupillary margin.
Pterygium excisions were performed on an outpa-
tient basis by the same surgeon (PSM) using the same
Int Ophthalmol
1 3
Author's personal copy
technique [16]. After excision using the bare scleral
technique under topical anesthesia (Proparacaine;
Alcon, Belgium), a sterile sponge (5 9 5 mm) soaked
in 810 drops of 0.2 mg/ml MMC (0.02 %) (mitomy-
cin-C; Kyowa, Japan) was applied over the corneo-
sclera and the area from where pterygium was excised
for a xed duration of 3 min. The sponge was removed
and the eye was irrigated with 20 ml of normal saline
0.9 %. This was followed by topical administration of
dexamethasone 0.1 % plus tobramycin 0.3 % (Tobra-
dex; Alcon, Belgium) and hydroxypropyl methylcel-
lulose (Tear Naturale II; Alcon, Belgium) four times a
day for 4 weeks. The dosage of MMC was calculated
in accordance with the international recommendations
[1719]. Patients were regularly followed up at
intervals of 3 months after the procedure for a
minimum period of 24 months. Any adverse effect
or physical ndings were noted on each visit. Recur-
rence of pterygium was dened as an encroachment of
brovascular connective tissue across the limbus and
onto the cornea for any distance in the position of the
previous lesion.
Classication of subjects was performed according
to age, gender, as well as site, type and grading of the
pterygium. Subjects were divided into two age
groups(1) B50 years and (2) [50 years. The poten-
tial factors were also classied accordingly (Table 1).
Data were entered in SPSS version 16. The results were
evaluated using frequencies, proportions, group means,
standard deviation and Pearsons chi squared test. A
P value of B0.05 was considered signicant.
Results
Atotal of 147 patients (147 eyes) based on our inclusion
criteria were enrolled in the study and were followed for
a minimum of 24 months (mean 38.6 months; range
2460 months). Twenty-six patients (in addition to the
147 patients) who were lost-to-follow-up during the
study period were excluded from the study; these cases
were similar to the study participants in terms of age,
gender and size of pterygium but their inclusion could
have biased the results so they were excluded. Ninety-
nine males and 48 females (male to female ratio 2:1)
aged between 16 and 90 years (mean SD
46.4 1.23 years) were included in the study. Primary
pterygium was present in 120 patients while secondary
pterygium was diagnosed in 27 patients. One hundred
and two eyes (69.4 %) were affected by grade 1
pterygium, 24 eyes (16.3 %) had grade 2, and 21 eyes
(14.3 %) had grade 3. In 129 eyes (87.7 %), pterygium
was located on the nasal side, in 16 eyes (10.9 %) it was
located on the temporal side, and two eyes (1.4 %) were
affected on both sides. Out of 147 eyes with pterygium,
66 were affected on the right eye and 81 on the left eye.
Baseline characteristics of patients are shown inTable 1.
The recurrence of pterygium was seen in 13 patients
(8.8 %) after a meantime of 6.77 months (SD9.38). Out
of 13 recurrences, 12 were in the \50 years age group
(P = 0.04, Pearsons chi squared test). Similarly, there
was a higher tendency of recurrence in males (10.1 %)
as compared to females (6.2 %) although this was not
signicant (P = 0.547). Most of the recurrences were
seen on the nasal side (9.3 %) while 6.3 % of pterygia
recurred on both sides (P = 1.00) Table 2.
In the group with recurrent pterygia, the recurrence
rate was greater (18.5 %) than in the group with primary
pterygium (6.7 %) (P = 0.050) with a mean (SD) time
of 3.20 (2.38) months as compared to 9.00 (11.54)
months. Adenite trend of recurrence was also noted on
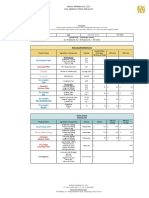
Table 1 Potential risk factors in pterygium recurrence
Variable Recurrence N (%) P value
a
Yes No
Age (years)
Mean SD 46.4 1.23 0.04
\50 12 (13.5) 77 (86.5)
[50 1 (1.7) 57 (98.3)
Gender
Male 10 (10.1) 89 (89.9) 0.54
Female 3 (6.2) 45 (93.8)
Type of pterygium
Primary 8 (6.7) 112 (93.3) 0.05
Recurrent 5 (18.5) 22 (81.5)
Grading of pterygium
1 6 (5.9) 96 (94.1) 0.06
2 5 (20.8) 19 (79.2)
3 2 (9.5) 19 (90.5)
Pterygium location
Nasal 12 (9.3) 117 (90.7) 1.00
Central 1 (6.2) 15 (93.8)
Temporal 0 (00) 2 (100)
N number of subjects, SD standard deviation
a
Pearsons chi squared test
Int Ophthalmol
1 3
Author's personal copy
further stratication of the subjects on the basis of
corneal involvement, with a higher rate of recurrence
seen in subjects with higher grades of corneal involve-
ment (P = 0.067). Similarly, when subjects with
primary pterygia were graded, there was a highly
signicant recurrence seen with higher grades of ptery-
gium (P = 0.008); however, the same was not seen in
participants with secondary pterygia (P = 0.334). The
role of pterygium grading in recurrence of pterygia is
shown in Table 3.
Corneal nebular opacity was a frequent nding,
being seen in seven patients (4.76 %) postoperatively
with only one patient developing a conjunctival cyst at
the site of excision.
Discussion
Pterygium remains an important health care issue in
patients globally [1] but especially in tropical and
Asian countries like Pakistan due to its hot and dusty
weather with high sun exposure. Bare surgical
removal of pterygium results in its high recurrence.
This is the reason that various adjunctive therapies
such as intraoperative topical application of MMC and
conjunctival autograft have been advocated to
increase the success rate of surgical outcome. The
present study was motivated by the invariably high
recurrence of pterygium not only in Pakistan but
worldwide [5, 20].
The recurrence rate of pterygium in the present
study was 8.8 %. In a recent clinical trial carried out in
the Pakistani population, Rahman et al. [21] estimated
a recurrence rate of 10 %. In another prospective
study, Cheng et al. [22] observed a recurrence rate of
7.9 % in subjects with primary pterygia and a
recurrence rate of 19.2 % in subjects with recurrent
pterygia. In a study carried out by Narsani et al. [23], a
recurrence rate of 6.97 %was seen in primary pterygia
patients who underwent conjunctival autograft as
compared to 16.13 % in patients treated by intraop-
erative MMC. In contrast, Frucht-pery et al. [24]
reported a recurrence rate of 6.6 % with intraoperative
MMC as compared to 13.3 % in the conjunctival
autograft group. In another study carried out by the
author (PSM), a recurrence rate of 25.9 % was seen in
the conjunctival autograft group as compared to 9.4 %
in the topical MMC group. Hence, the authors
preference for MMC-based treatment for patients is
based on his own experience [25].
However, comparisons between our study and
others are likely to relate to different study popula-
tions, settings and criteria used for grading. Age was
Table 2 Baseline characteristics of patients
Characteristics of
patients
No. of patients
(N = 147)
Frequency
Sex
Male 99 67.3
Female 48 32.7
Affected eye
Right 66 44.9
Left 81 55.1
Grading of pterygium
a
Primary 120 81.6
1 85 70.8
2 21 17.5
3 14 11.7
Recurrent 27 18.4
1 17 63.0
2 3 11.1
3 7 25.9
Site of pterygium
Nasal 129 87.8
Temporal 16 10.9
Central 2 1.4
Recurrence
Yes 13 8.8
No 134 91.2
a
Grading of pterygium was performed as described in
methods
Table 3 Effect of pterygium grading system on recurrence
Grading of pterygium Recurrence N (%) P value
a
Yes No
Primary
1 2 (2.4) 83 (97.6) 0.008
2 4 (19) 17 (81)
3 2 (14.3) 12 (85.7)
Recurrent
1 4 (23.5) 13 (76.5) 0.334
2 1 (33.3) 2 (66.7)
3 00 (00) 7 (100)
N number of subjects
a
Pearsons chi squared test
Int Ophthalmol
1 3
Author's personal copy
signicantly related to the recurrence of pterygium in
our study, with increasing number of cases of recur-
rence in younger age groups. Similar conclusions have
been drawn from numerous worldwide studies [22, 26,
27]. Female gender was not related to recurrence in the
target group, presumably due to the fact that women in
Pakistan are usually housewives whereas men are
commonly exposed to occupational and environmen-
tal hazards leading to a higher rate of recurrence.
Site of pterygium was also investigated for its role
in recurrence, mainly because of the fact that in most
cases, pterygia is always present on the nasal side;
however, there was no signicant association between
site and recurrence. Secondary pterygium has been
recognized as a risk factor for a higher recurrence rate
in numerous studies [21, 22, 28]. Similarly, in the
present study a highly signicant rate of recurrence of
18.5 % was observed in the secondary group as
compared to 6.7 % in the primary pterygium group. In
a recent prospective study carried out by Diaz et al.
[29], no recurrences were observed on follow-up in
group of patient with previous recurrent pterygia
treated with intraoperative MMC. Many grading
systems are currently being used for grading ptery-
gium; however, in our study we used the grading
system based on the extent of corneal involvement by
the brous pterygium. The same system of grading is
currently being used extensively in Asian countries as
well as some developed countries. There was a higher
tendency of recurrence in participants with higher
grades of corneal involvement with a recurrence rate
of 5.9 % in the grade 1 group as compared to 21 % in
the grade 2 group. Similar results have been obtained
in studies across Europe where a high rate of
recurrence has been associated with increased esh-
iness of the pterygia [30]. In the secondary pterygium
group, the same results could not be achieved due to
the small sample size, although a denite trend was
noted.
In conclusion, our study found signicant associ-
ations of recurrence with younger age as well as with
secondary pterygia. There was a trend for association
with grade, which did not reach signicance level for
the whole sample. For primary pterygia there was a
signicant increase in recurrence rate with higher
grades of pterygium. While this study fullls the
objective set by the study protocol for this project of
determining the recurrence of pterygiumby its grading
method, and to evaluate the potential role of various
other risk factors in its recurrence in patients assisted
with intraoperative topical MMC (0.02 %), there
remain certain limitations to this study due to the
small sample size in the recurrent pterygium group. A
large-scale prospective study with appropriate power
is recommended for evaluating the microstructural
changes in the eye to possibly understand the dynam-
ics of the different grading on pterygiumrecurrence. A
study to document the recurrence rates in pterygium
cases following the conjunctival autograft method
should be performed to determine the potential
differences in the factors limiting the success rate of
both methods.
Acknowledgments The authors are greatly indebted to Dr.
Tashfeen Ahmad, Associate Professor, Department of Surgery,
AKUH for his assistance in statistical analysis.
Conict of interest No conicting relationship exists for any
author.
Financial Support None.
References
1. Ang LP, Chua JL, Tan DT (2007) Current concepts and
techniques in pterygium treatment. Curr Opin Ophthalmol
18(4):308313
2. Gupta VP, Saxena T (2003) Comparison of single-drop
mitomycin C regime with other mitomycin C regimes in
pterygium surgery. Indian J Ophthalmol 51:5965
3. Mahar PS, Manzar N, Ahmad K (2011) The effect of intra-
operative use of topical mitomycin-C on intra-ocular pres-
sure in patients with pterygium excision. Asian J Ophthal-
mol 12:144148
4. DOmbrain A (1948) The surgical treatment of pterygium.
Br J Ophthalmol 32:6571
5. Hirst LW (2003) The treatment of pterygium. Surv Oph-
thalmol 48(2):145180
6. Mutlu FM, Sobaci G, Tatar T, Yildirim E (1999) A com-
parative study of recurrent pterygium surgery: limbal con-
junctival autograft transplantation versus mitomycin C with
conjunctival ap. Ophthalmology 106:817821
7. Sharma A, Gupta A, Ram J, Gupta A (2000) Low-dose
intraoperative mitomycin-Cversus conjunctival autograft in
primary pterygium surgery: long term follow-up. Ophthal-
mic Surg Lasers 31:301307
8. Kunitomo N, Mori S (1963) Studies on the pterygium. Part
4. Atreatment of the pterygium by mitomycin Cinstillation.
Acta Soc Ophthalmol Jpn 67:601607
9. Singh G, Wilson MR, Foster CS (1988) Mitomycin eye drops
as treatment for pterygium. Ophthalmology 95:813821
10. Mahar PS, Manzar N, Hassan M, Ahmad T (2010) The
effect of sub-conjunctival mitomycin-C on intra-ocular
pressure in various types of glaucoma. Asian J Ophthalmol
12:26
Int Ophthalmol
1 3
Author's personal copy
11. Oguz H, Basar E, Gurler B(1999) Intraoperative application
versus postoperative mitomycin C eye drops in pterygium
surgery. Acta Ophthalmol Scand 77(2):147150
12. Hata T, Hoshi T, Kanamori K, Matsumae A, Shima T, Su-
gawara R (1956) Mitomycin, a new antibiotic from Strep-
tomyces. I. J Antibiot (Tokyo) 9(4):141146
13. Qing-feng L, Liang X, Xiu-ying J, Qi-sheng Y, Xiao-hui Y,
Tong-tong C (2010) Epidemiology of pterygium in aged
rural population of Beijing, China. Chin Med J
123(13):16991701
14. Bradley JC, Yang W, Bradley RH, Reid TW, Schwab IR
(2010) The science of pterygia. Br J Ophthalmol 94(7):
815820
15. Gazzard G, Saw SM, Farook M, Koh D, Widjaja D, Chia SE
et al (2002) Pterygium in Indonesia: prevalence, severity
and risk factors. Br J Ophthalmol 86(12):13411346
16. Mahar PS, Nwokora GE (1993) Role of mitomycin-C in
pterygium surgery. Br J Ophthalmol 77:433435
17. Hayasaka S, Noda S, Yamamoto Y et al (1988) Postopera-
tive instillation of low dose mitomycin-C in the treatment of
primary pterygium. Am J Ophthalmol 106:715718
18. Rachmiel R, Leibe H, Levartovsky S (1995) Results of
treatment with topical mitomycin C 0.02 % following exci-
sion of primary pterygium. Br J Ophthalmol 79:233239
19. Panda A, Das GK, Tuli SW, Kumar A (1998) Randomized
trial of intra-operative mitomycin C in surgery for ptery-
gium. Am J Ophthalmol 125:5963
20. Lam DS, Wong AK, Fan DS, Chew S, Kwok PS, Tso MO
(1998) Intraoperative mitomycin C to prevent recurrence of
pterygium after excision: a 30-month follow-up study.
Ophthalmology 105(5):901904
21. Rahman A, Yahya K, Shariful Hasan K (2008) Recurrence
rate of pterygium following surgical excision with intraop-
erative versus postoperative mitomycin-C. J Coll Physicians
Surg Pak 18(8):489492
22. Cheng HC, Tseng SH, Kao PL, Chen FK (2001) Low-dose
intraoperative mitomycin C as chemoadjuvant for ptery-
gium surgery. Cornea 20(1):2429
23. Narsani AK, Jatoi SM, Gul S, Dabir SA(2008) Treatment of
primary pterygium with conjunctival autograft and mito-
mycin C. A comparative study. J Liaquat Uni Med Health
Sci 7(3):184187
24. Frucht-pery J, Raiskup F, Ilsar M, Landau D, Orucov F,
Solomon A (2006) Conjunctival autografting combined
with low-dose mitomycin C for prevention of primary
pterygium recurrence. Am J Ophthalmol 141(6):10441050
25. Mahar PS (1997) Conjunctival autograft versus topical
mitomycin C in treatment of pterygium. Eye 11:790792
26. Chen PP, Ariyasu RG, Kaza V, LaBree LD, McDonnell PJ
(1995) A randomized trial comparing mitomycin C and
conjunctival autograft after excision of primary pterygium.
Am J Ophthalmol 120(2):151160
27. Mastropasqua L, Carpineto P, Ciancaglini M et al (1996)
Long term results of intraoperative mitomycin C in the
treatment of recurrent pterygium. Br J Ophthalmol
80:288291
28. Mahar PS (1996) Role of mitomycin-C in reducing the
recurrence of pterygium after surgery. Pak J Ophthalmol
12(3):9194
29. D az L, Villegas VM, Emanuelli A, Izquierdo NJ (2008)
Efcacy and safety of intraoperative mitomycin C as
adjunct therapy for pterygium surgery. Cornea
27(10):11191121
30. Tan DTH, Chee SP, Dear KBG et al (1997) Effect of
pterygium morphology on pterygium recurrence in a con-
trolled trial comparing conjunctival autografting with bare
sclera excision. Arch Ophthalmol 115:12351240
Int Ophthalmol
1 3
Author's personal copy
Você também pode gostar
- 2021 Nexus Pharma Injection Price List FinalDocumento5 páginas2021 Nexus Pharma Injection Price List FinalRyu SanurAinda não há avaliações
- Nursing 102 Med-Surg PerioperaDocumento7 páginasNursing 102 Med-Surg PerioperaKarla FralalaAinda não há avaliações
- Information Sheet: Crystalline Silica DustDocumento2 páginasInformation Sheet: Crystalline Silica DustIoana UrsanAinda não há avaliações
- Sinus Floor Augmentation - Course NPDocumento204 páginasSinus Floor Augmentation - Course NPANAKIN HART100% (5)
- CeftriaxoneDocumento2 páginasCeftriaxoneFlora Angeli PastoresAinda não há avaliações
- Neuroscience: Science of The Brain in PolishDocumento72 páginasNeuroscience: Science of The Brain in PolishInternational Brain Research Organization100% (1)
- Connectors in FPDDocumento53 páginasConnectors in FPDsrinivaskalluri80% (5)
- Orthodontics!!Documento9 páginasOrthodontics!!Ayesha AwanAinda não há avaliações
- Title: Artificial Intelligence in Healthcare An Integrated Approach To Healthcare DeliveryDocumento13 páginasTitle: Artificial Intelligence in Healthcare An Integrated Approach To Healthcare DeliveryofhsaosdafsdfAinda não há avaliações
- Growth RotationDocumento57 páginasGrowth RotationAtul Koundel100% (1)
- tmpC47C TMPDocumento4 páginastmpC47C TMPFrontiersAinda não há avaliações
- tmp607F TMPDocumento5 páginastmp607F TMPFrontiersAinda não há avaliações
- The Course of Dry Eye After Phacoemulsification Surgery: Researcharticle Open AccessDocumento5 páginasThe Course of Dry Eye After Phacoemulsification Surgery: Researcharticle Open AccessDestia AnandaAinda não há avaliações
- Literature Review PterygiumDocumento7 páginasLiterature Review Pterygiumafmzzaadfjygyf100% (1)
- Medi 96 E5864Documento6 páginasMedi 96 E5864mono1144Ainda não há avaliações
- Comparison of Recurrence of Pterygium Following Excision by Bare Sclera Technique With and Without Mitomycin CDocumento80 páginasComparison of Recurrence of Pterygium Following Excision by Bare Sclera Technique With and Without Mitomycin CShoaib AbbasAinda não há avaliações
- Trends in Corneal TopographyDocumento7 páginasTrends in Corneal TopographygustavoecardosoAinda não há avaliações
- Jurnal Mata 5 KEVIN PDFDocumento10 páginasJurnal Mata 5 KEVIN PDFKevinAinda não há avaliações
- Jurnal Mata 5Documento6 páginasJurnal Mata 5Dahru KinanggaAinda não há avaliações
- Opth 14 2087Documento4 páginasOpth 14 2087Savitri IndrasariAinda não há avaliações
- Incidence of PostcataractDocumento8 páginasIncidence of PostcataractSurendar KesavanAinda não há avaliações
- Efficacy of Autologous Blood Clot in Primary Pterygium Surgery Compared With Suture Technique in A Tertiary Hospital of BangladeshDocumento7 páginasEfficacy of Autologous Blood Clot in Primary Pterygium Surgery Compared With Suture Technique in A Tertiary Hospital of BangladeshBOHR International Journal of Current Research in Optometry and Ophthalmology (BIJCROO)Ainda não há avaliações
- Comparison of Free Conjunctival Autograft Versus Amniotic Membrane Transplantation For Pterygium SurgeryDocumento5 páginasComparison of Free Conjunctival Autograft Versus Amniotic Membrane Transplantation For Pterygium SurgeryTri Novita SariAinda não há avaliações
- Aspiration and Steroid Injection-An Effective Approach For Auricular SeromaDocumento5 páginasAspiration and Steroid Injection-An Effective Approach For Auricular Seromasolikin ikinAinda não há avaliações
- 69 EdDocumento10 páginas69 EdAnna ListianaAinda não há avaliações
- Clinical Features of Herpes Simplex Keratitis in A Korean Tertiary Referral Center: Efficacy of Oral Antiviral and Ascorbic Acid On RecurrenceDocumento8 páginasClinical Features of Herpes Simplex Keratitis in A Korean Tertiary Referral Center: Efficacy of Oral Antiviral and Ascorbic Acid On RecurrenceGiorgos MousterisAinda não há avaliações
- Lower Eyelid Complications Associated With Transconjunctival Versus Subciliary Approaches To Orbital Floor FracturesDocumento5 páginasLower Eyelid Complications Associated With Transconjunctival Versus Subciliary Approaches To Orbital Floor Fracturesstoia_sebiAinda não há avaliações
- Jurnal New1Documento5 páginasJurnal New1Nurul Qomariah TAinda não há avaliações
- Glaucoma After Congenital Cataract SurgeryDocumento6 páginasGlaucoma After Congenital Cataract SurgerySamawi RamudAinda não há avaliações
- Clinical Study: Long-Term Effects of Cataract Surgery On Tear Film ParametersDocumento5 páginasClinical Study: Long-Term Effects of Cataract Surgery On Tear Film ParametersJohn ElfranAinda não há avaliações
- Keratoconus 2Documento39 páginasKeratoconus 2YOSEF DERDESAWEAinda não há avaliações
- Comparison of Limberg Flep and Adipofacial Flep in The Surgical Treatment of Pilonidal Sinus A Prospective Randomized Clinical StudyDocumento5 páginasComparison of Limberg Flep and Adipofacial Flep in The Surgical Treatment of Pilonidal Sinus A Prospective Randomized Clinical StudyAthenaeum Scientific PublishersAinda não há avaliações
- Survival and Complications of Zygomatic Implants (PDFDrive)Documento36 páginasSurvival and Complications of Zygomatic Implants (PDFDrive)Lê Minh KhôiAinda não há avaliações
- Prevalence and Risk Factor On Age Related Cataract and Surgery in Adults Over 50 Years Old in BInhu District, ChinaDocumento7 páginasPrevalence and Risk Factor On Age Related Cataract and Surgery in Adults Over 50 Years Old in BInhu District, ChinaAi AisyahAinda não há avaliações
- CO 2767 Alpay 120108Documento6 páginasCO 2767 Alpay 120108MaRia AnastasiaAinda não há avaliações
- El Beheiry2019Documento4 páginasEl Beheiry2019achmadaAinda não há avaliações
- Blepharochalasis: Clinical and Epidemiological Characteristics, Surgical Strategy and Prognosis - A Retrospective Cohort Study With 93 CasesDocumento7 páginasBlepharochalasis: Clinical and Epidemiological Characteristics, Surgical Strategy and Prognosis - A Retrospective Cohort Study With 93 CasesSaqar SharepourAinda não há avaliações
- 1 - Prevalence of Maxillary Sinus SeptaDocumento9 páginas1 - Prevalence of Maxillary Sinus SeptaLamis MagdyAinda não há avaliações
- Jurnal 6Documento7 páginasJurnal 6ayuAinda não há avaliações
- Cotofana 2021Documento9 páginasCotofana 2021Emrys1987Ainda não há avaliações
- External Dacryocystorhinostomy Outcomes in Patients With A History of DacryocystitisDocumento9 páginasExternal Dacryocystorhinostomy Outcomes in Patients With A History of DacryocystitisRegina HershaaAinda não há avaliações
- Five-Year Results of ViscotrabeculotomyDocumento10 páginasFive-Year Results of ViscotrabeculotomyChintya Redina HapsariAinda não há avaliações
- IncidenceDocumento11 páginasIncidenceNenad ProdanovicAinda não há avaliações
- 1 s2.0 S1607551X11000349Documento4 páginas1 s2.0 S1607551X11000349xxxAinda não há avaliações
- Abscess Volume in Orbital CellulitisDocumento7 páginasAbscess Volume in Orbital Cellulitisteu.yamAinda não há avaliações
- Actinic Cheilitis: Clinical Characteristics Observed in 75 Patients and A Summary of The Literature of This Often Neglected Premalignant DisorderDocumento9 páginasActinic Cheilitis: Clinical Characteristics Observed in 75 Patients and A Summary of The Literature of This Often Neglected Premalignant DisorderYustisia CharissaAinda não há avaliações
- Abses SeptumDocumento8 páginasAbses SeptumDian FahmiAinda não há avaliações
- The Effectiveness of Immediate Triamcinolone Acetonide Injection After Auricular Keloid Surgery: A Prospective Randomized Controlled TrialDocumento8 páginasThe Effectiveness of Immediate Triamcinolone Acetonide Injection After Auricular Keloid Surgery: A Prospective Randomized Controlled TrialMarande LisaAinda não há avaliações
- Sutureless and Glue Free Conjunctivo-Limbal Autograft in Primary Pterygium Surgery - Outcome S and Recurrence RateDocumento8 páginasSutureless and Glue Free Conjunctivo-Limbal Autograft in Primary Pterygium Surgery - Outcome S and Recurrence RateThomas KweeAinda não há avaliações
- Bacterial KeratitisDocumento6 páginasBacterial KeratitisMelia RahmayantiAinda não há avaliações
- Steriod Cataract PDFDocumento4 páginasSteriod Cataract PDFLisa IskandarAinda não há avaliações
- Ijced 21 004Documento7 páginasIjced 21 004Eduardo Jesús Núñez JordánAinda não há avaliações
- Piezoincisiones (Proceso Inflamatorio)Documento15 páginasPiezoincisiones (Proceso Inflamatorio)Ana Maria Clara HernándezAinda não há avaliações
- The Epidemiology and Clinical Features of Blepharoptosis in Taiwanese PopulationDocumento9 páginasThe Epidemiology and Clinical Features of Blepharoptosis in Taiwanese PopulationALYA MAULIDAAinda não há avaliações
- Clinical Characteristics and Surgical Outcomes in Patients With Intermittent ExotropiaDocumento6 páginasClinical Characteristics and Surgical Outcomes in Patients With Intermittent ExotropiaIkmal ShahromAinda não há avaliações
- Jabbar V and 2015Documento7 páginasJabbar V and 2015annisaAinda não há avaliações
- Cornea PDFDocumento4 páginasCornea PDFHariadhii SalamAinda não há avaliações
- Transplantation of Conjunctival Limbal Autograft and Amniotic Membrane Vs Mitomycin C and Amniotic Membrane in Treatment of Recurrent PterygiumDocumento6 páginasTransplantation of Conjunctival Limbal Autograft and Amniotic Membrane Vs Mitomycin C and Amniotic Membrane in Treatment of Recurrent PterygiumFrc 'Hario' FanachaAinda não há avaliações
- Analysis of Intraoperative and Postoperative Complications in Pseudoexfoliation Eyes Undergoing Cataract SurgeryDocumento4 páginasAnalysis of Intraoperative and Postoperative Complications in Pseudoexfoliation Eyes Undergoing Cataract SurgerymathyasthanamaAinda não há avaliações
- 2022 Article 2645Documento10 páginas2022 Article 2645MufassiraturrahmahAinda não há avaliações
- Keratopati BulosaDocumento7 páginasKeratopati BulosaShafira LusianaAinda não há avaliações
- CataractDocumento12 páginasCataracthelda fitria wahyuniAinda não há avaliações
- CataractDocumento3 páginasCataractSetiawan Arif WibowoAinda não há avaliações
- Abstracts COMAPI 2014 IJMSDocumento20 páginasAbstracts COMAPI 2014 IJMSfelipetheAinda não há avaliações
- JurdingDocumento8 páginasJurdingTanani 102014007Ainda não há avaliações
- Clinical Presentation and Microbial Analyses of Contact Lens Keratitis An Epidemiologic StudyDocumento4 páginasClinical Presentation and Microbial Analyses of Contact Lens Keratitis An Epidemiologic StudyFi NoAinda não há avaliações
- Coronectomy 2Documento14 páginasCoronectomy 2Rovian RosaliaAinda não há avaliações
- Jurnal MataDocumento7 páginasJurnal Mataokky_rahmatAinda não há avaliações
- Advances in Periodontal Surgery: A Clinical Guide to Techniques and Interdisciplinary ApproachesNo EverandAdvances in Periodontal Surgery: A Clinical Guide to Techniques and Interdisciplinary ApproachesSalvador NaresAinda não há avaliações
- tmpF178 TMPDocumento15 páginastmpF178 TMPFrontiersAinda não há avaliações
- Tmp1a96 TMPDocumento80 páginasTmp1a96 TMPFrontiersAinda não há avaliações
- Tmpa077 TMPDocumento15 páginasTmpa077 TMPFrontiersAinda não há avaliações
- tmpE3C0 TMPDocumento17 páginastmpE3C0 TMPFrontiersAinda não há avaliações
- tmp998 TMPDocumento9 páginastmp998 TMPFrontiersAinda não há avaliações
- tmp3656 TMPDocumento14 páginastmp3656 TMPFrontiersAinda não há avaliações
- tmp27C1 TMPDocumento5 páginastmp27C1 TMPFrontiersAinda não há avaliações
- tmpA7D0 TMPDocumento9 páginastmpA7D0 TMPFrontiersAinda não há avaliações
- tmp96F2 TMPDocumento4 páginastmp96F2 TMPFrontiersAinda não há avaliações
- tmp97C8 TMPDocumento9 páginastmp97C8 TMPFrontiersAinda não há avaliações
- Sickle Cell Disease, Epidemiology, Genetic History, Complication and ManagementDocumento52 páginasSickle Cell Disease, Epidemiology, Genetic History, Complication and ManagementAnastasiafynnAinda não há avaliações
- Ge Cumulative Rates ResortedDocumento81 páginasGe Cumulative Rates ResortedfishyfredAinda não há avaliações
- Saccharothrixsp Abh26 PDFDocumento7 páginasSaccharothrixsp Abh26 PDFAlia RahmaAinda não há avaliações
- Pre-Diabetes:: Don't Let It Lead To Type-2Documento1 páginaPre-Diabetes:: Don't Let It Lead To Type-2ARIA MINDAinda não há avaliações
- Galvus (Vildagliptin) : How Does It Work?Documento5 páginasGalvus (Vildagliptin) : How Does It Work?Radhakrishna KurupAinda não há avaliações
- Safety Reports Series: Radiation Protection in Newer Medical Imaging Techniques: Cardiac CTDocumento30 páginasSafety Reports Series: Radiation Protection in Newer Medical Imaging Techniques: Cardiac CTjiar001Ainda não há avaliações
- Synthesis TranexamicDocumento6 páginasSynthesis TranexamicChính MùAinda não há avaliações
- History of MedicineDocumento33 páginasHistory of MedicineBradley KenneyAinda não há avaliações
- Community Pharmacy Organization: Pharmaceutical Management.Documento12 páginasCommunity Pharmacy Organization: Pharmaceutical Management.pawannnnAinda não há avaliações
- SCREEMDocumento2 páginasSCREEMDranreb Berylle MasangkayAinda não há avaliações
- Infochap10 12Documento18 páginasInfochap10 12Nareeza AbdullaAinda não há avaliações
- ManjisthaDocumento2 páginasManjisthaporurAinda não há avaliações
- Mnemonics ShortDocumento139 páginasMnemonics ShortKelly HernandezAinda não há avaliações
- The Enigma of Facial Beauty: Esthetics, Proportions, Deformity, and ControversyDocumento6 páginasThe Enigma of Facial Beauty: Esthetics, Proportions, Deformity, and ControversyIsmaelLouGomezAinda não há avaliações
- WNHS Og AntepartumHaemorrhageDocumento17 páginasWNHS Og AntepartumHaemorrhagelydia amaliaAinda não há avaliações
- Conservative Treatment, Plate Fixation, or Prosthesis For Proximal Humeral Fracture. A Prospective Randomized StudyDocumento3 páginasConservative Treatment, Plate Fixation, or Prosthesis For Proximal Humeral Fracture. A Prospective Randomized StudyAndi Urviana AsrahAinda não há avaliações
- Acetone PDFDocumento118 páginasAcetone PDFNhn Neen100% (1)
- Path Lab Name: Onyedika Egbujo No: #671 Topic: PheochromocytomaDocumento4 páginasPath Lab Name: Onyedika Egbujo No: #671 Topic: PheochromocytomaOnyedika EgbujoAinda não há avaliações
- PAS HAndbookDocumento375 páginasPAS HAndbookJheanell JamesAinda não há avaliações
- Alprazolam Effect On ThyroidDocumento7 páginasAlprazolam Effect On ThyroidswatiAinda não há avaliações