Escolar Documentos
Profissional Documentos
Cultura Documentos
Clinical Lab Skills Assignment 2
Enviado por
Daniel WoodardDescrição original:
Título original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Clinical Lab Skills Assignment 2
Enviado por
Daniel WoodardDireitos autorais:
Formatos disponíveis
1 Running head: SKILLS LAB 2
Clinical Lab Skills Assignment 2
Erin D. Flanders
Winston Salem State University
2 Running head: SKILLS LAB 2
SKILLS LAB ASSIGNMENT 2
Unit II: Promoting and Maintaining Physiological and Psychosocial Integrity
Prior to this lab session, students will submit a typed response to the posted questions
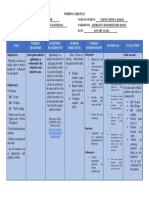
1. List the normal ranges for each vital sign.
Age
Temperature ()
Newborn
98.2 F (36.8 C)
(Axillary)
99.9 F (37.7 C) (Rectal)
98.6 F (37 C) (Oral)
98.6 F (37 C) (Oral)
98.6 F (37 C) (Oral)
98.6 F (37 C) (Oral)
96.8 F (36) (Oral)
1-3 yr
6-8 yr
10yr
Teens
Adults
> 70 yr
Pulse
(beats/min)
80-180
Respirations
(breaths/min)
30-60
Blood Pressure
(mm Hg)
73/55
80-140
75-120
75-110
60-100
60-100
60-100
20-40
15-25
15-25
15-20
12-20
15-20
90/55
95/75
102/62
102/80
120/80
120/80
2. List the equipment used for measuring each vital sign.
The equipment needed for temperature could be electronic and digital thermometers, tympanic
membrane thermometers, disposable single-use thermometers, temporal artery thermometers,
and automated monitoring devices. The equipment for measuring pulse is a stethoscope or a
Doppler ultrasound stethoscope. For respirations, one could use a stethoscope for listening or
monitoring arterial blood gas results and using a pulse oximeter to determine oxygenation of
blood. The equipment for blood pressure could be a sphygmomanometer, automated blood
pressure monitors, doppler ultrasound, and a direct electronic measurement.
3.
List rationales underlying each procedure.
The rationales for body temperature: The digital thermometer must be activated to record the
temperature.
3 Running head: SKILLS LAB 2
Discarding the probe cover ensures that it will not be reused accidentally on another
patient. Proper disposal prevents the spread of microorganisms. If necessary, the thermometer
should stay on the charger so that it is ready to use at all times.
If left unsupported, the weight of the probe tends to pull it away from the correct location.
The signal indicated the measurement is completed. The electronic thermometer provides a
digital display of the measured temperature.
Rationale for Obtaining Peripheral Pulse by Palpation:
Gloves are not usually worn to obtain a pulse measurement unless contact with blood or
body fluids is anticipated.
The site must be exposed for pulse assessment. Exposing only the site keeps the patient
warm and maintains his or her dignity.
The sensitive fingertips can feel the pulsation of the artery.
Rationale for Obtaining Respirations:
The patient may alter the rate of respirations if he or she is aware they are being counted.
Rationale for Obtaining Blood Pressure:
Measurement of blood pressure may temporarily impede circulation to the extremity.
The position of the arm can have a major influence when the blood pressure is measured.
This position places the brachial artery on the inner aspect of the elbow so that the bell or
diaphragm of the stethoscope can rest on it easily. This sitting position ensures accuracy.
4 Running head: SKILLS LAB 2
Clothing over the artery interferes with the ability to hear sounds and can cause
inaccurate blood pressure readings. A tight sleeve would cause congestion of blood and possibly
inaccurate readings.
Rationale for Obtaining All Vital Signs:
Assessment and measurement of vital signs at appropriate intervals provide important
data about the patient's health status. Bringing everything to the bedside conserves time and
energy. Arranging items nearby is convenient, saves time, and avoids unnecessary stretching and
twisting of muscles on the part of the nurse.
Hand hygiene and PPE prevent the spread of microorganisms. PPE is required based on
transmission precautions.
Identifying the patient ensures the right patient receives the intervention and helps
prevents errors.
Explanation relieves anxiety and facilitates cooperation. Dialogue encourages patient
participation and allows for individualized nursing care.
4.
List the time intervals for measuring the temperature by the various routes.
: if the patient has smoked, chewed gum, or consumed hot or cold food, wait 30 minutes before
taking an oral temperature. If patients axilla has been washed recently, wait 15 to 30 minutes
5.
List common sites for obtaining the pulse.
Common sites for obtaining the pulse are the temporal artery, carotid artery, brachial artery,
radial artery, femoral artery, popliteal artery, posterior tibial artery, and dorsalis pedis artery.
6.
List the correct procedure to obtain respiratory rate.
5 Running head: SKILLS LAB 2
The correct procedure to obtain a respiratory rate is to observe the patients respiration while
your fingers are still in place for the pulse measurement, note the rise and fall of the patients
chest, count the number of respirations with secondhand watch for 30 seconds then multiply by 2
to get the respiratory rate per minute. If respirations are abnormal, count for at least one full
minute. Note the depth and rhythm of the respirations. Remove gloves if you wore any and cover
the patient and help him or her to a position of comfort. Perform hand hygiene.
7.
List the correct procedure to obtain the blood pressure.
1. The correct procedure to obtain blood pressure: Check physician's order or
nursing plan for frequency of blood pressure measurement.
2. Perform hand hygiene and put on PPE, if indicated.
3. Identify the patient.
4. Close curtains around bed and close the door to the room. Discuss procedure with
patient and assess patient's ability to assist with the procedure. Validate that the
patient has relaxed for several minutes.
5. Select the appropriate arm for application of the cuff.
6. Have the patient assume a comfortable lying or sitting position with the forearm
supported at the level of the heart and the palm of the hand upward. If the patient
is sitting, have him or her sit back in the chair so that the chair supports his neck
or her back. In addition, make sure the patient keeps the legs uncrossed.
7. Expose the brachial artery by removing garments, or move a sleeve, if it is not too
tight, above the area where the cuff will be placed.
8. Palpate the location of the brachial artery. Center the bladder of the cuff over the
brachial artery, about midway on the arm. Line the artery marking on the cuff
6 Running head: SKILLS LAB 2
with the patient's brachial artery. The tubing should extend from the edge of the
cuff nearer the patient's elbow.
9. Wrap the cuff around the arm smoothly and snugly and fasten it.
10. Palpate the pulse at the brachial artery by pressing gently with the fingertips.
11. Tighten the screw valve on the air pump.
12. Inflate the cuff while continuing to palpate the artery. Note the point on the gauge
where the pulse disappears.
13. Deflate the cuff and wait 1 minute.
14. Assume a position that is no more than 3 feet away from the gauge.
15. Place the stethoscope earpieces in your ears.
16. Place the bell of the stethoscope firmly but with as little pressure as possible over
the brachial artery.
17. Pump the pressure 30 mm Hg above the point at which the systolic pressure was
palpated and estimated. Open the valve on the manometer and allow air to escape
slowly.
18. Note the point on the gauge at which the first faint, but clear, sound appears that
slowly increases in intensity. Note this number as the systolic pressure.
19. Note the point at which the sound completely disappears and record it as the
diastolic pressure.
20. Allow the remaining air to escape quickly. Repeat any suspicious reading, but
wait at least 1 minute. Deflate the cuff completely between attempts to check the
blood pressure.
7 Running head: SKILLS LAB 2
21. When measurement is completed, remove the cuff. Remove gloves, if worn.
Cover the patient and help him or her to a position of comfort.
22. Perform hand hygiene.
23. Clean the diaphragm of the stethoscope with the alcohol wipe. Clean and store the
sphygmomanometer, according to facility policy.
8.
List the correct procedure to obtain an oxygen saturation level.
The correct procedure to obtain an oxygen saturation level: 1. Review the chart for health
problems that would affect the reading. 2. Bring necessary equipment to the bedside stand or
overbed table. 3. Perform hand hygiene and put on PPE. 4. Identify the patient. 5. Close curtains
around the bed and close the door to the room, if possible. Explain what you are doing and why
you are going to do it. 6. Select an adequate site for application of the sensor. 8. Select the proper
equipment. 8. Prepare the monitoring site. Cleanse the selected area with the alcohol wipe or
disposable cleansing cloth. Allow the area to dry. 9. Apply the probe securely to skin. Make sure
that the light emitting sensor and the light-receiving sensor are aligned opposite each other. 10.
Connect the sensor probe to the pulse oximeter, turn the oximeter on, and check operation of the
equipment. 11. Set alarms on pulse oximeter. 12. Check oxygen saturation at regular intervals, as
ordered by primary care provider, nursing assessment, and signaled by alarms. Monitor
hemoglobin level. 13. Remove sensor on a regular basis and check for skin irritation or signs of
pressure. 14. Clean nondisposable sensors according to the manufacturers directions. Remove
PPE.
9.
Describe the formula for converting Fahrenheit to Centigrade.
8 Running head: SKILLS LAB 2
To convert from Fahrenheit, first subtract 32 from the temperature in Fahrenheit. Then multiply
the answer from the first step by five ninths (5/9). Add the degrees symbol and the temperature is
now in Centigrade (also known as Celsius)
9 Running head: SKILLS LAB 2
References
Carol R. Taylor, C. L. (2011). Fundamentals of Nursing: The Art and Science of Nursing Care.
Philadelphia: Wolters Kluwer Health.
Lynn, P. (2011). Taylor's Clinical Nursing Skills: A Nursing Process Approach. Philadelphia:
Wolters Kluwer Health.
Você também pode gostar
- Vital Signs Procedures ChecklistDocumento3 páginasVital Signs Procedures Checklistjuancristo90% (21)
- SOP Vital Sign Monitoring: Blood Pressure, Temperature, Pulse, RespirationDocumento3 páginasSOP Vital Sign Monitoring: Blood Pressure, Temperature, Pulse, RespirationShin Megami Auditore100% (1)
- Sepsis Case StudiesDocumento5 páginasSepsis Case StudiesRia Arcane0% (2)
- Vital Signs ProcedureDocumento10 páginasVital Signs ProcedureJojebelle Kate Iyog-cabanlet100% (3)
- Low Birth Weight Babies Respiratory DistressDocumento22 páginasLow Birth Weight Babies Respiratory Distressエド パジャロン100% (3)
- Vital Signs GuideDocumento4 páginasVital Signs GuideellithAinda não há avaliações
- Vital SignDocumento4 páginasVital SignGabriel JocsonAinda não há avaliações
- Self-Assessment Vital SignsDocumento2 páginasSelf-Assessment Vital SignscarlyAinda não há avaliações
- Taking The Vital SignsDocumento6 páginasTaking The Vital SignsAaron RoxasAinda não há avaliações
- Performance Evaluation ChecklistDocumento4 páginasPerformance Evaluation ChecklistJeleen LagaoAinda não há avaliações
- Osce Check List of Vital SignDocumento4 páginasOsce Check List of Vital SignAnonymous 0C4OZmRAinda não há avaliações
- Proper Vital Signs MonitoringDocumento7 páginasProper Vital Signs MonitoringCristoper BodionganAinda não há avaliações
- Vital Signs Procedure ChecklistDocumento10 páginasVital Signs Procedure Checklistako at ang exoAinda não há avaliações
- Checking The Vital SignsDocumento5 páginasChecking The Vital SignsRoger ViloAinda não há avaliações
- Measuring Vital SignsDocumento4 páginasMeasuring Vital SignsZYRAH LUKE E. VILBARAinda não há avaliações
- Guide to Measuring Vital SignsDocumento32 páginasGuide to Measuring Vital SignsJacqueline de AsisAinda não há avaliações
- Assessing Vital SignsDocumento3 páginasAssessing Vital SignsKaren Kates RafalloAinda não há avaliações
- BHS INGGRIS 1: Blood Pressure Recording ProceduresDocumento2 páginasBHS INGGRIS 1: Blood Pressure Recording ProceduresAgung PrasetyoAinda não há avaliações
- Vital Signs Taking ChecklistDocumento3 páginasVital Signs Taking ChecklistChelsea Manalo100% (1)
- Vital Signs Taking: Ms. Kristine Uy-Urgena, RN, MN College of Nursing Xavier University - Ateneo de Cagayan NCM 101 RleDocumento19 páginasVital Signs Taking: Ms. Kristine Uy-Urgena, RN, MN College of Nursing Xavier University - Ateneo de Cagayan NCM 101 RleJanieza BaltazarAinda não há avaliações
- Lab 2 Nursing Skill - Vital Sings 2021Documento10 páginasLab 2 Nursing Skill - Vital Sings 2021PHOEBE Ci100% (1)
- Vital Signs: Measuring Temperature, Pulse, Respiration & Blood PressureDocumento9 páginasVital Signs: Measuring Temperature, Pulse, Respiration & Blood PressureJeonoh FloridaAinda não há avaliações
- Basic Assessment and Basic Care ProceduresDocumento31 páginasBasic Assessment and Basic Care Proceduresjanice lopezAinda não há avaliações
- Checklist for VS TakingDocumento4 páginasChecklist for VS TakingGLAIZA PALATINOAinda não há avaliações
- Axillary MethodDocumento5 páginasAxillary MethodJerica Jaz F. VergaraAinda não há avaliações
- Assessing Vital SignsDocumento20 páginasAssessing Vital SignsKrish Lorrie100% (1)
- Checklist BPDocumento2 páginasChecklist BPHoneylouAzOpondaAinda não há avaliações
- Vital Signs 2024Documento50 páginasVital Signs 2024gntawfeqAinda não há avaliações
- Midterm Procedures With RationaleDocumento8 páginasMidterm Procedures With RationaleAisha CorobongAinda não há avaliações
- Summary OsceDocumento5 páginasSummary OsceAshley IshikaAinda não há avaliações
- Blood PressureDocumento18 páginasBlood PressureManar Magdy100% (1)
- ChecklistDocumento4 páginasChecklistjyoti singhAinda não há avaliações
- Worksample 2Documento1 páginaWorksample 2api-248146877Ainda não há avaliações
- Taking Blood PressureDocumento3 páginasTaking Blood PressureApril Iren Claire BalabalaAinda não há avaliações
- Module 3 CaregivingDocumento10 páginasModule 3 CaregivingRioja Anna MilcaAinda não há avaliações
- RD GuideDocumento10 páginasRD GuideRicah Mae AbingAinda não há avaliações
- Basic First Aid Vital Signs and Bandaging Techniques 11Documento42 páginasBasic First Aid Vital Signs and Bandaging Techniques 11Darlene CarmonaAinda não há avaliações
- Rubrics Vital Signs TakingDocumento6 páginasRubrics Vital Signs TakingRichard SluderAinda não há avaliações
- Postural HypotensionDocumento3 páginasPostural HypotensionSimran JosanAinda não há avaliações
- Vital Sign: Measuring A Radial Pulse, Counting Respiration, and Taking Axillary Temperature by Glass ThermometerDocumento17 páginasVital Sign: Measuring A Radial Pulse, Counting Respiration, and Taking Axillary Temperature by Glass ThermometerPrischeilla InkiriwangAinda não há avaliações
- Patient Assessment and Vital SignsDocumento6 páginasPatient Assessment and Vital SignsSai VijayaAinda não há avaliações
- CheatDocumento107 páginasCheatAngelica ValdezAinda não há avaliações
- Checklist For The VS Measurement (TPR and BP) A. Temperature A.1. Axillary Temperature (Digital Thermometer) Done Needs PracticeDocumento3 páginasChecklist For The VS Measurement (TPR and BP) A. Temperature A.1. Axillary Temperature (Digital Thermometer) Done Needs PracticeCyrillAinda não há avaliações
- Measuring Vital Signs: Lisa YusidaDocumento12 páginasMeasuring Vital Signs: Lisa YusidaLisa YusidaAinda não há avaliações
- Vital Signs Outline - NCM 103LDocumento4 páginasVital Signs Outline - NCM 103LataraxialliAinda não há avaliações
- Blood PressureDocumento9 páginasBlood Pressuregenevieve kryzleiAinda não há avaliações
- BIO 333 Lab2 Measuring Blood Pressure and RateDocumento2 páginasBIO 333 Lab2 Measuring Blood Pressure and RateLee nareoAinda não há avaliações
- SOP Guide for Measuring Vital SignsDocumento3 páginasSOP Guide for Measuring Vital SignsFitria NorkhalidaAinda não há avaliações
- To Gain The Trust and Cooperation of The Clients: Done Not DoneDocumento2 páginasTo Gain The Trust and Cooperation of The Clients: Done Not DoneBulajyo Pangngay JolinaAinda não há avaliações
- Common Tools and Equipment in Taking Vital Sign Thermometer: Lesson 3Documento3 páginasCommon Tools and Equipment in Taking Vital Sign Thermometer: Lesson 3Skye CheonAinda não há avaliações
- Standards of Operational Procedures: Measurement of Vital SignsDocumento6 páginasStandards of Operational Procedures: Measurement of Vital SignsSarita PurnamaAinda não há avaliações
- Demo On Vital SignsDocumento5 páginasDemo On Vital SignsLawrence Cada Nofies100% (3)
- Assessing Blood PressureDocumento4 páginasAssessing Blood PressureLiana Koh VillanuevaAinda não há avaliações
- Format-for-Blood Pressure-ProceduresDocumento3 páginasFormat-for-Blood Pressure-ProceduresfileacademicsAinda não há avaliações
- Vital Signs Vital Signs: Importance: ImportanceDocumento6 páginasVital Signs Vital Signs: Importance: ImportanceTyron KristianAinda não há avaliações
- Vital Signs Written ReportDocumento7 páginasVital Signs Written Reportkarl montanoAinda não há avaliações
- Guide student skill lab examDocumento15 páginasGuide student skill lab examAhmedrashaad MohammedAinda não há avaliações
- PROCEDURES IN VITAL SIGNS With RationaleDocumento3 páginasPROCEDURES IN VITAL SIGNS With Rationalegoyabeb59Ainda não há avaliações
- Procedure Steam Inhalation.Documento10 páginasProcedure Steam Inhalation.PINKI DEBAinda não há avaliações
- Assessing Blood PressureDocumento3 páginasAssessing Blood PressureSean DuayAinda não há avaliações
- Thoracocentasis: INTRODUCTION:-Thoracentasis Also Known As The Thoracocentasis or Plural Tap Is AnDocumento7 páginasThoracocentasis: INTRODUCTION:-Thoracentasis Also Known As The Thoracocentasis or Plural Tap Is AnaparnaAinda não há avaliações
- Human Diseases 8th Edition Zelman Test BankDocumento19 páginasHuman Diseases 8th Edition Zelman Test BankAshleyWilsonicye100% (11)
- Case Scenario - Nursing Care Plan (DR - Magsingal)Documento1 páginaCase Scenario - Nursing Care Plan (DR - Magsingal)Cristyl Shine BariaoAinda não há avaliações
- Guidelines for Exiting Health Case ManagementDocumento2 páginasGuidelines for Exiting Health Case ManagementDhamscen Lopez EscurelAinda não há avaliações
- NCP FdarDocumento11 páginasNCP FdarJhaymee PinedaAinda não há avaliações
- PPT Skenario A - G6 - Blok 14Documento66 páginasPPT Skenario A - G6 - Blok 14Ellysa CarolinnAinda não há avaliações
- Basic Assessment and Basic Care ProceduresDocumento31 páginasBasic Assessment and Basic Care Proceduresjanice lopezAinda não há avaliações
- Munder Aljanna Marie Nursing Assessment II Part 2 CPDocumento3 páginasMunder Aljanna Marie Nursing Assessment II Part 2 CPMohamadhizam M. PangcatanAinda não há avaliações
- Cod IDocumento11 páginasCod IMira AriantiAinda não há avaliações
- 3RD Quarter ExamDocumento6 páginas3RD Quarter ExamIvy Metchellyn OlazoAinda não há avaliações
- Simulator Model For Abnormal Pulse RateDocumento4 páginasSimulator Model For Abnormal Pulse RatemuthukumartharaniAinda não há avaliações
- NCP FeverDocumento3 páginasNCP FeverJenner NatividadAinda não há avaliações
- Questions G 4Documento8 páginasQuestions G 4Nader Smadi100% (2)
- Staffing Power Point Final EditionDocumento36 páginasStaffing Power Point Final EditionAnusha VergheseAinda não há avaliações
- F2F MeaslesDocumento7 páginasF2F MeaslesMichelle Gliselle Guinto MallareAinda não há avaliações
- Dibas PHD SynopsisDocumento8 páginasDibas PHD SynopsisDibash HembramAinda não há avaliações
- NCP FinalDocumento4 páginasNCP Finalmarkanthony3903Ainda não há avaliações
- Subjective: Short Term Goal: Independent: Short Term EvaluationDocumento2 páginasSubjective: Short Term Goal: Independent: Short Term EvaluationKyla Castro100% (1)
- Pediatric Assessment Tool Infancy to ToddlerDocumento6 páginasPediatric Assessment Tool Infancy to ToddlerMaha AmilAinda não há avaliações
- Adult Invig Inf TableDocumento6 páginasAdult Invig Inf TableRaoulSusanto SusantoAinda não há avaliações
- Tourniquet Use at The Boston Marathon Bombing: Lost in TranslationDocumento6 páginasTourniquet Use at The Boston Marathon Bombing: Lost in TranslationFabio Ferreira SaAinda não há avaliações
- Workshop On Early Warning Score System - Ali HaedarDocumento61 páginasWorkshop On Early Warning Score System - Ali HaedarGede Kevin Adhitya SaputraAinda não há avaliações
- Nursing Department: Care To Learn, Learn To Care Embracing World Class StandardsDocumento17 páginasNursing Department: Care To Learn, Learn To Care Embracing World Class Standardsmalinda0% (1)
- NCP - Chicken PoxDocumento4 páginasNCP - Chicken Poxhanna_lim0% (1)
- NURSING CARE PLAN - Hepatitis ADocumento2 páginasNURSING CARE PLAN - Hepatitis Aderic74% (19)
- Clincial Skills ChecklistDocumento6 páginasClincial Skills Checklistapi-97770622Ainda não há avaliações
- Normal Values of Vital SignsDocumento3 páginasNormal Values of Vital SignsMela VincoAinda não há avaliações
- Ponr InpDocumento23 páginasPonr InpAshen GiradoAinda não há avaliações
- Lesson 1 Use Tools Equipment Paraphernalia in CaregivingDocumento47 páginasLesson 1 Use Tools Equipment Paraphernalia in CaregivingÊirene Ballon100% (1)