Escolar Documentos
Profissional Documentos
Cultura Documentos
Boffetta Epidemiology 2004
Enviado por
Bruno ThiemeDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Boffetta Epidemiology 2004
Enviado por
Bruno ThiemeDireitos autorais:
Formatos disponíveis
Epidemiology of environmental and occupational cancer
Paolo Boffetta*
,1,2
1
International Agency for Research on Cancer, 150 cours Albert-Thomas, 69008 Lyon, France;
2
German Cancer Research Centre,
69120 Heidelberg, Germany
Environmental carcinogens, in a strict sense, include
outdoor and indoor air pollutants, as well as soil and
drinking water contaminants. An increased risk of
mesothelioma has consistently been detected among
individuals experiencing residential exposure to asbestos,
while results for lung cancer are less consistent. Several
good-quality studies have investigated lung cancer risk
from outdoor air pollution based on measurement of
specic agents. Their results tend to show an increased
risk in the categories at highest exposure, with relative
risks in the range 1.5. A causal association has been
established between exposure to environmental tobacco
smoke and lung cancer, with a relative risk in the order of
1.2. Radon is another carcinogen present in indoor air,
with a relative risk in the order of 1.06 for exposure at
100 Bq/m
3
. In several Asian populations, an increased risk
of lung cancer results among women from indoor pollution
from cooking and heating. There is strong evidence of an
increased risk of bladder, skin and lung cancers following
consumption of water with high arsenic contamination;
results for other drinking water contaminants, including
chlorination by-products, are inconclusive. A total of 29
occupational agents are established human carcinogens,
and another 30 agents are suspected carcinogens. In
addition, at least 12 exposure circumstances entail
exposure to carcinogens. Exposure is still widespread for
many important occupational carcinogens, such as asbes-
tos, coal tar, arsenic and silica, in particular in developing
countries. Although estimates of the global burden of
occupational and environmental cancer result in gures in
the order of 2% and less than 1%, respectively, these
cancers concentrate in subgroups of the population;
furthermore, exposure is involuntary and can, to a large
extent, be avoided.
Oncogene (2004) 23, 63926403. doi:10.1038/sj.onc.1207715
Keywords: air pollution; arsenic; environment; environ-
mental tobacco smoke; neoplasms; occupation; radon
Introduction
The concept of environment is often used with a broad
scope in the medical literature, including all nongenetic
factors such as diet, lifestyle and infectious agents. In
this broad sense, the environment is implicated in the
causation of the majority of human cancers (Tomatis
et al., 1990). In a more specic sense, however,
environmental factors include only the (natural or
man-made) agents encountered by humans in their
daily life, upon which they have no or limited personal
control. The most important environmental exposures,
dened in this strict sense, include outdoor and
indoor air pollution and soil and drinking water
contamination. Most environmental carcinogens occur
at higher concentrations in the workplace: since the
report of scrotal cancer among chimney sweeps by Pott
(1775), occupational cancer research has played a
pivotal role in the elucidation of environmental causes
of human cancer. Furthermore, control of occupational
exposure circumstances has proven to be feasible and
effective as compared to other cancer preventive
measures.
In the following sections the evidence linking ex-
posure to selected environmental factors and risk of
cancer will be reviewed, followed by a summary of
current knowledge on occupational carcinogens. Agents
whose exposure depends on lifestyle, such as solar
radiation and food additives, will not be considered, nor
agents occurring in the environment as a consequence of
accidents or warfare.
Environmental cancer
Cancer risk from environmental exposure to asbestos
Asbestos and asbestiform bres are naturally occurring
brous silicates with an important commercial use,
mainly in acoustical and thermal insulation. They can be
divided into two groups: chrysotile and the group of
amphiboles, including amosite, crocidolite, anthophyl-
lite, actinolite and tremolite bres. Chrysotile is the most
widely used type of asbestos. Although all types are
carcinogenic to the lung and mesothelioma, the biolo-
gical effects of amphiboles on the pleura and peritoneum
seem to be stronger than those of chrysotile (INSERM,
1997). The use of asbestos has been restricted or banned
in many countries.
In contrast to the many epidemiological studies
available on asbestos-exposed workers, there are few
studies on the health effects of nonoccupational (house-
hold and residential) exposure to asbestos. One type of
household exposure concerns cohabitants of asbestos *Correspondence: P Boffetta; E-mail: boffetta@iarc.fr
Oncogene (2004) 23, 63926403
& 2004 Nature Publishing Group All rights reserved 0950-9232/04 $30.00
www.nature.com/onc
workers and arises from dust brought home on clothes.
Other household sources of asbestos exposure are
represented by the installation, degradation, removal
and repair of asbestos-containing products. Residential
exposure mainly results from outdoor pollution related
to asbestos mining or manufacturing, in addition to
natural exposure from the erosion of asbestos or
asbestiform rocks. The assessment of nonoccupational
exposure to asbestos presents difculties, since levels are
generally low, and the duration and frequency of
exposure and the type of bre are seldom known with
precision.
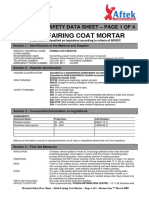
Table 1 summarizes the results of studies on risk of
pleural mesothelioma and lung cancer from environ-
mental (residential) exposure to asbestos. Studies were
available from various countries and, in most cases,
exposure was dened as residence near a mine or
another major source of asbestos exposure. A potential
limitation of these studies, in particular those without
assessments of exposure at the individual level (ecolo-
gical studies), is possible concomitant occupational or
household exposure to asbestos. The risk of mesothe-
lioma was greatly increased in all but one study among
individuals with environmental exposure to asbestos.
Results for lung cancer, however, are less consistent,
with an increased risk detected in studies from South
Africa and China, but not in studies from Europe and
North America. Imperfect control of confounding by
smoking and other lung carcinogens may explain the
lack of consistency.
Cancer risk from outdoor air pollution
Air pollution is a complex mixture of different gaseous
and particulate components, whose composition varies
greatly by locality and time. In recent decades, emissions
and air concentrations of traditional industrial air
pollutants, such as SO
2
and smoke particles, have
decreased, whereas there is an increasing or continued
problem with air pollution from vehicles, with emissions
of engine combustion products including volatile
organic compounds, nitrogen oxides and ne particu-
lates, as well as with secondarily increased ozone levels.
There is biological rationale for a carcinogenic potential
of numerous components of the air pollution mix,
including benzo[a]pyrene, benzene, some metals, parti-
cles (especially ne particles) and possibly ozone.
Many denitions of outdoor air pollution exposure
have been used in epidemiological studies. Earlier
analytical studies generally compared residence in urban
areas, where the air is considered more polluted, to
residence in rural areas, sometimes providing limited
data on the typical levels of some pollutants in the areas
studied. Other studies have attempted to address
exposure to specic components of outdoor air, provid-
ing risk estimates in relation to quantitative or
semiquantitative air pollution exposure assessments
(Hitosugi, 1968; Vena, 1982; Brownson et al., 1987;
Jedrychowski et al., 1990; Katsouyanni et al., 1991;
Mills et al., 1991; Jo ckel et al., 1992; Dockery et al.,
1993; Barbone et al., 1995; Pope et al., 1995; Zaridze
T
a
b
l
e
1
S
t
u
d
i
e
s
o
f
r
i
s
k
o
f
m
e
s
o
t
h
e
l
i
o
m
a
a
n
d
l
u
n
g
c
a
n
c
e
r
f
r
o
m
e
n
v
i
r
o
n
m
e
n
t
a
l
e
x
p
o
s
u
r
e
t
o
a
s
b
e
s
t
o
s
C
o
u
n
t
r
y
S
D
T
F
S
o
u
r
c
e
o
f
e
x
p
o
s
u
r
e
M
e
s
o
t
h
e
l
i
o
m
a
L
u
n
g
c
a
n
c
e
r
R
e
f
e
r
e
n
c
e
C
a
R
R
9
5
%
C
I
C
a
R
R
9
5
%
C
I
S
o
u
t
h
A
f
r
i
c
a
E
A
R
e
s
.
i
n
m
i
n
i
n
g
a
r
e
a
6
1
8
.
7
6
.
7
1
1
.
4
8
6
1
.
7
1
.
2
2
.
5
B
o
t
h
a
e
t
a
l
.
(
1
9
8
6
)
a
S
o
u
t
h
A
f
r
i
c
a
C
C
A
R
e
s
.
i
n
m
i
n
i
n
g
a
r
e
a
s
1
6
3
.
6
1
.
4
9
.
3
M
z
i
l
e
n
i
e
t
a
l
.
(
1
9
9
9
)
a
C
a
n
a
d
a
C
o
C
R
e
s
.
i
n
m
i
n
i
n
g
a
r
e
a
7
1
.
3
0
.
5
3
.
0
T
h
e
r
i
a
u
l
t
a
n
d
G
r
a
n
d
-
B
o
i
s
(
1
9
7
8
)
a
C
a
n
a
d
a
E
c
C
R
e
s
.
i
n
m
i
n
i
n
g
a
r
e
a
7
7
.
6
3
.
4
1
4
.
9
7
1
1
.
1
0
.
9
1
.
4
C
a
m
u
s
e
t
a
l
.
(
1
9
9
8
)
b
U
S
A
C
C
A
R
e
s
.
n
e
a
r
t
o
a
s
b
e
s
t
o
s
p
l
a
n
t
4
1
0
.
9
0
.
6
1
.
3
H
a
m
m
o
n
d
e
t
a
l
.
(
1
9
7
9
)
A
u
s
t
r
i
a
E
c
A
R
e
s
.
i
n
p
o
l
l
u
t
e
d
t
o
w
n
3
6
0
.
8
0
.
4
1
.
6
N
e
u
b
e
r
g
e
r
e
t
a
l
.
(
1
9
8
4
)
a
I
t
a
l
y
C
o
U
M
R
e
s
.
o
1
k
m
f
r
o
m
a
s
b
e
s
t
o
s
c
e
m
e
n
t
p
l
a
n
t
3
6
6
.
6
4
.
1
1
1
M
a
g
n
a
n
i
e
t
a
l
.
(
1
9
9
5
)
a
I
t
a
l
y
C
C
U
M
R
e
s
.
i
n
p
o
l
l
u
t
e
d
c
i
t
y
3
2
1
4
.
6
4
.
9
4
3
.
1
M
a
g
n
a
n
i
e
t
a
l
.
(
2
0
0
1
)
a
I
t
a
l
y
,
S
p
a
i
n
,
S
w
i
t
z
e
r
l
a
n
d
C
C
U
M
R
e
s
.
o
2
k
m
f
r
o
m
p
o
t
e
n
t
i
a
l
s
o
u
r
c
e
1
7
1
1
.
5
3
.
5
3
8
.
2
M
a
g
n
a
n
i
e
t
a
l
.
(
2
0
0
0
)
U
K
C
C
A
R
e
s
.
o
0
.
5
m
i
l
e
s
f
r
o
m
a
s
b
e
s
t
o
s
f
a
c
t
o
r
y
1
1
5
.
4
1
.
8
1
7
N
e
w
h
o
u
s
e
a
n
d
T
h
o
m
p
s
o
n
(
1
9
6
5
)
U
K
C
C
A
R
e
s
.
o
0
.
5
k
m
f
r
o
m
p
o
t
e
n
t
i
a
l
s
o
u
r
c
e
5
6
.
6
0
.
9
5
0
H
o
w
e
l
e
t
a
l
.
(
1
9
9
7
)
C
h
i
n
a
C
C
C
R
e
s
.
4
2
0
y
e
a
r
s
o
0
.
2
k
m
f
r
o
m
a
s
b
e
s
t
o
s
p
l
a
n
t
4
7
1
.
9
0
.
5
6
.
4
X
u
e
t
a
l
.
(
1
9
8
9
)
a
C
h
i
n
a
C
o
A
R
e
s
.
i
n
p
o
l
l
u
t
e
d
a
r
e
a
N
A
1
8
2
N
A
N
A
5
.
7
N
A
L
u
o
e
t
a
l
.
(
1
9
9
8
)
N
e
w
C
a
l
e
d
o
n
i
a
C
C
A
U
s
e
o
f
c
o
n
t
a
m
i
n
a
t
e
d
b
u
i
l
d
i
n
g
m
a
t
e
r
i
a
l
s
1
4
4
0
.
9
5
.
1
3
2
5
5
6
0
.
9
0
.
6
1
.
3
L
u
c
e
e
t
a
l
.
,
(
2
0
0
0
)
a
A
u
s
t
r
a
l
i
a
C
C
A
R
e
s
.
4
5
y
e
a
r
s
i
n
m
i
n
i
n
g
a
r
e
a
c
1
4
6
.
7
2
.
0
2
2
.
2
H
a
n
s
e
n
e
t
a
l
.
(
1
9
9
8
)
S
D
s
t
u
d
y
d
e
s
i
g
n
:
C
C
c
a
s
e
c
o
n
t
r
o
l
s
t
u
d
y
;
C
o
c
o
h
o
r
t
s
t
u
d
y
;
E
c
e
c
o
l
o
g
i
c
a
l
s
t
u
d
y
;
T
F
p
r
e
d
o
m
i
n
a
n
t
t
y
p
e
o
f
b
r
e
:
A
a
m
p
h
i
b
o
l
e
s
;
C
c
h
r
y
s
o
t
i
l
e
;
U
M
u
n
s
p
e
c
i
e
d
a
n
d
m
i
x
e
d
;
R
e
s
.
r
e
s
i
d
e
n
c
e
;
C
a
n
u
m
b
e
r
o
f
e
x
p
o
s
e
d
c
a
s
e
s
;
R
R
r
e
l
a
t
i
v
e
r
i
s
k
;
C
I
c
o
n
d
e
n
c
e
i
n
t
e
r
v
a
l
.
a
R
e
s
u
l
t
s
d
e
r
i
v
e
d
f
r
o
m
r
a
w
d
a
t
a
r
e
p
o
r
t
e
d
i
n
t
h
e
p
u
b
l
i
c
a
t
i
o
n
.
b
W
o
m
e
n
o
n
l
y
.
c
C
o
m
p
a
r
e
d
t
o
r
e
s
i
d
e
n
c
e
o
1
y
e
a
r
Environmental and occupational cancer
P Boffetta
6393
Oncogene
et al., 1995; Biggeri et al., 1996; Pawlega et al., 1997;
Abbey et al., 1999) or, in some cases, to more qualitative
exposure assessments (Pike et al., 1979; Xu et al., 1989).
Another type of study has addressed residence in the
proximity of specic sources of pollution, such as major
industrial emission sources or heavy road trafc.
Several cohort and casecontrol studies of outdoor air
pollution have been reported (Stocks and Campbell,
1955; Hammond and Horn, 1958a/b; Haenszel et al.,
1962; Haenszel and Taeuber, 1964; Dean, 1966; Buell
and Dunn, 1967; Buell et al., 1967; Hitosugi, 1968;
Hammond, 1972; Cederlo f et al., 1975; Dean et al.,
1977, 1978; Pike et al., 1979; Hammond and Garnkel,
1980; Doll and Peto, 1981; Vena, 1982; Tenkanen et al.,
1985; Brownson et al., 1987; Samet et al., 1987;
Tenkanen and Teppo, 1987; Xu et al., 1989; Jedry-
chowski et al., 1990; Holowaty et al., 1991; Katsouyanni
et al., 1991; Mills et al., 1991; Jo ckel et al., 1992;
Dockery et al., 1993; Tenkanen, 1993; Barbone et al.,
1995; Pope et al., 1995; Zaridze et al., 1995; Biggeri et al.,
1996; Engholm et al., 1996; Pawlega et al., 1997; Beeson
et al., 1998; Abbey et al., 1999; McDonnell et al., 2000;
Nyberg et al., 2000; Hoek et al., 2002; Pope et al., 2002).
Overall, the studies suggest relative risks (RRs) of up to
about 1.5 for urban vs rural residence or high vs low
estimated air pollution exposure. There is no clear
indication if early or late exposure is more important,
and data on possible interaction with smoking or
occupational exposures are inadequate. Among these
studies, four cohort (Mills et al., 1991; Dockery et al.,
1993; Pope et al., 1995, 2002; Abbey et al., 1999;
McDonnell et al., 2000; Hoek et al., 2002) and 10 case
control (Hitosugi, 1968; Vena, 1982; Brownson et al.,
1987; Jedrychowski et al., 1990; Katsouyanni et al.,
1991; Jo ckel et al., 1992; Barbone et al., 1995; Zaridze
et al., 1995; Pawlega et al., 1997; Nyberg et al., 2000)
studies were based on measurements of specic air
components. Selected results from these studies, with the
corresponding air pollution differentials, are presented
in Table 2: they tend to show an increased risk of lung
cancer in the categories at highest exposure, which does
not seem to be attributable to confounding factors. The
studies of lung cancer and air pollution, however, suffer
exposure misclassication, including dilution of the
sufciently exposed population by a considerable
number of minimally exposed persons.
To pinpoint possible industrial emissions responsible
for the suggested urban excess, populations living near
point sources of air pollution have also been studied.
Increased risks have been reported for living close to
industries such as smelters, foundries, chemical indus-
tries, and others with various emissions (Lloyd, 1978;
Shear et al., 1980; Gailey and Lloyd, 1983; Lloyd et al.,
1985a/b, 1986; Gailey and Lloyd, 1986; Smith et al.,
1987; Williams and Lloyd, 1988; Xu et al., 1989;
Barbone et al., 1995; Zaridze et al., 1995; Ko et al.,
1997; Bhopal et al., 1998; Petrauskaite et al., 2002).
Results of these studies were inconsistent, and con-
dence intervals of risk estimates were mostly wide.
A number of studies concern sources of inorganic
arsenic in air. Ecological studies suggested an increased
lung cancer risk (Blot and Fraumeni, 1975; Newman
et al., 1976; Pershagen et al., 1977; Matanoski et al.,
1981; Cordier et al., 1983; Xiao and Xu, 1985), which
was conrmed by some (Brown et al., 1984; Pershagen,
1985; Frost et al., 1987) but not all (Lyon et al., 1977;
Greaves et al., 1981; Rom et al., 1982; Marsh et al.,
1997, 1998) subsequent studies with individual informa-
tion on exposure: arsenic exposure level in some of these
studies, however, was likely to be low.
Limited results are available for cancers other than
the lung. In ecological studies, many individual cancers
have shown elevated urban/rural ratios, including
cancers of the mouth and throat, nasopharynx, oeso-
phagus, stomach, colon, rectum, larynx, female breast,
bladder and prostate (Levin et al., 1960; Goldsmith,
1980). Residual confounding by smoking or occupa-
tional exposures may be involved. Other ecological
studies have related cancer rates to air pollutant
measurements, or emission indexes or gures for fuel
consumption. For example, an ecological study in 19
European countries found an inverse temporal associa-
tion between gasoline use and leukaemia mortality or
morbidity, but a weak positive spatial association
(Swaen and Slangen, 1995).
Overall, the evidence for an increased lung cancer risk
from outdoor air pollution is quite strong, although
methodological problems in the available studies cau-
tion against a nal conclusion, while the evidence
concerning cancers other than lung cancer, including
childhood cancer, is not consistent, and is insufcient to
draw any conclusion on the presence or absence of a
causal association.
Cancer risk from exposure to environmental tobacco
smoke
Environmental tobacco smoke is composed of side-
stream and mainstream smoke, in which known,
probable or possible human carcinogens are present.
The International Agency for Research on Cancer
(IARC) has evaluated the evidence of a carcinogenic
risk from exposure to environmental tobacco smoke,
and has classied it as an established human carcinogen
(IARC, 2004). Confounding by dietary, occupational
and social class-related factors can be reasonably
excluded, and bias from misclassication of smokers is
not likely to explain the results. On that occasion, a
meta-analysis of epidemiological studies of lung cancer
and adult exposure to environmental tobacco smoke
was conducted, resulting in RRs of 1.22 (95% CI 1.12
1.32) in women and 1.36 (95% CI 1.021.82) in men
from spousal exposure, and of 1.15 (95% CI 1.051.26)
in women and 1.28 (95% CI 0.881.84) in men from
workplace exposure. Other meta-analyses have reached
very similar conclusions (Hackshaw et al., 1997;
Boffetta, 2002).
The evidence of a causal association between
environmental tobacco smoke exposure and cancers
in organs other than the lung is inconclusive (IARC,
2004).
Environmental and occupational cancer
P Boffetta
6394
Oncogene
Table 2 Relative risk of lung cancer and outdoor air pollution measurements in some studies with quantitative or semiquantitative exposure assessment
Location, study period, ref. Sex RR 95% CI Exposure contrast
a
Basis for exposure assessment for
individuals and/or areas
Comments
Cohort studies
USA, 19751991, Dockery
et al. (1993)
M+F 1.37 0.812.31 Per 18.9 mg/m
3
PM
2.5
City of residence in 1975. Pollutant
average 19791985.
Study range 1129.6 mg/m
3
PM
2.5
across six studied cities
USA, 19821998, Pope et al.
(2002)
M+F 1.08
1.13
1.011.16
1.041.22
Per 10 mg/m
3
PM
2.5
(19791983)
Per 10 mg/m
3
PM
2.5
(19992000)
City of residence in 1982. Pollutant
averages 19791983 and 19992000
Study range roughly 1030 or
520 mg/m
3
PM
2.5
(19791983 and
19992000)
USA, California, 19771992,
Beeson et al. (1998)
M
M
M
F
3.56
5.21
2.66
2.14
1.49.4
1.914.0
1.64.4
1.43.4
Per 556h/year above 200 mg/m
3
O
3
Per 24 mg/m
3
PM
10
Per 11 mg/m
3
SO
2
(3.72 ppb)
Per 11 mg/m
3
SO
2
(3.72 ppb)
Residential history 19731992 and
local monthly pollutant levels
19731992 used to calculate
individual subject averages over
19731992.
Range 988 h over study subjects
Netherlands, 19861994,
Hoek et al. (2002)
M+F 1.06
1.25
0.42.6
0.43.7
Per 10 mg/m
3
black smoke
Per 30 mg/m
3
NO
2
Residential history of last 14
residences up to 1986 matched by
GIS to regional and urban
background estimates plus local
exposure based on distance to
major road
Estimated range 9.635.8 mg/m
3
black smoke and 14.767.2 mg/m
3
NO
2
over study subjects
Casecontrol studies
Germany, ve cities, 1984
1988, Jo ckel et al. (1992)
M
M
1.16
1.82
0.62.1 High vs low time-weighted
semiquantitative index
Same, using 20 years lag
Lifetime residential history. BaP,
TSP, SO
2
data + local energy, SO
2
and coal use and degree of
industrialization 19001980
Italy, Trieste, 19791981,
19851986, Barbone et al.
(1995)
M 1.4 1.11.8 4294 mg/m
2
/day vs o175 of
particulate deposition
Last residence. Deposition
measured 19721977
Russia, Moscow, 19911993,
Zaridze et al. (1995)
F 2.6 1.25.6 4200 SO
2
, 460 NO
2
, 42400 CO,
4300 BS vs o50, o48, o1300, o60
Final 20 years of residential
history. Pollutant average
19711975
Never-smokers only
Poland, Krakow, 19921994,
Pawlega et al. (1997)
M 0.24 0.10.5 TSP 142 & SO
2
110 vs 78 & 71 Last residence. Pollutant average
19731980
Residual confounding by
occupation possible despite some
adjustment
Sweden, Stockholm, 1985
1990, Nyberg et al. (2000)
M 1.6 1.12.4 NO
2
X29.26 vs NO
2
o12.78 (Top
decile vs lowest quartile)
30-year residential history. NO
2
estimates based on historical
emission data and dispersion
modelling
a
mg/m
3
if not otherwise indicated
E
n
v
i
r
o
n
m
e
n
t
a
l
a
n
d
o
c
c
u
p
a
t
i
o
n
a
l
c
a
n
c
e
r
P
B
o
f
f
e
t
t
a
6
3
9
5
O
n
c
o
g
e
n
e
Cancer risk from residential radon exposure
The carcinogenicity of radon decay products has been
widely studied in occupationally exposed populations, in
particular underground miners (see below). This agent
causes lung cancer in humans, while the evidence for an
effect on other neoplasms is not conclusive (IARC,
2001). Although exposure levels in the houses are much
smaller than in underground mines, the duration of
exposure and the number of exposed individuals stress
the importance of residence as a source of exposure to
radon decay products. Several casecontrol studies of
lung cancer from residential radon exposure have been
reported in the literature, and their results have been
reviewed and summarized (Lubin and Boice, 1997;
Darby et al., 2001; IARC, 2001). A pooled RR of
1.06 (95% CI 1.011.10) has been calculated for
individuals exposed at 100 Bq/m
3
vs unexposed (Darby
et al., 2001), which is in agreement with the extrapola-
tion from the results of occupationally exposed popula-
tions. Results of studies reported after these pooled
analyses conrm these conclusions (Pisa et al., 2001;
Tomasek et al., 2001; Barros-Dios et al., 2002; Wang
et al., 2002).
Most studies of residential radon rely on the historical
reconstruction of exposure levels via household mea-
surements. This approach is subject to substantial
misclassication, most likely resulting in an under-
estimate of the risk. In a few studies, attempts were
made to correct such biases, and the estimated RR
increased by about 50% (Lagarde et al., 1997; Darby
et al., 1998). Furthermore, in one study, in which
cumulative radon exposure was estimated from surface
monitors rather than measurement in houses, the RR
was higher (1.63, 95% CI 1.072.93 for exposure at
100 Bq/m
3
) (Alavanja et al., 1999).
Cancer risk from other sources of indoor air pollution
Based on the observation of very high lung cancer rates
in some regions of China and elsewhere among women
who spend much of their time at home, exposure to
indoor air pollution from combustion sources used for
heating and cooking, as well as high levels of cooking oil
vapours resulting from some cooking methods, have
been identied as risk factors for lung cancer. Three
main groups of factors inuencing indoor air pollution
(smokiness) have been studied: (i) heating fuel: type of
fuel, type of stove or central heating, ventilation, living
area, subjective smokiness; (ii) cooking fuel: type of fuel,
type of stove or open pit, ventilation of kitchen, location
of cooking area in residence, frequency of cooking,
smokiness; and (iii) fumes from frying oils: type of oil,
frequency of frying, eye irritation when cooking. Many
of the results are inconclusive, and the interpretation is
difcult since the exposure measures used vary con-
siderably. Nonetheless, strong and signicant increases
in risk have repeatedly been reported and merit
consideration (Gao et al., 1987; Xu et al., 1989, 1991,
1996; Sobue, 1990; Wu-Williams et al., 1990; He et al.,
1991; Lan et al., 1993, 2002; Liu et al., 1993; Dai et al.,
1996; Du et al., 1996; Koo and Ho, 1996; Wang et al.,
1996; Ko et al., 1997; Zhong et al., 1999). If it appears
plausible that indoor air pollution from combustion or
cooking products (oil vapours in particular) could play a
role in the causation of lung cancer, the relevance of the
risks estimated in China for present-day conditions in
other countries is questionable. Frying is less common in
most other countries than in China, and kitchens are
often generally larger, better ventilated and separated
from the living quarters. Central heating is increasingly
common, and open combustion sources indoors are
infrequent.
Cancer risk from inorganic arsenic in drinking water
Inorganic arsenic causes cancer at various sites in
humans (IARC, 1987). The main source of environ-
mental exposure to arsenic for the general population is
through ingestion of contaminated water. A high level
of arsenic in groundwater (up to 25000 mg/l) is found in
many regions of the world, most signicantly around the
Gulf of Bengal, in South America and in Taiwan. There
is strong evidence of an increased risk of bladder, skin
and lung cancers following consumption of water with
high arsenic contamination (IARC, 2004). The evidence
for an increased risk of other cancers, such as those of
the liver, colon and kidney, are weaker but suggestive of
a systemic effect. Most of the available studies have been
conducted in areas at elevated arsenic content (typically
above 200 mg/l). The results of studies of bladder cancer
conducted in areas with low or intermediate contamina-
tion are suggestive of a possible increased risk (Bates
et al., 1995; Kurttio et al., 1999).
Cancer risk from water chlorination by-products
Drinking water may contain a variety of potentially
carcinogenic agents, including chlorination by-products,
resulting from the interaction of chlorine with organic
chemicals (IARC, 1991). Showering, bathing and
drinking represent the main sources of exposure to
chlorination by-products. Among the many halogenated
compounds that may be formed, trihalomethanes,
including chloroform, bromodichloromethane, chloro-
dibromomethane and bromoform, are those most
commonly found. Their concentrations of trihalo-
methanes show a wide range, mainly due to the
occurrence of water contamination by organic chemicals.
A meta-analysis of seven studies of bladder cancer
risk from consumption of chlorinated water resulted in
a RR of 1.21 (95% CI 1.091.34) (Morris et al., 1992).
This estimate was not modied after adjusting for
smoking. A doseresponse relationship was suggested in
three studies (Cantor et al., 1987; McGeehin et al., 1993;
King and Marrett, 1996). Results based on estimated
intake of trihalomethanes and on other disinfection by-
products are too sparse to allow a conclusion.
Despite the good consistency of the available studies
on bladder cancer, the uncertainties in exposure assess-
ment and possible residual confounding caution against
the conclusion that a causal link has been established
Environmental and occupational cancer
P Boffetta
6396
Oncogene
between consumption of chlorinated drinking water and
increased risk of bladder cancer (Cantor, 1997). The
evidence for an association between chlorination by-
products and cancers in organs other than the bladder is
inconclusive (Cantor, 1997).
Occupational cancer
A total of 29 occupational and environmental agents,
groups of agents and mixtures have been classied as
carcinogenic by IARC (19722004), as well as 12
exposure circumstances (Table 3). While some (e.g.
mustard gas) represent today a historic curiosity,
exposure is still widespread for carcinogens such as
asbestos, coal tar, arsenic and silica. Estimates of the
global burden of occupational cancer result in gures in
the order of 24% (Doll and Peto, 1981; Peto, 2001). It
should be stressed, however, that these cancers concen-
trate among exposed subjects (mainly male blue-collar
workers), among whom they may represent up to 20%
of total cancers (Boffetta et al., 1995). Furthermore,
unlike lifestyle factors, exposure is involuntary and can
be, to a large extent, avoided. In fact, reduction of
exposure to occupational carcinogens has taken place in
industrialized countries during recent decades. Efforts
should be made to avoid exposure also in developing
countries. Some of the most important known or
suspected occupational carcinogens are reviewed in
detail below.
Asbestos
Asbestos is an important occupational lung carcinogen,
rst documented following inhalation of asbestos bres
in the 1950s (Hughes and Weil, 1994). All different
forms of asbestos chrysotile and amphiboles, including
crocidolite, amosite and tremolite are carcinogenic to
humans, causing mesothelioma and lung cancer,
although the potency of chrysotile might be lower than
that of other types, in particular with respect to
mesothelioma risk (IPCS (International Programme on
Chemical Safety), 1998).
Studies of cancer risk from asbestos exposure have
been conducted among miners, manufacturers (asbes-
tos-cement, textile, friction materials) and applicators.
The interpretation of the results of these studies is
complicated by several factors: (i) dose, geological type
of bres and industry are all important determinants of
risk and are strictly correlated; (ii) the biologically
relevant exposures occurred 20 or more years before
appearance of the disease, and their quantitative
assessment is imprecise; (iii) the role of potential
confounders, in particular tobacco smoking, can hardly
be evaluated. In general, the risk of lung cancer is
smaller in studies of miners and friction product
manufacturers, is intermediate in studies of asbestos
cement and asbestos product manufacturers, and is
highest in studies of asbestos textile workers. This might
reect a stronger carcinogenic effect of individual, long
and thin bres, as those occurring in the textile industry,
as compared to grouped, short and coarse bres, as
those occurring in mining.
Tobacco smoking is the main cause of lung cancer,
and this applies also to cohorts of asbestos exposed
workers. Despite the limitations of the available studies,
which limit the precision of the estimate of the combined
effect of the two carcinogens, the relative risk of
Table 3 Occupational agents, classied by the IARC Monographs
programme as carcinogenic to humans (Group 1)
Agents, mixture, circumstance Main industry, use
Agents, groups of agents
4-Aminobiphenyl Pigment
Arsenic and arsenic compounds Glass, metal, pesticide
Asbestos Insulation, lter, textile
Benzene Chemical, solvent
Benzidine Pigment
Beryllium and beryllium
compounds
Aerospace
Bis(chloromethyl)ether and
chloromethyl methyl ether
a
Chemical intermediate
Cadmium and cadmium
compounds
Dye/pigment
Chromium[VI] compounds Metal plating, dye/pigment
Dioxin Chemical
Ethylene oxide Sterilant
Mustard gas
a
War gas
2-Naphthylamine Pigment
Nickel compounds Metallurgy, alloy, catalyst
Plutonium-239 and its decay
products
Nuclear industry
Radium-226 and its decay
products
a
Luminizing industry
Radium-228 and its decay
products
a
Luminizing industry
Radon-222 and its decay products Mining
Silica, crystalline Stone cutting, mining, glass
Solar radiation Agriculture
Talc containing asbestiform bres Paper, paints
Vinyl chloride Plastics
X- and g-radiation Medical
Mixtures
Coal-tar pitches
b
Construction, electrode
Coal-tars
b
Fuel, construction, chemical
Mineral oils, untreated
b
Metal
Shale-oils
b
Fuel
Soots
b
Pigment
Wood dust Wood
Exposure circumstances
Aluminum production
Auramine, manufacture of
a
Pigment
Boot and shoe manufacture and
repair
Coal gasication
Coke production
Furniture and cabinet making
Haematite mining (underground)
with exposure to radon
Iron and steel founding
Magenta, manufacture of
a
Pigment
Painter (occupational exposure as a)
Rubber industry
Strong inorganic-acid mists
containing sulphuric acid
Metallurgy
a
Agent mainly of historical interest.
b
Mixture of polycyclic aromatic
hydrocarbons
Environmental and occupational cancer
P Boffetta
6397
Oncogene
asbestos exposure seems to be higher among nonsmo-
kers than among smokers (Liddell, 2001). This suggests
less than multiplicative interaction, which is consistent
with a mechanism of carcinogenesis in which the two
agents act at least in part on the same stages of the
process of cancer development.
Heavy metals
Exposure to inorganic arsenic, known as a carcinogen
since the late 1960s, occurs mainly among workers
employed in hot smelting; other groups at increased risk
are fur handlers, manufacturers of sheep-dip com-
pounds and pesticides, and vineyard workers (IARC,
1987; Hayes, 1997). Workers exposed to arsenic suffer
from an increased risk of cancer of the lung, skin, and
possibly urinary bladder and liver. Chromium[VI]
compounds increase the risk for lung and sinonasal
cancer among chromate production workers, chromate
pigment manufacturers, chromium platers and ferro-
chromium producers (IARC, 1990a; Hayes, 1997). No
such risk has been detected among workers exposed
only to chromium[III] compounds (IARC, 1990a).
Studies of nickel miners, smelters, electrolysis workers
and high-nickel alloy manufacturers showed an in-
creased risk of lung and sinonasal cancer (IARC, 1990b;
Hayes, 1997). There is debate on whether all nickel
compounds are carcinogenic for humans: the available
evidence does not allow a clear separation between
different nickel salts to which workers are exposed. An
increased risk of lung cancer has been demonstrated
among workers in cadmium-based battery manufacture,
coppercadmium alloy workers and cadmium smelters
and recovery workers (IARC, 1993; Hayes, 1997).
Silica and other mineral dusts
An increased risk of lung cancer has been consistently
reported in cohorts of silicotic patients (IARC, 1997;
Steenland and Stayner, 1997). Many authors investi-
gated crystalline silica-exposed workers in foundries,
pottery, ceramics, diatomaceous earth mining, brick
making and stone cutting, some of whom might have
developed silicosis. An increased risk of lung cancer was
reported by some, but not all studies, and in the positive
studies the increase has been small (IARC, 1997;
Steenland and Stayner, 1997). Detailed doseresponse
analyses have suggested a linear relationship, with no
evidence of a threshold (Steenland et al., 2001). There is
inadequate evidence of a carcinogenic effect of exposure
to noncrystalline forms of silica (IARC, 1997).
Polycyclic aromatic hydrocarbons
Polycyclic aromatic hydrocarbons (PAHs) are a com-
plex and important group of chemicals formed during
incomplete combustion of organic material. They are
widespread in the human environment; diet and tobacco
smoke are two important sources of exposure of PAHs.
A number of occupational settings entail exposure to
high level of PAHs. These chemicals, however, occur
inevitably as complex mixtures of variable composition:
an assessment of the risk from individual PAHs is
therefore impossible. An increased risk of lung cancer
has been demonstrated in several industries and
occupations entailing exposure to PAHs such as
aluminium production, coal gasication, coke produc-
tion, iron and steel founding, tar distillation, roong
and chimney sweeping (Boffetta et al., 1997). An
increase has also been suggested in a few other
industries, including shale oil extraction, wood impreg-
nation, road paving, carbon black production and
carbon electrode manufacture with an exposurere-
sponse relationship in the studies with detailed exposure
information. Other cancers that have been denitely
associated with occupational exposure to PAHs are
those from the skin, in particular for coal-tar pitches,
coal-tars and untreated mineral oils, and the urinary
bladder, in particular following exposure to coal-tar
pitches and in aluminium and coal gasication workers
(Boffetta et al., 1997).
Motor vehicle and other engine exhausts represent an
important group of mixtures of PAHs, since they
contribute signicantly to air pollution. The available
epidemiological evidence strongly suggests 4050%
excess of lung cancer among those occupationally
exposed to diesel engine exhaust (Lipsett and Cample-
man, 1999). The evidence for other cancers is inade-
quate. Data on other types of exhausts, including
gasoline engines, do not allow any conclusions (IARC,
1989).
Strongly reactive chemicals
Occupational exposure to several strongly reactive
chemicals has been shown to cause cancer in humans.
Workers exposed to chloromethyl methyl ether and
bis(chloromethyl) ether are at increased risk of lung
cancer, in particular of small cell type (IARC, 1987;
Blair and Kazerouni, 1997). An increased risk of
laryngeal cancer has been demonstrated in studies
of workers exposed to strong inorganic acids in
particular sulphuric acid in metal plating, metal
treatment, battery manufacture and in the chemical
industry (IARC, 1992; Blair and Kazerouni, 1997). An
increased risk of liver angiosarcoma and possibly other
tumours has been reported in studies of workers
exposed to vinyl chloride (IARC, 1987).
Ionizing radiation
Exposure to X- and g-radiation causes leukaemia and
solid tumours in humans (IARC, 2000). Occupational
exposure occurs in several circumstances, notably in
medical professions and in the nuclear industry. An
increased risk of leukaemia, skin cancer and other solid
tumours has been described in early studies of radi-
ologists and other medical workers: exposure levels have
greatly decreased in recent decades and it is unclear
whether a residual risk still exists. Cancer risk among
nuclear power plant workers has been extensively
studied in several countries: the most accurate estimates
Environmental and occupational cancer
P Boffetta
6398
Oncogene
suggest an excess RR of leukaemia in the order of 2.2%
(95% CI 0.13.7) per Sv of exposure (IARC Study
Group on Cancer Risk among Nuclear Industry Work-
ers, 1994). No clear excess was found for solid tumours.
Data on cancer among other workers exposed to X- and
g-radiation (e.g. nuclear accident clean-up workers) are
also suggestive of an increased risk of leukaemia (IARC,
2000).
Underground miners exposed to radioactive radon
and its decay products, which emit a-particles, have been
consistently found to be at increased risk for lung cancer
(IARC, 2001). The risk increased with estimated
cumulative exposure and decreased with attained age,
time since exposure, and time since cessation of
exposure (National Research Council, 1999). The excess
RR estimated from occupational cohorts, which in-
cluded over 2500 cases of lung cancer occurring among
over 60 000 miners, has been estimated in the order of
0.0049 per working level month of exposure (Lubin
et al., 1995). Further renements of this estimates took
into account age at exposure and time since rst
exposure (National Research Council, 1999), as well as
smoking status, with a stronger effect being shown
among never-smokers than among smokers. An carci-
nogenic effect of radon exposure on organs other than
the lung is not substantiated.
Other radionuclides to which humans are, or have
been, exposed in the workplace include radium-226
(increased risk of osteosarcoma among watch-dial
painters) and plutonium-239 (increased risk of lung,
liver and bone neoplasms among heavily exposed
workers in plutonium production plants) (IARC, 2001).
Exposure circumstances
An increased risk of cancer has been demonstrated
among workers employed in several jobs and industries
(Table 3). While for some of these exposure circum-
stances the agents responsible for the excess cancer risk
have been identied (e.g. wood dust in furniture making,
mixtures of PAHs for aluminium, foundry, coke and
coal gasication workers), this has not been possible for
others, such as painters and rubber workers, which
limits the scope of preventive measures.
Suspected carcinogens
Some 31 occupational agents and three exposure
circumstances are classied as probable carcinogens
(Table 4). They include important chemicals such as tri-
and tetrachloroethylene, formaldehyde and butadiene.
The reasons for the classication as suspected rather
than established carcinogens lay mainly in the inade-
quacy of the available evidence from epidemiological
studies, due to limited statistical power to detect a small
excess of rare neoplasms, limitations in the available
exposure data and concomitant exposure to other
potentially hazardous chemicals.
The example of butadiene, an important occupational
agent which under experimental conditions causes
leukaemia in mice, is particularly illustrative (IARC,
1998). The most informative cohort study of workers
exposed to butadiene was conducted among workers
employed in the production of synthetic rubber based
on styrene and butadiene (Macaluso et al., 1996;
Sathiakumar et al., 1998). This study showed a clear
increased risk of leukaemia, based on 58 deaths, with a
doseresponse (RRs 1.0 (reference group), 1.5 (95% CI
0.73.2) and 1.7 (95% CI 0.83.9) in the three categories
of increasing butadiene exposure; P-value of test for
linear trend 0.03), which was not explained by exposure
to styrene or other agents. These results receive a limited
support by the only other large cohort study conducted
Table 4 Occupational agents, classied by the IARC Monographs
programme as probably carcinogenic to humans (Group 2A)
Agents, mixture, circumstance Main industry, use
Agents, groups of agents
Acrylamide Chemical, construction
Acrylamide Chemical, construction
Benz[a]anthracene
a
Combustion fumes
Benzidine-based dyes Paper, leather, textile dyes
Benzo[a]pyrene
a
Combustion fumes
1,3-Butadiene Plastics, rubber
Captafol Fungicide
a-Chlorinated toluenes Chemical intermediate
4-Chloro-ortho-toluidine Dye/pigment manufacture,
textiles
Dibenz[a,h]anthracene
a
Combustion fumes
Diethyl sulphate Chemical intermediate
Dimethylcarbamoyl chloride Chemical intermediate
Dimethyl sulphate Chemical intermediate
Epichlorohydrin Plastics/resins monomer
Ethylene dibromide Chemical intermediate,
fumigant
Formaldehyde Plastics, textiles, laboratory
agent
Glycidol Chemical intermediate
4,4
0
-Methylene bis (2-
chloroaniline) (MOCA)
b
Rubber manufacture
N-Nitrosodimethylamine
b
Chemical intermediate
Styrene-7,8-oxide Plastics, chemical
intermediate
Tetrachloroethylene Solvent, dry cleaning
Ortho-Toluidine Dyestuff, rubber
Trichloroethylene Solvent, dry cleaning, metal
1,2,3-Trichloropropane Solvent, chemical
intermediate
Tris(2,3-
dibromopropyl)phosphate
Plastics, textiles, ame
retardant
Vinyl bromide Plastics, textiles, monomer
Vinyl uoride Chemical intermediate
Mixtures
Creosotes
c
Wood preservation
Diesel engine exhaust
c
Transport
Nonarsenical insecticides
(spraying and application)
Agriculture
Polychlorinated biphenyls Electrical components
Exposure circumstances
Art glass, glass container and
pressed ware (manuf. of)
Hairdresser and barber
Petroleum rening
a
Component of mixtures of polycyclic aromatic hydrocarbons.
b
Agent
mainly of historical interest.
c
Mixture of polycyclic aromatic hydro-
carbons
Environmental and occupational cancer
P Boffetta
6399
Oncogene
among butadiene production workers (Divine and
Hartman, 1996), while no clear excess was present in
the remaining, smaller studies (Bond et al., 1992; Cowles
et al., 1994; Ward et al., 1996). Overall, the presence of a
causal association between butadiene exposure and
occurrence of cancer (leukaemia in particular) in
humans is plausible: this conclusion is supported by a
single large and very carefully conducted study and is
compatible with the results of an additional valid,
although less informative, study. The inconsistency in
the results of additional studies should be seen in the
light of potential limitations, namely limited power,
misclassication of leukaemia on death certicates and
nondifferential misclassication of exposure.
Conclusions
A number of circumstances of environmental exposure
to carcinogens has denitely been linked with an
increased risk of cancer in humans. For all of them, it
is not possible to quantify with precision the burden of
human cancer they cause. It is likely however that in
most populations, environmental cancer is responsible
for a relatively small proportion of total cancers, in the
order of 0.51% (Doll and Peto, 1981; Peto, 2001).
However, this proportion is likely to be higher in
populations with special exposure circumstances, such
as arsenic contamination of drinking water or proximity
to an important source of asbestos exposure. Further-
more, the involuntary nature of the exposure makes its
elimination a particularly important target in terms of
health equity.
Knowledge on occupational causes of cancer is more
advanced than in the case of other groups of carcino-
gens. However, current understanding of the relation-
ship between occupational exposures and cancer risk is
far from complete: for many experimental carcinogens
that occur in the workplace, little or no human cancer
data are available. Examples of such agents are ceramic
bres, acrylamide, dichloromethane and acetaldehyde:
they all cause tumours in experimental animals and no
adequate data in exposed humans are available. One
should also consider that the relatively low burden of
occupational cancer in industrialized countries is the
successful result of strict regulations on recognized
carcinogens. As in the case of environmental cancer, the
facts that exposure is involuntary and can be eliminated
give to prevention of occupational cancer a special
status among interventions towards cancer control.
References
Abbey DE, Nishino N, McDonnell WF, Burchette RJ,
Knutsen SF, Beeson WL and Yang JX. (1999). Am. J.
Respir. Crit. Care Med., 159, 373382.
Alavanja MC, Lubin JH, Mahaffey JA and Brownson RC.
(1999). Am. J. Public Health, 89, 10421048.
Barbone F, Bovenzi M, Cavallieri F and Stanta G. (1995). Am.
J. Epidemiol., 141, 11611169.
Barros-Dios JM, Barreiro MA, Ruano-Ravina A and Fig-
ueiras A. (2002). Am. J. Epidemiol., 156, 548555.
Bates MN, Smith AH and Cantor KP. (1995). Am. J.
Epidemiol., 141, 523530.
Beeson WL, Abbey DE and Knutsen SF. (1998). Environ.
Health Perspect., 106, 813822.
Bhopal RS, Moffatt S, Pless-Mulloli T, Phillimore PR, Foy C,
Dunn CE and Tate JA. (1998). Occup. Environ. Med., 55,
812822.
Biggeri A, Barbone F, Lagazio C, Bovenzi M and Stanta G.
(1996). Environ. Health Perspect., 104, 750754.
Blair A and Kazerouni N. (1997). Cancer Causes Control, 8,
473490.
Blot WJ and Fraumeni Jr JF. (1975). Lancet, 2, 142144.
Boffetta P. (2002). Scand. J. Work Environ. Health, 28, 3040.
Boffetta P, Jourenkova N and Gustavsson P. (1997). Cancer
Causes Control, 8, 444472.
Boffetta P, Kogevinas M, Simonato L, Wilbourn J and
Saracci R. (1995). Int. J. Occup. Environ. Health, 1,
315325.
Bond GG, Bodner KM, Olsen GW and Cook RR. (1992).
Scand. J. Work Environ. Health, 18, 145154.
Botha JL, Irwig LM and Strebel P. (1986). Am. J. Epidemiol.,
123, 3040.
Brown LM, Pottern LM and Blot WJ. (1984). Environ. Res.,
34, 250261.
Brownson RC, Reif JS, Keefe TJ, Ferguson SW and Pritzl JA.
(1987). Am. J. Epidemiol., 125, 2534.
Buell P and Dunn JE. (1967). Arch. Environ. Health, 15, 291
297.
Buell P, Dunn JE and Breslow L. (1967). Cancer, 20, 2139
2147.
Camus M, Siemiatycki J and Meek B. (1998). New Engl. J.
Med., 338, 15651571.
Cantor KP. (1997). Cancer Causes Control, 8, 292308.
Cantor K, Hoover R, Hartge P, Mason TJ, Silverman DT,
Altman R, Austin DF, Child MA, Key CR, Marrett LD,
Myers MH, Narayama AS, Levin LI, Sullivan JW, Swanson
GM, Thomas DB and West DW. (1987). J. Natl. Cancer
Inst., 79, 12691279.
Cederlo f R, Friberg L, Hrubek Z and Lorich U. (1975). The
Relationship of Smoking and Some Social Covariables to
Mortality and Cancer Morbidity: A Ten Year Follow-up in a
Probability Sample of 55000 Swedish Subjects Age 18 to 69, 2
volumes. Department of Environmental Hygiene, Karolins-
ka Institute: Stockholm.
Cordier S, Theriault G and Iturra H. (1983). Environ. Res., 31,
311322.
Cowles SR, Tsai SP, Snyder PJ and Ross CE. (1994). Occup.
Environ. Med., 51, 323329.
Dai XD, Lin CY, Sun XW, Shi YB and Lin YJ. (1996). Lung
Cancer, 14, 8591.
Darby S, Hill D and Doll R. (2001). Ann. Oncol., 12, 1341
1351.
Darby S, Whitley E, Silcocks P, Thakrar B, Green M, Lomas
P, Miles J, Reeves G, Fearn T and Doll R. (1998). Br. J.
Cancer, 78, 394408.
Dean G. (1966). BMJ, 5502, 15061514.
Dean G, Lee PN, Todd GF and Wicken AJ. (1977). Report on
a Second Retrospective Mortality Study in North-East
England, Part I: Factors Related to Mortality from Lung
Cancer, Bronchitis, Heart Disease and Stroke in Cleveland
County, with Particular Emphasis on the Relative Risks
Environmental and occupational cancer
P Boffetta
6400
Oncogene
Associated with Smoking Filter and Plain Cigarettes.
Tobacco Research Council: London.
Dean G, Lee PN, Todd GF and Wicken AJ. (1978). Report on
a Second Retrospective Mortality Study in North-East
England, Part II: Changes in Lung Cancer and Bronchitis
Mortality and in Other Relevant Factors Occurring in Areas
of North-East England, 196372. Tobacco Research Council:
London.
Divine BJ and Hartman CM. (1996). Toxicology, 113,
169181.
Dockery DW, Pope III CA, Xu X, Spengler JD, Ware JH, Fay
ME, Ferris Jr BG and Speizer FE. (1993). New Engl. J.
Med., 329, 17531759.
Doll R and Peto R. (1981). J. Natl. Cancer Inst., 66,
11911308.
Du YX, Cha Q, Chen XW, Chen YZ, Huang LF, Feng ZZ,
Wu XF and Wu JM. (1996). Lung Cancer, 14, 937.
Engholm G, Palmgren F and Lynge E. (1996). BMJ, 312,
12591263.
Frost F, Harter L, Milham S, Royce R, Smith AH, Hartley J
and Enterline P. (1987). Arch. Environ. Health, 42,
148152.
Gailey FA and Lloyd OL. (1983). Ecol. Dis., 2, 419431.
Gailey FA and Lloyd OL. (1986). Environ. Health Perspect.,
68, 187196.
Gao YT, Blot WJ, Zheng W, Ershow AG, Hsu CW, Levin LI,
Zhang R and Fraumeni Jr JF. (1987). Int. J. Cancer, 40,
604609.
Goldsmith JR. (1980). J. Environ. Pathol. Toxicol., 3, 205217.
Greaves WW, Rom WN, Lyon JL, Varley G, Wright DD and
Chiu G. (1981). Am. J. Ind. Med., 2, 1523.
Hackshaw AK, Law MR and Wald NJ. (1997). BMJ, 315,
980988.
Haenszel W, Loveland DB and Sirken MG. (1962). J. Natl.
Cancer Inst., 28, 9471001.
Haenszel W and Taeuber KE. (1964). J. Natl. Cancer Inst., 32,
803838.
Hammond EC. (1972). Environmental Factors in Respiratory
Disease, Lee DH (ed). Academic Press: New York, pp.
177198.
Hammond EC and Garnkel L. (1980). Prev. Med., 9,
206211.
Hammond EC, Garnkel L, Selikoff IJ and Nicholson WT.
(1979). Ann. NY Acad. Sci., 330, 417422.
Hammond EC and Horn D. (1958a). JAMA, 166, 11591172.
Hammond EC and Horn D. (1958b). JAMA, 166, 12941308.
Hansen J, de Klerk NH, Musk AW and Hobbs MST. (1998).
Am. J. Respir. Crit. Care Med., 157, 6975.
Hayes RB. (1997). Cancer Causes Control, 8, 371385.
He XZ, Chen W, Liu ZY and Chapman RS. (1991). Environ.
Health Perspect., 94, 913.
Hitosugi M. (1968). Bull. Inst. Public Health, 17, 237256.
Hoek G, Brunekreef B, Goldbohm S, Fischer P and van den
Brandt PA. (2002). Lancet, 360, 12031209.
Holowaty EJ, Risch HA, Miller AB and Burch JD. (1991).
Can. J. Public Health, 82, 304309.
Howel D, Arblaster L, Swinburne L, Schweiger M, Renvoize E
and Hatton P. (1997). Occup. Environ. Med., 54, 403409.
Hughes JM and Weill H. (1994). Epidemiology of Lung Cancer.
Lung Biology in Health and Disease, Samet JM (ed). Vol 74.
Marcel Dekker: New York, pp. 185205.
IARC (19722004). IARC Monographs on the Evaluation of
Carcinogenic Risks to Humans, Vols 180. International
Agency for Research on Cancer: Lyon.
IARC (1987). Overall Evaluations of Carcinogenicity: An
Updating of IARC Monographs Volumes 1 to 42, IARC
Monographs on the Evaluation of the Carcinogenic Risk of
Chemicals to Humans, Suppl 7 IARC: Lyon.
IARC (1989). Diesel and Gasoline Engine Exhausts and Some
Nitroarenes, IARC Monographs on the Evaluation of
Carcinogenic Risks to Humans, Vol 46. IARC: Lyon,
pp. 41185.
IARC (1990a). Chromium, Nickel and Welding, IARC Mono-
graphs on the Evaluation of Carcinogenic Risks to Humans,
Vol 49. IARC: Lyon, pp. 49256.
IARC (1990b). Chromium, Nickel and Welding, IARC Mono-
graphs on the Evaluation of Carcinogenic Risks to Humans,
Vol 49. IARC: Lyon, pp. 257445.
IARC (1991). Chlorinated Drinking Water; Chlorination By-
Products; Some Other Halogenated Compounds; Cobalt and
Cobalt Compounds, IARC Monographs on the Evaluation of
Carcinogenic Risks to Humans, Vol 52. IARC: Lyon.
IARC (1992). Occupational Exposures to Mists and Vapours
from Strong Inorganic Acids and Other Industrial Chemicals,
IARC Monographs on the Evaluation of Carcinogenic
Risks to Humans, Vol 54. IARC: Lyon, pp. 41119.
IARC (1993). Beryllium, Cadmium, Mercury and Exposures in
the Glass Manufacturing Industry, IARC Monographs on the
Evaluation of Carcinogenic Risks to Humans, Vol 58.
IARC: Lyon, pp. 119237.
IARC (1997). Silica, Some Silicates, Coal Dust and Para-
Aramid Fibrils, IARC Monographs on the Evaluation of
Carcinogenic Risks to Humans, Vol 68. IARC: Lyon,
pp. 41242.
IARC (1998). Re-evaluation of Some Organic Chemicals,
Hydrazine and Hydrogen Peroxide (Part One), IARC
Monographs on the Evaluation of Carcinogenic Risks to
Humans, Vol. 71. IARC: Lyon, pp. 109225.
IARC (2000). Ionizing Radiation, Part 1: X- and Gamma-
Radiation, and Neutrons, IARC Monographs on the
Evaluation of Carcinogenic Risks to Humans, Vol 75.
IARC: Lyon.
IARC (2001). Ionizing Radiation, Part 2: Some Internally
Deposited Radionuclides, IARC Monographs on the Evalua-
tion of Carcinogenic Risks to Humans, Vol 78. IARC: Lyon.
IARC (2004). Tobacco Smoking and Involuntary Tobacco
Smoke, IARC Monographs on the Evaluation of Carcino-
genic Risks to Humans, Vol 83. IARC: Lyon, (in press).
IARC Study Group on Cancer Risk among Nuclear Industry
Workers (1994). Lancet, 344, 10391043.
INSERM (1997). Effets sur la Sante des Principaux Types
dExposition a` lAmiante, (Expertise Collective INSERM).
Institut National de la Sante et de la Recherche Me dicale:
Paris.
IPCS (International Programme on Chemical Safety) (1998).
Chrysotile Asbestos, Environmental Health Criteria 203.
World Health Organization: Geneve.
Jedrychowski W, Becher H, Wahrendorf J and Basa-Cierpia-
lek Z. (1990). J. Epidemiol. Community Health, 44, 114120.
Jo ckel KH, Ahrens W, Wichmann HE, Becher H, Bolm-
Audorff U, Jahn I, Molik B, Greiser E and Timm J. (1992).
Int. J. Epidemiol., 21, 202213.
Katsouyanni K, Trichopoulos D, Kalandidi A, Tomos P and
Riboli E. (1991). Prev. Med., 20, 271278.
King WD and Marrett LD. (1996). Cancer Causes Control, 7,
596604.
Ko YC, Lee CH, Chen MJ, Huang CC, Chang WY, Lin HJ,
Wang HZ and Chang PY. (1997). Int. J. Epidemiol., 26,
2431.
Koo LC and Ho JH. (1996). Lung Cancer, 14, 4761.
Kurttio P, Pukkala E, Kahelin H, Auvinen A and Pekkanen J.
(1999). Environ. Health Perspect., 107, 705710.
Environmental and occupational cancer
P Boffetta
6401
Oncogene
Lagarde F, Pershagen G, Akerblom G, Axelson O, Baverstam
U, Damber L, Eno A, Svartengren M and Swedjemark
GA. (1997). Health Phys., 72, 269276.
Lan Q, Chapman RS, Schreinemachers DM, Tian L and He
X. (2002). J. Natl. Cancer Inst., 94, 826835.
Lan Q, Chen W, Chen H and He XZ. (1993). Biomed. Environ.
Sci., 6, 112118.
Levin ML, Haenszel W, Carroll BE, Gerhardt PR, Handy VH
and Ingraham SC. (1960). J. Natl. Cancer Inst., 24,
12431257.
Liddell FD. (2001). Ann Occup. Hyg., 45, 341356.
Lipsett M and Campleman S. (1999). Am. J. Public Health, 89,
10091017.
Liu Q, Sasco AJ, Riboli E and Hu MX. (1993). Am. J.
Epidemiol., 137, 145154.
Lloyd OL. (1978). Lancet, 1, 318320.
Lloyd OL, Ireland E, Tyrrell H and Williams F. (1986). J. Soc.
Occup. Med., 36, 28.
Lloyd OL, Smith G, Lloyd MM, Holland Y and Gailey F.
(1985a). Br. J. Ind. Med., 42, 475480.
Lloyd OL, Williams FL and Gailey FA. (1985b). Br. J. Ind.
Med., 42, 815823.
Lubin JH and Boice Jr JD. (1997). J. Natl. Cancer Inst., 89,
4957.
Lubin JH, Boice Jr JD, Edling C, Hornung RW, Howe GR,
Kunz E, Kusiak RA, Morrison HI, Radford EP, Samet JM,
Tirmarche M, Woodward A, Yao SX and Pierce DA.
(1995). J. Natl. Cancer Inst., 87, 817827.
Luce D, Bugel I, Goldberg P, Goldberg M, Salomon C, Billon-
Galland MA, Nicolau J, Quenel P, Fevotte J and Brochard
P. (2000). Am. J. Epidemiol., 151, 259265.
Luo S, Zhang Y, Mu S, Zhang C, Ma T and Liu X. (1998).
Hua Xi Yi Ke Da Xue Xue Bao, 29, 6365 (in Chinese).
Lyon JL, Fillmore JL and Klauber MR. (1977). Lancet, 2, 869.
Macaluso M, Larson R, Delzell E, Sathiakumar N, Hovinga
M, Julian J, Muir D and Cole P. (1996). Toxicology, 113,
190202.
Magnani C, Agudo A, Gonzalez CA, Andrion A, Calleja A,
Chellini E, Dalmasso P, Escolar A, Hernandez S, Ivaldi C,
Mirabelli D, Ramirez J, Turuguet D, Usel M and Terracini
B. (2000). Br. J. Cancer, 83, 104111.
Magnani C, Dalmasso P, Biggeri A, Ivaldi C, Mirabelli D and
Terracini B. (2001). Environ. Health Perspect., 109, 915919.
Magnani C, Terracini B, Ivaldi C, Botta M, Mancini A and
Andrion A. (1995). Occup. Environ. Med., 52, 362367.
Marsh GM, Stone RA, Esmen NA, Gula MJ, Gause CK,
Petersen NJ, Meaney FJ, Rodney S and Prybylski D. (1997).
Environ. Res., 75, 5672.
Marsh GM, Stone RA, Esmen NA, Gula MJ, Gause CK,
Petersen NJ, Meaney FJ, Rodney S and Prybylski D. (1998).
Arch. Environ. Health, 53, 1528.
Matanoski GM, Landau E, Tonascia J, Lazar C, Elliott EA,
McEnroe W and King K. (1981). Environ. Res., 25, 828.
McDonnell WF, Nishino-Ishikawa N, Petersen FF, Chen LH
and Abbey DE. (2000). J. Expo. Anal. Environ. Epidemiol.,
10, 427436.
McGeehin MA, Reif JS, Becher JC and Mangione EJ. (1993).
Am. J. Epidemiol., 138, 492501.
Mills PK, Abbey DE, Beeson WL and Petersen F. (1991).
Arch. Environ. Health, 46, 271280.
Morris RD, Audet AM, Angelillo IF, Chalmers TC and
Mosteller F. (1992). Am. J. Public Health, 82, 955963.
Mzileni O, Sitas F, Steyn K, Carrara H and Bekker P. (1999).
Tobacco Control, 8, 398401.
National Research Council (1999). Committee on Health Risks
of Exposure to Radon: BEIR VI, Health effects of exposure to
radon. National Academy Press: Washington, DC.
Neuberger M, Kundi M and Friedl HP. (1984). Arch. Environ.
Health, 39, 261265.
Newhouse M and Thompson H. (1965). Br. J. Ind. Med., 2,
261269.
Newman JA, Archer VE, Saccomanno G, Kuschner M,
Auerbach O, Grondahl RD and Wilson JC. (1976). Ann.
NY Acad. Sci., 271, 260268.
Nyberg F, Gustavsson P, Jarup L, Bellander T, Berglind N,
Jakobsson R and Pershagen G. (2000). Epidemiology, 11,
487495.
Pawlega J, Rachtan J and Dyba T. (1997). Acta Oncol., 36,
471476.
Pershagen G. (1985). Am. J. Epidemiol., 122, 684694.
Pershagen G, Elinder CG and Bolander AM. (1977). Environ.
Health Perspect., 19, 133137.
Peto J. (2001). Nature, 411, 390395.
Petrauskaite R, Pershagen G and Gurevicius R. (2002). Int. J.
Cancer, 99, 106111.
Pike MC, Jing JS, Rosario IP, Henderson BE and Menck HR.
(1979). Energy and Health, Breslow N, Whitemore A (eds)
SIAM: Philadelphia, PA, pp. 316.
Pisa FE, Barbone F, Betta A, Bonomi M, Alessandrini B and
Bovenzi M. (2001). Arch. Environ. Health, 56, 208215.
Pope III CA, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito
K and Thurston GD. (2002). JAMA, 287, 11321141.
Pope III CA, Thun MJ, Namboodiri MM, Dockery DW,
Evans JS, Speizer FE and Heath Jr CW. (1995). Am. J.
Respir. Crit. Care Med., 151, 669674.
Pott P. (1775). Chirurgical Observations. Hawes, Clarke and
Collins: London.
Rom WN, Varley G, Lyon JL and Shopkow S. (1982). Br. J.
Ind. Med., 39, 269272.
Samet JM, Humble CG, Skipper BE and Pathak DR. (1987).
Am. J. Epidemiol., 125, 800811.
Sathiakumar N, Delzell E, Hovinga M, Macaluso M, Julian
JA, Larson R, Cole P and Muir DCF. (1998). Occup.
Environ. Med., 55, 230235.
Shear CL, Seale DB and Gottlieb MS. (1980). Arch. Environ.
Health, 35, 335343.
Smith GH, Williams FL and Lloyd OL. (1987). Br. J. Ind.
Med., 44, 795802.
Sobue T. (1990). Int. J. Epidemiol., 19, 6266.
Steenland K, Mannetje A, Boffetta P, Stayner L, Atteld M,
Chen J, Dosemeci M, DeKlerk N, Hnizdo E, Koskela R and
Checkoway H. (2001). Cancer Causes Control, 12, 773784.
Steenland K and Stayner L. (1997). Cancer Causes Control, 8,
491503.
Stocks P and Campbell JM. (1955). BMJ, 2, 923929.
Swaen GM and Slangen JJ. (1995). Int. Arch. Occup. Environ.
Health, 67, 8593.
Tenkanen L. (1993). Cancer Causes Control, 4, 133141.
Tenkanen L, Hakulinen T, Hakama M and Saxen E. (1985).
Int. J. Cancer, 35, 637642.
Theriault GP and Grand-Bois L. (1978). Arch. Environ.
Health, 33, 1519.
Tenkanen L and Teppo L. (1987). Scand. J. Soc. Med., 15, 6772.
Tomasek L, Kunz E, Mu ller T, Hulka J, Heribanova A,
Matzner J, Placek V, Burian I and Holecek J. (2001). Sci.
Total Environ., 272, 4351.
Tomatis L, Aitio A, Day NE, Heseltine E, Kaldor J, Miller
AB, Parkin DM and Riboli E. (1990). Cancer: Causes,
Occurrence and Control, IARC Scientic Publications No
100 IARC: Lyon.
Environmental and occupational cancer
P Boffetta
6402
Oncogene
Vena JE. (1982). Am. J. Epidemiol., 116, 4256.
Wang SY, Hu YL, Wu YL, Li X, Chi GB, Chen Y and Dai
WS. (1996). Lung Cancer, 14, 99105.
Wang Z, Lubin JH, Wang L, Zhang S, Boice Jr JD, Cui H,
Zhang S, Conrath S, Xia Y, Shang B, Brenner A, Lei S,
Metayer C, Cao J, Chen KW, Lei S and Kleinerman RA.
(2002). Am. J. Epidemiol., 155, 554564.
Ward EM, Fajen JM, Ruder AM, Rinsky RA, Halperin WE
and Fessler-Flesch CA. (1996). Toxicology, 113, 157168.
Williams FL and Lloyd OL. (1988). Public Health, 102,
531538.
Wu-Williams AH, Dai XD, Blot W, Xu ZY, Sun XW, Xiao
HP, Stone BJ, Yu SF, Feng YP, Ershow AG, Sun J,
Fraumeni Jr JF and Henderson BE. (1990). Br. J. Cancer,
62, 982987.
Xiao HP and Xu ZY. (1985). NCI Monogr., 69, 5358.
Xu ZY, Blot WJ, Li G, Fraumeni Jr JF, Zhao DZ, Stone BJ,
Yin Q, Wu A, Henderson BE and Guan BP. (1991).
Relevance to Human Cancer of N-Nitroso Compounds,
Tobacco Smoke and Mycotoxins, ONeill IK, Chen J,
Bartsch H (eds). IARC Scientic Publications No 105.
IARC: Lyon, pp. 460465.
Xu ZY, Blot WJ, Xiao HP, Wu A, Feng YP, Stone BJ, Sun J,
Ershow AG, Henderson BE and Fraumeni Jr JF. (1989).
J. Natl. Cancer Inst., 81, 18001806.
Xu ZY, Brown L, Pan GW, Li G, Feng YP, Guan DX, Liu
TF, Liu LM, Chao RM, Sheng JH and Gao GC. (1996).
Lung Cancer, 14, 149160.
Zaridze DG, Zemlianaia GM and Aitakov ZN. (1995). Vestnik
Rossiiskoi Akademii Meditsinskikh Nauk, 4, 610 (in Russian).
Zhong LJ, Goldberg MS, Parent ME and Hanley JA. (1999).
Scand. J. Work Environ. Health, 25, 309316.
Environmental and occupational cancer
P Boffetta
6403
Oncogene
Você também pode gostar
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Asbestos Dust Respirators 1971Documento243 páginasAsbestos Dust Respirators 1971Bruno ThiemeAinda não há avaliações
- Rail Safety CanadaDocumento26 páginasRail Safety CanadaBruno ThiemeAinda não há avaliações
- Pattys Cap 84 TalcoDocumento16 páginasPattys Cap 84 TalcoBruno ThiemeAinda não há avaliações
- Beth Donovan 2000Documento5 páginasBeth Donovan 2000Bruno ThiemeAinda não há avaliações
- IARC Classification Site CancerDocumento12 páginasIARC Classification Site CancerBruno ThiemeAinda não há avaliações
- Yachting Guide DanubeDocumento46 páginasYachting Guide DanubeBruno ThiemeAinda não há avaliações
- Asbestos School 1980Documento3 páginasAsbestos School 1980Bruno ThiemeAinda não há avaliações
- Asbestos Dust Respirators 1971Documento243 páginasAsbestos Dust Respirators 1971Bruno ThiemeAinda não há avaliações
- NIOSH Confined Spaces 1986 PDFDocumento22 páginasNIOSH Confined Spaces 1986 PDFBruno ThiemeAinda não há avaliações
- Iron BrochureDocumento13 páginasIron BrochureBruno ThiemeAinda não há avaliações
- Mineral Physics and Crystallography - A Handbook of Physical Constants 1995 - AhrensDocumento357 páginasMineral Physics and Crystallography - A Handbook of Physical Constants 1995 - Ahrensarwin_nikfarjam9112Ainda não há avaliações
- Iron BrochureDocumento13 páginasIron BrochureBruno ThiemeAinda não há avaliações
- EPA Control Technologies Hazardous Pollutants 1991Documento260 páginasEPA Control Technologies Hazardous Pollutants 1991Bruno ThiemeAinda não há avaliações
- Safety MagnalenzDocumento29 páginasSafety MagnalenzBruno ThiemeAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- Dust in MiningDocumento27 páginasDust in Miningfun forAinda não há avaliações
- Msds Oreas (Rada)Documento10 páginasMsds Oreas (Rada)Heber Diaz ChavezAinda não há avaliações
- AFTEK - Penapatch Fairing Coat Mortar SDS 2009Documento4 páginasAFTEK - Penapatch Fairing Coat Mortar SDS 2009Aria NickbakhtAinda não há avaliações
- Toolbox Talk: The Hazards of Silica DustDocumento1 páginaToolbox Talk: The Hazards of Silica DustNadia RosdianshahAinda não há avaliações
- 5469 Greenlite 45 L Plus (Usa)Documento7 páginas5469 Greenlite 45 L Plus (Usa)Armani FernandesAinda não há avaliações
- Shahab 2016Documento10 páginasShahab 2016Shakeel MirwaniAinda não há avaliações
- Textbook Part 3Documento87 páginasTextbook Part 3CY OnuorahAinda não há avaliações
- Dr. S.K. Haldar's Lectures On Industrial Health For AFIH Students - Occu. Lung Dis Asbestosis Silicosis ByssinosisDocumento26 páginasDr. S.K. Haldar's Lectures On Industrial Health For AFIH Students - Occu. Lung Dis Asbestosis Silicosis ByssinosisDr. Prakash Kulkarni100% (2)
- MSDS AAC Hebel Blocks - 2002Documento4 páginasMSDS AAC Hebel Blocks - 2002aditarian .pAinda não há avaliações
- Occupational Health Hazards Due To Mine Dust: Unit-14Documento9 páginasOccupational Health Hazards Due To Mine Dust: Unit-14Dinesh dhakarAinda não há avaliações
- CemexDocumento2 páginasCemexdaniel878787Ainda não há avaliações
- Wax Emulsion Curing CompoundDocumento2 páginasWax Emulsion Curing CompoundSanjay KambleAinda não há avaliações
- Multiquip SP2S20HDocumento40 páginasMultiquip SP2S20Heltomy1Ainda não há avaliações
- 1874C 02RD MT 0640 0 PDFDocumento236 páginas1874C 02RD MT 0640 0 PDFShafi AshrafAinda não há avaliações
- Wk1of 2 - DoctorsDocumento44 páginasWk1of 2 - Doctorsry lr100% (1)
- Safety and Operating Instructions: Bulk PulverizerDocumento52 páginasSafety and Operating Instructions: Bulk PulverizerlidoAinda não há avaliações
- Chapter RDocumento21 páginasChapter RmanoharandaAinda não há avaliações
- Chapter 8 - Oil and Gas SafetyDocumento35 páginasChapter 8 - Oil and Gas SafetyEdgar LacsaAinda não há avaliações
- Unit 1 Introduction To Safety-1Documento16 páginasUnit 1 Introduction To Safety-1e smithAinda não há avaliações
- Muffle Furnace 6000 PDFDocumento56 páginasMuffle Furnace 6000 PDFAshraf MohamedAinda não há avaliações
- Pathology Vocabulary Review (Fox)Documento270 páginasPathology Vocabulary Review (Fox)DianaNitaAinda não há avaliações
- Material Safety Data Sheet: Section 1 - Product Identification and Company IdentificationDocumento9 páginasMaterial Safety Data Sheet: Section 1 - Product Identification and Company IdentificationecoscribdAinda não há avaliações
- Natural Gypsum MSDS 2017Documento6 páginasNatural Gypsum MSDS 2017Beautty Rahma ThikaAinda não há avaliações
- Soda Blaster ManualDocumento16 páginasSoda Blaster ManualmotomechAinda não há avaliações
- Msds-Oreas (Nram)Documento7 páginasMsds-Oreas (Nram)Heber Diaz ChavezAinda não há avaliações
- C-E Minerals: MSDS For Mulcoa 60/mulgrain 60/mulblast 60: Revision Date: 01/23/2013 Page 1 of 7Documento7 páginasC-E Minerals: MSDS For Mulcoa 60/mulgrain 60/mulblast 60: Revision Date: 01/23/2013 Page 1 of 7Muniruddin AmranAinda não há avaliações
- OSHA3768Documento6 páginasOSHA3768Shazayn KhanAinda não há avaliações
- LMR 2020Documento106 páginasLMR 2020VideoScoAinda não há avaliações
- ENVIRONMENTAL HEALTH AND SAFETY Module 1 To StudentsDocumento87 páginasENVIRONMENTAL HEALTH AND SAFETY Module 1 To StudentsNEERAJ KISHORE PAinda não há avaliações
- Silicosis in Artificial Stone Workers: Spectrum of Radiological High-Resolution CT Chest FindingsDocumento9 páginasSilicosis in Artificial Stone Workers: Spectrum of Radiological High-Resolution CT Chest FindingsFabio GigliottiAinda não há avaliações