Escolar Documentos
Profissional Documentos
Cultura Documentos
Management of Adult Febrile Neutropenia: 15011500-10123 99 Street Edmonton, Alberta T5J 3H1
Enviado por
Tio Prima STítulo original
Direitos autorais
Formatos disponíveis
Compartilhar este documento
Compartilhar ou incorporar documento
Você considera este documento útil?
Este conteúdo é inapropriado?
Denunciar este documentoDireitos autorais:
Formatos disponíveis
Management of Adult Febrile Neutropenia: 15011500-10123 99 Street Edmonton, Alberta T5J 3H1
Enviado por
Tio Prima SDireitos autorais:
Formatos disponíveis
15011500-10123 99 Street Edmonton, Alberta T5J 3H1
Management of Adult Febrile Neutropenia
Quick summary of the management of adult febrile neutropenia:
1. Fever >38.3 x 1 or >38 for >1 hr. in a patient who has received chemotherapy in last month.
2. Neutrophils <0.5 or likely to fall to <0.5.
3. 1 + 2 = febrile neutropenia.
4. Assess for site of infection, culture blood and assess renal and liver function as well as for
septic shock.
5. Treat with IV ceftazidime 2g q 8h plus IV fluids.
6. Admit the patient and telephone the Tom Baker Medical Oncologist on call (403) 944-1110 or
the CCI Medical Oncologist on call (780 432-8771) for consultation. Call the Capital Health
Authoritys, Critical Care Line (780-413-4000) if septic shock is a concern or (403) 944-1110 in
Calgary.
Background: Febrile neutropenia is considered a medical emergency. The use of empiric broadspectrum antibiotics has significantly reduced the mortality and morbidity of this common
chemotherapy complication. Rapid assessment and institution of the appropriate antibiotics are of
paramount importance. A patient on chemotherapy should not wait in the ER for assessment for
an extended period of time. Ideally a system would be in place for the rapid identification of a
potential patient with febrile neutropenia who would then immediately have a CBC drawn and
urgent assessment by a health care professional.
The following are guidelines on the management of a patient with febrile neutropenia. Every
patient has a unique presentation and should be managed as such. Daily reassessments are
required to ensure that the patient is recovering satisfactorily.
Assistance: Please notify the on call medical oncologist when any patient presents with febrile
neutropenia. Please notify the responsible medical oncologist for any additional concerns relating
to the care of a patient with febrile neutropenia. Another useful resource would be the on call
infectious diseases specialist at the University of Alberta Hospital or Foothills Hospital.
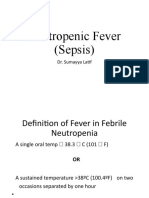
Fever: Fever is usually defined by a single oral temperature of >38.3 C or a sustained oral
temperature of >38.0 C for more than one hour. Patients are instructed to call telephone triage
or go to the nearest ER with any oral temperature >38.0 C.
9
Neutropenia: Neutropenia is defined by an ANC <0.5x10 cells/L or an ANC<1.0 with an expected
9
fall to <0.5x10 cells/L.
Assessment: A careful history and detailed examination is required for all patients suspected of
having febrile neutropenia. The assessment should include the following:
Mental status
Hydration status
Oral and pharyngeal mucosa
Skin including any indwelling IV sites
Respiratory system
Abdomen
AVOID rectal exam but include perirectal inspection for abscess
Cardiovascular system including signs of sepsis
Special considerations: beware of the possibility of meningitis, sinusitis, herpes simplex,
herpes zoster, thrush
Adult Febrile Neutropenia Protocol
March, 2008
Lab investigations: A complete hematological profile and chemistry profile should be done. The
latter is done to assess comorbidities, any end-organ effects of sepsis and to determine if any
antibiotic dose modifications or contraindications apply. These lab tests should include the
following:
CBC and differential
Transaminases, bilirubin, alkaline phosphatase
Electrolytes
Creatinine and urea
blood cultures
o aerobic and anaerobic
o peripheral and from any indwelling IV lines
urinalysis and urine culture (absence of pus cells on urinalysis does not rule out UTI in
the setting of neutropenia)
sputum gram stain and culture if productive
LP and CSF analysis should not be done routinely
Imaging investigations: Chest x-ray should be obtained even in the absence of pulmonary
symptoms or signs. Pulmonary infiltrates may not develop until the neutropenia begins to recover.
Thoracic CT has not been shown to improve outcomes in the absence of clinical pulmonary
abnormalities but can be considered in the setting of clinical abnormalities and a normal chest xray. Other imaging tests should be guided by the clinical picture.
Empiric antibiotic therapy: Seeding of the bloodstream by endogenous bacteria from the GI tract
is felt to be responsible for the majority of cases of febrile neutropenia. Many chemotherapy drugs
can have adverse effects on the mucosal barrier (i.e. mucositis). Blood cultures are positive in
about 30% of cases. Gram-positive organisms are isolated more commonly than gram-negative
organisms but the latter are associated with more severe infections including sepsis. Since febrile
neutropenia is considered a medical emergency with high mortality if untreated, empiric broadspectrum antibiotics must be administered immediately. Patients transferred from the ER to a
ward should already be receiving their antibiotics. Consider allergies, prior antibiotic history,
clinical picture and local flora as guides but the initial antibiotic therapy should be one of the
following broad spectrum regimens.
Broad spectrum antibiotics: The 2006 version of the CHA Bugs & Drugs provides an excellent
reference for the management of febrile neutropenia. A version is also available for regions
outside the Capital Health Authority (780-735-0007). Combination therapy is not clearly superior
to monotherapy in most circumstances. Ensure that appropriate dosing guidelines are followed
especially in the setting of renal dysfunction.
Monotherapy:
o Ceftazidime 2g IV q8h (standard regimen at ACB)
o Cefipime 2g IV q8h
o Imipenem 500mg IV q6h
o Meropenem 500 mg IV q6h
Combination therapy:
o Piperacillin-tazobactam 4.5 g IV q8h gentamicin 7mg/kg IV q24h or tobramycin
7mg/kg IV q24h or
Major -lactam allergy:
o Vancomycin 1g IV q12h and one of
Gentamicin 7mg/kg IV q24h
Tobramycin 7mg/kg IV q24h
Ciprofloxacin 400 mg IV q8-14 hours
Adult Febrile Neutropenia Protocol
March, 2008
Empiric vancomycin should not be used routinely but should be considered in the
following circumstances: obvious IV catheter/tunnel infection, positive gram-positive
culture with organism not yet identified, known colonization with MRSA or penicillinresistant S. pneumoniae, hypotension/shock, quinolone antibiotic prophylaxis. It should
be stopped on day 3-5 if culture reveals pathogens that dont require vancomycin.
Duration of antibiotic therapy: The duration of antibiotic coverage depends on the early clinical
course and the results of any cultures -especially blood cultures. If a definite source of infection is
identified such as a UTI or pneumonia, the treatment duration should be appropriate for those
infections. If a pathogen is identified in the blood cultures-especially gram negative bacilligenerally a 10-14 day course of antibiotics is recommended. If no source is identified either
clinically or on blood cultures, antibiotics can be stopped if the patient is afebrile and the ANC has
9
recovered to 0.5x10 cells/L although some recommend a minimum of 7 days of therapy. If the
fever resolves but the ANC is still low there is no consensus on duration of antibiotics but a
reasonable strategy would be to continue the antibiotics for 5-10 days depending on the clinical
picture. If the still neutropenic patient is unstable or has significant mucositis, antibiotics should be
continued for at least 14 days even if afebrile.
Colony stimulating factors: Granulocyte colony stimulating factor (GCSF) can decrease the
duration of neutropenia, fever and hospitalization but these benefits are modest and mortality is
unaffected. They can be considered in the hospitalized patient with pneumonia,
hypotension/sepsis, organ dysfunction or a patient on a regimen that is known to cause
prolonged neutropenia. Prophylactic GCSF is outside of the scope of this document.
Step-down to oral antibiotics: Patients who have rapidly improved on IV antibiotics and who are
afebrile, stable and no longer neutropenic can be switched to an appropriate oral regimen for the
balance of the chosen antibiotic duration. If these patients are stable, have no unmanaged
comorbidities and have a safe and reliable home environment they can also be discharged. If the
patient has been on a prophylactic quinolone prior to the FN episode, these should be avoided on
discharge. Ciprofloxacin (750mg BID) plus Clavulin (875mg BID) or Levofloxacin 500mg OD are
reasonable step-down regimens. Culture and sensitivity results can also guide therapy. These
results must be reviewed prior to discharge.
Persisting fever: Be aware that fever in the patient with cancer can be due to the disease itself but
a persisting fever in the neutropenic patient usually suggests an ongoing infection not adequately
treated by the current antibiotic regimen. The clinical picture must be thoroughly re-evaluated.
Blood or other culture results should be verified and repeat cultures obtained if fever persists for
more than 3 days. Empirically, vancomycin (1g IVq12h) is usually added at this point. Fungal
cultures should be obtained and empiric antifungal therapy is recommended if fever persists
beyond 5 days of appropriate antibacterial therapy. Please consult a medical oncologist or
infectious disease specialist for advice regarding the most appropriate agent. Be aware that viral
infections can also commonly occur in the patient with febrile neutropenia. Severe oral herpes
can look like severe mucositis. Viral swabs and empiric antiviral therapy should be considered.
Special circumstances: Patients with febrile neutropenia can occasionally present in septic shock
or have other critical care issues. These patients should be discussed with the medical oncologist
as soon as possible to determine if critical care is appropriate. Patients on potentially curative or
salvage regimens must be managed as aggressively as possible. It may be appropriate to contact
the nearest critical care specialist. It may be challenging to determine the appropriate level of
care for patients on palliative regimens and therefore advice should be sought in this regard from
the attending or on call medical oncologist.
Central venous catheter and tunnel infections as well as septic thrombosis, endocarditis and
osteomyelitis are special circumstances beyond the scope of this document and specific advice
Adult Febrile Neutropenia Protocol
March, 2008
from the appropriate specialist should be obtained. This also applies to any other situation not
covered here. A medical oncologist can provide direction as well.
Low risk febrile neutropenia: Mortality and morbidity from the appropriately managed case of
febrile neutropenia is very low. Inpatient management is considered the standard of care. There
is, however, a subpopulation of FN patients felt to be a very low risk of complications who may
benefit from outpatient management. Outpatient management should be reserved for centres with
considerable experience in identifying and managing this low risk group. At the CCI, an outpatient
program is currently being developed.
Você também pode gostar
- Onc EmergenciesDocumento4 páginasOnc EmergencieslanamdAinda não há avaliações
- BCCA Febrile Neutropenia GuidelinesDocumento2 páginasBCCA Febrile Neutropenia GuidelinesdenokayuMRAinda não há avaliações
- Bowels Open 6 Times Per 24 Hours: Document ControlDocumento7 páginasBowels Open 6 Times Per 24 Hours: Document ControlKeith PohlAinda não há avaliações
- Sumit Bhutani: Neutropenic FeverDocumento46 páginasSumit Bhutani: Neutropenic Feversumit240677Ainda não há avaliações
- Screenshot 2020-03-20 at 08.25.44 PDFDocumento10 páginasScreenshot 2020-03-20 at 08.25.44 PDFMiguel Angel Palacios FloresAinda não há avaliações
- Allergy Immunology (3) (MedicalBooksVN - Com)Documento9 páginasAllergy Immunology (3) (MedicalBooksVN - Com)malbertal1Ainda não há avaliações
- Pulmonary Infection GuidelinesDocumento16 páginasPulmonary Infection GuidelinesFawad AhmedAinda não há avaliações
- GDL Fever OncologyDocumento16 páginasGDL Fever OncologyZaini GhazaliAinda não há avaliações
- Dengue 15 Minutes FlipchartDocumento18 páginasDengue 15 Minutes FlipchartIsa MunsterAinda não há avaliações
- Stop COVID-19 management Handbook by Medical student Ahmed ElwahshDocumento13 páginasStop COVID-19 management Handbook by Medical student Ahmed Elwahshamr elfaresyAinda não há avaliações
- Pediatrics MS WordDocumento13 páginasPediatrics MS WordSamhitha SharmaAinda não há avaliações
- Oncologic Emergencies: SepsisDocumento4 páginasOncologic Emergencies: SepsisPilar KrammAinda não há avaliações
- Case 013: Fever in A Cirrhotic PatientDocumento5 páginasCase 013: Fever in A Cirrhotic PatientFitri 1997Ainda não há avaliações
- Neutropenic Fever Empiric TherapyDocumento5 páginasNeutropenic Fever Empiric TherapyRominaPulvermüllerSalvatierraAinda não há avaliações
- General Medicine SEQs SolvedDocumento33 páginasGeneral Medicine SEQs SolvedMajid Ahmed FareaAinda não há avaliações
- Role of Anticoagulant in Treatment Protocol of COVID 19 PatientsDocumento6 páginasRole of Anticoagulant in Treatment Protocol of COVID 19 PatientsBasma ElshazlyAinda não há avaliações
- Blood Transfusion PDFDocumento10 páginasBlood Transfusion PDFjamesAinda não há avaliações
- Passmedicine Feb 2018Documento1.896 páginasPassmedicine Feb 2018مصطفى محمد جواد كاظمAinda não há avaliações
- PeritonitisDocumento28 páginasPeritonitisdea_p27Ainda não há avaliações
- Cleveland Clinic Journal of Medicine 2013 BARON 354 9Documento6 páginasCleveland Clinic Journal of Medicine 2013 BARON 354 9Stephanie PlascenciaAinda não há avaliações
- Pneumonia: Recent Evidence Based UpdatesDocumento30 páginasPneumonia: Recent Evidence Based UpdatesAli AzamAinda não há avaliações
- Neutropenic SepsisDocumento38 páginasNeutropenic SepsisYS NateAinda não há avaliações
- Cefotaxime Drug Class, Uses, Side EffectsDocumento3 páginasCefotaxime Drug Class, Uses, Side EffectsKristi WrayAinda não há avaliações
- Saima Abbas M.D Infectious Diseases Fellow-PGY5 DocumentDocumento74 páginasSaima Abbas M.D Infectious Diseases Fellow-PGY5 DocumentJuliyanti FuAinda não há avaliações
- Guidelines For The Management of Acute Stroke: Emergency DepartmentDocumento10 páginasGuidelines For The Management of Acute Stroke: Emergency DepartmentUhuebor DavidAinda não há avaliações
- Pathology I Review 10Documento30 páginasPathology I Review 10i_areinamoAinda não há avaliações
- Typhoid GuidelinesDocumento3 páginasTyphoid GuidelinesMuthia Rahma AninditaAinda não há avaliações
- Clinical Practice Guideline On Neonatal Sepsis: Summarized by Dr. Catherine Chua October 2012Documento3 páginasClinical Practice Guideline On Neonatal Sepsis: Summarized by Dr. Catherine Chua October 2012Joey CuayoAinda não há avaliações
- Pediatric Hematology Oncology Ward Officer HandbookDocumento40 páginasPediatric Hematology Oncology Ward Officer HandbookLetchumana KrishnanAinda não há avaliações
- ΕΜΠΥΡΕΤΟ EKPADocumento25 páginasΕΜΠΥΡΕΤΟ EKPAElenaAinda não há avaliações
- Case Presentation MineDocumento30 páginasCase Presentation MineAshman AshAinda não há avaliações
- Medical Care: "Microbiology, Epidemiology, Clinical Manifestations, and Diagnosis of Leptospirosis"Documento5 páginasMedical Care: "Microbiology, Epidemiology, Clinical Manifestations, and Diagnosis of Leptospirosis"Lyra LorcaAinda não há avaliações
- CAP CURB-65 GuidelinesDocumento1 páginaCAP CURB-65 GuidelinesAndy LoakAinda não há avaliações
- San Pedro Hospital Case Vignette on Pulmonary TBDocumento7 páginasSan Pedro Hospital Case Vignette on Pulmonary TBShareen Joyce AgbayaniAinda não há avaliações
- Acute Colitis Protocol GuidelineDocumento8 páginasAcute Colitis Protocol GuidelineKhurram NadeemAinda não há avaliações
- Neutropenic Sepsis-Tls-Anaphylaxis-ExtravasationDocumento40 páginasNeutropenic Sepsis-Tls-Anaphylaxis-ExtravasationSA NodeAinda não há avaliações
- 2009-10-16 Current Antiviral Recommendations For Influenza TreatmentDocumento2 páginas2009-10-16 Current Antiviral Recommendations For Influenza Treatmenttamiprior5294Ainda não há avaliações
- Febrile Neutropenia ArunDocumento40 páginasFebrile Neutropenia ArunArun GeorgeAinda não há avaliações
- 2 - BM Suppression and NeutropeniaDocumento36 páginas2 - BM Suppression and NeutropeniaRobert ChristevenAinda não há avaliações
- JURNALDocumento33 páginasJURNALrike aprilianaAinda não há avaliações
- JURNALDocumento33 páginasJURNALrike aprilianaAinda não há avaliações
- Urinary Tract InfectionsDocumento6 páginasUrinary Tract InfectionswiraAinda não há avaliações
- Current Recommendations For The Management of Severe Sepsis & Septic ShockDocumento34 páginasCurrent Recommendations For The Management of Severe Sepsis & Septic ShockAmit KochetaAinda não há avaliações
- INP CU 10 GlomeruloDocumento5 páginasINP CU 10 GlomeruloMichelle Gliselle Guinto MallareAinda não há avaliações
- Febrile Neutropenia: Dr. Abdelkareem Wedaa EltohamyDocumento31 páginasFebrile Neutropenia: Dr. Abdelkareem Wedaa Eltohamyjehemir100% (1)
- Critically Ill Elderly Man with Disseminated Candidiasis Following Colonic SurgeryDocumento20 páginasCritically Ill Elderly Man with Disseminated Candidiasis Following Colonic SurgerysummiyaAinda não há avaliações
- Management of SepsisDocumento34 páginasManagement of SepsisTamim IshtiaqueAinda não há avaliações
- Guidelines For First-Line Empirical Antibiotic Therapy in AdultsDocumento1 páginaGuidelines For First-Line Empirical Antibiotic Therapy in AdultsAnonymous s4yarxAinda não há avaliações
- Issues in The Diagnosis and Management of Thombocytopenic DisordersDocumento45 páginasIssues in The Diagnosis and Management of Thombocytopenic Disorderspeter_mrAinda não há avaliações
- Pediatric Hematology Oncology CaseDocumento107 páginasPediatric Hematology Oncology CaseSayyed Ahmad KhursheedAinda não há avaliações
- Amikacin antibiotic for urinary tract infectionsDocumento17 páginasAmikacin antibiotic for urinary tract infectionsMc Crister SilangAinda não há avaliações
- Common ConditionsDocumento58 páginasCommon ConditionsdrakeAinda não há avaliações
- HPB Adverse Transfusion ReactionDocumento26 páginasHPB Adverse Transfusion ReactionFransiscus RivaldyAinda não há avaliações
- Managing Pregnant COVID PatientsDocumento17 páginasManaging Pregnant COVID Patientsfariska amanizataAinda não há avaliações
- Pediatric Hematology Oncology Ward Officer HandbookDocumento40 páginasPediatric Hematology Oncology Ward Officer HandbookAnonymous FSUnLYr4yAinda não há avaliações
- Pharmacological Therapies for NursesDocumento99 páginasPharmacological Therapies for NurseslAinda não há avaliações
- Lepto CPGDocumento51 páginasLepto CPGmajestymadrigalAinda não há avaliações
- Clinical Features: - Initial Symptoms in Patients With MeningitisDocumento12 páginasClinical Features: - Initial Symptoms in Patients With Meningitisyuii_48Ainda não há avaliações
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingAinda não há avaliações
- Espi 2018Documento38 páginasEspi 2018Tio Prima SAinda não há avaliações
- HIV in PregnancyDocumento10 páginasHIV in PregnancytioAinda não há avaliações
- Pekanbaru - Medan (7 Orang Rsu. Puri Husada)Documento3 páginasPekanbaru - Medan (7 Orang Rsu. Puri Husada)Tio Prima SAinda não há avaliações
- Dengue ResourcesDocumento1 páginaDengue Resourcesdamag3Ainda não há avaliações
- Departemen Ilmu Gizi FK USU MEDAN Upper Abdominal Discomfort Causes and DietDocumento25 páginasDepartemen Ilmu Gizi FK USU MEDAN Upper Abdominal Discomfort Causes and DietTio Prima SAinda não há avaliações
- PIS Spontan Terkait Gangguan HematologiDocumento17 páginasPIS Spontan Terkait Gangguan HematologitioAinda não há avaliações
- GDS-K25 Bahan KuliahDocumento30 páginasGDS-K25 Bahan KuliahLanna HarumiyaAinda não há avaliações
- (Kecacingan Faktor Resiko) 964 1916 1 SMDocumento16 páginas(Kecacingan Faktor Resiko) 964 1916 1 SMRenaldi RamadhaniAinda não há avaliações
- (Kecacingan Faktor Resiko) 964 1916 1 SMDocumento16 páginas(Kecacingan Faktor Resiko) 964 1916 1 SMRenaldi RamadhaniAinda não há avaliações
- Cover Letters WebDocumento10 páginasCover Letters WebMinh HoangAinda não há avaliações
- Dengue Hemorrhagic Fever With Special Emphasis On ImmunopathogenesisDocumento12 páginasDengue Hemorrhagic Fever With Special Emphasis On ImmunopathogenesisHadley AuliaAinda não há avaliações
- Varicella-Zoster Virus: Virology and Clinical ManagementDocumento19 páginasVaricella-Zoster Virus: Virology and Clinical ManagementTio Prima SAinda não há avaliações
- 8903160Documento3 páginas8903160Tio Prima SAinda não há avaliações
- Jurnal DBD 3 2010Documento10 páginasJurnal DBD 3 2010Sukma ArdiAinda não há avaliações
- 3.2. Mekanisme Trombositopenia Dan Kelainan Koagulasi Pada Infeksi DenguetDocumento26 páginas3.2. Mekanisme Trombositopenia Dan Kelainan Koagulasi Pada Infeksi DenguetTio Prima SAinda não há avaliações
- Guest Essay Envisioning A Sustainable Society: Is A Trademark Used Herein Under LicenseDocumento4 páginasGuest Essay Envisioning A Sustainable Society: Is A Trademark Used Herein Under LicenseTio Prima SAinda não há avaliações
- 8903160Documento3 páginas8903160Tio Prima SAinda não há avaliações
- Typhoid Fever Cellular ModelDocumento7 páginasTyphoid Fever Cellular ModelTio Prima SAinda não há avaliações
- Sustainability LinksDocumento2 páginasSustainability LinksTio Prima SAinda não há avaliações
- Pathogenesis Typhoid Fever PDFDocumento7 páginasPathogenesis Typhoid Fever PDFAry Nahdiyani Amalia100% (1)
- Current Progress in Dengue Vaccines: Review Open AccessDocumento9 páginasCurrent Progress in Dengue Vaccines: Review Open AccessTio Prima SAinda não há avaliações
- Diagnosing Fever of Unknown OriginDocumento6 páginasDiagnosing Fever of Unknown OriginTio Prima SAinda não há avaliações
- EScholarship UC Item 3p2984p2Documento3 páginasEScholarship UC Item 3p2984p2Tio Prima SAinda não há avaliações
- Distribusi Dan Faktor Resiko Lingkungan Penularan Leptospirosis Dikabupaten Demak, Jawa TengahDocumento9 páginasDistribusi Dan Faktor Resiko Lingkungan Penularan Leptospirosis Dikabupaten Demak, Jawa TengahTio Prima SAinda não há avaliações
- How To Guide To Writing An EssayDocumento11 páginasHow To Guide To Writing An EssaysuckmydickyyAinda não há avaliações
- ICAS Sustainability FAQsDocumento2 páginasICAS Sustainability FAQsTio Prima SAinda não há avaliações
- Environmental Factors Influence Leptospirosis IncidenceDocumento8 páginasEnvironmental Factors Influence Leptospirosis IncidenceTio Prima SAinda não há avaliações
- Mice: - /-+/ - Hematopoiesis, and Impaired Progenitor Function in Anemia, Thrombocytopenia, Leukocytosis, ExtramedullaryDocumento9 páginasMice: - /-+/ - Hematopoiesis, and Impaired Progenitor Function in Anemia, Thrombocytopenia, Leukocytosis, ExtramedullaryTio Prima SAinda não há avaliações
- Els Essay Outline1Documento3 páginasEls Essay Outline1api-246498555Ainda não há avaliações
- JurnalDocumento12 páginasJurnalIrara RaAinda não há avaliações
- Updated Antibiotic Pediatric Dosing 2020Documento2 páginasUpdated Antibiotic Pediatric Dosing 2020Wan Nur AdilahAinda não há avaliações
- Optimal Management of Chemotherapy-Related Adverse Events: Review ArticleDocumento9 páginasOptimal Management of Chemotherapy-Related Adverse Events: Review Articlekang soon cheolAinda não há avaliações
- Neutropenic FeverDocumento15 páginasNeutropenic Feverapi-3712326Ainda não há avaliações
- Treatment of Fever in Neutropenia in Pediatric Oncology PatientsDocumento6 páginasTreatment of Fever in Neutropenia in Pediatric Oncology PatientsRaíla SoaresAinda não há avaliações
- Febrile Neutropenia Topic DiscussionDocumento42 páginasFebrile Neutropenia Topic Discussionapi-647904873Ainda não há avaliações
- Treating Febrile NeutropeniaDocumento2 páginasTreating Febrile NeutropeniaAlvy SyukrieAinda não há avaliações
- Oncology Supportive Care Update BCPS 2021-1Documento106 páginasOncology Supportive Care Update BCPS 2021-1Mr.ShazAinda não há avaliações
- Antibiotic Guidelines (2020) - 0Documento55 páginasAntibiotic Guidelines (2020) - 0yudhit bessieAinda não há avaliações
- Approaches To Febrile Neutropenia 2011 IDSA-ECIL GuidelinesDocumento24 páginasApproaches To Febrile Neutropenia 2011 IDSA-ECIL GuidelinesHusein AssagafAinda não há avaliações
- Guias F y N SLIPEDocumento29 páginasGuias F y N SLIPERocio GAinda não há avaliações
- CLINICAL HAEMATOLOGY MCQsDocumento149 páginasCLINICAL HAEMATOLOGY MCQsHashim Ahmad100% (2)
- Extended Infusion of - Lactams Significantly Reduces Mortality A - 2023 - EcliniDocumento16 páginasExtended Infusion of - Lactams Significantly Reduces Mortality A - 2023 - Eclinironaldquezada038Ainda não há avaliações
- WHO MHP HPS EML 2021.03 EngDocumento48 páginasWHO MHP HPS EML 2021.03 EngEddy VarillasAinda não há avaliações
- Health PEI: Provincial Antibiotic Advisory Team Empiric Antibiotic Treatment Guidelines For Sepsis Syndromes in AdultsDocumento10 páginasHealth PEI: Provincial Antibiotic Advisory Team Empiric Antibiotic Treatment Guidelines For Sepsis Syndromes in AdultsFarmasi RSUD Kramat JatiAinda não há avaliações
- PENATALAKSANAAN INFEKSI PADA PASIEN KANKERDocumento18 páginasPENATALAKSANAAN INFEKSI PADA PASIEN KANKERSuci Fitriani SammuliaAinda não há avaliações
- ICON 2016 Febrile Neutropenia GuidelinesDocumento34 páginasICON 2016 Febrile Neutropenia GuidelinesTor Ja100% (1)
- Febrile NeutropeniaDocumento18 páginasFebrile Neutropeniajames njengaAinda não há avaliações
- Infections in The Neutropenic Patient-2001Documento27 páginasInfections in The Neutropenic Patient-2001Raisa_90Ainda não há avaliações
- Evaluation of The Patient With FeverDocumento4 páginasEvaluation of The Patient With Feverabu ubaidahAinda não há avaliações
- Sepsis GuidelinesDocumento1 páginaSepsis GuidelinesYezenashAinda não há avaliações
- Febrile Neutropenia GuidelineDocumento8 páginasFebrile Neutropenia GuidelineAslesa Wangpathi PagehgiriAinda não há avaliações
- Pan-London Haemato-Oncology Clinical GuidelinesDocumento37 páginasPan-London Haemato-Oncology Clinical GuidelinesMd. Tanvir AhammedAinda não há avaliações
- Case Presentation: Cagayan Valley Medical CenterDocumento57 páginasCase Presentation: Cagayan Valley Medical CenterGian PagadduAinda não há avaliações
- Fever in Children With ChemoteraphyDocumento23 páginasFever in Children With ChemoteraphyImanuel Far-FarAinda não há avaliações
- Asco GCSF 2015Documento16 páginasAsco GCSF 2015Alvy SyukrieAinda não há avaliações
- Wild 2017Documento7 páginasWild 2017fallenczarAinda não há avaliações
- CPG Rational Antibiotic Utilisation in Selected Paediatric ConditionsDocumento37 páginasCPG Rational Antibiotic Utilisation in Selected Paediatric ConditionsziggyshahdustAinda não há avaliações
- Application of The MASCC and CISNE Risk-Strati Fication Scores To Identify Low-Risk Febrile Neutropenic Patients in The Emergency DepartmentDocumento10 páginasApplication of The MASCC and CISNE Risk-Strati Fication Scores To Identify Low-Risk Febrile Neutropenic Patients in The Emergency DepartmentwiraAinda não há avaliações
- Febrile Neutropenia: Multinational Association For Supportive Care in Cancer (MASCC)Documento4 páginasFebrile Neutropenia: Multinational Association For Supportive Care in Cancer (MASCC)radwika anty100% (1)
- Neutropenic Fever Empiric TherapyDocumento5 páginasNeutropenic Fever Empiric TherapyRominaPulvermüllerSalvatierraAinda não há avaliações