Escolar Documentos
Profissional Documentos
Cultura Documentos
63: Perio Therapy II
Enviado por
NYUCD17Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
63: Perio Therapy II
Enviado por
NYUCD17Direitos autorais:
Formatos disponíveis
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
[Diagnosis and Treatment of Oral Diseases] [Lecture 51/52] [Periodontal Therapy I] by
Dr. ???]
[Slide 1] [Periodontal Therapy I]
[Dr. ???] You ready to go? So, I'm probably going to probably do a little bit of review today.
But talk almost entirely of initial therapy.
[Slide 2] [Initial Therapy]
[Dr. ???] Initial therapy is thought to be the most critical component of periodontal therapy.
Initial therapy really encompasses a number of elements. One of which is debridement - scaling
and root planing. Scaling. Another one is behavioral in the sense that it encompasses patient
education with respect to plaque control. And the more your patient understands why he or she is
controlling plaque, the more likely it is that he or she will continue to do that. And another key
element of initial therapy is whats called re-evalulation. Its outcome assessment. So, and these
are the goals. So basically, the overall goal is to stabilize and control the infection itself.
[Slide 3] [The goals of conservative, non-surgical]
[Dr. ???] Initial therapy is termed anti-infective therapy by some. And by definition, initial
therapy is non-surgical which is to say that its a closed procedure. Its done with instruments that
are placed subgingivally as is indicated. And one can only feel the site as opposed to visualize a
site. And when we think about a next step after initial therapy, which well talk about in detail - if
initial therapy fails to stabilize the infection, then we begin to think about actually visualizing the
site of infection through a surgical procedure. So thats the first element. The second is creating a
biocompatible root surface, which Ill talk in some detail about. We definitely want to remove
infected tissue. Its called degranulation- where we remove the hyperplastic, hyper vascular
tissue. And then, finally, determining the host response. And thats not only fro the point of view
of biology, which is another way of saying how does you patients immune system respond to
therapy, how well does the immune system in conjunction with treatment stabilize or manage
infection. But also, again, from a behavioral standpoint, does the patient understand and more
importantly, is compliant with respect to plaque control. So, thats sort of a two-fold approach to
host response. One being physiological, the other being behavioral.
[Slide 4] [What is therapeutic success?]
[Dr. ???] So what do we talk about when we think about therapeutic success?
[Slide 5] [Success following treatment]
[Dr. ???] And there are basically three outcomes that we can expect. One is compete
regeneration of all diseased tissues. Basically eliminating the infection, at the same time
regenerating all damaged and diseased tissues in the site. The second is healing. Basically
stabilization. And cessation of the stabilization of the progressive breakdown of the epithelial
attachment. So thats also called repair. So finally, simply the elimination of inflammation. So, the
first one, by definition, or by my definition gets 3 stars, the second outcome gets 2 stars, and the
third outcome, 1 star.
[Slide 6] [Complete regeneration]
[Dr. ???] So whats complete regeneration? Well, it only happens under one set of conditions.
And thats with respect to gingivitis. We know that simple plaque induced gingivitis is essentially
completely reversible. That given enough time, all the tissues that were diseased during the
inflammatory process are capable of reversing the disease process and repopulating the
!1
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
connective tissue with healthy cells. By contrast, periodontitis, which involves breakdown of the
epithelial attachment is not reversible.
[Slide 7] [Pocket healing (repair) and]
[Dr. ???] And what we can hope for is basicallyas it says here cessation of attachment loss.
Stopping the progression of the disease. So the whole thing of attachment loss in areas where
pockets were in evidence typically by means of a long junctional epithelial. Now that may be a
new term for you. Thats something youre familiar with, or not? Yes? Ok..So were not going
to spend whole lot of time about that. But for 2 fundamental reasons, we get reduction in probing
depth. One due to the long junctional epithelium formation and for the second due to shrinkage or
reduction in the size of inflamed and edematous tissue.
[Slide 8] [Elimination of inflammation]
[Dr. ???] And finally, we can eliminate inflammation without reducing probing depth, which is
a viable outcome, but not one that we really- we would really like to see repair. Repair is the most
we can expect from initial therapy.
[Slide 9] [The blue horizontal lines]
[Dr. ???] So here you see, um, the free gingival margin. Lets see. Up here is the free gingival
margin. This is a periodontal pocket. This is a cross section where you have the keratinized oral
epithelium, the sulcular epithelium. This is the enamel, this is the root surface. And this is the
periodontal pocket There is the free gingival margin, the epithelial attachment, or what remains of
the epithelial attachment. Where did the epithelial attachment begin, typically, in health? Where
would the epithelial attachment be in health? It would be near the CEJ. So this is really
representing the periodontal pocket. And finally, theres what remains of the PDL. You've got the
intact PDL here. And then, here, you can see these fibers are damaged but not gone away. And
this represents probably on the order of 1/10 of a millimeter. This will repair and actually
regenerate but when you look at the system overall, we really think about thats the idea that the
PDL cannot regenerate. Ok. So this is the pocket, and then this is the infiltrate- the inflammatory
infiltrate. Ok.
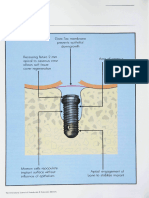
[Slide 10] [Healing subsequent to]
[Dr. ???] Now, when we treat cells, ok, sorry, when we treat the pocket, we are basically
exciting diseased tissue form the sulcular epithelium. Were making this part of the root what I
call biocompatible, and Ill explain that in a moment. Here is the curette in place. And the curette
stops where the epithelial attachment begins. Here it stops- theres still some damaged fiber. and
so the action of this instrument is to remove and root plane- remove debris, necrotic cementum,
calculus deposits, bacteria and then make this part as smooth as it possible OK? Now in general,
what happens is that when you have an empty space like this, its filled rather rapidly with repopulated with some cell type. And it turns out that the epithelium or the epithelial cells migrate
the most rapidly of the 4 populations of cells that are available. There are epithelial cells, there are
gingival connective tissue cells, there are bone cells. This is bone. And, finally, there are cells
from the PDL. Now if the PDL cells repopulated this area, then you can conceivably regenerate
the PDL itself and regenerate- recreate the attachment. But the epithelial cells win. And so what
happens is the epithelial cells populate the pocket.
[Slide 11] [Long Junctional Epithelium]
[Dr. ???] And they form whats called the long junctional epithelium. Now that is a barrier to
not only to the periodontal probe but its a barrier for bacteria. So its tantamount to a new
attachment but its not a new attachment - its a long junctional epithelium. Its not a connective
!2
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
tissue anatomical structure. Its made up of epithelial elements. And so this is what we can hope
for, in terms of significant positive outcome form non- surgical therapy. And here you can see a
few of these, fibers, the PDL fibers that were damaged have regenerated, and with it, some little
amount of bone regenerates. But again, this is a very, very, very small proportion of what amounts
to the epithelial apparatus. Now the smoother, the more biocompatible that root surface is, the
more likely it will form a long junctional epithelium. So theres a physiological basis or rationale
to what we call root plane. Root planing is simply creating a biocompatible surface upon which
epithelial cells will migrate, or through which they will migrate. And then form the long
junctional epithelium. Now does anyone have any questions about this? Ok. I hope its straight
forward.
[Slide 12] [Root planing]
[Dr. ???] This is a histological picture of the same. These are the deposits of calculus, plaque,
this is - here, calculus covered with plaque. Yuck. This is the suclcular epithelium. This is the
instrument in place, and it goes from the base of the pocket coronally. OK? And here is root
planing. The Gracie curette removes plaque, calculus, endotoxin-containing cementum from the
root surface. The arrow indicates the direction toward which the curette is pulled. So we place it
in the pocket to the depth of the sulcus and then move it coronally. And youve all had some little
experience in this in Introduction to Patient Care. Although, hopefully, none of you have
periodontal pockets.
[Slide 13] [What are the limitations )potential) of initial therapy?]
[Dr. ???] So what are the limitations, actually potential of initial therapy. In other words, what
are the limitations of non-surgical therapy?
[Slide 14] [Scaling and Root planing]
[Dr. ???] So this is a University of Michigan study that was done 35 years ago. And what was
compared was scaling and root planing, whats called a Widmans flap- modified Widmans flap,
and a surgical approach to pocket elimination
[Slide 15] [Scaling/Root planing images]
[Dr. ???] And the next slide shows these 3 techniques. Scaling and Root Planing which I dont
feel I need to explain. A modified Widman surgical approach. The blade goes from the sulcular
epithelium at the free gingival margin to the crest of the bone and this tissue is simply excised.
This oral epithelium and connective tissue remains in place. The 3rd technique is a flap
procedure. The blade is brought to the crest and then what is called a periosteal elevator is used to
push this tissue up and out. So you can imagine, this becomes the flap thats moved into the oral
cavity, so to speak, away from the bone. And you can see its been reduced in size. This is a
pocket elimination technique that basically reduces the height from the free gingival margin. And
at the same time what we can do is move this flap apically. Its called an apically positioned or
apically repositioned flap thereby eliminating a periodontal pocket. In this case, we cut open the
sulcular epithelium, root plane, and replace this flap. And in the closed procedure, initial therapy,
we simply root plane. So every one understand the difference between these 3 techniques? Ok.
[Slide 16] [Pocket depths: 4-6mm]
[Dr. ???] So what happens after 8 years? After 8 years, the pocket reduction among these three
techniques is indistinguishable which suggests that non-surgical therapy is just as effective, or it
can be just as effective as a surgical approach to pocket elimination. And you can see this is 4-6
millimeter pockets. What happens if a pocket is 7 or 8 or 10 millimeters? We know from studies
like this that a pocket greater than, deeper than 6 mm will not resolve. You really cant induce
!3
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
enough shrinkage and enough of a long junctional epithelium so that the probing depth is
significantly reduced within a 7mm pocket or 8 or 9 or 10. So, just about 5-6mm is the limit of
the effectiveness of non-surgical therapy. So if a patient presents to you with probing depths - and
anything that Im saying, is it, do you all understand when I say probing depths? Do you all
understand when I say probing depths, what I mean? Does anyone not understand? So a patient
comes in with generalized periodontitis probing depths ranging from 6 to 10 to 12 in the molar
region, you can rest assured that this patient will probably need surgery at some point. And whats
the point? It would be after reevaluation, after youve made the assessment of how effective
initial therapy has been. So residual sites, sites of residual disease, would then be referred to the
periodontist or the generalist who is interested in periodontal surgery for a surgical procedure.
[Slide 17] [Additional goals of periodontal therapy]
[Dr. ???] Next year, youll get a whole year of advanced periodontics. So I dont want to go
that much into this. There are additional goals of periodontalof initial therapy. Improved
contour to simplify plaque control. Well, this is periodontal therapy in general. Stabilize mobile
teeth, improve soft-tissue aesthetics and restore lost tissues. So this is periodontal therapy in
general, including initial therapy and surgical therapy. But you know, dont worry about this slide
today.
[Slide 18] [Periodontal Therapy II]
[Dr. ???] Umm, now were going to talk about in more specific terms, what to do with patients.
[Slide 19] [Initial Therapy]
[Dr. ???] This is initial therapy, Phase I therapy, Non Surgical Therapy, Cause-Related
Therapy, Anti-infective therapy, all the same. You want to stop the infection.
[Slide 20] [The goal of conservative, non-surgical therapy is to:]
[Dr. ???] And these are the goals of non surgical therapy. Eliminate the bacteria responsible for
periodontal destruction. You want to change the microflora from a pathogenic population to a
non-pathogenic population. You would like to create a bio-compatible root surface- that, you now
understand why. You need to remove diseased or infected tissues. And again, importantly, you
want to ascertain, understand, examine the response of the host both physiologically and
behaviorally.
[Slide 21] [Initial Therapy I: Hygiene Phase]
[Dr. ???] So heres initial therapy phase 1- Hygiene phase. What were doing here is instructing
the patient in oral hygiene techniques. We may introduce chemical plaque control. Whats that?
What do you think that is? Antimicrobial rinse. There are some patients who really cant manage,
because of arthritis, because of other impediments who cant manage, on a day to day basis,
plaque control, effectively. So, for some of those patients, we may recommend an antimicrobial.
We want to take away supra gingival plaque and calculus. We want to remove iatrogenic irritants.
Whats an example of an iatrogenic irritant? Fancy word for an overhanging margin, an open
contact, um, something that a dentist has done to create a problem for the patient. So you want to
try to identify and eliminate iatrogenic - meaning coming form the provider- mistakes, so to
speak. And finally removal of naturally occurring plaque retentive areas. What would be an
example of that. Anybody go to the orthodontist here? Ever? Did you start out, anybody- who
went to the orthodontist? So did you start out with really crowded teeth? Were they easy to
maintain plaque control? In some cases, its impossible to maintain plaque control with really
crowded teeth. Its a recommendation to go to the orthodontist simply to be able to keep you
!4
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
periodontal tissue healthy. There are many other reasons to go to he orthodontist. This is one of
them. Okay. Initial therapy II, scaling and root planing is more invasive. Its sub gingival and
were basically preparing the root surface for the long junctional epithelium. This typically
doesnt involve anesthesia. Phase II on the other hand, typically does. We anesthetize our patients
with local anesthesia to scale and root plane effectively.
[Slide 22] [Sequence of Treatment]
[Dr. ???] Now heres the sequence of treatment. We first collect clinical and radiographic
evidence, interpret the evidence. We make a diagnosis, we identify the risk factors. We make a
prognosis, formulate a treatment plan and treat the patient.
[Slide 23] [Sequence of Treatment]
[Dr. ???] So the first step is the first 3.
[Slide 24] [Health History]
[Dr. ???] So lets look. Heres a patient, 52 year old male with history of heart murmur, which
at this point may not be significant. Is a smoker and his family history doesn't include diabetes.
Why do I want to know about diabetes? Is it a risk factor for periodontal disease? Absolutely. So
this person - we want to at least identify one risk factor for periodontal disease. Hes smoking.
His approach to dental treatment has been what we call crisis care. What does that mean? When
theres a crisis, he goes. So is this a person that you think might be thinking ahead abut his
periodontal health? Probably not, so this may present a challenge when changing this patients
behavior. He brushes his teeth twice a day - most people do. He says hes under a lot of stress and
hes clenching and grinding his teeth and they keep him up at night. You know what that term is?
Its a parafunctional habit calledanyone? Its a b-word. Bruxism. Ok. And his teeth are really
sensitive to cold. Its consistent with clenching sometimes. Ok.
[Slide 25] [Oral Examination]
[Dr. ???] So his everything extra orally are within normal limits. And everything, in terms of
the soft tissue and outside of the teeth and periodontal tissues are also within normal limits.
[Slide 26] [Images]
[Dr. ???] So we look at the clinical picture and I circled this. What is this called? This is
blunting of the papilla. Something is going on there. And when I talked yesterday about how to
form or maintain the viability of the interdental papillae during restorative procedures. So it may
be this is a function of the fact that this crown was poorly contoured and didnt maintain the
papillae between tooth 13 and 14. It can also be that there is a defect here underlying in the bone
so that the interproximal bone has been lost and so the underlying support for the soft tissue is
also compromised. But its a sign that there is something going on. May not be that significant but
it may be significant. You can see everything else sort of looks normal. Theres inflammation and
some edema but nothing to get excited about. Now, this is a patient whose soft tissue may not
look as inflamed as you would expect for a patient whose plaque control is poor. Anyone think of
why that may be the case? Smoking. Somebody said smoking? Yeah. Thats true. So smokers
actually look a little healthier, if you dont look at them that carefully then they actually might be.
And the reason is, for one thing, constricts the peripheral blood vessels. So if thats going on in
the oral cavity, youre not going to see that much edema, youre not going to see that much
erythema, and you certainly wont see that much bleeding. Theres also a much more
foundational effect of smoking, and I talked about that as well, on the immune system. So the
inflammatory process itself is compromised. And smokers dont look inflamed, because their
!5
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
immune system cant do it. Okay? So its important to recognize the fact that, for example,
bleeding on probing in a smoker cant be used as an indication or not of inflammation. Its
different for people who dont smoke.
[Slide 27] [Clinical Examination I]
[Dr. ???] So here, the clinical exam. All the teeth are there. There are some restorations that are
poor. Theres a lot plaque, calculus, and some mobility and fremitus. Can anyone define fremitus?
You know what fremitus is? Can anyone? No? So when you close your teeth together, and clench
them and move your jaw back and forth, if you take the finger and you put it on the outside
surface of your maxillary teeth. If the teeth are in fremitus, youll feel them moving in response to
the functional activity of your lower jaw. By definition, mobility induced by function. Patients
with severe or pronounced fremitus, you can actually see teeth move. But the more subtle
fremitus, you feel with a finger. You just put it on the outside of the buccal surface of your
maxillary teeth, clench back and forth. And if theres mobility and fremitus youll feel it.
[Slide 28] [What comes first, radiographs or periodontal probing..?]
[Dr. ???] Ok. So what comes first? We have a blank sheet in front of us for charting and we
have a set of X-rays. What do we do first? Do we look at the films first? Or do we start charting
the clinical defects? Anybody offer a suggestion? And why? Who thinks we look at films first?
Anybody? Ok. So the rest of you dont vote or you think we do the charting first. Well, to me, and
this is a personal belief, to me, I would look at the films first.
[Slide 29] [Radiographs]
[Dr. ???] And why do I do that? Because the films are going to give me a road map. Theyre
going to tell me where to expect to see a soft tissue defect that would be consistent, for example,
with bone loss at a particular site. On the other hand, you can see Ive circled, youve got. This is
his film. This is the crown thats next to the blunted papilla.
[Slide 30] [Radiographs]
[Dr. ???] And you can see theres something right here. And Im going to make them bigger.
Theres something right here. These are two views. So what is that? That could be cement. It
could be calculus. Its something radiopaque. And if you were to probe between 14 and 15, you
might end up with a probing depth of 1 or 2 millimeters, because your probe got stuck on
whatever that radiopaque structure is. So what you would miss is the fact that theres probably a 5
or 6 or even 7 millimeter pocket between 14 and 15, not that you can tell theres a pocket from
the films, but this tell you to go looking between 14 and 15 for what you think may be a
periodontal defect. Ok? So again, by the same token, if this werent here, this little piece of
calculus or whatever, you had the films in front of you and you saw that bone loss between 14
and 15, you would absolutely make sure that when you probe you didnt miss something that you
think might be there. So thats the reason I think we should look at the film, actually, before we
start clinical charting. To give us a sense of what to expect, if nothing more.
[Slide 31] [Radiographs]
[Dr. ???] And here it is even bigger. Now what you see here- what does this slanted bone
represent? This is what is called a vertical defect. As opposed to a horizontal defect. So there s a
horizontal bone loss which occurs over a long period of time and is associated with chronic
disease. And then theres whats called vertical bone loss where you get these very sharp angle
from the horizontal plane of the alveolar ridge.
[Slide 32] [Radiographs]
!6
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
[Dr. ???] Now, this would be consistent with, for example, a deep periodontal pocket. Okay.
Any questions about this? And then theres a failed root canal, maybe. Maybe a perforation of an
anterior tooth. And this might be associated with a periodontal defect. Very often we see,
associated with failed RCT, especially if its a perforation of the root. And it seems to be a
perforation that might have been associated with this post - whats called and endo-perio or perioendo lesion. So that the one lesion becomes contiguous with the other. So knowing that theres
this defect in the tooth, again, you would make sure that between- this was 7? 9 and 10 and 10
and 11- that you would make sure that you've examined that really carefully and not missed what
might be a periodontal endodontic lesion.
[Slide 33] [Radiographic Analysis]
[Dr. ???] So here is the radiographic analysis. Uniform loss of alveolar crestal height, limited
mainly to posterior segments. Possible vertical defect on 15. Radiopacity, possible dental cement
on the distal aspect of #14. A failed root canal and a defective filling. So thats kind of your
radiographic analysis. And that goes in the progress notes. You need to write up what your
findings are. Ok. Is there furcation involvement? Its a very important issue. Does anyone know
what a furcation involvement means when I say furcation involvement? What does that mean?
Anyone? First, where would you find a furcation involvement. In front teeth or back?
[Class] Back
[Dr. ???] Ok. So you know what a furcation is.
[Slide 34] [Radiographs]
[Dr. ???] So furcation involvement is when periodontal infection reaches the level of furcation,
and you can begin to see it radiographically. And its not always that clear clinically. But
radiographically, for example, this radiolucency on these molars. The radiolucency here, the
radiolucency on this maxillary molar on the mesial aspect of the maxillary molar, the buccal
aspect of the maxillary molar and the distal aspect. And theres actually a very, sort of,
pathognomonic finding where, whats called the dark triangle. You see that here. Anyone not see
the dark triangle? Theres one here, and theres one here. And its formed by the fact that the
palatal root overlaps with the buccal or distobuccal or mesiobuccal root on the maxillary molar.
So for some of this, you have the 2 roots together, and for some of it, only one root is visible. And
so it looks like a radiolucent triangle. Knowing that this exists radiographically, you would go out
of your way with a Nabers probe to make sure that you found or you couldn't find a clinical
furcation. Itsand why do we need to know about clinical furcations? What does that have a
bearing on when were doing our diagnosis and work-up. We find teeth with furcation
involvements, what does that significant- why is that significant? What does it affect. It doesnt
affect the diagnosis but it does affect the prognosis. Because we know the prognosis is poor for
teeth that have furcation involvement, if only because its more difficult to manage, to stabilize a
periodontal infection in a furcation involved tooth. So all of these things were collecting. All of
the data were collecting which is clinical findings - you write a big list down, and on the basis of
that, and the other list of risk factors, we can make a prognosis. We can predict this patients
future. Not only for the patient, but for us- so that when youre treating a patient, you need to
know, as best as you can determine, what the outcome, possible outcomes are. So you can inform
the patient. And the more accurate, as I said a few days ago, the more accurate your prediction,
the smarter youll seem to your patients and youll get more and more interested in knowing
about their future. And when you think about it, thats who you want to see.
[Slide 35] [Clinical Examination II]
[Dr. ???] So the Clinical Examination II is, after we did the head and neck and intraoral, then
we do clinical examination 2, which is probing, bleeding on probing, assessment of calculus,
mobility. All of the clinical findings that we associated with teeth and the periodontal tissue.
!7
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
[Slide 36] [Bleeding-on-Probing (BOP)]
[Dr. ???] Ok, so here is bleeding on probing. So these are the signs.
[Slide 37] [Document Plaque and BOP]
[Dr. ???] And we get form this. Ill go back a little bit, just one slide.
[Slide 36] [Bleeding-on-Probing (BOP)]
[Dr. ???] So were going to do two things. Were going to look at the bleeding but were also
going to do something with respect, also, to plaque.
[Slide 38] [Probing Depths]
[Dr. ???] And on the basis of our chart, so here we have a chart where youve go the bleeding
sites circled. So these are the probing depths, the bleeding sites are circled and the number of plus
sites, which is how many sites bleed divided by the total number of sites gives you the gingival
score. (# of bleeding sites/number of sites = gingival score) Thats a score that gives you a
relative- a number, a quantitative number, that gives you a sense of how widespread the
inflammation is in a given patient. Now, this doesn't work for smokers, because smokers dont
bleed that easily. But for people that dont smoke, this is a very reliable indicator of the presence
or absence of inflammation. Plaque score is the same sort of algorithm- how many pluses are
there inter-proximally over how many inter-proximal sites. So the plaque score here is about
65%, the bleeding score is about 30%. Its not surprising in this patient who smokes. So not every
site thats should bleed will bleed. Thats what it comes down to. Anybody have a question?
So the next is just, Im going to go through the chart a little bit. So we have, just to begin with,
these are probing depths. The probing depths that are circled are where they bleed. C is for
calculus. This is the mucogingival junction. The free gingival margin. Plus for plaque, this upside
down or the V is indicating a furcation of a certain severity. Class I, class II, class II. Class I is an
open V. Class II is a closed V, a triangle, and Class III is a filled in triangle. So a Class I is a
furcation where the probe will only move into the furcation on a horizontal inclination or
orientation. The Class II is at least a millimeter and it goes apical. So the probe goes from a
horizontal orientation to more vertical. And a Class III furcation is a furcation that goes from the
buccal to the lingual - all the way through. So the wide range is Class II and theres a very, you
know, its just a very wide range of presentations for Class II furcations. Class I could be called
incipient or early. Class III is frankly severe. So theres that. So lets see, theres the mucogingival
junction. This is mobility- I, II, III which youll learn about. Theres, this is plaque. This is the
furcation, thats the free gingival margin.
[Slide 39] [Make a Clinical Diagnosis]
[Dr. ???] Ok. So were going to make a clinical diagnosis now. Is this periodontal health? No.
And theres lots of reasons why this is not the absence of periodontal disease. Is it gingivitis? The
answer to that is yeah. Theres gingivitis. Theres inflammation of the gingiva but its really
secondary to much more foundational, more serious conditions of periodontitis. And we know its
periodontitis because weve identified attachment loss. And finally, is it periodontitis? The answer
is yeah because not only have we identified attachment loss, but also alveolar bone loss.
[Slide 40] [Is this chronic or aggressive periodontitis?]
[Dr. ???] So is it chronic or aggressive? Now, have you had classification of periodontal
disease yet? Yes? Ok. So this is a little bit of a review. So what is it, chronic or aggressive? Its
chronic, the patient has never been treated. Hes pretty old. 52. Not pretty old. Pretty old. Pretty
!8
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
young. Then, and there are abundant local factors- plaque, calculus, no compliance, there's
smoking, all types of things that contribute to this guys disease. So this is in striking distinction to
aggressive disease which Ill talk about probably in about half hour.
[Slide 41] [So whats the definitive periodontal diagnosis?]
[Dr. ???] Ok. So whats the definitive periodontal diagnosis? Ok. Chronic periodontitis. And
we then need to say how severe is it? Its not simply chronic periodontitis. Is it mild, moderate, or
severe? And you can use this. These definitions. Somebody might call it a little bit more or less
severe, with one or two more millimeters one way or the other. But basically its either mild,
which is either incipient, or manageable, predictably, by non-surgical therapy. Moderate
periodontitis, by definition, more serious, more involved, the pocketing can be greater than 6.
And typically, this is not managed only by non-surgical therapy. And severe, again, by definition,
over 7mm of pocket depth or probing depth or attachment loss. And this is, without question, not
completely manageable with non-surgical therapy. So you can think of it, what can I treat
completely with scaling and root planing? That will be mild. What may need surgery? Probably,
need surgery- thats probably moderate. And what will definitely need surgery or is completely
hopeless, cant be treated? Thats without question, sever. So theres sort of a commonsensical
approach to this which makes much more sense than trying to remember definitions of how many
millimeters is associated with one versus the other. You can put it in a context of something thats
relatable - that makes much more sense, I think.
[Slide 42] [Probing depths]
[Dr. ???] So heres the chart again. Im not sure why I have it here. Oh, so I just wanted to
reiterate. This is pocketing of 4 and 5. Heres a 6 here and there. 5s and 6s. 3s and 4s. So
theres a range here. The deepest pocket is 6 so[Slide 43] [Diagnosis: Chronic generalized mid-moderate periodontitis]
[Dr. ???] SKIP
[Slide 44] [Sequence of Treatment]
[Dr. ???] It may be chronic generalized mild-moderate periodontitis. So youve got a mix, or
its sort of in the middle between whats frankly manageable, non surgically, which may be some
areas that may have to be treated surgically. So theres- its in between mild and moderate. So the
diagnosis is chronic mild to moderate. We also want to identify where it is. The extent of this- is it
localized or generalized? And there are lots of definitions that distinguish between localized and
generalized. But if it occurs in more than a few or several sites and more than a couple of
quadrants I would call it generalized. So again, you can look at it from a commonsensical
point of view in terms of its definition. Do not get hung up on how many, or 27 reasons to use a
rubber dam, that kind of memorization. You should really think of it in terms of the context, for
example, treating the patient.
[Slide 45] [Summary of Risk Factors]
[Dr. ???] Ok. So, next- weve made the diagnosis. Now we have to figure out the risk factors
and make a prognosis. S the risk factors are plaque, the pockets themselves are risk factors for
more plaque. Lack of compliance. Those are local factors. The systemic factors are smoking, and
previous so the patient walks in and he has attachment loss. So by definition, thats called a
previous loss of attachment. Why is that significant. Well, its significant because it speaks to, sort
of, an inherent susceptibility to periodontitis in this patient. Then you have to ask which of these
!9
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
are modifiable. So of all of these, which are modifiable? The only one thats not modifiable is
previous loss of attachment. You cant do anything about that, its like his age. Its a given. So the
other smoking and plaque control, you definitely can address. Definitely can address.
[Slide 46] [Determine the Prognosis]
[Dr. ???] So that goes into the prognosis. Theres a short term prognosis. Good, and what does
that mean? And youll more about this next year from Dr. Brawler, Dr. Kye.
[Slide 47] [Short-term prognosis]
[Dr. ???] But in short term prognosis, its basically whether or not your therapy on a short term
-you know the first 3 months of knowing a patient- whether that is going to be effective. It
probably will. The long term prognosis depends on whether or not we can eliminate or reduce the
threats. And that speaks to behavior, smoking as well as plaque control.
[Slide 48] [Sequence of Treatment]
[Dr. ???] And then finally, were going to formulate a treatment plan and treat the patient. So,
lets do that.
[Slide 49] [Initial Therapy]
[Dr. ???] Go back to initial therapy, re-evaluation, surgical therapy. Its the same algorithm.
Basically the same way to approach . And in fact, you can apply this directly to mineralization,
remineralization of carious teeth. Same way. We do initial therapy -fluoride. You wait to see
whether there is stabilization and remineralization and if not, you intervene surgically by placing
a restoration eliminating the caries surgically. So its the same algorithm.
[Slide 50] [Periodontal Treatment Treatment Plan (IT)]
[Dr. ???] So whats the periodontal treatment plan? Initial therapy? Oral hygiene instruction.
Now is this always the first step? No. What if hes in pain? What if theres some compelling
need? Theres a tooth that is hopelesss with respect to either restorative issues or is hopeless
periodontally? Well, it may be that you want to extract that tooth first. Take out the hopeless teeth.
Dont send the patient home- not that day, but another day- with a tooth that could end up with a
toothache. With real problems for him. So that, oral hygiene instruction, scaling and root planing
is not always the first step. A patient walks in with rampant decay. First step should be
stabilization - caries control. Then you can start to go back and address the periodontal issue. Ok.
So for this patient, you do an oral hygiene instruction. You do plaqu and calculus removal scaling and root planing. Smoking cessation. You might waant to think about what's called a night
guard. I don't want to get off on a topic but this would address the bruxism. And also talk to the
patient about the limitations of non-surgical therapy. So that's all part of the first steps taken with
respect to treating this patient appropriately. So now, were going to talk about, in a more detailed
way, initial therapy itself. Same three arrows.
[Slide 51] [Periodontal Therapy II]
[Dr. ???] And Ill just run through this quickly. This is the outline from the other day and were
going to look first at initial therapy I.
[Slide 52] [Initial Therapy]
[Dr. ???] SKIP
!10
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
[Slide 53] [Flow chart]
[Dr. ???] And it includes medical history and issues that may bear on prognosis. Hypertension,
for example, you need to take into account patients with medical issues in terms of listening, an
adequate or appropriate history. And this is the patient, also, who might be pre-diabetic. Were not
sure. But in terms of the medical history in general, these re the issues that are addressed before
you can pick up a periodontal instrument. And then also, there are issues like this. This can be a
painful lesion. So this would be under emergency treatment. So this is all coming before you
begin to treat the chronic and inflammatory disease that the patient is, sort of, walking around
with.
[Slide 54] [Flow chart]
[Dr. ???] So now we go to whats called here closed pocket therapy. Its a very strange way to
term it. But this is basically non-surgical therapy. And then theres the phase II- is surgical
therapy. And here you can see it says surgical, causal and corrective therapies. Now this not
periodontal disease. This is pronounced recession. It may be sensitive. It certainly may be an
aesthetic issue and so this would be addressed as corrective surgery in the surgical phase. Again,
this is just an aside to give you an idea of what is encompassed in each stage of treatment.
[Slide 55] [Flow chart]
[Dr. ???] Ok. And finally, theres the reevaluation and follow up. And here, you can see, this is
the surgical phase. This might be, yeah, oh, oh, oh, I know. So this is, when we talked about
surgery, theres corrective therapy and then whats called surgical causal in this outline. And this
surgical causal is just another way to say this is the phase II periodontal treatment- the surgical
treatment in sites that couldnt or didn't respond to non-surgical therapy. Alright.
[Slide 56] [Surgical intervention (Phase II therapy)]
[Dr. ???] And so, this is a typical periodontal therapy. You can see these are surgical incisions,
both buccally and lingually or palatally. And whats doing here- this is at the initial incision. So
what is the periodontist doing with these incisions? What do you think hes doing? Why do you
make this incision 2-3 mm from the free gingival margin? When hes finished with the surgery,
hes going to have no pockets and this is one way to eliminate the pocket. Surgically. Youre
excising the tissue that forms the pocket. And heres the flaps pushed back. And you can see
clearly that there has been bone loss around these teeth- on the palatal aspect especially. Theres a
little bit of the furcation thats visible right here. And this is the reason why non-surgical therapy
couldnt work in this patient. Because it was just too torturous. The root structures, the furcations,
and the depths of the defect made it impossible to definitively remove the causal agents of the
periodontal infection. Non-surgically. Ok.
So finally, heres the suturing. And you can see, this now where the free gingival margin is. It used
to be up here and now its down here. So whats happened? That pocket has disappeared. And this
is what it looks like- like six months or a year later. So this is now. Probing depth of, say, 2-3
mm. There is no pocketing. Theres no collecting of bacteria although there is induced, so to
speak, induced recession. Alright. Its almost 4:00, Im going to talk until almost 5. I thought I
had 2 hours today. Just 1 hour? Okay! So I have 2 hours next week. No? Are you sure I dont
have 2 hours today? Ok, Im going to see. If thats the case, Im going to stop right now and I
apologize. I thought I had until 5 today. On Monday? I have 2 hours Monday? Im just
completely confused. Thank you for your patience. Im going to , lets see. I just have to make a
note to myself.
Thank you. It was a pleasure. I really enjoy lecturing to you guys. I really do. Its an absolute
pleasure.
!11
Transcribed by Charles Buchanan
Date of the Lecture: 11/05/14
~Applause~
A smattering of applause, I love it.
!12
Você também pode gostar
- Rollin Life in Motion and Stillness of Life 2Documento159 páginasRollin Life in Motion and Stillness of Life 2Grigoras Elena Diana80% (5)
- 1000 Mcqs - Periodontics Plus September 2014 McqsDocumento16 páginas1000 Mcqs - Periodontics Plus September 2014 McqsSelvaArockiam86% (7)
- Advancing Conversations: Aubrey De Grey - Advocate For An Indefinite Human LifespanNo EverandAdvancing Conversations: Aubrey De Grey - Advocate For An Indefinite Human LifespanAinda não há avaliações
- Orthopaedic Management in Cerebral Palsy, 2nd EditionNo EverandOrthopaedic Management in Cerebral Palsy, 2nd EditionHelen Meeks HorstmannNota: 3 de 5 estrelas3/5 (2)
- Locator Overdenture Implant System Manual - INST1247Documento28 páginasLocator Overdenture Implant System Manual - INST1247gildeipiraAinda não há avaliações
- CasesDocumento49 páginasCasesYasmin Ismaiel100% (13)
- Integrated Esthetics in Periodontics and ImplantologyDocumento818 páginasIntegrated Esthetics in Periodontics and ImplantologyThanh Nhan DinhAinda não há avaliações
- Mechanical and Chemotherapeutic Home Oral Hygiene-1Documento6 páginasMechanical and Chemotherapeutic Home Oral Hygiene-1ceudmd3d100% (1)
- (General Pathology) - (Wound Healing) by (Dr. Craig)Documento24 páginas(General Pathology) - (Wound Healing) by (Dr. Craig)NYUCD17Ainda não há avaliações
- Transcription: 13 Jan Session 2 - Recording - 1Documento4 páginasTranscription: 13 Jan Session 2 - Recording - 1David ValbuenaAinda não há avaliações
- Lecture 1/2: Orientation and Basic ToolsDocumento7 páginasLecture 1/2: Orientation and Basic ToolsNYUCD17Ainda não há avaliações
- Good Morning ParisDocumento6 páginasGood Morning ParisCristinaMolasAinda não há avaliações
- Introduction To Biology 1Documento17 páginasIntroduction To Biology 1Samuel PonceAinda não há avaliações
- 02: Cell Responses To InjuryDocumento15 páginas02: Cell Responses To InjuryNYUCD17Ainda não há avaliações
- 21: Bone Wound Healing and OsseointegrationDocumento15 páginas21: Bone Wound Healing and OsseointegrationNYUCD17Ainda não há avaliações
- Lecture 8, Cysts of The Jaws 2 (Script)Documento27 páginasLecture 8, Cysts of The Jaws 2 (Script)JustDen09Ainda não há avaliações
- 41: Pathologic Aspects of Aging IDocumento12 páginas41: Pathologic Aspects of Aging INYUCD17Ainda não há avaliações
- Language Functions in Medical WritingDocumento10 páginasLanguage Functions in Medical WritingAfif Fadhilah IrsyadAinda não há avaliações
- Head & Neck Anatomy - Embryology & Pharyngeal Arches - INBDEDocumento13 páginasHead & Neck Anatomy - Embryology & Pharyngeal Arches - INBDEHạnh TrangAinda não há avaliações
- SpeakingDocumento6 páginasSpeakingLinh MaiAinda não há avaliações
- December, 11th 2013: What Is An Emergency?Documento11 páginasDecember, 11th 2013: What Is An Emergency?Sawsan Z. JwaiedAinda não há avaliações
- Introductionto Cranio Sacral TherapyDocumento77 páginasIntroductionto Cranio Sacral TherapyViki100% (2)
- Cons 10Documento11 páginasCons 10Sawsan Z. JwaiedAinda não há avaliações
- 57/58: Evaluation of Perio Patient and Radiographic ExaminationDocumento42 páginas57/58: Evaluation of Perio Patient and Radiographic ExaminationNYUCD17Ainda não há avaliações
- Neurostructural Integration Technique: A Better Way To Good Health! Michael J. Nixon-LivyDocumento66 páginasNeurostructural Integration Technique: A Better Way To Good Health! Michael J. Nixon-Livytheodora_bobes100% (1)
- Diagnosing and Treating The Patient With Restricted Mandibular Opening: A New ApproachDocumento8 páginasDiagnosing and Treating The Patient With Restricted Mandibular Opening: A New ApproachAmar BhochhibhoyaAinda não há avaliações
- Rifat Latifi MD, FACS (Auth.), Rifat Latifi (Eds.) - Surgery of Complex Abdominal Wall Defects-Springer-Verlag New York (2013)Documento219 páginasRifat Latifi MD, FACS (Auth.), Rifat Latifi (Eds.) - Surgery of Complex Abdominal Wall Defects-Springer-Verlag New York (2013)Vicente Bruno GuimaraesAinda não há avaliações
- 37: Gingiva IIDocumento8 páginas37: Gingiva IINYUCD17Ainda não há avaliações
- BioethicsDocumento6 páginasBioethicsDaniel MaysAinda não há avaliações
- Rejuvenation of The Anterior Neck 2014 Atlas of The Oral and MaxillofacialDocumento12 páginasRejuvenation of The Anterior Neck 2014 Atlas of The Oral and Maxillofaciallaljadeff12Ainda não há avaliações
- SteinerDocumento23 páginasSteinerAlejandra Zambrano ValeroAinda não há avaliações
- Assignment 1 - Informative, Analytical And/or Argumentative: Does P Rogress Pay?Documento11 páginasAssignment 1 - Informative, Analytical And/or Argumentative: Does P Rogress Pay?sandruAinda não há avaliações
- SURGICAL TALK FinalpptDocumento30 páginasSURGICAL TALK FinalpptRazeen RiyasatAinda não há avaliações
- Communication Skills in Palliative Care A Practical GuideDocumento17 páginasCommunication Skills in Palliative Care A Practical GuideMarcus Philip GonzalesAinda não há avaliações
- Teaching Care Plan - Open CholecystectomyDocumento4 páginasTeaching Care Plan - Open CholecystectomyWyen CabatbatAinda não há avaliações
- A Look at Painful Obstruction Syndromes v2 PDFDocumento17 páginasA Look at Painful Obstruction Syndromes v2 PDFSillytwitAinda não há avaliações
- Disorders of The Dental PulpDocumento13 páginasDisorders of The Dental PulpritabagadiaAinda não há avaliações
- Lfurbot,+aabp 1979 Proceedings 033 FS-BasicPharmacologyOfBovineRespiratorytherapDocumento5 páginasLfurbot,+aabp 1979 Proceedings 033 FS-BasicPharmacologyOfBovineRespiratorytherapNimai Nitai DasAinda não há avaliações
- Cephalometrics in Clinical Practice: Beverly Hills, CalifDocumento22 páginasCephalometrics in Clinical Practice: Beverly Hills, CalifDanilo Jose GomezAinda não há avaliações
- 2007 Tweed ProfileDocumento60 páginas2007 Tweed ProfileYeny Valdivia AlbornozAinda não há avaliações
- Mast Cell Activation Syndrome - The Functional Medicine ApproachDocumento34 páginasMast Cell Activation Syndrome - The Functional Medicine Approach0xcffaaAinda não há avaliações
- Ozone in Pain ManagementDocumento37 páginasOzone in Pain Managementsiddharthnair_1100% (1)
- Pneumo HemothoraxDocumento126 páginasPneumo HemothoraxLyra Jan Roo100% (1)
- Chapter 4 & 5Documento11 páginasChapter 4 & 5Claudine NaturalAinda não há avaliações
- MedicineDocumento6 páginasMedicineroxana kwiekAinda não há avaliações
- Why Do Ineffective Treatments Seem HelpfullDocumento7 páginasWhy Do Ineffective Treatments Seem HelpfullRazvan UngureanuAinda não há avaliações
- CH 8 Exercises and Vocab ONLY - No AnswersDocumento7 páginasCH 8 Exercises and Vocab ONLY - No Answerssalsabel AlagoriAinda não há avaliações
- Thesis On Facial PalsyDocumento8 páginasThesis On Facial Palsymelissalongmanchester100% (2)
- Lesson: Dr. Leon Hammer, M.DDocumento14 páginasLesson: Dr. Leon Hammer, M.DRocío JMAinda não há avaliações
- Plastic Surgery and Innovation in MedicineDocumento12 páginasPlastic Surgery and Innovation in MedicineIde Bagoes InsaniAinda não há avaliações
- Oral Histology Lecture 1Documento12 páginasOral Histology Lecture 1Mohamed Harun B. SanohAinda não há avaliações
- 135 2022F U3 Term Specialties VOCDocumento34 páginas135 2022F U3 Term Specialties VOCHương XuânAinda não há avaliações
- 05: Prenatal CF Development IIDocumento11 páginas05: Prenatal CF Development IINYUCD17Ainda não há avaliações
- Tweed ProfileDocumento60 páginasTweed ProfileJu Ju WareeratAinda não há avaliações
- Luo Vessels by J Yuen002Documento85 páginasLuo Vessels by J Yuen002Jonathan100% (3)
- Research Structure For Facial Nerve Palsy Treatment ModalitesDocumento3 páginasResearch Structure For Facial Nerve Palsy Treatment ModalitesZainab BelalAinda não há avaliações
- Advanced Medical English Course 2 TodoDocumento13 páginasAdvanced Medical English Course 2 TodoAntonio GarcíaAinda não há avaliações
- Bi SyndromesDocumento17 páginasBi Syndromesunbelievable686Ainda não há avaliações
- Healing Healthcare Through Philosophy Dr. Mark Zlomislić (Zlow Miss Litch)Documento23 páginasHealing Healthcare Through Philosophy Dr. Mark Zlomislić (Zlow Miss Litch)Zlom ProfAinda não há avaliações
- Re Ective Practice in Health Care and How To Re Ect EffectivelyDocumento3 páginasRe Ective Practice in Health Care and How To Re Ect EffectivelySteveAinda não há avaliações
- MTM Elhers Danlos and CFDocumento9 páginasMTM Elhers Danlos and CFFrancesca vitaleAinda não há avaliações
- ACT For Chronic Pain For Groups HandbookDocumento71 páginasACT For Chronic Pain For Groups HandbookLydia Collins100% (4)
- The Healing Side of Patient Care: A New PerspectiveNo EverandThe Healing Side of Patient Care: A New PerspectiveAinda não há avaliações
- Week of September 5Documento1 páginaWeek of September 5NYUCD17Ainda não há avaliações
- Happy: TurkeyDocumento8 páginasHappy: TurkeyNYUCD17Ainda não há avaliações
- Fall Newsletter #3Documento1 páginaFall Newsletter #3NYUCD17Ainda não há avaliações
- Fall Newsletter Nov 14Documento1 páginaFall Newsletter Nov 14NYUCD17Ainda não há avaliações
- Reminders:: T Shirt Design Contes T!Documento1 páginaReminders:: T Shirt Design Contes T!NYUCD17Ainda não há avaliações
- Week of September 12Documento1 páginaWeek of September 12NYUCD17Ainda não há avaliações
- Happy: TurkeyDocumento8 páginasHappy: TurkeyNYUCD17Ainda não há avaliações
- Week of November 9th, 2015 - Class of 2017 NewsletterDocumento9 páginasWeek of November 9th, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of November 2nd, 2015 - Class of 2017 NewsletterDocumento10 páginasWeek of November 2nd, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of November 30th, 2015 - Class of 2017 NewsletterDocumento9 páginasWeek of November 30th, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of September 8th - Class of 2017 NewsletterDocumento8 páginasWeek of September 8th - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of October 5th, 2015 - Class of 2017 NewsletterDocumento8 páginasWeek of October 5th, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of September 21st, 2015 - Class of 2017 NewsletterDocumento8 páginasWeek of September 21st, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of September 14, 2015 - Class of 2017 NewsletterDocumento7 páginasWeek of September 14, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of October 19th, 2015 - Class of 2017 NewsletterDocumento9 páginasWeek of October 19th, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of October 26th, 2015 - Class of 2017 NewsletterDocumento9 páginasWeek of October 26th, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of September 28, 2015 - Class of 2017 NewsletterDocumento8 páginasWeek of September 28, 2015 - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of August 31st - Class of 2017 NewsletterDocumento7 páginasWeek of August 31st - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of August 31st - Class of 2017 NewsletterDocumento7 páginasWeek of August 31st - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- Week of September 8th - Class of 2017 NewsletterDocumento8 páginasWeek of September 8th - Class of 2017 NewsletterNYUCD17Ainda não há avaliações
- September 2, 2015 MinutesDocumento3 páginasSeptember 2, 2015 MinutesNYUCD17Ainda não há avaliações
- September 2, 2015 MinutesDocumento3 páginasSeptember 2, 2015 MinutesNYUCD17Ainda não há avaliações
- D2 Council Meeting Minutes: 12:00 - 1:00pm Room 8SDocumento3 páginasD2 Council Meeting Minutes: 12:00 - 1:00pm Room 8SNYUCD17Ainda não há avaliações
- July 8, 2015 Meeting MinutesDocumento2 páginasJuly 8, 2015 Meeting MinutesNYUCD17Ainda não há avaliações
- 1-23-15 MinutesDocumento2 páginas1-23-15 MinutesNYUCD17Ainda não há avaliações
- 10-17-14 MinutesDocumento2 páginas10-17-14 MinutesNYUCD17Ainda não há avaliações
- 1-9-15 MinutesDocumento3 páginas1-9-15 MinutesNYUCD17Ainda não há avaliações
- 2-20-15 MinutesDocumento2 páginas2-20-15 MinutesNYUCD17Ainda não há avaliações
- Case Report: Segmental Odontomaxillary Dysplasia: Review of The Literature and Case ReportDocumento6 páginasCase Report: Segmental Odontomaxillary Dysplasia: Review of The Literature and Case ReportElisabeth FransiskaAinda não há avaliações
- Vto Seminar No.2Documento115 páginasVto Seminar No.2Dr Shivam Verma100% (1)
- Bedbath Checklist 2020Documento4 páginasBedbath Checklist 2020shaznay delacruzAinda não há avaliações
- Implant Failure 2-2Documento118 páginasImplant Failure 2-2فاطمه شبانهAinda não há avaliações
- Wiringtechniquesinmaxillofacialsurgery 121205104837 Phpapp01Documento41 páginasWiringtechniquesinmaxillofacialsurgery 121205104837 Phpapp01Varun Bharathi100% (1)
- Extraoral Library Codes: VERSION 5-81Documento26 páginasExtraoral Library Codes: VERSION 5-81Zsolt PerényiAinda não há avaliações
- Lazzara 1989 Imediate PlaccementDocumento13 páginasLazzara 1989 Imediate PlaccementNawaf RuwailiAinda não há avaliações
- Oral Mucous Membrane: by - Arindam MondalDocumento92 páginasOral Mucous Membrane: by - Arindam MondalMohammed hisham khanAinda não há avaliações
- Board Buster PDFDocumento457 páginasBoard Buster PDFSheetal Soham Marathe100% (1)
- AbutmentDocumento69 páginasAbutmentDevendra Chhonkar100% (2)
- Mucogingival SurgeryDocumento53 páginasMucogingival SurgeryAbhijeet Shete100% (3)
- Case PresentationDocumento8 páginasCase Presentation。Ainda não há avaliações
- 3320 PDFDocumento7 páginas3320 PDFLouis HutahaeanAinda não há avaliações
- Filament End-Rounding Quality in Electric ToothbrushesDocumento4 páginasFilament End-Rounding Quality in Electric ToothbrushesGeorgiana BlagociAinda não há avaliações
- The Role of Gingival Connective TissueDocumento17 páginasThe Role of Gingival Connective Tissueabdulkarim bashaAinda não há avaliações
- Mapeh-6 2020Documento5 páginasMapeh-6 2020pot poootAinda não há avaliações
- Dental Anatomy & Physiology: April 2014Documento19 páginasDental Anatomy & Physiology: April 2014Anna PruteanuAinda não há avaliações
- Labial Cervical Groove QuintessenceDocumento7 páginasLabial Cervical Groove QuintessenceSaurabh Kumar GuptaAinda não há avaliações
- B.O.P.T. Technique: Dr. Ignazio LoiDocumento32 páginasB.O.P.T. Technique: Dr. Ignazio LoiTeresa LealAinda não há avaliações
- FPD - lec.SAS.11 Complete Crown and Posterior PVCDocumento11 páginasFPD - lec.SAS.11 Complete Crown and Posterior PVCDian Alaissa MencianoAinda não há avaliações
- Advanced Endodontics - Informa Healthcare 1 Edition (January 13, 2006) PDFDocumento375 páginasAdvanced Endodontics - Informa Healthcare 1 Edition (January 13, 2006) PDFAndra AnduAinda não há avaliações
- Jurnal Porio 1Documento3 páginasJurnal Porio 1Neo YustindraAinda não há avaliações
- 2017 Chapple Periodontal Health and Gingival Diseases and Conditions On An Intact and A Reduced Periodontium Consensus ReportDocumento10 páginas2017 Chapple Periodontal Health and Gingival Diseases and Conditions On An Intact and A Reduced Periodontium Consensus ReportSANTIAGO URIBE GOMEZAinda não há avaliações
- Surgical Crown LengtheningDocumento96 páginasSurgical Crown LengtheningJevin Stivie Cialy100% (2)
- Scopin 2019 Carillas PerioDocumento15 páginasScopin 2019 Carillas PeriojotapintorAinda não há avaliações