Escolar Documentos
Profissional Documentos
Cultura Documentos
DRF
Enviado por
jangnoesaTítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
DRF
Enviado por
jangnoesaDireitos autorais:
Formatos disponíveis
RESEARCH
CONFLICTING PRIORITIES: EMERGENCY NURSES
PERCEIVED DISCONNECT BETWEEN PATIENT
SATISFACTION AND THE DELIVERY OF
QUALITY PATIENT CARE
Author: Mary L. Johansen, PhD, NE-BC, RN, Newark, NJwwwwww
Introduction: As hospitals compete for patients and their
healthcare dollars, the emergency nurse is being asked to
provide excellent nursing care to customers rather than
patients. This has changed the approach in delivering quality
care and has created favorable conditions for conflict as the
nurse tries to achieve specific patient satisfaction goals.
Methods: A sample of 9 emergency nurses from 2 hospitals
in northern New Jersey participated in focus groups designed
to learn about the types of conflict commonly encountered, and
to identify the attitudes and understanding of the emergency
nurses experiencing conflict and how interpersonal conflict is
dealt with.
Results: Thematic content analysis identified an overarching
theme of conflicting priorities that represented a perceived
disconnect between the priority of the ED leadership to
achieve high patient satisfaction scores and nurses priority to
urses working in the emergency department are
confronted with conflict every day. Conflict is an
inevitable part of life when one works in a fast-paced
and demanding environment. The ED environment provides
favorable conditions for conflict as the nurse navigates constant
change, people who are in extremely vulnerable emotional positions, demanding workloads, poor communication, and critical
incidents such as unexpected patient deaths.1-3 Compounding
Mary L. Johansen, Member, ENA Chapter 24, is Assistant Clinical Professor,
Rutgers University, College of Nursing, Newark, NJ.
For correspondence, write: Mary L. Johansen, PhD, NE-BC, RN, Rutgers
University, College of Nursing, Ackerson Hall, Room 324, 180 University
Avenue, Newark, NJ 07102; E-mail: mjohanse@rutgers.edu.
J Emerg Nurs 2014;40:13-9.
Available online 26 July 2012.
0099-1767/$36.00
Copyright 2014 Emergency Nurses Association. Published by Elsevier Inc.
All rights reserved.
http://dx.doi.org/10.1016/j.jen.2012.04.013
January 2014
VOLUME 40 ISSUE 1
provide quality care. Three interacting sub-themes were
identified: (1) staffing levels, (2) leaders dont understand, and
(3) unrealistic expectations. The study also found that
avoidance was the approach to manage conflict.
Discussion: The core conflict of conflicting priorities was
based on the emergency nurses perception that while patient
satisfaction is important, it is not necessarily an indicator of
quality of care. Interacting sub-themes reflect the way in
which conflict priorities were influenced by patient satisfaction
and the nurses ability to provide quality care. Avoidant
conflict management style was used to resolve conflicting
priorities because nurses perceive that there is not enough
time to address conflict even though it could impact on work
stress and patient care.
Key words: Conflict management; Emergency department conflict;
Patient satisfaction; Quality patient care
the problem is the requirement placed on the emergency nurse
to achieve specific patient satisfaction goals. The comparison of
hospitals on topics that are important to consumers has led to
the determination by hospitals that superior patient satisfaction
is vital to their financial success and has refocused the efforts of
the nurse to view patients as customers.4,5 This focus places an
enormous burden on emergency nurses to provide hotel service quality patient care in a smooth, holistic, and speedy manner, which is not always congruent with the ED environment
or even the patients medical needs.
Interpersonal conflict or conflict between individual
members of the health care team is the most common
source of conflict in the emergency department.6 Although
it is generally viewed as confrontational behavior, conflict
has multiple meanings. In the literature, it is defined as
inherent differences in goals, needs, desires, responsibilities,
perceptions, and ideas that are generally predictable. 7
When conflict is not resolved well, it can become problematic quickly and negative consequences can occur, such as
work stress, burnout, absenteeism, decreased productivity,
WWW.JENONLINE.ORG
13
RESEARCH/Johansen
and reduced quality of care. 8,9 These negative consequences contribute to high staff turnover that occurs at a
time when emergency nurses are needed more than ever.2,4
Although ED environments are among the most
demanding and stressful in health care,2,10 little is known
about nurses perceptions of conflicts. Managing conflicts is
among the key challenges facing the emergency nurse, and
it is in the interest of the nurse not to avoid conflict in the
emergency department but to productively manage disagreements with skilled communication. Both the American Association of Critical Care Nurses11 and The Joint Commission
(JC)10 recognize that proficiency in communication skills is
an essential element to a healthy work environment among
members of the health care team. Good communication also
improves relationships with patients and families, who are the
consumers of nursing care. A breakdown in communication
and collaboration can lead to disruptive behaviors by the
involved parties and increased patient errors.3,8,10 Handling
conflicts in an efficient and effective manner may result in
improved quality, patient safety, and staff morale and may
reduce work stress for the emergency nurse.
Although conflict is an inevitable characteristic of work
environments, it is not conflict but rather the style with
which the individual manages conflict that is important
and that directly affects worker and patient outcomes.12
Effective resolution of conflict depends on assessing the nature of the conflict and selecting the most appropriate management style for the situation. Research suggests that the
conflict management style rendered by the nurse in response
to conflict may directly affect her level of work stress and also
may affect the clinical outcomes of the patient.13-16 The aims
of this study were to: (1) learn more about the types of conflict emergency nurses are commonly encountering, (2) identify the ideas, attitudes, understanding, and thinking patterns
of the emergency nurse regarding the phenomenon of conflict, and (3) to understand how emergency nurses currently
deal with interpersonal conflict.
Method
RESEARCH DESIGN
A qualitative research design featuring focus groups composed of nurses working in the emergency department was
used in this study. Qualitative research allows the individuals
perspective of phenomena to be studied in the context in
which the event occurs, providing rich descriptions that
enable the reader to understanding the reality of the phenomenon being studied.17,18 Focus groups rather than individual
interviews were used because group interaction is thought to
be a significant attribute that helps people explore and clarify
views that are less accessible in one-on-one interviews.
14
JOURNAL OF EMERGENCY NURSING
Focus groups produce insight and a rich amount of
experiential information that allows the participants to hear
and respond to diverse viewpoints.18-20 Focus group interaction may reveal more about what the emergency nurse
understands of a particular conflict and the reasoning
behind her or his conflict resolution approach.18
A focus group discussion guide was developed by the
researcher. This guide included items related to the most vexing and recurring types of conflicts that emergency nurses
encounter at work, who the conflict is most often with and
what it is about, and how the individual nurse and the organization handle such conflict. Finally, participants were asked
about training in managing conflict in the emergency department and the types of factors that might be used to measure
whether the training was effective in helping the emergency
department do its job better or more successfully.
RESEARCH SETTING
The nurse participants were recruited from 2 acute care
facilities located in Northern New Jersey. One focus
group was held in a private conference room at each organization where the staffs are employed. The date, time,
and location of the room were disclosed only to focus
group nurse participants.
RESEARCH PROCEDURE
Institutional Review Board approval was obtained. Strict adherence to the requirements for the protection of human subjects
were followed, and the investigator completed the human subjects training and followed the policies and procedures related
to safe and ethical practices, confidentiality, and informed consent. Loss of confidentiality and emotional discomfort were
potential risks when describing experiences. Precautions were
taken to minimize these risks by thoroughly explaining the
study, using a trained moderator, and emphasizing that participation was voluntary. The nurses were asked to sign an
informed consent document before the start of the session
and were informed that they could choose to withdraw at
any time and/or choose not to answer any questions that made
them uncomfortable. Because the intent of this study was to
understand how nurses think and talk about a particular topic,
purposive sampling rather than random sampling was used to
select the focus group participants.18,19
The chief nursing officer and the nursing leadership
of the 2 acute care facilities assisted in providing access to
the emergency nurses. The principal investigator (PI)
recruited nurses from each emergency department who
met the inclusion criteria, that is, being currently
employed as a professional registered nurse in a hospital-based emergency department in the United States
and being a direct patient care provider. Contact was
VOLUME 40 ISSUE 1
January 2014
Johansen/RESEARCH
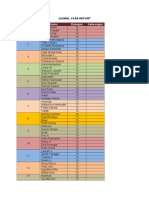
TABLE 1
TABLE 2
Demographic characteristics of the sample
Variable
Gender
Male
Female
Race
African American/black
Alaskan Native or
American Indian
Asian
Hispanic
Pacific Islander
Caucasian/white
Mixed race
Highest nursing degree
Diploma
Associate degree
Baccalaureate degree
Masters degree
Magnet
Yes
No
Board certification in
emergency nursing
Yes
No
Conflict resolution training
Yes
No
Current position
Staff nurse
Charge nurse
Team leader/shift coordinator
Descriptive data for the sample
1
8
10
90
0
0
0
0
1
0
1
8
0
0
0
10
90
0
2
2
3
2
22
22
33
22
6
3
67
33
1
8
10
90
5
4
56
44
8
0
1
90
0
10
made through an E-mail invitation that explained the
purpose of the study, the consent for participation, and
an explanation of how the rights of the nurse would be
protected. Nurses who were interested in the study were
asked to respond to the E-mail invitation and subsequently were contacted by the PI. Only the selected individuals had access to this information.
SAMPLE
Nine nurses participated in 2 focus groups. The majority of
the nurses were white women (n = 8) who were employed
full time as staff nurses and were not board certified in
January 2014
VOLUME 40 ISSUE 1
Variable
Mean
SD
Range
Age (y)
Years of nursing
experience
Years of ED nursing
experience
Years worked in current
position
37.3
16.88
11.98
16.09
23-59 y
2-42 y
11.77
10.88
2-31 y
9.1
9.83
6 mo-26 y
emergency nursing. Two thirds of the nurses worked in
facilities designated as magnet hospitals, and almost 25%
had received some type of formal training in conflict resolution. More than half of the nurses were baccalaureate prepared (Table 1).
The mean age of the nurses was 37.3 years (SD,
11.98). One third of the nurses had 30 years or more of
experience (n = 3), whereas the remaining two thirds had
2 to 13 years experience (n = 6). Two thirds of the nurses
had less than 7 years experience (n = 6), and the remaining third had 20 to 31 years of ED experience (n = 3)
and had worked in their present position for more than
1 year. Descriptive data for the sample are presented in
Table 2.
DATA COLLECTION
Nurse participants meeting the inclusion criteria were
divided into two groups with 4 to 5 nurses per group. Each
focus group session was digitally recorded to capture accurate data for typed verbatim transcripts. The PI and focus
group nurse participants sat around a table to facilitate the
discussion. A demographic questionnaire was distributed
to the group. The PI followed a focus group guide while
conducting each session. The focus group sessions lasted
30 to 45 minutes.
DATA ANALYSIS
The focus group recorded session was transcribed verbatim and checked for accuracy through careful review(s)
by the PI, who read the transcript while listening to
the digital recording. Although transcript-based analysis
is time consuming, it is the most rigorous way of drawing out key comments.19
Thematic content analysis was used to analyze focus
group data. A list of common themes was extracted from
the texts by the researcher to give expression to the communality of voices across participants.20 The transcribed
text was read as a whole first and then uploaded into
WWW.JENONLINE.ORG
15
RESEARCH/Johansen
Atlas-Ti to facilitate analysis. Codes were generated
through careful readings from the transcripts by the PI.
Codes were reviewed and collapsed into a coding template
that then was used to consistently label data segments that
contained similar material.18-20 The Atlas-ti computer software program was used to organize the coded segments and
relate them to a particular theme or sub-theme. Analysis of
the themes was conducted to enable the PI to answer the
research questions: (1) What types of conflicts are commonly encountered? (2) What are the ideas, attitudes,
understanding and thinking patterns of the emergency
nurse experiencing a conflict? and (3) How do emergency
nurses currently deal with interpersonal conflict?
Results
The results identified insightful information regarding the
conflicts emergency nurses are encountering and how they
currently deal with them. In general, the nurse participants
defined conflict as a disagreement that interfered with the
delivery of patient care and was associated with negative
emotional reactions. During the nurses discussion of their
experience of conflict in the ED workplace, an overarching
theme emerged, conflicting priorities, that could have an
impact on their work stress and patient care. The ED leadership priority was perceived to be achieving high patient
satisfaction scores, whereas the priority for the emergency
nurses was to provide quality care. This core conflict was
based on the emergency nurses perception that although
patient satisfaction is important, it is not necessarily an
indicator of quality of care. When speaking about patient
satisfaction, one nurse explained,
That makes us feel like we are servants, maybe like waitresses,
or I dont knowI mean, we do serve the population and we
are supposed to do that, but I (ah) its kind of demeaning,
actually, I think cause we are all doing a good job and we are
working as fast as we can and do the best quality we can for
everybody, but its never enough!
This overarching theme of conflicting priorities
encompassed 3 interacting sub-themes:
1. Staffing levels
2. Leaders dont understand
3. Unrealistic expectations
STAFFING LEVELS
Conflict with staffing levels and patient flow was a leading
issue of distress for the nurse participants. The doors to the
emergency department never close. Patient flow is contin-
16
JOURNAL OF EMERGENCY NURSING
uous but with peaks of patient volume throughout the day.
Although established staffing patterns guide the safe assignment of patients to nurses, any drastic fluctuation in census
or patient acuity can affect the nurse-to-patient ratio. This
situation provides a significant source of frustration for the
nurses and illustrates the conflict priorities. One nurse stated, You are going to be overwhelmed with the number of
people you are going to get.
This sentiment was echoed by other nurses, who perceived that the driving force behind patient throughput
from triage to the main emergency department was
patient satisfaction:
If you are staffed for 40 (patients) and you have 40 patients in
your ED but you have another 20 in your waiting room,
those 20 are coming back. Who is increasing that ratio?
We are constantly pushed to the edge that these patients need
to come back, and thats a safety issue.
Managers want the ER to run efficiently with whatever
staffing is there. Patient satisfaction is what they are concerned with.
In these situations, conflict arose between the nurse
and the charge nurse. For example, one participant noted,
The charge nurse is pressuring [us] to bring those patients
back. Why is the charge nurse continuing to bring us these
patients that nobody wants?
The participants also placed a strong emphasis on patient
acuity and its contributory role in staffing level conflict. One
nurse described the fragile relationship between patient
assignments, acuity, stress, and conflict: You may be getting
your sixth patient and another nurse may have 2, but she may
be on a one to one with those 2 patients, and you have no
knowledge so you are building up hostility.
Several nurses pointed out that there is a double standard when it comes to staffing levels in the emergency
department and the rest of the hospital. This double standard also was a frequent source of distress and frustration.
A host of comments illustrated this point:
With high acuity throughout the institution, you have a ratio of 1 to 1 or 1 to 2 and in the ED you dont have any
dynamic of ratios. You can have 3 critically ill patients and
3 other patients.
It doesnt matter how many ICU patients you have, you
just repeatedly keep getting the ICU just because its your
turn, it doesnt matter what the acuity is.
I dont understand how within an institution you can
have a state directive that you have to have 1 nurse to
2 patients in this setting but a couple of floors down
that doesnt apply at all. There is something very wrong
with that.
VOLUME 40 ISSUE 1
January 2014
Johansen/RESEARCH
LEADERS DONT UNDERSTAND
Conflicts with the ED leadership team/management
were described in detail by the participants. Nurses
observed that managers look at the computer screen
and count numbers.
Participants shared comments such as There is really
no consideration for the staff because its the patients who
are bringing in the scores that are bringing in everything
else that runs the hospital and I think the safety issue
is overlooked sometimes by management because our
(hospital) goal is patient satisfaction.
The nurses perceived a generalized lack of support
when patient volume and acuity were exceeding the
immediate available resources: You can have three critically ill patients and three other patients and management
doesnt step in and provide backup in the sense of dividing
up the assignments, pulling more staff.
Further, nurses indicated that after the volume and acuity diminish, the nurses are left to answer for all of the care
that was rendered as well as the care that was not rendered:
It becomes a very dangerous situation and its kinda because the environment is so hectic its overlooked until
it calms down and then youre asked to answer for things
that you had no awareness of. That level of stress for anyone who works in the ER is a very important dynamic and
I think throughout the United States its something thats
not looked at.
UNREALISTIC EXPECTATIONS
An important issue that emerged in the thematic analysis
was meeting what nurses perceived as unrealistic expectations of the organization. In an attempt to drive up patient
satisfaction scores, many hospitals are implementing programs to decrease overall waiting times and, more specifically, times to be seen by a physician. The nurses refer to
these time requirements as unreasonable because they create unrealistic expectations among patients of when they
are going to be seen, creating conflict between the nurse
and the patient: For the most part they [patients] expect
to be seen NOW and they expect to be seen immediately
by the doctor. One nurse shared, Ive had somebody
from this ER call 911 in 8 minutes because they [the
patient] werent seen quick enough and wanted to be
transferred to another hospital.
These target times also have created conflict between
the nurse and the physician because physicians likewise
are being held to a strict time requirement:
There is your conflict because you are giving a nurse who
has three critical care patients more patients but yet your
January 2014
VOLUME 40 ISSUE 1
process is designed to have a patient seen by a doctor within 20 minutes of arrival and the thing is that nobody wants
to take responsibility.
Nurses relating to this comment also added:
One doctor would expect you to take their patient before another doctor. They dont like to be put second to
each other. When physicians come at you, that they want
their patients to take priority.
The charge nurse is also caught in this time conflict
with the nurse and the management: Because the charge
nurse is pressuring to bring those patients back because she
has to respond to our director or whoever else who said,
Why are these people leaving?
DEALING WITH CONFLICT
To answer the final question, nurses were asked about how
they dealt with conflict. The predominant approach used by
the emergency nurse participants to resolve these conflicts
was avoidance. The style was chosen because it provided
minimal interruption. Numerous comments described the
frustrations experienced by the nurse:
Its not a matter that you dont deal with though, and you
dont have the time to deal with it. Your focus is on patient
care and that is what you set as your priority and you
manage it the best way you can.
So many patients and you have so many things to do and
you are so busy you just dont even have time to say anything, you just know that whats best for the patient you
have to care of the patient and just move on.
Discussion
The overarching theme identified by focus group participants was conflicting priorities that represented a perceived
disconnect between a focus on patient satisfaction and the
delivery of quality patient care. The nurses perceived that
the priority of the ED and hospital leadership was patient
satisfaction, whereas nurses priority was to provide quality
care. This perceived disconnect may lie in the conceptual
understanding of what constitutes quality care. The quality
of care in the emergency department has not been
addressed in the empirical literature. Established National
Database of Nursing Quality Indicators (NDNQI) indicators were developed primarily for inpatients. Now is the
time to validate NDNQI measures that are appropriate
in the emergency department and develop specific ones
for this setting.
The NDNQI5 provides operational definitions for
nurse-sensitive acute quality care indicators, which include
WWW.JENONLINE.ORG
17
RESEARCH/Johansen
pressure ulcers, falls, nosocomial infections, and patient
satisfaction as it relates to pain management, patient education, overall care, and nursing care. The ambulatory environment of the emergency department differs from that of
an inpatient setting. The mandatory elements of care
defined by regulatory bodies, expanding technologies for
documentation and care delivery, and frequent change present a complex maze of practice challenges for the ED
nurse, suggesting that there might be difference in how
quality of care should be defined and measured in the
emergency department. In this study, the nurses perception of quality of care was globally described as, taking care of those patients as you really want to take care
of them. Defining what quality of care means to the ED
nurse broadens our understanding of how quality should
be measured. This is an important first step toward
developing nurse-sensitive quality indicators that are
valid, reliable, and relevant to the emergency department.
As hospitals compete for patients and their health care
dollars, the emergency nurse is being asked to provide
excellent nursing care to customers rather than patients.
This situation is attributable in part to the fact that hospitals rely on patient satisfaction and Hospital Consumer
Assessment of Healthcare Providers and Systems scores to
measure their effectiveness in delivering health care services.21 This disconnect to deliver hotel services that
patients can appreciate rather than quality clinical care that
may not be tangible gave the nurses in this study the
impression that their contribution was not valued.
The sub-themes reflected the way that conflicting priorities affected nurses perceptions of their ability to provide
quality care. The use of patient satisfaction as the tool
employed to measure and evaluate how hospital expectations and goals are met placed pressure upon the relationships between nurses and patients, nurses and physicians,
nurses and charge nurses, and nurses and management.
The emergency nurses in this study reported feeling frustrated and powerless because management did not listen
to their issues of concern regarding unrealistic expectations
of overall waiting times and when patients are going to be
seen by a physician. Although appropriate staffing ratios in
the emergency department has been a conundrum for leadership/ management, participants verbalized a generalized
lack of support when patient volume and acuity exceeded
the immediate available resources.
Findings from this study reflect many of the conflict
issues that were identified in a recent survey of nurses conducted by the Center for American Nurses that examined
the nurses perception of conflict in the workplace. Respondents (n = 858) identified the need for effective leadership
to resolve conflict. The JC10 suggests that a proactive way
18
JOURNAL OF EMERGENCY NURSING
of addressing conflict issues, working through them, and
moving toward resolution supportive environment may
be achieved through collaborative practice and inter-professional dialogues across disciplines. This study shows that
ED leadership expectations affect both nurses and physician relationships and may have an effect on collaborative
practice in emergency departments.
Another major finding in this study is the perception
of the emergency nurse that there is not enough time to
address conflict even though it could have an impact on
work stress and patient care. Research has established that
the use of an avoidant conflict management style, as
demonstrated by the focus group participants, is related
to higher levels of work stress.13-15 This strategy prevents
the root problem from being addressed, and thus the conflict may persist. The JC10 has expressed concern about
this avoidance behavior because it can lead to very poor
communication, which certainly leads to poor patient
outcomes. It also can lead to a higher level of stress in
the nurse.
LIMITATIONS
The study findings are limited in terms of generalization.
This study was limited to only 2 emergency departments
from Northern New Jersey. Nevertheless, the data from
this study can provide insight into the nature of conflict
as defined as disagreements experienced by emergency
nurses, which can be applied to other ED settings that have
contextual similarities to those in which the data were collected.20 The sizes of the focus groups were not ideal.
However, the data attained was nevertheless rich and
meaningful. An additional limitation was the use of focus
groups rather than individual interviews, which has the
potential for peers to affect or limit the discussion and
the worthwhile information obtained.18-20
IMPLICATIONS FOR EMERGENCY NURSES
Emergency nurses need to be proactive about ensuring that
their contributions to patient care are measured.22 A collaborative effort by the ED leadership and nurses is needed to
ensure that nurse-sensitive quality indicators are included in
reports of hospital quality.4 To make this effort work, the
nurses and ED leaders first must agree on operational definitions of patient satisfaction and quality care. Data collection
instruments must include nurse-sensitive indicators that
measure the concepts of both patient satisfaction and quality
care.21 Quality indicators may include acute care NDNQI
measures such as falls and patient satisfaction as it relates
to pain management, patient education, nursing care, and
overall care. Examples of potential indicators appropriate
for the ED include triage quality (assessment and duration)
VOLUME 40 ISSUE 1
January 2014
Johansen/RESEARCH
and nurse activity (ongoing direct assessment and intervention). Quality indicators that are perceived as important by
ED nurses need to be developed and tested.
Demonstrating concern and providing a rationale for
decisions that affect the staff nurse go a long way to highlighting the importance of constructive relationships that
can effectively manage conflict.4 The ED leadership needs
to actively listen, develop structures to facilitate this collaborative process of resolving identified issues, and provide a
rationale for decisions as appropriate.2,10,23,24
Conclusion
Changes in health care delivery have required emergency
departments to reevaluate how they are delivering patient
care. Health care administrators have recognized that fiscal
viability is linked to patient satisfaction.21 Their efforts to
view patients as customers have changed the way nurses
approach the delivery of quality care and has created favorable conditions for conflict as the nurse tries to achieve specific patient satisfaction goals, such as reduced wait times,
while providing quality care. Findings from these focus
groups suggest that the emergency nurses perceptions of
the importance of patient satisfaction and quality of care
differ from those of patients and ED/hospital leadership.
This mismatch influences the nurses perception of leaders
understanding and the support from leadership/management in their approach to resolving staffing issues and organizational expectations. The important first step toward
developing nurse-sensitive quality indicators is defining
what patient satisfaction and quality of care means to the
ED nurse. ED leadership needs to recognize that conflicting priorities is not only a staff issue but an organizational
issue as well, because poor communication provides a work
environment that lends itself to conflict and stress.
REFERENCES
1. Emergency Nurses Association. Violence in the emergency department.
http://www.ena.org/government/Advocacy/Violence/Pages/Default.
aspx. Accessed November 30, 2011.
2. Institute of Medicine (IOM), 2006. Hospital-based emergency care:
at the breaking point. http://www.iom.edu/CMS/3809/16107/35007.
Accessed November 30, 2011.
3. Oster NS, Doyle CJ. Critical incident stress and challenges for the
emergency workplace. Emerg Med Clin North Am. 2000;18:339-413.
4. Dougherty C. Customer service in the emergency department. Top
Emerg Med. 2005;27:265-72.
January 2014
VOLUME 40 ISSUE 1
5. The National Database of Nursing Quality Indicators. https://www.
nursingquality.org/. Accessed April 26, 2012.
6. Cox KB. The effects of unit morale and interpersonal relations on conflict in the nursing unit. J Adv Nurs. 2001;35:17-25.
7. Almost J. Conflict within nursing work environments: concept analysis.
J Adv Nurs. 2006;53:444-54.
8. Aiken L, Kanai-Pak M, Sloane D, Poghosyan L. Poor work environment
and nurse inexperience are associated with burnout, job dissatisfaction
and quality deficits in Japanese hospitals. J Clin Nurs. 2008;17:3324-9.
9. Shader K, Broome M, Broome C, West M, Nash M. Factors influencing
satisfaction and anticipated turnover for nurses in an academic medical
center. J Nurs Adm. 2001;31:210-6.
10. Joint Commission. Sentinel event alert: behaviors that undermine a culture of safety. http://www.jointcommission.org/SentinelEvents/Sentinel
EventAlert/. Published 2006. Accessed November 1, 2011.
11. American Association of Critical Care Nurses. Standards for establishing
and sustaining healthy work environments: a journey to excellence.
http://www.aacn.org/WD/HWE/Docs/HWEStandards.pdf. Accessed
April 26, 2012.
12. Laschinger H, Purdy N, Cho J, Almost J. Antecedents and consequences
of nurse managers perceptions of organizational support. Nurs Econ.
2006;24:20-7.
13. Friedman R, Tidd S, Currall S, Tsai J. What goes around comes around:
the impact of personal conflict style on work conflict and stress. Int J
Confl Manage. 2000;11:32-55.
14. Montoro-Rodriguez J, Small J. The role of conflict resolution styles
on nursing staff morale, burnout and job satisfaction in long-term
care. J Aging Health. 2006;18:385-406.
15. Sportsman S, Hamilton P. Conflict management styles in the health
professions. J Prof Nurs. 2007;23:157-66.
16. Vivar CG. Putting conflict management into practice: a nursing case
study. J Nurs Manage. 2006;14:201-6.
17. Parahoo K. Nursing Research: Principles, Process and Issues. London: Macmillan; 1997.
18. Plummer-DAmato P. Focus group methodology part 2: considerations
for analysis. Int J Ther Rehabil. 2008;15:123-8.
19. Krueger RA. Focus Groups: A Practical Guide for Applied Research. 3rd ed.
Thousand Oaks, CA: Sage; 2000.
20. Sandelowski M, Barroso J. Handbook for Synthesizing Qualitative
Research. 1st ed. New York, NY: Springer; 2007.
21. Hospital Consumer Assessment of Healthcare Providers and Systems. HCAHPS: patients perspectives of care survey. https://www.
cms.gov/HospitalQualityInits/30-HospitalHCAHPS.asp. Accessed
November 3, 2011.
22. Yellen E. The influence of nurse-sensitive variables on patient satisfaction [research]. AORN J. 2003;2(783-788):790-3.
23. Friesen MA, DeWitty V, Osborne J, Rosenkranz A. Nurses perceptions
of conflict in the workplace: results of the Center for American Nurses.
Nurs First Online J. 2009;2:12-6.
24. Gerardi D. Using mediation techniques to manage conflict and create
healthy work environments. AACN Clin Issues. 2004;15:182-95.
WWW.JENONLINE.ORG
19
Você também pode gostar
- Jadwal Case ReportDocumento3 páginasJadwal Case ReportjangnoesaAinda não há avaliações
- The Yellow House: A Memoir (2019 National Book Award Winner)No EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Nota: 4 de 5 estrelas4/5 (98)
- Confounding Variable Is Information. This Research Employs A Close QuestionnaireDocumento1 páginaConfounding Variable Is Information. This Research Employs A Close QuestionnairejangnoesaAinda não há avaliações
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNo EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeNota: 4 de 5 estrelas4/5 (5794)
- Self-Assessment or Self Deception? A Lack of Association Between Nursing Students' Self-Assessment and PerformanceDocumento9 páginasSelf-Assessment or Self Deception? A Lack of Association Between Nursing Students' Self-Assessment and PerformancejangnoesaAinda não há avaliações
- Jadwal Kuliah Farmakologi SPDocumento1 páginaJadwal Kuliah Farmakologi SPjangnoesaAinda não há avaliações
- The Little Book of Hygge: Danish Secrets to Happy LivingNo EverandThe Little Book of Hygge: Danish Secrets to Happy LivingNota: 3.5 de 5 estrelas3.5/5 (400)
- Dapus Acak2Documento1 páginaDapus Acak2jangnoesaAinda não há avaliações
- Metlit Bab IIDocumento20 páginasMetlit Bab IIjangnoesaAinda não há avaliações
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNo EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureNota: 4.5 de 5 estrelas4.5/5 (474)
- Variables and An Operational DefinitionDocumento39 páginasVariables and An Operational DefinitionjangnoesaAinda não há avaliações
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNo EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryNota: 3.5 de 5 estrelas3.5/5 (231)
- Cdd161304-Manual Craftsman LT 1500Documento40 páginasCdd161304-Manual Craftsman LT 1500franklin antonio RodriguezAinda não há avaliações
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNo EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceNota: 4 de 5 estrelas4/5 (895)
- Achievement Test Science 4 Regular ClassDocumento9 páginasAchievement Test Science 4 Regular ClassJassim MagallanesAinda não há avaliações
- Team of Rivals: The Political Genius of Abraham LincolnNo EverandTeam of Rivals: The Political Genius of Abraham LincolnNota: 4.5 de 5 estrelas4.5/5 (234)
- Rekapan Belanja JKNDocumento5 páginasRekapan Belanja JKNAPOTEK PUSKESMAS MALEBERAinda não há avaliações
- Never Split the Difference: Negotiating As If Your Life Depended On ItNo EverandNever Split the Difference: Negotiating As If Your Life Depended On ItNota: 4.5 de 5 estrelas4.5/5 (838)
- EdExcel A Level Chemistry Unit 4 Mark Scheme Results Paper 1 Jun 2005Documento10 páginasEdExcel A Level Chemistry Unit 4 Mark Scheme Results Paper 1 Jun 2005MashiatUddinAinda não há avaliações
- The Emperor of All Maladies: A Biography of CancerNo EverandThe Emperor of All Maladies: A Biography of CancerNota: 4.5 de 5 estrelas4.5/5 (271)
- Esomeprazol Vs RabeprazolDocumento7 páginasEsomeprazol Vs RabeprazolpabloAinda não há avaliações
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNo EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaNota: 4.5 de 5 estrelas4.5/5 (266)
- 742210V01Documento2 páginas742210V01hakim_zadehAinda não há avaliações
- 03 - Air Ticket Request & Claim Form 2018Documento1 página03 - Air Ticket Request & Claim Form 2018Danny SolvanAinda não há avaliações
- ARI 700 StandardDocumento19 páginasARI 700 StandardMarcos Antonio MoraesAinda não há avaliações
- The Unwinding: An Inner History of the New AmericaNo EverandThe Unwinding: An Inner History of the New AmericaNota: 4 de 5 estrelas4/5 (45)
- Well Being Journal December 2018 PDFDocumento52 páginasWell Being Journal December 2018 PDFnetent00100% (1)
- ICT ContactCenterServices 9 Q1 LAS3 FINALDocumento10 páginasICT ContactCenterServices 9 Q1 LAS3 FINALRomnia Grace DivinagraciaAinda não há avaliações
- R. Raghunandanan - 6Documento48 páginasR. Raghunandanan - 6fitrohtin hidayatiAinda não há avaliações
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNo EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersNota: 4.5 de 5 estrelas4.5/5 (345)
- GEC PE 3 ModuleDocumento72 páginasGEC PE 3 ModuleMercy Anne EcatAinda não há avaliações
- PED16 Foundation of Inclusive Special EducationDocumento56 páginasPED16 Foundation of Inclusive Special EducationCHARESS MARSAMOLO TIZONAinda não há avaliações
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyNo EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyNota: 3.5 de 5 estrelas3.5/5 (2259)
- Thornburg Letter of RecDocumento1 páginaThornburg Letter of Recapi-511764033Ainda não há avaliações
- JIDMR SCOPUS Ke 4 Anwar MallongiDocumento4 páginasJIDMR SCOPUS Ke 4 Anwar Mallongiadhe yuniarAinda não há avaliações
- AD Oracle ManualDocumento18 páginasAD Oracle ManualAlexandru Octavian Popîrțac100% (2)
- Guia Laboratorio Refrigeración-2020Documento84 páginasGuia Laboratorio Refrigeración-2020soniaAinda não há avaliações
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNo EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreNota: 4 de 5 estrelas4/5 (1090)
- 134.4902.06 - DM4170 - DatasheetDocumento7 páginas134.4902.06 - DM4170 - DatasheetVinicius MollAinda não há avaliações
- RX Gnatus ManualDocumento44 páginasRX Gnatus ManualJuancho VargasAinda não há avaliações
- Zemoso - PM AssignmentDocumento3 páginasZemoso - PM AssignmentTushar Basakhtre (HBK)Ainda não há avaliações
- Man Wah Ranked As Top 10 Furniture Sources For U.S. MarketDocumento2 páginasMan Wah Ranked As Top 10 Furniture Sources For U.S. MarketWeR1 Consultants Pte LtdAinda não há avaliações
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)No EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Nota: 4.5 de 5 estrelas4.5/5 (121)
- UntitledDocumento2 páginasUntitledapi-236961637Ainda não há avaliações
- Cardiovascular SystemDocumento47 páginasCardiovascular SystemAtnasiya GadisaAinda não há avaliações
- Biomedical EngineeringDocumento5 páginasBiomedical EngineeringFranch Maverick Arellano Lorilla100% (1)
- Tool 10 Template Working Papers Cover SheetDocumento4 páginasTool 10 Template Working Papers Cover Sheet14. Đỗ Kiến Minh 6/5Ainda não há avaliações
- Functional Capacity Evaluation: Occupational Therapy's Role inDocumento2 páginasFunctional Capacity Evaluation: Occupational Therapy's Role inramesh babu100% (1)
- A Walk in The Physical - Christian SundbergDocumento282 páginasA Walk in The Physical - Christian SundbergKatie MhAinda não há avaliações
- Apport D Un Fonds de Commerce en SocieteDocumento28 páginasApport D Un Fonds de Commerce en SocieteJezebethAinda não há avaliações
- Linkage 2 Lab ReportDocumento25 páginasLinkage 2 Lab Reportapi-25176084883% (6)
- Food DirectoryDocumento20 páginasFood Directoryyugam kakaAinda não há avaliações