Escolar Documentos
Profissional Documentos
Cultura Documentos
10 Pathophysiology Diagram
Enviado por
Dizerine Mirafuentes RolidaDescrição original:
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
10 Pathophysiology Diagram
Enviado por
Dizerine Mirafuentes RolidaDireitos autorais:
Formatos disponíveis
B.
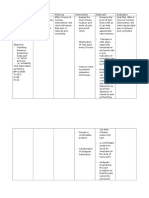
DIAGRAM OF PATHOPHYSIOLOGY
Non Modifiable
Modifiable
Age (54 y/o)
Smoking
Male
Diet high in fat
Alcohol Consumption
Nonspecific injury to arterial wall (endothelial injury)
Desquamation of endothelial living
decreased elasticity of blood vessels
and formation of plaques on blood vessels
Increased permeability or adhesion of molecules
Lipids (LDL, VLDL) and platelets assimilate in the area
Oxidized LDL attracts monocytes and macrophages to the site
Plaques begin to form from cells w/c imbibed into the endothelium
narrowing of the Blood Vessels
Lipids are engulfed by the cells (foam cells) and smooth
Muscle cells develop.
Disruption of plaque continuous aggregation of platelets
Thrombus formation
necrosis and scarring of the vascular endothelium
52
Rapid increase in size of the thrombus in coronary artery wall
Coronary Artery Disease (CAD)
Nursing Management
1. Monitor blood pressure, apical heart
rate, and respirations every 5
minutes during an anginal attack.
2. Maintain continuous ECG monitoring
or obtain a 12-lead ECG, as
directed, monitor for arrhythmias and
ST elevation.
3. Place patient in comfortable position
and administer oxygen, if prescribed,
to enhance myocardial oxygen
supply.
4. Identify specific activities patient
may engage in that are below the
level at which anginal pain occurs.
5. Reinforce the importance of notifying
nursing staff whenever angina pain
is experienced.
6. Encourage supine position for
dizziness caused by antianginals.
7. Be alert to adverse reaction related
to abrupt discontinuation of betaadrenergic blocker and calcium
channel blocker therapy. These drug
must be tapered to prevent a
rebound phenomenon; tachycardia,
increase in chest pain, and
hypertension.
Angina, Shortness of
breath, Dyspnea,
Heart Attack
Medical Management
1. Antianginal medications
(nitrates, beta-adrenergic
blockers, calcium channel
blockers, and angiotensin
converting enzyme inhibitors) to
promote a favorable balance of
oxygen supply and demand.
2. Antilipid medications to
decrease blood cholesterol and
tricglyceride levels in patients
with elevated levels.
3. Antiplatelet agents to inhibit
thrombus formation.
4. Folic acid and B complex
vitamins to reduce
homocysteine levels.
Surgical Management
1. Percutaneous
transluminal coronary
angioplasty or
intracoronary
atherectomy, or
placement of
intracoronarystent.
2. Coronary artery
bypass grafting.
3. Transmyocardial
revascularization.
53
8. Explain
to
the
patient
the
importance of anxiety reduction to
assist to control angina.
9. Teach
the
patient
relaxation
techniques.
10. Review specific factors that affect
CAD development and progression;
highlight those risk factors that can
be modified and controlled to
reduce the risk.
Prognosis
Restoration of Health
If not treated:
Good Prognosis
Chronic Obstructive Pulmonary Disease
(COPD)
Anterior wall MI (Myocardial Infarction)
Bad Prognosis
Death
Você também pode gostar
- NCLEX Practice Test For OncologyDocumento26 páginasNCLEX Practice Test For OncologyDizerine Mirafuentes Rolida100% (4)
- Basic Concept Map - RH IncompatibilityDocumento1 páginaBasic Concept Map - RH IncompatibilityTechnoShindoAinda não há avaliações
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationDocumento4 páginasAssessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationTedd CamilingAinda não há avaliações
- Duran, Fatima Medriza B. - Partial Npi For RleDocumento11 páginasDuran, Fatima Medriza B. - Partial Npi For Rlenot your medz duranAinda não há avaliações
- Case Scenario Peritoneal DialysisDocumento9 páginasCase Scenario Peritoneal DialysisDE LEON, CRONICA FAY G.Ainda não há avaliações
- Sample Club ConstitutionDocumento4 páginasSample Club ConstitutionDizerine Mirafuentes RolidaAinda não há avaliações
- 01.54.107033-1.6 SE-12 Series Electrocardiograph User Manual - EDAN 2 PDFDocumento182 páginas01.54.107033-1.6 SE-12 Series Electrocardiograph User Manual - EDAN 2 PDFFelix LeeAinda não há avaliações
- Zimbabwe School Examinations Council: Physical Education, Sport & Mass Displays 4002/02Documento8 páginasZimbabwe School Examinations Council: Physical Education, Sport & Mass Displays 4002/02Elton Maregere100% (7)
- Chest X-RayDocumento101 páginasChest X-RayRizka RamadaniAinda não há avaliações
- Drug Study and NCP (Craniotomy)Documento2 páginasDrug Study and NCP (Craniotomy)Deinielle Magdangal Romero100% (1)
- NafarinDocumento2 páginasNafarinianecunar100% (2)
- Soapie Charting: Date/ Time/ ShiftDocumento2 páginasSoapie Charting: Date/ Time/ Shiftspain michaelisAinda não há avaliações
- NCPDocumento4 páginasNCPyasayayasay yasayAinda não há avaliações
- Liceo de Cagayan University College of NursingDocumento29 páginasLiceo de Cagayan University College of Nursingchin41686Ainda não há avaliações
- NCP Ch31 p991-992Documento2 páginasNCP Ch31 p991-992Ala'a Abd Mansor100% (2)
- Concept Map of Nasal ObstructionDocumento2 páginasConcept Map of Nasal ObstructionChad Viajar100% (1)
- Cefipime HCL (AXERA)Documento2 páginasCefipime HCL (AXERA)Kristine YoungAinda não há avaliações
- Ceftriaxone Drug StudyDocumento2 páginasCeftriaxone Drug StudyRose EchevarriaAinda não há avaliações
- Pathophysiology of Meniere FinalDocumento1 páginaPathophysiology of Meniere Final1S VILLEGAS GabrielAinda não há avaliações
- SildenafilDocumento2 páginasSildenafilSheryl Ann PedinesAinda não há avaliações
- Nursing Care Plan NCP Group 3 Fatigue ..Documento2 páginasNursing Care Plan NCP Group 3 Fatigue ..Aerron Severus Secano ShuldbergAinda não há avaliações
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NDocumento2 páginasNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaAinda não há avaliações
- Discharge Plan Methods InstructionsDocumento5 páginasDischarge Plan Methods InstructionsKirk CabasaAinda não há avaliações
- CASE STUDY PheumoniaDocumento5 páginasCASE STUDY PheumoniaEdelweiss Marie CayetanoAinda não há avaliações
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Client Centered PathophysiologyDocumento3 páginas"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Client Centered PathophysiologyCarl Elexer Cuyugan Ano50% (2)
- CiticolineDocumento2 páginasCiticolineKerima Danica Lising GayoAinda não há avaliações
- NCPDocumento4 páginasNCPAndrea BroccoliAinda não há avaliações
- NCP Ineffective Cardiopulmonary PerfusionDocumento3 páginasNCP Ineffective Cardiopulmonary PerfusionjamiemapanaoAinda não há avaliações
- University of Santo Tomas College of Nursing NCM 103 Ms Case # 2Documento4 páginasUniversity of Santo Tomas College of Nursing NCM 103 Ms Case # 2steffiAinda não há avaliações
- Amlodipine CPDocumento2 páginasAmlodipine CPRose EchevarriaAinda não há avaliações
- Pa Tho Physiology of ScoliosisDocumento1 páginaPa Tho Physiology of Scoliosisbwester2222Ainda não há avaliações
- Drug Study - Epidural AnesthesiaDocumento5 páginasDrug Study - Epidural AnesthesiaMarie PotayreAinda não há avaliações
- LeadershipDocumento1 páginaLeadershipchoobiAinda não há avaliações
- DP HyperthyroidismDocumento6 páginasDP HyperthyroidismTracy May CandolitaAinda não há avaliações
- PHASE 2 NCP (Injury, Risk For Bleeding)Documento3 páginasPHASE 2 NCP (Injury, Risk For Bleeding)NE TdrAinda não há avaliações
- Mosegor Vita Is A Vitamin SupplementDocumento1 páginaMosegor Vita Is A Vitamin SupplementlolabayAinda não há avaliações
- Cloxacillin: By: Edamarie B. CabasaDocumento11 páginasCloxacillin: By: Edamarie B. CabasaIrene Grace BalcuevaAinda não há avaliações
- NCP H MoleDocumento6 páginasNCP H MoleMina RacadioAinda não há avaliações
- Posterior Mold: PurposeDocumento3 páginasPosterior Mold: PurposeSheryl Ann Barit PedinesAinda não há avaliações
- SLCN Gazette Magazine, Volume 1, Issue 1, 2019Documento20 páginasSLCN Gazette Magazine, Volume 1, Issue 1, 2019Mayzelle RizAinda não há avaliações
- NCPDocumento3 páginasNCPArien CaleonAinda não há avaliações
- Revised NCP (Baiae)Documento9 páginasRevised NCP (Baiae)Jennifer BactatAinda não há avaliações
- Ineffective Breathing PatternDocumento7 páginasIneffective Breathing PatternJanmae JivAinda não há avaliações
- Potts Disease NCP .. JustificationDocumento8 páginasPotts Disease NCP .. JustificationMicah SalesAinda não há avaliações
- Pathophysiology PRINTDocumento1 páginaPathophysiology PRINTNichole Audrey SaavedraAinda não há avaliações
- NCP Acute PainDocumento3 páginasNCP Acute Painmanoelsterg50% (2)
- Discharge Instructions - Laparoscopic Cholecystectomy: ActivityDocumento2 páginasDischarge Instructions - Laparoscopic Cholecystectomy: ActivityAnne Marie Angelica BilonoAinda não há avaliações
- Clarithromycin Drug StudyDocumento1 páginaClarithromycin Drug StudyDivine LavaAinda não há avaliações
- NCP Acute Pain Related To Presence of Postoperative Surgical IncisionDocumento2 páginasNCP Acute Pain Related To Presence of Postoperative Surgical IncisionPebbles PangilinanAinda não há avaliações
- Acute Pain OsteosarcomaDocumento8 páginasAcute Pain OsteosarcomaMaryjoy Gabriellee De La Cruz100% (1)
- OsteomyelitisDocumento1 páginaOsteomyelitisJohara Mae De RamaAinda não há avaliações
- Ov Ov OvDocumento15 páginasOv Ov OvHayyana Mae Taguba LadiaAinda não há avaliações
- Pathophysiology PDFDocumento3 páginasPathophysiology PDFJenievieve MerzaAinda não há avaliações
- Case Study AppendicitisDocumento6 páginasCase Study AppendicitisPrincess Camille ArceoAinda não há avaliações
- Schematic Diagram Pathophysiology (Book-Based) COPD and TuberculosisDocumento1 páginaSchematic Diagram Pathophysiology (Book-Based) COPD and Tuberculosispragna novaAinda não há avaliações
- (Brand Name) & Date Ordered General Class and Family Specific IndicationDocumento2 páginas(Brand Name) & Date Ordered General Class and Family Specific IndicationNicole Grace VillegasAinda não há avaliações
- PathophysiologyDocumento4 páginasPathophysiologyDante SalesAinda não há avaliações
- Gout N C P BY BHERU LALDocumento1 páginaGout N C P BY BHERU LALBheru LalAinda não há avaliações
- NCP N SOPIEDocumento9 páginasNCP N SOPIEDonna DavidAinda não há avaliações
- Nursing Care of Uremic SyndromeDocumento11 páginasNursing Care of Uremic Syndromeyoedha_banditozz50% (2)
- Drug-Study NCPDocumento5 páginasDrug-Study NCPMURILLO, FRANK JOMARI C.Ainda não há avaliações
- RituximabDocumento2 páginasRituximabBigBoosting100% (2)
- Aspirin Drug SummDocumento2 páginasAspirin Drug SummWarren0% (1)
- 10 Pathophysiology DiagramDocumento3 páginas10 Pathophysiology DiagramDizerine Mirafuentes RolidaAinda não há avaliações
- Medically Compromised PatientDocumento32 páginasMedically Compromised Patientمحمد عبدالهادي إسماعيلAinda não há avaliações
- Iii. Laboratory and Diagnostic Examinations Hematology October 24, 2014 Examination Result Normal Values InterpretationDocumento22 páginasIii. Laboratory and Diagnostic Examinations Hematology October 24, 2014 Examination Result Normal Values InterpretationDizerine Mirafuentes RolidaAinda não há avaliações
- Ovarian Serous Cystadenoma of Mrs. A of Bishop Joseph Regan Memorial Hospital 2014Documento1 páginaOvarian Serous Cystadenoma of Mrs. A of Bishop Joseph Regan Memorial Hospital 2014Dizerine Mirafuentes RolidaAinda não há avaliações
- Symptomatology Symptomatology Actual Symptom Implication: Health-Topics/topics/cad/signs - HTMLDocumento5 páginasSymptomatology Symptomatology Actual Symptom Implication: Health-Topics/topics/cad/signs - HTMLDizerine Mirafuentes RolidaAinda não há avaliações
- Ix. Pharmacological ManagementDocumento20 páginasIx. Pharmacological ManagementDizerine Mirafuentes RolidaAinda não há avaliações
- Review Pa MoreDocumento150 páginasReview Pa MoreDizerine Mirafuentes RolidaAinda não há avaliações
- COPAR ReadingDocumento2 páginasCOPAR ReadingDizerine Mirafuentes RolidaAinda não há avaliações
- A Typology of Nursing Problems in Family Nursing PracticeDocumento3 páginasA Typology of Nursing Problems in Family Nursing PracticeDizerine Mirafuentes RolidaAinda não há avaliações
- 10 Pathophysiology DiagramDocumento3 páginas10 Pathophysiology DiagramDizerine Mirafuentes RolidaAinda não há avaliações
- Pharmacology-Final Na JudDocumento17 páginasPharmacology-Final Na JudDizerine Mirafuentes RolidaAinda não há avaliações
- 5 AssessmentDocumento15 páginas5 AssessmentDizerine Mirafuentes RolidaAinda não há avaliações
- Alterations in Vascular IntegrityDocumento1 páginaAlterations in Vascular IntegrityDizerine Mirafuentes RolidaAinda não há avaliações
- VI. Pathophysiology A. Written PathophysiologyDocumento2 páginasVI. Pathophysiology A. Written PathophysiologyDizerine Mirafuentes RolidaAinda não há avaliações
- Ix. Pharmacologic Management Brand Name Classification Indication Mechanism of Action Dosage and Frequency Adverse Reactions Nursing ConsiderationDocumento21 páginasIx. Pharmacologic Management Brand Name Classification Indication Mechanism of Action Dosage and Frequency Adverse Reactions Nursing ConsiderationDizerine Mirafuentes RolidaAinda não há avaliações
- Maternal ReviewerDocumento61 páginasMaternal ReviewerDizerine Mirafuentes Rolida100% (1)
- Review of AnaphysioDocumento8 páginasReview of AnaphysioDizerine Mirafuentes RolidaAinda não há avaliações
- Iv. Review of Anatomy and PhysiologyDocumento9 páginasIv. Review of Anatomy and PhysiologyDizerine Mirafuentes RolidaAinda não há avaliações
- Ch42 NCP IneffectiveCoping 1075-1076Documento2 páginasCh42 NCP IneffectiveCoping 1075-1076Dizerine Mirafuentes RolidaAinda não há avaliações
- Article Ii Declaration of Principles and State PoliciesDocumento59 páginasArticle Ii Declaration of Principles and State PoliciesDizerine Mirafuentes RolidaAinda não há avaliações
- Leadership and Management LectureDocumento32 páginasLeadership and Management LectureDizerine Mirafuentes RolidaAinda não há avaliações
- A Detailed Lesson Plan in SCIENCE UPDATED 1Documento10 páginasA Detailed Lesson Plan in SCIENCE UPDATED 1Denver Jewel AlcaydeAinda não há avaliações
- Krok Key WordsDocumento50 páginasKrok Key WordsKeller 0Ainda não há avaliações
- BRN 301-400 PediDocumento46 páginasBRN 301-400 PediJoyzoeyAinda não há avaliações
- All MRCP Theory Notes For DR Abeer in One PDFDocumento3.151 páginasAll MRCP Theory Notes For DR Abeer in One PDFRumana Ali100% (2)
- Libble Eu PDFDocumento15 páginasLibble Eu PDFemilAinda não há avaliações
- Digital Image Processing Clusters: CLUSTER 1A - Statistical Classification Algorithms, Logistic RegressionDocumento2 páginasDigital Image Processing Clusters: CLUSTER 1A - Statistical Classification Algorithms, Logistic Regressionneo223344Ainda não há avaliações
- Dr. Basuki - Gagal JantungDocumento86 páginasDr. Basuki - Gagal JantungGifanichan MvpshawolandromedaAinda não há avaliações
- Abdominal Examination PrintDocumento8 páginasAbdominal Examination Printmofath6854Ainda não há avaliações
- Electrocardiografia BasicaDocumento49 páginasElectrocardiografia BasicaENRIQUEVERSAGAinda não há avaliações
- Pnle Exam Part 1Documento14 páginasPnle Exam Part 1bAinda não há avaliações
- On-X® Mitral Heart ValveDocumento20 páginasOn-X® Mitral Heart ValveChaitanya Sai TAinda não há avaliações
- 1856 George R. Calhoun Report of The Consulting Surgeon On SpermatorrhoeaDocumento25 páginas1856 George R. Calhoun Report of The Consulting Surgeon On SpermatorrhoeaLeandro LuccisanoAinda não há avaliações
- How I Bypassed My Bypass-SurgeryDocumento4 páginasHow I Bypassed My Bypass-Surgeryharinag49Ainda não há avaliações
- Ecg QuizDocumento5 páginasEcg QuizCHOIR LIFEAinda não há avaliações
- Cyanotic Congenital Heart DiseaseDocumento21 páginasCyanotic Congenital Heart DiseaseAdditi SatyalAinda não há avaliações
- Angiography 50%Documento17 páginasAngiography 50%Nova SipahutarAinda não há avaliações
- SCA IT Interactive Display PDFDocumento15 páginasSCA IT Interactive Display PDFRameshAinda não há avaliações
- Practice Test Planner - 2023-24 (TYM) Phase-02Documento4 páginasPractice Test Planner - 2023-24 (TYM) Phase-02harsh0401kingAinda não há avaliações
- Pharmacology Bullet ReviewDocumento342 páginasPharmacology Bullet ReviewBenjamin Joel BreboneriaAinda não há avaliações
- Sport - Cardiology Course - Program PDFDocumento4 páginasSport - Cardiology Course - Program PDFNico IonaşcuAinda não há avaliações
- Basic Business Statistics 12th Edition Berenson Test BankDocumento26 páginasBasic Business Statistics 12th Edition Berenson Test BankBobbyMasseyaoep100% (52)
- CVS ExamDocumento35 páginasCVS Examtravis efraimAinda não há avaliações
- Enrollment FormDocumento3 páginasEnrollment FormgauravpassionAinda não há avaliações
- Electrocardiogram EcgDocumento10 páginasElectrocardiogram EcgBaha'aeddin HammadAinda não há avaliações
- Heart and Neck VesselsDocumento3 páginasHeart and Neck VesselsMark ElbenAinda não há avaliações
- Cardiomegaly ArticlebykashafshehzadDocumento7 páginasCardiomegaly Articlebykashafshehzadbellatania yudaAinda não há avaliações
- Articulo 6 - Non-Invasive - Flexible - and - Stretchable - Wearable - Sensors - With - Nano-Based - Enhancement - For - Chronic - Disease - CareDocumento38 páginasArticulo 6 - Non-Invasive - Flexible - and - Stretchable - Wearable - Sensors - With - Nano-Based - Enhancement - For - Chronic - Disease - CareGuillermo Prieto AvalosAinda não há avaliações