Escolar Documentos
Profissional Documentos
Cultura Documentos
AMEE Guide Supplements - Workplace-Based Assessment As An Educational Tool. Guide Supplement 31.1-Viewpoint1
Enviado por
Saeed Al-YafeiTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
AMEE Guide Supplements - Workplace-Based Assessment As An Educational Tool. Guide Supplement 31.1-Viewpoint1
Enviado por
Saeed Al-YafeiDireitos autorais:
Formatos disponíveis
2009; 31: 5960
AMEE guide supplements: Workplace-based
assessment as an educational tool. Guide
supplement 31.1 Viewpoint1
HOSSAM HAMDY
Med Teach Downloaded from informahealthcare.com by Marshall University on 10/28/14
For personal use only.
University of Sharjah, United Arab Emirates
Over the last two decades, important global reforms have
taken place in medical education at the undergraduate and
postgraduate levels. Emphasis on outcome based education
led to the development and refinement of performance based
assessment instruments and tools in order to assess these
outcomes (Friedman & Mennin 1991). All this has been linked
to the issue of quality and standards in medical education.
In the UK, the Calman and GMC Tomorrows Doctors
reports were key in the revolutionary change in undergraduate
and postgraduate training. The reports clearly stated that
supervision and feedback are crucial . . .. The integration of
theoretical teaching with practical work, progressive assessment and feedback to teachers and trainees are essential
(Calman 1993; General Medical Council 1993).
In the US, the Accreditation Committee of Graduate Medical
Educators (ACGME 2000) had a similar effect on residency
training programmes through the six general competencies for
evaluating residents.
The culture of training of doctors is changing from being
opportunistic to structured, planned cycles of activities,
blended with service and evaluating the trainees performance
and progress from one level to the next.
The assessment of what the trainee does in real life
on-the-job is what is now commonly described as workplacebased assessment or in-vivo assessment. This is in contrast to
in-vitro assessment which evaluates what the trainee can do
in controlled representations of practice such as the OSCE
(Rethans 1991).
In the UK, the Royal College of General Practitioners have
defined workplace-based assessment as: the evaluation of a
doctors progress over time in their performance in those areas
of professional practice best tested in the workplace
(Swanwick & Chana 2005; Deighan 2007). It should include
a process of collection of evidence of performance over the
difference phases of training.
As it is well known in education assessment drives
learning, workplace-based assessment plays a pivotal role in
aligning training and learning with assessment. On the Millers
pyramid of conceptual assessment of clinical competencies, it
represents measurement at the top of the pyramid, does in a
real work environment and a high degree of authenticity
(Miller 1990).
Workplace-based training has suffered at the undergraduate clerkship and postgraduates residency training levels
from lack of observaxtion of the trainee, poor assessment of
clinical competencies when encountering real patients and
no or poor feedback. In order to increase the effectiveness of
workplace-based training, these problems need to be
addressed and rectified.
The tasks performed by the trainee should be observed and
effective feedback provided; addressing the quality of
performance using defined criteria and description of specific
behaviour rather than general statements of good or bad
performance. The headline results of the BEME systematic
review on assessment, feedback and physicians clinical
performance indicated that feedback can change physicians
clinical performance when provided systematically over
multiple years by an authoritative credit source. (Veloski
et al. 2006).
The AMEE guide 31 on Workplace-based assessment as an
educational tool by Norcini & Burch (2007) gives a
comprehensive description of assessment tools commonly
used in North America and UK. The authors are well known
authorities in the field and have contributed to the development of some of the described instruments e.g. mini-CEX
(Norcini et al. 2003). The five sections of the guide cover the
main literature on the efficacy and prevalence of formative
assessment and feedback, common methods of workplacebased assessment, faculty development on how to be an
effective supervisor in giving feedback and challenges in
implementation.
In reading the Guide, I would like to highlight four points:
1.
2.
Workplace-based assessment is equally valuable for the
trainee and the trainer. It should be considered as an
integral component of an experiential learning cycle
which includes a planning phase, observation phase
and a reflection phase on performance expressed in
a constructive feedback to both the trainee and the
trainer leading to a new cycle of planning and
improvement of the training programme.
The Guide explicitly describes workplace-based assessment as a formative tool with a primary objective
of providing feedback based on observation of
Correspondence: Hossam Hamdy, College of Medicine, University of Sharjah, United Arab Emirates. Email: profhossamhamdy@yahoo.com
ISSN 0142159X print/ISSN 1466187X online/09/0100592 2009 Informa Healthcare Ltd.
DOI: 10.1080/01421590802298215
59
H. Hamdy
Med Teach Downloaded from informahealthcare.com by Marshall University on 10/28/14
For personal use only.
3.
4.
performance by the supervisors or other stakeholders;
multi-source feedback. Using these methods for
summative assessment needs better control of the
confounding variables, which are always related to
the real workplace environment and are directly linked
to the healthcare delivery system, context of practice
and variables in the complexity of the patients
problems encountered.
The mini-CEX, which has gained popularity in postgraduate settings, requires 1214 encounters with real
patients in order to achieve a reliability co-efficient of
0.8 (Norcini et al. 2003). The main advantage of this
method is its authenticity by using real patients. On the
other hand, it is important to notice that it assesses a
component of the encounter, not its totality. Another
method which is described in the literature and not
mentioned in the guide is the direct observation
clinical encounter examination (DOCE), described
by Hamdy et al. (2003) as a summative assessment
in the clerkship phase and on a final comprehensive
examination. Students encounter four real patients
with different health problems in different age groups.
Focused history taking, physical examination, reasoning, decision making and communication skills with
real patients are observed and assessed using a
checklist. The generalizability coefficient reported was
0.84 indicating high reliability. Although this method
was not reported in postgraduate residency programmes, it has potential for use as both a formative
and summative assessment method. Its main advantage
is evaluation of the encounter in its totality and the
small number of patients needed in sampling students
or trainees performance.
The guide emphasises the importance of training
faculty on how to use these methods, how to give
feedback and after collecting this information, what to
do with it. Before introducing these methods in
postgraduate or undergraduate medical education
programmes, effective training of faculty and supervisors should take place in order to ensure its successful
implementation and develop their skills in providing
high quality and honest feedback, particularly in the
face of poor and under-performers.
Applying these methods in a busy workplace is a difficult task
which necessitates the identification of interested clinical
60
educators who have the time or will give the time to supervise
the training and create a culture of observation of performance
and feedback.
Declaration of interest: The authors report no conflicts of
interest. The authors alone are responsible for the content and
writing of the paper.
Notes on contributor
Prof HOSSAM HAMDY is the Vice Chancellor for Medical & Health
Sciences College at the College of Medicine, University of Sharjah and
Professor of Surgery and Medical Education.
Note
1. This AMEE guide was published as: Norcini J, Burch V. 2007.
Workplace-based assessment as an educational tool: AMEE
Guide no. 31. Med Teach 29:855871.
References
ACGME (Accreditation Council for Graduate Medical Education) 2000.
Outcome project: General competencies [on line]. Available at http://
www.acgme.org/outcome (accessed June 2007).
Calman KC. 1993. Medical education: A look into the future. Postgrad Med
Educ. 69(supplement 2):5355.
Deighan M. 2007. The learning and teaching guide (London, UK: Royal
College of General Practitioners).
Friedman M, Mennin SP. 1991. Rethinking critical issues in performance
assessment. Acad Med 66:390395.
General Medical Council. 1993. Tomorrows doctors: Recommendations on
undergraduate medical education (London, GMC).
Hamdy H, Prasad K, Williams R, Salih FA. 2003. Reliability and validity of
the direct observation clinical encounter examination (DOCEE).
Med Educ 37:205212.
Miller GE. 1990. The assessment of clinical skills/competence/performance.
Acad Med. 65:563567.
Norcini J, Blank L, Duffy FD, Fortina G. 2003. The mini-CEX: A method of
assessing clinical skills. Ann Intern Med 138:476481.
Norcini J, Burch V. 2007. Workplace-based assessment as an educational
tool: AMEE guide no 31. Med Teach 29:855871.
Rethans JJ. 1991. Does competence predict performance? Standardized
patients as a means to investigate the relationship between competence
and performance of general practitioners. Thesis (Amsterdam: Thesis)
Publishers.
Swanwick T, Chana N. 2005. Workplace assessment for licensing in general
practice. Discussion paper. Br J Gen Pract 6:461467.
Veloski J, Boex JR, Grusberger M, Evans A, Wolfson DB. 2006. BEME guide
no. 7. Systematic review of the literature on assessment, feedback and
physicians clinical performance. Med Teach 28:117128.
Você também pode gostar
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- How To Write A Journal ArticleDocumento50 páginasHow To Write A Journal ArticleSaeed Al-Yafei80% (5)
- Lesson Plan - Contemporary Arts From The PhilippinesDocumento4 páginasLesson Plan - Contemporary Arts From The PhilippinesEljay Flores96% (25)
- 22 Self-Actualization Tests & Tools To Apply Maslow's TheoryDocumento34 páginas22 Self-Actualization Tests & Tools To Apply Maslow's TheoryIbrahim HarfoushAinda não há avaliações
- Nephrology MCQsDocumento7 páginasNephrology MCQsSaeed Al-Yafei67% (6)
- Assessment Form 2 PDFDocumento1 páginaAssessment Form 2 PDFAgnes Bansil Vitug100% (1)
- Skelly S Mcqs in Tropical MedicineDocumento29 páginasSkelly S Mcqs in Tropical MedicineSaeed Al-Yafei92% (13)
- Cognitive PsychologyDocumento22 páginasCognitive PsychologySaeed Al-Yafei100% (6)
- How To Write A Scientific Original ArticleDocumento67 páginasHow To Write A Scientific Original ArticleSaeed Al-YafeiAinda não há avaliações
- Speak Out Intermediate Tests Track ListingDocumento1 páginaSpeak Out Intermediate Tests Track Listingbob43% (7)
- What Makes A Good TeacherDocumento4 páginasWhat Makes A Good TeacherJravi ShastriAinda não há avaliações
- Diagnosis of Gastrointestinal Bleeding in AdultsDocumento8 páginasDiagnosis of Gastrointestinal Bleeding in AdultsSaeed Al-YafeiAinda não há avaliações
- Endnote 7 TrainingDocumento84 páginasEndnote 7 TrainingSaeed Al-Yafei100% (2)
- Preparatory Lecture: Confounding and BiasDocumento144 páginasPreparatory Lecture: Confounding and BiasSaeed Al-YafeiAinda não há avaliações
- Probability Calculation in MinesweeperDocumento2 páginasProbability Calculation in MinesweeperBrayan Perez ContrerasAinda não há avaliações
- Exam Steps and Process - Read FirstDocumento3 páginasExam Steps and Process - Read FirstDeejaay2010Ainda não há avaliações
- The Implications of The Dodo Bird Verdict For Training in Psychotherapy Prioritizing Process ObservationDocumento4 páginasThe Implications of The Dodo Bird Verdict For Training in Psychotherapy Prioritizing Process ObservationSebastian PorcelAinda não há avaliações
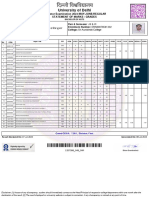
- University of Delhi: Semester Examination 2023-MAY-JUNE:REGULAR Statement of Marks / GradesDocumento2 páginasUniversity of Delhi: Semester Examination 2023-MAY-JUNE:REGULAR Statement of Marks / GradesFit CollegeAinda não há avaliações
- Information Brochure & Guidelines For Filling of Online Application Form For Recruitment of Non-Teaching Positions in Delhi UniversityDocumento106 páginasInformation Brochure & Guidelines For Filling of Online Application Form For Recruitment of Non-Teaching Positions in Delhi UniversityVidhiLegal BlogAinda não há avaliações
- Cambridge Aice Marine Science SyllabusDocumento32 páginasCambridge Aice Marine Science Syllabusapi-280088207Ainda não há avaliações
- Resume 2021 RDocumento3 páginasResume 2021 Rapi-576057342Ainda não há avaliações
- Mslearn dp100 14Documento2 páginasMslearn dp100 14Emily RapaniAinda não há avaliações
- Department of Theatre and Film Studies: Nnamdi Azikiwe UniversityDocumento7 páginasDepartment of Theatre and Film Studies: Nnamdi Azikiwe Universityanon_453956231Ainda não há avaliações
- Structure of Academic TextsDocumento22 páginasStructure of Academic TextsBehappy 89Ainda não há avaliações
- Drivers Ed Homework AnswersDocumento7 páginasDrivers Ed Homework Answersafnogtyaiergwk100% (1)
- Marketing Management Course OutlineDocumento3 páginasMarketing Management Course OutlineShehryar HumayunAinda não há avaliações
- Advisory Assignment Order Junior High SchoolDocumento1 páginaAdvisory Assignment Order Junior High SchoolJaz and Ysha's ChannelAinda não há avaliações
- GCSE New Spec Performance MarksheetDocumento2 páginasGCSE New Spec Performance MarksheetChris PowellAinda não há avaliações
- Algebraic FractionsDocumento11 páginasAlgebraic FractionsSafiya Shiraz ImamudeenAinda não há avaliações
- Building Your Weekly SDR Calendar-Peer Review Assignment-Mohamed AbdelrahmanDocumento3 páginasBuilding Your Weekly SDR Calendar-Peer Review Assignment-Mohamed AbdelrahmanrtwthcdjwtAinda não há avaliações
- Linux AdministrationDocumento361 páginasLinux AdministrationmohdkmnAinda não há avaliações
- Barnard College, Title IX, Dismissal LetterDocumento3 páginasBarnard College, Title IX, Dismissal LetterWhirlfluxAinda não há avaliações
- HR Questions InterviewDocumento54 páginasHR Questions InterviewAlice AliceAinda não há avaliações
- 4-ProjectCharterTemplatePDF 0Documento5 páginas4-ProjectCharterTemplatePDF 0maria shintaAinda não há avaliações
- YPD Guide Executive Summary PDFDocumento2 páginasYPD Guide Executive Summary PDFAlex FarrowAinda não há avaliações
- Bbfa4034 Accounting Theory & Practice 1: MAIN SOURCE of Reference - Coursework Test + Final ExamDocumento12 páginasBbfa4034 Accounting Theory & Practice 1: MAIN SOURCE of Reference - Coursework Test + Final ExamCHONG JIA WEN CARMENAinda não há avaliações
- Virtue Ethics FinalDocumento19 páginasVirtue Ethics FinalAlna JaeAinda não há avaliações
- PHD Ordinance Msubaroda IndiaDocumento15 páginasPHD Ordinance Msubaroda IndiaBhagirath Baria100% (1)
- Project 2 ExampleDocumento6 páginasProject 2 ExampleShalomAinda não há avaliações