Escolar Documentos
Profissional Documentos
Cultura Documentos
Gadolinium Contrast Toxicity in Patients With Kidney Disease PDF
Enviado por
Thiago Teruya0 notas0% acharam este documento útil (0 voto)
87 visualizações9 páginasReports of a previously rare condition entitled nephrogenic systemic fibrosis (NSF) have recently emerged in patients with advanced kidney disease. The risk of developing NSF is increased with larger doses of gadolinium (or multiple exposures) underlying pro-inflammatory states (in particular vascular endothelial dysfunction) and per-haps some currently unrecognized cofactors.
Descrição original:
Título original
gadolinium contrast toxicity in patients with kidney disease.pdf
Direitos autorais
© © All Rights Reserved
Formatos disponíveis
PDF, TXT ou leia online no Scribd
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoReports of a previously rare condition entitled nephrogenic systemic fibrosis (NSF) have recently emerged in patients with advanced kidney disease. The risk of developing NSF is increased with larger doses of gadolinium (or multiple exposures) underlying pro-inflammatory states (in particular vascular endothelial dysfunction) and per-haps some currently unrecognized cofactors.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
0 notas0% acharam este documento útil (0 voto)
87 visualizações9 páginasGadolinium Contrast Toxicity in Patients With Kidney Disease PDF
Enviado por
Thiago TeruyaReports of a previously rare condition entitled nephrogenic systemic fibrosis (NSF) have recently emerged in patients with advanced kidney disease. The risk of developing NSF is increased with larger doses of gadolinium (or multiple exposures) underlying pro-inflammatory states (in particular vascular endothelial dysfunction) and per-haps some currently unrecognized cofactors.
Direitos autorais:
© All Rights Reserved
Formatos disponíveis
Baixe no formato PDF, TXT ou leia online no Scribd
Você está na página 1de 9
Current Drug Safety, 2008, 3, 67-75 67
1574-8863/08 $55.00+.00 2008 Bentham Science Publishers Ltd.
Gadolinium-Contrast Toxicity in Patients with Kidney Disease: Nephro-
toxicity and Nephrogenic Systemic Fibrosis
Mark A. Perazella
*
Section of Nephrology, Department of Medicine, Yale University School of Medicine, New Haven, Connecticut 06520-
8029, USA
Abstract: Gadolinium is widely employed as a contrast agent for magnetic resonance imaging (MRI) and has generally
been considered to be safe. As with iodinated radiocontrast, concern for contrast-induced nephropathy existed with gado-
linium-contrast as it possessed many similar qualities (hyperosmolar, renal excretion via glomerular filtration). Early stud-
ies in low risk patients suggested a benign renal profile, however, recent studies raise the possibility of nephrotoxicity. In
addition, reports of a previously rare condition entitled nephrogenic systemic fibrosis (NSF) have recently emerged in pa-
tients with advanced kidney disease and have been linked to exposure to gadolinium-contrast. Nephrogenic systemic fi-
brosis is a debilitating disorder in which progressive and severe fibrosis of the skin and other systemic organs that leads to
significant disability and is associated with increased mortality. Initially reported most commonly in end stage renal dis-
ease (ESRD) patients receiving dialysis, it is also described in patients with severe acute kidney injury (AKI) and ad-
vanced chronic kidney disease (stages 4 and 5) not requiring dialysis. In addition to underlying kidney disease, the risk of
developing NSF is increased with larger doses of gadolinium (or multiple exposures), exposure to specific gadolinium
chelates (non-ionic, linear), underlying pro-inflammatory states (in particular vascular endothelial dysfunction), and per-
haps some currently unrecognized cofactors. No clearly effective therapies exist for NSF, although recovery from AKI
and establishment of normal kidney function with renal transplantation appear to reverse or stabilize the disease in some
cases. Avoidance of gadolinium exposure appears to be the best approach for patients who maintain risk factors. When
gadolinium exposure occurs, aggressive hemodialysis following exposure may be useful as gadolinium is efficiently re-
moved by this extracorporeal technique. Peritoneal dialysis clearance of gadolinium is poor, but aggressive peritoneal di-
alysis prescriptions have not been studied for gadolinium removal.
Keywords: Gadolinium, nephrotoxicity, nephrogenic systemic fibrosis, chronic kidney disease, end stage kidney disease, mag-
netic resonance imaging, radiocontrast-induced nephropathy.
INTRODUCTION
Magnetic resonance imaging (MRI) is a commonly used
imaging technique for numerous organ systems including the
central nervous system, hepatic structures, and the vascula-
ture. MR images are significantly enhanced by use of gado-
linium-based contrast agents. They often provide images that
are superior to those obtained with computed tomography
(CT) scan and have the advantage of avoiding iodinated ra-
diocontrast agents which have more overall toxicity (allergic
and non-allergic reactions). Thus, MRI has been considered a
relatively safe alternative to CT scan in situations where a
contrast agent is thought required for enhanced image at-
tainment. However, two complications of gadolinium-
contrast (Gd-contrast) have come to light in recent times.
First, concern for contrast-induced nephropathy from Gd-
contrast has been raised as several studies over the past dec-
ade demonstrate nephrotoxicity following Gd-contrast ad-
ministration in patients with underlying kidney disease and
other co-morbidities. Gd-contrast agents are hyperosmolar
and completely eliminated from the body via renal excretion
(glomerular filtration). Second, and even more concerning is
*Address correspondence to this author at the Section of Nephrology, De-
partment of Medicine, Yale University School of Medicine, New Haven,
Connecticut 06520-8029, USA; Tel: 203-785-4184; Fax: 203-785-7068;
E-mail: mark.perazella@yale.edu
the recognition that Gd-contrast exposure in patients with
significant kidney disease may trigger the development of
nephrogenic systemic fibrosis (NSF), a debilitating and often
devastating systemic fibrosing condition that is most clini-
cally prominent in the skin [1-12]. This review will focus on
these clinically important complications of Gd-contrast.
GADOLINIUM CONTRAST: GENERAL PROPER-
TIES AND PHARMACOKINETICS
Gadolinium (Gd) is a metal of the lanthanide series
(atomic number 64 on element chart) which has paramag-
netic properties that disturb relaxation of water protons and
by shortening relaxation times, increases signal intensity.
This quality makes it extremely useful as an intravenous
and/or intra-arterial contrast agent for MRI/MRA to enhance
images of various body organs and tissues. As it is a metal, it
must be in an ionic form to be soluble in water and allow it
to be injected as a contrast agent that distributes throughout
the body. However, gadolinium in this free ionic form (Gd
3+
)
is highly toxic to humans (and animals). It precipitates in
several tissues including the liver, lymph nodes, and bones.
Gd
3+
obstructs passage of calcium through ion channels of
muscle cells and nerve tissue cells thereby reducing neuro-
muscular transmission, and interferes with intracellular en-
zymes and cell membranes. In order to avoid these toxic ef-
fects, Gd
3+
must be sequestered by non-toxic substances
[13]. This is achieved by binding Gd
3+
to another agent,
68 Current Drug Safety, 2008, Vol. 3, No. 1 Mark A. Perazella
which is known generically as a chelate. Chelates are large
organic molecules that form a stable complex with Gd
3+
, do
not readily dissociate in vivo, and make the ion biochemi-
cally inert [13,14]. The properties of the various Gd-
chelates allow classification of Gd-contrast into four main
categories based on their biochemical structure (linear versus
macrocyclic) and their charge (ionic versus non-ionic). Mac-
rocyclic chelates bind Gd
3+
more tightly than linear chelates,
tend to be more stable both in vitro and in vivo, and possess
lower dissociation rates [15]. Simply stated, macrocyclic
chelates stick more tightly to Gd
3+
than do linear chelates;
this has implications for possible toxicity. This aspect of
chelate characteristics is important to prevent liberation of
free Gd
3+
from its chelate, a process known as transmetala-
tion. This phenomenon entails release of free Gd
3+
from its
chelate ligand, which then binds with another endogenous
metal such as zinc or copper, allowing free Gd
3+
to bind an
endogenous ligand such as phosphorus. The commonly em-
ployed Gd-contrasts approved by the Food and Administra-
tion Drug (FDA) and their characteristics are noted in Table
1. The recommended dose of a Gd-contrast agent for a non-
vascular MR study is 0.1 mmol/kg. When imaging of vascu-
lar structures (MRA) is required, higher doses of Gd-contrast
(0.3-0.4 mmol/kg) are often utilized. Until recently, Gd-
contrast agents were FDA approved only for MRI studies at
the 0.1 mmol/kg dose. Gadoteridol (macrocyclic chelate) is
the only MR chelate approved at the higher 0.3 mmol/kg
dose. Most MRA studies are often performed using Gd-
contrasts at dose levels that are considered off-label.
Following intravenous injection, Gd-contrasts are rapidly
distributed into the extracellular space, quickly equilibrating
between the plasma and interstitial compartments. The ma-
jority are restricted to the extracellular space and have lim-
ited protein binding. As a result of their exclusion from the
intracellular compartment, Gd-contrasts have small volumes
of distribution (Vd), approximately 0.26-0.28 L/kg body
weight. They do not undergo biotransformation and are
eliminated unchanged by the kidneys via glomerular filtra-
tion without any contribution from tubular secretion. Renal
clearance of Gd-contrasts ranges from 1.1 to 1.6 ml/min/kg
in individuals with normal renal function (approximating the
creatinine clearance). The Gd-contrasts maintain a mean
terminal half-life (T
1/2
) of approximately 1.6 hours. Over
95% of an injected dose is eliminated within 24 hours with
less than 3% being eliminated in the feces [13,14,16]. The
Vd for intravenous Gd-contrasts (gadobenate dimeglumine
studied) is similar for patients with moderate (creatinine
clearance [CrCl], 31-60 ml/min; n=15) and severe (CrCl, 15-
30 ml/min; n=17) kidney disease when compared with
healthy subjects. However, the mean terminal T
1/2
is longer
in moderate (5.6 hours) and severe (9.2 hours) kidney dis-
ease than in healthy subjects (1.6 hours). Mean blood and
renal clearance are both much lower in moderate (56 ml/min;
47 ml/min) and severe (31 ml/min; 22 ml/min) kidney dis-
ease than in normal subjects (183 ml/min; 118 ml/min).
Comparable pharmacokinetics of Gd-contrasts in patients
with underlying kidney disease have been reported in other
studies [17,18]. Thus, it is predictable that tissue gadolinium
exposure is prolonged in the setting of decreased kidney
function. The relatively small molecular weight (500 Da),
small Vd (0.28 L/kg), and negligible protein binding charac-
teristics of Gd-contrasts make them ideal for removal with an
extracorporeal therapy such as hemodialysis. In one study,
the T
1/2
of Gd-contrasts of non-dialyzed CKD stage 5 (CrCl
=2-10 ml/min) patients was quite prolonged at 34.3 hours
but decreased significantly to 2.6 hours following hemo-
dialysis [19]. In another study the average Gd-contrast elimi-
nation from serum using hemodialysis was 73.8% with one
treatment, 92.4% with 2 treatments and 98.9% after the 3
rd
treatment [20,21]. Peritoneal dialysis on the other hand was
an ineffective method of Gd-contrast removal (T
1/2
of 52.7
hours) [19]. This study suffers by the use of what is now
considered an inadequate peritoneal dialysis prescription (2.0
liter volumes x 4 exchanges over a 24 hour period).
GADOLINIUM-CONTRAST AND NEPHROTOXIC-
ITY
Iodinated radiocontrast-media induced nephrotoxicity is
well described and common. However, the issue of Gd-
contrast induced nephrotoxicity is somewhat controversial
and generally overlooked. Initial pharmaceutical trials exam-
ined the potential adverse renal effects of Gd-contrast. Since
Gd-contrasts have characteristics very similar to those of
iodinated radiocontrast, in particular hyperosmolality and
renal clearance entirely dependent upon glomerular filtration,
nephrotoxicity was an obvious concern of both manufactur-
ers and physicians. Animal studies demonstrate nephrotoxic-
ity with gadolinium contrast when given in high doses (0.6-
3.0 mmol/kg) to rats with normal kidney function [22].
Histopathology demonstrates vacuolization and necrosis of
proximal tubular cells. The lower observed risk of Gd-based
contrast as compared with iodinated radiocontrast may relate
to mechanism of nephrotoxicity. Iodinated radiocontrast
causes renal injury primarily through induction of vasocon-
striction, whereas Gd-based contrast has not been shown to
promote renal ischemia. Early studies in normal healthy sub-
jects as well as small groups of patients with mild to moder-
ate levels of underlying kidney disease suggested a reasona-
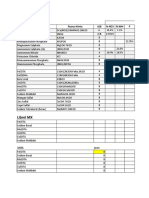
Table 1. FDA Approved Gadolinium Contrast Agents
Gado Formulation
Osmolality
(mosm/l)
Charge
Molecular
Structure
Stability Con-
stant
Excess Chelate
(mg/ml)
Gado Market
Share* (2006)
Gadodiamide (Omniscan) 900 Non-ionic Linear 10
14.9
12 34%
Gadopentetate (Magnevist) 1960 Ionic Linear 10
18.1
0.4 47%
Gadoversetamide (OptiMARK) 1110 Non-ionic Linear 10
15
28.4 8%
Gadobenate (MultiHance) 1970 Ionic Linear 10
18.4
0.1 6%
Gadoteridol (Prohance) 630 Non-ionic Cyclic 10
17.1
0.23 5%
Abbreviations: Gado, gadolinium. * Contrast Media Industry Guide data.
Gadolinium-Contrast and Kidney Disease Current Drug Safety, 2008, Vol. 3, No. 1 69
bly favorable renal safety profile [23, 24]. Even up until re-
cently, the Gd-contrasts were considered relatively safe for
use in patients with kidney disease, even with the high doses
required for renovascular imaging, where most other imaging
techniques were inadequate (renal scans and ultrasonogra-
phy) or were too risky (CT with iodinated contrast). The im-
portance of this issue deserves emphasis. Numerous patients
considered at high risk for radiocontrast-induced nephropa-
thy (RCIN) from an iodinated radiocontrast study are ex-
posed to a Gd-contrasts as a "renal safe" alternative. Critical
review of the literature on this subject does not, unfortu-
nately, allow a definitive answer to the question of Gd-
contrast nephrotoxicity. Some but not all of the studies pub-
lished on this subject over the past decade will be reviewed;
recognizing that other negative studies were published prior
to and during this time period.
Gadolinium-Contrast Studies Supporting Renal Safety
Several studies are available in this time period suggest-
ing that Gd-contrast agents lack any significant nephrotoxic-
ity (Table2). A retrospective study published in 1996 exam-
ined a cohort of 64 patients with mild CKD as defined by
baseline serum creatinine concentration of 2.0 1.4 mg/dl
[25]. All patients received both Gd-contrast and iodinated
contrast at separate times, thus serving as their own control.
The rate of contrast-induced nephrotoxicity, as defined by a
rise in serum creatinine concentration of 0.5 mg/dl following
each exposure, was compared between the 2 different expo-
sures. The dose of Gd-contrasts administered during the
study ranged from 0.2 to 0.4 mmol/kg. No patient receiving
Gd-contrasts developed nephrotoxicity as compared with
17% of patients receiving iodinated radiocontrast.
A prospective study of 32 patients with moderate (CrCl,
31-60 ml/min) and severe (CrCl, 10-30 ml/min) kidney dis-
ease was undertaken to examine Gd-contrast pharmacokinet-
ics and renal safety [26]. Patients received 0.2 mmol/kg of
intravenous gadobenate dimeglumine, which has an osmolal-
ity of 1970 mosm/L. 24-hour urine CrCl before and at days
1, 2, 3, 5, and 7 following gadobenate dimeglumine exposure
were measured. No patients received any form of contrast
prophylaxis prior to or during the study. There was no sig-
nificant change in CrCl at any time point in the study, sup-
porting the absence of any clinically important nephrotoxic-
ity.
Patients with kidney disease (defined as a serum creatin-
ine concentration greater than 1.5 mg/dl) were studied using
gadopentetate dimeglumine (0.4 mmol/kg dose) as an alter-
native imaging agent in patients who were allergic to iodi-
nated radiocontrast [26]. 31 patients underwent 34 digital
subtraction angiographies (DSAs) with this hyperosmolar
agent (1960 mosm/L). Only one out of 34 studies was com-
plicated by contrast-induced nephropathy, which was defined
as an increase in serum creatinine concentration greater than
0.5 mg/dl.
In 2000, a study in patients with CKD (serum creatinine
greater than 1.5 mg/dl; mean =2.2 mg/dl; range =1.6-3.6
mg/dl) and peripheral vascular disease was undertaken to
compare nephrotoxicity of nonionic radiocontrast with CO2
supplemented with either Gd-contrast (up to 0.4 mmol/kg of
gadodiamide) or nonionic radiocontrast [27]. 40 patients un-
derwent 42 lower extremity angiograms using one of the
following contrast protocols: radiocontrast =15, gadodia-
mide =20, CO2 =7. All received 300-5000 ml of normal
saline prior to contrast exposure as prophylaxis. Contrast-
induced nephropathy was defined as an increase in serum
creatinine concentration greater than 0.5 mg/dl at 48 hours
post procedure. Contrast-induced nephropathy developed in
6 out of 15 (40%) radiocontrast studies but only 1 out of 20
gadodiamide exposures (5%).
Table 2. Studies Supporting Renal Safety of Gadolinium-Contrast Agents
Author (Year) Study Contrast Agent Dose (mmol/kg) Renal Function ([Cr] in mg/dl) Result
Prince (1996) Retrospective, N=64
[Cr] 2d pre and 2d post,
CIN 0.5 mg/dL
Gadopentetate
Gadodiamide
Gadoteridol
0.2 - 0.4 [Cr] >1.5,
Mean [Cr] =2.01.4
CIN:
RC- 11/64 (17%)
Gado- 0/64 (0%)
Swan (1999) Prospective, double blind random, 32 pts (2:
1),
CIN >0.5 mg/dL
Gabobenate
dimeglumine
0.2 CrCl 10-30,
CrCl 31-60,
24 hr urine
No CIN
Hammer (1999) N =31, 34 DSAs,
Mean age 53.1
CIN >0.5 mg/dL
Gadopentetate 0.4 [Cr] >1.5
CIN: 1/34 (3%)
Spinosa (2000) N =40, LE angiograms
42 procedures
RC- 15, Gado- 20
CIN 0.5 mg/dL at 48 hr
Gadodiamide up to 0.4 [Cr] >1.5,
Mean [Cr] =2.2,
Range [Cr] =1.6-3.6
IC- 6/15 (40%)
Gado- 1/20 (5%)
Spinosa (2001) Consecutive patients treated with Gado +
CO2,
CIN >0.5 mg/dL at 48 hr
Gadodiamide <0.3 [Cr] >1.5, CIN: 3/95 (3%)
Sancak (2001) N =16, IV Gado for upper extremity or SVC Gadodiamide 0.3 Mean [Cr] =1.5,
Range [Cr] =1.2-1.8
Largest increase in
[Cr] =0.2 mg/dL
Rieger (2002) Prospective, N =29, 32 procedures (IA & IV)
CIN >0.5 mg/dL at 72 hr
Gadopentetate 0.34 0.06 [Cr] >1.5
Mean [Cr] 3.61.4
1/29 (atheroemboli)
Abbreviations: Gado, gadolinium; RC, iodinated radiocontrast; CrCl, creatinine clearance; [Cr], serumcreatinine concentration; CIN, contrast-induced nephropathy; ref, reference;
DSA, digital subtraction angiogram; LE, lower extremity; SVC, superior vena cava; IV, intravenous; IA, intra-arterial.
70 Current Drug Safety, 2008, Vol. 3, No. 1 Mark A. Perazella
The same authors published another study again support-
ing Gd-contrast safety in patients with CKD and ischemic
nephropathy [28]. 146 consecutive patients with a serum
creatinine concentration greater than 1.5 mg/dl underwent
renal angiography using a combination of CO
2
and gadodia-
mide. Contrast-induced nephropathy was defined as an in-
crease in serum creatinine concentration greater than 1.5
mg/dl at 48 hours; 95 patients had data available for study.
Three patients (3.2%) developed nephrotoxicity, less than
what is commonly seen in similar patients exposed to iodi-
nated radiocontrast.
In 2001, 16 patients with mild CKD (mean serum creatin-
ine concentration =1.5 mg/dl; range =1.2-1.8 mg/dl) un-
derwent intravenous studies with gadodiamide at a dose of
0.3 mmol/kg [29]. No patient developed clinically significant
kidney dysfunction. The largest increase in serum creatinine
concentration was 0.2 mg/dl.
Lastly, a study published in 2002 prospectively examined
29 patients with chronic kidney disease (mean serum creatin-
ine concentration of 3.6 mg/dl; range, 1.6-7.0 mg/dl) who
received 0.34 mmol/kg (range, 0.23-0.44 mmol/kg) of
gadopenetate dimeglumine [30]. In contrast to other studies,
intravenous saline was employed as Gd-contrast prophy-
laxis. A total of 32 procedures were performed on these
patients. None of the patients developed Gd-contrast neph-
roxicity as defined as an increase in serum creatinine concen-
tration >0.5 mg/dl, over a 3 day period of observation [30].
One patient developed acute kidney injury; however, this
was attributed to renal atheroemboli rather than Gd-contrast
injury.
Gadolinium-Contrast Studies Supporting Nephrotoxicity
In contrast to the prior reports supporting renal safety,
four studies suggest that Gd-contrast agents exhibit variable
degrees of nephrotoxicity (Table 3). An uncontrolled retro-
spective study published in 2003 examined the effect of both
intra-arterial (n=42) and intravenous (n=153) gadopentetate
dimeglumine (1960 mOsm/L) on kidney function in patients
with underlying CKD [31]. The average dose of high osmo-
lality gadopenetate dimeglumine was 0.28 mmol/kg and no
contrast prophylaxis was provided. Patients who received
intravenous and intra-arterial gadopentetate dimeglumine
had mean baseline serum creatinine concentrations of 2.1
mg/dl (estimated CrCl =61 ml/min) and 2.6 mg/dl (esti-
mated CrCl = 40 ml/min), respectively. Contrast-induced
nephropathy, defined as an increase in serum creatinine con-
centration >1.0 mg/dl within 48 hours developed in 3.5%
(7/195) of the entire population: 1.9% (3/153) with intrave-
nous and 9.5% (4/42) with intra-arterial administration. In
the 7 patients who developed nephrotoxicity, the average
baseline serum creatinine concentration was 2.5 mg/dl (esti-
mated CrCl =33 ml/min); 4 had diabetes and 5 hypertension
suggesting that these may be risk factors for Gd-contrast
related nephrotoxicity. Although this study was uncontrolled,
the high rate of acute kidney injury seen in this population
was evidence for Gd-contrast nephrotoxicity. While en-
hanced nephrotoxicity from intra-arterial use of Gd-contrast
is likely, complications (i.e., atheroemboli) from the artery
manipulation by the procedure confounds the study results.
In a prospective study, 21 CKD patients with a serum
creatinine concentration greater than 1.5 mg/dl (eGFR <50
ml/min/m
2
) were randomized to either high dose gadobutrol
(1603 mosm/L, 0.34 to 0.90 mmol/kg) or iohexol (820
mOsm/L iodinated radiocontrast) for digital subtraction an-
giography [32]. Ten patients receiving gadobutrol had a
baseline eGFR of 34 ml/min and 60% had diabetes while the
iohexol group (n =11) had an eGFR of 29 ml/min with 36%
of the patients having diabetes; both groups received intrave-
nous fluids prior to contrast. Contrast-induced nephropathy
(50% decrease in eGFR within 48 hours) developed in 45%
of iohexol patients and 50% of gadobutrol patients; none of
which required renal replacement therapy.
In a retrospective study, 91 patients with CKD stage 3 (n
=50) and 4 (n =41) were examined for nephrotoxicity (in-
crease in serum creatinine concentration of 0.5 mg/dl within
24-72 hours) of Gd-contrast exposure [33]. The patients re-
ceived one of three different Gd-contrast preparations (2 with
high-osmolality, 1 with low-osmolality) at 0.2 mmol/kg.
Contrast prophylaxis was not employed. Approximately 20%
of patients had diabetes and 80% hypertension. Eleven pa-
tients (12.1%) developed contrast-induced nephropathy,
Table 3. Studies Supporting Nephrotoxicity of Gadolinium-Contrast Agents
Author (Year) Study Contrast Agent Dose (mmol/kg) Renal Function ([Cr] in mg/dl) Result
Sam (2003) N =195 with CKD
No control group
CIN >1.0 mg/d at 48 hr with
oligoanuria
Gadopentetate 0.28 CrCl <80 ml/min,
CrCl =38.216 ml/min
CIN: 7/195
MRA: 3/153 (1.9%)
DSA: 4/42 (9.5%)
Erley (2004) Randomized prospective
N =21
CIN >50% decrease in GFR
Gadobutrol =10
Iohexol =11
0.570.17 [Cr] >1.5 or
CrCl <50 ml/min/1.73m
2
CIN:
Gado: 5/10 (50%)
RC: 5/11 (45%)
Briguori (2006) Retrospective, N =25, (historical
controls, N =32)
CIN 0.5 mg/dL within 48 hr or
dialysis within 5 days
Gadodiamide =8
Gadobutrol =17
3: 1 mixture with RC
0.60.3
0.28-1.23
[Cr] >2 mg/dL or
CrCl <40 ml/min
CIN:
Gado: 7/25 (28%)
RC: 2/32 (6.5%)
Ergun (2006) Retrospective, N =91
[Cr] measured pre-Gado, days 1,
3, and 7, and 1 mo,
CIN 0.5 mg/dL within 72 hr
Gadopentetate
Gadodiamide
Dotarem
0.2
Stage 3 and 4 CKD
Mean [Cr] =33 ml/min Range
CrCl =15-58
CIN: 11/91 (12.1%)
CKD Stage 4: 9/11 with
CIN
Abbreviations: CKD, chronic kidney disease; Gado, gadolinium; RC, iodinated radiocontrast; CIN, contrast-induced nephropathy; [Cr], serumcreatinine concentration; MRA, mag-
netic resonance angiography; DSA, digital subtraction angiography; CrCl, creatinine clearance; mo, month; hr, hours; GFR, glomerular filtration rate.
Gadolinium-Contrast and Kidney Disease Current Drug Safety, 2008, Vol. 3, No. 1 71
again suggesting that Gd-contrasts can be nephrotoxic. Six of
these patients had diabetes mellitus and 9 had stage 4 CKD.
The type of Gd-contrast (i.e., high versus low osmolality)
administered to the patients who developed RCIN was not
noted. No patient required renal replacement therapy for
acute kidney injury.
A prospective study in 25 patients with CKD (mean se-
rum creatinine concentration of 2.3 mg/dl) and a matched
historical control (n =32) examined the nephrotoxicity of 2
different Gd-contrast agents administered during cardiac
catheterization (34). Contrast prophylaxis with 0.45% saline
and N-acetylcysteine was provided to all patients. In the Gd-
contrast group, a contrast mixture that contained 0.6
mmol/kg of Gd-contrast and 0.4 ml/kg of iso-osmolar non-
ionic radiocontrast was compared with the same iso-osmolar
radiocontrast agent alone in the historical control group. The
2 contrast protocols are considered equivalent based on the
concept of "X-ray attenuating doses". In the Gd-contrast/iso-
osmolar contrast group, 28% of patients developed an in-
crease in serum creatinine concentration of 0.5 mg/dl within
48 hours as compared with 6.5% in the radiocontrast alone
historical control group [34].
Gadolinium-Contrast Nephrotoxicity: What Should We
Conclude?
Drawing a conclusion from the information reviewed
above is difficult. The majority of studies suggest safety, but
clearly Gd-contrast-induced nephrotoxicity can develop. One
is hampered by data from studies that use variable designs
with small numbers, patients with varying levels of kidney
function, wide ranges of Gd-contrast osmolality and dose,
non-uniform measures of kidney function, erratic use of con-
trast prophylaxis, and poor controls or lack of control groups
altogether. Clearly, better studies are required that employ
adequate numbers of high-risk patients (CKD 3 and 4, dia-
betic nephropathy) and the use of appropriate contrast pro-
phylaxis (intravenous fluids, N-acetylcysteine). That being
said, there appears to be adequate data to suggest that Gd-
contrast agents have enough of a nephrotoxic potential that
caution should be exercised in their use in patients with stage
4/5 CKD, and possibly even more so in patients with ad-
vanced CKD and diabetes. Non-contrast studies (ultrasound,
CO
2
) may be preferred. If this is not possible, it would seem
reasonable to consider some form(s) of contrast prophylaxis
in higher-risk patients receiving Gd-contrasts. Higher doses
(>0.3-0.4 mmol/kg) and arterial injection of Gd-contrast
agents appear to enhance risk. Whether the use of higher
osmolality Gd-contrast agents increase the nephrotoxicity is
uncertain since the nephrotoxic potential of Gd-contrasts at
different osmolalities have not been systematically exam-
ined. Regardless, it is prudent to employ the lowest dose of
Gd-contrast possible to achieve adequate image quality in
higher-risk patients. There is no evidence that these maneu-
vers would be efficacious, but the similarities of Gd-contrast
nephrotoxicity to that of typical iodinated radiocontrast-
induced nephropathy make these suggestions reasonable.
GADOLINIUM-CONTRAST AND NEPHROGENIC
SYSTEMIC FIBROSIS
In 1997, several renal transplant recipients with failed
allografts requiring chronic dialysis (n =9), ESRD patients
on chronic dialysis (n =5), and one patient with AKI were
noted to develop a previously unrecognized fibrosing disor-
der of the skin [7]. This new disease entity was descriptively
coined nephrogenic fibrosing dermopathy (NFD) after de-
tailed examination of the clinical and histopathologic data of
14 cases by Cowper and colleagues [7]. A case control study
of 8 patients with NSF undertaken by the Centers for Disease
Control and Prevention (CDC) and California Department of
Health could not identify a specific etiology or trigger, but
found advanced kidney dysfunction as a common thread.
Following the subsequent recognition that fibrosis also oc-
curred in systemic organs and the role of the circulating fi-
brocyte in the fibrosing reaction, the name was changed to
nephrogenic systemic fibrosis (NSF). This process symmet-
rically affects the extremities more so than the trunk, the face
is always spared. Initial signs and symptoms include sharp
pain and burning associated with redness and swelling of the
skin. These changes progress over a matter of weeks to
months to extensive dermal fibrosis (entire limbs), often pro-
ducing severe joint contractures and marked limitations in
mobility. This may lead to a wheelchair dependent or bed
bound state [6]. Involvement of systemic organs such as the
liver, heart, lungs, diaphragm, esophagus and skeletal muscle
has also been reported and may be associated with fatal con-
sequences [6,7].
Literature Review on the Gadolinium-NSF Link
After the initial report of cases in 2000, the NSF literature
consisted predominantly of case reports/case series with the
cause being ascribed to any of a number of potential agents
or associations. Included were exposure to high-dose
erythropoietin, presence of anti-phospholipid antibodies (and
other hypercoaguable states), vascular injury and vascular
surgical procedures, ischemia, and liver failure (in particular
hepatorenal syndrome and liver transplantation). Despite
this, no unifying agent or risk factor except for underlying
kidney disease was identified. A major breakthrough oc-
curred in 2006 when Grobner reported the development of
NSF in 5 ESRD patients exposed to gadodiamide in the set-
ting of metabolic acidosis [2]. Subsequent to this report, a
number of centers have replicated this association. Marck-
mann and colleagues described 13 patients in Denmark who
developed symptoms of NSF within 2 to 75 days post expo-
sure to gadodiamide [3]. Eight patients had ESRD (one on
peritoneal dialysis), while 5 had advanced (stage 5) CKD not
yet on dialysis. All had courses complicated by vascular in-
jury and none had acidosis. A small case control study from
Connecticut noted NSF in 3 patients exposed to gadolinium
contrast (2 gadodiamide, 1 gadopentetate) demonstrating an
incidence of 4.3 cases per 1000 patient years [35]. This was
associated with an absolute risk of 3.4% for development of
NSF in an exposed patient.
In California, another 12 patients were noted to develop
NSF following gadodiamide exposure (2-11 weeks), with an
odds ratio of 22.3 [4]. Four patients were suffering from
AKI, eight had ESRD on dialysis, and 33% of the patients
had some form of vascular injury. Another 6 patients with
variable levels of kidney disease were described in Texas to
develop NSF following gadodiamide [5]. The onset of symp-
toms ranged form 19 days to 2 months. The CDC published
their findings in MMWR (3/5/07) of a case control study of
72 Current Drug Safety, 2008, Vol. 3, No. 1 Mark A. Perazella
19 patients with confirmed NSF from 2 St. Louis area hospi-
tals [36]. Of these patients, 11 were maintained on hemo-
dialysis, 6 on peritoneal dialysis, and 2 had temporary hemo-
dialysis for AKI. The attack rate for peritoneal dialysis (4.6
cases/100 patients) was much higher than for hemodialysis
(0.61/100 patients), suggesting worse clearance of Gd-
contrast with peritoneal dialysis. The type and dose of Gd-
contrast was not noted, but hypothyroidism, edema and deep
venous thrombosis were significant risk factors for develop-
ment of NSF. In one case; however, they could not document
exposure to Gd-contrast. Physicians from Wisconsin re-
ported another 13 cases of NSF following gadodiamide ad-
ministration noting that an underlying pro-inflammatory state
(major surgery, infection, vascular event or thrombosis) was
an important risk factor [37]. They also confirmed the high
mortality (31%) associated with this disease state. They,
however, incorrectly classified 2 patients with AKI as CKD
stage 3. Most recently, a case control study of 19 patients
with NSF from the Denmark group described that high cu-
mulative gadodiamide dose, elevated serum calcium and
phosphate concentrations and high dose epoietin- (trend)
increase the risk of developing NSF [38]. It is notable that
NSF has been reported in most European countries including
Denmark, United Kingdom, Austria, Belgium, the Nether-
lands, Norway, Sweden, and Switzerland [1,39].
The FDA has also linked NSF to Gd-contrast exposure
and has released two Public Health Advisories, one in 6/06
reporting NSF in 25 ESRD patients after Gd-contrast expo-
sure[10], and an update in 12/06 increasing this number to
90 patients[11]. An NSF registry was created in 2001 to col-
lect data on all cases of NSF [7] and to date greater than 95%
of 239 cases of NSF (where data are available) have been
linked to exposure to gadolinium [25]. Gadodiamide has
been implicated in approximately 85% of these cases and
gadopentetate in 15%. The vast majority of patients that de-
velop NSF are dialysis-dependent (~90%), although it has
also been described in patients with advanced CKD not yet
on dialysis, patients with a poorly functioning renal trans-
plant and those with acute kidney injury [6,7].
Further evidence of the importance of Gd-contrast agents
as a trigger for NSF was provided by documentation of Gd
3+
within the tissues of patients with NSF using scanning elec-
tron microscopy and energy dispersive X-ray spectroscopy
[40,41]. In addition to this qualitative evidence, High and
coworkers quantified the concentration of Gd
3+
in tissues of
the NSF patients previously examined [42]. They found that
the NSF tissues contained 35-150 fold higher amounts (5-
106 parts per million [ppm]) than the tissues of healthy sub-
jects (0.477-1.77 ppm) exposed to Gd-contrast. The authors
speculate that phagocytosis of Gd
3+
retained in tissues by
macrophages results in production of profibrotic cytokines
that eventuate in dermal and/or systemic fibrosis.
Animal Research Examining Gadolinium-NSF Link
An obvious area of research to examine the potential for
gadolinium-contrast agents to promote the development of
NSF is studies in animals. Interestingly, rats exposed to
daily, high dose gadolinium-contrast for 28 days developed
numerous skin lesions that included hair loss, erythema,
thickening, ulceration and crusting. These lesions were at-
tributed to zinc deficiency from transmetalation of zinc by
the gadolinium chelate [22]. Recently, an abstract was pre-
sented at the International Society of Nephrology/World
Congress of Nephrology in Rio de J aniero, Brazil [43]. 40
rats with normal kidney function were exposed to 2 types of
high dose gadolinium (2.5 mmol/kg of either gadodiamide or
gadopentetate), gadodiamide (2.5 mmol/kg) without its ex-
cess sodium caldiamide chelate, or saline control daily for 28
days. Rats exposed to gadodiamide without excess chelate
developed NSF-like skin lesions within 6 days, those ex-
posed to gadodiamide with excess chelate developed NSF-
like skin lesions at 16 days, while the gadopentetate and sa-
line exposed rats did not develop skin lesions. Although
histopathology was note reported, higher gadolinium concen-
trations were found in the tissues of the 2 groups of rats that
developed NSF. This experiment suggests that gadodiamide,
due to the process of transmetalation with release of gadolin-
ium, is more likely to cause NSF than gadopentetate, at least
in rats.
In the 7 published reports (total of 58 patients) where the
specific MR contrast agent was identified, the Gd-contrast
administered was gadodiamide in all but one, which was
gadopentetate [2-5, 36-38]. While the initial inclination is to
ascribe NSF to this particular agent, care must be taken be-
fore gadodiamide is blamed as specifically responsible for
NSF since this agent is one of the more commonly used Gd-
contrasts. In fact, gadodiamide and gadopentetate are the
most commonly used Gd-contrast agents claiming 81% of
the market share for 2006 per the Contrast Media Industry
Guide (CMIG) report. Also, according to the FDA Med-
Watch reporting system, as of 1/07 there have been more
than 100 cases of NSF in which 85 were associated with ex-
posure to gadodiamide (Omniscan), 21 with gadopentetate
(Magnevist), 6 with gadoversetamide (OptiMARK), and one
with gadobenate (MultiHance), although this patient also
received gadodiamide. More recently (3/07), Bayer Health
Care stated that they were aware of 42 cases of NSF associ-
ated with exposure to gadopentetate (Magnevist) [44]. As
noted above, the NSF registry implicates gadodiamide in
approximately 85% of these cases and gadopentetate in 15%
[7]. Each of these NSF associated preparations is a linear
Gd-contrast agent. To date, there are no reports of NSF asso-
ciated with gadoteridol (ProHance), a cyclic Gd-contrast.
Gadodiamide and NSF
If gadodiamide is more likely to cause NSF than the other
Gd-contrast agents, what factors make it unique in this re-
gard? One theory relates to its stability, its ability to bind to
and sequester Gd
+3
. Gadodiamide has the lowest stability
constant and highest dissociation rate of the five Gd-contrast
preparations available in the United States (Table 1). Be-
cause of this decreased stability, the Gd
+3
ion of
gadodiamide
is more likely to dissociate from its stabilizing chelate moi-
ety than other Gd-contrast agents. Because of this fact, ex-
cess chelate (12 mg/ml of sodium calcium diamide) is added
to the commercial formulations of gadodiamide in an attempt
to diminish freely circulating Gd
3+
[14,15]. The stability con-
stant of gadoversetamide is essentially the same as gadodia-
mide, however the excess chelate in this preparation is even
greater at 28.4 mg/ml (sodium calcium versetamide), and is
tempting to use this as an explanation for the decreased cases
of NSF associated with gadoversetamide compared to
Gadolinium-Contrast and Kidney Disease Current Drug Safety, 2008, Vol. 3, No. 1 73
gadodiamide. However, the stability constant of gadopen-
tetate is 1000 times greater than either gadodiamide or gado-
versetamide and this agent is now the second most common
Gd-contrast associated with NSF. This may relate to its more
widespread use, but it still calls into question the concept of
relative toxicity being related to chelate stability. At the pre-
sent time, it is risky to blame this disease on specific agents
and I agree with the FDA [11] that it must be assumed to be
a class effect until more data are available.
The dose of Gd-contrast utilized appears to be impor-
tantly associated with the development of NSF. A typical
non-vascular MRI examination employs 0.1 mmol/kg while
an MRA often utilizes up to 0.3 mmol/kg of Gd-contrast. In
the 5 cases reported from Austria, the dose of Gd-contrast
was approximately 0.26 mmol/kg if one assumes a 70 kg
body weight [2]. The 13 cases reported from Denmark re-
ported an average contrast volume of 18.5 mmol, which
would be 0.26 mmol/kg for a 70 kg individual [3]. Only one
patient received less than a 10 mmol dose. In the study by
Broome, gadodiamide was administered at double dose
(0.2 mmol/kg) in each of the patients in whom NSF subse-
quently developed [4]. During the six-year period of this
report, 559 MRI examinations (301 with gadolinium-contrast
and 258 without contrast) were performed on 168 patients
with advanced kidney disease receiving dialysis. Since there
were no cases of NSF in the patients receiving an MR study
performed without Gd-contrast, the calculated odds ratio for
gadolinium causing NSF was 22.3. Of the 301 MR studies
utilizing Gd-contrast, 207 were performed using a dose of
0.2 mmol/kg while the remaining 94 received 0.1 mmol/kg.
Since none of the cases of NSF occurred in patients receiving
0.1 mmol/l of Gd-contrast, the odds ratio of developing NSF
with the higher dose of Gd-contrast was 12.1 [4]. Review of
all of the published literature generally supports the en-
hanced risk with higher Gd-contrast dose. The NSF registry
also supports this contention as the majority of patients with
NSF were exposed to high doses of and multiple exposures
to Gd-contrast. These data suggest that the risk of NSF is
significantly correlated to the dose of Gd-contrast adminis-
tered and patients would therefore be at much higher risk if
receiving an MRA as opposed to a typical non-vascular MRI
study.
Why should Gd-contrast have the potential to trigger the
development of NSF in patients with underlying kidney dis-
ease? Certainly, reduced kidney function increases the T
1/2
of
Gd-contrast considerably as it is slowly excreted by the kid-
neys in acute kidney injury, advanced stages of chronic kid-
ney disease (CKD stages 4 and 5), and dialysis-dependent
ESRD where it requires three hemodialysis treatments to
remove >95% of the administered dose. Thus, significant
renal impairment is associated with increased time for trans-
metalation and prolonged tissue exposure, which may pro-
mote deposition of toxic Gd
3+
leading to fibrosis. In addition,
the association of higher doses Gd-contrast increasing the
risk of developing NSF also supports this hypothesis as these
higher doses would further increase and prolong tissue expo-
sure in the setting of impaired excretion.
Compared with other conditions and complications that
afflict ESRD patients, NSF appears to be a relatively rare
condition occurring in only 5% of patients receiving
gadodiamide in the report from Denmark [3]. There are nu-
merous patients in the United States alone with ESRD and
advanced CKD, most of which have significant co-
morbidities that require radiographic imaging. It is very
likely that MR studies are commonly used in this population
to assess vascular disease and other end organ pathology. If
therefore seems reasonable to assume that many patients
with advanced kidney disease that have received an MR
study with gadolinium have been spared this abysmal com-
plication. Thus a combination of risk factors or cofactors are
likely required for NSF to occur. Clearly, advanced kidney
disease is a requisite. The dose of Gd-contrast appears to
play a role and the specific Gd-contrast (gadodiamide) util-
ized may also be a factor. All of the published studies and
the data from the NSF registry describe the presence of vas-
cular/endothelial injury (hypercoaguable states, venous
thrombosis, vascular surgery) and perhaps a proinflamma-
tory state (infection, major surgery) in NSF patients. A num-
ber of other cofactors may also be important including meta-
bolic acidosis, intravenous iron dosing, increased serum cal-
cium and phosphate concentrations, and high dose erythro-
poietin, but they are hardly confirmed. Fig. (1) demonstrates
the factors potentially responsible for the development of
NSF following Gd-contrast exposure.
Prevention and Treatment of NSF
Currently, there is no effective therapy for NSF. Physical
therapy plays an important role in increasing and maintaining
the mobility of affected limbs and joints. Renal transplanta-
tion has anecdotally improved or stabilized NSF in patients
who have excellent graft function. Extracorporeal photo-
pheresis has shown some hope while others with variable
response include steroids, pentoxyphylline, plasmapheresis,
and intravenous sodium thiosulfate [45,46]. Since NSF is
still relatively rare and sporadic, none of these maneuvers
have been tested in a controlled clinical trial.
What recommendations can be made regarding the use of
Gd-contrast-based MR studies in high-risk patients? The
vast majority of cases of NSF occur in patients with ESRD
receiving hemodialysis or peritoneal dialysis. However, ap-
proximately 10% of the cases develop in patients with acute
kidney injury (many requiring dialysis), patients with ad-
vanced CKD stage 4 (estimated GFR 15-30 ml/min) and in
patients with CKD stage 5 not receiving renal replacement
therapy (estimated GFR <15 ml/min). Thus, for the time
being, it would seem reasonable to try to avoid administra-
tion of all types of Gd-contrast to patients with these charac-
teristics. This recommendation is even stronger when con-
sidering an MRA in this population, as the higher contrast
dose required with those studies appears to significantly in-
crease the risk of NSF. Alternative imaging modalities (ul-
trasonography, PET scan, CO
2
angiography, MRI without
contrast, CT scan without contrast) should be employed in
these patients whenever possible, including studies using
iodinated radiocontrast when necessary. Using iodinated
radiocontrast in patients with advanced CKD not on dialysis
puts patients at risk for radiocontrast-induced nephropathy
and may tip them over into a situation that may require
temporary or permanent dialysis. Iodinated radiocontrast-
induced nephropathy is more likely to occur than is NSF
induced by Gd-contrast exposure in this group of patients.
However, since radiocontrast-induced nephropathy is poten-
74 Current Drug Safety, 2008, Vol. 3, No. 1 Mark A. Perazella
tially reversible while NSF is not, a Gd-contrast-based study
may be a better choice in this group. If an MR study with
contrast (especially MRA) were felt to be absolutely required
in a patient with ESRD or CKD 4 or 5 not on dialysis, the
lowest possible dose of Gd-contrast should be used and if
feasible, a Gd-contrast other than gadodiamide. Also, until
further data are available on this topic, it would seem prudent
to perform hemodialysis both immediately following, and
again the day after the MR study to accelerate Gd-contrast
elimination, in patients already receiving hemodialysis. This
maneuver should also be entertained for CKD patients (not
currently on chronic dialysis) and patients maintained on
chronic peritoneal dialysis who receive a Gd-contrast (MRA)
study. This is obviously a very inconvenient strategy, but this
aggressive approach underscores the concern over, and un-
certainty surrounding, the development of this devastating
condition. Obviously, these are difficult decisions that can
only be made utilizing input from the physician requesting
the MR study, the nephrologist and the radiologist. There
will be situations that Gd-contrast administration cannot be
avoided in a high-risk patient.
CONCLUSION
In conclusion, Gd-contrast agents can no longer be as-
sumed to be as safe as they have traditionally been consid-
ered when administered to patients with underlying kidney
disease. Although the toxicity profile of the Gd-contrast
agents may be narrower than that associated with iodinated
radiocontrast agents, they are clearly not entirely benign.
Nephrotoxicity can occur in high risk patients who receive a
large dose (>0.3-0.4 mmol/kg) and intra-arterial injection of
Gd-contrast. NSF can be a catastrophic complication of Gd-
contrast exposure and we should make a concerted effort to
avoid this dreaded condition. There is strong evidence that
NSF is related to a tissue response to the toxic effects of
gadolinium. Hopefully, future work in this field will provide
more clearly identifiable risk factors and preventative ma-
neuvers that will allow us to give advice beyond simple
avoidance altogether. This will be important information as
MR Gd-contrast studies play an important role in the diagno-
sis, treatment and follow-up of a vast array of medical condi-
tions in patients with kidney disease.
REFERENCES
[1] Perazella MA, Rodby RA. Gadoliniumuse in patients with kidney
disease: A cause for concern. Semin Dial 2007; 20: 179-84.
[2] Grobner T. Gadolinium-a specific trigger for the development of
nephrogenic fibrosing dermopathy and nephrogenic systemic fibro-
sis? Nephrol Dial Transplant 2006; 21: 1104-08.
[3] Marckmann P, Skov L, Rossen, et al. Nephrogenic systemic fibro-
sis: suspected etiological role of gadodiamide used for contrast-
enhanced magnetic resonance imaging. J Am Soc Nephrol 2006;
17: 2359-62.
[4] Broome DR, Girguis MS, Baron PW, et al. Gadodiamide-
associated nephrogenic systemic fibrosis: Why radiologists should
be concerned. Am J Roentgenol 2007; 188(2): 586-92.
[5] Khurana A, Runge VM, Narayanan M, et al. Nephrogenic systemic
fibrosis: A review of 6 cases temporally related to gadodiamide in-
jection (Omniscan). Invest Radiol 2007; 42: 139-45.
Fig. (1). Speculative mechanism by which gadolinium might trigger nephrogenic systemic fibrosis. In the setting of kidney disease (1), im-
paired renal excretion of high dose gadolinium prolongs the T
1/2
and enhances the chance for dissociation of gadolinium from its chelate (2),
allowing increased tissue exposure. Pro-inflammatory conditions (3), vascular trauma and endothelial dysfunction allows free Gd
3+
to more
easily enter tissues, where macrophages phagocytose the metal and produce local profibrotic cytokines as well as signals that attract circulat-
ing fibrocytes to the tissues. Other co-factors (4), such as increased serum calcium and phosphorus, metabolic acidosis, intravenous iron ther-
apy and high dose intravenous erythropoietin may also enhance the development of NSF through various effects. Once in tissues, circulating
fibrocytes and perhaps Gd
3+
(through direct effects on collagen) induce a fibrosing process that is indistinguishable from normal scar forma-
tion. Abbreviations: Gd
3+
, gadolinium; cyto, cytokines; cF, circulating fibrocyte.
Gadolinium-Contrast and Kidney Disease Current Drug Safety, 2008, Vol. 3, No. 1 75
[6] Galan A, Cowper SE, Bucala R. Nephrogenic systemic fibrosis
(nephrogenic fibrosing dermopathy). Curr Opin Rheumatol 2006;
18(6): 614-17.
[7] Cowper SE. Nephrogenic Fibrosing Dermopathy [NFD/NSF Web-
site]. 2001-2007. Available at http: //www.icnfdr.org Accessed
6/1/2007.
[8] Thomsen HS, Morcos SK, Dawson P. Is there a causal relation
between the administration of gadolinium based contrast media and
the development of nephrogenic systemic fibrosis. Clin Radiol
2006; 61: 905-06.
[9] Thomsen HS. Nephrogenic systemic fibrosis: a serious late adverse
reaction to gadodiamide. Eur Radiol 2006; 16: 2619-21.
[10] Food and Drug Administration (2006) Public Health Advisory:
Gadolinium-containing contrast agents for magnetic resonance im-
aging (MRI). http: //www.fda.gov/cder/drug/advisory/gadolinium_
agents.htm.
[11] Food and Drug Administration (2006) Public Health Advisory:
Gadolinium-containing contrast agents for magnetic resonance im-
aging (MRI). http: //www.fda.gov/cder/drug/advisory/gadolinium_
agents_20061222.htm
[12] Perazella MA. Nephrogenic systemic fibrosis, gadolinium, and
chronic kidney disease: Is there a link? Clin J Am Soc Nephrol
2007; 2: 200-02.
[13] Bellin MF. MR contrast agents, the old and the new. Eur J Radiol
2006; 60: 314-23.
[14] Lorusso V, Pascolo L, Fernetti C, et al. Magnetic resonance con-
trast agents: from the bench to the patient. Curr Pharm Des 2005;
11: 4079-4098.
[15] Runge VM. Safety of magnetic resonance contrast media. Top
Magn Reson Imag 2001; 12(4): 309-14.
[16] Swan SK, Lambrecht LJ , Townsend R, et al. Safety and pharma-
cokinetic profile of gadobenate dimeglumine in subjects with renal
impairment. Invest Radiol 1999; 34(7): 443-55.
[17] Reinton V, Berg KJ , Svaland MG, et al. Pharmacokinetics of
gadodiamide injection in patients with moderately impaired renal
function. Acta Radiol 1994; 1: 56-61.
[18] Schuhmann-Giampieri G, Krestin G. Pharmacokinetics of Gd-
DTPA in patients with chronic renal failure. Invest Radiol 1991;
11: 975-79.
[19] J offe P, Thomsen HS, Meusel M. Pharmacokinetics of gadodia-
mide injection in patients with severe renal insufficiency and pa-
tients undergoing hemodialysis or continuous ambulatory perito-
neal dialysis. Acta Radiol 1998; 5: 491-502.
[20] Saitoh T, Hayasaka K, Tanaka Y, et al. Dialyzability of gadodia-
mide in hemodialysis patients. Radiat Med 2006; 24: 445-51.
[21] Okada S, Katagirir K, Kumazaki T, et al. Safety of gadolinium
contrast agent in hemodialysis patients. Acta Radiol 2001; 42: 339-
41.
[22] Wible J H, Troup CM, Hynes MR, et al. Toxicological assessment
of gadoversetamide injection (OptiMARK), a new contrast-
enhancement agent for use in magnetic resonance imaging. Invest
Radiol 2001; 36: 401-12.
[23] Niendorf HP, Alhassan A, Haustein J , Clauss W, Cornelius I.
Safety and risk of gadolinium-DTPA: extended clinical experience
after more than 5,000,000 applications. Adv MRI Contrast 1993; 2:
12-19.
[24] Bellin MF, Deray G, Assogba U, et al. Gd-DOTA: evaluation of its
renal tolerance in patients with chronic renal failure. Magn Reson
Imaging 1992; 10: 115-18.
[25] Prince MR, Arnoldus C, Friscoli J K. Nephrotoxicity of high-dose
gadolinium compared with iodinated contrast. J Magn Reson Imag-
ing 1996; 6 (1): 162-66.
[26] Hammer FD, Goffette PP, Malaise J , Mathurin P. Gadolinium
dimeglumine: An alternative contrast agent for digital subtraction
angiography. Eur Radiol 1999; 9(1): 128-36.
[27] Spinosa DJ , Angle J F, Hagspiel KD, et al. Lower extremity arteri-
ography with use of iodinated contrast material or gadodiamide to
supplement CO2 angiography in patients with renal insufficiency. J
Vasc Interv Radiol 2000; 11(1): 35-43.
[28] Spinosa DJ , Matsumoto AH, Angle J F, et al. Safety of CO2- and
gadodiamide-enhanced angiography for the evaluation and percu-
tanwous treatment of renal artery stenosis in patients with chronic
renal insufficiency. Am J Roentgenol 2001; 176(5): 1305-11.
[29] Sancak T, Bilgic S, Sanldilek U. Gadodiamide as an alternative
contrast agent in intravenous digital subtraction angiography and
interventional procedures of the upper extremity veins. Cardiovasc
Intervent Radiol 2002; 25(1): 49-52.
[30] Reiger J , Sitter T, Toepfer M, Linsenmaier U, Pfeofer KJ , Schiffl
H. Gadolinium as an alternative contrast agent for diagnostic and
interventional angiographic procedures in patients with impaired
renal function. Nephrol Dial Transplant 2002; 17: 824-28.
[31] Sam AD, Morasch MD, Collins J , et al. Safety of gadolinium con-
trast angiography in patients with chronic renal insufficiency. J
Vasc Surg 2003; 38: 313-18.
[32] Erley CM, Bader BD, Berger ED. Gadolinium-based contrast me-
dia compared with iodinated media for digital subtraction angi-
ography in azotemic patients. Nephrol Dial Transplant 2004; 19:
2526-2531.
[33] Ergun I, Keven K, Uruc I, et al. The safety of gadoliniumin pa-
tients with stage 3 and 4 renal failure. Nephrol Dial Transplant
2006; 21: 697-700.
[34] Briguori C, Colombo A, Airoldi F, et al. Gadolinium-based con-
trast agents and nephrotoxicity in patients undergoing coronary ar-
tery procedures. Catheter Cardiovasc Interv 2006; 67: 175-80.
[35] Deo A, Fogel M, Cowper SE. Nephrogenic systemic fibrosis: A
population study eaxmining the relationship of disease develop-
ment to gadolinium exposure. Clin J Am Soc Nephrol 2007; 2: 264-
67.
[36] Nephrogenic fibrosing dermopathy associated with exposure to
gadolinium-containing contrast agents-St. Louis, Missouri, 2002-
2006. Morb Mortal Wkly Rep 2007; 56 (7): 137-41.
[37] Sadowski EA, Bennett LK, Chan MR, et al. Nephrogenic systemic
fibrosis: Risk factors and incidence estimation. Radiology 2007;
243: 148-57.
[38] Marckmann P, Skov L, Rossen K, Heaf J , Thomsen HS. Case-
control study of gadodiamide-related nephrogenic systemic fibro-
sis. Nephrol Dial Transplant 2007; Epub doi: 10/1093.
[39] Personal communication, Henrik S. Thomsen, Department of Diag-
nostic Radiology, Copenhagen University, Denmark.
[40] High WA, Ayers RA, Chandler J , et al. Gadolinium is detectable
within the tissue of patients with nephrogenic systemic fibrosis. J
Am Acad Dermatol 2007; 56: 21-26.
[41] Boyd AC, Zic J A, Abraham J L. Gadolinium deposition in nephro-
genic fibrosing dermopathy. J Am Acad Dermatol 2007; 56; 27-30.
[42] High WA, Eng M, Ayers RA, Cowper, SE. Gadolinium is quantifi-
able within the tissue of patients with nephrogenic systemic fibro-
sis. J Am Acad Dermatol 2007; 56: 1-2.
[43] Peitsch H, Sieber M, Frenzel T, Weinmann H. Nephrogenic sys-
temic fibrosis: Are gadolinium-based MRI contrast agents a possi-
ble trigger? Poster presentation World Congress of Nephrol-
ogy/International Society of Nephrology, Rio de J aniero, Brazil,
2007.
[44] Magnevist Safety Information: NSF/NFD Update. Available at
http: //www.imaging.bayerhealthcare.com/html/magnevist/nsf_nfd.
html?WT.mc_id=berleximaging.com.
[45] Yerram P, Saab G, Karuparthi P, et al. Nephrogenic systemic fibro-
sis: A mysterious disease in patients with renal failure-role of gado-
linium-based contrast media in causation and the beneficial effect
of intravenous sodiumthiosulfate. Clin J Am Soc Nephrol 2007; 2:
258-63.
[46] Gilliet M, Cozzio A, Burg G, et al. Successful treatment of three
cases of nephrogenic fibrosing dermopathy with extracorporeal
photopheresis. Br J Dermatol 2005; 152: 531-36.
Received: J une 1, 2007 Revised: J uly 10, 2007 Accepted: J uly 11, 2007
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Operation Manual - IDU - FXFQ-PVEDocumento5 páginasOperation Manual - IDU - FXFQ-PVEJM ArcillaAinda não há avaliações
- AC178 InterimCriteriaforInspectionandVerificationofConcreteandReinforcedandUnreinforcedMasonryusingFRPDocumento7 páginasAC178 InterimCriteriaforInspectionandVerificationofConcreteandReinforcedandUnreinforcedMasonryusingFRPBayram AygunAinda não há avaliações
- Excel Meracik Nutrisi Bandung 11 Feb 2018Documento30 páginasExcel Meracik Nutrisi Bandung 11 Feb 2018Ariev WahyuAinda não há avaliações
- Welcome To MY Presentation: Advanced Dyeing & PrintingDocumento26 páginasWelcome To MY Presentation: Advanced Dyeing & PrintingShumi NaharAinda não há avaliações
- Project Work Chem1Documento15 páginasProject Work Chem1UMESH BIKRAM SHAHAinda não há avaliações
- Lab ReportDocumento8 páginasLab ReportHenrique PradoAinda não há avaliações
- Yellow Passion Fruits Headspace Werkhoff1998Documento18 páginasYellow Passion Fruits Headspace Werkhoff1998mapollo2000Ainda não há avaliações
- MelamineDocumento18 páginasMelamineSurjendu MaityAinda não há avaliações
- Chemical Exergy Calculation CharpterDocumento10 páginasChemical Exergy Calculation CharpterFernanda PerezAinda não há avaliações
- Product Data Sheet Metco 9MBM / 9MBH Plasma Spray GunDocumento4 páginasProduct Data Sheet Metco 9MBM / 9MBH Plasma Spray GunMuhammad ZulfaqarAinda não há avaliações
- Swing Arm Calculation and Analysis JournalDocumento5 páginasSwing Arm Calculation and Analysis JournalBálají SèlvakümárAinda não há avaliações
- Basic Dental PharmacologyDocumento152 páginasBasic Dental PharmacologyDr-Mohamed KandeelAinda não há avaliações
- Aci y Sus NormasDocumento14 páginasAci y Sus NormasJUAN AGUILARAinda não há avaliações
- There Are Three Main Groups of Resin:: Polyester ResinsDocumento1 páginaThere Are Three Main Groups of Resin:: Polyester ResinsmukeshAinda não há avaliações
- Bondstrand™ LD Series: ApplicationsDocumento4 páginasBondstrand™ LD Series: ApplicationsMathan KumarAinda não há avaliações
- Question Paper SSC 32Documento18 páginasQuestion Paper SSC 32Tarun BediAinda não há avaliações
- Aspen Internet Process Manual2006 - 5-Usr PDFDocumento18 páginasAspen Internet Process Manual2006 - 5-Usr PDFBabak Mirfendereski100% (1)
- Welding Metallurgy - Unit 12 - WEEK 11 PDFDocumento3 páginasWelding Metallurgy - Unit 12 - WEEK 11 PDFDilipAinda não há avaliações
- Sunscreen-1Documento14 páginasSunscreen-1faikaAinda não há avaliações
- Copper Accelerated Salt Spray (CASS) and Salt Spray Test For Gardobond X 4707 A2Documento15 páginasCopper Accelerated Salt Spray (CASS) and Salt Spray Test For Gardobond X 4707 A2Tito Tamaro PasaribuAinda não há avaliações
- Duhok Polytechnic University: Unit Operation Laboratory of Unit OperationDocumento7 páginasDuhok Polytechnic University: Unit Operation Laboratory of Unit OperationMUHAMMAD AKRAMAinda não há avaliações
- Lab 7 - BioeactorDocumento43 páginasLab 7 - Bioeactornur athilahAinda não há avaliações
- United States Patent (10) Patent No.: US 7,806,945 B2: The To In... TDocumento21 páginasUnited States Patent (10) Patent No.: US 7,806,945 B2: The To In... TesiAinda não há avaliações
- Diatomite Supported by CaO:MgO Nanocomposite As Heterogeneous Catalyst For Biodiesel Production From Waste Cooking OilDocumento8 páginasDiatomite Supported by CaO:MgO Nanocomposite As Heterogeneous Catalyst For Biodiesel Production From Waste Cooking Oilnajiha_tahirAinda não há avaliações
- Experiment 08 To Determine Deflection Components of A Semi-Circular Bar Subjected To Diametrical LoadingDocumento7 páginasExperiment 08 To Determine Deflection Components of A Semi-Circular Bar Subjected To Diametrical LoadingKhurram SattarAinda não há avaliações
- Chemistry ReviewerDocumento14 páginasChemistry ReviewerJaliesa Ann ValdezAinda não há avaliações
- Class 12 Important QuestionsDocumento4 páginasClass 12 Important Questionsmisraadyasha6Ainda não há avaliações
- AAMA 620-02 Voluntary Specfications For High Performance...Documento9 páginasAAMA 620-02 Voluntary Specfications For High Performance...zaheerahmed77Ainda não há avaliações
- Durometer Types & Specifications: Type Model No. Force Indenter Description ApplicationsDocumento2 páginasDurometer Types & Specifications: Type Model No. Force Indenter Description ApplicationsDarwin_Sidney100% (1)
- Paper Industry Case Study PDFDocumento4 páginasPaper Industry Case Study PDFanitha venkatAinda não há avaliações