Escolar Documentos
Profissional Documentos
Cultura Documentos
Economic of Academic Medical Centre
Enviado por
Yoga Rossi Widya UtamaDireitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Economic of Academic Medical Centre
Enviado por
Yoga Rossi Widya UtamaDireitos autorais:
Formatos disponíveis
PERS PE C T IV E
The Economics of Graduate Medical Education
From the Harvard Kennedy School of Government, Cambridge, MA (A.C.); Yale University
School of Medicine, New Haven, CT (D.K.);
and Project HOPE, Bethesda, MD (G.R.W.).
This article was published on May 14, 2014,
at NEJM.org.
1. Health policy brief: graduate medical education. Health Affairs. August 16, 2012 (http://
www.healthaffairs.org/healthpolicybriefs/brief
.php?brief_id=73).
2. Becker GS. Human capital: a theoretical
and empirical analysis, with special reference
to education. New York: National Bureau of
Economic Research, Columbia University
Press, 1964.
3. Iglehart JK. Support for academic medical centers revisiting the 1997 Balanced
Budget Act. N Engl J Med 1999;341:299304.
4. Volpp KG, Konetzka RT, Zhu J, Parsons L,
Peterson E. Effect of cuts in Medicare re
imbursement on process and outcome of
care for acute myocardial infarction patients.
Circulation 2005;112:2268-75.
5. Seshamani M, Schwartz JS, Volpp KG.
The effect of cuts in Medicare reimbursement on hospital mortality. Health Serv Res
2006;41:683-700.
DOI: 10.1056/NEJMp1402468
Copyright 2014 Massachusetts Medical Society.
The Economics of Academic Medical Centers
Atul Grover, M.D., Ph.D., Peter L. Slavin, M.D., and Peters Willson, M.P.P.M.
ost economists seem to
view graduate medical education (GME) training graduates of medical schools to become independently practicing
physicians as a stand-alone
effort, without considering its
relationship to other activities of
major teaching hospitals within
academic medical centers (AMCs).
Payments with a GME label are
often examined in isolation,
rather than as part of the complex economics of AMCs, whose
missions include training physicians, conducting groundbreaking research, providing a full
financial gains for themselves or
affiliated physicians, to increase
the volume of patients, to improve
the quality of services, to provide
community benefit, or to achieve
some combination of these goals.1
Nearly all AMCs are not-for-profit and have a responsibility to provide community benefit that goes
beyond charity care, through intertwined missions and services
that independently may not always generate a financial margin
but are indispensable to the health
of individuals and communities.
Residents and fellows are
trained in a variety of clinical en-
The cost of GME extends well beyond the costs
partially covered by direct GME support.
Investments in research and complex clinical
activities are critical to the environment
for robust, diverse training programs.
spectrum of clinical care, and
improving community health.
The literature offers a variety
of models to explain the economic behavior of hospitals, particularly not-for-profits to clarify,
for example, whether they are
seeking primarily to maximize
2360
vironments and settings, many of
which lose money but are critical
for new physicians experiential
learning. Service lines such as obstetrics, geriatrics, and inpatient
psychiatry are poorly reimbursed
and often absent or undersized
in nontraining settings. Yet these
services are often retained in
AMCs because they benefit the
community and are vital to training health care professionals.
Teaching-hospital members of
the Association of American
Medical Colleges (AAMC) represent only 5% of all hospitals, but
their clinicians (who are on the
faculty of AMC medical schools)
provide a disproportionate share
of care to vulnerable patients.
Historically, AMCs have provided
37% of all charity care and 26%
of all Medicaid hospitalizations,
as well as a disproportionate
share of many other community
services, often at a financial loss
(see graph). AMCs also provide
highly specialized services for
entire regions of the country and
receive 38% of transfers from
other hospitals that cannot care
for patients with complex needs.2
Teaching hospitals operate
nearly all regional standby services for example, 80% or
more of level 1 trauma and burn
centers. These services require
specialized facilities, equipment,
and personnel, including physicians in multiple specialties, that
must be on site or within minutes of the hospital. The costs for
these resources are incurred daily
so the hospitals can be in con-
n engl j med 370;25nejm.orgjune 19, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 8, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
PE R S PE C T IV E
The Economics of Academic Medical Centers
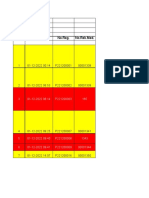
Percentage of Hospitals Offering Service
COTH hospitals
100
Nonteaching hospitals
90
90
79
80
70
58
60
57
54
50
40
33
30
25
18
20
10
0
11
4
Burn Unit Psychiatric Psychiatric
Emergency Outpatient
Services
Services
Pediatric
Intensive
Care
Pediatric
Pediatric
Cardiology Emergency
Services Department
Percentage of U.S. COTH Member Hospitals and Nonteaching Hospitals Offering
Selected Services.
Data are from an analysis conducted by the Association of American Medical Colleges of data from the American Hospital Association from fiscal year 2012. COTH
denotes Council of Teaching Hospitals.
stant readiness, regardless of when
the next plane crash, tornado,
bombing, or other mass-casualty
incident occurs. Moreover, to be
designated as a level 1 trauma
center, an institution must engage
in training and research, which
further increase the costs of the
standby service. Surgeons and
many other physicians in training gain invaluable experience in
these centers by learning how to
stabilize the critically ill or injured,
which benefits future patients.
While training at AMCs, residents also gain exposure to biomedical and health systems research, the opportunity to care
for patients with rare diseases,
and care-redesign efforts for
acutely and chronically ill patients. More than half of all National Institutes of Health extramural research grant funding
went to AMC faculty members in
fiscal year 2011, according to
AAMC analyses. Yet the indirect
cost reimbursement associated
with grant funding does not cov-
er the full cost of the infrastructure needed to support the research mission. As a result,
AMCs must subsidize the research mission, contributing up
to 30% of its support,3 which often amounts to hundreds of millions of dollars in cross-subsidies
from clinical or other revenue
streams. AMC research activities
contribute to the training of all
M.D.Ph.D.s and have resulted in
advances such as the polio vaccine, the first pancreas transplantation, the first neonatal intensive care unit, and the first gene
therapy for cystic fibrosis.
Many medical and surgical
subspecialty fellows are required
to spend at least 1 year conducting research with only institutional support. Although not all
physicians will ultimately pursue
careers in biomedical research,
future clinicians need to understand the process of how new
knowledge is acquired and validated, how to help their patients
gain access to clinical trials, how
to participate in postmarketing
surveillance by the Food and Drug
Administration, and how to conduct community-based research.
The synergies among AMCs
four missions create an intellectual and learning environment
that is ideally suited for the
training of physicians. In this
environment, questions are constantly asked, assumptions are
challenged, and new approaches
to care are tested. It is the AMCs
responsibility to support and
nurture this atmosphere and ensure that it permeates the highly
specialized inpatient settings,
outpatient departments, community health centers, and private
physician offices where physician
training occurs.
In U.S. teaching hospitals, the
direct costs of training residents
and fellows including trainee
stipends and benefits, faculty supervision, simulation and other
equipment, salaries for administrative staff, and overhead
amount to more than $16 billion
annually. Medicare is the largest
explicit supporter of direct GME
expenses, contributing just over
$3 billion,4 while grant programs
from Veterans Affairs, the Department of Defense, Medicaid,
and the Public Health Service
contribute more modest support.
Most of the direct cost of GME is
borne by the teaching hospitals
themselves.
Some economists have suggested that trainees are low-cost,
skilled labor that make money
for AMCs despite their inability
to bill directly for patient services. However, we are aware of
no empirical analyses that suggest that trainees increase clinical revenue sufficiently to offset
the investment required to support training. In addition, the
n engl j med 370;25nejm.orgjune 19, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 8, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
2361
PERS PE C T IV E
The Economics of Academic Medical Centers
cost of training has increased
substantially in recent years owing to a series of unfunded mandates, including more stringent
educational requirements, decreased duty hours, and strict supervision requirements.
The cost of GME extends well
beyond the costs partially covered by direct GME support. Investments in research and complex clinical activities are critical
to the environment for robust,
diverse training programs. No
explicit investments in these additional costs are made in the
current reimbursement system.
When the Medicare inpatient
prospective payment system was
created, the adjustment for indirect medical education was made
to serve as a proxy to partially
reimburse teaching hospitals for
the higher complexity of care
and unique services that AMCs
provide to communities. That adjustment is a hospital-specific
payment intended to help support these institutional costs.5
Highly specialized services such
as burn centers would be at risk
in the absence of this public support. For-profit hospitals that
have a fiduciary responsibility to
generate a financial return to
shareholders are less likely to invest in burn centers and to have
residency training programs.
Well-trained physicians require exposure to the full spectrum of health care for a broad
patient population, diverse in
demographic, economic, and
health status, from the richest to
the poorest, from the healthiest
to the sickest, and with the most
common to the rarest of conditions all of which require investments beyond supervisory
educational time. New physicians
need exposure to the most wellestablished medical practices but
also to the processes by which
advances in prevention, diagnosis, and treatment are achieved.
As a potential physician shortage looms and the need for public investment in physician training grows, there have been calls
for greater accountability for the
public support that teaching hospitals receive to conduct physician education. The AAMC has
endorsed legislation that would
yield greater transparency of
public support for AMCs but also
more data on the costs incurred
in maintaining a robust training
environment. The same legislation would also create a reasonable system of rewards and penalties to ensure that AMCs train
physicians who have the right
mix of skills, can work in teams,
are conscious of the finite nature
of resources, and are able to de-
velop better and more affordable
systems of care. A continued and
more accountable investment in
GME-writ-large will benefit U.S.
health care for decades to come.
Disclosure forms provided by the authors
are available with the full text of this article
at NEJM.org.
From the Association of American Medical
Colleges, Washington, DC (A.G., P.W.); and
Massachusetts General Hospital and the
Department of Health Care Policy, Harvard
Medical School both in Boston (P.L.S.).
This article was published on May 14, 2014,
at NEJM.org.
1. Newhouse JP. Toward a theory of nonprofit institutions: an economic model of a
hospital. Am Econ Rev 1970;60:64-74.
2. Huderson A, Haberman M, Conroy J.
Medicare patient hospital transfers in the
era of health care reform. Washington, DC:
Association of American Medical Colleges,
2013 (https://www.aamc.org/download/
333654/data/april2013analysisinbrief
-medicarepatienthospitaltransfersinthee
.pdf).
3. Dzau VJ, Cho A, Ellaissi W, et al. Transforming academic health centers for an uncertain future. N Engl J Med 2013;369:991-3.
4. Medicare payments for graduate medical
education: what every medical student, resident, and advisor needs to know. Washington, DC: Association of American Medical
Colleges, 2013 (https://members.aamc.org/
eweb/upload/Medicare%20Payments%
20for%20Graduate%20Medical%
20Education%202013.pdf).
5. Anderson GF, Lave JR, Russe CM, Neuman P. Providing hospital services: the
changing financial environment. Baltimore:
Johns Hopkins University Press, 1989:107.
DOI: 10.1056/NEJMp1403609
Copyright 2014 Massachusetts Medical Society.
Tuberculosis Control in New York City A Changing Landscape
Michelle Macaraig, Dr.P.H., M.P.H., Joseph Burzynski, M.D., M.P.H., and Jay K. Varma, M.D.
ince the introduction of chemotherapy for treating tuberculosis, political commitment and
stable, sufficient funding have
been the primary predictors of
success for tuberculosis-control
2362
programs, and their absence has
resulted in tuberculosis epidemics. Over the past decade, the
federal funding for tuberculosiscontrol programs in the United
States has decreased by more
than 15%, even without adjusting for inflation, according to
the Centers for Disease Control
and Prevention. The incidence of
tuberculosis continues to decline
nationally, but in recent years
n engl j med 370;25nejm.orgjune 19, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 8, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Você também pode gostar
- Your Urgent Feedback Is Needed ASAP: Remain Blessed YoursDocumento1 páginaYour Urgent Feedback Is Needed ASAP: Remain Blessed YoursYoga Rossi Widya UtamaAinda não há avaliações
- Your Urgent Feedback Is Needed ASAP: Remain Blessed YoursDocumento1 páginaYour Urgent Feedback Is Needed ASAP: Remain Blessed YoursYoga Rossi Widya UtamaAinda não há avaliações
- Journal of NeurosurgeryDocumento9 páginasJournal of NeurosurgeryYoga Rossi Widya UtamaAinda não há avaliações
- Neuropsychopharmacology ReviewsDocumento22 páginasNeuropsychopharmacology ReviewsYoga Rossi Widya UtamaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (119)
- Vishal Seminar Report StrokeDocumento40 páginasVishal Seminar Report StrokeVishal kaushikAinda não há avaliações
- Corrosion and Its Objective QuestionsDocumento2 páginasCorrosion and Its Objective QuestionsSrinivasan Alagappan100% (4)
- Blessed Are Those Who MournDocumento7 páginasBlessed Are Those Who MournPatrick MabbaguAinda não há avaliações
- Proposed Rule: Airworthiness Directives: Bell Helicopter Textron CanadaDocumento3 páginasProposed Rule: Airworthiness Directives: Bell Helicopter Textron CanadaJustia.comAinda não há avaliações
- Communicating Across AgesDocumento35 páginasCommunicating Across AgesConrad TarihoranAinda não há avaliações
- Monica Stelly Resume 2017Documento2 páginasMonica Stelly Resume 2017api-355097199Ainda não há avaliações
- Lappasieugd - 01 12 2022 - 31 12 2022Documento224 páginasLappasieugd - 01 12 2022 - 31 12 2022Sri AriatiAinda não há avaliações
- 6d Class 10Documento10 páginas6d Class 10Euna DawkinsAinda não há avaliações
- ICH Topic Q 3 B (R2) Impurities in New Drug Products: European Medicines AgencyDocumento14 páginasICH Topic Q 3 B (R2) Impurities in New Drug Products: European Medicines AgencyJesus Barcenas HernandezAinda não há avaliações
- 30 Natural Ways To Help Treat Polycystic Ovary SyndromeDocumento12 páginas30 Natural Ways To Help Treat Polycystic Ovary SyndromeArun AchalamAinda não há avaliações
- Motor Doosan DV11Documento220 páginasMotor Doosan DV11David Catari100% (4)
- CX-5 BX-10 No. 1 & 1.5 Fluid Cylinder PartsDocumento5 páginasCX-5 BX-10 No. 1 & 1.5 Fluid Cylinder PartsPierreAinda não há avaliações
- ADA Concept GuideDocumento10 páginasADA Concept GuidemoalpohoAinda não há avaliações
- Save Our Forests Through Sustainable DevelopmentDocumento33 páginasSave Our Forests Through Sustainable DevelopmentGeehthanJIAinda não há avaliações
- Kawasaki Ultra 250x Manual de Taller PDFDocumento477 páginasKawasaki Ultra 250x Manual de Taller PDFAntonio Jose Planells100% (3)
- Stomach CancerDocumento19 páginasStomach CancerChristofer MadrigalAinda não há avaliações
- Vocational training at BHELDocumento36 páginasVocational training at BHELafAinda não há avaliações
- Intellectual Property: Impact of Exhaustion of Intellectual Property Right On Pharmaceutical Industry in VietnamDocumento26 páginasIntellectual Property: Impact of Exhaustion of Intellectual Property Right On Pharmaceutical Industry in VietnamSơn BadGuyAinda não há avaliações
- ITC's diverse businesses: cigarettes, packaging, hotels, paperboards, stationery, matches, incense sticks, retail, food, exportsDocumento1 páginaITC's diverse businesses: cigarettes, packaging, hotels, paperboards, stationery, matches, incense sticks, retail, food, exportsShashank JainAinda não há avaliações
- 10893259-PIB 背钳弹簧保持架垫片落物事件Documento2 páginas10893259-PIB 背钳弹簧保持架垫片落物事件xlzyydf2015Ainda não há avaliações
- Lecture 4 Part 1 PDFDocumento11 páginasLecture 4 Part 1 PDFBashar AntriAinda não há avaliações
- GEK_30375M Lubrication SpecificationsDocumento34 páginasGEK_30375M Lubrication SpecificationsMARITZA GABRIELA ARIZABAL MEDINAAinda não há avaliações
- ADDITIONAL SOLVED PROBLEMS AND MINICASESDocumento155 páginasADDITIONAL SOLVED PROBLEMS AND MINICASESMera Birthday 2021Ainda não há avaliações
- Soap Making: Borax (NaDocumento15 páginasSoap Making: Borax (Naa aAinda não há avaliações
- PC 4. Emulsiones Tipo MayonesasDocumento10 páginasPC 4. Emulsiones Tipo MayonesasmadarahuchihaAinda não há avaliações
- Calcul BADocumento15 páginasCalcul BAHanane BenGamraAinda não há avaliações
- Masagana High School: Module 4: Planning For Continuing Professional Development and Lac PlanningDocumento6 páginasMasagana High School: Module 4: Planning For Continuing Professional Development and Lac PlanningjhonaAinda não há avaliações
- Marital Rape in IndiaDocumento8 páginasMarital Rape in IndiaSHUBHANK SUMANAinda não há avaliações
- Work Procedure For CCB Installation of Raised Floor 2Documento13 páginasWork Procedure For CCB Installation of Raised Floor 2ResearcherAinda não há avaliações
- Simonson 20033wDocumento15 páginasSimonson 20033wbahrul.hidayah@yahoo.comAinda não há avaliações